Single Laboratory Validation (SLV) Fundamentals: A Guide for Reliable Analytical Results
This article provides a comprehensive guide to Single Laboratory Validation (SLV), a critical process for establishing the reliability of analytical methods within one laboratory.
Single Laboratory Validation (SLV) Fundamentals: A Guide for Reliable Analytical Results
Abstract
This article provides a comprehensive guide to Single Laboratory Validation (SLV), a critical process for establishing the reliability of analytical methods within one laboratory. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles of SLV, a step-by-step methodological approach for implementation, strategies for troubleshooting common pitfalls, and techniques for evaluating method performance against established standards. The content synthesizes current guidelines and best practices to equip laboratories with the knowledge to generate inspection-ready, defensible data that ensures product quality and patient safety.
What is Single Laboratory Validation? Building Your Core Understanding
Single-Laboratory Validation (SLV) represents a critical process in pharmaceutical and clinical laboratories, establishing documented evidence that an analytical method is fit for its intended purpose within a specific laboratory environment. This comprehensive technical guide examines SLV's fundamental role in ensuring data reliability, regulatory compliance, and patient safety throughout the method lifecycle. Framed within the broader context of analytical quality management, SLV serves as the practical implementation bridge between manufacturer validation and routine laboratory application, providing scientists with verified performance characteristics specific to their operational conditions. For researchers and drug development professionals, mastering SLV protocols is essential for generating defensible data that meets both scientific rigor and regulatory standards in pharmaceutical development and clinical diagnostics.
Single-Laboratory Validation (SLV) constitutes a systematic approach for establishing the performance characteristics of an analytical method when implemented within a specific laboratory setting. According to International Vocabulary of Metrology (VIM3) definitions, verification represents "provision of objective evidence that a given item fulfils specified requirements," whereas validation establishes that "the specified requirements are adequate for the intended use" [1]. In practical laboratory applications, SLV occupies the crucial space between comprehensive method validation (primarily a manufacturer's responsibility) and ongoing quality control, ensuring that methods transferred to individual laboratories maintain their reliability despite variations in personnel, equipment, and environmental conditions.
The fundamental distinction between validation and verification lies in their scope and purpose. Method validation comprehensively establishes performance characteristics for a new diagnostic tool, which remains primarily a manufacturer concern. Conversely, method verification constitutes a laboratory-focused process to confirm specified performance characteristics before a test system is implemented for patient testing or product release [1]. This distinction places SLV as a user-centric activity, confirming that pre-validated methods perform as expected within the unique operational context of a single laboratory.
In regulated laboratory environments, SLV provides the foundational evidence required for accreditation under international standards including ISO/IEC 17025 for testing laboratories and ISO 15189 for medical laboratories [1]. The process embodies the practical implementation of quality management systems, directly supporting correct diagnosis, risk assessment, and effective therapeutic monitoring in healthcare, while ensuring reliability in pharmaceutical quality control.
Core Validation Parameters and Acceptance Criteria
SLV protocols investigate multiple analytical performance characteristics to provide comprehensive method assessment. These parameters collectively ensure methods generate reliable, accurate, and precise data under normal operating conditions. The following table summarizes the essential validation parameters, their definitions, and typical acceptance criteria based on international guidelines [2] [3].
Table 1: Essential SLV Parameters and Acceptance Criteria
| Parameter | Definition | Testing Methodology | Acceptance Criteria |
|---|---|---|---|
| Accuracy | Closeness of agreement between accepted reference value and value found | Analysis of known concentrations vs. reference materials; spike recovery studies [3] | Recovery of 95-105% for 9 determinations over 3 concentration levels [2] [3] |
| Precision | Closeness of agreement between independent results under specified conditions | Repeatability (intra-assay) and intermediate precision (different days, analysts, equipment) [3] | %RSD ≤2% for 6 replicates at target concentration [2] |
| Specificity | Ability to measure analyte accurately despite potential interferents | Resolution of closely eluted compounds; peak purity tests using PDA/MS [3] | Resolution ≥1.5 between critical pairs; no interference from matrix [3] |
| Linearity | Ability to obtain results directly proportional to analyte concentration | Minimum of 5 concentration levels across specified range [3] | Correlation coefficient (r²) ≥ 0.99 [2] |
| Range | Interval between upper and lower analyte concentrations with acceptable precision, accuracy, and linearity | Verification across low, medium, and high concentrations | Established based on intended method application [3] |
| LOD | Lowest concentration of analyte that can be detected | Signal-to-noise ratio (3:1) or statistical calculation (3×SD/slope) [3] | Signal-to-noise ratio ≥3:1 [2] [3] |
| LOQ | Lowest concentration of analyte that can be quantified with acceptable precision and accuracy | Signal-to-noise ratio (10:1) or statistical calculation (10×SD/slope) [3] | Signal-to-noise ratio ≥10:1; precision and accuracy within ±20% [2] [3] |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters | Deliberate changes to pH (±0.2), temperature (±5°C), mobile phase composition [2] | No significant impact on accuracy, precision, or specificity [2] |
These parameters form the foundation of SLV protocols, with specific acceptance criteria tailored to the analytical method's intended application. The precision parameter encompasses three distinct measurements: repeatability (intra-assay precision under identical conditions), intermediate precision (within-laboratory variations including different days, analysts, or equipment), and reproducibility (collaborative studies between different laboratories) [3]. For SLV, repeatability and intermediate precision are essential, while reproducibility typically falls outside single-laboratory scope.
The mathematical foundation for these parameters includes rigorous statistical treatment. Random error, representing imprecision, is calculated as the standard error of estimate (Sy/x), which is the standard deviation of points about the regression line [1]. Systematic error, reflecting inaccuracy, is detected through linear regression analysis where the y-intercept indicates constant error and the slope indicates proportional error [1].
SLV Experimental Workflow and Protocol Implementation
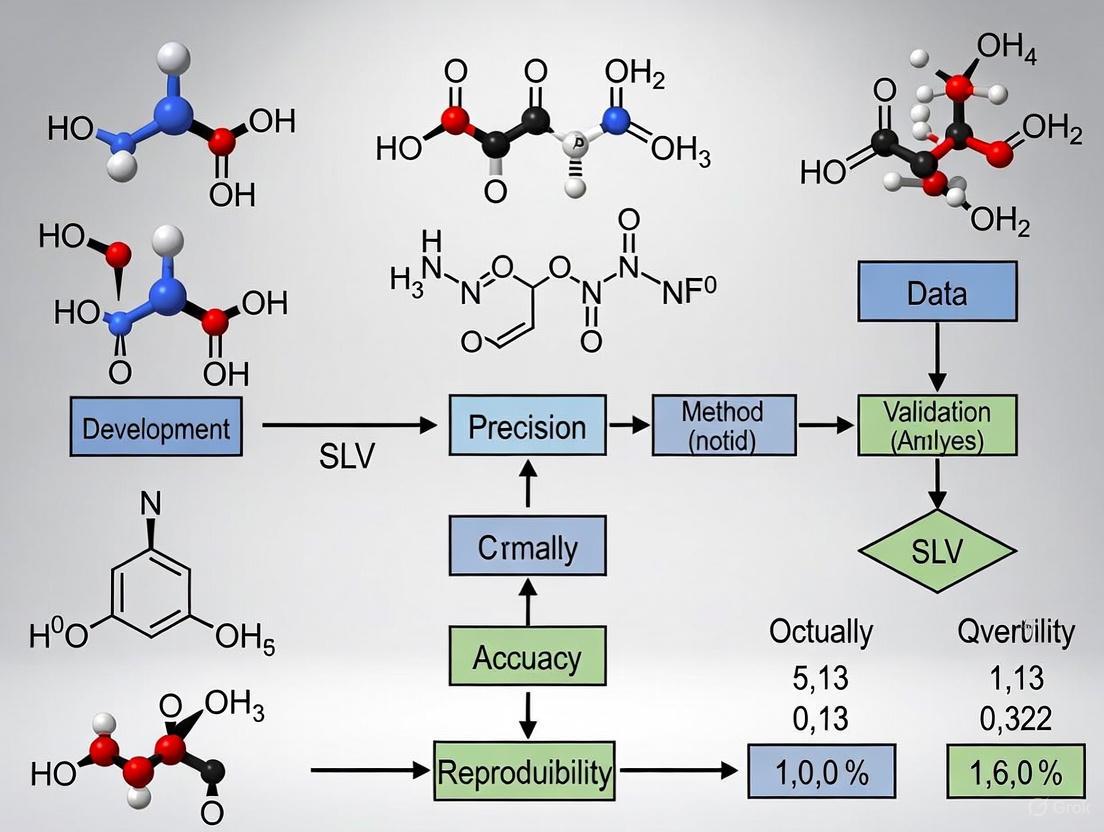
Implementing a robust SLV protocol requires meticulous planning and execution across sequential phases. The following workflow diagram illustrates the comprehensive SLV process from planning through documentation:
Diagram 1: Comprehensive SLV Workflow
Validation Plan Development
The validation plan establishes the strategic foundation for SLV, defining the scope, objectives, and success criteria. This document specifies the method's intended use, analytical performance characteristics to be evaluated, and predefined acceptance criteria based on regulatory guidelines and method requirements [2]. A well-constructed validation plan explicitly defines the experimental design, including sample types, number of replicates, statistical methods, and matrix effect testing protocols to ensure real-world applicability [2]. During this phase, collaboration with quality assurance (QA) and information technology (IT) departments is essential to address data integrity concerns and system access requirements proactively [2].
Experimental Execution
The experimental phase systematically investigates each validation parameter through controlled laboratory studies. Accuracy assessment requires data collection from a minimum of nine determinations across three concentration levels, reporting percent recovery of the known, added amount or the difference between mean and true value with confidence intervals [3]. Precision evaluation encompasses both repeatability (same analyst, same day) through nine determinations covering the specified range and intermediate precision using experimental design that monitors effects of different days, analysts, or equipment [3].
Specificity must be demonstrated through resolution of the two most closely eluted compounds, typically the major component and a closely eluted impurity [3]. Modern specificity verification increasingly incorporates peak purity testing using photodiode-array (PDA) detection or mass spectrometry (MS) to distinguish minute spectral differences not readily observed by simple overlay comparisons [3]. For linearity and range, guidelines specify a minimum of five concentration levels, with data reporting including the equation for the calibration curve line, coefficient of determination (r²), residuals, and the curve itself [3].
Documentation and Reporting
Comprehensive documentation provides the auditable trail demonstrating method validity. The validation report includes an executive summary highlighting key findings, detailed experimental results for each parameter, statistical analysis, and conclusions with formal sign-off by relevant stakeholders (analytical chemist, QA lead, lab manager) [2]. This documentation workflow ensures transparent reporting of any deviations or corrective actions, however minor, maintaining integrity throughout the validation process [2].
Critical Reagents and Research Solutions
Successful SLV implementation requires carefully selected reagents and materials that ensure method reliability. The following table details essential research reagent solutions and their functions within validation protocols:
Table 2: Essential Research Reagent Solutions for SLV
| Reagent/Material | Function in SLV | Critical Quality Attributes |
|---|---|---|
| Certified Reference Materials | Establish accuracy and trueness through comparison to accepted reference values [3] | Certified purity, stated uncertainty, stability documentation |
| System Suitability Standards | Verify chromatographic system performance prior to validation runs [3] | Reproducible retention, peak shape, and resolution characteristics |
| Matrix-Matched Calibrators | Account for matrix effects in biological and pharmaceutical samples [1] | Commutability with patient samples, appropriate analyte-free matrix |
| Quality Control Materials | Monitor precision across validation experiments [1] | Multiple concentration levels, stability, representative matrix |
| Forced Degradation Samples | Demonstrate specificity and stability-indicating capabilities [2] | Controlled degradation under stress conditions (heat, light, pH) |
| Interference Check Solutions | Evaluate analytical specificity against potential interferents [1] | Common interferents (hemoglobin, lipids, bilirubin, concomitant drugs) |
These reagents form the foundation of reliable SLV protocols, with quality attributes directly impacting validation outcomes. Certified reference materials, in particular, require verification of their uncertainty specifications and stability profiles to ensure accuracy measurements are scientifically defensible [3]. Matrix-matched calibrators must demonstrate commutability with actual patient samples to avoid misleading recovery results in clinical method validations [1].
Error Analysis and Measurement Uncertainty
Understanding and quantifying measurement errors represents a fundamental aspect of SLV, with direct implications for method reliability and patient safety. The following diagram illustrates the error classification and quantification framework:
Diagram 2: Error Analysis Framework
The primary purpose of method validation and verification is error assessment—determining the scope of possible errors within laboratory assay results and the extent to which this degree of errors could affect clinical interpretations and patient care [1]. Random error arises from unpredictable variations in repeated measurements and is quantified using standard deviation (SD) and coefficient of variation (CV) [1]. In SLV protocols, random error is calculated as the standard error of estimate (Sy/x), representing the standard deviation of the points about the regression line [1].
Systematic error reflects inaccuracy where control observations shift consistently in one direction from the mean value. Systematic errors manifest as either constant error (affecting all measurements equally) or proportional error (increasing with analyte concentration) [1]. Through linear regression analysis comparing test method results to reference values, the y-intercept indicates constant error while the slope indicates proportional error [1].
Total Error Allowable (TEa) represents the combined random and systematic error permitted by clinical requirements, available analytical methods, and proficiency testing expectations [1]. CLIA 88 has published allowable errors for numerous clinical tests, with recent expansions to include newer assays such as HbA1c and PSA [1]. The error index, calculated as (x-y)/TEa where x and y represent compared methods, provides a standardized approach for assessing method acceptability against established performance standards [1].
Measurement uncertainty expands upon traditional error analysis by providing a quantitative indication of result quality. Uncertainty estimation combines standard uncertainty (Us) from precision data and bias uncertainty (UB) from accuracy studies, resulting in combined standard uncertainty (Uc) and expanded uncertainty (U) using appropriate coverage factors [1]. This comprehensive approach to error quantification ensures methods meet both statistical and clinical performance requirements before implementation.
Advanced SLV Strategies and Lifecycle Management
For experienced professionals, advanced SLV strategies enhance efficiency and provide deeper methodological understanding. Design of Experiments (DoE) methodologies enable simultaneous investigation of multiple variables, efficiently uncovering interactions between factors such as pH and temperature that might be missed in traditional one-factor-at-a-time approaches [2]. DoE creates mathematical models of method behavior, supporting robust operational ranges rather than fixed operating points.
Statistical control charts provide enhanced monitoring beyond basic %RSD thresholds. Implementing X̄–R charts enables detection of subtle methodological drifts before they trigger formal revalidation requirements, supporting proactive method maintenance [2]. These tools transition SLV from a one-time event to continuous method performance verification.
Method transfer protocols establish formal frameworks for moving validated methods between laboratories or instrument platforms. A well-designed transfer plan compares critical parameters across systems, confirming equivalency through parallel testing and statistical analysis [2]. This approach ensures method integrity during technology upgrades or multisite implementations.
SLV represents the beginning, not the conclusion, of methodological quality management. A comprehensive lifecycle approach includes periodic reviews (typically annual or following major instrument service), defined change control procedures specifying revalidation triggers for modifications to critical reagents, software, or procedural steps, and ongoing specificity monitoring through forced-degradation studies to confirm stability-indicating capabilities [2]. This proactive management strategy safeguards against unexpected compliance gaps while maintaining methodological fitness for purpose throughout its operational lifetime.
Single-Laboratory Validation stands as an indispensable discipline within pharmaceutical and clinical laboratories, providing the critical link between manufacturer validation and routine analytical application. Through systematic assessment of accuracy, precision, specificity, and additional performance parameters, SLV delivers documented evidence of method reliability under actual operating conditions. The structured protocols, statistical rigor, and comprehensive documentation requirements detailed in this technical guide establish a foundation for generating scientifically defensible data that supports both regulatory compliance and patient care decisions. As analytical technologies advance and regulatory expectations evolve, the principles of SLV remain constant: ensuring that every method implemented within a laboratory demonstrates proven capability to deliver results fit for their intended purpose, ultimately contributing to medication safety, diagnostic accuracy, and therapeutic efficacy.
Analytical method validation is a foundational pillar in pharmaceutical development and quality control, providing documented evidence that a laboratory procedure is fit for its intended purpose. For scientists conducting single-laboratory validation (SLV) research, understanding the interconnected regulatory landscape is crucial for generating scientifically sound and compliant data. Three principal guidelines form the cornerstone of modern analytical validation: ICH Q2(R1), FDA guidance on analytical procedures, and USP General Chapter <1225>. While these frameworks share common objectives, each possesses distinct emphases and applications that laboratory researchers must navigate to ensure regulatory compliance and methodological rigor.
The validation paradigm has undergone a significant shift from treating validation as a one-time event to managing it as a dynamic lifecycle process. This evolution is embodied in the recent alignment of USP <1225> with ICH Q14 on analytical procedure development and the principles outlined in USP <1220> for the Analytical Procedure Life Cycle (APLC) [4]. For the SLV researcher, this means validation strategies must now extend beyond traditional parameter checks to demonstrate ongoing "fitness for purpose" through the entire method lifespan, from development and validation to routine use and eventual retirement [4].
Core Regulatory Guidelines
ICH Q2(R1): The International Benchmark
ICH Q2(R1), titled "Validation of Analytical Procedures: Text and Methodology," represents the globally recognized standard for validating analytical procedures. This harmonized guideline combines the former Q2A and Q2B documents, providing a unified framework for the validation of analytical methods used in pharmaceutical registration applications [5].
Scope and Application: ICH Q2(R1) establishes the fundamental validation parameters and methodologies required to demonstrate that an analytical procedure is suitable for detecting or quantifying an analyte in a specific matrix. It provides the foundational concepts that have been adopted by regulatory authorities worldwide, creating a streamlined path for international submissions [6] [5].
Key Validation Parameters: The guideline systematically defines the critical characteristics that require validation based on the type of analytical procedure (identification, testing for impurities, assay). These core parameters provide the structural framework for most modern validation protocols [6] [5].
FDA Guidance on Analytical Procedures
The U.S. Food and Drug Administration provides specific guidance for analytical procedures and methods validation that builds upon the ICH foundation while addressing regional regulatory requirements.
Regulatory Framework: The FDA's approach emphasizes method robustness as a critical parameter, requiring demonstration of analytical reliability under varying conditions [6]. The guidance includes detailed recommendations for life-cycle management of analytical methods and specific expectations for revalidation procedures [6].
Application-Specific Guidance: The FDA tailors its validation recommendations to specific product categories. For example, the agency has issued separate guidance documents for tobacco product applications, which recommend how manufacturers can provide validated and verified data for analytical procedures used in premarket submissions [7]. This demonstrates the FDA's risk-based approach to validation requirements across different product types with varying public health impacts.
USP <1225>: Compendial Validation Standards
United States Pharmacopeia General Chapter <1225> "Validation of Compendial Procedures" provides specific guidance for validating analytical methods used in pharmaceutical testing, with particular relevance to methods that may become compendial [8] [6].
Categorical Approach: USP <1225> outlines validation requirements for four categories of analytical procedures: Category I (identification tests), Category II (quantitative tests for impurities), Category III (limit tests), and Category IV (assay procedures) [6]. Each category has specific validation parameter requirements that form the basis for demonstrating method suitability.
Evolving Framework: USP <1225> is currently undergoing significant revision to align with modern validation paradigms. The proposed revision, published in Pharmacopeial Forum PF 51(6), adapts the chapter for validation of both non-compendial and compendial procedures and provides connectivity to related USP chapters, particularly <1220> Analytical Procedure Life Cycle [9] [4]. This revision introduces critical concepts including "Reportable Result" as the definitive output supporting compliance decisions and "Fitness for Purpose" as the overarching goal of validation [9].
Table 1: Comparison of Key Validation Parameters Across Regulatory Guidelines
| Validation Parameter | ICH Q2(R1) | FDA Guidance | USP <1225> |
|---|---|---|---|
| Accuracy | Required | Required | Required |
| Precision | Required | Required | Required |
| Specificity | Required | Required | Required |
| Detection Limit | Required | Required | Required |
| Quantitation Limit | Required | Required | Required |
| Linearity | Required | Required | Required |
| Range | Required | Required | Required |
| Robustness | Recommended | Emphasized | Recommended |
| System Suitability | Not covered | Referenced | Required |
Method Validation Versus Verification
A critical distinction for SLV researchers is understanding the difference between method validation and method verification, as the regulatory requirements and scientific approaches differ significantly.
Method Validation is a comprehensive, documented process that proves an analytical method is acceptable for its intended use. It involves rigorous testing and statistical evaluation of all relevant parameters and is typically required when developing new methods or substantially modifying existing ones [10] [8].
Method Verification confirms that a previously validated method performs as expected under specific laboratory conditions. It involves limited testing to demonstrate the laboratory's ability to execute the method properly and is typically employed when adopting compendial or standardized methods [10] [8].
For USP compendial methods, laboratories typically perform verification rather than full validation, as the method has already been validated by USP [8]. However, for non-compendial or modified compendial methods, full validation is necessary to demonstrate reliability for the specific application [8].
Experimental Protocols for Validation Parameters
Accuracy Assessment Protocol
Accuracy demonstrates the closeness of agreement between the value accepted as a true reference value and the value found through testing [6] [5].
Experimental Methodology: Prepare a minimum of nine determinations across the specified range of the procedure (e.g., three concentrations/three replicates each). For drug assay methods, this typically involves spiking placebo with known quantities of analyte relative to the target concentration (e.g., 80%, 100%, 120%). Compare results against accepted reference values using statistical intervals for evaluation [4] [8].
