Validating Macronutrient Intake: A Comprehensive Guide to Dietary Assessment Methods for Research and Drug Development
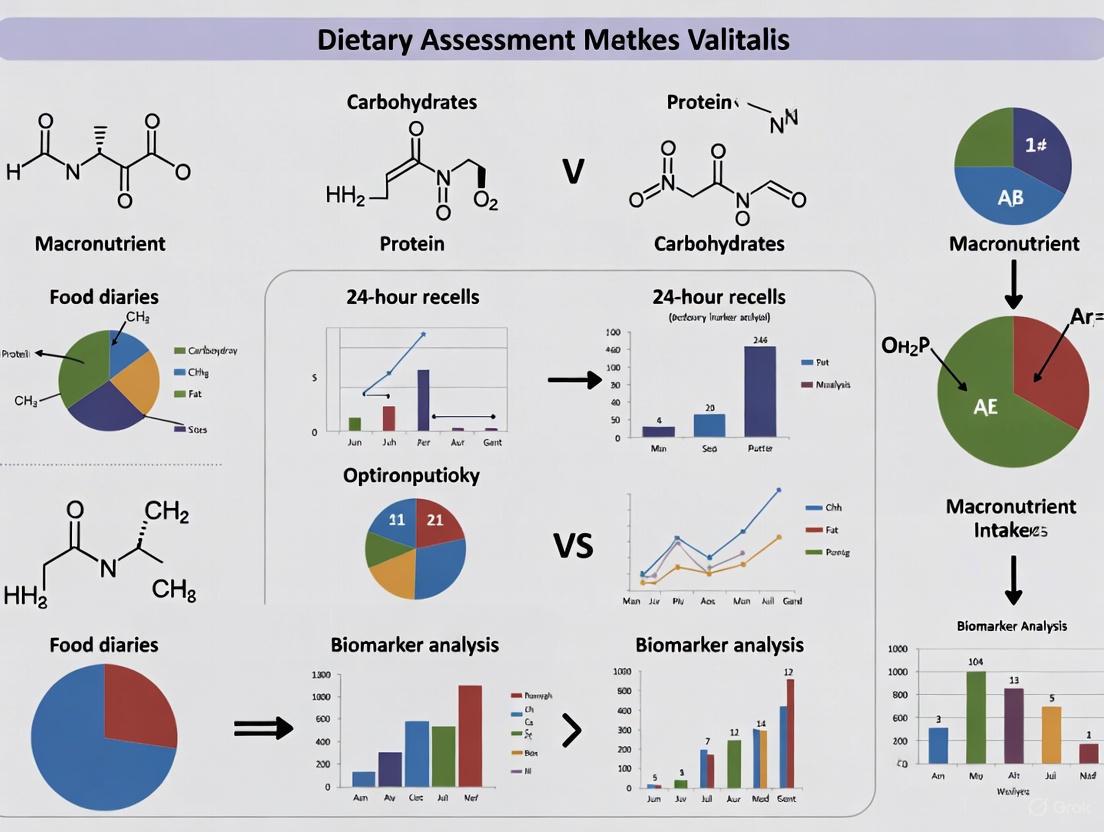
This article provides a systematic review of contemporary dietary assessment methodologies for validating macronutrient intake, tailored for researchers and drug development professionals.
Validating Macronutrient Intake: A Comprehensive Guide to Dietary Assessment Methods for Research and Drug Development
Abstract
This article provides a systematic review of contemporary dietary assessment methodologies for validating macronutrient intake, tailored for researchers and drug development professionals. It explores the evolution from traditional, error-prone methods to advanced artificial intelligence and biomarker-based approaches. The content covers foundational principles, practical applications of novel technologies, strategies to overcome common validation challenges, and comparative analyses of method accuracy. By synthesizing recent evidence from validation studies and meta-analyses, this guide aims to equip professionals with the knowledge to select appropriate methodologies, interpret validation data critically, and implement robust dietary assessment protocols in clinical and research settings to enhance data reliability in nutrition-related studies and pharmaceutical development.
Foundations of Dietary Assessment: Understanding Traditional Methods and Their Limitations in Macronutrient Validation
The Critical Role of Accurate Macronutrient Data in Clinical Research and Drug Development
Accurate macronutrient data serves as the cornerstone of high-quality clinical research, particularly in studies investigating the links between diet, health outcomes, and therapeutic efficacy. In the context of drug development, precise quantification of carbohydrate, protein, and fat intake is essential for understanding how nutritional status influences drug metabolism, patient responsiveness, and treatment outcomes. The integrity of this data directly impacts the validity of research findings and subsequent public health recommendations. Despite technological advancements, significant challenges persist in dietary assessment methodology, with studies consistently revealing systematic underestimation of energy and macronutrient intake across various assessment tools [1]. Recent research demonstrates that even when following identical dietary guidelines, the degree of food processing significantly impacts weight loss and body composition outcomes, underscoring the critical importance of data quality beyond basic macronutrient matching [2]. This application note provides a comprehensive framework for validating macronutrient data in clinical research settings, featuring structured protocols, analytical tools, and evidence-based methodologies to enhance data integrity across study designs.
Quantitative Landscape: Current Evidence on Macronutrient Assessment Accuracy
Table 1: Validation Metrics for Dietary Assessment Methods from Recent Evidence
| Assessment Method | Energy Validation (vs. Reference) | Macronutrient Correlation | Key Limitations | Context of Validation |
|---|---|---|---|---|
| AI-Based Methods | Correlation >0.7 in 6/13 studies [3] | Correlation >0.7 for macronutrients in 6/13 studies [3] | Moderate risk of bias in 61.5% of studies; mostly preclinical settings [3] | Systematic review of 13 studies (2017-2024) [3] |
| Dietary Record Apps | Pooled effect: -202 kcal/d (95% CI: -319, -85) [1] | Carbohydrates: -18.8 g/d; Fat: -12.7 g/d; Protein: -12.2 g/d [1] | High heterogeneity (I²=72%); learning effects not controlled [1] | Meta-analysis of 11-14 studies (2013-2019) [1] |
| Standardized Diet Histories | Moderate-good agreement for specific nutrients (kappa K=0.48-0.68) [4] | Varies by nutrient and population | Recall bias, social desirability bias, interviewer effects [4] | Eating disorder outpatient clinic (n=13) [4] |
| Controlled Feeding Trials | Direct measurement via provided diets [2] | Direct control and manipulation | High resource burden; limited generalizability | RCT comparing UPF vs. MPF diets (n=55) [2] |
Impact of Data Quality on Clinical Outcomes
The UPDATE randomized controlled trial provides compelling evidence about how data quality and food characterization beyond basic macronutrients significantly impact clinical outcomes. When diets were matched according to the UK Eatwell Guide standards, the minimally processed food (MPF) diet resulted in significantly greater weight loss (-2.06% vs. -1.05%, P=0.024) and superior improvements in body composition compared to the ultra-processed food (UPF) diet, despite nearly identical macronutrient profiles [2]. This finding has profound implications for drug development trials where weight changes might confound assessment of therapeutic efficacy. Additionally, the MPF diet led to significantly greater reductions in fat mass (-0.98 kg, P=0.004), body fat percentage (-0.76%, P=0.010), and triglycerides (-0.25 mmol l⁻¹, P=0.004) compared to the UPF diet [2]. These outcomes demonstrate that conventional macronutrient tracking alone is insufficient for predicting metabolic responses and that the quality and processing characteristics of food must be incorporated into high-quality nutritional assessment.
Methodological Framework: Protocols for Macronutrient Validation
Protocol 1: Controlled Feeding Trial Design for Macronutrient Validation
Objective: To establish causal relationships between precisely controlled macronutrient interventions and clinical outcomes while minimizing participant reporting bias.
Experimental Workflow:
Procedural Details:
- Participant Selection: Recruit adults with BMI ≥25 to <40 kg/m² and habitual ultra-processed food intake ≥50% of calories to ensure relevance to target populations [2]
- Dietary Protocol Development: Formulate both experimental and control diets to adhere to national dietary guidelines (e.g., UK Eatwell Guide) with careful matching of presented energy density, macronutrients, and fiber while varying only the degree of food processing [2]
- Blinding and Compliance: Implement single-blinding where participants are unaware of the primary outcome being measured; use dietitian consultations to enhance adherence and monitor compliance through regular check-ins [5]
- Outcome Assessment: Measure primary outcome (percent weight change) and secondary outcomes (body composition, cardiometabolic biomarkers, appetite measures) at baseline and 8-week endpoints using standardized protocols and calibrated equipment [2]
Key Quality Controls:
- Use identical nutrient analysis software/databases for both diet development and assessment
- Maintain diet consistency through centralized food preparation or detailed provision protocols
- Implement quality control checks for anthropometric measurements across all study timepoints
Protocol 2: AI-Assisted Dietary Assessment Validation Framework
Objective: To validate artificial intelligence-based dietary intake assessment (AI-DIA) methods against traditional dietary assessment and biomarker reference standards.
Experimental Workflow:
Procedural Details:
- Technology Selection: Choose AI-DIA methods incorporating deep learning (46.2% of validated methods) or machine learning (15.3%) approaches for food recognition, portion size estimation, and nutrient analysis [3]
- Reference Standards: Employ multiple reference standards including weighed food records, 24-hour recalls, and biomarkers (doubly labeled water for energy, urinary nitrogen for protein) to address different types of measurement error [1]
- Study Settings: Conduct validation in both preclinical (controlled) and clinical (free-living) settings to assess performance across different conditions; 61.5% of current evidence comes from preclinical settings [3]
- Statistical Analysis: Calculate correlation coefficients (target >0.7 for macronutrients), mean differences, error decomposition, and appropriate agreement statistics (ICC, kappa) based on the reference standard used [3] [1]
Key Quality Controls:
- Control for order effects by randomizing the sequence of assessment methods
- Account for learning effects with adequate training and practice sessions
- Ensure identical nutrient databases between compared methods when evaluating technology performance alone
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagent Solutions for Macronutrient Validation Research
| Category | Specific Tool/Solution | Function in Macronutrient Research | Evidence Base |
|---|---|---|---|
| AI-Based Dietary Assessment | Food Recognition Assistance and Nudging Insights [3] | Automated food identification and portion size estimation from images | Validation studies showing correlation >0.7 for energy and macronutrients [3] |
| Controlled Diet Formulation | Eatwell Guide-Compliant Diet Patterns [2] | Standardized reference diets for intervention studies | RCT demonstrating significant clinical differences between MPF and UPF versions [2] |
| Biomarker Reference Methods | Doubly Labeled Water (DLW) [1] | Objective measure of total energy expenditure for energy intake validation | Recommended as reference standard in validation studies [1] |
| Body Composition Analysis | Bioelectrical Impedance Analysis [2] | Tracking changes in fat mass, muscle mass, and body water in response to interventions | Detected significant differences between diet groups in RCT [2] |
| Nutrient Database Management | Standardized Food Composition Tables [1] | Consistent nutrient calculation across assessment methods | Reduces heterogeneity in validation studies (I² from 72% to 0%) [1] |
| Dietary Intake Software | GB HealthWatch, mediPIATTO [3] | Traditional dietary assessment with comprehensive nutrient analysis | Used as comparators in AI-DIA validation studies [3] |
Advanced Applications: Integrating Precision Nutrition into Clinical Trials
Protocol 3: Personalized Nutrition Approach for Clinical Trial Stratification
Objective: To implement nutrigenomic and metabolomic profiling for participant stratification in clinical trials, enhancing detection of intervention effects through reduced inter-individual variability.
Methodological Framework:
Procedural Details:
- Participant Characterization: Collect genomic data (nutrient-related polymorphisms), pre-intervention metabolomic profiles, gut microbiome composition, and baseline response tests (postprandial glucose and triglyceride measurements) [6]
- Stratification Algorithm: Apply machine learning algorithms to identify clusters of participants with similar metabolic characteristics and predicted nutritional responses based on the PREDICT-1 study methodology (achieving r=0.77 for glycemic response prediction) [6]
- Trial Design: Incorporate stratified randomization to ensure balanced representation of different nutritional response phenotypes across study arms, or intentionally enrich for specific subgroups most likely to respond to the nutritional intervention
- Outcome Analysis: Conduct both intention-to-treat analyses and pre-specified subgroup analyses based on nutritional phenotypes to identify heterogeneous treatment effects
Implementation Considerations:
- The heritability of postprandial blood glucose responses is approximately 48%, highlighting the significant influence of genetic factors on nutritional responses [6]
- Integrate continuous glucose monitors and other wearable sensors for real-time response monitoring in free-living participants
- Plan for sufficient sample size to power subgroup analyses, as nutritional response clusters may represent smaller proportions of the general population
The critical role of accurate macronutrient data in clinical research and drug development demands rigorous validation frameworks, appropriate technology selection, and careful attention to methodological details. Evidence from controlled feeding trials demonstrates that even with matched macronutrient profiles, food processing characteristics significantly influence clinical outcomes including weight loss, body composition, and cardiometabolic risk factors [2]. Emerging technologies such as AI-based dietary assessment show promise with correlation coefficients exceeding 0.7 for energy and macronutrients in nearly half of validation studies, though concerns about bias and predominance of preclinical evidence remain [3]. Traditional dietary apps consistently demonstrate underestimation of energy (-202 kcal/d) and macronutrient intake, highlighting the need for improved assessment methods [1]. The integration of precision nutrition approaches—incorporating genetic, metabolic, and microbiome profiling—offers exciting opportunities to reduce variability and enhance signal detection in nutrition-focused clinical trials [6]. By implementing the structured protocols, validation methodologies, and analytical frameworks presented in this application note, researchers can significantly strengthen the quality and impact of macronutrient data in clinical research and drug development programs.
Accurate assessment of dietary intake is fundamental to nutritional epidemiology, clinical nutrition, and public health policy. The validity of data linking diet to health outcomes and the effectiveness of dietary interventions hinges on the precision of the methods used to measure nutritional exposure [7]. Among the most established dietary assessment tools are the traditional methods: food records, 24-hour dietary recalls (24HR), and food frequency questionnaires (FFQs). Each method possesses distinct strengths, limitations, and optimal applications, particularly in the context of macronutrient intake validation research [7] [8].
This systematic review synthesizes current evidence on these three cornerstone methodologies. It provides a comparative analysis of their utility in measuring energy and macronutrient intake, detailed experimental protocols for their application, and visual workflows to guide researchers in selecting and implementing the most appropriate method for their specific scientific inquiries in drug development and nutritional validation research.
Comparative Analysis of Traditional Dietary Assessment Methods
The choice of a dietary assessment method is critical and depends on the research question, study design, sample characteristics, and required precision [7]. Table 1 summarizes the core characteristics, while Table 2 provides a quantitative summary of method performance from validation studies.
Table 1: Core Characteristics of Traditional Dietary Assessment Methods
| Feature | 24-Hour Dietary Recall (24HR) | Food Record | Food Frequency Questionnaire (FFQ) |
|---|---|---|---|
| Primary Purpose | Detailed intake for a specific past day [9] | Comprehensive recording of current intake [7] | Assessment of habitual intake over a long period (months to a year) [7] [10] |
| Time Frame | Short-term (previous 24 hours) [7] | Short-term (typically 3-4 days) [7] | Long-term (habitual intake) [7] [10] |
| Data Collection | Interviewer-administered or automated self-administered [7] [9] | Self-administered by participant [7] | Typically self-administered, can be interviewer-administered [7] [10] |
| Memory Reliance | Specific memory [9] | No memory requirement (prospective) [9] | Generic memory [9] |
| Participant Burden | Moderate (30-60 min per recall) [9] | High (requires literacy and motivation) [7] | Low to Moderate (once completed) [7] |
| Researcher Burden | High (training, interview, coding) [7] | Low to Moderate (data checking and coding) | Low (data processing only) [7] |
| Major Error Type | Random (day-to-day variation) [7] [9] | Random and Systematic (reactivity) [7] | Systematic (measurement error) [7] [9] |
| Reactivity Potential | Low (unannounced) [9] | High (may alter diet for ease of recording) [7] | Low [7] [9] |
Table 2: Quantitative Performance in Macronutrient Validation Studies
| Method | Comparison Standard | Energy Correlation/ Difference | Macronutrient Correlation/ Difference | Key Findings |
|---|---|---|---|---|
| Food Record | Doubly Labeled Water (DLW) | Significant under-reporting common [8] | Variable under-reporting | Considered less biased than FFQ but prone to reactivity [7] [8] |
| 24-Hour Recall | Doubly Labeled Water (DLW) | Least biased estimator; under-reporting still occurs [7] [8] | Macronutrients more stable than vitamins/minerals [7] | Multiple non-consecutive recalls required to estimate usual intake [7] [9] |
| FFQ | Multiple 24HRs | Correlations ~0.57-0.63 for energy [10] | Correlations: Protein (0.56-0.62), Lipids (0.51-0.55), Carbs (0.42-0.51) [10] | Effective for ranking individuals by intake rather than measuring absolute intake [7] [10] |
| Digital Food Record Apps | Traditional Food Records | Pooled mean difference: -202 kcal/day (underestimation) [1] | Underestimation: Carbs (-18.8 g/d), Fat (-12.7 g/d), Protein (-12.2 g/d) [1] | Heterogeneity decreases when using consistent food composition databases [1] |
Detailed Methodological Protocols
The 24-Hour Dietary Recall (24HR) Protocol
The 24HR is a structured interview designed to capture detailed information about all foods and beverages consumed by a respondent in the previous 24-hour period [9].
Application Note: The 24HR is ideal for obtaining detailed, quantitative data on recent intake at the group or population level. It is well-suited for cross-sectional studies like the National Health and Nutrition Examination Survey (NHANES) and for use as a reference instrument to validate other dietary tools like FFQs [7] [9]. Its open-ended nature allows it to capture a wide variety of foods.
Step-by-Step Protocol:
- Recruitment & Scheduling: Recruit participants and schedule the interview. Unannounced recalls are preferred to minimize reactivity and changes to usual diet [9].
- Initial Briefing: Obtain informed consent. Explain the purpose is to collect a detailed list of all foods and drinks consumed from midnight to midnight the previous day.
- The Interview - Automated Multiple-Pass Method (AMPM): This method uses multiple passes to enhance completeness and accuracy [9].
- Pass 1 - Quick List: The respondent lists all foods and beverages consumed the previous day without interruption.
- Pass 2 - Forgotten Foods: The interviewer uses specific probes to cue memories for commonly forgotten items (e.g., sweets, beverages, snacks, condiments).
- Pass 3 - Time and Occasion: For each item, the interviewer collects the time of consumption and the name of the eating occasion.
- Pass 4 - Detail Cycle: The interviewer probes for detailed descriptions of each food (e.g., preparation method, brand names, additions like fats and sugar) and precise portion sizes using visual aids like food models, pictures, or household measures.
- Pass 5 - Final Review: The interviewer summarizes the entire recall for the respondent to verify completeness and accuracy.
- Data Management: Audio-record the interview (with permission) for quality control. Code the data using a linked nutrient composition database (e.g., Food Patterns Equivalents Database - FPED) and food composition database. Automated systems like ASA24 can handle most coding [9].
- Repeat Administration: To account for day-to-day variation and estimate usual intake, collect multiple 24HRs (at least two) on non-consecutive, random days for each participant [7] [9].
The following workflow visualizes the standardized 5-pass protocol:
The Food Record Protocol
The food record, or diet diary, is a prospective method where the participant records all foods, beverages, and supplements consumed as they are consumed [7].
Application Note: Food records provide highly quantitative data and are considered a strong reference method, though they are subject to reactivity. They require a literate, cooperative, and motivated population. Typically, 3-4 days of recording (including both weekdays and weekend days) are used to account for daily variation without overburdening participants [7].
Step-by-Step Protocol:
- Participant Training: Conduct a comprehensive training session. Train participants to:
- Record items immediately before or after consumption.
- Describe foods in detail (brands, cooking methods, recipes).
- Estimate portion sizes accurately using provided tools (digital scales, measuring cups, spoons, or photographic aids). Weighed records are the gold standard.
- Record time of day and eating occasion.
- Note any leftovers or forgotten items.
- Recording Period: Provide a structured diary (paper or digital) and portion size estimation tools. Define the recording period (e.g., 3-4 consecutive days).
- Real-Time Data Entry: Participants record all dietary intake in real-time throughout the designated period.
- Diary Review and Clarification: Upon completion, a researcher reviews the diary with the participant to clarify entries, resolve ambiguities, and fill in any missing details.
- Data Processing: Code the dietary data using a suitable nutrient composition database. Recipe ingredients must be disaggregated.
- Participant Training: Conduct a comprehensive training session. Train participants to:
The Food Frequency Questionnaire (FFQ) Protocol
An FFQ is designed to capture an individual's usual intake over a long period by asking about the frequency of consumption from a fixed list of food items [7] [10].
Application Note: FFQs are cost-effective for large-scale epidemiological studies where the goal is to rank individuals by their intake rather than measure absolute intake. They can be semi-quantitative (including portion sizes) or qualitative (using assumed portion sizes) [7]. Their validity is highly dependent on being tailored to the specific population's diet [10] [11].
Step-by-Step Protocol:
- Questionnaire Selection/Development: Select or develop an FFQ with a food list that reflects the dietary habits of the target population and includes major sources of the macronutrients of interest [10] [11]. For the PERSIAN Cohort, a 113-item semi-quantitative FFQ was developed and validated [10].
- Administration: The FFQ can be self-administered or interviewer-administered. Provide clear instructions at the beginning.
- Frequency Response: For each food item, the participant indicates their usual frequency of consumption over the reference period (e.g., the past year) using categories such as "never," "1-3 times per month," "once a week," "2-4 times per week," "daily," etc. [10].
- Portion Size Estimation: For semi-quantitative FFQs, the participant selects a usual portion size from predefined options (e.g., small, medium, large) often accompanied by photographs or common household measures [10] [11].
- Data Processing: FFQ responses are converted to daily intake amounts for each food item. These are then linked to a nutrient database to compute average daily nutrient intakes.
The high-level decision process for selecting the appropriate traditional method is summarized below:
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Research Reagents and Tools for Dietary Assessment Validation
| Item | Function & Application | Examples & Notes |
|---|---|---|
| Nutrient Composition Database | Converts reported food consumption into estimated nutrient intakes. Critical for all methods. | USDA FoodData Central; country-specific databases (e.g., Palestinian Food Atlas [12]). Must be compatible with the dietary assessment tool. |
| Food Patterns Equivalents Database (FPED) | Converts foods into guidance-based food groups (e.g., cups of fruit, tsp of added sugars). | Used with USDA dietary data to assess adherence to dietary guidelines [9]. |
| Visual Portion Size Aids | Standardizes the estimation of food amounts by participants and interviewees. | Food models, photographs, atlases, or household utensils (cups, spoons). Essential for 24HR and food records [10] [12]. |
| Automated 24HR System | Standardizes the interview process, reduces interviewer burden, and automates data coding. | ASA24 (Automated Self-Administered 24-hour recall) [7] [9]. |
| Validated FFQ | A population-specific questionnaire to assess habitual diet. | Must be developed and validated for the target population (e.g., PERSIAN Cohort FFQ [10], DIGIKOST-FFQ [13]). |
| Recovery Biomarkers | Objective, non-self-report measures to validate energy and specific nutrient intake. | Doubly Labeled Water (DLW) for energy; urinary nitrogen for protein; urinary sodium/potassium [7] [8]. Considered the gold standard for validation. |
Food records, 24-hour recalls, and FFQs each provide a unique lens through which to view dietary intake, and the choice among them should be a deliberate one dictated by the research question and constraints. The 24HR generally offers the least biased estimate for group-level energy and macronutrient intake, the food record provides high detail at the cost of high participant burden, and the FFQ enables efficient ranking of individuals by habitual intake in large-scale studies. The ongoing integration of technology, such as automated self-administered tools and image-based methods, promises to reduce burden and error, further refining the accuracy of macronutrient validation research [1] [12]. A critical best practice is to always use a method validated for the specific population under study and to account for the pervasive issue of under-reporting, particularly for energy intake.
Accurate dietary assessment is fundamental to validating macronutrient intake in clinical and research settings. However, self-reported dietary data are compromised by inherent methodological limitations including recall bias, measurement errors, and significant participant burden [14]. These challenges persist across diverse populations, from athletes to adolescents, and despite advancements in technology-assisted methods [15] [16]. Understanding the nature, magnitude, and mitigation strategies for these limitations is crucial for researchers and drug development professionals interpreting dietary data or designing nutritional intervention studies. The reliability of macronutrient validation research directly depends on recognizing how these factors influence data quality and subsequent health outcome associations.
Quantitative Evidence of Assessment Limitations
Empirical studies consistently demonstrate systematic errors across various dietary assessment methods. The following tables summarize key quantitative findings on reliability, validity, and misreporting from recent research.
Table 1: Validity and Reliability of Digital Dietary Assessment Tools in Specific Populations
| Tool/Population | Nutrients with Poor Validity | Nutrients with Good Validity | Reliability Findings | Source |
|---|---|---|---|---|
| MyFitnessPal (Canadian Endurance Athletes) | Total energy, carbohydrates, protein, cholesterol, sugar, fibre [15] | Not applicable | Low inter-rater reliability for sodium and sugar; differences driven by gender [15] | [15] |
| Cronometer (Canadian Endurance Athletes) | Fibre, Vitamins A & D [15] | All other nutrients assessed [15] | Good to excellent inter-rater reliability for all nutrients [15] | [15] |
| myfood24 (Healthy Danish Adults) | Energy (ρ=0.38 vs. TEE), Protein (ρ=0.45), Potassium (ρ=0.42) [17] | Folate (ρ=0.62 with serum folate) [17] | Strong reproducibility (ρ ≥ 0.50) for most nutrients; lower for fish (ρ=0.30) and Vitamin D (ρ=0.26) [17] | [17] |
Table 2: Common Sources and Magnitude of Dietary Assessment Errors
| Error Type | Primary Sources | Impact on Data Quality | Evidence |
|---|---|---|---|
| Systematic Misreporting | Social desirability bias, memory-related bias, reactivity bias [16] | Underestimation of energy intake; macronutrient skewing [16] | 87% of adults classified as "acceptable reporters" via Goldberg cut-off; indicates 13% significant misreporting [17] |
| Database Errors | Use of non-verified user entries (e.g., MFP), varying fortification practices, brand differences [15] | Inaccurate micronutrient and macronutrient profiling [15] | CRO's use of verified databases (CNF, USDA) resulted in superior validity vs. MFP's user-uploaded entries [15] |
| Recall & Memory Bias | Long recall windows (e.g., 24-hr), complex meals, irregular eating patterns in adolescents [16] | Incomplete food item recall, inaccurate portion size estimation [14] [16] | Shorter recall windows (2-hr, 4-hr) proposed to reduce memory reliance in ecological momentary assessment [16] |
| Participant Burden | Weighed food records, prolonged recording periods, complex tracking interfaces [18] [16] | Low compliance rates, reactivity (altered diet during assessment) [16] | High burden methods (e.g., weighed records) require high participant motivation; leads to dropout or non-representative intake [16] |
Experimental Protocols for Mitigation and Validation
To counteract these limitations, researchers have developed robust protocols that integrate technology and methodological rigor. The following sections detail specific experimental approaches.
Protocol for Evaluating a Digital Dietary Assessment Tool
This protocol, adapted from a study evaluating the Traqq app among adolescents, provides a framework for validating digital tools against reference methods [16].
Objective: To quantitatively evaluate the accuracy, usability, and user perspectives of a digital dietary assessment app using repeated short recalls in a specific population.
Study Design: A mixed-methods approach spanning multiple phases.
- Phase 1 (Quantitative Evaluation): Participants download the target app and complete a demographic questionnaire. Dietary intake is assessed via the app on multiple random, non-consecutive days, employing varying recall windows (e.g., 2-hour and 4-hour recalls). Reference methods, such as interviewer-administered 24-hour recalls and a Food Frequency Questionnaire (FFQ), are conducted in parallel. Usability is evaluated using standardized scales (e.g., System Usability Scale) and an experience questionnaire.
- Phase 2 (Qualitative Evaluation): Semi-structured interviews are conducted within a subsample of participants to explore user experiences in depth.
- Phase 3 (Co-creation): Based on the analyzed data, co-creation sessions are held with participants to inform app customization and improve suitability for the target population.
Key Methodological Considerations:
- Recruitment: Target sample size of ~100 participants, stratified by age or other relevant demographics.
- Reference Methods: Use multiple methods (e.g., 24-hour recalls, FFQ, biomarkers) to triangulate validity.
- Blinding: Raters inputting food records into different tools should be blinded to each other's inputs to minimize bias [15].
- Data Analysis: Compare estimated intakes from the target app with reference methods using correlation analyses, Bland-Altman plots for assessing bias, and statistical tests for agreement.
Protocol for Validation Against Dietary Biomarkers
This protocol uses objective biomarkers to assess the validity and reproducibility of a dietary assessment tool, minimizing reliance on self-report [17].
Objective: To assess the validity and reproducibility of a dietary assessment tool against dietary intake biomarkers in a healthy adult population.
Study Design: A repeated cross-sectional study.
- Visits: The study includes an information meeting, a screening visit, and two main study visits (V1 at baseline, V2 at week 5).
- Dietary Assessment: Participants complete a 7-day weighed food record (WFR) using the target tool (e.g., myfood24) before both V1 and V2.
- Biomarker Collection: On the final day of each WFR, participants collect a 24-hour urine sample (for biomarkers like urea and potassium). At V1 and V2, fasting blood samples are drawn (e.g., for serum folate), and resting energy expenditure is measured via indirect calorimetry.
- Anthropometrics: Body weight and height are measured to ensure weight stability (e.g., deviation <2.5% between visits), confirming adherence to habitual diet.
Key Methodological Considerations:
- Biomarker Selection: Choose biomarkers with established relationships to dietary intake (e.g., urinary nitrogen for protein, serum folate for fruit/vegetable intake) [17].
- Standardization: Provide kitchen scales and detailed instructions for weighed food records and urine collection.
- Reproducibility Analysis: Assess tool reliability by comparing nutrient intakes from the first and second WFRs using correlation analyses.
The Scientist's Toolkit: Key Research Reagents and Materials
Essential materials and methodological components for conducting rigorous dietary assessment validation studies are listed below.
Table 3: Essential Research Reagents and Materials for Dietary Validation Studies
| Item | Specification/Example | Primary Function in Research |
|---|---|---|
| Validated Digital Tool | Cronometer, myfood24, Traqq | Automated nutrient calculation from food intake records; reduces manual entry error and processing time [15] [16] [17]. |
| Reference Database | Canadian Nutrient File (CNF), USDA FNDDS, ESHA Food Processor | Provides verified, standardized nutrient profiles for foods; serves as the gold standard for validity testing [15] [19]. |
| Biomarker Assays | 24-hour Urinary Nitrogen/Potassium, Serum Folate, Doubly Labeled Water | Offers objective measures of intake for specific nutrients, independent of self-report errors [14] [17]. |
| Portion Control Aids | Kitchen Scales (Digital), Photographic Atlas, Standardized Utensils | Improves accuracy of portion size estimation, a major source of measurement error in self-reports [17]. |
| Energy Expenditure Device | Indirect Calorimetry System | Measures resting energy expenditure (REE) to apply Goldberg cut-offs for identifying misreporters of energy intake [17]. |
| Structured Questionnaires | System Usability Scale (SUS), Demographic Forms, Food Frequency Questionnaire (FFQ) | Quantifies user experience, characterizes the study population, and assesses habitual diet as a reference method [16]. |
The inherent limitations of dietary assessment are pervasive but can be managed through rigorous study design. Key strategic recommendations for researchers include:
- Tool Selection: Prioritize tools that use verified, context-specific food composition databases over those reliant on unvetted user-generated content [15].
- Method Triangulation: Combine multiple assessment methods (e.g., short recalls, biomarkers, FFQs) to counteract the weaknesses of any single approach [16] [17].
- Participant-Centric Design: Employ user-centered design and co-creation, especially for challenging populations like adolescents, to reduce burden and improve compliance and accuracy [16].
Dietary assessment is a cornerstone of nutritional science, essential for validating macronutrient intake in research and clinical practice. The field is undergoing a profound transformation, moving from subjective, memory-dependent methods toward objective, technology-enhanced approaches [20] [21]. This evolution aims to overcome long-standing limitations of traditional techniques, including recall bias, portion size misestimation, and high participant burden [22] [21]. Artificial intelligence (AI) technologies are now reshaping the dietary assessment landscape, offering unprecedented capabilities for precise food recognition, nutrient estimation, and personalized nutrition planning [23] [20]. For researchers and drug development professionals, understanding this methodological shift is crucial for designing robust studies that generate reliable, quantitative macronutrient data for clinical validation research.
Traditional Dietary Assessment Methods: Foundations and Limitations
Traditional dietary assessment methods have provided the foundation for nutritional epidemiology and clinical research for decades. These approaches rely heavily on participant memory and honesty, making them susceptible to systematic errors that can compromise data quality in validation studies [21].
Table 1: Comparison of Traditional Dietary Assessment Methods
| Method | Data Collection Approach | Key Advantages | Key Limitations | Best Use Cases |
|---|---|---|---|---|
| 24-Hour Dietary Recall | Trained interviewer collects detailed information about all foods/beverages consumed in previous 24 hours [24] | Minimal participant burden; does not alter eating behavior; appropriate for diverse populations [21] | Relies heavily on memory; underreporting common; single day not representative of usual intake [21] | Population-level intake estimates; large epidemiological studies |
| Food Frequency Questionnaire (FFQ) | Self-reported frequency of consumption for specific food items over extended period (months/year) [24] | Captures long-term dietary patterns; cost-effective for large studies; automated analysis available [25] | Memory dependent; limited accuracy for absolute nutrient intake; portion size estimation challenging [25] | Ranking individuals by intake levels; studying diet-disease relationships |
| Food Records/Diaries | Detailed documentation of all foods/beverages as consumed, typically for 3-7 days [21] | Minimizes memory bias; provides quantitative data; can capture seasonal variation | High participant burden; may alter normal eating patterns; requires literacy and motivation [21] | Metabolic studies; clinical trials requiring detailed intake data |
| Diet History Interview | Comprehensive interview assessing habitual intake, food preferences, and eating patterns [22] | Provides context for dietary habits; captures complex eating behaviors | Time-intensive; requires skilled interviewer; susceptible to social desirability bias [22] | Clinical nutrition assessment; eating disorder evaluation |
The limitations of these traditional methods are particularly pronounced in validation research. Studies comparing dietary intake data against nutritional biomarkers reveal significant discrepancies. For example, research in eating disorder populations found only moderate agreement between diet history interviews and biochemical markers, with correlations varying substantially by nutrient [22]. Energy and protein intake often show systematic underreporting, especially in specific populations [21]. These measurement errors present substantial challenges for macronutrient validation studies where precision is paramount.
The Rise of Technology-Enhanced Dietary Assessment
Image-Assisted Dietary Assessment (IADA)
Image-assisted dietary assessment represents a paradigm shift from memory-based recall to visual documentation. Early systems required trained staff to analyze food images, but recent advancements have integrated artificial intelligence to automate the process [21]. The fundamental premise involves capturing images of meals before and after consumption, then using computer vision algorithms to identify foods and estimate portion sizes.
The technological evolution of IADA has progressed through distinct phases. Before 2015, systems relied on handcrafted machine learning algorithms that processed images through sequential steps: food segmentation, item identification, volume estimation, and nutrient calculation [21]. Since 2015, deep learning algorithms have dominated the field, substantially improving accuracy through convolutional neural networks. The most recent innovation involves end-to-end deep learning and multi-task learning approaches that simultaneously handle multiple aspects of dietary assessment within a single network architecture [21].
Artificial Intelligence and Machine Learning Applications
AI is revolutionizing dietary assessment across multiple dimensions, from automated food recognition to personalized nutrition recommendations. Machine learning algorithms can identify complex, non-linear relationships between dietary patterns and health outcomes that might elude traditional statistical methods [20]. These capabilities are particularly valuable for precision nutrition approaches that integrate genetic, metabolic, and behavioral data to develop individualized dietary recommendations [23].
Several AI-powered platforms demonstrate the potential of these technologies:
- goFOOD: A smartphone-based system utilizing deep learning to estimate micronutrient and energy content from food images, including support for stereo image pairs from dual-camera smartphones [20]
- VBDA (Vision-Based Dietary Assessment): Employs computer vision to automatically detect dietary details from meal images, with recent implementations using multi-task learning for comprehensive nutrient assessment [20]
- AI-Enhanced Chatbots: Provide personalized dietary guidance and tracking support, improving adherence to nutritional interventions [20]
Table 2: Technology-Enhanced Dietary Assessment Tools
| Tool/Platform | Core Technology | Output Metrics | Validation Status | Research Applications |
|---|---|---|---|---|
| goFOOD/goFOODLITE | Deep Learning, Computer Vision | Energy, Micronutrients, Food identification | Pilot testing (n=42); 69% user satisfaction with logging features [20] | Real-time dietary tracking; nutritional epidemiology |
| VBDA Systems | Multi-task Learning, Computer Vision | Food categories, portion sizes, nutrient estimates | Laboratory validation; accuracy improvements over traditional methods [20] [21] | Food environment research; portion size estimation studies |
| Wearable Sensors | Continuous Monitoring, Bio-sensors | Glucose responses, eating episodes, energy expenditure | Varies by device; some CGM systems clinically validated | Metabolic research; personalized nutrition interventions |
| AI-Based Classification | Machine Learning, Natural Language Processing | Food processing level, diet quality scores | NHANES validation against HEI-2020 [26] | Food policy research; diet-disease association studies |
Experimental Protocols for Dietary Assessment Validation
Protocol 1: Validation of Image-Based Assessment Tools
Purpose: To validate the accuracy of AI-powered dietary assessment tools against traditional methods and direct observation.
Materials:
- Smartphone with camera or dedicated dietary assessment device
- Standardized placemats for scale reference
- Food scale (digital, precision ±1g)
- Nutrition analysis software (e.g., FNDDS, USDA database)
- AI-based dietary assessment application (e.g., goFOOD prototype)
Procedure:
- Study Setup: Recruit participants representing target population demographics. Obtain informed consent and institutional review board approval.
- Food Preparation: Prepare standardized meals with varying complexity (single foods, mixed dishes, multi-component meals).
- Image Acquisition: Capture images of each meal from multiple angles (45°, 90°) under consistent lighting conditions before consumption.
- Direct Measurement: Weigh each food component using digital scales; record exact weights and brands.
- AI Analysis: Process images through the AI dietary assessment system to generate food identification and portion size estimates.
- Traditional Assessment: Conduct 24-hour dietary recalls by trained interviewers blinded to direct measurement results.
- Data Analysis: Compare nutrient estimates from AI system and 24-hour recall against direct measurement values (ground truth).
Validation Metrics:
- Food identification accuracy (% correctly identified items)
- Portion size estimation error (mean absolute percentage error)
- Nutrient calculation accuracy (intraclass correlation coefficients)
- Systematic bias assessment (Bland-Altman analysis)
Protocol 2: Biomarker Validation of Dietary Intake
Purpose: To validate self-reported dietary intake against nutritional biomarkers in clinical populations.
Materials:
- Standardized diet history protocol [22]
- Blood collection equipment (vacutainers, centrifuge, storage tubes)
- Automated biochemical analyzer
- Nutritional biomarkers (cholesterol, triglycerides, protein, albumin, iron, hemoglobin, ferritin, TIBC, red cell folate) [22]
Procedure:
- Participant Screening: Recruit participants meeting inclusion criteria (specific clinical populations, age ranges). Exclude those with conditions affecting biomarker metabolism.
- Dietary Assessment: Administer standardized diet history by trained dietitian within 7 days of biomarker collection [22].
- Biomarker Collection: Collect fasting blood samples following standard phlebotomy procedures.
- Sample Processing: Centrifuge blood samples, aliquot serum/plasma, and store at -80°C until analysis.
- Laboratory Analysis: Process samples using validated laboratory methods for targeted nutritional biomarkers.
- Data Analysis:
- Calculate energy-adjusted nutrient intakes
- Perform Spearman's rank correlation between dietary estimates and biomarkers
- Compute kappa statistics for agreement between dietary and biomarker measures
- Conduct Bland-Altman analysis to assess systematic bias
Interpretation:
- Moderate to good agreement: kappa > 0.4 [22]
- Significant correlation: p < 0.05
- Consider confounding factors (supplement use, metabolic disorders, inflammation)
Classification Systems for Food Quality Assessment
Beyond nutrient quantification, classifying foods by quality and processing level is increasingly important in nutritional epidemiology. Several validated systems enable standardized assessment:
NOVA Classification: Categorizes foods into four groups based on processing extent: unprocessed/minimally processed, processed culinary ingredients, processed foods, and ultra-processed foods [26] [27]. While widely used, NOVA has limitations including subjective application and poor adaptation to certain cultural contexts [27].
Moderation Food Classification: A novel nutrient-based method identifying foods high in added sugars, saturated fat, refined grains, and sodium using thresholds aligned with Dietary Guidelines for Americans [26]. This system demonstrates strong validity, with moderation food intake showing high inverse correlation with Healthy Eating Index-2020 scores (r = -0.72) [26].
GR-UPFAST: A culture-specific tool developed for assessing ultra-processed food consumption in Greek populations, demonstrating good internal consistency (Cronbach's α = 0.766) and significant correlation with body weight (rho = 0.140, p = 0.039) [27].
Diagram 1: Evolution of dietary assessment methods showing transition from traditional approaches with inherent limitations to technology-enhanced solutions and future directions. The color progression indicates methodological advancement over time.
Table 3: Research Reagent Solutions for Dietary Assessment Validation
| Resource | Type | Key Features | Application in Research |
|---|---|---|---|
| ASA24 (Automated Self-Administered 24-hour Recall) | Software Tool | Free, web-based, automated 24-hour dietary recall system [24] | Population studies; validation comparator; high-throughput data collection |
| Food and Nutrient Database for Dietary Studies (FNDDS) | Database | Comprehensive nutrient values for ~7,000 foods; linked to NHANES [19] | Nutrient calculation standardization; epidemiological research; diet-disease association studies |
| Register of Validated Short Dietary Assessment Instruments | Toolkit | Repository of validated short dietary screeners with methodological details [25] [24] | Tool selection for specific populations; validation study design; cross-study comparability |
| USDA Food Patterns Equivalents Database (FPED) | Database | Converts foods to 37 USDA Food Patterns components [19] | Diet quality assessment; adherence to dietary guidelines; policy-relevant research |
| Nutritional Biomarkers | Biochemical Assays | Objective measures of nutrient intake (cholesterol, triglycerides, iron, folate, etc.) [22] | Validation of self-reported intake; assessment of nutritional status; metabolic studies |
| Image-Assisted Dietary Assessment (IADA) | Technology Platform | AI-powered food recognition and portion estimation from images [21] | Reduced burden dietary assessment; real-time monitoring; validation of traditional methods |
The evolution of dietary assessment from memory-dependent to technology-enhanced methods represents a fundamental shift in nutritional science research methodology. While traditional tools like 24-hour recalls and food frequency questionnaires remain valuable for specific applications, AI-powered technologies offer unprecedented opportunities to improve accuracy, reduce participant burden, and capture the complexity of dietary intake [20] [21]. For researchers conducting macronutrient validation studies, the integration of multiple assessment approaches—including image-based analysis, sensor technologies, and nutritional biomarkers—provides a robust framework for generating high-quality, validated dietary data. Future advancements will likely focus on standardizing these emerging technologies, improving their accessibility across diverse populations, and further integrating multi-omics data for comprehensive nutritional assessment [23]. This methodological evolution promises to enhance the precision and reliability of nutrition research, ultimately strengthening the evidence base for dietary recommendations and clinical practice.
Accurate dietary assessment is fundamental for understanding diet-disease relationships, informing public health policy, and developing nutritional interventions [28] [7]. However, self-reported dietary intake data are notoriously subject to both random and systematic measurement errors, complicating the interpretation of research findings [7] [8]. Consequently, rigorous validation of dietary assessment methods is essential. Within the context of macronutrient intake validation research, three key methodological approaches have emerged as standard for evaluating validity: correlation coefficients to measure association strength, Bland-Altman analysis to assess agreement, and biomarker comparison for objective verification [22] [8] [29]. This document outlines the application, interpretation, and integration of these core validation metrics, providing structured protocols and benchmarks for researchers conducting validation studies of dietary assessment methods.
Core Validation Metrics: Principles and Interpretation
The validation of dietary assessment methods relies on a suite of statistical tools that evaluate different aspects of measurement performance. The table below summarizes the purpose, interpretation guidelines, and key considerations for the three primary metrics discussed in this document.
Table 1: Key Validation Metrics for Dietary Assessment Methods
| Metric | Primary Purpose | Interpretation Guidelines | Key Considerations |
|---|---|---|---|
| Correlation Coefficients | Quantifies the strength and direction of the association between two methods [22] [30]. | - Spearman's rho ≥ 0.5: Good to strong correlation [30].- ~0.3: Considered meaningful for validity [29].- Kappa (K) > 0.4: Moderate agreement; > 0.6 Good agreement [22]. | Does not measure agreement; sensitive to the range of intakes in the study population [22]. |
| Bland-Altman Analysis | Evaluates the agreement between two methods by analyzing the differences between them across the range of intakes [22] [30]. | - Mean Difference (Bias): Systematic over- or under-reporting.- Limits of Agreement (LoA): (Mean Difference ± 1.96SD) defines the range where 95% of differences lie.- A plot visually reveals bias, trends, and outliers. | High agreement is indicated by a mean difference near zero and narrow LoA. Plots can identify proportional bias [30]. |
| Biomarker Comparison | Provides an objective, non-self-report reference to quantify measurement error [8] [29]. | - Doubly Labeled Water (DLW): Gold standard for total energy expenditure (validation of energy intake) [8] [29].- Urinary Nitrogen: Objective measure of protein intake [29].- Poor correlation suggests method inaccuracy or physiological confounders [31]. | Considered the most rigorous validation approach but is costly, invasive, and limited to specific nutrients [7] [8]. |
Experimental Protocols for Validation Studies
Protocol for a Comprehensive Biomarker Validation Study
The following protocol, adapted from a state-of-the-art validation study, integrates all three key metrics against objective biomarkers [29].
Aim: To validate a novel dietary assessment method (e.g., Experience Sampling-based Dietary Assessment Method - ESDAM) for energy, macronutrient, and food group intake.
Design: A prospective observational study over four weeks.
Participants:
- Sample Size: Minimum of 100 participants to detect a correlation of 0.3 with 80% power and a 5% alpha error [29].
- Eligibility: Healthy adults (18-65 years), stable body weight, not pregnant/lactating, no medically prescribed diets.
Methods and Timeline:
- Weeks 1-2 (Baseline):
- Weeks 3-4 (Intervention & Biomarker Assessment):
- Participants use the novel dietary assessment method (e.g., ESDAM) for the entire period.
- Biomarker Data Collection:
- Doubly Labeled Water (DLW): Administer an oral dose of DLW. Collect urine samples on days 1, 2, 8, and 9 (or over 14 days) to measure total energy expenditure [8] [29].
- Urinary Nitrogen: Collect 24-hour urine samples (e.g., on two separate days) to estimate protein intake [29].
- Blood Samples: Collect fasting blood samples to analyze:
- Compliance Monitoring: Use blinded continuous glucose monitoring to identify eating episodes and cross-verify participant compliance with the dietary app [29].
Validation Analysis:
- Correlation Analysis: Calculate Spearman's rank correlation coefficients between nutrient intakes from the novel method and those from the 24-HDRs and biomarker values [22] [29].
- Bland-Altman Analysis: Plot the differences between the novel method and the reference methods (24-HDRs and biomarkers) against their means to assess bias and limits of agreement [22] [30].
- Method of Triads: Use this statistical technique to quantify the correlation between each of the three measurements (novel method, 24-HDR, and biomarker) and the unknown "true" intake, thereby quantifying the measurement error of each method [29].
Protocol for a Comparative Validity Study Using Biochemical Indicators
This protocol is suited for validating a Food Frequency Questionnaire (FFQ) or diet history against biochemical status indicators [22] [31].
Aim: To examine the relationship between nutrient intake assessed by a dietary tool and corresponding nutritional biomarkers in a specific clinical population.
Design: Cross-sectional secondary data analysis.
Participants:
- A targeted sample (e.g., n=100 [31] or n=13 for a pilot study [22]) of a specific population (e.g., patients with peripheral arterial disease [31] or an eating disorder [22]).
Methods:
- Dietary Assessment: Administer the FFQ or diet history to participants.
- Biomarker Measurement: Collect fasting blood samples within a close timeframe (e.g., 7 days) of the dietary assessment. Analyze for specific biomarkers (e.g., vitamins A, C, D, E, zinc, iron, iron-binding capacity, triglycerides) [22] [31].
- Data Processing: Adjust nutrient intakes for total energy intake to account for confounding by total consumption [22].
Statistical Analysis:
- Correlation: Calculate Spearman's rank correlation coefficients between energy-adjusted nutrient intakes and their corresponding serum biomarker levels [22] [31].
- Agreement Statistics: Compute simple and weighted kappa statistics to assess the agreement in quartile classification between the dietary method and biomarker [22].
- Bland-Altman Analysis: Apply the Bland-Altman method to visually and quantitatively assess the agreement between the two measures across the range of intakes [22].
Workflow and Logical Diagrams
The following diagram illustrates the logical sequence of applying validation metrics in a dietary assessment validation study.
Figure 1: A logical workflow for validating dietary assessment methods, integrating the three key validation metrics.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key materials and tools required for conducting rigorous dietary validation studies.
Table 2: Essential Research Reagents and Solutions for Dietary Validation
| Item | Function/Application | Specification Notes |
|---|---|---|
| Doubly Labeled Water (DLW) | Gold-standard biomarker for measuring total energy expenditure (TEE) to validate reported energy intake [8] [29]. | Requires precise dosing based on body weight and collection of multiple urine samples over 7-14 days. |
| Urinary Nitrogen Analysis Kits | Objective recovery biomarker for validating protein intake estimates from dietary tools [29]. | Typically requires 24-hour urine collections from participants on multiple days. |
| Serum Carotenoid Assays | Concentration biomarker used as an objective indicator for fruit and vegetable consumption [29]. | Analyzed from fasting blood samples; reflects intake over preceding weeks. |
| Erythrocyte Membrane Fatty Acid Profiling | Biomarker for assessing long-term intake of specific fatty acids (e.g., omega-3, omega-6 PUFAs) [29]. | Provides a longer-term reflection of dietary fat intake compared to plasma. |
| Validated 24-Hour Dietary Recall (24-HR) | A standard self-reported reference method for detailed, short-term dietary intake [7] [29]. | Can be interviewer-administered or automated (e.g., ASA-24). Multiple non-consecutive recalls, including weekend days, are needed [28]. |
| Statistical Software (e.g., STATA, R) | For performing correlation, kappa statistics, Bland-Altman analysis, and the method of triads [22] [29]. | Custom scripts for Bland-Altman plots and method of triads are often required. |
Advanced Methodologies in Practice: Implementing AI, Biomarkers, and Digital Tools for Macronutrient Assessment
Accurate dietary assessment is a cornerstone of nutritional epidemiology and clinical research, essential for validating macronutrient intake and understanding its link to health outcomes. Traditional methods, such as 24-hour recalls and food diaries, are often hampered by recall bias, measurement errors, and high participant burden [3] [32]. Artificial Intelligence (AI), particularly deep learning (DL) and machine learning (ML), is transforming this field by introducing automated, objective, and scalable tools for dietary assessment. These technologies enhance the precision of data collection and open new avenues for real-time monitoring and personalized nutrition research, offering powerful solutions for macronutrient intake validation studies [33] [34].