Data Interpretation: Calculate percent recovery for each concentration and overall mean recovery. Acceptance criteria vary based on method type but typically fall within 98-102% for drug substance assays and 95-105% for impurity determinations at the quantification limit [8].
Precision Evaluation Protocol
Precision validation encompasses repeatability, intermediate precision, and reproducibility [6] [5].
Repeatability (Intra-assay Precision): Perform a minimum of nine determinations covering the specified range (e.g., three concentrations/three replicates) or six replicates at 100% of the test concentration. The replication strategy should reflect the final routine testing procedure that will generate the reportable result [4] [8].
Intermediate Precision: Demonstrate method reliability under variations occurring within a single laboratory over time, including different analysts, equipment, days, and reagent lots. The experimental design should incorporate the same replication strategy used for routine testing to properly capture time-based variability [4].
Statistical Evaluation: Express precision as relative standard deviation (RSD). For assay validation of drug substances, typical acceptance criteria for repeatability is RSD ≤ 1.0% for HPLC methods, while intermediate precision should show RSD ≤ 2.0% [8].
Specificity and Selectivity Protocol
Specificity demonstrates the ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [6] [5].
For Identification Tests: Demonstrate positive responses for samples containing the target analyte and negative responses for samples without the analyte or with structurally similar compounds.
For Assay and Impurity Tests: Use chromatographic methods to demonstrate baseline separation of analytes from potential interferents. For stability-indicating methods, stress samples (acid, base, oxidative, thermal, photolytic) should demonstrate no co-elution of degradation products with the main analyte [8].
For Chromatographic Methods: Report resolution factors between the analyte and closest eluting potential interferent. Typically, resolution > 2.0 between critical pairs demonstrates adequate specificity [8].
Table 2: Validation Protocol Requirements by Analytical Procedure Category
| Procedure Type | Accuracy | Precision | Specificity | LOD/LOQ | Linearity | Range |
|---|---|---|---|---|---|---|
| Identification | - | - | Yes | - | - | - |
| Impurity Testing | ||||||
| • Quantitative | Yes | Yes | Yes | Yes (LOQ) | Yes | Yes |
| • Limit Test | - | - | Yes | Yes (LOD) | - | - |
| Assay | ||||||
| • Content/Potency | Yes | Yes | Yes | - | Yes | Yes |
| • Dissolution | Yes | Yes | - | - | Yes | Yes |
The Validation Workflow and Lifecycle Approach
The modern validation paradigm has shifted from a one-time exercise to an integrated lifecycle approach, as illustrated below:
This lifecycle approach integrates with the broader quality system through knowledge management, where data generated during method development, platform knowledge from similar methods, and experience with related products constitute legitimate inputs to validation strategy [4].
Essential Research Reagents and Materials
Successful method validation requires carefully selected, well-characterized reagents and materials. The following toolkit represents essential components for pharmaceutical analytical methods:
Table 3: Essential Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Reference Standard | Provides the true value for accuracy determination and calibration curve establishment | Certified purity (>98.5%), proper storage conditions, stability documentation |
| Placebo/Blank Matrix | Evaluates specificity/selectivity by detecting potential interference from sample matrix | Represents final formulation without active ingredient, matches composition |
| Chromatographic Columns | Separation component for specificity and selectivity demonstrations | Multiple column lots from different manufacturers, appropriate selectivity |
| Mobile Phase Components | Creates separation environment in chromatographic methods | HPLC-grade or better, specified pH range, organic content, buffer concentration |
| System Suitability Standards | Verifies chromatographic system performance before and during validation experiments | Resolution mixture, tailing factor standards, precision standards |
Current Regulatory Developments and Future Directions
The regulatory landscape for analytical method validation continues to evolve, with several significant developments impacting SLV research:
USP <1225> Revision: The proposed revision of USP <1225>, currently open for comment until January 31, 2026, represents a fundamental shift in validation philosophy [9]. The updated chapter emphasizes "fitness for purpose" as the overarching goal and introduces the "reportable result" as the definitive output supporting compliance decisions [9] [4]. This revision better aligns with ICH Q2(R2) principles and integrates with the analytical procedure lifecycle described in USP <1220> [9].
Enhanced Statistical Approaches: The revised validation frameworks introduce more sophisticated statistical methodologies, including the use of statistical intervals (confidence, prediction, tolerance) as tools for evaluating precision and accuracy in relation to decision risk [9] [4]. Combined evaluation of accuracy and precision is described in more detail than in previous versions, recognizing that what matters for reportable results is the total error combining both bias and variability [4].
Risk-Based Validation Strategies: Modern guidelines increasingly encourage risk-based approaches that match validation effort to analytical criticality and complexity [8]. This represents a shift from the traditional category-based approach that prescribed specific validation parameters based solely on method type rather than method purpose [4].
For single-laboratory validation researchers, staying current with these evolving standards while maintaining robust, defensible validation practices remains essential for generating regulatory-ready data and ensuring product quality and patient safety.
Single-Laboratory Method Validation (SLV) is a critical process that establishes documented evidence, through laboratory studies, that an analytical procedure is fit for its intended purpose within a single laboratory environment [3]. For researchers and drug development professionals, SLV forms the foundational pillar of data integrity, ensuring that the results generated are reliable, consistent, and defensible before a method is transferred to other laboratories or submitted for regulatory approval. The process demonstrates that the performance characteristics of the method meet the requirements for the intended analytical application, providing an assurance of reliability during normal use [3] [11]. In a regulated environment, SLV is not merely good scientific practice but a mandatory compliance requirement for institutions adhering to standards from bodies like the FDA, ICH, and ISO [3] [1].
The core parameters discussed in this guide—Accuracy, Precision, Specificity, Linearity, Range, LOD, LOQ, and Robustness—represent the fundamental analytical performance characteristics that must be investigated during any method validation protocol [3]. These parameters collectively provide a comprehensive picture of a method's capability and limitations. The following workflow outlines the typical stages of analytical method development and validation within a single laboratory context.
Core Validation Parameters: Definitions and Experimental Protocols
This section details the eight core validation parameters, providing their formal definitions, regulatory significance, and detailed experimental methodologies for assessment in a single-laboratory setting.
Accuracy
Accuracy is defined as the closeness of agreement between an accepted reference value and the value found in a sample [3] [12]. It reflects the trueness of measurement and is typically expressed as percent recovery of a known, added amount [3]. Accuracy should be established across the specified range of the method [3].
Experimental Protocol:
- For Drug Substances: Compare results to the analysis of a standard reference material, or to a second, well-characterized method [3].
- For Drug Products: Analyze synthetic mixtures of the drug product spiked with known quantities of components [3].
- For Impurities: Spike the drug substance or product with known amounts of impurities (if available) and determine the recovery [3].
- Data Collection: Collect data from a minimum of nine determinations over a minimum of three concentration levels covering the specified range (e.g., three concentrations, three replicates each) [3]. Recovery is often expected to be within 95–105% for the assay of the drug substance or product [2].
Precision
Precision expresses the closeness of agreement (degree of scatter) among a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [3] [11]. It is commonly broken down into three tiers:
- Repeatability (Intra-assay Precision): Precision under the same operating conditions over a short interval of time [3]. Assessed with a minimum of nine determinations covering the specified range (three concentrations, three repetitions each) or a minimum of six determinations at 100% of the test concentration [3]. Results are reported as %RSD (Relative Standard Deviation), with an aim for ≤2% for assay methods [2].
- Intermediate Precision: Within-laboratory variations due to random events such as different days, different analysts, or different equipment [3] [12]. An experimental design (e.g., two analysts preparing and analyzing replicates on different HPLC systems) is used, and results are compared using statistical tests (e.g., Student's t-test) [3].
- Reproducibility (Between-laboratory): Precision between laboratories, typically assessed during collaborative studies for method standardization [3] [13].
Experimental Protocol for Repeatability:
- Prepare a homogeneous sample at 100% of the test concentration.
- Analyze a minimum of six independent replicates of this sample.
- Calculate the mean, standard deviation (SD), and %RSD of the results.
- Compare the %RSD against pre-defined acceptance criteria.
Specificity
Specificity is the ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [3] [11]. It ensures that a peak's response is due to a single component.
Experimental Protocol:
- For Chromatographic Methods: Inject blanks, placebo samples, stressed samples (forced degradation), and samples spiked with potential interferents (impurities, excipients) [3].
- Peak Purity Assessment: Use photodiode-array (PDA) detection or mass spectrometry (MS) to demonstrate that the analyte peak is pure and not co-eluting with any other peak [3]. Modern PDA software compares spectra across the peak to determine purity.
- Resolution: Demonstrate resolution between the analyte and the most closely eluting potential interferent. Resolution (Rs) should typically be >1.5 [3].
Linearity
Linearity is the ability of the method to elicit test results that are directly, or by a well-defined mathematical transformation, proportional to the analyte concentration within a given range [3] [12].
Experimental Protocol:
- Prepare a minimum of five (recommended six) standard solutions whose concentrations span the intended range (e.g., 80-120% of the target concentration) [3] [11].
- Analyze each solution in a random order to avoid time-based bias.
- Plot the analyte response against the concentration.
- Perform linear regression analysis to calculate the slope, y-intercept, and coefficient of determination (r²). The correlation coefficient (r) should be ≥ 0.99 [2] [11].
Range
The range of an analytical method is the interval between the upper and lower concentrations (inclusive) of analyte for which it has been demonstrated that the method has a suitable level of precision, accuracy, and linearity [3] [11]. It is derived from the linearity study.
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
- LOD: The lowest concentration of an analyte in a sample that can be detected, but not necessarily quantified, under the stated experimental conditions. It is a limit test [3].
- LOQ: The lowest concentration of an analyte in a sample that can be quantitatively determined with acceptable precision and accuracy [3].
Experimental Protocols:
- Signal-to-Noise Ratio (S/N): Most common for chromatographic methods. The LOD is typically a S/N of 3:1, and the LOQ is a S/N of 10:1 [3] [2].
- Standard Deviation of the Response and Slope: LOD = 3.3σ/S and LOQ = 10σ/S, where σ is the standard deviation of the response (from the blank or low-concentration samples) and S is the slope of the calibration curve [3] [1].
- Visual Evaluation: Determine by analysis of samples with known concentrations of analyte.
Robustness
The robustness of an analytical procedure is a measure of its capacity to remain unaffected by small, deliberate variations in method parameters and provides an indication of its reliability during normal usage [3] [13]. It is typically evaluated during the method development phase.
Experimental Protocol (Screening Design):
- Identify Factors: Select critical method parameters (e.g., mobile phase pH (±0.2), flow rate (±5%), column temperature (±5°C), wavelength) [2] [13].
- Design Experiment: Use a multivariate screening design (e.g., full factorial, fractional factorial, or Plackett-Burman design) to efficiently study multiple factors simultaneously [13].
- Perform Analysis: Execute the experimental runs and monitor critical quality attributes (e.g., retention time, resolution, tailing factor).
- Analyze Data: Use statistical analysis to identify which factors have a significant effect on the method's performance. Establish system suitability test limits based on these findings [13].
The diagram below illustrates the key factors and responses typically evaluated in a robustness study for a chromatographic method.
The table below provides a consolidated summary of the core validation parameters, their definitions, and typical experimental acceptance criteria for a quantitative assay, serving as a quick reference for researchers.
Table 1: Summary of Core Validation Parameters and Typical Acceptance Criteria for a Quantitative Assay
| Parameter | Definition | Typical Experimental Protocol & Acceptance Criteria |
|---|---|---|
| Accuracy [3] | Closeness of agreement between the measured value and a true or accepted reference value. | Protocol: Analyze a minimum of 9 determinations over 3 concentration levels.Criteria: Mean recovery of 95-105% [2]. |
| Precision [3] | Closeness of agreement between a series of measurements from multiple sampling of the same homogeneous sample. | Protocol (Repeatability): 6 replicates at 100% test concentration.Criteria: %RSD ≤ 2.0% for assay [2]. |
| Specificity [3] | Ability to measure the analyte unequivocally in the presence of other components. | Protocol: Inject blank, placebo, and stressed samples. Use PDA or MS for peak purity.Criteria: No interference; resolution >1.5 from closest eluting peak. |
| Linearity [3] [11] | Ability to obtain results directly proportional to analyte concentration. | Protocol: Minimum of 5 concentrations across the specified range (e.g., 80-120%).Criteria: Correlation coefficient r ≥ 0.990 [2] [11]. |
| Range [3] [11] | The interval between the upper and lower concentrations for which linearity, accuracy, and precision are demonstrated. | Derived from the linearity and accuracy studies. Must be specified (e.g., 80-120% of target concentration). |
| LOD [3] | Lowest concentration of analyte that can be detected. | Protocol: Based on S/N ratio or LOD=3.3σ/S.Criteria: S/N ratio ≥ 3:1. |
| LOQ [3] | Lowest concentration of analyte that can be quantified with acceptable precision and accuracy. | Protocol: Based on S/N ratio or LOQ=10σ/S.Criteria: S/N ratio ≥ 10:1; Precision (%RSD) and Accuracy at LOQ should be documented. |
| Robustness [13] | Capacity of the method to remain unaffected by small, deliberate variations in method parameters. | Protocol: Deliberately vary parameters (e.g., pH, flow rate, temperature) in a structured design.Criteria: System suitability criteria are met despite variations. |
Essential Research Reagent Solutions and Materials
The successful execution of validation protocols requires high-quality materials and reagents. The following table lists key items essential for conducting method validation studies.
Table 2: Key Research Reagent Solutions and Materials for Method Validation
| Item | Function in Validation |
|---|---|
| Certified Reference Standards [3] | Used to establish accuracy and linearity. Provides an analyte of known identity and purity to serve as the benchmark for all measurements. |
| High-Purity Solvents & Reagents | Ensure the baseline response (noise) is minimized, critical for LOD/LOQ determinations, and prevent introduction of interfering species affecting specificity. |
| Placebo Matrix | A sample containing all components except the analyte, used in specificity and accuracy (recovery) studies to confirm the absence of interference from excipients or the sample matrix [3]. |
| System Suitability Test Solutions [3] | A reference preparation used to verify that the chromatographic system is adequate for the analysis before and during the validation runs. Typically tests for resolution, tailing factor, and precision. |
| Stressed Samples (Forced Degradation) | Samples exposed to stress conditions (e.g., heat, light, acid/base) to generate degradants, which are used to validate the stability-indicating property and specificity of the method [2]. |
The rigorous assessment of the eight core validation parameters—Accuracy, Precision, Specificity, Linearity, Range, LOD, LOQ, and Robustness—is fundamental to establishing the scientific soundness and regulatory credibility of any analytical method developed within a single laboratory. This guide has provided detailed experimental methodologies and acceptance criteria aligned with international guidelines [3] [14]. A well-executed SLV provides documented evidence that the method is fit for its intended purpose, instills confidence in the generated data, and forms a solid foundation for subsequent method transfer or collaborative studies [11]. As the analytical lifecycle progresses, continuous monitoring and controlled revalidation ensure the method remains in a validated state throughout its operational use [2].
The Critical Link Between SLV, Data Integrity, and Patient Safety
In the development and monitoring of pharmaceuticals, the integrity of data is not merely a regulatory requirement—it is the very bedrock of patient safety. Single-laboratory validation (SLV) serves as the critical scientific foundation upon which this data integrity is built. SLV represents the comprehensive process of establishing, through extensive laboratory studies, that an analytical method is reliable, reproducible, and fit for its intended purpose within a single laboratory environment prior to multilaboratory validation [15]. This rigorous demonstration of methodological robustness is paramount for generating trustworthy data that informs decisions across the entire drug lifecycle, from initial development to post-market surveillance.
The consequences of analytical inadequacy are severe. In the broader healthcare context, poor data quality is not just a technical problem; it is a direct patient safety risk [16]. When professionals doubt the information in front of them, clinical decisions are compromised, highlighting that digital transformation and advanced analytics can only move at the speed of trust. This whitepaper examines the integral relationship between SLV, data integrity, and patient safety, providing researchers and drug development professionals with the technical frameworks necessary to uphold these fundamental standards.
Single-Laboratory Validation: Principles and Protocols
Defining SLV and Its Strategic Importance
Single-laboratory validation is the essential first step in demonstrating that an analytical method meets predefined acceptance criteria for its intended application before transfer to other laboratories. The strategic importance of SLV lies in its ability to provide a controlled, initial assessment of method performance, identifying potential issues early and reducing costs associated with method failure during subsequent collaborative studies [15].
For the pharmaceutical researcher, SLV is particularly crucial when developing methods for novel compounds or complex matrices where standardized methods may not exist. This process ensures that validated methods are essential for regulators, the industry, and basic and clinical researchers alike, creating a foundation of trust in the data generated [15]. By incorporating accurate chemical characterization data in clinical trial reports, there is potential for correlating material content with effectiveness, ultimately leading to more conclusive findings about drug safety and efficacy.
Core Validation Parameters and Experimental Protocols
A robust SLV must systematically evaluate specific performance characteristics to ensure the method is fit for purpose. The experimental protocols for assessing these parameters must be meticulously designed and executed to generate defensible data.
Table 1: Essential SLV Parameters and Experimental Protocols
| Validation Parameter | Experimental Protocol | Acceptance Criteria |
|---|---|---|
| Accuracy/Trueness | Analysis of samples spiked with known quantities of analyte across the validated range; comparison to reference materials or comparison with a validated reference method [15]. | Mean recovery of 70-120% with RSD ≤10% for pharmaceutical applications, though specific criteria may vary based on analyte and matrix. |
| Precision | Repeated analysis (n≥6) of homogeneous samples at multiple concentration levels; includes repeatability (intra-day) and intermediate precision (inter-day, different analysts, different instruments) [15]. | RSD ≤5% for repeatability, ≤10% for intermediate precision, depending on analyte concentration and method complexity. |
| Specificity/Selectivity | Analysis of placebo or blank samples, samples with potentially interfering compounds, and stressed samples (e.g., exposed to light, heat, acid/base degradation) to demonstrate separation from interferents [15]. | No interference at the retention time of the analyte; peak purity confirmation using diode array or mass spectrometric detection. |
| Linearity and Range | Analysis of minimum 5 concentration levels across the claimed range, with each level prepared and analyzed in duplicate; evaluation via linear regression analysis [15]. | Correlation coefficient (r) ≥0.990; residuals randomly distributed around the regression line. |
| Limit of Detection (LOD) & Quantification (LOQ) | LOD: Signal-to-noise ratio of 3:1; LOQ: Signal-to-noise ratio of 10:1 with acceptable accuracy and precision (≤20% RSD) at this level [15]. | LOQ should be at or below the lowest concentration in the calibration curve with acceptable accuracy and precision. |
| Robustness/Ruggedness | Deliberate, small variations in method parameters (e.g., mobile phase pH ±0.2 units, column temperature ±5°C, flow rate ±10%); evaluation of impact on results [15]. | Method remains unaffected by small variations; system suitability criteria still met. |
The experimental workflow for establishing these parameters follows a logical progression from initial method development through to final validation, as illustrated below:
Figure 1: SLV Experimental Workflow - This diagram illustrates the systematic progression of single-laboratory validation from initial development through troubleshooting to final completion.
Data Integrity and Data Validity: The Analytical Framework
Distinguishing Between Data Integrity and Validity
In the context of pharmaceutical analysis, a clear distinction must be drawn between data integrity and data validity, as both represent critical but distinct aspects of data quality:
Data Integrity refers to the maintenance and assurance of the consistency, accuracy, and reliability of data throughout its complete lifecycle [17]. It ensures that data remains unaltered and uncompromised from its original state when created, transmitted, or stored. Data integrity is concerned with the "wholeness" and "trustworthiness" of data, focusing on preventing unauthorized modifications, ensuring completeness, and maintaining accuracy across the data's entire existence [18].
Data Validity refers to the extent to which data is accurate, relevant, and conforms to predefined rules or standards [18]. It ensures that data meets specific criteria or constraints, making it suitable for its intended purpose. Data validity checks if data is properly formatted, within acceptable ranges, and consistent with predefined business rules or scientific requirements.
Table 2: Comparative Analysis: Data Integrity vs. Data Validity
| Aspect | Data Integrity | Data Validity |
|---|---|---|
| Primary Focus | Overall trustworthiness and protection of data throughout its lifecycle [17] | Conformance to predefined rules and fitness for intended purpose [18] |
| Temporal Scope | Entire data lifecycle (creation, modification, storage, transfer, archiving) [17] | Point-in-time assessment against specific criteria |
| Key Measures | Access controls, audit trails, encryption, backup systems, error detection [17] [18] | Validation rules, data entry checks, automated validation, manual review [18] |
| Risk Addressed | Unauthorized alteration, data corruption, incomplete data, fabrication | Incorrect data entry, out-of-range values, improper formatting |
| Impact on Patient Safety | Prevents systematic data corruption that could affect multiple studies or decisions [16] | Prevents individual data points from leading to incorrect conclusions |
Implementing Data Integrity Controls in the Laboratory
The implementation of robust data integrity controls is essential for maintaining trust in analytical data. Key measures include:
- Access Controls: Limit system and data access based on user roles and responsibilities to prevent unauthorized modifications [18]. Implement unique user credentials and regularly review access privileges.
- Audit Trails: Maintain secure, computer-generated, time-stamped electronic audit trails that independently record user activities [18]. These trails must be retained for the entire data lifecycle and regularly reviewed.
- Data Validation and Verification: Implement validation rules during data entry and automated validation checks to verify accuracy and completeness before data storage [18].