Performance Benchmarks of AI Dietary Assessment Tools
The following tables summarize the performance metrics of various AI approaches as reported in recent validation studies, providing researchers with benchmarks for tool selection.
Table 1: Performance of Image-Based Dietary Assessment AI Systems
| System / Model Name | Primary AI Technique | Key Nutrients Assessed | Reported Performance Metrics |
|---|---|---|---|
| DietAI24 [35] | Multimodal LLM with RAG | 65 nutrients & components (Macro & Micronutrients) | 63% reduction in Mean Absolute Error (MAE) for food weight & 4 key nutrients vs. baselines |
| goFOOD 2.0 [33] | Computer Vision, Deep Learning | Energy (Caloric) Intake | Moderate agreement with dietitians in real-world validation [33] |
| RGB-D Fusion Network [32] | Deep Learning (Convolutional Neural Network) | Caloric Intake | Mean Absolute Error (MAE): 15% |
| Keenoa App [3] | Not Specified | Energy, Macronutrients | Correlation >0.7 for energy and macronutrients vs. traditional methods |
| General AI-DIA Methods [3] | Deep Learning, Machine Learning | Energy, Macro- and Micronutrients | 61.5% of studies reported correlation >0.7 for energy and macronutrients |
Table 2: Performance of Non-Image-Based and Specialized AI Models
| System / Model Type | Input Data | Application / Nutrient Focus | Reported Performance Metrics |
|---|---|---|---|
| Sound & Jaw Motion Model [32] | Wearable Sensor Data (Sound, Jaw Motion) | Food Intake Detection | Classification Accuracy: Up to 94% |
| ML Prediction Models [36] | Food Composition Data | Predicting Micronutrients after Cooking | 31% lower average error vs. retention-factor baseline method |
| AI Nutrition Recommender (AINR) [37] | User Profiles, Expert Rules, Meal DB | Personalized Meal Plan Accuracy | High accuracy in caloric/macronutrient suggestions, ensures diversity |
| Intelligent Diet Recommendation System [38] | Body Composition Data, ML | Personalized Diet Plans | Error rate < 3% for personalized plan recommendations |
Application Notes & Experimental Protocols
Protocol: Validation of Image-Based AI Dietary Assessment Tools
This protocol outlines the methodology for validating the accuracy of an image-based AI system (e.g., goFOOD, DietAI24) for macronutrient intake estimation against traditional dietary assessment methods [33] [3].
1. Objective: To determine the relative validity and accuracy of an AI-based dietary intake assessment (AI-DIA) tool in estimating energy and macronutrient intake compared to weighed food records or dietitian-led 24-hour recalls.
2. Materials and Reagents:
- AI-DIA Tool: A smartphone application with integrated AI for food recognition and nutrient estimation (e.g., DietAI24 [35]).
- Reference Method Materials: Digital food scales, standardized food composition database (e.g., FNDDS [35]), and data recording forms.
- Participants: A cohort of free-living adults. Sample sizes in recent studies range from 36 to 136 participants [3].
3. Experimental Procedure:
- Step 1: Study Design. A cross-sectional or randomized controlled trial design is employed where participants concurrently use the AI-DIA tool and complete the reference method for a set period (e.g., 3-7 days) [3] [37].
- Step 2: Data Collection.
- AI-DIA Method: Participants are trained to capture images of all meals and snacks before and after consumption using the smartphone app. The AI system automatically processes images for food identification, portion size estimation, and nutrient analysis [33] [35].
- Reference Method: Participants weigh and record all food and drink items consumed using provided digital scales and logs. Alternatively, a dietitian conducts a 24-hour recall using a multiple-pass method [3].
- Step 3: Data Processing. Nutrient intake data (energy, protein, fat, carbohydrates) from the AI-DIA tool and the reference method are extracted and compiled for statistical analysis.
4. Data Analysis:
- Correlation Analysis: Calculate Pearson or Spearman correlation coefficients to assess the strength of the relationship between nutrient estimates from the two methods. A correlation >0.7 is considered strong [3].
- Bland-Altman Analysis: Plot the mean differences between the two methods against their averages to evaluate bias and limits of agreement [3].
- Error Metrics: Compute Mean Absolute Error (MAE) and Root Mean Square Error (RMSE) to quantify the average magnitude of estimation errors [35].
Protocol: Development of a Personalized Nutrition Recommendation System
This protocol describes the workflow for building and validating an AI-based system that generates personalized weekly meal plans, suitable for intervention studies [37] [39].
1. Objective: To develop and technically validate an AI-based nutrition recommender (AINR) that generates balanced, personalized weekly meal plans tailored to user profiles and nutritional requirements.
2. Materials and Reagents:
- Expert-Validated Meal Database: A structured database of meals with detailed nutritional information, ideally culturally specific (e.g., Mediterranean database [37]).
- User Profile Data: Demographic information, anthropometrics (height, weight), physical activity level (PAL), health goals, allergies, and cultural preferences [37] [38].
- AI Models: A combination of knowledge-based rules (from nutritional guidelines) and machine learning or generative models (e.g., Variational Autoencoders, LLMs) [37] [39].
3. System Workflow and Validation Procedure:
- Step 1: User Profiling. The system calculates the user's Daily Energy Requirement (DER) and macronutrient targets based on entered profile data using established equations (e.g., Mifflin-St Jeor) and expert rules [37].
- Step 2: Meal Filtering and Retrieval. The system filters the meal database based on user constraints (allergies, cuisine preference) and seasonality [37].
- Step 3: Meal Plan Synthesis. An algorithm (e.g., generative model, optimizer) synthesizes daily and weekly meal plans from the filtered pool of meals. It ensures adherence to DER, macronutrient balance, food group variety, and diversity [37] [39].
- Step 4: Validation. The system's performance is evaluated on thousands of generated user profiles. Key metrics include:
- Filtering Accuracy: Percentage of meal plans that correctly exclude allergens or unwanted foods.
- Nutritional Accuracy: Difference between the total recommended energy/macronutrients in the plan and the user's calculated DER/targets. High accuracy is demonstrated by error rates <3% [38].
- Diversity and Balance: Assessment of meal repetition and adherence to food-based dietary guidelines [37].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Components for AI-Driven Dietary Assessment Research
| Component / Tool | Function / Description | Example(s) from Literature |
|---|---|---|
| Standardized Food Database | Provides authoritative, structured nutritional data for food items, essential for training AI models and converting food identifications into nutrient values. | Food and Nutrient Database for Dietary Studies (FNDDS) [35] |
| Expert-Validated Meal Database | A curated collection of meals with precise nutritional information and attributes, used for developing and testing recommendation systems. | Mediterranean Meals Database (Spanish & Turkish cuisines) [37] |
| Multimodal Large Language Model (MLLM) | An AI model that can process and understand both images and text. Used for advanced food recognition and description from meal photos. | GPT-4V (Vision) or similar models integrated via API [35] |
| Retrieval-Augmented Generation (RAG) | A technique that grounds an LLM's responses in external, authoritative databases (like FNDDS) to improve accuracy and reduce factual hallucinations. | DietAI24 Framework [35] |
| Wearable Sensors | Devices that capture passive data related to eating behaviors, such as jaw motion, wrist movement, and swallowing sounds, for objective intake monitoring. | Smartwatches, e-arbuds, or specialized wearable devices [32] [34] |
| Computer Vision Models | Deep learning models (e.g., CNNs) specifically designed for image analysis tasks, including food detection, classification, and portion size estimation. | Convolutional Neural Networks (CNNs) like NutriNet [3] |
| Generative AI Model | A deep learning model used to create new data instances, such as generating novel but nutritionally-sound meal combinations for personalized plans. | Variational Autoencoder (VAE) [39] |
Accurate dietary assessment is a cornerstone of nutritional epidemiology and is vital for understanding the link between dietary intake and health outcomes [3]. Traditional methods, including food records, 24-hour recalls, and food frequency questionnaires (FFQs), are susceptible to measurement errors, recall bias, and place a significant burden on participants [40] [3]. The emergence of image-based and image-assisted dietary assessment methods, powered by artificial intelligence (AI), offers a promising solution to these challenges by enhancing objectivity, simplifying the data collection process, and improving accuracy [41] [42]. This document outlines the application notes and experimental protocols for these methods within the context of macronutrient intake validation research, providing researchers and drug development professionals with the tools to implement and validate these technologies.
Image-based food recognition systems (IBFRS) typically involve several phases: food detection and segmentation in an image, classification of food items, and estimation of volume, calories, and nutrients [42]. Deep learning, particularly Convolutional Neural Networks (CNNs), has become the dominant approach, often outperforming other methods, especially when trained on large, diverse datasets [43] [42].
The tables below summarize key performance metrics from recent validation studies, providing a benchmark for researchers evaluating such systems.
Table 1: Performance Metrics of Automated Food Recognition Technologies
| Technology / Study | Core Method | Identification/Classification Accuracy | Key Performance Findings |
|---|---|---|---|
| Automatic Image Recognition (AIR) App [41] | CNN-based automatic image recognition | 86% (189/220 dishes) correctly identified | Significantly higher accuracy and time efficiency compared to voice input reporting (VIR) [41]. |
| EfficientNetB7 with Lion Optimizer [43] | Deep learning model on a 32-class food dataset | 99% accuracy (32-class) | Mean Absolute Error (MAE): 0.0079; Mean Squared Error (MSE): 0.035; Root Mean Squared Error (RMSE): 0.18 [43]. |
| Photo-Assisted Dietary (PAD) Intake Assessment [40] | Image-assisted with standardized food atlas | N/A | Demonstrated significantly higher consistency with weighed food records than 24-hour recall for cereals, vegetables, and meats (P < 0.05) [40]. |
Table 2: Correlation of AI-Based Methods with Traditional Assessment for Nutrient Estimation
| Nutrient Type | Number of Studies with Correlation >0.7 | Example Traditional Reference Method |
|---|---|---|
| Calories | 6 out of 13 studies [3] | 3-day food diary, weighed food records [3] |
| Macronutrients | 6 out of 13 studies [3] | 3-day food diary, weighed food records [3] |
| Micronutrients | 4 out of 13 studies [3] | 3-day food diary, weighed food records [3] |
Detailed Experimental Protocols
Protocol 1: Validation of an Automatic Image Recognition (AIR) App
This protocol is adapted from a randomized controlled trial evaluating an AIR app against a voice-input control in a young adult population [41].
- Objective: To assess the reporting accuracy, time efficiency, and user perception of an AIR mobile application compared to a voice input reporting (VIR) application under authentic dining conditions.
- Materials:
- Smartphones (standardized model and operating system, e.g., Android).
- AIR and VIR applications installed on the devices.
- A predefined menu (e.g., 17 dishes) representing a typical meal (one staple, one main course, three side dishes).
- Data collection server for image processing.
- Participant Recruitment:
- Recruit a cohort (e.g., n=42) from the target population (e.g., young adults aged 20-25).
- Randomly assign participants to the AIR (n=22) and VIR (n=20) groups.
- Procedure:
- Provide all participants with the same type of smartphone with the assigned app installed.
- Present each participant with the standardized test meal.
- Instruct participants to use their assigned app to report all dishes in the meal.
- For the AIR group: Participants capture a single image of the entire meal. The app automatically recognizes dishes, and users select the correct name from suggestions or use voice input for unrecognized items. They then confirm and input portion sizes and cooking methods.
- For the VIR group: Participants capture an image of the meal and then use voice input to report food names, portion sizes, and cooking methods for each dish sequentially.
- Record the time taken to complete the reporting for each participant.
- Data Analysis:
- Accuracy: Calculate the percentage of dishes correctly identified and reported in each group. Compare groups using statistical tests (e.g., t-test, P < 0.05).
- Time Efficiency: Compare the mean time to complete reporting between groups using statistical tests.
- User Perception: Administer the System Usability Scale (SUS) to both groups and compare scores.
Protocol 2: Implementing a Photo-Assisted Dietary (PAD) Intake Assessment
This protocol is based on a study validating a PAD method against the gold-standard weighing method in a cafeteria setting [40].
- Objective: To validate the accuracy and feasibility of a PAD method for estimating food weight in a free-living population.
- Materials:
- Standardized set of bowls with known dimensions (e.g., base area 120 cm², varying heights for different food types).
- A pre-developed food atlas containing images of ~70 food items in the standardized bowls from multiple angles (top, 45°).
- Participants' smartphones with a communication app (e.g., WeChat).
- Digital food scales (for validation phase).
- Participant Recruitment:
- Recruit participants from the target populations (e.g., college students, n=76; elderly individuals, n=121) to assess feasibility across groups.
- Procedure for Validation Study:
- In a controlled cafeteria setting, provide participants with a buffet-style dinner served in the standardized bowls.
- Instruct participants to capture photos of their food before and after consumption.
- Weigh each food item served to and leftover by each participant using digital scales (weighing method).
- The following day, conduct a 24-hour recall with the participants for comparison.
- Trained dietary assessors, blinded to the weighed data, use the food atlas to estimate the volume and then the mass of each food item from the photos.
- Data Analysis:
- Accuracy: Compare the food mass estimated via PAD and 24-hour recall to the mass from the weighing method. Calculate absolute and relative differences (D%). Use Bland-Altman analysis to assess limits of agreement.
- Feasibility: Report the proportion of participants who successfully completed the PAD recording and analyze feedback from questionnaires.
Protocol 3: Enhancing Adherence with Tailored Prompting
This protocol provides a methodology for improving user adherence in image-based dietary records, a critical factor for data quality [44].
- Objective: To evaluate the effect of tailored text message prompts on adherence to an image-based dietary record.
- Materials:
- Image-based dietary recording app (e.g., Easy Diet Diary).
- Text messaging system for sending prompts.
- Participant Recruitment:
- Recruit participants (e.g., n=37) meeting inclusion criteria (adults with smartphone and internet access).
- Procedure:
- Baseline: Participants complete a 3-day text-based dietary record to establish habitual meal times.
- Randomization: Participants are randomized to one of six study sequences, each with a unique order of three prompt conditions:
- Control: No prompts.
- Standard: Prompts sent at fixed times (e.g., 7:15 AM, 11:15 AM, 5:15 PM).
- Tailored: Prompts sent 15 minutes before each participant's individual habitual meal times, derived from the baseline record.
- Intervention: Participants complete multiple 3-day image-based dietary records, each separated by a 7-day washout period. They receive prompts according to the condition for that period.
- Data Collection: The number of images captured per participant per day is automatically logged.
- Data Analysis:
- Use linear mixed-effects models to analyze the effect of prompt setting on the image capture rate (images/day), accounting for participant effects and study order.
Workflow Diagrams
Adherence Study Workflow with Tailored Prompting
Automated Image Recognition (AIR) App User Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Image-Based Dietary Assessment Research
| Item | Function/Description | Example/Specification |
|---|---|---|
| Standardized Serveware | Provides visual cues for portion size estimation via a food atlas. Critical for volume-to-mass conversion. | Bowls with identical base area (e.g., 120 cm²) but varying heights for different food types (e.g., staples, meats) [40]. |
| Pre-Developed Food Atlas | A reference image library used by trained assessors to identify foods and estimate volumes from participant photos. | Contains ~150 images of 70+ food items, photographed from multiple angles (overhead, 45°) in standardized serveware [40]. |
| Deep Learning Model Architectures | The core AI engine for automatic food detection and classification from images. | Architectures such as ResNet50, EfficientNetB5-B7, and CNN-based models, often pre-trained on large datasets like ImageNet [41] [43] [42]. |
| Publicly Available Food Datasets (PAFDs) | Used for training and validating food recognition algorithms. Requires diversity and scale. | Datasets with tens of thousands of images across dozens or hundreds of food classes, often including mixed dishes [43] [42]. |
| Data Augmentation Pipeline | A software process to artificially expand training datasets, improving model robustness and reducing overfitting. | Includes image transformations: rotation (±10-15°), translation, shearing, zooming, and brightness/contrast adjustment [43]. |
The objective validation of self-reported dietary intake is a fundamental challenge in nutritional science, epidemiology, and clinical drug development. Nutritional biomarkers provide a critical solution by offering objective, quantitative measures of nutrient exposure, absorption, and metabolism [45] [46]. Unlike traditional dietary assessment methods such as Food Frequency Questionnaires (FFQs) and 24-hour recalls, which are susceptible to recall bias and measurement error, biomarkers deliver reproducible data that can reliably verify macronutrient intake [47] [4]. This verification is particularly crucial in clinical trials where nutrition can significantly influence treatment outcomes, drug efficacy, and metabolic health markers [48]. The integration of biomarker data enables researchers to move beyond subjective reporting to obtain validated nutritional metrics that strengthen the scientific rigor of dietary intervention studies.
The application of nutritional biomarkers extends across the research spectrum, from validating short food frequency questionnaires in intermittent fasting studies [47] to constructing sophisticated models like nutrition-based aging clocks using machine learning algorithms [49]. Furthermore, in clinical populations such as individuals with eating disorders, where self-reported dietary data may be compromised, biomarkers provide an essential objective measure to validate diet history assessments [4]. As precision medicine advances, the role of nutritional biomarkers in developing personalized dietary strategies for conditions like atherosclerosis highlights their growing importance in both research and clinical practice [48].
Key Biomarkers for Macronutrient Validation
This section catalogs well-established biomarkers for each macronutrient category, providing researchers with a reference for selecting appropriate verification tools for their specific study designs and objectives.
Table 1: Biomarkers for Carbohydrate Intake and Metabolism
| Biomarker | Biological Matrix | Physiological Role | Interpretation & Clinical Significance |
|---|---|---|---|
| Glucose | Plasma, Serum | Primary circulatory sugar; direct energy source | Reflects recent carbohydrate intake and metabolism; homeostatic dysregulation indicates metabolic issues [45]. |
| Insulin | Plasma | Hormone regulating cellular glucose uptake | Paired with glucose to assess insulin resistance or sensitivity; key in metabolic phenotyping [45]. |
| HbA1c (Glycated Hemoglobin) | Whole Blood | Irreversible product of hemoglobin and glucose | Measure of average blood glucose levels over the past 2-3 months; gold standard for long-term glycemic control [45]. |
| Fructosamine | Serum | Glycated serum proteins | Reflects average glucose over 2-3 weeks; useful for shorter-term monitoring than HbA1c. |
Table 2: Biomarkers for Protein Status and Intake
| Biomarker | Biological Matrix | Physiological Role | Interpretation & Clinical Significance |
|---|---|---|---|
| Albumin | Serum | Major plasma protein; maintenance of osmotic pressure | Marker of chronic protein status and inflammation; longer half-life (~20 days) [45] [4]. |
| Prealbumin (Transthyretin) | Serum | Thyroxine and retinol-binding protein | Sensitive indicator of recent nutritional changes due to short half-life (~2 days); responds quickly to dietary intervention [45]. |
| Amino Acid Profiles | Plasma, Urine | Quantification of individual amino acids | Provides insight into protein metabolism, dietary protein quality, and specific metabolic pathways [49] [45]. |
| Urea Nitrogen | Serum, Urine | End-product of protein catabolism | Correlates with dietary protein intake; useful for estimating nitrogen balance. |
Table 3: Biomarkers for Fat Intake and Metabolism
| Biomarker | Biological Matrix | Physiological Role | Interpretation & Clinical Significance |
|---|---|---|---|
| Fatty Acid Profiles | Plasma, Erythrocytes, Adipose Tissue | Composition reflects dietary fat intake | Specific fatty acids (e.g., omega-3 from fish oil) serve as direct biomarkers of intake; profiles inform about metabolic health [45]. |
| Cholesterol (Total, LDL, HDL) | Serum | Structural and metabolic lipid | Measures lipid metabolism status; primary biomarker for cardiovascular risk assessment [45] [48]. |
| Triglycerides | Serum | Storage and transport form of fats | Reflects recent fat intake and metabolic status; elevated levels associated with cardiovascular risk [4]. |
| Trimethylamine N-Oxide (TMAO) | Plasma | Gut microbiome-derived metabolite from dietary choline and L-carnitine | Emerging biomarker linking dietary fat, gut microbiome, and cardiovascular disease pathogenesis [50] [48]. |
Experimental Protocols for Biomarker Validation
Protocol 1: Validation of Dietary Assessment Tools Against Biomarkers
This protocol is designed to test the validity of subjective dietary assessment methods, such as FFQs or diet histories, by comparing their results with objective biomarker measurements. The approach is adapted from validation studies detailed in the search results [47] [4].
- Step 1: Study Population Recruitment. Recruit a participant cohort representative of the target population for the dietary assessment tool. For a pilot validation study, a sample size of approximately 10-15 participants per group can provide preliminary data, though larger samples are needed for definitive validation [47] [4]. Collect comprehensive demographic and anthropometric data.
- Step 2: Concurrent Data Collection.
- Dietary Data: Administer the dietary assessment tool (e.g., a short FFQ [47] or a detailed diet history [4]). Ensure standardized administration by trained personnel to minimize interviewer bias.
- Biomarker Sampling: Collect biological samples (blood, urine) for biomarker analysis within a close timeframe (e.g., within 7 days [4]) of the dietary assessment.
- Step 3: Laboratory Analysis. Process samples according to established methods. For example:
- Plasma Glucose, Insulin, Lipids: Use standardized clinical chemistry analyzers.
- Amino Acids and Vitamins: Employ liquid chromatography-tandem mass spectrometry (LC-MS/MS) for high sensitivity and specificity [49].
- Urinary Oxidative Stress Markers: Quantify using LC-MS/MS and normalize to creatinine levels [49].
- Step 4: Data Analysis and Agreement Testing.
- Correlation Analysis: Calculate Spearman’s rank correlation coefficients to assess the strength of the relationship between reported nutrient intake and biomarker levels [4].
- Method Agreement: Use Bland-Altman plots to visualize the agreement between methods and identify any systematic biases [47] [4].
- Categorical Agreement: Apply kappa statistics to evaluate the agreement in nutrient intake categorization (e.g., deficient/sufficient). Interpret kappa values as: ≤0.2 (poor), >0.2-0.4 (fair), >0.4-0.6 (moderate), >0.6-0.8 (good), >0.8-1.0 (very good) [4].
Diagram 1: Dietary Tool Validation Workflow
Protocol 2: Advanced Biomarker Panel for Metabolic Phenotyping
This protocol leverages high-throughput technologies to generate a comprehensive metabolic profile, useful for constructing predictive models (e.g., aging clocks [49]) or for deep phenotyping in precision nutrition trials [48].
- Step 1: Pre-Analytical Sample Handling. Implement standardized protocols to minimize pre-analytical variation. For plasma, use EDTA tubes and separate plasma within 30 minutes of collection. Store all samples at -80°C until analysis. For urine, collect first-morning voids and aliquot after centrifugation [49].
- Step 2: Multi-Omic Biomarker Profiling.
- Amino Acids and Vitamins: Quantify 9 amino acids (e.g., ethanolamine, L-serine, L-proline, taurine) and 13 vitamins (B1, B2, B3, B5, B6, B7, 5-methyltetrahydrofolate, A, D2, D3, E, K1, MK4) using LC-MS/MS [49].
- Oxidative Stress Markers: Quantify urinary 8-oxoGuo and 8-oxodGuo using LC-MS/MS, with creatinine correction for normalization [49].
- Fatty Acid Profiling: Analyze plasma phospholipid fatty acids or erythrocyte membrane fatty acids using gas chromatography-mass spectrometry (GC-MS).
- Inflammatory Biomarkers: Measure high-sensitivity C-reactive protein (hs-CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-α) via immunoassays.
- Step 3: Body Composition Analysis. Perform bioelectrical impedance analysis (BIA) to measure key body composition metrics such as basal metabolic rate (BMR), muscle mass, total body water, extracellular water, and fat mass [49]. Ensure measurements are taken under standardized conditions (e.g., fasted state, no intense prior exercise).
- Step 4: Data Integration and Model Building.
- Data Preprocessing: Normalize data, handle missing values, and scale features as appropriate.
- Machine Learning Application: Utilize algorithms such as Light Gradient Boosting Machine (LightGBM), random forest, or XGBoost to build predictive models [49].
- Model Validation: Evaluate model performance using metrics like Mean Absolute Error (MAE) and the Coefficient of Determination (R²), validated via train-test splits or cross-validation [49].
Applications in Research and Clinical Practice
The utilization of nutritional biomarkers for macronutrient verification has diverse and impactful applications across biomedical research and patient care, enabling more rigorous and personalized approaches.
- 1. Enhancing Validity in Nutritional Epidemiology: Biomarkers correct for measurement errors inherent in self-reported dietary data. For example, in a study on intermittent fasting, a short FFQ was validated against weighted food records, revealing that while most questions were valid, data on snacking and whole-grain consumption were unreliable, demonstrating how biomarkers can identify and mitigate specific biases in dietary assessment tools [47].
- 2. Personalizing Nutrition for Chronic Disease Management: In atherosclerosis management, biomarkers enable personalized nutrition plans that move beyond one-size-fits-all recommendations. Polymorphisms in the
APOA2gene can influence body mass index and lipid levels, while omega-3 fatty acids can modulate microRNA expression impacting lipid metabolism. This allows for dietary interventions tailored to an individual's genetic, microbiome, and metabolomic profile, offering a more effective strategy for cardiovascular risk reduction [48]. - 3. Objective Monitoring in Clinical Populations: Biomarkers are indispensable in clinical populations where self-report is highly unreliable. A study in patients with eating disorders found moderate to good agreement between diet history and biomarkers for nutrients like iron and cholesterol. The study highlighted that accuracy improved with larger intakes and that including dietary supplements in the assessment was crucial, providing an objective basis for nutritional rehabilitation in this sensitive population [4].