- Error Handling Mechanisms: Establish procedures to capture and address data inconsistencies or exceptions promptly, with alerts to notify relevant personnel about potential integrity issues [18].
The Patient Safety Connection: From Laboratory to Clinic
Pharmacovigilance: The Clinical Extension of Analytical Quality
The principles of SLV and data integrity extend directly into clinical practice through pharmacovigilance, defined as "the science and research relating to the detection, assessment, understanding and prevention of adverse effects or any other medicine/vaccine related problem" [19]. Pharmacovigilance represents the clinical manifestation of the quality continuum that begins with analytically sound laboratory data.
Pharmacovigilance has evolved from "a largely recordkeeping function to proactively identifying safety issues ('signals') and taking actions to minimize or mitigate risk to patients" [20]. This progression mirrors the evolution of quality systems in analytical laboratories from simple data recording to proactive quality risk management. The signal management process in pharmacovigilance directly parallels method validation in the laboratory, both systematically assessing potential risks to ensure patient safety.
Consequences of Data Quality Failures in Healthcare
The direct impact of poor data quality on patient safety is increasingly recognized as a critical healthcare challenge. Recent findings indicate that:
- 64% of healthcare professionals believe digital patient data is incomplete, and half report they must double-check its accuracy before acting [16].
- 47% of healthcare professionals have observed patient safety risks arising directly from digital health technologies [16].
- Inaccurate patient tracking lists can lead to patients being overlooked, particularly dangerous when dealing with referral backlogs where patients await initial clinical contact [16].
These data quality issues represent more than mere administrative inefficiencies; they constitute a serious and ongoing patient safety risk that can directly affect clinical decision-making [16]. The relationship between data quality and patient safety forms an interconnected system where failures at any stage can compromise the entire process:
Figure 2: Data Quality Impact Pathway - This diagram illustrates how robust processes create a safety continuum (top), while failures at any stage compromise patient safety (bottom).
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of SLV requires specific materials and reagents tailored to the analytical methodology and matrix. The following toolkit outlines essential solutions for pharmaceutical method validation:
Table 3: Essential Research Reagent Solutions for SLV
| Reagent/Material | Function in SLV | Application Examples |
|---|---|---|
| Certified Reference Standards | Provide traceable, quality-controlled substances for method calibration and accuracy determination [15]. | Quantification of active pharmaceutical ingredients, impurity profiling, method calibration. |
| Stable Isotope-Labeled Internal Standards | Compensate for matrix effects, extraction efficiency variations, and instrument fluctuations in mass spectrometry [15]. | LC-MS/MS quantification of drugs and metabolites in biological matrices. |
| Matrix-Matched Calibrators | Account for matrix effects by preparing standards in the same matrix as samples (e.g., plasma, urine, tissue homogenates) [15]. | Bioanalytical method validation for pharmacokinetic studies. |
| Quality Control Materials | Monitor method performance over time at defined concentrations (low, medium, high) across the analytical range [15]. | Ongoing method verification, inter-day precision assessment. |
| Sample Preparation Reagents | Enable extraction, purification, and concentration of analytes from complex matrices [15]. | Solid-phase extraction cartridges, protein precipitation solvents, derivatization reagents. |
The critical link between single-laboratory validation, data integrity, and patient safety forms an unbreakable chain connecting laboratory science to clinical outcomes. SLV provides the foundational evidence that analytical methods are capable of generating reliable data, while robust data integrity measures ensure this reliability is maintained throughout the data lifecycle. This analytical rigor directly supports pharmacovigilance activities and clinical decision-making that protects patients from harm.
For researchers, scientists, and drug development professionals, upholding these standards is both a scientific imperative and an ethical obligation. As the industry moves toward increasingly sophisticated analytical technologies and data systems, the fundamental principles outlined in this whitepaper remain constant: rigorous method validation, uncompromising data integrity, and an unwavering focus on patient safety must guide all aspects of pharmaceutical development and monitoring. By maintaining this culture of quality, the scientific community can ensure that patients receive medications whose benefits have been accurately characterized and whose risks are properly understood and managed.
Method validation is an essential component of quality assurance in analytical chemistry, ensuring that analytical methods produce reliable data fit for their intended purpose. Within regulated environments, two primary approaches exist for establishing method validity: Single Laboratory Validation (SLV) and Full Validation (often achieved through an interlaboratory collaborative trial). The fundamental distinction lies in their scope and applicability—SLV establishes that a method is suitable for use within a single laboratory, while full validation demonstrates its fitness for purpose across multiple laboratories.
These processes are governed by international standards and guidelines from organizations including ISO, IUPAC, and AOAC INTERNATIONAL. For researchers and drug development professionals, selecting the appropriate validation pathway has significant implications for resource allocation, regulatory compliance, and the reliability of generated data. This guide examines the technical principles, applications, and procedural details of both approaches to inform strategic decision-making in research and development.
Core Principles and Definitions
Single Laboratory Validation (SLV)
Single Laboratory Validation refers to the process where a laboratory conducts studies to demonstrate that an analytical method is fit for its intended purpose within that specific laboratory [21]. SLV determines key performance characteristics of a method—such as accuracy, precision, and selectivity—to prove reliability for a defined analytical system [21]. The results of an SLV are primarily valid only for the laboratory that conducted the study [22].
SLV serves several critical functions: ensuring method viability before committing to a formal collaborative trial, providing evidence of reliability when collaborative trial data is unavailable, and verifying that a laboratory can correctly implement an "off-the-shelf" validated method [21]. In medical laboratories, the SLV approach acts as an assessment of the entire analytical system, incorporating all available information on potential uncertainty influences on the final result [23].
Full Validation
Full Validation typically involves an interlaboratory method performance study (collaborative study/trial) conforming to internationally accepted protocols [21]. This approach establishes method performance characteristics through a structured study across multiple independent laboratories, providing a broader assessment of method robustness across different environments, operators, and equipment.
Full validation represents the most comprehensive approach for methods intended for widespread or regulatory use. The International Harmonised Protocol and ISO standards specify minimum requirements for laboratories and test materials to constitute a full validation [21]. Once fully validated through a collaborative trial, user laboratories need only verify that they can achieve the published performance characteristics, significantly reducing the validation burden on individual laboratories [21] [22].
Comparative Analysis: SLV vs. Full Validation
When to Select Each Approach
The decision between SLV and full validation depends on multiple factors including intended method application, regulatory requirements, available resources, and timeline constraints.
Single Laboratory Validation is appropriate when:
- Assessing method viability before investing in a formal collaborative trial [21]
- Collaborative trial data is unavailable or conducting a formal interlaboratory study is impractical [21]
- The method will be used in only one laboratory for specialized applications [22]
- Dealing with infrequent product manufacturing or small batch production [24]
- Working with products not in their final design or expected to be modified [24]
Full Validation is necessary when:
- The method is intended for widespread use across multiple laboratories [21]
- Regulatory compliance requires fully validated methods (e.g., food testing, pharmaceutical submissions) [21]
- Standardized methods are being developed for publication or regulatory recognition
- The total cost of a collaborative trial is justified by widespread use of the method [21]
Procedural and Resource Requirements
The following table compares key procedural aspects of SLV versus full validation for sterilization dose setting, illustrating typical differences in scope and resource commitment:
Table 1: Comparison of Procedural Requirements for Sterilization Dose Setting
| Test Component | Full Validation | Single Lot Validation |
|---|---|---|
| Bioburden Testing | 30 unirradiated samples (10 from each of 3 production lots) [24] | 10 unirradiated samples from the single lot to be validated [24] |
| Tests of Sterility | 10 samples irradiated at verification dose [24] | 10 samples per lot tested [24] |
| Applicability | Applies to future lots with controlled processes [24] | Applies only to the specific lot tested [24] |
| Time Investment | Longer initial timeline but no delay for future lots [24] | Shorter initial timeline but requires validation for each new lot [24] |
Advantages and Disadvantages
Each validation approach offers distinct advantages and poses specific limitations that must be considered during method development planning.
Table 2: Advantages and Disadvantages of Each Validation Approach
| Validation Type | Advantages | Disadvantages |
|---|---|---|
| Full Validation | • Lowest cost per test for ongoing validations [24] • Least total product used to reach full validation [24] • No delay in use of new lots awaiting test results [24] • Recognized as gold standard for regulatory acceptance | • Requires samples from multiple independent production lots [24] • Higher initial resource investment • Requires periodic dose audits to maintain validation status [24] |
| Single Laboratory Validation | • Ideal for new products with no immediate plans for future production [24] • Lower initial test costs if ongoing production not needed [24] • Costs can be spread over time [24] • No dose audits until full validation achieved [24] | • Results apply only to the specific lot tested [24] • Each new lot requires separate validation before release [24] • Potentially higher total cost if multiple lots produced over time [24] • Limited recognition for regulatory submissions |
Experimental Protocols and Methodologies
Single Laboratory Validation Protocol
SLV requires systematic assessment of multiple method performance characteristics to establish fitness for purpose. The specific characteristics evaluated depend on the method type and intended application, but typically include:
Selectivity/Specificity: Demonstrate the method's ability to measure the analyte accurately in the presence of potential interferents. This involves testing samples with and without interferents and comparing results [21].
Accuracy/Trueness: Assess through spike/recovery experiments using certified reference materials (when available) or by comparison with a reference method. Recovery experiments involve fortifying sample matrix with known analyte quantities and measuring the recovery percentage [21] [23].
Precision: Evaluate through repeatability (same analyst, same equipment, short time interval) and within-laboratory reproducibility (different analysts, equipment, days). Precision is typically expressed as standard deviation or coefficient of variation [23].
Linearity and Range: Establish the analytical range where method response is proportional to analyte concentration. Prepare and analyze calibration standards across the anticipated concentration range [21].
Limit of Detection (LOD) and Quantification (LOQ): Determine the lowest analyte concentration detectable and quantifiable with acceptable precision. Based on signal-to-noise ratio or statistical evaluation of blank samples [21].
Measurement Uncertainty: For medical laboratories, the SLV approach combines random uncertainty (from Internal Quality Control data) and systematic uncertainty (from bias estimation) using the formula: Combined uncertainty = √(random uncertainty² + systematic uncertainty²) [23].
Full Validation Protocol
Full validation through collaborative trials follows internationally standardized protocols:
Method Comparison Study: Initially validates the method against a reference method in one laboratory [22].
Interlaboratory Study: Multiple laboratories (minimum number specified by relevant protocol) analyze identical test materials using the standardized method protocol. ISO 16140-2 specifies separate protocols for qualitative and quantitative microbiological methods [22].
Statistical Analysis: Results from participating laboratories are collected and statistically analyzed to determine method performance characteristics including reproducibility, repeatability, and trueness [21] [22].
Certification Process: Data generated can serve as a basis for certification of alternative methods by independent organizations [22].
For sterilization validation, full validation requires bioburden testing from three different production lots, bioburden recovery efficiency validation, bacteriostasis/fungistasis testing, and sterility tests at the verification dose [24].
Decision Framework for Validation Strategy
The following diagram illustrates the decision-making process for selecting between SLV and full validation:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method validation requires specific materials and reagents tailored to the analytical methodology. The following table outlines essential categories and their functions:
Table 3: Essential Research Reagent Solutions for Method Validation
| Reagent/Material | Function in Validation | Application Examples |
|---|---|---|
| Certified Reference Materials (CRMs) | Establish trueness through analysis of materials with certified analyte concentrations [21] | Quantifying method bias, establishing measurement traceability |
| Reference Methods | Provide comparator for evaluating accuracy of new or alternative methods [21] [22] | Method comparison studies as required by ISO 16140 series |
| Selective Culture Media | Validate method selectivity and specificity in microbiological analyses [22] | Confirmation procedures, identification methods validation |
| Internal Quality Control (IQC) Materials | Monitor method precision and stability over time [23] | Determining within-laboratory reproducibility, random uncertainty |
| Proficiency Testing Samples | Assess laboratory performance relative to peers and estimate systematic uncertainty [23] | External quality assessment (EQA), bias estimation |
Implementation in Regulated Environments
Regulatory Framework and Standards
Method validation operates within a comprehensive framework of international standards and regulatory requirements:
ISO Standards: The ISO 16140 series provides detailed protocols for microbiological method validation, with Part 2 covering alternative method validation, Part 3 addressing verification in user laboratories, and Part 4 covering single-laboratory validation [22].
IUPAC/AOAC Guidelines: Provide harmonized protocols for method validation across chemical and biological disciplines, including the Statistics Manual of AOAC INTERNATIONAL with guidance on single laboratory studies [21].
ICH Guidelines: Prescribe minimum validation requirements for tests supporting drug approval submissions, particularly for pharmaceutical applications [21].
Verification of Validated Methods
For laboratories implementing previously validated methods, verification demonstrates the laboratory can satisfactorily perform the method. ISO 16140-3 outlines a two-stage process: implementation verification (testing one item from the validation study) and item verification (testing challenging items within the laboratory's scope) [22].
Selecting between Single Laboratory Validation and Full Validation represents a critical strategic decision in method development and implementation. SLV provides a practical approach for methods with limited application scope, offering flexibility and reduced initial resource commitment. Full Validation, while requiring greater initial investment, provides broader recognition and suitability for methods intended for widespread or regulatory use.
The decision framework presented enables researchers and drug development professionals to make informed choices based on method application, regulatory requirements, and available resources. As regulatory expectations continue to evolve, understanding the scope, limitations, and appropriate application of each validation approach remains fundamental to producing reliable analytical data in pharmaceutical research and development.
Executing SLV: A Step-by-Step Protocol for Laboratory Scientists
Single-laboratory validation (SLV) represents a critical process where a laboratory independently establishes, through documented studies, that the performance characteristics of an analytical method are suitable for its intended application. Within a broader thesis on the fundamentals of SLV research, this foundational step ensures that a method provides reliable, accurate, and reproducible data before it is put into routine use or considered for a full inter-laboratory collaborative study. SLV serves as the bedrock of data integrity, providing stakeholders with confidence in the results that drive critical decisions in drug development, quality control, and regulatory submissions [2] [25]. A well-structured SLV protocol, with unambiguous acceptance criteria, is not merely a regulatory formality but a core component of good scientific practice that prevents costly rework and project delays.
The development of a detailed protocol is the most pivotal phase in the SLV process. It transforms the abstract goal of "method validation" into a concrete, executable, and auditable plan. This document precisely defines the scope, objectives, and experimental design, ensuring that all studies are performed consistently and that the resulting data can be evaluated against pre-defined standards of acceptability [2] [26]. In the context of a validation lifecycle, a robust SLV protocol directly supports future method transfers and continuous improvement initiatives, embedding quality at the very foundation of the analytical method [2].
Core Components of an SLV Protocol
A comprehensive SLV protocol is a multi-faceted document that meticulously outlines every aspect of the validation study. Its primary function is to eliminate ambiguity and ensure the study generates data that is both scientifically sound and defensible during audits.
Defining Scope, Objectives, and Applicability
The protocol must begin with a clear statement of purpose. This section defines the analyte of interest, the sample matrices (e.g., active pharmaceutical ingredient, finished drug product, biological fluid), and the intended use of the method (e.g., stability testing, release testing, impurity profiling) [26]. The objectives should be Specific, Measurable, Achievable, Relevant, and Time-bound (SMART). For instance, an objective may be, "To validate a reverse-phase HPLC-UV method for the quantification of Active X in 50 mg tablets over a range of 50% to 150% of the nominal concentration, demonstrating accuracy within 98-102% and precision with an RSD of ≤2.0%."
Detailed Experimental Design
This section is the operational core of the protocol. It provides a step-by-step guide for the experimental work, ensuring consistency and reproducibility. Key elements include:
- Sample Preparation: Detailed procedures for preparing standards, blanks, and quality control (QC) samples at various concentration levels, including the specific solvents, dilution schemes, and stabilization techniques to be used [2].
- Instrumentation and Conditions: A complete description of the analytical instrument (e.g., HPLC, GC) and its configuration, including column type, mobile phase composition, flow rate, temperature, and detection settings [27].
- Number of Replicates and Runs: The protocol must specify the number of replicates for each validation parameter (e.g., a minimum of six replicates at one concentration level for precision) and whether intermediate precision will involve different analysts, instruments, or days [2] [25].
Defining Validation Parameters and Acceptance Criteria
This component explicitly lists the performance characteristics to be evaluated and the quantitative standards for judging their acceptability. These parameters form the basis for the scientific assessment of the method's fitness for purpose. The subsequent section of this guide provides a detailed breakdown of these parameters and their typical acceptance criteria.
Documentation and Data Analysis Procedures
The protocol must specify the format for raw data collection (e.g., electronic lab notebooks, chromatographic data systems) and the statistical methods that will be used to calculate results like mean, standard deviation, %RSD, and regression coefficients [2] [26]. Adherence to ALCOA++ principles (Attributable, Legible, Contemporaneous, Original, Accurate, plus Complete, Consistent, Enduring, and Available) for data integrity is paramount [28].
The following workflow diagram illustrates the logical sequence and key decision points in developing and executing an SLV protocol.
SLV Protocol Development and Execution Workflow
Validation Parameters and Acceptance Criteria
The following table summarizes the core validation parameters, their definitions, common experimental methodologies, and examples of scientifically rigorous acceptance criteria for a pharmaceutical SLV.
Table 1: Core Validation Parameters and Acceptance Criteria for SLV
| Parameter | Definition & Purpose | Recommended Experimental Methodology | Example Acceptance Criteria |
|---|---|---|---|
| Specificity | Ability to unequivocally assess the analyte in the presence of potential interferents (e.g., impurities, matrix). | Compare chromatograms of blank matrix, placebo, standard, and stressed samples (e.g., heat, light, acid/base) [2]. | Baseline separation of analyte peak from all potential interferents; Peak purity index ≥ 990. |
| Accuracy | Closeness of agreement between the measured value and a reference value. | Spike and recovery: Fortify blank matrix with known analyte concentrations (e.g., 3 levels, 3 replicates each) [2]. | Mean recovery of 98–102%; RSD ≤ 2% at each level. |
| Precision | Degree of scatter among a series of measurements. Includes repeatability and intermediate precision. | Analyze multiple preparations (n=6) of a homogeneous sample at 100% concentration. Repeat on different days/analysts [2]. | Repeatability: RSD ≤ 2%. Intermediate Precision: RSD ≤ 2.5% and no significant statistical difference between days/analysts. |
| Linearity | Ability of the method to produce results directly proportional to analyte concentration. | Prepare a minimum of 5 concentration levels across the stated range (e.g., 50%, 75%, 100%, 125%, 150%) [2]. | Correlation coefficient (r) ≥ 0.998; y-intercept not significantly different from zero. |
| Range | The interval between the upper and lower concentration levels for which accuracy, precision, and linearity are established. | Defined by the linearity and accuracy studies. | The range over which linearity, accuracy, and precision meet all acceptance criteria. |
| LOD / LOQ | Limit of Detection (lowest detectable level) and Limit of Quantification (lowest quantifiable level). | Signal-to-Noise ratio of 3:1 for LOD and 10:1 for LOQ, confirmed by experimental analysis [2]. | LOD/LOQ concentrations confirmed by analysis with accuracy of 80-120% and precision of RSD ≤ 10% for LOQ. |
| Robustness | Capacity to remain unaffected by small, deliberate variations in method parameters. | Deliberately alter a single parameter (e.g., flow rate ±0.1 mL/min, temperature ±2°C, pH ±0.1 units) [2]. | System suitability criteria are met for all variations; No significant impact on key results (e.g., retention time, resolution). |
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of an SLV is contingent on the quality of the materials used. The following table details key reagents and consumables that are essential for executing a robust validation study, particularly in chromatographic analysis.
Table 2: Essential Research Reagents and Materials for SLV
| Item | Function in SLV | Critical Considerations |
|---|---|---|
| Certified Reference Standards | Serves as the benchmark for quantifying the analyte and establishing accuracy. | Must be of known identity, purity, and stability, traceable to a recognized standard body [2]. |
| Chromatography Columns | The heart of the separation system, critical for specificity, efficiency, and robustness. | Multiple lots from the same supplier should be screened to assess performance consistency [2]. |
| High-Purity Solvents & Reagents | Used for mobile phase, sample, and standard preparation. | Grade appropriate for the technique (e.g., HPLC-grade) to minimize baseline noise and ghost peaks [27]. |
| Blank Matrix | The analyte-free sample material used for preparing calibration standards and QCs. | Must be representative and confirmed to be free of interference at the analyte's retention time [26]. |
| System Suitability Test (SST) Mixture | A test mixture used to verify that the total chromatographic system is fit for purpose before analysis. | Typically contains the analyte and key impurities to measure critical parameters like plate count, tailing factor, and resolution [27]. |
Advanced Strategy: Design of Experiments for Robustness Testing
For seasoned professionals, moving beyond the traditional one-factor-at-a-time (OFAT) approach to robustness testing is a key strategy for deepening method understanding. Design of Experiments (DoE) is a structured, statistical approach that allows for the efficient evaluation of multiple method parameters and their interactions simultaneously [2].
A typical DoE for robustness might investigate three factors—such as mobile phase pH, column temperature, and percent organic solvent—each at two levels (high and low). This would constitute a 2^3 full factorial design, requiring only 8 experiments to not only evaluate the main effect of each factor but also all two-factor and the three-factor interactions. This is far more efficient and informative than an OFAT approach. The data generated can be used to create a mathematical model of the method's behavior, identifying which parameters have a significant effect on the results and defining a method operable design region (MODR)—a combination of parameter ranges within which the method will perform as specified. The relationship between DoE factors and the resulting model can be visualized as follows:
DoE Approach to Robustness Testing
Common Pitfalls and Mitigation Strategies in SLV Planning
Even with a protocol in place, several common pitfalls can compromise an SLV study. Proactive planning is required to avoid them.
- Pitfall 1: Incomplete Test Matrix. An undersized experimental design fails to adequately challenge the method across its entire range and against all potential variables [25].
- Pitfall 2: Undefined Revalidation Triggers. A method is considered "validated forever," leading to its use under changed conditions without an assessment of impact [2].
- Mitigation: Document clear change-control thresholds in the method SOP. Define the specific changes (e.g., new reagent lot, instrument model, sample matrix) that will trigger a partial or full revalidation [2].
- Pitfall 3: Ignoring System Suitability Test (SST) Failures. Proceeding with analysis despite an SST failure invalidates the subsequent data and indicates a poorly understood or controlled system [25].
- Pitfall 4: Skipping Matrix Effect Testing. Validating a method only in a simple solvent and then applying it to a complex, real-world sample matrix can lead to inaccuracy due to suppression or enhancement effects [25].
A meticulously developed SLV protocol, with its clear acceptance criteria, is not the end of the planning process but the beginning of a method's validated lifecycle. It is the foundational document that ensures scientific rigor, regulatory compliance, and operational efficiency. By investing the necessary effort in pre-validation planning—encompassing a thorough definition of parameters, a well-designed experimental strategy, and the use of high-quality materials—research scientists and drug development professionals can establish a robust foundation for generating reliable analytical data. This disciplined approach ensures that methods are not only "fit-for-purpose" at the outset but also remain so throughout their operational life, thereby solidifying the integrity of the entire drug development pipeline.
In the context of Single-Laboratory Validation (SLV), understanding and quantifying uncertainty is fundamental to demonstrating the reliability of analytical methods. SLV acts as a comprehensive assessment of the entire analytical system, evaluating all potential influences on the final result. This approach is particularly valuable for laboratories developing and validating methods for in-house use, forming the core of a research thesis focused on establishing robust, defensible, and fit-for-purpose analytical procedures. A properly executed SLV reduces the likelihood of underestimating measurement uncertainty in the final budget by incorporating data from routine quality management activities [23].
The SLV framework calculates uncertainty for the analytical procedure itself, which is then assigned to individual sample results. This assignment is valid provided the sample's measured value is not too different (within 2-3 times) from the values used to determine the uncertainty, a criterion generally met in medical laboratories where data falls within the clinically relevant range [23]. This guide outlines a practical framework for assessing the two primary components of uncertainty—random and systematic—within a single-laboratory setting.
Theoretical Foundation: Systematic and Random Uncertainty
Uncertainty in analytical measurement arises from multiple potential sources, which can be categorized as either random or systematic. The SLV approach is designed to capture both types of influences within a single, combined uncertainty estimate [23].
Random Uncertainty: This component arises from unpredictable, stochastic variations in the measurement process. It is quantified through within-laboratory reproducibility, typically assessed using Internal Quality Control (IQC) data recorded over a prolonged period. This data incorporates changes in operator, days, and reagent batches, but is performed using the same analytical method, thus covering the entire analytical process. Random uncertainty is expressed as either the Standard Deviation (SD) or Coefficient of Variation (CV%), depending on whether an absolute or relative uncertainty is required [23].
Systematic Uncertainty: This component, often related to bias, represents a consistent, directional deviation of the laboratory's results from the true value. It reflects the uncertainty associated with inaccuracy. Systematic uncertainty can be measured through comparison with reference procedures, analysis of certified reference materials, inter-laboratory comparisons, and spiking experiments. In practice, data from External Quality Assessment (EQA) or proficiency testing schemes is frequently used for this assessment [23].
The two components are combined into an overall combined uncertainty using the root sum of squares method, as defined by the equation: Combined uncertainty = (random uncertainty² + systematic uncertainty²)^1/2 [23].
A Practical Framework for Assessment
Implementing the framework requires a structured, step-by-step approach to separately quantify the random and systematic components before combining them.
Assessing Random Uncertainty
The random uncertainty contribution is derived from the within-laboratory reproducibility data, primarily sourced from Internal Quality Control (IQC).
Experimental Protocol for Random Uncertainty [23]:
- Data Collection: Collect IQC data for a prolonged period (e.g., 3-6 months or more) that encompasses changes in operator, days, and reagent batches.
- Multiple Levels: Use multiple levels of IQC that cover the entire analytical measurement range of the assay.
- Calculate Dispersion: For each QC level, calculate the standard deviation (SD) for absolute uncertainty or the coefficient of variation (CV%) for relative uncertainty. Low concentration levels (near the limit of detection) typically require absolute uncertainties (SD), while higher concentrations benefit from relative uncertainties (CV%).
- Combine Results: Combine the uncertainty from each QC level using the root of the sum of squares: Random uncertainty = ( (QC Level 1)² + (QC Level 2)² ... )^1/2 Here, "QC Level" refers to the SD or CV calculated for that specific level.
Assessing Systematic Uncertainty
The systematic uncertainty originates from the bias of the method. EQA results provide a robust foundation for this assessment.
Experimental Protocol for Systematic Uncertainty using EQA [23]:
- Data Collection: Gather data from successive EQA surveys, focusing on the laboratory's result and the assigned consensus value (mean or median) for a peer group using the same method and reagent.
- Calculate Laboratory Bias: For each EQA sample, calculate the bias: Bias = lab result – consensus result.
- Determine Overall Bias (RMS): Calculate the Root Mean Square (RMS) of the biases from multiple surveys to get a robust estimate of the laboratory's overall bias: RMS = ( (Sum of all biases²) / number of surveys )^1/2.
- Estimate Consensus Value Uncertainty (UCref): Calculate the uncertainty of the consensus value for each survey: U = Sample SD / (number of respondents)^1/2. Then, combine these across multiple surveys: UCref = ( (Sum of U²) / n )^1/2.
- Combine to Get Systematic Uncertainty: Finally, combine the two components to determine the total systematic uncertainty: Systematic uncertainty = (RMS² + UCref²)^1/2.
Combining the Components
The final step is to combine the quantified random and systematic uncertainties into a single combined standard uncertainty using the formula previously mentioned [23]. This combined uncertainty represents the standard uncertainty of the procedure and can be expanded to a desired confidence level (e.g., 95%) by multiplying by a coverage factor (k), typically k=2.
The logical relationship and workflow for assessing these components are visualized in the following diagram.
Key Reagents and Materials for SLV Experiments
The experimental protocols for determining uncertainty rely on specific materials and reagents to ensure the validity of the data produced. The following table details these essential components.
Table 1: Key Research Reagent Solutions for Uncertainty Assessment
| Item Name | Function in Uncertainty Assessment |
|---|---|
| Internal Quality Control (IQC) Materials | Used to monitor daily performance and calculate within-laboratory reproducibility (random uncertainty). They are typically available at multiple concentration levels [23]. |
| Certified Reference Materials (CRMs) | Provide a traceable value and are used to assess method bias, a key component of systematic uncertainty, by comparing the measured value to the certified value [23]. |
| External Quality Assessment (EQA) Samples | Allow a laboratory to compare its performance with a peer group consensus, enabling the calculation of bias and its uncertainty for systematic error estimation [23]. |
| Calibrators | Materials with known assigned values used to establish the analytical measuring scale (calibration curve). Their uncertainty contributes to the overall systematic uncertainty of the method. |
Data Analysis and Performance Standards
Quantifying uncertainty allows a laboratory to judge whether its method's performance is fit for purpose. This involves comparing the estimated total error of the measurement procedure against established Allowable Total Error (ATE) goals or limits [29].
Quantifying Total Error and Setting Goals
Total Analytical Error (TAE) is a key metric that combines the effects of both random (imprecision) and systematic (bias) errors into a single expression. The parametric model for TAE, often used in laboratory quality assessment, is [29]: TAE = |Bias| + z × SD~WL~ Where Bias is the systematic error, SD~WL~ is the within-laboratory imprecision, and z is the z-score for a desired confidence interval (e.g., 1.96 for 95%).
CLSI guideline EP46 differentiates between ATE "goals" (ideal, aspirational performance) and "limits" (minimum acceptable performance). These can be set based on several models [29]:
- Clinical outcome-based models: The impact of the error on clinical decision-making.
- Biological variation data: Based on the inherent within-subject and between-subject biological variation of the analyte.
- Peer-group performance: What is achievable by the majority of laboratories (state-of-the-art).
Table 2: Framework for Setting Analytical Performance Goals
| Basis for Goal Setting | Description | Application in SLV |
|---|---|---|
| Clinical Outcomes | Defines performance based on the impact on medical decisions. The most clinically relevant but often difficult to establish. | The ultimate benchmark for determining if a method is truly "fit-for-purpose." |
| Biological Variation | Uses population-based data on natural biologic fluctuations to set goals for imprecision (CV%), bias (%), and total error. | Provides standardized, evidence-based goals for a wide range of analytes [29]. |
| Regulatory/Proficiency Testing Criteria | Uses performance standards set by regulatory bodies or EQA providers. | Defines the minimum performance required for regulatory compliance. |
| State-of-the-Art | Based on the best performance currently achievable by leading laboratories or technologies. | Useful for evaluating new methods or technologies during development. |
Integrating Sigma Metrics for Quality Assessment
The Sigma metric provides a powerful tool for quantifying process capability in the laboratory. It integrates the ATE goal with the method's observed imprecision and bias [29]: Sigma Metric = (ATE - |Bias|) / CV A higher Sigma value indicates a more robust and reliable method. A Sigma value of 6 represents world-class performance, while a value below 3 is generally considered unacceptable.
Advanced Topics: Lifecycle Management and Best Practices
A method's validation and uncertainty profile are not static. A comprehensive SLV research thesis must address the ongoing lifecycle management of the analytical procedure.
Revalidation and Change Control: A method is not "done" once initially validated. Laboratories must plan for periodic reviews and revalidation triggered by events such as changes in critical reagents, instrumentation, or software. Documenting change-control thresholds in Standard Operating Procedures (SOPs) is essential to safeguard against unexpected performance gaps [2].
Risk Management and Robustness: During method development and validation, robustness testing should be conducted. This involves deliberately introducing small, deliberate changes to operational parameters (e.g., pH ±0.2 units, temperature ±5°C) to evaluate the method's susceptibility to variation. This practice helps build a method that is less prone to high uncertainty in routine use [2].
Comprehensive Documentation: Meticulous documentation is the foundation of a defensible SLV. The workflow should include a Validation Plan & Protocol, a detailed Standard Operating Procedure (SOP), raw data collection, statistical analysis, and a final Validation Report signed off by relevant stakeholders [2]. This documentation forms the core evidence for any research thesis on the topic.
Utilizing Internal Quality Control (IQC) and EQA Data for Robustness and Reproducibility
In the framework of single-laboratory method validation (SLV), the strategic integration of Internal Quality Control (IQC) and External Quality Assessment (EQA) data transcends its traditional role of compliance monitoring to become a powerful source of evidence for a method's fundamental robustness and long-term reproducibility. This technical guide provides researchers and drug development professionals with advanced protocols to transform raw quality control data into quantitative, defensible metrics—such as Sigma-metrics and Total Error—that objectively demonstrate analytical method performance. By implementing the detailed methodologies herein, laboratories can build a compelling data-driven case for their methods' reliability, even within a single-laboratory setting, thereby fostering greater confidence in research outcomes and regulatory submissions.
In single-laboratory method validation (SLV), the terms robustness and reproducibility carry specific, critical meanings. Robustness refers to the capacity of an analytical method to remain unaffected by small, deliberate variations in method parameters, indicating its reliability during normal usage. Reproducibility, in the context of SLV, is demonstrated by the method's ability to produce precise and consistent results over an extended period under various routine conditions, such as different operators, instruments, and reagent lots.
While initial method validation provides a snapshot of performance under controlled conditions, the true test of a method's value is its sustained performance. A 2025 study on blood gas analyzers highlights that intelligent quality management systems, which leverage ongoing IQC data, can significantly improve both the precision and accuracy of analytical methods over time compared to traditional QC approaches [30]. This longitudinal performance data is the bedrock of demonstrating reproducibility.
The synergy between IQC and EQA creates a powerful feedback loop for continuous method verification. IQC provides high-frequency, internal data to monitor daily stability, while EQA offers an external, unbiased assessment of a method's accuracy against peer laboratories or reference materials. The 2025 IFCC recommendations underscore that laboratories must establish a structured approach for planning IQC procedures, including the frequency of assessments and the definition of acceptability criteria, all within the framework of the method's intended use [31].
Fundamentals of IQC and EQA
Internal Quality Control (IQC): The First Line of Defense
IQC involves the routine analysis of stable control materials alongside patient or test samples to verify that an analytical procedure is performing within pre-defined limits. Its primary function is to monitor the ongoing validity of examination results, providing assurance that the output is correct and fit for its clinical or research purpose [32]. A robust IQC system is not merely about running controls; it is about implementing a statistical process control (SPC) strategy. This typically involves:
- Levey-Jennings Control Charts: Graphical tools that plot control values over time against the method's established mean and standard deviation (SD).
- Westgard Multi-Rules: A set of statistical rules (e.g., 1
2s, 13s, 22s, R4s) used to detect both random and systematic errors, thereby reducing the probability of false rejections while maintaining high error detection [32].
The core objective is to distinguish between inherent, random variation (noise) and significant systematic shifts (bias) or increases in imprecision that could invalidate test results.
External Quality Assessment (EQA): The Objective Benchmark
EQA, also known as proficiency testing, involves the blind analysis of samples provided by an external scheme organizer. The results are then compared against a target value, which may be derived from a reference method or a consensus of participating laboratories. EQA provides an independent check on a laboratory's analytical accuracy and is a mandatory requirement for accreditation under standards like ISO/IEC 17025 and ISO 15189 [32].
The quantitative data from EQA is crucial for calculating bias—a core component of measurement uncertainty and total error calculations. By participating in EQA, a laboratory can verify that its method is not only precise but also accurate when compared to an external standard.
The Integrated QA Framework
The relationship between IQC, EQA, and the overall quality system is synergistic. IQC is the daily, ongoing monitor, while EQA provides periodic, external validation. Findings from EQA can inform adjustments to IQC limits and procedures, while trends in IQC can predict and prevent future EQA failures. This integrated system forms the laboratory's Quality Assurance and Improvement Program (QAIP) [33].
The following workflow diagram illustrates how IQC and EQA data integrate within a continuous quality improvement cycle:
Experimental Protocols for Data Utilization
Protocol 1: Calculating Sigma-Metrics for Performance Assessment
Objective: To quantify the analytical performance of a method using a Sigma-metric, which provides a universal scale for assessing robustness.
Methodology:
- Determine Allowable Total Error (TEa): Source the TEa from regulatory or clinical guidelines (e.g., CLIA'88, Rilibak, or biological variation databases) [30]. This is the maximum error clinically or analytically allowable.
- Calculate Bias from EQA: Use data from at least two EQA cycles. For each cycle, calculate the percentage bias:
Bias (%) = [(Lab Result - Target Value) / Target Value] * 100. Use the average absolute bias for the Sigma calculation. - Determine Imprecision from IQC: Using a minimum of 20 data points from a stable period of IQC data at a medically relevant concentration, calculate the standard deviation (SD) and then the coefficient of variation (CV%):
CV% = (SD / Mean) * 100. - Calculate Sigma: Use the formula:
Sigma = (TEa - |Bias|) / CV%.
Interpretation: A Sigma value of 6 represents world-class performance, 4 is good, and below 3 is considered poor and requires substantial improvement [30].
Protocol 2: Estimating Total Error (TE)
Objective: To provide a single value that combines random error (imprecision) and systematic error (bias), offering a complete picture of a method's accuracy.
Methodology:
- Gather Components: Use the same Bias and Imprecision (as SD) values calculated in Protocol 1.
- Calculate Total Error: Apply the formula:
TE = |Bias| + 2 * SD[30]. - Compare to Specification: The estimated TE should be compared to the allowable TEa. A method is generally considered acceptable if its estimated TE is less than the allowable TEa.
Protocol 3: Evaluating QC Performance (Pfr, Ped, ADT)
Objective: To statistically evaluate the effectiveness of the chosen IQC rules and frequency.
Methodology (based on 2025 research):
- Probability of False Rejection (Pfr): The likelihood that a stable analytical process will trigger a QC rejection rule. This is calculated based on the control limits and rules used (e.g., a 1
2srule has a high Pfr) [30]. - Probability of Error Detection (Ped): The likelihood that the QC system will detect a critical systematic or random error. A higher Ped is desirable. It is calculated as:
Ped = cumulative normal standard distribution (z = sigma - DL - 1.65), where DL is the control limit [30]. - Average Detection Time (ADT): The average number of samples or time units processed before an out-of-control condition is detected. A shorter ADT is better. It is derived from the Overall Average Run Length (ARL):
ADT = ARL × sampling time[30].
A 2025 comparative study of blood gas analyzers demonstrated that intelligent QC modes could achieve a higher Ped and a lower ADT for most parameters compared to traditional QC, leading to faster error detection and improved quality management [30].
Data Analysis and Performance Metrics
The quantitative data derived from the protocols above provides an objective foundation for claims of robustness and reproducibility. The following table summarizes key performance metrics from a 2025 study comparing traditional and intelligent QC for blood gas analysis, illustrating how these metrics are applied in practice [30].
Table 1: Performance Metrics for Blood Gas Analysis (BGA): Traditional vs. Intelligent QC (Adapted from [30])
| Analyte | QC Mode | Bias (%) | CV% | Sigma (σ) | TE | Ped | ADT |
|---|---|---|---|---|---|---|---|
| pH | Traditional | -0.03 | 0.36 | 5.5 | 0.75 | 0.45 | 2.22 |
| Intelligent | -0.02 | 0.28 | 6.8 | 0.58 | 0.62 | 1.61 | |
| pCO₂ | Traditional | 1.15 | 2.10 | 3.3 | 5.35 | 0.31 | 3.23 |
| Intelligent | 0.85 | 1.65 | 4.3 | 4.15 | 0.52 | 1.92 | |
| Na+ | Traditional | 0.51 | 0.89 | 3.9 | 2.29 | 0.41 | 2.44 |
| Intelligent | 0.42 | 1.05 | 3.4 | 2.52 | 0.35 | 2.86 |
Abbreviations: CV%: Coefficient of Variation; TE: Total Error; Ped: Probability of Error Detection; ADT: Average Detection Time.
Analysis of Table 1: The data clearly shows that for most parameters (pH, pCO₂), the intelligent QC system yielded superior performance: lower bias, lower imprecision (CV%), higher Sigma-metrics, lower Total Error, a higher probability of detecting errors (Ped), and a faster average time to detection (ADT). This provides quantitative, data-driven evidence for the enhanced robustness offered by the intelligent QC system. For sodium (Na+), the intelligent system showed slightly worse imprecision, leading to a lower Sigma value, which highlights the importance of method-specific optimization.
The Scientist's Toolkit: Essential Research Reagent Solutions
The validity of IQC and EQA data is contingent on the quality of the materials used. The following table details key reagents and their functions in a robust quality control system.
Table 2: Key Research Reagent Solutions for Quality Control
| Reagent/Material | Function & Importance in QC |
|---|---|
| Third-Party Control Materials (Liquid, Assayed/Unassayed) | Provides an independent verification of analyzer performance, unbiased by manufacturer-calibrated values. Essential for detecting calibration drift [34]. |
| Process Control Solutions (PCS) | Used in intelligent QC systems (e.g., iQM2) for continuous, real-time monitoring of the analytical process. They help detect errors within the analysis cycle that might be missed by periodic QC [30]. |
| Certified Reference Standards (e.g., USP standards) | Provides the highest order of traceability and accuracy for method validation and for assigning target values to in-house control materials. Critical for establishing method correctness [35]. |
| Matrix-Matched Control Materials | Controls formulated to mimic the patient sample matrix (e.g., serum, whole blood). They ensure that the QC process accurately challenges the entire analytical system, including pre-treatment steps. |
Advanced Integration for Enhanced Reproducibility
The Risk-Based Approach to IQC Frequency
The 2025 IFCC recommendations advocate for a risk-based approach to determining IQC frequency, moving beyond a one-size-fits-all model. The frequency of IQC and the number of patient samples between QC events (run size) should be determined by [31]:
- The Sigma level of the assay.
- The clinical criticality of the analyte.
- The feasibility of re-analyzing samples (e.g., short stability of blood gas samples).
- The time frame for result release.
This approach ensures that resources are focused on methods with higher risk of failure, thereby directly enhancing the reproducibility of critical results.
Measurement Uncertainty (MU) from IQC and EQA
The ISO 15189:2022 standard requires laboratories to evaluate measurement uncertainty (MU) where relevant [31]. A practical "top-down" approach uses existing IQC and EQA data:
- IQC data is used to estimate the imprecision component of MU.
- EQA data is used to estimate the bias component of MU.
By combining these, a laboratory can calculate an uncertainty budget that provides an interval within which the true value of a measured quantity is expected to lie. This is a powerful, data-driven statement about the method's reliability.
The Method Validation and Monitoring Workflow
The entire process, from initial validation to ongoing monitoring of robustness and reproducibility, can be summarized in the following workflow:
In the realm of single-laboratory method validation, the systematic utilization of IQC and EQA data moves the narrative from simple compliance to one of demonstrable scientific rigor. By implementing the protocols outlined in this guide—calculating Sigma-metrics, estimating Total Error, and evaluating QC performance—researchers can generate quantitative, defensible evidence of their method's robustness and long-term reproducibility. This data-driven approach, integrated within a risk-based framework as recommended by the latest international standards, not only strengthens the credibility of research and development data but also builds a foundation of trust for regulatory submissions and ultimately, patient safety in drug development.