- 4. Development of Predictive Health Models: Biomarkers are foundational for constructing predictive models of health and aging. A study successfully built a highly accurate nutrition-related aging clock (MAE: 2.59 years, R²: 0.88) using plasma amino acids, vitamins, urinary oxidative stress markers, and BIA-derived body composition metrics. This model demonstrates how biomarker panels can quantify biological aging and assess the impact of nutritional interventions on the aging process itself [49].
Table 4: The Scientist's Toolkit: Essential Reagents and Platforms
| Category/Item | Specific Examples | Function & Application in Biomarker Analysis |
|---|---|---|
| LC-MS/MS Systems | Agilent 1290 UPLC/6490 MS, Sciex Triple Quad systems | Gold-standard for quantitative analysis of small molecules (amino acids, vitamins, oxidative stress markers) with high sensitivity and specificity [49]. |
| Automated Clinical Analyzers | Hitachi 7600 series, Roche Cobas systems | High-throughput, automated quantification of standard clinical biomarkers (glucose, lipids, albumin, HbA1c) [49] [4]. |
| BIA Devices | Tsinghua Tongfang BCA-2A, InBody series | Non-invasive assessment of body composition (muscle mass, fat mass, body water), a key component of nutritional status [49]. |
| Specialized Reagents | 8-oxo-[15N5]dGuo, 8-oxo-[13C1]Guo, deuterated fatty acids | Isotopically labeled internal standards for precise and accurate quantification of biomarkers via mass spectrometry [49]. |
| DNA/RNA Analysis Kits | Genotyping arrays, RNA-seq kits, miRNA profiling panels | For nutrigenomic applications to analyze gene-diet interactions, polymorphisms (e.g., APOA2), and epigenetic modifications [48]. |
Diagram 2: Biomarker Integration and Applications
Background: Accurate dietary assessment in low-literacy populations presents significant challenges, including participant burden, memory reliance, and systematic measurement error [7]. Traditional methods like 24-hour recalls and food frequency questionnaires often require literacy and advanced cognitive skills, limiting their effectiveness and accuracy in these settings [51] [52]. Hybrid systems that integrate voice recording and image capture offer a promising solution by reducing literacy barriers and enhancing data quality for macronutrient intake validation research.
Core Principle: This approach leverages voice recording to capture detailed food descriptions actively (overcoming literacy barriers) and image capture to passively document portion sizes and food types (reducing memory reliance and quantification errors) [53] [54]. The synergy of these data streams creates a richer, more valid dataset for subsequent nutritional analysis.
Key Validation Findings: Recent studies demonstrate the relative validity and high acceptability of hybrid dietary assessment methods.
Table 1: Relative Validity of Hybrid Dietary Assessment Systems for Energy Intake
| Study & Population | Assessment Method | Reference Method | Mean Difference in Energy (kcal) | Statistical Significance |
|---|---|---|---|---|
| VISIDA - Cambodian Mothers [54] | Voice-Image System (Period 1) | 24-hour Recalls | -296 (95% CI: -410 to -181) | Statistically Significant |
| VISIDA - Cambodian Mothers [54] | Voice-Image System (Period 2) | 24-hour Recalls | -274 (95% CI: -390 to -158) | Statistically Significant |
| VISIDA - Cambodian Children [54] | Voice-Image System (Period 1) | 24-hour Recalls | -158 (95% CI: -227 to -89) | Statistically Significant |
| VISIDA - Cambodian Children [54] | Voice-Image System (Period 2) | 24-hour Recalls | -127 (95% CI: -198 to -57) | Statistically Significant |
| base2Diet - General Adults [53] | Voice-Based Logging | Comparison via Engagement Metrics | 1.7x more logging events | Statistically Significant (P=.03) |
Acceptability and Adherence: Hybrid systems show markedly improved user engagement. The base2Diet study found the voice-based logging arm had a 1.5 times higher number of active days per participant and a significantly lower attrition rate compared to the text-based arm [53]. In the VISIDA study, most mothers (84.3%) found the smartphone app "easy" or "very easy" to use for collecting dietary intake [54].
Experimental Protocols
Protocol: Validation of a Hybrid Dietary Assessment System
This protocol outlines the procedure for validating a hybrid voice-image system against a reference method to estimate macronutrient and energy intake in a low-literacy population, based on the validated VISIDA system methodology [54].
Objective: To determine the relative validity, test-retest reliability, and acceptability of a hybrid voice-image dietary assessment system.
Population: Adults and/or children from low-literacy settings. Sample size calculation should be based on equivalent relative validity studies, often targeting ~150 household dyads (e.g., mother and child) for sufficient power [54].
Ethical Considerations: Approval must be obtained from relevant national and institutional human research ethics committees. Informed consent must be provided by all participants in their native language, with special consideration for verbal consent recorded via audio file for illiterate participants [54].
Study Design: A free-living, observational design with data collected across multiple recording periods over approximately four weeks.
Table 2: Data Collection Timeline for Validation Studies
| Week | Data Collection Method | Schedule | Data Collected |
|---|---|---|---|
| Week 1 | Hybrid System Recording | 3 non-consecutive days | Voice descriptions and images of all foods/beverages consumed. |
| Weeks 2-3 | Interviewer-Administered 24-hour Recalls | 3 non-consecutive days | Detailed recall of previous 24-hour intake using multiple-pass method. |
| Week 4 | Hybrid System Recording | 3 non-consecutive days | Voice descriptions and images of all foods/beverages consumed (for reliability). |
| Post-Study | Acceptability Survey | After final recording | Qualitative feedback on system usability and burden. |
Protocol: Implementing the Hybrid Data Capture Workflow
This protocol details the step-by-step procedure for participants and researchers to collect dietary data using the hybrid system.
Materials:
- Smartphone with hybrid data capture application installed.
- Optional portable scale for weighing foods (if high precision is required).
Participant Procedure:
- Initiation: For each eating occasion, the participant opens the application on the smartphone.
- Image Capture: Before eating, the participant captures one or more images of the food and beverages, ensuring the entire meal is visible in the frame.
- Voice Recording: The participant activates the voice recording function and describes:
- The types of food and beverages (e.g., "steamed rice," "chicken curry," "green leafy vegetables").
- The estimated quantity or portion size (e.g., "one small bowl," "two pieces").
- Any additional details like brand names, cooking methods (e.g., "fried," "boiled"), or ingredients.
- Submission: The participant submits the combined image-voice entry. The application automatically time-stamps the record.
Researcher/Data Processor Procedure:
- Data Processing: Voice recordings are transcribed, either manually or using automated speech recognition (ASR) and natural language processing (NLP) tools [53].
- Data Integration: The transcribed food descriptions are linked with their corresponding images.
- Nutrient Analysis: A trained nutritionist uses the integrated data (images for portion size estimation and text for food identification) to code entries and estimate nutrient intake using appropriate food composition tables or databases (e.g., Nutritionix API) [53].
- Data Analysis: Estimated nutrient intakes from the hybrid system are compared to those from the reference method (e.g., 24-hour recalls) using statistical analyses like linear mixed models to assess relative validity [54].
System Workflow and Signaling Pathways
The following diagram illustrates the integrated workflow of the hybrid dietary assessment system, from data capture to nutrient analysis.
Figure 1: Workflow of a hybrid voice-image dietary assessment system.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Hybrid Dietary Assessment Research
| Item Name | Function/Application | Example/Specification |
|---|---|---|
| Mobile Application | The core platform for data capture. Requires both image and audio recording capabilities. | Custom iOS/Android app (e.g., base2Diet [53]) with a simple user interface. |
| Natural Language Processing (NLP) API | Automatically processes voice recordings to extract food items and quantities into structured text data. | Nutritionix API [53] or similar, capable of parsing natural language food descriptions. |
| Speech Recognition Framework | Converts spoken language into text within a mobile application. | Platform-specific frameworks like Apple's Speech Framework for iOS [53]. |
| Food Composition Database | Provides the nutritional content (macronutrients, micronutrients) for identified food items. | Integrated with the NLP API or used separately (e.g., USDA FoodData Central). |
| Data Integration & Storage Platform | Manages, links, and stores the paired image and text data securely, often in the cloud. | Firebase Cloud Storage [53] or similar secure server infrastructure. |
| Portable Digital Scales | (Optional) For calibrating portion size estimates from images in validation sub-studies. | High-precision, battery-operated kitchen scales. |
| Nutrition Literacy Assessment Tool | For characterizing the study population and controlling for nutrition literacy as a covariate. | Nutrition Literacy Assessment Instrument (NLit) [55]. |
Mathematical Optimization Models for Dietary Pattern Analysis and Recommendation Development
Mathematical optimization has emerged as a powerful computational approach for transforming dietary guidance from general principles into precise, evidence-based recommendations. These models enable researchers to solve complex nutritional problems by identifying optimal dietary patterns that meet specific nutritional, economic, and environmental constraints. The core principle involves using algorithms to find the best possible solution from a set of alternatives while satisfying multiple competing requirements simultaneously [56]. In the context of dietary assessment methods for macronutrient intake validation research, optimization models provide a rigorous framework for testing hypotheses about nutritional adequacy, validating dietary patterns against biomarker data, and establishing quantitative relationships between food components and health outcomes.
The application of mathematical optimization in nutrition science has evolved substantially, progressing from simple linear programming for addressing nutrient deficiencies to sophisticated multi-objective models that balance nutritional adequacy, sustainability, cost, and cultural acceptability [57]. Within macronutrient validation research, these models serve as critical tools for determining whether theoretically optimal dietary patterns can indeed meet physiological requirements when implemented in real-world settings, thereby bridging the gap between epidemiological observations and biochemical validation.
Key Optimization Methodologies
Linear and Goal Programming
Linear programming (LP) represents the most established optimization methodology in nutritional epidemiology. LP models minimize or maximize a linear objective function (e.g., diet cost or nutrient intake) subject to linear constraints (e.g., nutritional requirements, food consumption limits) [56]. The mathematical formulation typically follows this structure:
Objective: Minimize/Maximize Z = c₁x₁ + c₂x₂ + ... + cₙxₙ
Subject to: a₁₁x₁ + a₁₂x₂ + ... + a₁ₙxₙ ≤ b₁ a₂₁x₁ + a₂₂x₂ + ... + a₂ₙxₙ ≥ b₂ ... xᵢ ≥ 0 for all i
Where xᵢ represents the quantity of food i, cᵢ represents the cost or nutrient density coefficient for food i, aᵢⱼ represents the nutritional composition matrix, and bᵢ represents the constraint boundaries (nutrient requirements) [56].
Extensions of LP, particularly linear goal programming, allow for multiple, often conflicting objectives to be considered simultaneously, making them particularly valuable for balancing competing priorities in dietary recommendations, such as simultaneously minimizing cost while maximizing nutritional adequacy and minimizing environmental impact [56].
Within-Food-Group Optimization
Traditional diet modeling often operates at the food group level, but recent methodological advances have demonstrated the significant advantages of within-food-group optimization. This approach recognizes the substantial variability in nutrient composition and environmental impact between individual foods within the same group [57].
By optimizing at the individual food level rather than at the food group level, researchers can achieve more precise dietary recommendations that better reflect real-world consumption patterns. This granular approach has been shown to achieve nutritional adequacy with significantly less dietary change (23% versus 44% for between-group optimization alone) while still achieving substantial environmental benefits (15-36% reduction in greenhouse gas emissions) [57]. For macronutrient validation research, this methodology enables more accurate modeling of dietary substitutions that maintain similar culinary functions and sensory properties while improving nutritional profiles.
Multi-Objective Optimization for Sustainability
Contemporary diet optimization models increasingly incorporate sustainability objectives alongside traditional nutritional considerations. These multi-objective frameworks simultaneously address nutritional adequacy, environmental impact (particularly greenhouse gas emissions), economic constraints, and cultural acceptability [57]. The mathematical complexity of these models requires sophisticated solving algorithms that generate Pareto-optimal frontiers—sets of solutions where improvement in one objective (e.g., lower environmental impact) necessitates compromise in another (e.g., higher cost) [57].
Figure 1: Multi-Objective Optimization Framework for balancing competing dietary priorities
Quantitative Applications and Outcomes
Optimization in Dietary Guideline Development
Mathematical optimization serves as the computational backbone for developing national dietary guidelines worldwide. The 2025 Dietary Guidelines Advisory Committee employed food pattern modeling to determine how modifications to food group quantities affect nutrient adequacy across diverse population subgroups [58]. Their systematic approach analyzed variations in dairy, fruits, vegetables, grains, and protein foods to establish quantitative dietary patterns that meet nutritional requirements while accommodating cultural preferences and environmental considerations [58].
Table 1: Dietary Pattern Modeling Analyses from 2025 Dietary Guidelines Advisory Committee
| Analysis Type | Key Questions Addressed | Primary Outcomes |
|---|---|---|
| Basis Nutrient Profiles | Should foods with lower nutrient density contribute to food group nutrient profiles? | Established refined nutrient profiling methodology for food groups and subgroups [58] |
| Dairy and Fortified Soy Alternatives | What are nutrient intake implications when modifying dairy quantities or replacing with alternatives? | Quantified nutrient trade-offs in dairy substitutions and modifications [58] |
| Protein Foods Optimization | How do shifts between animal and plant-based protein sources affect nutrient adequacy? | Determined optimal balances between protein subgroups in both Healthy U.S.-Style and Vegetarian Patterns [58] |
| Within-Food-Group Variations | How do nutrient profiles differ when calculated using intakes of specific population groups? | Documented significant variations in nutrient densities across demographic segments [58] |
Environmental and Economic Optimization
The integration of sustainability objectives into dietary optimization has yielded quantitatively significant findings. Research demonstrates that within-food-group optimization can achieve substantial environmental benefits while requiring less dramatic dietary changes, potentially enhancing consumer acceptance [57].
Table 2: Environmental and Acceptability Outcomes of Diet Optimization Approaches
| Optimization Strategy | GHGE Reduction Potential | Required Dietary Change | Nutritional Adequacy | Consumer Acceptability |
|---|---|---|---|---|
| Between-Food-Group Only | 30% reduction | 44% change from baseline | Achievable with major food group restructuring | Lower due to substantial dietary shifts [57] |
| Combined Within- and Between-Group | 30% reduction | 23% change from baseline | Achievable with modified food quantities within familiar groups | Higher due to preservation of familiar food patterns [57] |
| Within-Food-Group Only | 15-36% reduction | Minimal to moderate change | Fully achievable while maintaining current food group proportions | Highest due to minimal disruption to eating patterns [57] |
Experimental Protocols and Methodologies
Protocol for Diet Optimization Analysis
Objective: To develop nutritionally adequate, culturally acceptable, and environmentally sustainable dietary patterns using mathematical optimization.
Input Data Requirements:
- Food consumption data from national surveys (e.g., NHANES, WWEIA)
- Nutrient composition database (e.g., FNDDS)
- Food group classification system (e.g., FPED, WWEIA Food Categories)
- Environmental impact data (e.g., GHGE for food items)
- Food prices and cost data [19] [58]
Constraint Definition:
- Nutritional constraints: Define upper and lower bounds for energy, macronutrients, and micronutrients based on Dietary Reference Intakes
- Food consumption constraints: Set minimum and maximum consumption limits for food groups based on current consumption patterns
- Environmental constraints: Define acceptable GHGE boundaries relative to current dietary patterns
- Acceptability constraints: Limit degree of change from current consumption patterns [57] [58]
Optimization Procedure:
- Formulate objective function (minimize cost, GHGE, or dietary change)
- Implement model in optimization software (e.g., R, Python with optimization libraries)
- Validate model with sensitivity analysis
- Generate optimal dietary patterns
- Test nutrient adequacy through simulation analyses [57] [58]
Figure 2: Diet Optimization Experimental Workflow showing key methodological stages
Protocol for Within-Food-Group Diet Optimization
Objective: To improve nutritional adequacy and sustainability through substitutions within food groups while minimizing dietary change.
Food Group Classification:
- Classify individual food items into hierarchical food group structure
- Maintain sufficient granularity to capture nutrient variability within groups
- Define food groups based on culinary use and nutrient composition [57]
Modeling Approach:
- Calculate current consumption patterns at individual food level
- Define nutrient profiles for each food item
- Establish GHGE values for each food item
- Set constraints to limit total dietary change
- Implement optimization to minimize GHGE while meeting nutritional requirements [57]
Analysis Outputs:
- Optimized food quantities at individual food level
- Comparison of nutritional adequacy before and after optimization
- Calculation of GHGE reduction
- Quantification of degree of dietary change required [57]
Research Reagent Solutions
Table 3: Essential Research Resources for Dietary Optimization Studies
| Research Tool | Specifications | Application in Optimization Research |
|---|---|---|
| NHANES/WWEIA Dietary Data | Nationally representative survey data with 24-hour dietary recalls | Provides baseline consumption patterns for optimization models; enables population-specific analyses [19] |
| FNDDS (Food and Nutrient Database for Dietary Studies) | Comprehensive database with energy and 64 nutrients for ~7,000 foods | Serves as primary nutrient composition source for constraint definition in optimization models [19] |
| FPED (Food Pattern Equivalents Database) | Converts FNDDS foods into 37 USDA Food Patterns components | Enables food group-based optimization and adherence assessment to dietary guidelines [19] |
| GHGE Database for Foods | Life cycle assessment data expressing environmental impact in CO₂ equivalents | Allows incorporation of sustainability objectives into multi-criteria optimization [57] |
| Linear Programming Software | Optimization tools (e.g., R lpSolve, Python PuLP, GAMS) | Computational engines for solving linear and non-linear optimization problems [56] |
Implementation Considerations
Data Quality and Cultural Adaptations
The successful application of mathematical optimization in dietary pattern analysis depends critically on input data quality. High-quality, representative food consumption data and comprehensive nutrient databases are prerequisites for generating valid recommendations [56]. Additionally, optimization models must incorporate sociocultural factors to ensure the practical implementation of generated dietary patterns. This includes respecting traditional foodways, accounting for food accessibility issues, and considering culinary practices [56].
In sub-Saharan Africa, for example, optimization studies have explicitly prioritized locally available foods and traditional dietary patterns while addressing region-specific nutrient deficiencies [56]. Similarly, the development of the GR-UPFAST assessment tool in Greece demonstrates the importance of adapting international classification systems (like NOVA) to local food environments and consumption patterns [27].
Validation and Acceptability Testing
Optimized dietary patterns require rigorous validation before implementation. The 2025 Dietary Guidelines Advisory Committee employed diet simulation analyses to test whether diets adhering to updated USDA Food Patterns would achieve nutrient adequacy across diverse population subgroups [58]. These simulations incorporated variation in dietary intakes and tested robustness across different demographic and socioeconomic groups.
Consumer acceptance represents another critical validation dimension. Research indicates that the degree of dietary change required significantly influences acceptability, with smaller changes generally being more readily adopted [57]. Within-food-group optimization strategies demonstrate particular promise for enhancing acceptability while still achieving substantial improvements in nutritional adequacy and sustainability.
Overcoming Validation Challenges: Addressing Bias, Technical Limitations, and Implementation Barriers
Identifying and Mitigating Systematic Underreporting in Digital Dietary Records
Systematic underreporting of energy and nutrient intake is a pervasive challenge that undermines the validity of dietary assessment methods, including emerging digital tools. Despite technological advancements in digital dietary recording, evidence demonstrates a strong and consistent systematic underreporting of energy intake across adult and child studies [59]. This underreporting is not random but follows predictable patterns, varying significantly with body mass index (BMI) and affecting nutrients differentially [1] [59]. The fundamental limitation of self-reported dietary data persists even as assessment methods transition from traditional paper-based records to digital platforms including mobile applications with image recognition and barcode scanning capabilities [28] [60].
Understanding and addressing this systematic underreporting is crucial for macronutrient intake validation research, where accurate quantification of energy, carbohydrate, protein, and fat consumption forms the basis for establishing diet-health relationships and evaluating nutritional interventions. The problem is particularly salient in obesity research, where underreporting increases with BMI, potentially confounding studies of energy balance [59]. Recent meta-analyses confirm that dietary record apps consistently underestimate intake, with a pooled effect of -202 kcal/day for energy intake compared to reference methods [1]. This systematic error not only affects absolute intake values but also attenuates diet-disease relationships in epidemiological research, potentially obscuring important associations between nutrition and health outcomes [59].
Quantitative Evidence of Systematic Underreporting
Magnitude of Underreporting Across Assessment Methods
Table 1: Documented Underreporting in Dietary Assessment Methods
| Assessment Method | Reported Energy Underestimation | Affected Nutrients | Population Characteristics | Citation |
|---|---|---|---|---|
| Dietary Record Apps | -202 kcal/day (pooled effect) | Carbohydrates (-18.8 g/day), Fat (-12.7 g/day), Protein (-12.2 g/day) | General population | [1] |
| 7-day Food Diary | 34% less than TEE measured by DLW | Not specified | Obese women (BMI 32.9±4.6 kg/m²) | [59] |
| Traditional Self-report Instruments | 47% for protein intake | Protein specifically | Women undergoing weight loss treatment | [59] |
| Digital Food Records | Increasing with BMI | Macronutrients differentially | Higher BMI individuals | [28] [59] |
The evidence synthesized in Table 1 reveals consistent patterns of underreporting across different assessment methodologies. Digital dietary tools, despite their technological advantages, demonstrate significant underestimation of energy and nutrients when compared against objective biomarkers [1]. The problem is not merely one of magnitude but also of differential reporting, with protein being least underreported compared to other macronutrients [59]. This selective underreporting suggests that not all foods are omitted equally, with certain food categories being more susceptible to underreporting than others.
The relationship between underreporting and BMI presents a particular challenge for nutritional epidemiology. Research indicates that underreporting varies as a function of BMI, with individuals having higher BMI showing greater discrepancies between self-reported intake and objectively measured energy expenditure [59]. This systematic bias potentially confounds studies examining relationships between diet and obesity, as the measurement error is correlated with the outcome of interest. Furthermore, evidence suggests that underreporting is associated with concerns about body weight rather than weight status alone, occurring in individuals with anorexia nervosa who perceive themselves as having excess body fat [59].
Variability in Nutrient Reporting
Table 2: Nutrient-Specific Reporting Accuracy in Digital Dietary Records
| Nutrient/Food Category | Minimum Days for Reliable Estimate (r>0.8) | Reporting Accuracy Trends | Day-of-Week Effects | Citation |
|---|---|---|---|---|
| Water, Coffee, Total Food Quantity | 1-2 days | Higher accuracy | Minimal | [28] |
| Macronutrients (Carbohydrates, Protein, Fat) | 2-3 days | Moderate underreporting | Significant weekend effects | [28] |
| Micronutrients | 3-4 days | Higher variability | Not specified | [28] |
| Meat and Vegetables | 3-4 days | Category-dependent | Not specified | [28] |
The data in Table 2 highlights how reporting accuracy varies substantially across different nutrient types and food categories. While some aspects of diet, such as water and coffee consumption, can be reliably captured with minimal assessment days, other nutrients require more extended monitoring periods [28]. This variability has important implications for study design in macronutrient validation research, as the optimal assessment period differs depending on the nutrients of interest.
Temporal patterns significantly influence reporting accuracy, with studies revealing higher energy, carbohydrate, and alcohol intake on weekends, particularly among younger participants and those with higher BMI [28]. This day-of-week effect underscores the importance of including both weekdays and weekends in dietary assessment protocols, as exclusive focus on either period would yield systematically biased estimates of usual intake. Intraclass correlation coefficient analyses further demonstrate that specific day combinations outperform others for reliability, suggesting that strategic selection of assessment days can optimize data quality without increasing participant burden [28].
Experimental Protocols for Detecting Underreporting
Biomarker Validation Framework
The gold standard approach for detecting and quantifying systematic underreporting involves comparison of self-reported dietary intake against objective biomarkers. The following protocol outlines a comprehensive validation framework adapted from current methodological research:
Protocol 1: Multi-Method Validation Against Biomarkers
- Objective: To quantify the magnitude and patterns of systematic underreporting in digital dietary records by comparing against objective biomarkers of intake.
- Design: Prospective observational study with duration of 4 weeks [29].
- Participants: Target sample of 115 healthy volunteers, recruited based on specific eligibility criteria including stable body weight (±5% during last 3 months) and no medical conditions requiring therapeutic diets [29].
- Reference Biomarkers and Methods:
- Doubly Labeled Water (DLW): Administered according to standard protocols to measure total energy expenditure as a reference for energy intake under weight-stable conditions [29] [59].
- Urinary Nitrogen: Collected through 24-hour urine samples to provide an objective measure of protein intake [29].
- Serum Carotenoids: Measured via blood sampling as a biomarker for fruit and vegetable consumption [29].
- Erythrocyte Membrane Fatty Acids: Analyzed to validate reported intake of specific fatty acids and food sources [29].
- Digital Dietary Assessment: Participants complete digital dietary records using the designated application for a 2-week period, with prompts designed to capture real-time intake [29].
- Comparison Methods: Three interviewer-administered 24-hour dietary recalls conducted by trained nutrition professionals [29].
- Compliance Monitoring: Blinded continuous glucose monitoring serves as an objective method to assess compliance with dietary recording prompts and identify eating episodes [29].
- Statistical Analysis:
- Calculate mean differences between digital records and biomarker values using paired t-tests or Wilcoxon signed-rank tests.
- Assess correlations using Spearman's rank correlation coefficients.
- Develop Bland-Altman plots to visualize agreement and identify systematic biases.
- Apply the method of triads to quantify measurement error components from digital records, 24-hour recalls, and biomarkers in relation to true unknown intake [29].