Within the framework of single-laboratory method validation (SLV), the comparison of methods experiment stands as a cornerstone practice for estimating the inaccuracy of a new measurement procedure. This process involves comparing results from a candidate method against those from a reference or established comparative method using clinically relevant patient specimens. The fundamental objective is to identify and quantify systematic errors or biases that could impact clinical decision-making, thereby ensuring that the new method provides results that are reliable and fit for their intended diagnostic purpose [10].
Method validation, as a comprehensive process, proves that an analytical method is acceptable for its intended use, assessing parameters such as accuracy, precision, and specificity [10]. In the context of SLV, where a laboratory often verifies that a previously validated method performs as expected in its specific environment, the comparison of methods experiment provides critical evidence of analytical accuracy under real-world conditions [10]. This guide details the experimental protocols, data analysis techniques, and practical considerations for successfully executing this essential validation component.
Theoretical Foundations and Definitions
Key Concepts in Method Comparison
- Inaccuracy: The systematic deviation between the measurement results obtained by the candidate method and the true value or an accepted reference value. It represents the total systematic error of a measurement procedure.
- Systematic Error (Bias): A consistent, directional difference between the candidate method and the comparative method across the measuring interval.
- Patient Specimens: Authentic clinical samples used for method comparison, which preserve the matrix effects and interferences encountered in routine practice, unlike processed quality control materials.
- Single-Laboratory Validation (SLV): The process whereby a laboratory establishes, through extensive testing, that the performance characteristics of a method meet the specified requirements for its intended analytical application [10].
Distinction Between Method Validation and Verification
It is crucial to distinguish between method validation and method verification, as their requirements for comparison studies differ. Method validation is a comprehensive process conducted to prove a new method is fit-for-purpose, requiring a full comparison of methods experiment to establish accuracy [10]. Conversely, method verification confirms that a previously validated method performs satisfactorily in a user's laboratory, often involving a more limited comparison to ensure performance matches established claims [10]. The comparison of methods experiment described herein is structured for a full validation context.
Experimental Design and Protocol
Specimen Selection and Preparation
The integrity of the comparison experiment hinges on appropriate specimen selection. The following table outlines the key considerations:
Table 1: Specimen Selection Criteria for Method Comparison
| Criterion | Detailed Requirement | Rationale |
|---|---|---|
| Number | Minimum of 40 patient specimens, though 100+ provides more reliable estimates. | Ensures sufficient statistical power to detect clinically significant biases. |
| Concentration Range | Should cover the entire medically relevant reportable range. | Allows evaluation of constant and proportional biases across all potential clinical values. |
| Distribution | Approximately 50% of samples should have values outside the reference interval. | Ensures adequate representation of abnormal values, which are critical for clinical diagnosis. |
| Matrix | Use only authentic human patient specimens (serum, plasma, urine, etc.). | Preserves protein interactions, drug metabolites, and other matrix effects that can affect accuracy. |
| Stability | Analyze specimens within their known stability period; avoid repeated freeze-thaw cycles. | Preforms artifactural results due to sample degradation. |
The Core Experimental Workflow
The following diagram illustrates the logical workflow for executing a comparison of methods experiment, from initial planning through to final decision-making.
Execution Protocol
- Instrument Calibration: Ensure both the candidate and comparative methods are properly calibrated according to manufacturer specifications prior to analysis.
- Sample Analysis: Analyze all selected patient specimens in duplicate on both the candidate and comparative methods. The order of analysis should be randomized to minimize the effects of instrument drift and sample deterioration over time.
- Data Collection: Record all results in a structured format, ensuring that each patient specimen has a paired result from both methods. Any analytical repeats or outliers should be flagged and documented.
Data Analysis and Interpretation
Statistical Techniques for Estimating Inaccuracy
The primary statistical tools for analyzing method comparison data are regression analysis and difference plotting (Bland-Altman). The following table summarizes the core quantitative measures and their interpretation.
Table 2: Key Statistical Metrics for Estimating Inaccuracy
| Metric | Calculation / Method | Interpretation |
|---|---|---|
| Passing-Bablok Regression | Non-parametric method that is robust to outliers and non-normal data distribution. | The intercept (a) indicates constant bias. The slope (b) indicates proportional bias. |
| Bland-Altman Plot | Plots the difference between methods against the average of both methods for each specimen. | Visualizes the average bias (systematic error) and the limits of agreement (random error). |
| Average Bias | Mean of (Candidate Result - Comparative Result) for all specimens. | A single value estimate of the overall systematic error between the two methods. |
| Correlation Coefficient (r) | Measures the strength of the linear relationship between the two methods. | A high r-value (>0.975) suggests good agreement, but is insufficient alone as it can mask systematic bias. |
Advanced Data Visualization
Creating a combined visualization of the regression and difference plot provides a comprehensive view of the method's performance. The DOT script below can be adapted to represent the final analytical output.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful execution of a comparison of methods experiment relies on a suite of essential materials and reagents. The following table details these key items and their critical functions in the experimental process.
Table 3: Key Research Reagent Solutions and Essential Materials
| Item / Reagent | Critical Function in the Experiment |
|---|---|
| Certified Reference Materials (CRMs) | Used for preliminary calibration verification of both methods to ensure they are operating on a traceable scale before patient sample analysis. |
| Pooled Human Serum/Plasma | Serves as a commutable matrix for preparing quality control samples analyzed throughout the experiment to monitor analytical stability and precision. |
| Stabilized Patient Pools | Retain the complex matrix of real patient samples and are used to assess long-term method reproducibility and sample-specific interferences. |
| Interference Test Kit | Contains solutions of common interferents (e.g., bilirubin, hemoglobin, lipids) to systematically evaluate the susceptibility of the candidate method. |
| Matrix-Specific Diluents | Essential for protocols requiring sample dilution to ensure linearity and to avoid introducing dilution-related bias that is non-commutable. |
| Calibrators Traceable to Higher-Order Standards | Provide the foundational metrological traceability chain, ensuring that the magnitude of any observed bias can be accurately assessed. |
Common Pitfalls and Mitigation Strategies
A significant proportion of laboratory errors originate in the pre-analytical phase, with studies indicating that 61.9% to 68.2% of all laboratory errors occur before analysis begins, often outside the direct control of the laboratory [36]. These pre-analytical pitfalls directly threaten the integrity of a method comparison study.
- Specimen Misidentification and Mislabeling: A mislabeled specimen creates a fundamental data pair mismatch, rendering that data point invalid and potentially skewing statistical results. Such errors are a common pre-analytical error and are often under-reported [37]. Mitigation: Implement strict protocols for labeling specimens at the time of collection using at least two patient identifiers. Barcoding systems, while helpful, are not foolproof and must be part of a broader quality system [38].
- Poor Specimen Integrity: Errors such as improper collection technique, delayed transport, or improper storage can alter analyte concentration or introduce interferences [36]. For example, delayed transport of microbiology specimens can lead to overgrowth of bacteria, while improper storage can cause degradation [36]. Mitigation: Standardize all collection and handling procedures. Ensure rapid transport and processing, and document any deviations from protocol, excluding affected specimens from the analysis.
- Inadequate Specimen Volume and Stability: Using an insufficient number of patient specimens or a narrow concentration range can lead to statistically underpowered studies that fail to detect clinically significant biases. Mitigation: Adhere to the minimum recommendation of 40 specimens, with a target of over 100, and ensure the concentration range covers the entire clinical reportable range, including pathological levels.
Integrating Findings into the Broader SLV Framework
The comparison of methods experiment does not exist in isolation. Its findings must be integrated with other validation parameters to form a complete picture of method performance. The systematic error (bias) estimated from this experiment should be combined with the random error (imprecision) estimated from a replication experiment to determine the method's total analytical error (TAE). This TAE is then compared against predefined, clinically allowable total error limits to make the final judgment on the method's acceptability.
Furthermore, the results inform other aspects of the SLV. Evidence of significant proportional bias may necessitate adjustments to the calibration process. Observed outliers might indicate susceptibility to specific interferences, warranting a dedicated interference study. Ultimately, the comparison of methods experiment provides the critical inaccuracy data required for the objective, evidence-based decision to implement a new method in a clinical laboratory setting, ensuring the safety and efficacy of patient diagnostics.
This guide provides a structured framework for researchers and scientists to compile a comprehensive, audit-ready validation report for single-laboratory validated (SLV) analytical methods. Adherence to this structure ensures regulatory compliance, demonstrates scientific rigor, and instills confidence in your method's reliability.
The Analytical Method Validation Blueprint
Analytical method validation is the process of proving that a testing method is accurate, consistent, and reliable under various conditions [39]. It confirms that the method works for every batch, formulation, and analyst, much like ensuring a recipe turns out perfectly regardless of who bakes it or which oven they use [39].
For a single laboratory, creating a validation report that is "audit-ready" means it is structured to allow a regulator or auditor to easily confirm that the method has been validated in accordance with accepted global standards, primarily the ICH Q2(R2) guideline [39]. The report is the definitive record of this process, proving your method is fit for purpose.
Core Components of an Audit-Ready Validation Report
An audit-ready report must systematically address all key validation criteria as defined by ICH Q2(R2). The following table summarizes these essential elements and their reporting requirements.
Table 1: Essential Validation Criteria and Reporting Requirements per ICH Q2(R2)
| Validation Criterion | Objective | Key Data to Report | Typical Acceptance Criteria |
|---|---|---|---|
| Specificity/Selectivity | Demonstrate the method can accurately distinguish the target analyte from other components [39]. | Chromatograms or spectra of blank, placebo, and standard; description of resolution from potential interferents. | No interference observed at the retention time of the analyte. |
| Linearity | Demonstrate the method's response is proportional to the analyte's concentration [39]. | Calibration curve data (concentration vs. response); correlation coefficient (R²); y-intercept and slope. | R² ≥ 0.99 (or as justified for the method). |
| Range | The interval between the upper and lower concentrations for which linearity, accuracy, and precision have been established. | Justification based on the intended use of the method (e.g., 70%-130% of test concentration). | Meets accuracy and precision criteria across the entire range. |
| Accuracy | Measure the closeness of test results to the true value [39]. | % Recovery for spiked samples; comparison of mean result to true value. | Recovery of 98–102% (or as justified for the analyte level). |
| Precision | Repeatability:Precision under the same operating conditions [39].Intermediate Precision:Precision within-laboratory variations (different days, analysts, equipment) [39]. | % Relative Standard Deviation (%RSD) for multiple measurements of a homogeneous sample. | %RSD < 2.0% (or as justified for the method). |
| Limit of Detection (LOD) | The lowest amount of analyte that can be detected [39]. | Signal-to-noise ratio (e.g., 3:1) or based on standard deviation of the response. | Signal-to-noise ratio ≥ 3:1. |
| Limit of Quantification (LOQ) | The lowest amount of analyte that can be quantified with acceptable accuracy and precision [39]. | Signal-to-noise ratio (e.g., 10:1) or based on standard deviation of the response; supported by accuracy/precision data at LOQ. | Signal-to-noise ratio ≥ 10:1; Accuracy and Precision meet criteria. |
| Robustness | Measure the method's capacity to remain unaffected by small, deliberate variations in method parameters [39]. | Data showing the impact of varied parameters (e.g., pH, temperature, flow rate) on results (e.g., %RSD, retention time). | The method remains specific, accurate, and precise under all varied conditions. |
Experimental Protocols for Key Validation Experiments
Protocol for Establishing Accuracy and Precision
This protocol is designed to generate the quantitative data required for the Accuracy and Precision sections of the validation report.
- Sample Preparation: Prepare a minimum of three concentration levels (e.g., 80%, 100%, 120% of the target concentration), each in triplicate [39].
- Analysis: Analyze all nine samples in a single sequence for repeatability. For intermediate precision, a second analyst should repeat the entire process on a different day using a different instrument, if possible.
- Data Analysis:
- Accuracy: For each concentration level, calculate the mean recovery percentage.
Recovery (%) = (Mean Measured Concentration / Theoretical Concentration) * 100. - Precision (Repeatability & Intermediate Precision): Calculate the %RSD for the triplicate measurements at each concentration level for each analyst.
%RSD = (Standard Deviation / Mean) * 100.
- Accuracy: For each concentration level, calculate the mean recovery percentage.
Protocol for Robustness Testing
Robustness testing proves the method is reliable despite minor, expected fluctuations in operational parameters.
- Identify Critical Parameters: Select key method parameters that may vary (e.g., mobile phase pH ±0.2 units, column temperature ±2°C, flow rate ±5%).
- Experimental Design: Use a single, homogenous sample solution. Vary one parameter at a time (OFAT) from the nominal conditions while keeping others constant.
- Analysis and Reporting: Analyze the sample under each varied condition. Report the effect on critical method attributes, such as retention time, resolution from the nearest peak, and tailing factor. The method is considered robust if all results remain within predefined acceptance criteria under the slightly varied conditions [39].
Workflow Diagram: The Path to an Audit-Ready Report
The following diagram visualizes the end-to-end process of analytical method validation and report creation, from planning to final approval.
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of a validated method is contingent on the quality of the materials used. The following table outlines essential reagents and materials, their critical functions, and key quality control considerations.
Table 2: Key Research Reagents and Materials for Method Validation
| Reagent/Material | Critical Function in Validation | Key Quality Attributes & Handling |
|---|---|---|
| Reference Standard | Serves as the benchmark for quantifying the analyte and establishing method accuracy [39]. | Certified purity and identity; proper storage conditions to maintain stability; use within expiration date. |
| High-Purity Solvents | Form the mobile phase, dissolve samples, and can significantly impact baseline noise and peak shape. | HPLC/GC grade or equivalent; low UV absorbance; free from particulate matter and impurities. |
| Chromatographic Column | The core component for separation, directly impacting specificity, retention time, and resolution [39]. | Column chemistry, dimensions, and particle size as specified; documented performance under validated conditions. |
| Buffer Salts & Additives | Control mobile phase pH and ionic strength, critical for analyte retention, peak shape, and robustness [39]. | High-purity grade; pH monitoring and adjustment; stability of prepared solutions over time. |
| System Suitability Standards | Verify that the total analytical system is suitable for the intended analysis on the day it is performed. | A defined mixture to confirm parameters like plate count, tailing factor, and %RSD before sample analysis. |
Ensuring Regulatory Success
An audit-ready validation report is more than a collection of data; it is a coherent narrative that demonstrates control over the analytical process. By adhering to the ICH Q2(R2) framework, providing complete and well-organized data, and preemptively addressing potential auditor questions through rigorous robustness testing, the report becomes a powerful tool for regulatory compliance [39]. This diligence ensures product quality and safety, ultimately protecting the consumer and upholding the integrity of the scientific and regulatory process.
Beyond the Basics: Overcoming Common SLV Challenges and Pitfalls
Single-laboratory method validation (SLV) serves as a critical foundation for ensuring the reliability, accuracy, and reproducibility of analytical data before a method is transferred to other laboratories or undergoes full inter-laboratory validation. Within this framework, two pitfalls consistently challenge researchers: the establishment of inappropriate acceptance criteria and the demonstration of incomplete specificity. These shortcomings can compromise data integrity, lead to costly rework, and ultimately undermine confidence in analytical results that drive critical decisions in drug development.
This guide examines the root causes of these common mistakes, provides actionable strategies for prevention, and outlines detailed experimental protocols to ensure your validation work meets the rigorous standards expected by regulatory bodies and the scientific community. A proactive approach to these aspects of validation safeguards not only your data but also the project timelines and resources that depend on it.
The Critical Role of Specificity in SLV
Understanding Specificity and Common Pitfalls
Specificity is the ability of an analytical method to unequivocally assess the analyte in the presence of other components that may be expected to be present in the sample matrix [3] [11]. This includes impurities, degradation products, isomers, and excipients. A method lacking specificity is fundamentally flawed, as it cannot guarantee that the measured signal originates solely from the target analyte.
Incomplete specificity often manifests during method development and validation through several key failures:
- Failure to Assess All Potential Interferences: A common oversight is not testing for interference from all known and potential impurities, degradation products, and matrix components [2].
- Over-reliance on Retention Time: In chromatographic methods, using only retention time for peak identification without confirming peak purity is a significant risk [3].
- Inadequate Forced Degradation Studies: For stability-indicating methods, failing to subject the sample to appropriate forced degradation conditions (e.g., heat, light, acid, base, oxidation) to demonstrate that the method can separate and quantify the analyte from its degradation products [2].
Experimental Protocols for Establishing Specificity
A robust specificity study must prove that the method can unambiguously quantify the analyte in the presence of a representative sample matrix.
Protocol 1: Specificity via Forced Degradation and Peak Purity
- Sample Preparation: Prepare the following solutions in triplicate:
- Blank: The sample matrix (e.g., placebo formulation) without the analyte.
- Analyte Standard: A pure reference standard of the analyte at the target concentration.
- Stressed Sample: The drug substance or product subjected to forced degradation conditions (e.g., 0.1M HCl, 0.1M NaOH, 3% H₂O₂, heat, light) to generate approximately 5-20% degradation.
- System Suitability Solution: A mixture of the analyte and all available known impurities to demonstrate resolution.
- Analysis: Inject all solutions into the chromatographic system (e.g., HPLC with DAD or MS detection).
- Data Analysis and Acceptance Criteria:
- Peak Purity: For the analyte peak in the stressed sample, use a photodiode-array (PDA) detector or mass spectrometry (MS) to demonstrate spectral homogeneity and confirm the absence of co-eluting impurities [3]. The peak purity index should meet pre-defined thresholds.
- Resolution: Resolution between the analyte peak and the closest eluting impurity/degradation product must be greater than 2.0 [3].
- Interference: The blank matrix should show no interfering peaks at the retention time of the analyte or impurities.
Protocol 2: Specificity via Spiked Samples
- Sample Preparation: Prepare a control sample (analyte in matrix) and a test sample by spiking the control sample with all available known impurities and potential interferents at specified levels (e.g., at the specification limit).
- Analysis: Analyze both samples.
- Data Analysis and Acceptance Criteria: The measured concentration of the analyte in the spiked sample should not significantly differ from that in the control sample (e.g., recovery of 98-102%). This demonstrates that the impurities do not interfere with the quantitation of the analyte.
Table 1: Key Parameters for Specificity Assessment
| Parameter | Experimental Requirement | Acceptance Criteria |
|---|---|---|
| Peak Purity | Analysis of stressed samples using DAD or MS | No significant spectral heterogeneity detected; purity angle < purity threshold [3] |
| Resolution | Injection of analyte-impurity mixture | Resolution (Rs) ≥ 2.0 between analyte and all known impurities [3] |
| Interference Check | Analysis of blank matrix (placebo) | No interference at the retention times of the analyte and impurities (interference < LOD/LOQ) [11] |
Visualizing the Specificity Workflow
The following diagram illustrates the logical workflow for a comprehensive specificity assessment, integrating both forced degradation and peak purity verification.
The Pitfalls of Inappropriate Acceptance Criteria
Common Mistakes in Setting Acceptance Criteria
Acceptance criteria are the predefined benchmarks that a method's performance characteristics must meet to be considered valid. Inappropriate criteria can render a validation study meaningless.
Mistake 1: Using Arbitrary or Generic Standards Adopting one-size-fits-all benchmarks without context for the specific method and its intended use is a fundamental error. For instance, applying a generic "%R&R (Gage Repeatability and Reproducibility) needs to be below 10%" rule without considering the process capability and the risk of misclassifying products is a critical misstep [40]. A gauge with a higher %R&R might be perfectly acceptable for a stable process, while one with a lower %R&R might be unacceptable for a highly variable process.
Mistake 2: Disconnection from Business Impact and Risk Criteria set without linking them to tangible business outcomes, such as reducing scrap, improving customer satisfaction, or preventing costly recalls, are often misaligned [40]. This can result in overly strict criteria that burden operations or overly loose ones that allow defects to slip through.
Mistake 3: Overlooking the Full Spectrum of Capability Metrics Focusing solely on a single metric like precision (%RSD) while ignoring other critical performance indicators like bias, linearity, or stability provides an incomplete picture of method capability [40] [3]. A method might have excellent precision but significant bias, leading to inaccurate results.
Mistake 4: A Siloed, Non-Collaborative Approach Allowing only the quality control (QC) department to define criteria without input from process engineering, manufacturing, and R&D can result in unrealistic criteria that don't reflect all technical requirements or practical constraints [40] [41].
Mistake 5: Static Criteria in a Dynamic Environment Treating acceptance criteria as immutable and failing to revisit them after process changes, equipment upgrades, or major nonconformances leads to outdated criteria that no longer reflect the current state [40].
Strategies for Defining Fit-for-Purpose Acceptance Criteria
Strategy 1: Base Criteria on Risk of Misclassification Use risk assessments, process capability studies, and product requirements to define acceptable levels of measurement variation. The criteria should reflect the chance of misclassifying a good product as bad (producer's risk) or a bad product as good (consumer's risk) [40].
Strategy 2: Adopt a Cross-Functional Approach Engage stakeholders from quality control, process development, manufacturing, and regulatory affairs early in the MSA planning process. This ensures criteria are realistic, practical, and reflect all user needs [40] [41].
Strategy 3: Implement a Holistic Validation Protocol Define acceptance criteria for all relevant method performance characteristics, not just one or two. This ensures a comprehensive evaluation of the method's suitability.