Protocol for Identifying Participant-Specific Underreporting
Protocol 2: Individual-Level Underreporting Detection
- Objective: To develop and apply a standardized approach for identifying systematic underreporting at the individual participant level in digital dietary records.
- Plausibility Assessment:
- Calculate reported energy intake (rEI) as captured by the digital dietary record.
- Estimate resting energy expenditure (REE) using validated equations (e.g., Mifflin-St Jeor) based on measured height, weight, age, and sex.
- Determine physical activity level (PAL) through accelerometry or validated questionnaires.
- Calculate predicted total energy expenditure (pTEE) as: pTEE = REE × PAL.
- Apply the Goldberg cutoff method to identify implausible reporters by comparing the ratio of rEI to pTEE against established thresholds [59].
- Biological Plausibility Check:
- Compare reported protein intake against estimated requirements based on body weight (0.8 g/kg for adults).
- Assess the consistency of reported micronutrient intake with established deficiency thresholds.
- Data Quality Indicators:
- Analyze the number of food items reported per eating occasion.
- Assess the frequency of missing common food items (e.g., fats used in cooking, condiments, beverages).
- Evaluate the proportion of generic versus brand-specific food entries.
- Examine patterns of repeated food entries suggesting limited dietary variety.
- Statistical Analysis:
- Classify participants as under-reporters, plausible reporters, or over-reporters based on multiple criteria.
- Conduct sensitivity analyses excluding under-reporters to assess impact on study outcomes.
- Develop correction factors based on identified patterns of underreporting.
Mitigation Strategies for Systematic Underreporting
Technical and Design-Based Solutions
Modern digital dietary assessment tools offer several technological advantages that can be leveraged to reduce systematic underreporting:
Enhanced User Experience Design:
- Implement image-based food capture with automatic portion size estimation to reduce participant burden and improve quantification accuracy [28] [60].
- Incorporate barcode scanning for packaged foods to automatically retrieve nutritional information from comprehensive databases, minimizing manual entry errors [28].
- Utilize machine learning algorithms for food identification and nutrient estimation from food images, providing real-time feedback to users [28].
- Design user-friendly interfaces with autocomplete functionality and frequently consumed food lists to streamline the logging process [60].
Contextual Data Collection:
- Integrate ecological momentary assessment (EMA) techniques to capture dietary intake in real-time, reducing reliance on memory [29] [61].
- Implement experience sampling methodology with strategically timed prompts to record recent intake, minimizing recall bias [29].
- Incorporate contextual information such as location, time, and social environment to identify patterns associated with underreporting [61].
Data Quality Assurance:
- Develop automated data quality checks that flag improbable entries (e.g., extremely low energy intake, missing meals) in real-time.
- Create prompting systems that request clarification for ambiguous entries or potential omissions.
- Implement portion size estimation aids using reference objects or augmented reality to improve quantification accuracy.
Analytical Correction Methods
When underreporting cannot be prevented through design improvements, statistical approaches can help mitigate its impact on research outcomes:
Protocol 3: Statistical Correction for Systematic Underreporting
- Objective: To apply statistical methods that correct for systematic underreporting in digital dietary records.
- Energy Adjustment Methods:
- Calculate energy density of diets (nutrient intake per 1000 kcal) to account for systematic underreporting of total intake.
- Apply nutrient residual models by regressing nutrient intake on total energy intake and using the residuals in analyses.
- Utilize multivariate nutrient density methods that express nutrients as percentages of total energy intake.
- Measurement Error Models:
- Implement regression calibration methods using biomarker substudies to estimate measurement error structure.
- Apply method of triads incorporating digital records, traditional recalls, and biomarkers to estimate true intake.
- Develop correction factors based on established underreporting patterns by BMI category, age, and sex.
- Multiple Imputation Approaches:
- Use biomarker data from validation subsamples to impute calibrated intake values for the full study population.
- Develop multivariate imputation models that account for correlated underreporting across nutrients.
- Sensitivity Analyses:
- Conduct analyses excluding participants identified as under-reporters based on Goldberg cutoffs.
- Perform quantile regression to assess differential effects across the intake distribution.
- Apply probabilistic sensitivity analyses to quantify uncertainty introduced by underreporting.
Research Reagent Solutions for Dietary Assessment Studies
Table 3: Essential Research Reagents and Tools for Dietary Intake Validation
| Reagent/Tool Category | Specific Examples | Research Application | Key Features | Citation |
|---|---|---|---|---|
| Digital Dietary Assessment Platforms | MyFoodRepo app, ASA24, ESDAM | Primary data collection for dietary intake | Image recognition, barcode scanning, automated nutrient database linkage | [28] [29] [62] |
| Biomarker Validation Tools | Doubly labeled water (DLW), Urinary nitrogen, Serum carotenoids, Erythrocyte membrane fatty acids | Objective verification of reported intake | Quantifies energy expenditure, protein intake, fruit/vegetable consumption, fatty acid intake | [29] [59] |
| Reference Nutritional Databases | Swiss Food Composition Database, USDA FNDDS, Open Food Facts | Standardized nutrient composition data | Comprehensive coverage, regular updates, integration with assessment tools | [28] [19] |
| Portion Estimation Aids | Standard portion sizes, Image libraries, Augmented reality tools | Improved quantification of food intake | Visual references, standardized weights, 3D modeling for volume estimation | [28] |
| Physical Activity Monitors | Accelerometers, Pedometers, Heart rate monitors | Assessment of energy expenditure | Objective movement data, estimation of physical activity level for plausibility checks | [59] |
| Data Quality Control Tools | Automated plausibility checks, Goldberg cutoff calculators, Data cleaning algorithms | Identification of systematic underreporting | Real-time feedback, statistical thresholds for implausible reports | [59] |
The research reagents detailed in Table 3 represent essential components of a comprehensive approach to identifying and mitigating systematic underreporting in digital dietary records. These tools enable researchers to implement the multi-faceted strategy necessary for addressing this complex methodological challenge. By integrating digital assessment platforms with biomarker verification and robust data quality controls, researchers can significantly enhance the validity of macronutrient intake data collected through digital means.
The National Institutes of Health has supported the development of several key resources in this domain, including the Automated Self-Administered 24-hour Dietary Assessment Tool (ASA24), which provides researchers with a freely available, comprehensive system for dietary data collection [62] [61]. Similarly, the development of specialized databases like the USDA Food and Nutrient Database for Dietary Studies (FNDDS) and the USDA Food Pattern Equivalents Database (FPED) enables standardized analysis of food group and nutrient intakes across different studies [19]. These resources, combined with emerging biomarker technologies, create a powerful toolkit for advancing the field of dietary assessment methodology.
Systematic underreporting remains a significant challenge in digital dietary assessment, but a multifaceted approach incorporating technological innovations, optimized study designs, and advanced statistical methods can substantially mitigate its impact. The protocols and frameworks presented herein provide researchers with practical strategies for identifying, quantifying, and correcting for systematic underreporting in macronutrient validation research. By implementing these approaches, the research community can enhance the validity of digital dietary records and strengthen the evidence base linking diet to health outcomes.
Future directions in this field should focus on further development of objective intake biomarkers, refinement of machine learning approaches for automated food recognition, and creation of standardized correction methods that can be applied across diverse populations. As digital dietary assessment methods continue to evolve, maintaining rigorous attention to measurement error sources will be essential for advancing nutritional epidemiology and clinical nutrition research.
Dietary assessment for macronutrient intake validation research faces significant complexities when applied to special populations. These groups, including individuals with eating disorders (EDs), those from low-income settings, and pediatric patients, present unique physiological, psychological, and socioeconomic confounding factors that can substantially impact data quality and interpretation. Understanding these confounders is essential for developing validated assessment protocols that yield meaningful results in nutritional epidemiology and clinical trials. This application note examines key confounding factors and provides tailored methodological guidance for research involving these vulnerable populations, framed within the broader context of dietary assessment validation science.
Socioeconomic Confounders in Eating Disorder Research
Empirical Evidence of Socioeconomic Influences
Table 1: Socioeconomic Factors and Eating Disorder Symptoms in Adolescents (ALSPAC Study Findings) [63] [64] [65]
| Socioeconomic Indicator | Association with ED Symptoms | Effect Size | Population |
|---|---|---|---|
| Financial Hardship | Increased odds of disordered eating | OR: 1.06 (95% CI: 1.04-1.10) per 1-point increase | Adolescents aged 14-18 years |
| Parental Education | Increased odds of disordered eating | OR: 1.80 (95% CI: 1.46-2.23) for compulsory vs. university education | Adolescents aged 14-18 years |
| Financial Hardship | Increased weight and shape concerns | Coefficient: 0.02 (95% CI: 0.01-0.04) | Adolescents aged 14-18 years |
| Financial Hardship | Increased body dissatisfaction | Coefficient: 0.22 (95% CI: 0.06-0.37) | Adolescents aged 14-18 years |
| Household Income <$75,000 | Increased odds of binge-eating disorder | AOR: 2.05 (95% CI: 1.21-3.46) | Early adolescents (10-14 years) |
Recent longitudinal evidence challenges historical assumptions that eating disorders primarily affect affluent populations. Data from the Avon Longitudinal Study of Parents and Children (ALSPAC) demonstrates that adolescents from socioeconomically deprived backgrounds show significantly higher rates of disordered eating behaviors, body dissatisfaction, and weight and shape concerns [63] [65]. These findings suggest substantial socioeconomic patterning in eating disorder symptoms, with financial hardship and lower parental educational attainment serving as significant risk factors.
The ALSPAC study, which followed 7,824 participants from childhood through adolescence, employed comprehensive socioeconomic assessments including parental income, education, occupation, financial hardship scores, and area-level deprivation indices [63] [64]. The findings indicate that each 1-point increase on a financial hardship scale (range: 0-15) was associated with a 6% increase in odds of disordered eating behaviors, while lower parental education was associated with 80% higher odds of disordered eating compared to children of university-educated parents [63].
Access to Care as a Confounding Variable
Table 2: Barriers to Eating Disorder Diagnosis and Treatment in Low-Income Populations [63] [65] [66]
| Barrier Category | Specific Challenges | Impact on Research |
|---|---|---|
| Diagnostic Barriers | Under-identification in clinical settings, attribution of symptoms to other causes, lack of provider awareness | Selection bias in clinical samples, underrepresentation in treatment studies |
| Treatment Access | Financial constraints, limited insurance coverage, transportation challenges, fewer specialized services | Differential access to care affecting longitudinal outcomes |
| Cultural & Linguistic | Language barriers, cultural stigma, mistrust of healthcare systems | Reduced participation and retention in research studies |
| Structural | Fewer referrals from primary care, longer pathways to specialized care | Delayed intervention affecting disease progression studies |
Research indicates that individuals from lower socioeconomic backgrounds face significant barriers in accessing eating disorder diagnosis and treatment, creating substantial selection bias in clinical studies [63] [65]. Register-based studies that derive diagnoses from clinical records may consequently show higher incidence of eating disorders in affluent populations, while population-based studies capturing self-reported symptoms reveal higher prevalence in deprived groups [63]. This discrepancy highlights how healthcare access inequalities can confound epidemiological understanding of eating disorder distribution across socioeconomic groups.
Pediatric-Specific Confounding Factors
Developmental Considerations in Pediatric Eating Disorders
Table 3: Developmental Considerations in Pediatric Eating Disorder Assessment [67] [68]
| Developmental Factor | Assessment Challenge | Methodological Adaptation |
|---|---|---|
| Cognitive Development | Limited abstract reasoning ability, concrete thinking | Use of visual aids, simplified response formats, age-appropriate language |
| Metabolic Requirements | Higher energy and nutrient needs for growth | Adjustment of reference standards for age and developmental trajectory |
| Psychological Development | Emerging body image, peer influence susceptibility | Developmentally appropriate assessment tools, consideration of social context |
| Communication Skills | Limited ability to describe internal states, emotions | Multi-informant approach (parent, teacher, child reports) |
| Family Dynamics | Parent-child interactions around food and eating | Inclusion of family system assessment, observation of mealtime behaviors |
Pediatric populations present unique developmental considerations that confound dietary assessment. The peak age of eating disorder onset occurs at approximately 16 years, with increasing cases observed in early adolescence and even childhood [67] [68]. Assessment tools must accommodate developmental variations in cognitive ability, emotional awareness, and communication skills. Furthermore, diagnostic criteria developed for adults may not adequately capture clinical presentations in younger populations, requiring specialized assessment protocols.
Early-onset eating disorders (before age 14) show distinct clinical patterns, including higher likelihood of previous psychiatric disorders such as depression, obsessive-compulsive disorder, or anxiety [68]. Additionally, children and adolescents participating in sports emphasizing thinness or weight requirements (e.g., gymnastics, dance, athletics) demonstrate elevated eating disorder risk, introducing potential confounding through activity-specific subcultures [68].
Validation Challenges in Pediatric Populations
Standard dietary assessment methods face particular challenges in pediatric populations with eating disorders. Standard food records and 24-hour recalls assume certain cognitive abilities and memory functions that may be compromised in both developmental eating disorders and associated states of malnutrition [4]. Research indicates that starvation symptoms impact cognitive function, potentially affecting a child's ability to accurately describe food portion sizes and frequency of consumption [4].
Binge eating episodes in pediatric populations present additional assessment complications. These episodes often involve highly stressful situations with loss of control and consumption of large amounts of food in short periods, which may influence episodic memory of the type and quantity of food consumed [4]. This is particularly challenging in early adolescents who may have limited metacognitive abilities to accurately recall these experiences.
Eating Disorder-Specific Methodological Challenges
Pathophysiology-Driven Assessment Barriers
The core psychopathology of eating disorders introduces unique methodological challenges for dietary assessment. Individuals with anorexia nervosa may exhibit cognitive changes associated with starvation that impact memory, attention, and executive function [4]. Those with bulimia nervosa and binge-eating disorder often experience shame and secrecy around binge episodes, leading to underreporting. Ritualistic eating behaviors in various eating disorders may complicate standard assessment approaches that assume typical meal patterns.
Dietary restriction patterns also present validation challenges. Research indicates that dietary assessment accuracy may vary with intake level, with one pilot study suggesting that measurement of dietary protein and iron becomes more accurate as intake increases in eating disorder populations [4]. This pattern contradicts assumptions of consistent measurement error across intake levels in general population validation studies.
Supplement Use and Unconventional Behaviors
Eating disorder populations frequently engage with dietary supplements, laxatives, diuretics, and other substances to influence weight or shape, introducing confounding factors not typically encountered in general population dietary assessment [4]. One study found that significant correlations between dietary iron and serum biomarkers were only apparent when dietary supplements were included in assessments [4]. This highlights the critical importance of comprehensive questioning about non-food substance use in eating disorder research.
Recommended Experimental Protocols
Protocol for Dietary Assessment in Low-Income and Eating Disorder Populations
Experimental Workflow: Dietary Assessment in Special Populations
Protocol Title: Multi-Method Dietary Assessment with Biomarker Validation in Special Populations
Objective: To validate dietary assessment methods against nutritional biomarkers in eating disorder populations across socioeconomic strata.
Methodology Details:
Participant Characterization:
- Collect comprehensive socioeconomic data: household income, parental education, financial hardship scale (0-15), occupation, and area-level deprivation indices [63] [64]
- Document eating disorder diagnosis, duration, and specific behaviors (binge eating, purging, restriction)
- Assess psychological comorbidities and cognitive function status
- Record supplement and medication use
Dietary Assessment Methods:
- Diet History Interview: Administered by trained dietitian with expertise in eating disorders, including targeted questioning on restrictive periods, binge episodes, and typical eating patterns [4]
- 24-Hour Recalls: Multiple recalls on non-consecutive days (including weekdays and weekends) using the Automated Self-Administered 24-hour recall (ASA-24) system when possible [7]
- Food Records: 3-4 day records with detailed portion size estimation aids, acknowledging potential reactivity in eating disorder populations [7]
- Food Frequency Questionnaires: Semi-quantitative FFQs assessing habitual intake over previous 3-6 months, with careful attention to foods commonly associated with binge episodes [7]
Biomarker Collection:
- Blood collection within 7 days of dietary assessment for nutritional biomarkers [4]
- Analysis of protein (albumin), iron (ferritin, total iron-binding capacity), lipids (cholesterol, triglycerides), and other relevant biomarkers
- Consideration of recovery biomarkers (doubly labeled water, urinary nitrogen) when feasible [7]
Protocol for Pediatric-Specific Dietary Assessment
Experimental Workflow: Pediatric Dietary Assessment
Objective: To develop and validate age-appropriate dietary assessment methods for pediatric populations with eating disorders.
Methodology Details:
Developmentally Appropriate Assessment Tools:
- Implement visual aids including food models, portion size images, and age-appropriate digital interfaces [69]
- Conduct cognitive interviewing to ensure comprehension of dietary assessment questions
- Modify recall periods to match developmental capacity (shorter periods for younger children)
- Use concrete examples and age-appropriate language for describing foods and eating behaviors
Multi-Informant Approach:
- Collect dietary information from both child and parent reports
- Obtain school meal records when available
- Incorporate teacher observations of meal behaviors when appropriate
- Resolve discrepancies between reports through structured clarification protocols
Family Context Assessment:
- Document family meal patterns and food environment
- Assess parental attitudes about weight and dieting
- Evaluate family history of eating disorders and related mental health conditions
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Dietary Assessment in Special Populations
| Research Tool | Specific Application | Technical Considerations |
|---|---|---|
| ASA-24 (Automated Self-Administered 24-hour Recall) | Self-administered 24-hour dietary recall | Reduces interviewer burden, available free for researchers, may require literacy and technology access [7] |
| Food Frequency Questionnaires (FFQ) | Assessment of habitual dietary intake over extended periods | Can be nutrient-specific or population-specific; must be validated for target population; limited food item list [7] |
| Diet History Interview Protocol | Comprehensive dietary assessment by trained clinician | Requires standardized protocol and interviewer training; effective for capturing complex eating patterns [4] |
| Visual Aid Tools for Portion Estimation | Enhanced portion size assessment in children and low-literacy populations | Food models, photographs, or digital interfaces; must be culturally appropriate [69] |
| Nutritional Biomarkers | Objective validation of self-reported dietary intake | Serum triglycerides, cholesterol, albumin, iron studies; timing relative to dietary assessment critical [4] |
| Socioeconomic Assessment Batteries | Standardized measurement of socioeconomic confounders | Financial hardship scales, education and occupation coding, area-level deprivation indices [63] [64] |
| Eating Disorder Examination (EDE) or KSADS | Diagnostic characterization and symptom severity | Structured interviews requiring trained administrators; KSADS specifically designed for child/adolescent populations [66] |
Data Analysis Considerations for Confounding Adjustment
Analysis of dietary assessment data in special populations requires specialized statistical approaches to address confounding. Recommended methodologies include:
- Multivariable Regression Models: Adjust for socioeconomic indicators (mutually adjusting income, education, occupation), demographic factors, and clinical characteristics [63] [64]
- Stratified Analysis: Conduct separate analyses across socioeconomic strata, age groups, and diagnostic categories to identify differential effects
- Measurement Error Modeling: Account for systematic underreporting or overreporting using biomarker calibration studies [7] [4]
- Multiple Imputation: Address missing data, particularly from higher attrition rates in lower socioeconomic groups [63] [65]
Analytical approaches should avoid adjusting for variables on the causal pathway between socioeconomic position and eating outcomes (e.g., body mass index, adverse life experiences), which may introduce bias [63] [64]. Directed acyclic graphs (DAGs) are recommended for identifying appropriate confounding adjustment sets based on explicit causal assumptions.
Dietary assessment validation research in special populations requires careful consideration of population-specific confounding factors. Socioeconomic status, developmental stage, and eating disorder psychopathology significantly impact both dietary behaviors and assessment accuracy. Methodological adaptations including multi-method assessment, biomarker validation, developmentally appropriate tools, and comprehensive confounding measurement are essential for generating valid, meaningful data. Future research should prioritize the development and validation of targeted dietary assessment methods that address the unique challenges posed by these populations, with particular attention to reducing socioeconomic disparities in eating disorder research participation and representation.
Accurate dietary assessment is fundamental for validating macronutrient intake in research, yet accurately measuring dietary exposures through self-report is notoriously difficult due to both random and systematic measurement error [7]. Traditional methods, including food records, 24-hour recalls, and food frequency questionnaires, face challenges such as participant burden, reactivity, and measurement inaccuracies [7]. The emergence of digital tools, particularly image-based dietary assessment applications, offers potential to mitigate some of these limitations by standardizing data collection and reducing participant burden [12]. However, the validity of these tools and the nutritional data they produce is contingent upon two foundational elements: standardized validation protocols and robust, culturally-relevant food composition databases. This article details technical optimizations in these areas, providing application notes and protocols for researchers and scientists engaged in macronutrient intake validation studies.
Standardizing Dietary Assessment Validation Protocols
Comparative Validation Framework
A critical step in technical optimization is the validation of new dietary assessment tools against established reference methods. The following protocol, adapted from a study validating the "Ghithaona" smartphone application, provides a structured framework for this process [12].
- Objective: To assess the relative validity of a novel dietary assessment tool (e.g., a smartphone application) for measuring energy and macronutrient intake against a traditional 3-Day Food Record (3-DFR).
- Population: A sample of approximately 70 participants is often sufficient for a method comparison study, though larger samples are preferable. The population should be representative of the intended end-users (e.g., university students, specific patient groups) and must meet inclusion criteria such as device ownership and ability to use the application [12].
- Study Design:
- A within-subjects, cross-over design is recommended where each participant utilizes both the novel tool and the reference method.
- To minimize learning effects and order bias, dietary intake should be recorded using the novel application over a period (e.g., 2 consecutive weekdays and 1 weekend day), followed by a washout period. The reference 3-DFR is then completed in the subsequent week on corresponding days [12].
- Participant anthropometrics (e.g., self-reported weight and height) and sociodemographic data should be collected at baseline.
- Data Analysis:
- Mean Differences: Use paired t-tests or Wilcoxon signed-rank tests to compare mean intakes of energy and macronutrients between the two methods.
- Correlation: Ascertain agreement using Pearson correlation coefficients.
- Bland-Altman Plots: Construct Bland-Altman plots to visualize the limits of agreement between the two methods and identify any systematic bias [12].
Table 1: Key Outcomes from a Smartphone App Validation Study [12]
| Metric | 3-DFR Mean Intake | App Mean Intake | P-Value | Correlation Coefficient (r) |
|---|---|---|---|---|
| Energy (kcal) | 2254 kcal | 2201 kcal | > 0.05 | 0.58 |
| Carbohydrates (g) | 286.1 g | 280.3 g | > 0.05 | 0.54 |
| Fat (g) | 87.7 g | 86.6 g | > 0.05 | 0.47 |
| Protein (g) | 79.9 g | 78.5 g | > 0.05 | 0.26 |
Meta-Analysis of Validation Studies
A systematic review and meta-analysis of 14 validation studies performed on dietary record apps reveals critical insights for protocol standardization. The pooled data indicates that apps tend to underestimate consumption, with a mean difference of -202 kcal/day for energy intake compared to traditional methods [1]. High heterogeneity (I² = 72%) across studies was a major finding, largely attributed to the use of different food-composition tables (FCTs) between the app and the reference method. When the same FCT was used, heterogeneity dropped to 0% and the underestimation was reduced to a non-significant -57 kcal/day [1]. This underscores that variance in nutrient databases is a primary source of measurement error, and protocols must mandate the use of a unified FCT for both the tool being validated and the reference method to ensure accurate results.
The following workflow diagram outlines the key stages of a robust validation study, from participant recruitment to data synthesis.
Validation study workflow
Optimizing Food Composition Databases
Core Database Structures and Integration
The accuracy of any dietary assessment, digital or traditional, is fundamentally limited by the quality and comprehensiveness of the Food Composition Database (FCDB) it relies upon. Optimizing FCDBs involves structuring them for both comprehensiveness and interoperability with established national food pattern models.
Table 2: Essential Components of an Optimized Food Composition Database
| Database Component | Description | Function in Dietary Assessment |
|---|---|---|
| Core Nutrient Data | Provides energy and nutrient values for thousands of foods and beverages (e.g., for energy and 64 nutrients) [19]. | Serves as the foundational dataset for calculating individual nutrient intakes from reported food consumption. |
| Food Pattern Equivalents | Converts consumed foods into components of standard dietary patterns (e.g., 37 USDA Food Pattern components) [19]. | Enables the assessment of diet quality and adherence to dietary guidelines by quantifying intake of food groups (e.g., whole fruits, refined grains). |
| Culturally-Tailored Food Items | Includes locale-specific foods, traditional dishes, and customary portion sizes (e.g., as in the "Palestinian Food Atlas") [12]. | Ensures the database is relevant to the study population, reducing misclassification and portion size estimation errors. |
| Hierarchical Food Categories | Organizes foods into mutually exclusive categories based on use and nutrient content (e.g., 167 WWEIA categories) [19]. | Facilitates the analysis of food sources of nutrients and dietary components, aiding in public health monitoring. |
The relationship between these database components and their role in supporting research and public health is illustrated below.
Food database structure and applications
Protocol for Database Enhancement and Management
A proactive, science-based approach to database management is essential for maintaining its relevance and accuracy. The following protocol, reflective of the FDA's Human Foods Program priorities, outlines a continuous improvement cycle [70]:
- Premarket Review Optimization: Streamline processes for evaluating manufacturer submissions for new food ingredients, additives, and Generally Recognized as Safe (GRAS) substances to ensure novel products are incorporated into the FCDB in a timely manner [70].
- Post-Market Signal Detection and Prioritization: Implement advanced tools, such as AI-powered horizon-scanning engines (e.g., Warp Intelligent Learning Engine - WILEE), to monitor the food supply for new data, emerging ingredients, and trends. This informs the prioritization of substances for re-assessment [70].