Table 2: Example Acceptance Criteria for Key Analytical Parameters
| Performance Characteristic | Experimental Methodology | Example Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a minimum of 9 determinations over 3 concentration levels (e.g., 80%, 100%, 120%) [3]. Report as % recovery. | Mean recovery: 98.0–102.0% [2] |
| Precision (Repeatability) | Analyze a minimum of 6 replicates at 100% of the test concentration [3]. Report as %RSD. | %RSD ≤ 2.0% [2] |
| Linearity | Analyze a minimum of 5 concentration levels. Calculate the correlation coefficient (r) and the coefficient of determination (r²). | r² ≥ 0.990 [2] [11] |
| Range | The interval between the upper and lower concentration levels for which linearity, accuracy, and precision are demonstrated. | Defined by the linearity study, must encompass the intended use concentration. |
| LOD / LOQ | Based on signal-to-noise ratio or standard deviation of the response [2] [3]. | S/N ≥ 3:1 for LOD; S/N ≥ 10:1 for LOQ [3] [11] |
| Robustness | Deliberate, small changes to operational parameters (e.g., pH ±0.2, temp ±2°C). Monitor system suitability. | Method continues to meet all system suitability criteria [2] [11] |
The Scientist's Toolkit: Essential Reagents and Materials
A successful SLV study requires carefully selected, high-quality materials. The following table details key research reagent solutions and their critical functions in the validation process.
Table 3: Essential Materials for Single-Laboratory Validation
| Item | Function & Importance in SLV |
|---|---|
| Certified Reference Standard | Provides the benchmark for accuracy and trueness assessment. Its purity and traceability are foundational to all quantitative results [1]. |
| Placebo/Blank Matrix | Used in specificity testing to demonstrate no interference from excipients or sample components other than the analyte [11]. |
| Available Impurities/Degradants | Critical for establishing specificity, resolution, and for spiking studies to prove the method can separate and quantify the analyte from its potential impurities. |
| Forced Degradation Reagents | Acids, bases, oxidants, etc., used to generate degradants and demonstrate the stability-indicating properties of the method [2]. |
| System Suitability Test (SST) Mix | A mixture of the analyte and key impurities used to verify the chromatographic system's performance (e.g., resolution, efficiency, tailing) is adequate before analysis [2]. |
In single-laboratory method validation, the twin pillars of robust specificity and fit-for-purpose acceptance criteria are non-negotiable. Incomplete specificity undermines the very foundation of the method by creating uncertainty about what is being measured, while inappropriate acceptance criteria provide a false sense of security about the method's performance. By adopting the detailed experimental protocols and strategic frameworks outlined in this guide—including rigorous forced degradation studies, cross-functional collaboration for criteria setting, and a holistic view of method performance—researchers and drug development professionals can avoid these costly pitfalls. A method validated with this disciplined approach will generate reliable, defensible data that accelerates development and ensures product quality and patient safety.
The Impact of Insufficient Method Optimization and Poor Physiochemical Understanding
In the rigorous world of analytical science, particularly within pharmaceutical development and food safety testing, single-laboratory method validation (SLV) serves as a critical foundation for establishing method reliability. The Interstate Shellfish Sanitation Conference (ISSC) explicitly recognizes SLV as a pathway for method acceptance within the National Shellfish Sanitation Program, highlighting its importance in regulatory frameworks [42]. When properly executed, SLV provides a framework for demonstrating that an analytical method is fit for its intended purpose within a specific laboratory environment.
However, the validation process is fundamentally compromised by two pervasive issues: insufficient method optimization and inadequate physiochemical understanding. These deficiencies introduce substantial risks throughout the method lifecycle, leading to unreliable data, regulatory non-compliance, and potential public health consequences. This technical guide examines the impact of these shortcomings through a scientific lens, providing detailed protocols for mitigation within the context of SLV research, as defined by standards such as the ISO 16140 series which is dedicated to method validation and verification in the food chain [22].
The Critical Role of Method Optimization in SLV
Method optimization is the deliberate process of refining analytical procedures to ensure robust performance before formal validation begins. Within an SLV framework, where a single laboratory establishes method validity without an interlaboratory study, the stakes for this preliminary work are exceptionally high [22].
Consequences of Incomplete Optimization
Insufficient optimization manifests in several critical performance failures during validation and subsequent routine use:
- Precision Degradation: A lack of optimization in sample preparation or instrument parameters directly causes high variability. As noted in laboratory best practices, precision should be broken into repeatability (same analyst, same day) and intermediate precision (different days, analysts, or instruments), with a target of ≤2% %RSD for six replicates at one concentration level [2]. Without this, method precision fails validation criteria.
- Accuracy Drift: Inaccurate recovery rates stem from unoptimized sample cleanup, chromatography, or detection settings. Recovery studies should fortify known amounts of analyte into real samples, targeting 95–105% recovery; consistent deviation outside this window necessitates revisiting sample prep or instrument settings [2].
- Specificity Failures: Inadequate optimization of separation or detection parameters results in unresolved interferents. The ISO 16140 standards emphasize the importance of demonstrating that an assay zeroes in on the target analyte without interference [22] [2].
Table 1: Quantitative Impact of Optimization Deficiencies on Validation Parameters
| Validation Parameter | Target Performance | Impact of Poor Optimization |
|---|---|---|
| Precision (%RSD) | ≤ 2% [2] | Can exceed 10-15%, failing acceptance criteria |
| Accuracy (% Recovery) | 95-105% [2] | Systematic biases (e.g., 80-90% or 110-120%) |
| Linearity (R²) | ≥ 0.99 [2] | Lower correlation (e.g., R² < 0.98) |
| LOD/LOQ | S/N 3:1 (LOD), 10:1 (LOQ) [2] | Falsely elevated detection and quantitation limits |
| Robustness | Survives deliberate parameter variations [2] | Method fails with minor, inevitable operational changes |
The Optimization-Validation Workflow
A structured workflow is essential to connect optimization directly to successful validation. The following diagram outlines this critical pathway, from initial setup to final validation, emphasizing the iterative nature of optimization.
The Foundation of Physiochemical Understanding
Beyond operational parameters, a profound understanding of the physiochemical principles governing the analytical method is non-negotiable. This understanding encompasses the molecular interactions between the analyte, matrix, and analytical instrumentation.
The Role of Interfacial Phenomena
The critical importance of physiochemical understanding is exemplified by research into droplet evaporation on micro/nanostructured surfaces. Studies have shown that the solid-liquid-vapor (slv) interface can contribute 16–48% of the total droplet evaporation rate on microstructured surfaces, with the scale of this interface estimated to be 253–940 µm for a 4 µL water droplet [43]. This has direct implications for analytical methods involving sample evaporation, where poor understanding of these interactions leads to:
- Irreproducible Sample Deposition: In HPLC autosamplers or sample concentration steps, variable evaporation rates directly impact the final analyte concentration introduced into the instrument.
- Analytical Bias: The evaporation rate at the slv interface increases with a decrease in the initial contact angle or an increase in droplet volume [43]. Ignoring these factors introduces systematic errors that are difficult to detect without controlled experiments.
Impact on Separation Sciences
In chromatographic method development, poor physiochemical understanding manifests in several ways:
- Ignoring Thermodynamic Relationships: Failure to account for the effects of mobile phase pH, temperature, and solvent strength on retention factor (k), selectivity (α), and resolution (Rs).
- Neglecting Surface Chemistry: Overlooking the interactions between the analyte and the stationary phase surface, or the role of residual silanols in silica-based columns, leads to tailing peaks and variable retention times.
Integrated Experimental Protocols for SLV
To mitigate the risks described, the following integrated protocols combine rigorous optimization with deep physiochemical understanding.
Protocol 1: Systematic Robustness Testing
This protocol is designed to probe method boundaries and identify critical parameters before validation.
- Parameter Selection: Identify at least 5-7 critical method parameters (e.g., mobile phase pH ±0.2 units, column temperature ±5°C, % organic solvent ±2%) [2].
- Experimental Design: Employ a Design of Experiments (DoE) approach, such as a Plackett-Burman or Fractional Factorial design, to efficiently explore multiple variables and their interactions simultaneously [2].
- Response Monitoring: Key responses include retention time, resolution, peak area, and tailing factor.
- Data Analysis: Use statistical modeling to identify parameters with a significant effect (p < 0.05) on critical responses. Establish a system suitability test (SST) boundary for each.
Protocol 2: Forced Degradation for Specificity and Stability
This protocol ensures the method can accurately measure the analyte in the presence of potential degradants, confirming physiochemical specificity.
- Stress Conditions: Subject the analyte to stress conditions including acid/base, oxidative, thermal, and photolytic degradation [2].
- Sample Analysis: Analyze stressed samples to demonstrate resolution between the analyte peak and degradation products.
- Peak Purity Assessment: Use diode-array or mass spectrometric detection to confirm analyte peak homogeneity.
- Validation: Success is achieved when the method provides clear separation and accurate quantitation of the analyte despite the presence of degradants.
Research Reagent Solutions and Essential Materials
The following reagents and materials are fundamental to executing the protocols above and building a robust, well-understood method.
Table 2: Key Research Reagent Solutions for Method Optimization and Validation
| Reagent/Material | Function and Critical Role |
|---|---|
| Characterized Reference Standard | Provides the benchmark for identifying the target analyte and establishing key validation parameters like linearity and accuracy. Its purity is foundational to all results. |
| Relevant Blank Matrices | Essential for testing method specificity and demonstrating the absence of interferents from the sample itself, a core requirement [2]. |
| System Suitability Test (SST) Mixtures | A critical solution containing the analyte and key potential interferents to verify that the chromatographic system is operating correctly before a validation run [2]. |
| Stressed Samples (Forced Degradation Products) | Used in Protocol 2 to prove the stability-indicating capability of the method and its specificity against degradants [2]. |
| Buffers and Mobile Phases (Multiple pH/Solvent Strengths) | Crucial for understanding the physiochemical behavior of the analyte and optimizing for robustness during method development. |
A Framework for Risk Mitigation in SLV
To systematically address the challenges of insufficient optimization and poor physiochemical understanding, laboratories should adopt a risk-managed SLV framework. The following workflow integrates continuous assessment and refinement, aligning with the lifecycle approach encouraged by standards like ISO/IEC 17025 [2].
In the context of single-laboratory method validation, the risks posed by insufficient method optimization and a superficial physiochemical understanding are profound and multifaceted. They compromise the fundamental validity of analytical data, leading to decisions based on false premises in drug development and food safety monitoring. The integrated experimental protocols and risk mitigation framework presented provide a scientifically-grounded pathway to overcome these challenges. By adopting a rigorous, principles-based approach that treats optimization and understanding as inseparable components of validation, researchers can ensure their SLV outcomes are not only compliant with standards like the ISO 16140 series [22] but are also fundamentally reliable, robust, and defensible.
Ensuring Specimen Stability and Proper Handling to Prevent Skewed Results
In single-laboratory method validation (SLV) research, the integrity of analytical results is fundamentally dependent on the conditions of the specimens before they ever reach the analytical instrument. Errors occurring during the pre-analytical phase—encompassing specimen collection, handling, storage, and transport—are a predominant source of inaccuracies, accounting for 46% to 68% of all laboratory errors [44]. For a single laboratory developing and validating its own methods, establishing a rigorous protocol for specimen management is not merely a preliminary step; it is a core component of demonstrating that a method is fit-for-purpose. Specimen stability must be experimentally demonstrated under the specific conditions the laboratory employs, as instability can directly compromise key validation parameters such as accuracy, precision, and robustness [45]. This guide outlines the fundamental principles and practical protocols for ensuring specimen stability, thereby safeguarding the integrity of your SLV research.
Foundational Principles of Specimen Management
Effective specimen management is a holistic process that spans the entire lifecycle of a sample. Adherence to the following principles is essential for maintaining analyte stability and ensuring the traceability required for rigorous SLV.
The Specimen Lifecycle
The journey of a specimen from collection to disposal must be meticulously controlled and documented. Key stages include [46]:
- Collection: Following defined procedures for patient preparation, tube type, and anticoagulant use.
- Processing: Immediate separation of serum or plasma, and aliquoting to prevent continued cell contact.
- Storage & Transport: Maintaining conditions (temperature, time) known to preserve analyte stability.
- Pre- & Post-Analysis Storage: Ensuring stable conditions before testing and for retained samples.
- Chain of Custody: Maintaining an unambiguous record of the specimen's location, condition, and handling throughout its life.
Standardized Terminology and Conditions
To avoid ambiguity in SLV protocols and reports, it is recommended to use standardized terminology for storage conditions rather than specific temperatures. This practice ensures consistency and helps reconcile minor differences in equipment between sites [46]. The proposed terms are:
- Room temperature: 15–25°C
- Refrigerated: 2–8°C
- Frozen: (-15)–(-25)°C
- Ultra-frozen: ≤ -60°C
All storage units must be continuously monitored with alerts for temperature excursions, and a disaster recovery plan should be in place [46].
Key Variables Affecting Specimen Stability
Stability is influenced by a matrix of variables that must be systematically evaluated during method development. The following diagram illustrates the core decision-making workflow for determining specimen stability, adaptable for various analyte types.
Pre-Collection and Collection Variables
Factors determined before and during the blood draw significantly impact downstream stability [44] [47].
- Patient Preparation: Posture (e.g., supine vs. seated), fasting status, and circadian rhythms can influence analyte concentrations. For example, cortisol is highest in the morning.
- Medications and Interfering Substances: Biotin supplements (>5 mg/day) can interfere with immunoassays and should be withheld for at least one week before testing.
- Collection Technique: Tourniquet time should be minimal to prevent hemolysis. Using a 21-gauge needle or larger and allowing alcohol to dry completely before venipuncture reduces the risk of in-vitro hemolysis.
- Order of Draw: Adhering to a specified order prevents cross-contamination from anticoagulants. A typical sequence is: 1. Blood cultures, 2. Sodium citrate tubes, 3. Serum tubes, 4. Lithium heparin, 5. EDTA tubes [44].
- Anticoagulant Selection: For flow cytometry, Sodium Heparin and EDTA are versatile, but specific assays may require specialized preservatives like CytoChex for extended stability [47].
Post-Collection Handling and Storage
After collection, time and temperature are the most critical factors.
- Serum/Plasma Separation: Prolonged contact between serum/plasma and cells causes erroneous results for analytes like potassium, which can increase due to leakage from red blood cells. Separation should occur within 30-60 minutes of collection [48] [44].
- Temperature and Time: Stability is analyte-specific. A study on 17 biochemical analytes found most were stable for 30 days at -20°C, but amylase activity decreased significantly after just 7 days, indicating it must be tested fresh [48].
- Freeze-Thaw Cycles: The impact of multiple freeze-thaw cycles must be evaluated for sensitive analytes, especially in cerebrospinal fluid (CSF) research for biomarkers like Aβ1-42, T-tau, and P-tau [49].
Experimental Protocols for Stability Assessment in SLV
For a single laboratory to claim a method is validated, it must provide empirical data proving specimen stability under the conditions of its specific operational workflow.
Protocol for Evaluating Serum Analyte Stability
This protocol is designed to determine the stability of common biochemical analytes in serum under frozen storage conditions, a common scenario in SLV.
Objective: To determine the stability of key biochemical analytes in human serum stored at -20°C for up to 30 days [48].
Materials and Reagents: Table: Essential Research Reagent Solutions for Serum Stability Studies
| Item | Function/Description | Example/Comment |
|---|---|---|
| Serum Tubes | Collects blood and permits clot formation. | Plastic Vacuette serum tubes (e.g., BD Vacutainer) [48]. |
| Aliquoting Tubes | For storing separated serum. | 1.5 mL Eppendorf tubes [48]. |
| Centrifuge | Separates serum from blood cells. | Standard clinical centrifuge (e.g., 3500 rpm for 10 min) [48]. |
| Autoanalyzer | Measures analyte concentrations. | Olympus AU 400, Roche AVL electrolyte analyzer [48]. |
| Quality Control (QC) Serum | Monitors analytical precision and calculates clinical significance. | Commercial QC material with known target ranges [48]. |
Methodology:
- Sample Collection and Processing: Collect fasting venous blood into serum tubes. Allow tubes to clot for 30 minutes at room temperature. Centrifuge at 3500 rpm for 10 minutes. Visually inspect serum for hemolysis or lipemia and discard unsuitable samples [48].
- Baseline Measurement (T1d): Immediately analyze an aliquot of the freshly separated serum for all target analytes.
- Aliquoting and Storage:
- Pool the remaining serum from each subject.
- Aliquot into multiple 1.5 mL Eppendorf tubes.
- Store aliquots at -20°C for defined durations (e.g., 7 days/T7d, 15 days/T15d, 30 days/T30d) [48].
- Analysis of Stored Samples: Remove stored aliquots at each time point, thaw (if frozen), and analyze using the same autoanalyzer and reagents as the baseline measurement.
Data Analysis:
- Statistical Significance: Use repeated-measures ANOVA to identify statistically significant changes (p < 0.05) over time [48].
- Clinical Significance: Calculate the Significant Change Limit (SCL). The SCL is defined as the baseline mean value ± 3.0 times the usual standard deviation (USD). The USD is derived from internal quality control data. A change beyond the SCL is considered clinically significant, regardless of statistical outcome [48].
Quantitative Stability Data for Common Biochemical Analytes
The following table summarizes exemplary data from a stability study, illustrating how to present and interpret results for an SLV report. Table: Stability of Biochemical Analytes in Serum Stored at -20°C [48]
| Analyte | Stability Duration (Days at -20°C) | Statistical Significance (p<0.05) | Clinical Significance (Exceeds SCL) |
|---|---|---|---|
| Sodium (Na+) | 30 | No (except T15d) | No |
| Potassium (K+) | 30 | No | No |
| Urea | 30 | No | No |
| Creatinine | 30 | No | No |
| Uric Acid | 30 | No | No |
| Amylase | 0 (Unstable after 7 days) | Yes (at T7d, T15d, T30d) | Yes |
| Alkaline Phosphatase (ALP) | 30 | Yes (decrease) | No |
| Total Protein | 30 | No | No |
| Albumin | 30 | Yes (on T30d) | No |
| Cholesterol | 30 | Yes (on T15d) | No |
| Triglycerides | 30 | Yes (on T7d) | No |
Application-Specific Stability Considerations
Stability protocols must be tailored to the specimen type and analytical technique, as requirements can differ dramatically.
Flow Cytometry Specimens
For flow cytometry used in immunophenotyping or pharmacodynamic studies, stability is multidimensional.
- Specimen Type: Peripheral whole blood is most common, but Peripheral Blood Mononuclear Cells (PBMC) and solid tissues (e.g., tumor, spleen) are also used. Tissues require disruption into single-cell suspensions [47].
- Critical Parameters: Stability assessment must evaluate light scatter properties and marker expression. For example, the granulocyte population in EDTA blood may show degradation in forward and side scatter within 24 hours at room temperature [47].
- Acceptance Criteria: Precision of the assay is often used to set stability limits. Relative percent change from baseline and careful examination of fluorescence plots are standard evaluation methods [47].
Cerebrospinal Fluid (CSF) and Specialized Specimens
CSF is a precious and labile specimen, necessitating highly controlled pre-analytical handling for neurodegenerative disease biomarkers.
- Influencing Factors: Stability is affected by collection tube type, centrifugation parameters, freezing delay, storage temperature (-20°C vs. -80°C), and freeze-thaw cycles [49].
- Standardization: For biobanking or multi-site studies, a consensus protocol for CSF collection and biobanking is critical to ensure sample integrity and the comparability of results [49].
Ensuring specimen stability is not a standalone activity but an integral part of demonstrating that an analytical method is fit-for-purpose in single-laboratory method validation. By systematically addressing the entire specimen lifecycle—from patient preparation and collection to long-term storage—researchers can identify and control the major sources of pre-analytical variation. The experimental data generated through structured stability studies, as outlined in this guide, provides the empirical evidence required to define acceptable specimen handling conditions in the laboratory's Standard Operating Procedures (SOPs). This rigorous approach solidifies the foundation of the entire analytical process, ensuring that the results generated in SLV are reliable, reproducible, and ultimately, scientifically defensible.
Strategies for Investigating All Potential Interferences in Complex Sample Matrices
Within the framework of single-laboratory method validation (SLV), the investigation of potential interferences is a critical component for establishing a method's fitness for purpose [26]. Interferences are defined as the effects of components in the sample, other than the analyte, on the measurement of the quantity [50]. In complex matrices—such as biological fluids, environmental samples, or food products—the risk of interferences is significantly heightened. These effects can manifest as false positives, suppressed or enhanced signal response, or an overall loss of precision and accuracy, ultimately compromising the reliability of the analytical data [51] [50]. A systematic investigation of all potential interferences is, therefore, not merely a regulatory checkbox but a fundamental scientific activity to ensure that the method produces data that is accurate, reliable, and defensible.
This guide provides a detailed strategy for identifying, evaluating, and mitigating interferences, with a focus on practical, actionable protocols that can be implemented within a single laboratory.
Classifying Interferences in Analytical Methods
A logical first step in a systematic investigation is to categorize the nature of potential interferences. This classification informs the selection of appropriate detection and mitigation strategies. Interferences can be broadly divided into two main categories, each with specific sub-types.
Spectroscopic Interferences
These occur when an interfering species contributes directly to the analyte's signal. They are particularly relevant in techniques like ICP-MS but have analogues in other spectroscopies [51].
- Isobaric Interferences: Caused by different elements or molecules having the same nominal mass-to-charge ratio (m/z). An example is ¹⁰⁰Mo interfering with ¹⁰⁰Ru [51].