- Systematic Re-assessment: Establish a public-facing framework and list for prioritizing chemicals and nutrients for post-market assessment based on new scientific evidence, ensuring FCDBs reflect current safety and nutritional science [70].
- Stakeholder Engagement and Data-Sharing: Develop formal agreements with industry and international partners to facilitate food safety and composition data sharing. This collaborative approach maximizes resources and enhances the depth and accuracy of the FCDB [70].
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and digital tools required for conducting validation research and maintaining food composition databases.
Table 3: Essential Research Reagents and Tools for Dietary Assessment Validation
| Item / Solution | Function in Research | Specification / Example |
|---|---|---|
| National Dietary Dataset | Provides nationally representative consumption data to inform study design and benchmark findings. | "What We Eat in America" (WWEIA), NHANES [19]. |
| Reference Food Database | The authoritative source of nutrient values used as the standard for validating new tools or updating other databases. | USDA Food and Nutrient Database for Dietary Studies (FNDDS) [19]. |
| Biochemical Recovery Biomarkers | Objective, non-self-report measures used to validate the accuracy of energy and nutrient intake data. | Doubly labeled water for energy intake; urinary nitrogen for protein intake [7]. |
| Dietary Assessment Application | A digital tool for real-time, image-based food recording; reduces memory bias and participant burden. | Applications like "Ghithaona," tailored with culturally-specific food lists and portion sizes [12]. |
| Contrast Checker Tool | Ensures that all text and user interface elements in digital tools meet WCAG accessibility guidelines (e.g., 4.5:1 ratio for normal text), guaranteeing usability for all participants [71]. | WebAIM Contrast Checker or similar tools to verify color contrast ratios [72]. |
| Genomic Surveillance Network | A network of labs that performs whole-genome sequencing on foodborne pathogens to improve food safety data and trace contamination sources. | GenomeTrakr network data integrated into platforms like PN 2.0 [70]. |
Participant-related challenges represent a significant source of measurement error in dietary assessment for macronutrient intake validation research. These methodological biases can substantially impact data quality, potentially obscuring valid diet-health relationships and compromising the scientific integrity of nutritional studies [7]. This application note addresses three fundamental participant-related challenges: literacy and cognitive burden, compliance and participant burden, and social desirability and approval biases. We provide evidence-based protocols and analytical frameworks to identify, quantify, and mitigate these sources of error, thereby enhancing the validity of macronutrient intake assessment in research settings. The strategies outlined are particularly crucial for studies aiming to quantify absolute intake of proteins, fats, and carbohydrates, where precision is paramount for validating biomarkers and establishing dose-response relationships.
Social desirability bias introduces systematic error by prompting participants to alter their reported intake of foods perceived as socially desirable or undesirable. The table below summarizes key quantitative findings on the magnitude and direction of these effects across different population subgroups.
Table 1: Quantified Effects of Social Desirability and Approval Biases on Dietary Reporting
| Bias Type | Population | Effect Size | Direction of Effect | Reference |
|---|---|---|---|---|
| Social Desirability | Middle-aged adults | ~50 kcal/point on social desirability scale (~450 kcal over interquartile range) | Downward bias in energy reporting | [73] |
| Social Desirability | Women vs. Men | Effect approximately twice as large in women | Greater under-reporting in women | [73] |
| Social Desirability | Individuals with high fat/energy intake | Largest downward bias | Selective under-reporting of "bad" foods | [73] |
| Social Approval | Young adult females vs. males | Significantly higher in females (p=0.009) | Positive correlation with overall diet quality (p=0.002) | [74] |
| Social Approval | Young adult females | Significant associations | Positive correlation with dairy (p<0.001); Negative with vegetables (p=0.045) | [74] |
Experimental Protocols for Bias Assessment and Mitigation
Protocol 1: Assessment of Social Desirability and Approval Biases
Objective: To quantitatively measure social desirability and social approval traits in study participants for use as covariates in statistical adjustment of dietary intake data.
Materials:
- Marlowe-Crowne Social Desirability Scale Short-Form (SDS)
- Martin-Larsen Approval Motivation Scale (AMS)
- Standardized administration environment (in-person or digital)
Procedure:
- Baseline Assessment: Administer both SDS and AMS at study enrollment, prior to any dietary data collection.
- Standardized Instructions: Provide participants with neutral instructions emphasizing that there are no right or wrong answers.
- Scale Administration:
- For SDS, participants respond to 10 items (e.g., "I'm always willing to admit it when I make a mistake") using a dichotomous (True/False) format.
- For AMS, participants rate 20 items (e.g., "I sometimes tell lies if I have to") on a 5-point Likert scale from "strongly disagree" to "strongly agree."
- Scoring:
- Calculate total SDS score by summing responses indicating socially desirable responses (range 0-10).
- Calculate total AMS score by summing all responses after reverse-coding appropriate items (range 20-100).
- Statistical Application:
- Include continuous SDS and AMS scores as covariates in multivariate models analyzing macronutrient intake data.
- Conduct stratified analyses for participants scoring above the 75th percentile on either scale to assess differential reporting patterns.
Validation Notes: These scales have demonstrated internal consistency with Cronbach alpha coefficients ranging from 0.61-0.93 in previous nutritional studies [75] [74]. Research indicates these traits are relatively stable, typically requiring only baseline assessment except in long-term studies (>1 year) where re-administration at interim periods may be warranted.
Protocol 2: Digital Dietary Assessment with Reduced Literacy Demands
Objective: To implement a dietary assessment method that minimizes literacy and cognitive barriers while capturing habitual macronutrient intake.
Materials:
- Smartphone with camera capability
- MyFoodRepo or similar dietary tracking application with image capture and barcode scanning
- Integrated food composition database
Procedure:
- Participant Training:
- Conduct a 30-minute individualized training session on application use.
- Provide visual guides for optimal food photography.
- Demonstrate barcode scanning for packaged foods.
- Data Collection:
- Instruct participants to capture images of all foods and beverages before and after consumption.
- Prompt participants to scan barcodes of packaged food items when available.
- For mixed dishes, encourage brief voice memos describing composition.
- Data Processing:
- Use automated image recognition for food identification where possible.
- Employ trained annotators to review portions, segmentations, and food classifications.
- Implement direct communication channel between annotators and participants to clarify uncertainties.
- Duration:
Validation Notes: This approach has demonstrated high adherence rates in digital cohorts, with participants logging over 315,000 meals across 23,335 participant days [28]. Image-based methods reduce reliance on memory and literacy while providing objective records of food consumption.
Protocol 3: Compliance Monitoring in Dietary Assessment Studies
Objective: To objectively monitor and enhance participant compliance with dietary assessment protocols.
Materials:
- Continuous glucose monitor (CGM) as objective reference for eating episodes
- Digital dietary assessment platform with timestamp capability
- Protocol adherence checklist
Procedure:
- Baseline Setup:
- Apply CGM to participants at study initiation.
- Synchronize timestamps between CGM and dietary assessment application.
- Compliance Assessment:
- Compare CGM-derived eating episodes (glucose excursions) with self-reported eating occasions.
- Calculate compliance rate as: (Number of CGM-correlated eating episodes / Total number of CGM-detected eating episodes) × 100.
- Adherence Enhancement:
- Implement automated reminder systems for data entry.
- Provide real-time feedback on data completeness.
- Establish incentive structures for protocol adherence (e.g., compensation tiers based on completeness).
- Participant Support:
- Assign study staff for technical troubleshooting.
- Conduct mid-study check-ins to address challenges.
- Simplify reporting requirements based on participant feedback.
Validation Notes: Blinded continuous glucose monitoring serves as an objective method to assess compliance with dietary assessment prompts [29]. Studies implementing similar compliance protocols have achieved participation rates sufficient for detecting correlation coefficients of ≥0.30 with 80% power [29].
Research Reagent Solutions
Table 2: Essential Materials and Tools for Dietary Assessment Research
| Item | Specification | Research Application | Validation Evidence |
|---|---|---|---|
| Marlowe-Crowne Social Desirability Scale Short-Form | 10-item dichotomous scale | Measures defensive tendency to avoid criticism | Cronbach alpha 0.61-0.93 in nutritional studies [75] [74] |
| Martin-Larsen Approval Motivation Scale | 20-item Likert scale | Measures need for positive responses in testing situations | Differentiates from social desirability; associated with dietary misreporting [74] |
| MyFoodRepo Digital Platform | Image recognition, barcode scanning, manual entry | Reduces literacy demands for dietary assessment | Validated against national dietary surveys; 76.1% entries via photographs [28] |
| Doubly Labeled Water (DLW) | ²H₂¹⁸O isotopic measurement | Objective measure of total energy expenditure as reference | Gold standard for validating energy intake assessment [29] [14] |
| 24-Hour Dietary Recall (24HR) | Multiple-pass interview method | Reference method for self-reported dietary intake | Less biased for energy estimation than FFQs; requires multiple administrations [7] |
| Continuous Glucose Monitor (CGM) | Interstitial glucose measurement | Objective reference for eating episode timing | Detects unreported eating occasions for compliance validation [29] |
Workflow Diagrams for Participant Screening and Dietary Assessment
Figure 1: Participant Screening and Method Selection Workflow. This diagram outlines the sequential process for evaluating participant characteristics and assigning appropriate dietary assessment methods to minimize measurement error.
Figure 2: Dietary Assessment and Validation Protocol. This workflow illustrates the process for determining adequate assessment duration and integrating biomarker validation to establish habitual macronutrient intake.
Addressing participant-related challenges in dietary assessment requires a multifaceted approach that recognizes the interconnected nature of literacy barriers, compliance issues, and social desirability biases. The protocols and frameworks presented here provide researchers with practical tools to enhance the validity of macronutrient intake data through method selection tailored to participant characteristics, objective compliance monitoring, and statistical adjustment for measured biases. Implementation of these strategies is particularly crucial for studies validating macronutrient biomarkers or establishing precise diet-health relationships, where measurement error can significantly impact scientific conclusions and subsequent public health recommendations. Future methodological development should continue to integrate emerging technologies with psychological insights to further minimize participant-introduced measurement error in nutritional research.
Accurate dietary assessment is fundamental to establishing valid links between nutritional intake and health outcomes, forming the critical evidence base for public health policies and clinical guidelines [7] [76]. However, nutritional research findings, particularly from observational studies, have been repeatedly criticized for their potential lack of trustworthiness, often stemming from various forms of bias that can distort the true diet-disease relationship [76] [77]. The trustworthiness of nutritional evidence is increasingly questioned when results from large prospective cohort studies fail to be replicated in randomized controlled trials (RCTs), as witnessed with fiber intake and colorectal cancer risk or vitamin E and cardiovascular disease [76]. This discrepancy highlights the critical need for rigorous, standardized frameworks to evaluate risk of bias (RoB) in dietary studies, especially those focused on validating dietary assessment methods against objective criteria [76].
The challenges in nutritional research are multifaceted, encompassing both methodological and human factors. Investigator bias represents a particularly insidious challenge, defined as "acts of omission or commission that arise from ignorance, hubris or excessive attachment to beliefs" [77]. This bias can infiltrate multiple research stages—from question formulation and method selection to analytical techniques and interpretation—potentially misinforming dietary guidelines and eroding public trust in nutrition science [77]. Furthermore, the inherent limitations of self-reported dietary data, including recall bias, social desirability bias, and measurement error, compound these challenges [7] [76]. Without robust quality assessment frameworks, the credibility of dietary validation studies remains questionable, undermining evidence-based nutrition policy and practice.
Established Risk of Bias Assessment Tools
Frameworks for Different Study Designs
Systematic evaluation of dietary validation studies requires distinct tools tailored to different study designs. The table below summarizes the primary RoB assessment tools applicable to nutritional research:
Table 1: Risk of Bias Assessment Tools for Nutritional Studies
| Tool Name | Target Study Design | Key Domains Assessed | Strengths | Common Applications in Nutrition |
|---|---|---|---|---|
| Cochrane RoB 2.0 [76] | Randomized Controlled Trials | Selection, performance, attrition, detection, reporting biases | Well-established, validated, includes adherence assessment | Dietary intervention trials, supplement studies |
| ROBINS-I [76] | Non-Randomized Studies | Confounding, participant selection, intervention classification, deviations, missing data, outcome measurement, selective reporting | Specifically designed for observational studies | Cohort studies on diet-disease relationships |
| Newcastle-Ottawa Scale (NOS) [76] | Non-Randomized Studies | Selection, comparability, exposure/outcome | Widely used, simple scoring system | Nutritional cohort studies (though limited by poor discrimination) |
| ROBIS [76] | Systematic Reviews | Study eligibility, identification, data collection, synthesis | Focuses on review process rather than primary studies | Meta-analyses of nutritional interventions |
The Cochrane RoB tool for RCTs assesses six domains of potential bias: (i) selection bias, (ii) performance bias, (iii) attrition bias, (iv) detection bias, (v) reporting bias, and (vi) other biases [76]. Recent updates in the RoB 2.0 version now include the evaluation of dietary adherence within the domain assessing deviations from intended interventions, addressing a crucial aspect of nutritional trials [76]. For non-randomized studies (NRS), which constitute a significant proportion of nutritional evidence, ROBINS-I (Risk Of Bias In Non-randomized Studies - of Interventions) provides a more appropriate assessment framework by evaluating specific biases common in observational designs [76].
A critical distinction in quality assessment lies between methodological quality and risk of bias. While the former investigates whether researchers conducted their work to the highest possible standards, the latter focuses specifically on factors that might systematically distort the results [76]. A study performed to the highest attainable standards may still have significant RoB if, for example, blinding participants to dietary interventions is impossible—a common challenge in nutrition research [76].
Limitations of Current Assessment Approaches
Current approaches to quality assessment in nutritional research reveal significant limitations. An analysis of 50 nutrition-specific systematic reviews of NRS found that 40% conducted no study quality assessment whatsoever, while 38% used the Newcastle-Ottawa Scale [76]. The NOS has been criticized for its arbitrary definitions and poor discriminatory power, with one empirical study demonstrating that 91% of observational nutritional studies were rated as high-quality, suggesting an inappropriately low threshold for this designation [76].
Additional challenges include the proliferation of assessment tools—a systematic review identified 86 different tools to assess study quality in NRS, creating inconsistency in domain selection and weighting across nutritional evidence syntheses [76]. This heterogeneity undermines the comparability of findings across studies and systematic reviews, complicating the formulation of evidence-based dietary recommendations.
Critical Bias Domains in Dietary Validation Research
Measurement Error in Dietary Assessment
Dietary validation studies are particularly susceptible to measurement error, which represents a fundamental domain of potential bias. All self-reported dietary assessment methods—including food records, 24-hour recalls, and food frequency questionnaires—are subject to both random and systematic measurement errors [7]. The accuracy of self-reported data can be partially assessed by comparison with recovery biomarkers, though such biomarkers exist only for energy, protein, sodium, and potassium, limiting comprehensive validation for most nutrients [7].
Specific methods introduce distinct error profiles. Food records are prone to reactivity, whereby participants change their usual dietary patterns during recording periods, often selecting foods perceived as healthier or easier to document [7]. Food frequency questionnaires rely on generic memory and cognitive averaging over time, introducing errors in portion size estimation and frequency reporting [7]. 24-hour dietary recalls reduce reactivity by capturing intake after consumption but depend heavily on participant memory and effective probing techniques [7].
The GARD screener attempts to mitigate these biases by incorporating principles from Assembly Theory to objectively quantify food and food behavior complexity, blinding participants to scoring criteria to reduce the Hawthorne effect (behavior change due to observation awareness) [78]. This approach recognizes that both what people eat and how they eat—including social context and mindfulness—contribute to dietary complexity and health outcomes [78].
Investigator and Systematic Biases
Beyond methodological limitations, dietary validation research is vulnerable to biases introduced by researchers themselves. Investigator bias manifests when researchers' passionate beliefs, career interests, or unconscious preferences influence study conception, design, conduct, analysis, or interpretation [77]. This bias can affect how research questions are framed, with investigators potentially manipulating Population, Intervention, Comparator, Outcome, and Time (PICOT) variables to favor desired outcomes [77].
In dietary assessment, investigator bias may emerge through:
- Selection of inappropriate comparators in controlled trials (e.g., comparing nuts to refined carbohydrate snacks rather than other healthy options) [77]
- Differential intensity of intervention delivery between study arms [77]
- Biased covariate selection in statistical models, leading to over-adjustment or residual confounding [77]
- Unspecified exploratory analyses vulnerable to p-hacking and selective reporting [77]
Additionally, systematic biases in participant reporting present significant challenges. Social desirability bias leads to over-reporting of foods perceived as healthy (e.g., fruits and vegetables) and under-reporting of less healthy options [76] [4]. This phenomenon is particularly pronounced in populations with eating disorders, where cognitive changes from starvation, binge eating episodes, and disordered eating behaviors further compromise reporting accuracy [4].
Application of Quality Assessment Frameworks
Experimental Protocol for Dietary Validation Studies
Implementing rigorous quality assessment requires standardized protocols for dietary validation research. The following workflow outlines key stages in validation studies with integrated bias assessment checkpoints:
Figure 1: Quality Assessment Workflow for Dietary Validation Studies
This protocol emphasizes continuous bias evaluation throughout the research process. At the study conception stage, researchers should explicitly document the rationale for their research question and potential conflicts of interest [77]. During method selection, the choice of assessment method (e.g., 24-hour recall, food record, FFQ) should align with the research question, study design, sample characteristics, and reference timeframe [7]. For participant recruitment, strategies should minimize selection bias and document participation rates [76].
The data collection phase requires standardized protocols with trained interviewers, particularly for methods like diet history, where interviewer skill significantly impacts data quality [4]. Biomarker analysis should incorporate appropriate recovery (e.g., doubly labeled water for energy) and concentration biomarkers where possible to objectively validate self-reported intake [7] [4]. During statistical analysis, researchers should pre-specify analytical approaches, justify covariate selection, and account for measurement error using specialized statistical techniques [7] [77]. Finally, interpretation should acknowledge limitations and avoid overstating findings, particularly for exploratory analyses [77].
Protocol for Web-Based Dietary Assessment Validation
The validation of technology-assisted dietary assessment tools requires specific methodological considerations. The following protocol adapts the approach used in the validation of Nutrition Data, a web-based program for nutritional analysis:
Table 2: Validation Protocol for Web-Based Dietary Assessment Tools
| Stage | Procedure | Quality Control Measures | Outcome Assessment |
|---|---|---|---|
| Participant Training | Standardized instruction on tool functions, portion size estimation, and data entry | Verify comprehension through test entries; provide reference materials | User competency assessment; troubleshooting common issues |
| Data Collection | Parallel administration of web-based tool and reference method (e.g., 24-hour recalls) on same days | Unannounced recall timing; standardized interviewer training; prompts for forgotten foods | Comparison of energy and nutrient intakes between methods |
| Usability Assessment | Administration of acceptability questionnaire evaluating ease of use, helpfulness, recommendation likelihood | Anonymous completion to reduce social desirability bias; quantitative and qualitative feedback | Usability scores; qualitative feedback on features and challenges |
| Statistical Analysis | Paired sample t-tests/Wilcoxon tests for mean differences; correlation analysis; Bland-Altman plots for agreement | Account for multiple testing; pre-specify acceptable agreement thresholds | Significance testing; correlation coefficients; limits of agreement |
This protocol was successfully implemented in a validation study of Nutrition Data against 24-hour recalls in adults with type 1 diabetes, demonstrating no significant differences in mean dietary intakes between methods and high user acceptability, with 70% of participants finding the tool easy to use and 73% willing to recommend it to others [79]. The Bland-Altman analysis in this study showed no clear patterns of bias, though relatively wide limits of agreement highlighted the importance of appropriate statistical evaluation [79].
Emerging Technologies and Methodological Innovations
Artificial Intelligence in Dietary Assessment
Artificial intelligence (AI) technologies are introducing innovative approaches to dietary assessment with potential for reducing traditional measurement biases. AI-based dietary assessment (AI-DIA) methods leverage machine learning (ML), deep learning (DL), and data mining techniques to improve the accuracy and efficiency of dietary intake estimation [3]. A systematic review of 13 validation studies on AI-DIA methods reported correlation coefficients exceeding 0.7 for calorie estimation in six articles and for macronutrients in six studies, demonstrating promising validity compared to traditional assessment methods [3].
The DietAI24 framework represents a significant advancement, integrating multimodal large language models (MLLMs) with Retrieval-Augmented Generation (RAG) technology to ground visual recognition in authoritative nutrition databases rather than relying on the model's internal knowledge [35]. This approach achieves a 63% reduction in mean absolute error for food weight estimation and four key nutrients compared to existing methods when tested on real-world mixed dishes [35]. By enabling accurate identification of specific food variants and comprehensive nutrient estimation across 65 distinct nutrients and food components, this framework addresses a critical limitation of existing systems that focus primarily on basic macronutrients [35].
Complexity-Based Assessment Approaches
Novel theoretical frameworks are emerging to address fundamental limitations in conventional dietary assessment. The GARD screener applies Assembly Theory to objectively quantify food and food behavior complexity, distinguishing between high-complexity foods (e.g., fresh plants, fermented foods) and low-complexity foods (e.g., ultra-processed items) based on quantifiable molecular and behavioral complexity [78]. This approach challenges conventional dietary assessments that treat calories from different foods as metabolically equivalent, instead recognizing that food structure and eating context significantly influence health outcomes [78].
The GARD screener incorporates specific bias-mitigation strategies by blinding participants to scoring criteria and asking only about previous day intake to reduce recall bias and the Hawthorne effect [78]. Validation studies demonstrate alignment with established diet patterns, with Mediterranean diets averaging +22 and the Standard American Diet averaging -10 on the GARD complexity scale [78].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Dietary Validation Studies
| Reagent Category | Specific Tools | Function in Validation Research | Application Considerations |
|---|---|---|---|
| Reference Biomarkers | Doubly labeled water (energy), urinary nitrogen (protein), urinary sodium/potassium | Objective validation of self-reported intake; "recovery" biomarkers for energy and specific nutrients | High cost; specialized analytical requirements; participant burden |
| Concentration Biomarkers | Serum lipids (fat intake), carotenoids (fruit/vegetable intake), erythrocyte fatty acids | Complementary objective measures of specific nutrient exposure | Reflect intake but not exact quantification; influenced by metabolism |
| Standardized Assessment Platforms | ASA24 (Automated Self-Administered 24-hour recall), Nutrition Data, DietAI24 | Digital data collection with integrated nutrient analysis | Requires technological literacy; database quality varies; customization needs |
| Statistical Packages | MSM (Multiple Source Method), SPADE, SAS, R, STATA | Modeling usual intake from short-term instruments; correcting for measurement error | Specialized expertise required; method assumptions must be verified |
| Image-Assisted Tools | Food image recognition algorithms, wearable cameras, portion size estimation apps | Objective food documentation; reduced reliance on memory | Privacy concerns; analytical burden; technical limitations with mixed dishes |
This toolkit provides researchers with essential resources for implementing rigorous dietary validation studies. The selection of appropriate biomarkers is particularly crucial, as they provide objective measures to validate self-reported data, though with important limitations in availability, cost, and interpretation [7] [4]. Digital platforms like ASA24 reduce interviewer burden and costs while allowing participants to respond at their own pace, though they may not be feasible for all study populations [7]. Statistical methods that account for within-person variation and measurement error are essential for deriving habitual intake estimates from short-term assessment methods [7].
Robust quality assessment frameworks are indispensable for advancing the validity and credibility of dietary validation research. By systematically addressing critical bias domains—including measurement error, investigator bias, and methodological limitations—through established tools like Cochrane RoB and ROBINS-I, researchers can significantly enhance the trustworthiness of nutritional evidence [76]. The integration of emerging technologies, including artificial intelligence and complexity-based assessment approaches, offers promising avenues for overcoming persistent methodological challenges in dietary assessment [78] [35] [3].
Future directions should emphasize the development of standardized, nutrition-specific bias assessment criteria that can be consistently applied across studies and systematic reviews. Furthermore, increased attention to investigator bias and non-financial conflicts of interest is essential for addressing the root causes of biased research questions, methods, and interpretations [77]. As dietary assessment methodologies continue to evolve with technological advancements, maintaining rigorous validation standards and quality assessment protocols will ensure that resulting data reliably inform both clinical practice and public health policy.
Comparative Validity Assessment: Analyzing Method Performance Across Platforms and Populations
Accurate dietary assessment is a cornerstone of nutritional epidemiology, enabling researchers to understand the complex relationships between diet and health outcomes [7]. The emergence of digital tools, particularly smartphone applications, has transformed dietary assessment, offering potential solutions to long-standing challenges such as participant burden, cost, and real-time data capture [1] [3]. However, the validity of these methods must be rigorously established before they can be reliably deployed in research and clinical practice. This is particularly critical for measuring energy and macronutrient intake, fundamental variables in metabolic research and drug development.
This document provides application notes and experimental protocols framed within a broader thesis on validating dietary assessment methodologies. It synthesizes current evidence from validation studies and meta-analyses, with a specific focus on performance metrics for energy and macronutrients, to guide researchers in designing robust validation studies for dietary assessment tools.
Performance Metrics for Energy and Macronutrient Assessment: A Meta-Analytic Perspective
Recent systematic reviews and meta-analyses have quantitatively synthesized validation evidence for modern dietary assessment methods, providing crucial insights into their measurement performance for energy and macronutrients.
Meta-Analysis of Dietary Record Apps
A comprehensive meta-analysis of 14 validation studies compared dietary record apps against traditional assessment methods, revealing systematic patterns in measurement error [1]. The analysis demonstrated that mobile dietary record apps consistently underestimated energy intake compared to reference methods, with a pooled effect of -202 kcal/day (95% CI: -319, -85 kcal/day). However, the heterogeneity among studies was substantial (I² = 72%), indicating significant variability in performance across different apps or study designs.
A critical finding emerged when studies were stratified by whether the app and reference method used the same food-composition database. This stratification reduced heterogeneity to 0%, with a much smaller pooled effect of -57 kcal/day (95% CI: -116, 2 kcal/day) [1]. This suggests that differences in underlying nutrient databases contribute significantly to apparent measurement error, highlighting the importance of standardizing this component in validation studies.
For macronutrients, after excluding outliers, the meta-analysis revealed the following pooled estimation differences [1]:
- Carbohydrates: -18.8 g/day (I² = 54%)
- Fat: -12.7 g/day (I² = 73%)
- Protein: -12.2 g/day (I² = 80%)
The high heterogeneity for macronutrients suggests that app performance varies considerably depending on the specific nutrient and possibly the food composition database used.
Table 1: Meta-Analysis of Mobile Dietary Record App Validity for Energy and Macronutrients
| Nutrient | Number of Studies | Pooled Difference (App vs. Reference) | Heterogeneity (I²) |
|---|---|---|---|
| Energy | 11 | -202 kcal/day (95% CI: -319, -85) | 72% |
| Energy (same FCT) | 4 | -57 kcal/day (95% CI: -116, 2) | 0% |
| Carbohydrates | 8 | -18.8 g/day | 54% |
| Fat | 8 | -12.7 g/day | 73% |
| Protein | 8 | -12.2 g/day | 80% |
Emerging Artificial Intelligence-Based Methods
The field of dietary assessment is rapidly evolving with the integration of artificial intelligence (AI). A recent systematic review of AI-based dietary assessment methods (AI-DIA) found promising results, with six studies reporting correlation coefficients exceeding 0.7 for energy estimation between AI methods and traditional assessments [3]. Similarly, six studies achieved correlations above 0.7 for macronutrients, and four studies reached this threshold for micronutrients [3].
AI techniques employed in these systems include deep learning (46.2% of studies) and machine learning (15.3%), with applications ranging from food recognition to nutrient estimation [3]. These technologies demonstrate potential for automating dietary assessment while maintaining accuracy, though most validation studies to date have been conducted in preclinical settings (61.5%), indicating the need for more real-world validation [3].
Experimental Protocols for Validation Studies
Robust validation of dietary assessment methods requires carefully controlled experiments comparing new methods against established reference standards. The following protocols outline recommended approaches for validating energy and macronutrient assessment.
Protocol 1: Biomarker-Based Validation for Energy and Protein
The most rigorous validation of dietary assessment methods employs recovery biomarkers, which provide objective, non-self-reported measures of intake [7] [80].
Reference Method: Doubly labeled water (DLW) for total energy expenditure (as a marker of energy intake) and urinary nitrogen for protein intake [80].
Study Design: Prospective observational study with a duration of 4 weeks [80].
Participants: Target sample of 115 healthy volunteers to detect correlation coefficients of ≥0.30 with 80% power and alpha error probability of 0.05 [80].
Procedure:
- Weeks 1-2: Collect baseline data including socio-demographic and biometric data. Administer three 24-hour dietary recalls (24-HDR) on non-consecutive days.
- Weeks 3-4: Implement the test method (e.g., Experience Sampling-based Dietary Assessment Method - ESDAM) while simultaneously administering biomarker protocols:
- Doubly Labeled Water: Measure total energy expenditure over 14 days.
- Urinary Nitrogen: Collect 24-hour urine samples to estimate protein intake.
- Blood Sampling: Analyze serum carotenoids (fruit/vegetable intake) and erythrocyte membrane fatty acids (dietary fat composition) [80].
Statistical Analysis:
- Calculate mean differences and Spearman correlations between test method and biomarker values.
- Construct Bland-Altman plots to assess agreement.
- Apply the method of triads to quantify measurement error of the test method, 24-HDR, and biomarkers in relation to true dietary intake [80].
Protocol 2: Relative Validity Against Traditional Dietary Assessment
For studies where biomarker methods are not feasible, comparison against traditional dietary assessment methods provides relative validity evidence.
Reference Method: Multiple 24-hour dietary recalls (24-HDR) or food records, considered the least biased self-reported estimators of energy intake [7].
Study Design: Cross-sectional or prospective comparative study.
Participants: Minimum of 3-4 days of assessment per participant to account for day-to-day variation. Larger sample sizes (n≥100) recommended for correlation analyses [7] [80].
Procedure:
- Administer the test method (e.g., dietary app) and reference method concurrently.
- For 24-HDR reference: Collect multiple recalls on non-consecutive days, including weekdays and weekends, using trained interviewers and standardized probes [7].
- For food record reference: Participants record all foods, beverages, and supplements consumed during the designated period, ideally with weighing/measuring [7].
- Ensure the same food composition database is used for both test and reference methods to minimize database-related discrepancies [1].
Statistical Analysis:
- Paired t-tests or Wilcoxon signed-rank tests for systematic differences.
- Pearson or Spearman correlation coefficients for relative validity.
- Cross-classification analysis to assess agreement in quartile ranking.
Visualization of Validation Study Workflows
The Researcher's Toolkit: Essential Reagents and Materials
Successful validation of dietary assessment methods requires specific reagents, technologies, and analytical tools. The following table details essential components of the researcher's toolkit.
Table 2: Research Reagent Solutions for Dietary Assessment Validation
| Category | Item | Specification/Function | Application Example |
|---|---|---|---|
| Biomarkers | Doubly Labeled Water | H₂¹⁸O and ²H₂O for measuring total energy expenditure via isotope elimination | Gold standard validation of energy intake assessment [80] |
| Biomarkers | Urinary Nitrogen | 24-hour urine collection for nitrogen analysis to estimate protein intake | Validation of protein intake assessment [80] |
| Biomarkers | Serum Carotenoids | HPLC analysis of β-carotene, lutein, etc. as biomarkers of fruit/vegetable intake | Validation of food group intake assessment [80] |
| Biomarkers | Erythrocyte Fatty Acids | GC analysis of membrane fatty acid composition as biomarker of dietary fat intake | Validation of fatty acid intake assessment [80] |
| Reference Methods | 24-Hour Dietary Recall | Structured interview by trained dietitian using multiple passes | Reference method for relative validity studies [7] [80] |
| Reference Methods | Weighed Food Records | Digital scales and detailed recording protocols | Reference method with minimal estimation error [7] |
| Digital Tools | Dietary Assessment Apps | Mobile applications for real-time dietary recording (e.g., Keenoa, Asken) | Test methods for validation [3] [81] |
| Digital Tools | AI-Based Analysis Platforms | Deep learning systems for food recognition (e.g., NutriNet) | Automated food identification and nutrient estimation [3] |
| Analytical Resources | Food Composition Databases | Standardized nutrient databases (e.g., USDA, NUBEL) | Nutrient analysis from food intake data [1] [80] |
| Analytical Resources | Statistical Software | R, Stata, SPSS for advanced statistical analysis (method of triads, Bland-Altman) | Data analysis and calculation of validity metrics [1] [80] |
The validation of dietary assessment methods for energy and macronutrients remains a complex but essential endeavor in nutritional research. Current evidence indicates that digital methods, including mobile apps and AI-based systems, show promise but consistently demonstrate a tendency toward underestimation of energy and macronutrients compared to reference methods. The substantial heterogeneity in validation study results highlights the importance of standardized protocols, including the use of consistent food composition databases and appropriate reference methods.
Future validation studies should prioritize biomarker-based designs where feasible, incorporate larger and more diverse populations, and account for the interdependencies between macronutrients in their analytical approaches. As technology continues to evolve, maintaining rigorous validation standards will be crucial for ensuring that new dietary assessment tools generate reliable data for research and clinical applications.
Table 1: Correlation Coefficients Between AI-Based and Traditional Dietary Assessment Methods for Energy and Macronutrients
| Dietary Component | Number of Studies Reporting Correlation >0.7 | Typical Correlation Range | Key Findings |
|---|---|---|---|
| Energy (Calories) | 6 studies [3] | >0.7 [3] | AI methods show strong correlation for total energy intake estimation. |
| Macronutrients | 6 studies [3] | >0.7 [3] | Reliable correlations for proteins, fats, and carbohydrates. |
| Micronutrients | 4 studies [3] | >0.7 [3] | Moderate to strong correlations, though slightly less consistent than for macronutrients. |
Table 2: Performance Metrics of Specific AI-Based Dietary Assessment Tools
| AI Tool / System Name | Core Technology | Application / Context | Reported Performance / Accuracy |
|---|---|---|---|
| goFOOD 2.0 | Computer Vision, Deep Learning [33] | Automated dietary assessment via food images [33] | Moderate agreement with dietitians; accuracy affected by mixed dishes and portion sizing [33]. |
| Intelligent Diet Recommendation System (IDRS) | Machine Learning, 3D Body Modeling [38] | Personalized diet plan generation [38] | Error rate of <3% for personalized diet recommendations [38]. |
| Keenoa | Image-based App [3] | Dietary intake validation [3] | Studied for relative validity against 3-day food diaries [3]. |
| NutriNet | Deep Convolutional Neural Network [3] | Food and drink image detection [3] | Comparative performance against other architectures like AlexNet [3]. |
| Diet Engine | Deep Learning (YOLOv8) [82] | Real-time food recognition and nutrient estimation [82] | 86% classification accuracy [82]. |
| ML-enhanced Logistic Regression (ML-LR) | Machine Learning with SHAP analysis [83] | Identifying risk factors for child malnutrition [83] | Identified 13 significant risk factors vs. 6 by conventional econometric LR [83]. |
Experimental Protocols
Protocol for Validating an AI-Based Dietary Assessment Tool
This protocol outlines the steps for a comparative validation study, pitting an AI-based method against traditional dietary assessment tools [3].
I. Study Design and Participant Recruitment
- Design: Cross-sectional comparative or validation study [3].
- Participants: Recruit a sample of participants representative of the target population. Sample sizes in existing studies range from 36 to 136 participants [3].
- Setting: Study can be conducted in pre-clinical (controlled) or clinical (real-world) settings [3].
II. Data Collection Procedures
- AI Method:
- Participants use a smartphone app (e.g., an image-based system like
goFOODorKeenoa) to capture images of all food and beverages consumed before and after meals [3] [33] [34]. - The AI system automatically processes the images to identify food items and estimate portion sizes/volume using computer vision and deep learning models [33] [82].
- Nutrient analysis is performed by linking identified foods to a standard nutritional database [34].
- Participants use a smartphone app (e.g., an image-based system like
- Traditional Reference Method:
- Participants concurrently complete a 3-day weighed food record or multiple 24-hour dietary recalls administered by a trained dietitian [3].
- Dietitians analyze the food records using the same nutritional database as the AI system to ensure comparability.
III. Data Analysis and Validation
- Statistical Analysis: Calculate correlation coefficients (Pearson or Spearman) between the AI-estimated intakes and the traditional method intakes for energy, macronutrients, and micronutrients [3].
- Validation Metrics: Report additional metrics such as mean absolute error (MAE), root mean squared error (RMSE), and Bland-Altman plots to assess agreement and systematic bias [3] [84]. A correlation coefficient > 0.7 is typically considered indicative of good agreement [3].
Protocol for Developing a Machine Learning Model for Nutritional Outcome Prediction
This protocol describes the workflow for creating an ML model to predict a nutritional outcome, such as calorie needs or malnutrition risk, and comparing its performance to traditional statistical models [83] [84].
I. Data Preparation
- Data Source: Utilize a large-scale dataset with demographic, anthropometric, and health data (e.g., NHANES, Demographic and Health Surveys) [83] [84].
- Variable Selection: Define predictors (e.g., age, sex, height, weight, physical activity level, dietary diversity, maternal BMI) and the target outcome (e.g., daily caloric needs, malnutrition status) [83] [84].
- Data Preprocessing: Handle missing data, normalize numerical features, and encode categorical variables. Split the dataset into training and testing sets (e.g., 80/20 split).
II. Model Training and Comparison
- Machine Learning Model:
- Traditional Model:
- Performance Evaluation:
- Evaluate both models on the held-out test set.
- For regression (calorie prediction), report MAE, RMSE, and R². For classification (malnutrition risk), report AUC, accuracy, precision, and recall [83] [84].
- Use SHAP (SHapley Additive exPlanations) analysis to interpret the ML model's outputs and identify the most important predictive factors [83].
Workflow and Relationship Visualizations
AI vs Traditional Dietary Assessment Validation
ML vs Traditional Model Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Dietary Intake Validation Research
| Item | Category | Function in Research |
|---|---|---|
| Standardized Food Composition Database (e.g., USDA) | Data Resource | Provides the foundational nutritional data (energy, macros, micros) for converting food intake information into nutrient values. Essential for ensuring both AI and traditional methods use the same reference. |
| AI-Based Dietary Assessment App (e.g., goFOOD, Keenoa) | Software Tool | Enables automated, image-based food intake recording and analysis. Used as the intervention or test method in validation studies to reduce recall bias and improve scalability [3] [33] [34]. |
| Doubly Labeled Water (DLW) | Biomarker | Serves as an objective, gold-standard method for validating total energy expenditure (TEE). Used to assess the accuracy of self-reported energy intake data from both traditional and AI methods [34]. |
| Trained Dietitian / Nutritionist | Human Resource | Conducts 24-hour dietary recalls or analyzes food records for the traditional reference method. Their expertise is crucial for accurate food identification and portion size estimation, against which AI performance is benchmarked [3]. |
| Machine Learning Library (e.g., Scikit-learn, XGBoost) | Software Tool | Provides algorithms for developing predictive models of nutritional needs or outcomes (e.g., calorie estimation, malnutrition risk). Allows comparison against traditional statistical formulas [83] [84]. |
| SHAP (SHapley Additive exPlanations) | Interpretation Tool | An explainable AI (XAI) library that interprets the output of machine learning models. It helps identify the most important features (risk factors) driving predictions, making black-box models more transparent and actionable for researchers [83]. |
Accurate dietary assessment is a fundamental pillar of nutritional research, essential for investigating the relationship between diet and health outcomes, informing public health policies, and developing effective nutritional interventions [80]. However, traditional self-reported methods, such as Food Frequency Questionnaires (FFQs), 24-hour dietary recalls (24-HDRs), and diet histories, are susceptible to significant measurement errors, including recall bias, social desirability bias, and misreporting [28] [4]. These limitations complicate the identification of true diet-health relationships, as the strength of observed associations can be attenuated by poor data quality [28].
Biomarker-based validation represents a paradigm shift towards objective verification of dietary intake. Biomarkers provide independent, physiological measures of nutrient consumption, thereby overcoming many of the biases inherent in self-reporting [85]. This document details application notes and experimental protocols for validating self-reported macronutrient intake against objective biomarkers, providing a critical methodological framework for research within a thesis on dietary assessment validation.
Key Biomarkers and Validation Protocols
The following section outlines the primary biomarkers and standardized protocols for validating energy and macronutrient intake.
Energy Intake: Doubly Labeled Water (DLW)
The doubly labeled water (DLW) method is the gold standard for assessing total energy expenditure (TEE) in free-living individuals. Under conditions of weight stability, energy intake is equivalent to TEE, providing a robust reference for validating self-reported energy intake [86] [80].
Experimental Protocol:
- Baseline Sample Collection: Participants provide a baseline urine sample before administration of the isotopic tracers.
- Isotope Administration: Participants orally consume a dose of water containing known concentrations of two stable isotopes: ^2H (deuterium) and ^18O (oxygen-18).
- Post-Dose Sample Collection: Urine samples are collected at regular intervals over a period of 10-14 days. Typical collection points are 4, 5, and 6 hours post-dose on day one, and again on days 7, 10, and 14, though protocols may vary.
- Analysis: The elimination rates of ^2H and ^18O from the body are determined by measuring isotope concentrations in the urine samples using isotope ratio mass spectrometry.
- Calculation: Carbon dioxide production rate is calculated from the difference in elimination rates between the two isotopes. This value is then used to calculate total energy expenditure.
Protein Intake: Urinary Nitrogen
Urinary nitrogen (N) excretion serves as a reliable biomarker for protein intake, as the majority of nitrogen consumed and metabolized is excreted in urine [86] [80].
Experimental Protocol:
- Sample Collection: Participants collect all urine produced over a 24-hour period. It is critical to ensure complete collection, as this is a major potential source of error.
- Storage: Urine is collected in pre-weighed containers with preservative (e.g., boric acid) and stored refrigerated or frozen until analysis.
- Analysis: Total nitrogen content in the 24-hour urine collection is quantified using the Kjeldahl method or by chemiluminescence.
- Calculation: Protein intake is estimated from urinary nitrogen using the following formula, which accounts for non-urinary nitrogen losses and the average nitrogen content of protein:
- Protein Intake (g/day) = (Urinary Nitrogen (g/day) + 2) * 6.25 The constant "2" represents an estimate of nitrogen lost through feces, skin, and other routes.
Fatty Acid Intake: Erythrocyte Membrane Fatty Acids
The composition of fatty acids in erythrocyte membranes reflects the medium-to-long-term intake of dietary fatty acids, providing an objective measure for validating reported fat consumption [80].
Experimental Protocol:
- Blood Collection: A fasting blood sample (e.g., 10-20 mL) is collected from each participant into tubes containing an anticoagulant such as EDTA.
- Processing: Erythrocytes (red blood cells) are separated from plasma and other components by centrifugation. The red blood cell pellet is washed with a saline solution to remove contaminants.
- Lipid Extraction: Lipids are extracted from the erythrocytes using organic solvents like a chloroform-methanol mixture.
- Analysis: Fatty acid methyl esters (FAMEs) are prepared from the extracted lipids and analyzed using gas chromatography (GC) with flame ionization detection (FID) or mass spectrometry (MS). This identifies and quantifies the relative proportions of individual fatty acids (e.g., omega-3 and omega-6 PUFAs).
Integrated Validation Study Workflow
A comprehensive validation study integrates multiple biomarkers and self-reported methods. The workflow below outlines the key stages for a robust validation study design.
Quantitative Data on Dietary Assessment Reliability
Determining the minimum number of days required for reliable dietary assessment is crucial for study design. The following table summarizes findings from a large digital cohort study on the minimum days required to estimate usual intake for various nutrients [28].
Table 1: Minimum Days Required for Reliable Dietary Assessment
| Nutrient / Food Group | Reliability Threshold (r) | Minimum Days Required | Notes |
|---|---|---|---|
| Water / Coffee | > 0.85 | 1-2 days | Least variable, easiest to estimate. |
| Total Food Quantity | > 0.85 | 1-2 days | |
| Carbohydrates | 0.8 | 2-3 days | |
| Protein | 0.8 | 2-3 days | |
| Fat | 0.8 | 2-3 days | |
| Most Micronutrients | 0.8 | 3-4 days | |
| Meat & Vegetables | 0.8 | 3-4 days | More variable food groups. |
Key Findings: The data indicates that 3-4 days of dietary data collection, ideally non-consecutive and including at least one weekend day, are sufficient for reliable estimation of most macronutrients and micronutrients [28]. This finding is critical for designing the dietary assessment component of validation studies, balancing reliability with participant burden.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Reagents and Materials for Biomarker Validation
| Item | Function / Application | Example Biomarkers |
|---|---|---|
| Stable Isotopes (^2H, ^18O) | Tracers for the Doubly Labeled Water method to measure total energy expenditure. | Energy Intake [86] [80] |
| Urine Collection Kits | For complete 24-hour urine collection and preservation prior to nitrogen analysis. | Protein Intake [86] [80] |
| Blood Collection Tubes | For collecting fasting blood samples; EDTA tubes are standard for erythrocyte analysis. | Erythrocyte Fatty Acids, Serum Carotenoids [80] |
| Liquid Chromatography-Mass Spectrometry | For high-throughput metabolomic profiling and discovery of novel dietary biomarkers. | Candidate Biomarker Discovery [85] |
| Gas Chromatograph | For separation, identification, and quantification of individual fatty acids. | Erythrocyte Membrane Fatty Acids [80] |
| Validated Dietary Assessment Tool | Self-reported method for capturing dietary intake (e.g., ESDAM, 24-HDR, FFQ). | Reported intake for correlation [86] [27] |
Advanced Considerations and Methodological Refinements
Biomarker Discovery and the Method of Triads
Beyond validating self-report, advanced research aims to discover new biomarkers. The Dietary Biomarkers Development Consortium (DBDC) employs a 3-phase approach: (1) identification of candidate compounds through controlled feeding trials and metabolomic profiling of blood and urine; (2) evaluation of candidate biomarkers in studies of various dietary patterns; and (3) validation in independent observational settings [85].
The Method of Triads is a powerful statistical technique used in validation studies to quantify the correlation between three measurements: the self-reported dietary data (e.g., FFQ), a more precise reference method (e.g., 24-HDR), and the biomarker. This method allows researchers to estimate the true validity coefficient of the self-report tool and understand the measurement error structure of each method in relation to the unknown 'true' intake [80].
Special Populations and Clinical Considerations
Validation approaches may require adaptation in specific populations. For instance, in individuals with eating disorders, cognitive changes associated with starvation and the stress of binge-eating episodes can impact recall and reporting accuracy [4]. One pilot study found that the diet history method showed moderate to good agreement for dietary cholesterol and iron when compared with serum biomarkers in this population [4]. This highlights the importance of targeted questioning, consideration of dietary supplement use, and the potential for differential measurement error across population subgroups.
Cross-population reliability refers to the consistency and reproducibility of dietary assessment methods when applied across diverse demographic groups, including variations in age, sex, socioeconomic status, and cultural backgrounds. Establishing this reliability is fundamental to ensuring that nutritional research findings are valid, generalizable, and applicable to the populations they intend to serve. In the context of macronutrient intake validation research, the complex interplay between assessment methodologies and population characteristics introduces unique challenges that must be systematically addressed through rigorous experimental design [7].
The gold standard for large-scale dietary monitoring in the United States is the National Health and Nutrition Examination Survey (NHANES), which incorporates What We Eat in America (WWEIA) as its dietary component. This comprehensive approach collects data through 24-hour dietary recalls and examines intake patterns across prioritized sociodemographic variables, including age/life stage, sex, race and/or ethnicity, and socioeconomic indicators [19]. However, even well-established methods like these require continuous validation to ensure their reliability across diverse subpopulations, especially as new technologies and assessment platforms emerge.
Quantitative Comparison of Dietary Assessment Reliability
Reliability Metrics Across Assessment Methods
Table 1: Comparative reliability of different dietary assessment methods for macronutrient measurement
| Assessment Method | Population Characteristics | Reliability Metric | Energy | Carbohydrates | Protein | Fat |
|---|---|---|---|---|---|---|
| Food Record Apps (Meta-analysis) | Mixed populations across 11 studies | Mean difference from reference (kcal/g) | -202 kcal/day [87] | -18.8 g/day [87] | -12.2 g/day [87] | -12.7 g/day [87] |
| MyFoodRepo Digital App | Swiss adults (N=958) | Minimum days for reliability (r>0.8) | 2-3 days [28] | 2-3 days [28] | 2-3 days [28] | 2-3 days [28] |
| Vienna Food Record | Austrian adults (N=35) | Intraclass Correlation Coefficient (ICC) | 0.95 [88] | 0.71-0.89 [88] | 0.73-0.91 [88] | 0.75-0.90 [88] |
| Semi-Quantitative FFQ | Serbian young adults (N=93) | Pearson correlation vs 24HR | 0.45-0.65 [89] | 0.41-0.62 [89] | 0.39-0.58 [89] | 0.43-0.60 [89] |
| myfood24 Web-Based Tool | Danish adults (N=71) | Spearman's correlation vs biomarkers | 0.38 (vs TEE) [17] | 0.42 (urinary K) [17] | 0.45 (urinary protein) [17] | 0.30-0.40 [17] |
Demographic Factors Influencing Reliability
Table 2: Impact of demographic factors on dietary assessment reliability
| Demographic Factor | Impact on Measurement Reliability | Evidence Strength | Recommended Protocol Adjustments |
|---|---|---|---|
| Age/Life Stage | Children and elderly show greater portion size estimation errors; young adults more likely to use digital tools effectively [28] [18] | Strong consistency across multiple validation studies [19] [28] | Age-appropriate portion size estimation aids; technology interface tailored to digital literacy |
| Socioeconomic Status | Lower income associated with higher under-reporting, particularly for energy-dense foods [19] [7] | Demonstrated in NHANES analyses but cannot assess causality [19] | Multiple non-consecutive assessment days; building rapport to reduce social desirability bias |
| BMI Category | Systematic under-reporting correlated with higher BMI [28] | Strong evidence from doubly labeled water studies [28] | Objective biomarkers where possible; assessment of plausible energy intake reports |
| Cultural/Linguistic Background | FFQs require cultural adaptation; non-native language increases measurement error [89] [18] | Demonstrated in FFQ validation studies across populations [89] | Culturally appropriate food lists; bilingual researchers or validated translations |
| Weekday vs Weekend | Significant intake differences for energy, carbohydrates, alcohol [28] | Strong evidence from digital cohort (N=958) [28] | Include both weekday and weekend days in assessment period |
Experimental Protocols for Cross-Population Reliability Testing
Core Protocol: Multi-Group Validation Design
Objective: To evaluate the reliability of a dietary assessment method across diverse demographic groups while controlling for methodological variables.