- Polyatomic Interferences: Arise from molecular ions formed from the plasma gas, solvent, or sample matrix. For instance, ArC⁺ can interfere with the measurement of ⁵²Cr⁺ in ICP-MS [51].
- Doubly Charged Ions: Elements with low second ionization potentials can form M²⁺ ions, which are detected at half their mass. For example, ¹³⁶Ba²⁺ can interfere with ⁶⁸Zn⁺ [51].
Non-Spectroscopic Interferences (Matrix Effects)
This is a catch-all term for interferences that alter the analyte's response without contributing directly to its signal. They are a major challenge in techniques like LC-MS and immunoassays [50] [52].
- Ion Suppression/Enhancement: In LC-MS, co-eluting matrix components can affect the ionization efficiency of the analyte in the source, leading to suppressed or enhanced signals [50].
- Sample Transport Effects: Physical properties of the sample (viscosity, surface tension) can alter nebulization efficiency [51].
- Chemical Interferences: In immunoassays, components like phospholipids, proteins, or carbohydrates can bind to the analyte or antibodies, skewing results [52].
Table 1: Categorization of Interferences and Their Characteristics
| Interference Type | Cause | Common Techniques Affected |
|---|---|---|
| Isobaric | Different isotope with same nominal mass | ICP-MS |
| Polyatomic | Molecular ions from plasma/solvent/matrix | ICP-MS |
| Doubly Charged Ions | Formation of M²⁺ species | ICP-MS |
| Ion Suppression/Enhancement | Co-eluting matrix affects ionization | LC-ESI/MS, LC-APCI/MS |
| Physical Matrix Effects | Viscosity, surface tension differences | ICP-MS, LC-MS |
| Chemical Binding | Interaction with antibodies or reagents | Immunoassays |
Experimental Protocols for Detecting and Evaluating Interferences
A robust interference investigation employs a combination of qualitative and quantitative experiments. The following protocols are designed to be integrated into a SLV plan.
The Post-Column Infusion Method (Qualitative Assessment)
This method provides a powerful visual map of ionization suppression/enhancement zones throughout a chromatographic run [50] [53].
Detailed Protocol:
- Setup: Configure the LC-MS system with a post-column T-piece. The mobile phase flows from the column, and a solution of the analyte at a constant concentration is infused post-column via a syringe pump at a low flow rate (e.g., 10 µL/min) [50].
- Analysis: Inject a blank sample extract (a processed sample without the analyte) and perform a standard chromatographic run.
- Data Collection & Interpretation: Monitor the signal of the infused analyte. A stable signal indicates no matrix interference. A depression in the signal indicates ion suppression at that retention time, while an increase indicates ion enhancement [50]. This helps identify "clean" and "dirty" regions of the chromatogram for method optimization.
The Post-Extraction Spike Method (Quantitative Assessment)
This method provides a quantitative measure of the matrix effect (ME) for a specific analyte at a defined concentration [50] [50].
Detailed Protocol:
- Preparation:
- Prepare (A) a neat standard solution in mobile phase or buffer.
- Prepare (B) a blank matrix sample extracted according to the method, then spiked with the analyte post-extraction at the same concentration as (A).
- Analysis: Analyze both (A) and (B) and record the analyte response (e.g., peak area).
- Calculation: Calculate the Matrix Effect (ME%) using the formula:
Specificity and Selectivity via Spiking Experiments
This protocol tests the method's ability to measure the analyte unequivocally in the presence of other components [2].
Detailed Protocol:
- Sample Preparation:
- Analyze a blank matrix to confirm the absence of endogenous interference at the analyte's retention time.
- Spike the blank matrix with the target analyte at a relevant concentration (e.g., near the LOQ).
- Individually spike the blank matrix with potentially interfering substances (e.g., metabolites, structurally similar compounds, salts, lipids) at high, physiologically relevant concentrations.
- Analysis and Acceptance Criterion: Analyze all samples. The method is considered specific if the measurement of the analyte in the presence of interferents is within ±15-20% of the measurement without interferents, and if there is no significant peak overlap [2].
Recovery Studies for Accuracy and Matrix Interference
Recovery experiments assess the efficiency of the entire analytical process and can reveal losses or interferences related to sample preparation [2] [52].
Detailed Protocol:
- Preparation:
- Prepare (A) a blank matrix sample.
- Prepare (B) the same blank matrix sample spiked with a known quantity of the analyte before sample preparation (pre-extraction spike).
- Prepare (C) the blank matrix sample spiked with the same quantity of analyte after sample preparation (post-extraction spike).
- Analysis: Process all samples according to the method and analyze them.
- Calculation: Calculate the percent recovery using the formula:
Percent Recovery = [(Concentration in B - Concentration in A) / Spiked Concentration] × 100[52].- Recovery is typically acceptable within 80-120% [52]. Low recovery indicates possible analyte loss, binding, or degradation during sample preparation, while a difference between pre- and post-extraction spike recoveries points directly to matrix effects [50].
The following workflow diagrams the strategic application of these key experimental protocols within a method validation process.
Quantitative Data Analysis and Acceptance Criteria
Data derived from interference studies must be evaluated against pre-defined, scientifically justified acceptance criteria. The following table summarizes key parameters and their typical benchmarks.
Table 2: Key Parameters and Acceptance Criteria for Interference Studies
| Study Type | Parameter Measured | Calculation Formula | Typical Acceptance Criteria | Interpretation |
|---|---|---|---|---|
| Post-Extraction Spike | Matrix Effect (ME%) | (Response of Spiked Blank Matrix / Response of Neat Standard) × 100% [50] |
85–115% | Values within range indicate minimal matrix effect. |
| Recovery | Percent Recovery | [(Spiked Sample Conc. - Native Sample Conc.) / Spiked Amount] × 100% [52] |
80–120% [52] | Measures accuracy; values outside range indicate loss or interference. |
| Specificity | Signal Change | (Response with Interferent - Response without Interferent) / Response without Interferent) × 100% |
±15–20% | Method is specific if change is within tolerance. |
| Comparison of Methods | Systematic Error (Bias) | Yc = a + bXc; SE = Yc - Xc (at decision level Xc) [54] |
Based on allowable total error | Estimates inaccuracy attributable to the method vs. a comparator. |
For data from comparison of methods experiments, linear regression analysis is a powerful tool. It allows estimation of systematic error at critical medical decision concentrations. The systematic error (SE) at a given concentration (Xc) is calculated from the regression line (Y = a + bX) as SE = Yc - Xc. The correlation coefficient (r) is more useful for assessing the adequacy of the data range than method acceptability; an r ≥ 0.99 generally indicates a sufficient range for reliable regression estimates [54].
Mitigation Strategies: A Tiered Approach
When interference is identified, a tiered approach should be applied to manage it.
Primary Strategies (Minimization)
These strategies aim to remove or reduce the interference at its source.
- Chromatographic Optimization: Adjusting the gradient, changing the column chemistry, or modifying the mobile phase pH can separate the analyte from co-eluting interferents, as identified by the post-column infusion experiment [50].
- Sample Clean-up: Incorporating a solid-phase extraction (SPE) or protein precipitation step that selectively retains the analyte while removing matrix components [50].
- Alternative Ionization Sources: Switching from electrospray ionization (ESI), which is highly prone to matrix effects, to atmospheric pressure chemical ionization (APCI) can sometimes reduce sensitivity to certain interferences [50].
Secondary Strategies (Compensation)
When minimization is insufficient, compensation techniques are used to account for the remaining interference.
- Internal Standardization: The use of a stable isotope-labeled internal standard (SIL-IS) is the gold standard for compensating for matrix effects in mass spectrometry. The IS experiences nearly identical suppression/enhancement as the analyte, allowing for accurate correction [50].
- Matrix-Matched Calibration: Preparing calibration standards in the same blank matrix as the samples. This is effective only if a consistent, representative, and interference-free blank matrix is available [50] [52].
- Standard Addition: The most effective way to compensate for matrix effects, where the calibration is performed by spiking the sample itself with increasing amounts of analyte. This is highly accurate but labor-intensive and not suitable for high-throughput analysis [50].
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and materials crucial for conducting rigorous interference studies.
Table 3: Essential Research Reagent Solutions for Interference Investigations
| Item | Function / Purpose | Key Considerations |
|---|---|---|
| Blank Matrix | For preparing calibration standards, QCs, and for spiking experiments (post-extraction spike, recovery) [50]. | Must be free of the target analyte and representative of the sample matrix. Can be challenging to obtain for some biological fluids. |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | To compensate for variability in sample preparation and matrix effects during MS analysis [50]. | Should be added to the sample at the earliest possible step. Must be physiochemically identical to the analyte but distinguishable by mass. |
| Analyte Standard (High Purity) | For preparing spiked samples, calibration curves, and for post-column infusion experiments [50]. | Purity must be well-characterized to ensure accuracy of spiking experiments. |
| Potential Interferent Standards | To experimentally challenge the method's specificity (e.g., metabolites, co-administered drugs, common matrix components like phospholipids) [2]. | Should be selected based on the sample type and the known biology/chemistry of the system. |
| Sample Dilution Buffer | To reduce the concentration of interfering components in the sample [52]. | The same buffer should be used for diluting both samples and standards. Optimal dilution factor must be determined experimentally. |
Integrating Interference Assessment into the Method Validation Lifecycle
Investigation of interferences is not a one-time activity. It is an integral part of the method lifecycle, as defined in the Eurachem guide on the fitness for purpose of analytical methods [26]. The findings from these studies must be thoroughly documented in the validation report, and the chosen mitigation strategies must be incorporated into the final method Standard Operating Procedure (SOP).
Revalidation should be triggered when there is a change in the sample matrix that could introduce new interferences, or when a change is made to the method that could alter its selectivity (e.g., a new lot of critical reagents, a change in chromatographic column) [2] [26]. By adopting this systematic and lifecycle-oriented approach, researchers can ensure their methods remain robust, accurate, and fit for their intended purpose, even when applied to the most complex sample matrices.
Implementing a QbD (Quality by Design) Approach for More Robust Method Development
Quality by Design (QbD) represents a fundamental paradigm shift in pharmaceutical development, moving away from traditional empirical, retrospective quality checks toward a systematic, proactive methodology that builds quality into products and processes from the outset [55] [56]. Rooted in the International Council for Harmonisation (ICH) guidelines Q8-Q11, QbD emphasizes scientific understanding and quality risk management to enhance product robustness and regulatory flexibility [56]. For analytical method development, this translates to designing methods that consistently deliver reliable performance by understanding and controlling sources of variability, rather than merely testing the final output [55].
This approach is particularly crucial in the context of Single-Laboratory Validation (SLV) research, where a laboratory must demonstrate that a newly developed method is fit for its intended purpose before broader implementation [35] [42]. Implementing QbD principles in SLV provides a structured framework for establishing method robustness, ensuring that methods transferred to other laboratories or applied to new matrices will perform reliably, thereby reducing the risk of method failure during technology transfer or regulatory submission [57].
Core Principles and Components of QbD in Method Development
The QbD framework for analytical methods is built upon several key components that work in concert to ensure method robustness.
The Analytical Target Profile (ATP) and Critical Quality Attributes (CQAs)
The Analytical Target Profile (ATP) is the cornerstone of QbD and serves as the formal definition of the method's requirements. It is a prospective summary of the analytical procedure's performance characteristics, ensuring the method is suitable for its intended purpose [55] [58]. The ATP explicitly defines what the method must achieve, including criteria for accuracy, precision, sensitivity, specificity, and robustness [55].
Following the ATP, Critical Quality Attributes (CQAs) are identified. CQAs are the measurable properties of the analytical method that most directly impact its ability to meet the ATP [55] [56]. For a chromatographic method, typical CQAs include resolution between peaks, tailing factor, retention time, and precision [55] [58].
Table 1: Relationship between ATP, CQAs, and Analytical Method Parameters [55]
| Element | Definition | Example | Role in QbD Approach |
|---|---|---|---|
| Analytical Target Profile (ATP) | The desired outcome/performance of the analytical method | "Assay of drug X must be ≥ 98% and ≤ 102%" | Guides all method development objectives |
| Critical Quality Attributes (CQAs) | Attributes affecting method performance aligned to ATP | Peak resolution, retention time, precision | Key measurable factors controlled during development |
| Specificity | Ability to measure the analyte distinctly | Clear separation of active compound in HPLC | Ensures method is selective and reliable |
| Linearity | Method's ability to elicit proportional test results | 50–150% concentration range with R² ≥ 0.999 | Confirms quantitative capability |
| Robustness | Capacity to remain unaffected by small changes | Minor flow rate or temperature shifts | Indicates method reliability under varied conditions |
Risk Assessment and Design of Experiments (DoE)
Risk assessment is a systematic process used to identify and rank potential method variables (e.g., instrument settings, reagent quality, environmental conditions) that could impact the CQAs [55] [56]. Tools such as Failure Mode and Effects Analysis (FMEA) and Ishikawa (fishbone) diagrams are commonly employed to facilitate this process [55] [57]. The output prioritizes factors for subsequent investigation.
Design of Experiments (DoE) is the statistical backbone of QbD. Instead of the inefficient one-factor-at-a-time (OFAT) approach, DoE involves systematically varying multiple factors simultaneously to model their individual and interactive effects on the CQAs [56] [58]. This efficient experimentation allows for the identification of a Method Operable Design Region (MODR), which is the multidimensional combination of input variables (e.g., pH, column temperature, gradient time) demonstrated to provide assurance of method performance [55]. Operating within the MODR ensures method robustness despite minor, expected variations.
Diagram 1: QbD method development workflow showing key stages from ATP definition to continuous monitoring.
A Step-by-Step QbD Implementation Framework for SLV
Integrating QbD into SLV involves a series of structured steps that build upon each other to create a deep, documented understanding of the method.
Step 1: Define the Analytical Target Profile (ATP)
The first step is to prospectively define the ATP based on the method's intended use. For an SLV study aimed at quantifying an active ingredient, the ATP should include quantifiable targets for accuracy (e.g., 98-102% recovery), precision (e.g., %RSD < 2.0%), linearity (e.g., R² > 0.998), range, and specific criteria for specificity against known impurities [35] [58]. This ATP will anchor all subsequent development and validation activities.
Step 2: Identify Critical Quality Attributes (CQAs)
With the ATP defined, identify the CQAs that are critical for achieving those goals. For instance, if the ATP requires accurate quantification of a main component in the presence of degradants, then chromatographic resolution between the analyte and the nearest eluting degradant becomes a CQA. Similarly, injection precision and peak tailing may be CQAs if they directly impact the precision and accuracy stated in the ATP [55].
Step 3: Conduct Risk Assessment
Perform a systematic risk assessment to identify all potential factors that could influence the CQAs. A team-based approach using an Ishikawa diagram is highly effective for brainstorming factors related to instrumentation, materials, methods, environment, and personnel [57]. This is followed by a more formal FMEA to score factors based on their severity, occurrence, and detectability, resulting in a Risk Priority Number (RPN). This process separates low-risk factors (which can be fixed or monitored) from high-risk factors (which require further study via DoE) [57].
Diagram 2: Ishikawa (fishbone) diagram for risk assessment in HPLC method development, categorizing potential failure sources.
Step 4: Perform DoE Studies
Focus DoE studies on the high-risk factors identified in the previous step. A typical approach might use a full or fractional factorial design to screen for significant factors, followed by a response surface methodology (e.g., Central Composite Design) to model and optimize the region of operation [56]. The responses measured in the DoE are the CQAs (e.g., resolution, peak area, retention time). The resulting model allows for the prediction of method performance within the studied space and defines the MODR [55] [58].
Step 5: Verify the MODR and Establish a Control Strategy
Verify the predicted MODR through experimental confirmation runs. Once verified, a control strategy is implemented to ensure the method remains in a state of control throughout its lifecycle. This includes system suitability tests (SSTs) that monitor key CQAs before each analytical run, as well as controls for critical reagents, columns, and instrument qualification [56] [57]. The control strategy is the practical outcome of the QbD process, providing ongoing assurance of method robustness.
Step 6: Continuous Monitoring and Lifecycle Management
QbD is a lifecycle approach. Data from routine use of the method, including SST results and performance during method transfers, should be continuously monitored. This data can be used to refine the MODR or control strategy under a robust change management system, facilitating continuous improvement without requiring major regulatory submissions for minor changes [56] [57].
Experimental Protocols and Key Methodologies
Protocol for a DoE-Based Robustness Test
This protocol is designed to empirically define the MODR for a Reverse-Phase HPLC method.
- Define Factors and Ranges: Based on the risk assessment, select 4-6 critical factors (e.g., mobile phase pH (±0.2 units), organic modifier concentration (±2-5%), column temperature (±5°C), and flow rate (±0.1 mL/min). Set realistic ranges that represent expected variations in routine use.
- Select DoE Model: A fractional factorial design (e.g., Resolution V) is often sufficient for robustness testing, as it efficiently estimates main effects and two-factor interactions with a manageable number of experimental runs.
- Execute Experiments: Run the experiments in a randomized order to minimize the impact of uncontrolled variables. Use a qualified UHPLC/HPLC system. For each run, record the responses (CQAs) such as retention time of the main peak, resolution from the closest eluting peak, tailing factor, and peak area.
- Analyze Data: Use statistical software to fit a model to the data. Analyze Analysis of Variance (ANOVA) tables to identify which factors have a statistically significant effect (p-value < 0.05) on each CQA. Generate contour plots or response surfaces to visualize the relationship between factors and responses.
- Define the MODR: The MODR is the region within the experimental space where all CQAs consistently meet the acceptance criteria defined in the ATP. This is a region of guaranteed robustness, not just a single setpoint.
Protocol for a QbD-Driven Single-Laboratory Validation
This protocol integrates QbD principles into the standard SLV process, as exemplified by the CoQ10 UHPLC study [35].
- Pre-Validation with MODR Verification: Before formal validation begins, perform a few confirmation runs within the MODR to verify that the method performs as expected.
- Validation per Regulatory Guidelines: Conduct the standard validation tests as per ICH Q2(R1) or USP <1225>, but using the knowledge gained from the QbD studies.
- Specificity: Demonstrate analyte peak purity and separation from placebo and known impurities, as confirmed during risk assessment and DoE [35].
- Linearity: Prepare and analyze calibration standards across the specified range (e.g., 50% to 200% of target concentration). The correlation coefficient, y-intercept, and residual plots should meet ATP criteria [35].
- Accuracy (Recovery): Spike the analyte into a placebo matrix at multiple levels (e.g., 50%, 100%, 150%). Calculate the mean percent recovery, which should be within predefined limits (e.g., 98-102%) [35].
- Precision:
- Repeatability: Analyze six independent samples at 100% of the test concentration. The %RSD should meet the ATP target (e.g., <2.0%) [35].
- Intermediate Precision (Ruggedness): Demonstrate reproducibility by having a second analyst perform the analysis on a different day and/or using a different instrument. The combined data should still meet precision criteria [35] [57].
- LOD/LOQ: Determine via signal-to-noise ratio or standard deviation of the response, as required by the ATP [35].
- Solution Stability: Evaluate standard and sample solution stability over time (e.g., 24-48 hours) under storage conditions (e.g., room temperature, refrigerated) to define the handling parameters [35].
Table 2: Key Reagents and Materials for a QbD-Based Chromatographic Method [35] [57] [58]
| Category | Item | Function / Critical Attribute | QbD Consideration |
|---|---|---|---|
| Reference Standards | Coenzyme Q10 Reference Standard [35] | Quantification of the analyte; defines method accuracy. | Purity, stability, and proper storage are Critical Material Attributes (CMAs). |
| Chromatography | UHPLC/HPLC System [35] [58] | Separation and detection of analytes. | Dwell volume, flow rate accuracy, and detector linearity are CMPs. |
| C18 Column (e.g., 2.1 x 50 mm, 2.6 µm) [35] | Stationary phase for separation. | Column chemistry, lot-to-lot variability, and temperature are high-risk factors. | |
| Solvents & Reagents | HPLC Grade Solvents (Acetonitrile, Alcohol) [35] | Mobile phase components. | Grade, purity, and UV transparency are CMAs. Composition and pH are CMPs. |
| HPLC Grade Water | Mobile phase and sample preparation. | Purity and freedom from contaminants are CMAs. | |
| Sample Prep | Volumetric Flasks, Pipettes | Accurate dilution and preparation of standards/samples. | Calibration and technique are potential noise factors controlled via procedure. |
| Syringe Filters (e.g., 0.45 µm) | Clarification of samples prior to injection. | Membrane material (nylon, PTFE) can adsorb analyte; a risk assessment is needed. |
The Impact and Future of QbD in Analytical Science
The implementation of QbD yields significant, measurable benefits. Studies indicate that QbD can reduce batch failures by up to 40% and significantly cut development time and costs by minimizing unplanned revalidation and investigation of out-of-specification results [56]. Furthermore, the deep process understanding underpinning the MODR provides greater regulatory flexibility, as changes within the approved design space do not require prior regulatory approval [56] [59].
The future of QbD is intertwined with digitalization and advanced analytics. Emerging trends include the use of AI-driven predictive modeling to accelerate design space exploration, the application of digital twins for real-time method simulation and troubleshooting, and the integration of QbD principles with continuous manufacturing and advanced Process Analytical Technology (PAT) [56]. For SLV, these advancements promise to make robust, QbD-developed methods the standard, ensuring quality and efficacy from the laboratory to commercial production.