Population Sampling Framework:
- Recruit a minimum of 100 participants per demographic subgroup of interest, based on power calculations from previous validation research [17] [80]
- Stratify recruitment by age (18-35, 36-50, 51-70 years), sex, BMI categories (normal weight, overweight, obese), and socioeconomic indicators
- Include specific consideration for vulnerable populations: pregnant women, older adults, and low-income groups [19] [18]
Assessment Protocol:
- Baseline assessment: Collect demographic, anthropometric, and socioeconomic data
- Dietary assessment: Implement the test method (e.g., dietary app, FFQ) alongside an appropriate reference method
- Reference method selection:
- Temporal framework: Minimum 3-4 non-consecutive days including one weekend day [28]
- Compliance monitoring: Use continuous glucose monitoring or other objective compliance measures where feasible [80]
Statistical Analysis Plan:
- Calculate intraclass correlation coefficients (ICC) for test-retest reliability within each subgroup [88]
- Compute Pearson or Spearman correlations between test method and reference standard by subgroup [17]
- Assess mean differences using paired t-tests or Bland-Altman plots with 95% limits of agreement [88] [87]
- Employ linear mixed models to examine effects of demographic factors on measurement error [28]
Specialized Protocol: Cultural Adaptation of Food Frequency Questionnaires
Objective: To adapt and validate a dietary assessment tool for a specific cultural or ethnic population.
Adaptation Phase:
- Food list development: Identify culturally specific foods through focus groups, market surveys, and existing dietary data [89]
- Portion size determination: Establish appropriate portion sizes using common household measures specific to the culture
- Frequency categories: Ensure frequency categories (e.g., "per day," "per week") are culturally appropriate and easily understood
- Translation and back-translation: For non-English speakers, use formal translation protocols with reconciliation of discrepancies [18]
Validation Phase:
- Administer adapted FFQ and reference method (multiple 24-hour recalls or food records) to a representative sample (N≥93, based on Serbian validation) [89]
- Include cognitive interviewing to assess comprehension and cultural relevance of questions
- Analyse by food group and nutrient to identify specific areas of measurement error
- Test for differential item functioning across cultural subgroups within the population
Figure 1: Cross-Population Reliability Testing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and tools for dietary assessment validation
| Tool/Reagent | Function | Application Notes | Quality Indicators |
|---|---|---|---|
| Doubly Labeled Water | Objective measure of total energy expenditure | Considered gold standard for validating energy intake reporting [80] | ≥95% purity; established laboratory analysis protocols |
| 24-Hour Urinary Nitrogen | Biomarker for protein intake | Requires complete 24-hour urine collection; participant training essential [17] | Creatinine analysis to assess completeness of collection |
| Serum Carotenoids | Biomarker for fruit and vegetable intake | Relative measure influenced by metabolism and food matrix effects [17] [80] | HPLC analysis; fasting blood samples required |
| Electronic Food Composition Databases | Nutrient calculation from food intake data | Must be population-specific (e.g., USDA FNDDS, BLS, local adaptations) [19] [89] | Regular updates; comprehensive food coverage; transparent sourcing |
| Standardized Portion Aids | Visual aids for portion size estimation | Should be culturally appropriate (e.g., household measures, common utensils) [88] [89] | Validated against weighed portions; culturally relevant items |
| Digital Diet Assessment Platforms | Mobile data collection and nutrient analysis | Include myfood24, ASA-24, MyFoodRepo, and custom applications [87] [17] [28] | User-friendly interface; offline capability; data export functions |
Analysis of Methodological Consistency Across Populations
The search for consistent dietary assessment across diverse populations reveals several critical considerations. First, method reliability varies substantially across demographic groups, with systematic patterns of under-reporting associated with BMI, age, and socioeconomic status [28] [7]. Second, technological solutions show promise but require rigorous validation within target populations, as demonstrated by the consistent underestimation of intake by dietary apps across multiple studies [87]. Third, cultural adaptation is not merely a translational exercise but requires fundamental reconsideration of food lists, portion sizes, and eating patterns [89] [18].
The optimal number of assessment days represents a key practical consideration, with recent evidence from digital cohorts suggesting 3-4 days (including one weekend day) provides sufficient reliability for most macronutrients in diverse populations [28]. This represents a refinement of earlier recommendations and has significant implications for reducing participant burden in large-scale studies.
Future methodological development should focus on addressing systematic reporting biases through objective biomarker calibration and developing culturally intelligent assessment tools that can adapt to diverse eating patterns while maintaining measurement consistency across populations. This dual approach will enhance the cross-population reliability essential for advancing nutritional epidemiology and public health policy.
Cost-Benefit Analysis (CBA) serves as a crucial decision-support tool in public health nutrition, providing a systematic framework for evaluating the economic efficiency of dietary interventions and assessment methods. Within macronutrient intake validation research, CBA helps stakeholders determine whether the benefits of implementing a new dietary assessment protocol justify its costs, particularly when compared to existing methodologies [90]. The fundamental principle of CBA involves quantifying both the monetary costs and health-economic benefits of dietary assessment methods, then comparing them to determine net social benefit [91].
Recent systematic reviews highlight CBA's growing application in food environment interventions, demonstrating its value for capturing broader societal impacts beyond immediate health outcomes [91]. This approach is particularly relevant for validation research, where researchers must balance the practical constraints of implementation against the methodological rigor required to produce scientifically valid results. The integration of CBA with health impact assessment (HIA) methodologies, including disability-adjusted life years (DALYs) and willingness-to-pay (WTP) measures, creates a powerful interdisciplinary framework for evaluating regulatory instruments and dietary assessment technologies [90].
Methodological Framework for CBA in Validation Research
Core Components of the CBA Framework
A rigorous CBA framework for dietary assessment validation research incorporates multiple interconnected components that collectively support robust economic evaluation. The table below outlines these essential elements and their applications in macronutrient intake validation studies.
Table 1: Core Components of CBA Framework in Dietary Assessment Validation Research
| Component | Description | Application in Macronutrient Validation |
|---|---|---|
| Cost Identification | Comprehensive cataloging of all resources required | Includes personnel time, technology acquisition, participant recruitment, data collection instruments, and analysis software [91] |
| Benefit Quantification | Measurement of positive outcomes in monetary terms | encompasses improved accuracy in energy intake measurement, better health outcomes from more precise dietary data, and research efficiency gains [90] |
| Time Horizon Consideration | Appropriate timeframe for capturing costs and benefits | Matches the validation study duration while accounting for long-term implementation of successful methods [92] |
| Perspective Analysis | viewpoint from which the analysis is conducted | societal, healthcare system, researcher, or participant perspectives each yield different cost-benefit calculations [90] |
| Uncertainty Analysis | Assessment of variability in cost and benefit estimates | Particularly important given measurement errors inherent in dietary assessment methods [87] |
Integrating Methodological Rigor with Practical Constraints
Methodological rigor in CBA requires careful attention to multilevel research characteristics, as dietary assessment validation operates across individual, technological, organizational, and societal levels [92]. Implementation scientists recommend eight key characteristics for rigorous multilevel research, including mapping the multilevel context, defining level-specific constructs, specifying temporal scope, and aligning measurement choices with theoretical frameworks [92].
Quantitative rigor demands systematic data quality assurance procedures throughout the research process, including checking for duplicates, managing missing data, identifying anomalies, testing psychometric properties, and verifying normality of distribution [93]. These procedures ensure that the cost and benefit data underlying CBA calculations meet scientific standards for reliability and validity.
Application Notes: CBA Protocol for Dietary Assessment Validation
Experimental Protocol for Validating Dietary Assessment Methods
The following protocol provides a detailed methodology for conducting validation studies of dietary assessment methods with integrated CBA components.
Phase 1: Study Design and Planning
- Objective Setting: Clearly define validation objectives and determine appropriate reference methods (e.g., doubly labeled water for energy intake, biomarkers for specific nutrients) [87]
- Sample Size Calculation: Conduct power analysis to determine sufficient participant numbers, accounting for expected attrition and variability in dietary intake [94]
- Cost Identification Worksheet: Develop comprehensive spreadsheet documenting all anticipated costs categories:
- Personnel (researchers, nutritionists, data analysts)
- Technology (mobile devices, apps, specialized software)
- Laboratory analyses (biomarker verification)
- Participant compensation and retention expenses
- Overhead (space, utilities, administrative support) [91]
Phase 2: Data Collection and Management
- Parallel Assessment: Implement test method and reference method simultaneously while minimizing participant burden and assessment interference [87]
- Quality Assurance Checks: Institute systematic data cleaning procedures including checking for duplicates, managing missing data, identifying anomalies, and verifying data ranges [93]
- Document Time Investments: Record staff time dedicated to training, data collection, entry, cleaning, and analysis for accurate cost calculation
Phase 3: Data Analysis and Validation Metrics
- Statistical Comparison: Calculate correlation coefficients, limits of agreement, mean differences, and Bland-Altman analyses for energy and macronutrient intake [95]
- Cost-Benefit Calculation:
- Sum all documented costs from Phases 1-2
- Quantify benefits including improved accuracy, time savings compared to reference method, and projected health benefits from more accurate assessment
- Compute net present value using appropriate discount rate [90]
- Uncertainty Analysis: Conduct sensitivity analyses on key parameters to test robustness of CBA results [91]
Data Analysis and Presentation Protocol
Quantitative Analysis Workflow:
- Data Cleaning and Preparation: Apply systematic quality assurance procedures including missing data analysis, anomaly detection, and verification of data distributions [93]
- Descriptive Statistics: Calculate means, standard deviations, and ranges for all measured variables including energy and macronutrient intake
- Validation Statistics:
- Compute correlation coefficients (Pearson or Spearman) between test and reference methods
- Perform Bland-Altman analysis to assess limits of agreement
- Calculate mean differences and percentage agreement for energy and macronutrients [95]
- Cost-Benefit Calculation:
- Sum all direct and indirect costs
- Monetize benefits including time savings, improved accuracy, and health outcomes
- Calculate net present value using formula: [ NPV = \sum{t=0}^{T} \frac{Bt - Ct}{(1 + r)^t} ] where (Bt) = benefits in year t, (C_t) = costs in year t, r = discount rate [90]
Reporting Standards:
- Present both significant and non-significant findings to avoid selective reporting [93]
- Include comprehensive description of methodological limitations and potential biases
- Provide sufficient statistical detail to enable replication, including effect sizes and confidence intervals [94]
- Use appropriate visualizations (tables, Bland-Altman plots) that clearly represent the data and relationships
Table 2: Validation Metrics for Dietary Assessment Methods in Macronutrient Research
| Validation Metric | Calculation Method | Interpretation Guidelines | Application in CBA |
|---|---|---|---|
| Correlation Coefficient | Pearson's r or Spearman's ρ | Strong: ≥0.80, Moderate: 0.60-0.79, Fair: 0.30-0.59, Poor: <0.30 [87] | Higher correlations increase benefit of new method through improved accuracy |
| Mean Difference | ( \frac{1}{n}\sum{i=1}^n (yi - x_i) ) where y=test method, x=reference | Closer to zero indicates better agreement; systematic over/underestimation patterns | Significant biases may increase costs through need for calibration or adjustment |
| Limits of Agreement (Bland-Altman) | Mean difference ± 1.96 × SD of differences | Wider intervals indicate poorer agreement between methods | Wider limits decrease benefit value due to reduced precision |
| Intraclass Correlation Coefficient | Variance components from mixed models | <0.5 poor, 0.5-0.75 moderate, 0.75-0.9 good, >0.9 excellent reliability | Higher ICC increases benefit through more consistent measurements |
| Cost-Benefit Ratio | Total benefits / Total costs | Ratio >1 indicates benefits exceed costs | Primary outcome for economic evaluation of method implementation |
Visualization of Methodological Rigor Framework in CBA
The following diagram illustrates the key characteristics of methodological rigor in multilevel implementation research applied to dietary assessment validation studies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for Dietary Assessment Validation Studies
| Tool/Reagent | Specifications | Function in Validation Research | Cost-Benefit Considerations |
|---|---|---|---|
| Web-Based Dietary Assessment Platforms | Customizable food frequency questionnaires or 24-hour recall systems | Enable efficient data collection with built-in completeness checks and automated nutrient calculation [95] | Higher initial development cost offset by reduced data entry time and errors |
| Mobile Dietary Record Applications | Smartphone apps with barcode scanning, image capture, and textual food input | Facilitate real-time dietary recording in free-living conditions [87] | Technology costs balanced against improved compliance and portion size estimation |
| Reference Method Materials | Doubly labeled water, urinary nitrogen kits, biomarkers for specific nutrients | Provide objective validation standards for energy and macronutrient intake [87] | High analytical costs necessitate careful sample size justification through power analysis |
| Statistical Analysis Software | R, Python, SAS, SPSS with specialized packages for validation statistics | Enable comprehensive data analysis including correlation, agreement, and cost-benefit calculations [93] | Licensing costs vs. analytical capability and reproducibility benefits |
| Data Quality Assurance Tools | Missing data analysis protocols, anomaly detection algorithms, normality tests | Ensure reliability and validity of collected dietary and cost data [93] | Implementation time investment prevents costly erroneous conclusions |
| Visualization Software | Gephi for network analysis, ggplot2 for statistical graphics, Graphviz for workflows | Create publication-quality diagrams and data visualizations [96] | Open-source options reduce financial barriers while maintaining professional output |
Integrated CBA Decision Framework for Method Selection
The following workflow illustrates the decision process for selecting dietary assessment methods based on both validation metrics and cost-benefit considerations.
Implementation Protocol for CBA-Informed Decisions
Decision-Making Algorithm:
- Establish Minimum Validation Thresholds: Before CBA, determine minimum acceptable values for key validation metrics based on research objectives and field standards [87]
- Concurrent CBA and Validation Assessment: Evaluate methodological rigor and economic efficiency simultaneously rather than sequentially
- Contextual Factor Integration: Consider organizational capacity, technological infrastructure, and population characteristics that may affect both costs and benefits
- Stakeholder Value Weighting: Incorporate preferences of relevant stakeholders (researchers, clinicians, participants, policymakers) in the interpretation of CBA results [90]
Handling Mixed Outcomes:
- When validation results are adequate but CBA is negative, investigate cost-reduction strategies or targeted implementation in higher-value contexts
- When CBA is positive but validation metrics are borderline, consider whether method refinement could improve accuracy without substantially increasing costs
- Document decision rationale transparently, including how practical implementation considerations were weighed against methodological rigor standards [92]
This integrated framework enables researchers and decision-makers to balance the competing demands of scientific rigor and practical implementation, ensuring that dietary assessment methods selected for macronutrient intake validation research provide both methodological soundness and economic value.
Conclusion
The validation of macronutrient intake requires a multifaceted approach that strategically combines traditional methods with emerging technologies. Current evidence indicates that AI-enhanced dietary assessment methods show significant promise, with multiple studies reporting correlation coefficients exceeding 0.7 for calories and macronutrients compared to traditional methods, though a tendency for underestimation remains a concern. The integration of objective biomarkers provides crucial validation anchors, particularly in clinical populations where reporting biases may be pronounced. Future directions should focus on standardizing validation protocols, expanding research in diverse populations and real-world settings, improving the interoperability of food composition databases, and developing more sophisticated AI algorithms that can better account for complex eating behaviors. For biomedical and clinical research, these advancements will enable more precise nutritional epidemiology, enhance the quality of diet-related intervention studies, and support the development of more targeted nutritional therapies and pharmaceuticals. Interdisciplinary collaboration between nutrition scientists, technology developers, and clinical researchers will be essential to advance the field toward more accurate, feasible, and scalable dietary assessment solutions.
References
- 1. A Systematic Review and Meta-Analysis of Validation ... [https://www.sciencedirect.com/science/article/pii/S2161831322005099]
- 2. Ultraprocessed or minimally processed diets following ... [https://www.nature.com/articles/s41591-025-03842-0]
- 3. Validity and accuracy of artificial intelligence-based dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229984/]
- 4. a pilot comparative validation study exploring the diet history ... [https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-025-01392-x]
- 5. The Essential Role of Dietitians in Clinical Trials [https://www.rdnutritionconsultants.com/single-post/essential-role-of-dietitians-in-clinical-trials]
- 6. Goals in Nutrition Science 2020-2025 - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7923694/]
- 7. Overview of Dietary Assessment Methods for Measuring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8338737/]
- 8. Validity of Dietary Assessment Methods When Compared ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00850/full]
- 9. 24-hour Dietary Recall (24HR) At a Glance [https://dietassessmentprimer.cancer.gov/profiles/recall/]
- 10. Comparisons to 24-Hour Dietary Recalls and Selected ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12569992/]
- 11. Smartphone Validation of a Food Frequency Questionnaire ... [https://www.sciencedirect.com/science/article/pii/S2475299125029610]
- 12. Development and validation of a smartphone image-based ... [https://www.nature.com/articles/s41598-022-19545-2]
- 13. Reproducibility and comparison of a digital food frequency ... [https://foodandnutritionresearch.net/index.php/fnr/article/view/10366]
- 14. Measurement Errors in Dietary Assessment Using Self- ... [https://www.sciencedirect.com/science/article/pii/S2161831322008274]
- 15. Reliability and Validity of Nutrient Assessment Applications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550805/]
- 16. Protocol for a Mixed Methods Study [https://www.researchprotocols.org/2025/1/e70194]
- 17. Validity and reproducibility of a web-based dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187487/]
- 18. Exploring Dietary Assessment Methods Used to Measure ... [https://www.mdpi.com/2072-6643/17/2/360]
- 19. Data Analysis for the 2025 Guidelines Committee Report [https://www.dietaryguidelines.gov/2025-advisory-committee-report/data-analysis]
- 20. Investigation and Assessment of AI's Role in Nutrition—An ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11723148/]
- 21. Advancements in Using AI for Dietary Assessment Based ... [https://www.jmir.org/2024/1/e51432/]
- 22. Dietary assessment methodologies in eating disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC12482415/]
- 23. A Scoping Review of Artificial Intelligence for Precision ... [https://www.sciencedirect.com/science/article/pii/S2161831325000341]
- 24. Nutrition and Dietetic Resources: Dietary Assessment Tools [https://libguides.mssm.edu/nutrition-dietetic-resources/dietary-assessment-tools]
- 25. Short Dietary Assessment Instruments | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/diet/screeners/]
- 26. Development and evaluation of a nutrient-based method ... [https://www.medrxiv.org/content/10.1101/2025.03.20.25324317v2.full-text]
- 27. Development and Validation of a New Tool for Assessing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12621074/]
- 28. Minimum days estimation for reliable dietary intake ... [https://www.nature.com/articles/s41430-025-01644-8]
- 29. Protocol of the validation of the experience sampling-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587619/]
- 30. Development and validation of an online tool for assessing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12594016/]
- 31. Biochemical validation of a food frequency questionnaire ... [https://www.sciencedirect.com/science/article/pii/S0939475325000882]
- 32. Artificial Intelligence Applications to Measure Food and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11638690/]
- 33. Artificial Intelligence in Nutrition and Dietetics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563881/]
- 34. Navigating next-gen nutrition care using artificial ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1518466/full]
- 35. DietAI24 as a framework for comprehensive nutrition ... [https://www.nature.com/articles/s43856-025-01159-0]
- 36. Machine learning models to predict micronutrient profile in ... [https://www.sciencedirect.com/science/article/pii/S2665927123000680]
- 37. An AI-based nutrition recommendation system [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1546107/full]
- 38. Intelligent diet recommendation system powered by ... [https://www.sciencedirect.com/science/article/pii/S2405457725029249]
- 39. AI nutrition recommendation using a deep generative ... [https://www.nature.com/articles/s41598-024-65438-x]
- 40. The Validity and Feasibility of Utilizing the Photo-Assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10818835/]
- 41. Automatic Image Recognition Meal Reporting Among Young ... [https://mhealth.jmir.org/2025/1/e60070]
- 42. Applying Image-Based Food-Recognition Systems on ... [https://www.sciencedirect.com/science/article/pii/S2161831323000935]
- 43. A deep learning model with machine vision system for ... [https://www.nature.com/articles/s41598-025-15755-6]
- 44. Tailored Prompting to Improve Adherence to Image-Based ... [https://mhealth.jmir.org/2024/1/e52074]
- 45. Unlocking Nutritional Secrets: Biomarkers Guide [https://www.numberanalytics.com/blog/ultimate-guide-biomarkers-nutritional-status-macronutrients]
- 46. of Micronutrients and Phytonutrients and Their... Biomarkers [https://pubmed.ncbi.nlm.nih.gov/36839326/]
- 47. Dietary assessment in intermittent fasting: validation of a ... [https://pubmed.ncbi.nlm.nih.gov/40791239/]
- 48. Personalized Nutrition Biomarkers and Dietary Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429899/]
- 49. Utilizing nutrition-related biomarkers to develop a ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1563220/full]
- 50. in Biomarkers | SpringerLink Nutrition [https://link.springer.com/referencework/10.1007/978-3-031-07389-2?error=cookies_not_supported&error=cookies_not_supported&error=cookies_not_supported&code=1733f7a5-20a7-4a46-a77e-3f128ff347e0&code=21be631b-0af8-4210-959f-025349b9fbd5&code=9b51baf6-45f1-4437-af0d-fac0ae3c5237]
- 51. Measuring energy, macro and micronutrient intake in UK children and... [https://bmcnutr.biomedcentral.com/articles/10.1186/s40795-019-0312-9]
- 52. Qualitative approaches to dietary assessment [https://www.fao.org/4/y5825e/y5825e07.htm]
- 53. Automated Diet Capture Using Voice Alerts and Speech ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10230351/]
- 54. An Image-Voice Dietary Assessment System for Estimating ... [https://www.jmir.org/2025/1/e65939]
- 55. Nutrition literacy predicts adherence to healthy/unhealthy diet patterns... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6827561/]
- 56. Relevance of Mathematical Optimization as a Tool for Diet ... [https://www.sciencedirect.com/science/article/pii/S2161831325001164]
- 57. Within-food-group optimization improves nutritional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518068/]
- 58. Food Pattern Modeling for the 2025 Advisory Committee ... [https://www.dietaryguidelines.gov/2025-advisory-committee-report/food-pattern-modeling]
- 59. Traditional Self-Reported Dietary Instruments Are Prone to ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2020.00090/full]
- 60. Improving dietary data collection tools for better nutritional ... [https://www.sciencedirect.com/science/article/pii/S2666990022000180]
- 61. A Decade of Dietary Assessment Methodology Research at ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10196585/]
- 62. Dietary Assessment | EGRP/DCCPS/NCI/NIH [https://epi.grants.cancer.gov/dietary-assessment/]
- 63. Family Socioeconomic Position and Eating Disorder ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368680/]
- 64. findings from the ALSPAC cohort [https://www.medrxiv.org/content/10.1101/2025.01.12.25320417v2.full-text]
- 65. Childhood Poverty Linked to Higher Risk of Adolescent ... [https://www.ajmc.com/view/childhood-poverty-linked-to-higher-risk-of-adolescent-eating-disorders]
- 66. The social epidemiology of binge-eating disorder and ... [https://jeatdisord.biomedcentral.com/articles/10.1186/s40337-023-00904-x]
- 67. Diagnosis and treatment of eating disorders in children and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10960190/]
- 68. Eating disorders: Involvement of pediatricians in their ... [https://www.analesdepediatria.org/en-eating-disorders-involvement-pediatricians-in-articulo-S2341287925002558]
- 69. Validation of a Visually Aided Dietary Assessment Tool to ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.844156/full]
- 70. Human Food Program (HFP) FY 2025 Priority Deliverables [https://www.fda.gov/about-fda/human-foods-program/human-food-program-hfp-fy-2025-priority-deliverables]
- 71. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 72. Color Contrast Guidelines for Text & UI Accessibility [https://daily.dev/blog/color-contrast-guidelines-for-text-and-ui-accessibility]
- 73. Social desirability bias in dietary self-report may ... [https://pubmed.ncbi.nlm.nih.gov/7635601/]
- 74. Gender differences in social desirability and approval ... [https://www.sciencedirect.com/science/article/abs/pii/S019566632200126X]
- 75. An Exploratory study of compliance with dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3259302/]
- 76. assessing risk of bias and rating the certainty of evidence [https://link.springer.com/article/10.1007/s00394-020-02464-1]
- 77. The impact of investigator bias in nutrition research [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1513343/full]
- 78. Diet to Data: Validation of a Bias-Mitigating Nutritional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348917/]
- 79. Validation of a web-based dietary assessment program ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1395252/full]
- 80. Protocol of the validation of the experience sampling-based ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-025-01232-3]
- 81. Relationship Among Macronutrients, Dietary Components ... [https://www.jmir.org/2025/1/e64749]
- 82. Artificial intelligence in personalized nutrition and food ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1636980/full]
- 83. Machine learning vs. traditional logistic regression: predictive ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-25621-9]
- 84. An Integrated AI Framework for Personalized Nutrition ... [https://www.mdpi.com/2076-3417/15/17/9283]
- 85. The Dietary Biomarkers Development Consortium: An ... [https://www.sciencedirect.com/science/article/pii/S2475299125028951]
- 86. Protocol of the validation of the experience sampling ... [https://pubmed.ncbi.nlm.nih.gov/41194100/]
- 87. A Systematic Review and Meta-Analysis of Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634532/]
- 88. Reliability and validity of assessing energy and nutrient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6350393/]
- 89. Development and Evaluation of the Reliability of a Semi- ... [https://www.mdpi.com/2072-6643/16/15/2490]
- 90. Health impact assessment and cost‒benefit analysis [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0326946]
- 91. Systematic review on the use of cost-benefit analysis to ... [https://pubmed.ncbi.nlm.nih.gov/40916133/]
- 92. Eight characteristics of rigorous multilevel implementation ... [https://implementationscience.biomedcentral.com/articles/10.1186/s13012-023-01302-2]
- 93. Quantitative Data Quality Assurance, Analysis and Presentation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056448/]
- 94. Methodological rigor in quantitative L2 research [https://www.sciencedirect.com/science/article/abs/pii/S2772766125000941]
- 95. A validation study comparing energy and nutrient intake ... [https://www.sciencedirect.com/science/article/pii/S089990072300360X]
- 96. Gephi - The Open Graph Viz Platform [https://gephi.org/]