Proving Method Performance: Statistical Analysis and Comparative Assessment
Within the framework of single-laboratory method validation (SLV), demonstrating that a new analytical method produces reliable and accurate results is paramount. This process often requires a comparison against a reference method to quantify the agreement between the two measurement techniques [60]. Such comparison studies are a core component of demonstrating that a method is "fit for purpose," providing documented evidence that it performs reliably under the specific conditions of your laboratory [3]. While simple correlation was once commonly used for this task, it is an inadequate measure of agreement because it assesses the strength of a relationship between two variables, not the size of their differences [61]. Two robust statistical techniques have emerged as the standards for method comparison: linear regression analysis and Bland-Altman difference plots. This guide provides an in-depth examination of these methods, offering researchers in drug development detailed protocols for their implementation and interpretation within an SLV context.
Core Concepts in Method Comparison
The Inadequacy of Correlation
A high correlation coefficient (r) does not mean two methods agree. Two methods can be perfectly correlated yet have consistently different results, a fact that correlation alone will not reveal [61]. The core objective of a method comparison study is not to establish if two methods are related, but to quantify the size and nature of the differences between them and to determine if these differences are acceptable for the intended clinical or analytical use [61].
Defining the Comparison Method
The choice of a comparison method is critical. Ideally, it should be a reference method with well-defined accuracy. In practice, the comparison is often made against the current routine service method that the new method is intended to replace [60]. The primary goal then shifts to understanding the systematic changes, or bias, that will occur when switching from the old to the new method.
Bland-Altman Difference Plot Analysis
The Bland-Altman plot, also known as the Altman-Bland plot, is a powerful graphical method to assess agreement between two quantitative measurement techniques [61]. It moves beyond correlation to directly visualize the differences between paired measurements.
Theoretical Foundation
The Bland-Altman analysis quantifies agreement by calculating the mean difference between the two methods, which estimates the average bias, and constructing limits of agreement (LoA) [61]. These statistical limits are defined as the mean difference ± 1.96 standard deviations of the differences. This interval is expected to contain approximately 95% of the differences between the two measurement methods [61].
Experimental Protocol for a Bland-Altman Study
- Sample Selection: Obtain a set of 20-30 samples that span the entire reportable range of the methods. The samples should cover low, medium, and high concentrations to adequately assess bias across the analytical measurement range [60].
- Paired Measurements: Analyze each sample using both the new (Test) method and the reference (Comparison) method. The order of analysis should be randomized to avoid systematic bias.
- Data Calculation:
- For each sample
i, calculate the difference between the two methods:Difference_i = (Test Method Result_i - Comparison Method Result_i). - For each sample
i, calculate the average of the two methods:Average_i = (Test Method Result_i + Comparison Method Result_i) / 2.
- For each sample
- Statistical Analysis:
- Calculate the mean difference (
d), which represents the average bias. - Calculate the standard deviation (SD) of the differences.
- Calculate the 95% Limits of Agreement:
d - 1.96*SD(lower limit) andd + 1.96*SD(upper limit).
- Calculate the mean difference (
- Graphical Representation: Create a scatter plot.
- The X-axis represents the
Averageof the two measurements for each sample. - The Y-axis represents the
Differencebetween the two measurements for each sample. - Plot a horizontal line at the mean bias.
- Plot two additional horizontal lines representing the upper and lower limits of agreement.
- The X-axis represents the
The following workflow diagram illustrates the key steps in creating and interpreting a Bland-Altman plot:
Interpretation and Clinical Decision
The Bland-Altman plot provides a clear visual assessment of the data. The following table summarizes the key elements to evaluate during interpretation:
Table 1: Key Elements for Interpreting a Bland-Altman Plot
| Element | Interpretation | What to Look For |
|---|---|---|
| Mean Difference (Bias) | The average systematic difference between the two methods. | A line close to zero indicates little average bias. A line consistently above or below zero indicates a constant systematic error. |
| Limits of Agreement (LoA) | The range within which 95% of differences between the two methods are expected to fall. | A narrow interval indicates good agreement. A wide interval indicates high random error or variability between methods. |
| Distribution of Data Points | The spread of the differences across the range of measurement. | Data points should be randomly scattered around the mean bias line, without obvious patterns. |
| Presence of Trends | Indicates proportional error or non-constant bias. | A funnel-shaped pattern (increasing spread with higher averages) suggests heteroscedasticity. A sloped pattern of the data points suggests a proportional bias. |
It is critical to understand that the Bland-Altman method defines the intervals of agreement but does not determine if those limits are acceptable [61]. The acceptability of the bias and limits of agreement is a scientific and clinical decision, often based on pre-defined goals derived from biological variation, clinical guidelines, or regulatory requirements for the specific analyte [60] [61].
Linear Regression Analysis
Linear regression is another fundamental technique for method comparison, used to model the relationship between two methods and identify constant and proportional systematic errors [60].
Theoretical Foundation
Ordinary least squares (OLS) linear regression finds the line that best predicts the results of the test method (Y) from the results of the reference method (X). The regression line is defined by the equation Y = bX + a, where:
- Slope (b): Estimates proportional systematic error. A slope of 1 indicates no proportional difference. A slope >1 indicates the test method yields proportionally higher results, and a slope <1 indicates the opposite.
- Y-intercept (a): Estimates constant systematic error. An intercept of 0 indicates no constant difference. A positive or negative intercept indicates the test method is consistently higher or lower by a fixed amount, regardless of concentration.
Experimental Protocol for a Linear Regression Study
- Sample Selection: As with the Bland-Altman plot, use 20-30 samples covering the entire reportable range [60].
- Paired Measurements: Analyze each sample using both the test and reference methods.
- Data Analysis:
- Plot the test method results (Y) against the reference method results (X).
- Perform linear regression to calculate the slope, intercept, and coefficient of determination (R²).
- For a more rigorous analysis, especially when both methods have error, use Deming regression or Passing-Bablok regression instead of ordinary least squares [61].
- Interpretation:
- Use the slope and intercept to calculate the predicted systematic error at critical medical decision concentrations.
- Assess the residuals (the difference between the observed Y value and the value predicted by the regression line) to check the model's assumptions.
Diagnostic Plots for Regression Validation
After performing a regression analysis, it is essential to examine the residuals to verify the model's assumptions and identify any outliers or patterns that the model failed to capture [62]. The base R plot() function for an lm object provides four key diagnostic plots. The relationships between these plots and their purpose in diagnosing a regression model are shown below:
Table 2: Key Diagnostic Plots for Linear Regression Analysis [62]
| Plot Type | Primary Purpose | Interpretation of a "Good" Model | Problem Indicated by a "Bad" Plot |
|---|---|---|---|
| Residuals vs Fitted | To detect non-linearity and heteroscedasticity (non-constant variance). | Residuals are randomly scattered around zero, forming a horizontal band. | A distinct pattern (e.g., a U-shape or funnel-shape) suggests the model is missing a non-linear relationship or has heteroscedasticity. |
| Normal Q-Q | To assess if the residuals are normally distributed. | The data points closely follow the straight dashed line. | Points deviating severely from the line indicate non-normality of residuals, which can affect hypothesis tests. |
| Scale-Location | To check the assumption of homoscedasticity (constant variance). | A horizontal line with equally spread points. | A rising or falling red smooth line indicates that the variance of the residuals is not constant. |
| Residuals vs Leverage | To identify influential observations that disproportionately affect the regression results. | All points are well within the Cook's distance contours. | Points in the upper or lower right corner, outside the Cook's distance lines, are influential and may need investigation. |
The following table provides a consolidated summary of the two core methods, highlighting their respective purposes, outputs, and strengths.
Table 3: Comparative Summary of Difference Plots and Linear Regression for Method Validation
| Aspect | Bland-Altman (Difference) Plot | Linear Regression Analysis |
|---|---|---|
| Primary Purpose | To assess the agreement between two methods by quantifying and visualizing the differences. | To model the functional relationship between two methods and identify components of systematic error. |
| Key Outputs | Mean bias (constant error), 95% Limits of Agreement (random error). | Slope (proportional error), Y-intercept (constant error), R² (shared variance). |
| Data Presentation | Plots the difference between methods against their average. | Plots the test method result against the reference method result. |
| Strengths | Intuitively shows the magnitude and range of differences. Directly answers "How much do the two methods disagree?". Easy to overlay with clinically acceptable limits. | Separates total systematic error into constant and proportional components. Allows prediction of bias at specific decision levels. |
| Limitations | Does not explicitly separate constant and proportional bias in its basic form. | Can be misleading if only R² is reported. OLS regression assumes the reference method is without error. |
| Best Use Case | When the goal is to understand the typical discrepancy a patient might see between the old and new method. | When the goal is to understand the nature of the bias (constant vs. proportional) to potentially correct the new method. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key materials and resources required for conducting a robust method comparison study in a regulated laboratory environment.
Table 4: Essential Research Reagents and Materials for Method Comparison Studies
| Item | Function / Purpose | Specifications & Considerations |
|---|---|---|
| Stable, Matrix-Matched Samples | To provide a range of concentrations for comparison. Should mimic patient samples. | 20-30 samples covering the full reportable range (low, medium, high). Matrix should match clinical samples (e.g., human serum, plasma). Stability must be verified for the duration of the study [60]. |
| Reference Standard / Material | To establish traceability and accuracy for the comparative method. | Should be a certified reference material (CRM) or a primary standard, if possible. For routine comparisons, the calibrator set for the established method serves this role [60]. |
| Quality Control (QC) Materials | To monitor the performance and stability of both measurement methods during the study. | At least two levels (low and high) of commercially available or internally prepared QC materials. Analyzed at the beginning and end of each run to ensure methods are in control [2]. |
| Statistical Software | To perform regression, Bland-Altman, and other statistical calculations with accuracy and generate diagnostic plots. | R, Python (with Pandas/NumPy/SciPy), SPSS, or specialized tools like ChartExpo for advanced visualizations [63] [62]. |
| System Suitability Test (SST) Reagents | To verify that the analytical system (especially for chromatographic methods) is operating correctly before the comparison run. | A defined mixture that checks critical performance parameters like resolution, peak tailing, and reproducibility as per the method SOP [3]. |
Estimating Systematic Error at Critical Medical Decision Concentrations
Within the framework of Single-Laboratory Method Validation (SLV) research, the precise estimation of systematic error at critical medical decision concentrations stands as a cornerstone for ensuring the reliability of analytical data. Systematic error, or bias, refers to a consistent or proportional difference between observed values and the true value of an analyte [64] [1]. Unlike random error, which affects precision, systematic error skews results in a specific direction, potentially leading to incorrect medical interpretations, misdiagnoses, or inappropriate treatment decisions [64]. The "comparison of methods" experiment is the critical study designed to estimate this inaccuracy using real patient specimens, thereby providing an assessment of a method's trueness before it is deployed for routine patient testing [54] [65].
The objective of this guide is to provide researchers and drug development professionals with a detailed protocol for executing a comparison of methods experiment, with a focused analysis on quantifying systematic error at those analyte concentrations that directly influence clinical decision-making. This process is a fundamental component of the demonstration that a method is fit for its intended purpose within a single laboratory's unique environment and patient population [1].
Foundational Concepts and Experimental Planning
Types of Systematic Error in Analytical Methods
Systematic error in analytical methods can be categorized based on its behavior across the measuring interval, which has direct implications for how it is quantified and addressed.
- Constant Systematic Error: This error remains the same absolute value across the analytical range of the method. For example, a method might consistently report values 2 mg/dL higher than the true value, regardless of the analyte's concentration. This is often revealed as a non-zero y-intercept in a regression analysis [1].
- Proportional Systematic Error: This error changes in proportion to the concentration of the analyte. A method with proportional error might report values that are 5% higher than the true value, leading to a larger absolute bias at higher concentrations. This is represented by the slope of the regression line deviating from 1.0 [54] [1].
The following diagram illustrates the logical workflow for identifying and addressing these errors through a comparison of methods study.
Workflow for Systematic Error Estimation
The Comparison of Methods Experiment: Purpose and Design
The primary purpose of the comparison of methods experiment is to estimate the inaccuracy or systematic error of a new test method by comparing its results against those from a established comparative method using patient samples [54]. The experimental design is critical for obtaining reliable error estimates.
Key Factors in Experimental Design:
- Comparative Method: The ideal comparative method is a reference method with well-documented correctness. When using a routine method, differences must be interpreted carefully, as discrepancies could originate from either method [54].
- Number of Specimens: A minimum of 40 different patient specimens is recommended. The quality and range of concentrations are more critical than the total number; specimens should cover the entire working range and represent the expected spectrum of diseases [54] [65].
- Replication and Timing: While single measurements are common, duplicate analyses help identify sample mix-ups or transposition errors. The experiment should be conducted over a minimum of 5 days to minimize systematic errors from a single run and reflect long-term performance [54].
- Specimen Stability: Specimens should be analyzed by both methods within two hours of each other to prevent stability-related differences from being misattributed as analytical error. Specific handling procedures must be defined in advance [54].
Quantitative Assessment and Data Analysis
Graphical Data Inspection and Statistical Calculations
The initial analysis involves graphing the data to gain a visual impression of the relationship and potential errors between the two methods.
Graphing the Data: For methods expected to show one-to-one agreement, a difference plot (test result minus comparative result versus comparative result) is ideal. It allows for visual inspection of the scatter around the zero line and helps identify outliers and patterns suggesting constant or proportional error. For methods not expected to agree one-to-one, a comparison plot (test result versus comparative result) is used to visualize the line of best fit and identify discrepant results [54].
Calculating Appropriate Statistics: Linear regression analysis is the preferred statistical tool when data cover a wide analytical range. It provides slope (b) and y-intercept (a), which describe the proportional and constant systematic error, respectively. The systematic error (SE) at a specific medical decision concentration ((Xc)) is calculated as: (Yc = a + bXc) (SE = Yc - X_c) [54] The correlation coefficient (r) is also calculated, but its primary utility is to assess whether the data range is wide enough for reliable regression estimates (r ≥ 0.99 is desirable) [54].
Performance Parameters and Equations
The following table summarizes the key performance parameters and equations used in the quantitative assessment of systematic error.
Table 1: Key Parameters and Equations for Estimating Systematic Error
| Parameter | Equation/Symbol | Description & Interpretation | ||
|---|---|---|---|---|
| Random Error | (Sy/x = \sqrt{\frac{\sum(yi - Yi)^2}{(n-2)}}) | Standard error of the estimate; measures scatter of points around the regression line [1]. | ||
| Regression Line | (Y = a + bX) | Linear model relating Test Method (Y) to Comparative Method (X) [54] [1]. | ||
| Y-Intercept (a) | – | Estimates constant systematic error. A value significantly different from zero indicates a constant bias [54] [1]. | ||
| Slope (b) | – | Estimates proportional systematic error. A value significantly different from 1.0 indicates a proportional bias [54] [1]. | ||
| Systematic Error (SE) at (X_c) | (SE = (a + bXc) - Xc) | Total systematic error at a specific medical decision concentration ((X_c)) [54]. | ||
| Total Error (TE) | (TE = | Bias | + 2*CV) | An estimate of the total error of a method, combining systematic and random error components. |
Experimental Protocols and Implementation
Detailed Protocol: The Comparison of Methods Experiment
This protocol provides a step-by-step guide for conducting a robust comparison of methods study.
Objective: To estimate the systematic error (inaccuracy) of a new test method at critical medical decision concentrations by comparison with a validated comparative method.
Materials and Reagents:
- Test method instrument and reagents.
- Comparative method instrument and reagents.
- A minimum of 40 unique patient specimens (serum, plasma, etc., as applicable).
- Control materials for both methods.
- Data collection worksheet or spreadsheet.
Procedure:
- Specimen Selection: Select patient specimens to cover the entire reportable range of the test. Include specimens from patients with a spectrum of conditions that might be encountered in routine practice [54].
- Experimental Schedule: Analyze approximately 8-10 patient specimens per day over at least 5 different days. Analyze test and comparative methods within two hours of each other to ensure specimen stability [54].
- Analysis Order: Analyze specimens in a randomized order to avoid systematic bias due to run order or time-related drift.
- Data Recording: Record the result for each specimen from the test method (Y-value) and the comparative method (X-value) in a dedicated worksheet.
- Quality Control: Run control materials according to laboratory standard operating procedures for both methods throughout the experiment to ensure both systems are in control.
Data Analysis:
- Graphical Inspection: Create a difference plot or a comparison plot. Inspect for outliers and any obvious patterns indicating error [54].
- Statistical Calculation: Perform linear regression analysis on the data to obtain the slope (b), y-intercept (a), standard error of the estimate (S~y/x~), and correlation coefficient (r).
- Error Estimation: Using the regression equation, calculate the systematic error ((SE)) at each critical medical decision concentration ((X_c)) relevant to the analyte.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials for Method Comparison Studies
| Item | Function / Purpose |
|---|---|
| Characterized Patient Pools | Patient specimens pooled to create materials with known, stable concentrations at critical medical decision levels; used for precision and accuracy studies. |
| Commercial Control Materials | Independent quality control materials with assigned ranges; used to monitor the stability and performance of both the test and comparative methods during the study. |
| Certified Reference Materials (CRMs) | Materials with values certified by a recognized national or international body; provide the highest level of traceability for assessing trueness and calibrating the comparative method. |
| Interference Test Kits | Commercial kits containing high-purity substances (e.g., bilirubin, hemoglobin, lipids) to test the analytical specificity and potential for biased results due to common interferents. |
| Calibrators | Solutions of known concentration used to establish the analytical calibration curve for both the test and comparative methods. |
Interpretation, Judgment, and Integration into SLV
Judging Method Acceptability and Integration with Other Validation Parameters
The final step in the process is to judge whether the observed systematic error, combined with the method's random error, is acceptable for clinical use.
Decision Making: Method performance is judged by comparing the estimated errors to defined quality standards. A common approach is to use Allowable Total Error (TE~a~), such as those specified by CLIA or other proficiency testing programs [65] [1]. A Method Decision Chart can be constructed where the y-axis represents systematic error (bias) and the x-axis represents random error (imprecision, as CV). The operating point (CV, Bias) is plotted. If this point falls within the region defined by the TE~a~ limit, method performance is considered acceptable [65].
Integration with SLV: The comparison of methods experiment is not performed in isolation. It is part of a comprehensive SLV plan that also includes experiments to determine precision (random error), reportable range, and analytical specificity (e.g., interference studies) [65]. The systematic error estimated from the comparison experiment should be consistent with findings from recovery experiments, which can separately estimate constant and proportional error components [65]. The following diagram synthesizes how the assessment of systematic error fits within the broader SLV framework.
SLV Data Synthesis for Decision
The rigorous estimation of systematic error at critical medical decision concentrations is a non-negotiable component of Single-Laboratory Method Validation. Through a carefully designed comparison of methods experiment, followed by robust graphical and statistical analysis, laboratories can quantify the bias of a new method and make a defensible decision about its suitability for clinical use. This process, when integrated with other validation studies, ensures that the methods implemented are not only precise but also accurate, thereby safeguarding patient care and supporting the integrity of data in drug development and clinical research.
In single-laboratory method validation (SLV), the completeness of a measurement result requires both a measured value and a quantitative statement of its uncertainty [66]. This uncertainty parameter characterizes the dispersion of values that could reasonably be attributed to the measurand and is fundamental to assessing result reliability for drug development applications [66]. The integration of random and systematic error components provides researchers with a comprehensive framework for evaluating analytical method performance, ensuring results are fit for their intended purpose in pharmaceutical development and quality control.
Measurement uncertainty arises from multiple potential sources throughout the analytical process, including pre-analytical, analytical, and post-analytical phases [66]. However, for the specific context of SLV, the focus remains predominantly on the analytical phase, encompassing both the inherent imprecision of the measurement system (random error) and the directional biases that may affect accuracy (systematic error) [1]. Proper characterization and combination of these elements allow scientists to place appropriate confidence intervals around results, enabling meaningful comparisons with specification limits or results from other laboratories [67] [66].
Fundamental Error Components: Random and Systematic Errors
Definitions and Characteristics
Understanding the distinction between random and systematic errors is foundational to uncertainty calculation in analytical chemistry and pharmaceutical sciences.
Random Errors: These are statistical fluctuations (in either direction) in the measured data due to the precision limitations of the measurement device [67]. Random errors arise from unpredictable variations in the measurement process and can be evaluated through statistical analysis. They manifest as scatter in results and can be reduced by averaging over a large number of observations [67]. In chromatographic method validation, random error is quantified through precision studies, including repeatability (same analyst, same day) and intermediate precision (different days, analysts, or instruments) [2] [3].
Systematic Errors: These are reproducible inaccuracies that are consistently in the same direction [67]. Unlike random errors, systematic errors cannot be detected or reduced by increasing the number of observations, though they can sometimes be corrected through calibration or applying correction factors [67]. In method validation, systematic error relates to accuracy - the closeness of agreement between an accepted reference value and the value found [3]. Sources include calibration errors, instrument drift, and methodological biases [67].
Practical Manifestations in Pharmaceutical Analysis
In laboratory practice, these errors present distinct patterns. Random error appears as the typical scatter of control values around the mean, exceeding both upper and lower control limits, while systematic error manifests as a shift in one direction where control observations may exceed only one side of the control limits [1]. For chromatographic methods in pharmaceutical analysis, random error might originate from injection volume variability, detector noise, or sample preparation inconsistencies, whereas systematic error could stem from mobile phase preparation errors, incorrect calibration standard concentrations, or spectral interferences [2] [3].
Table 1: Comparison of Random and Systematic Error Characteristics
| Characteristic | Random Error | Systematic Error |
|---|---|---|
| Direction | Varies unpredictably | Consistent direction |
| Reducible through replication | Yes | No |
| Quantified by | Standard deviation, %RSD | Bias, recovery % |
| Detectable via | Repeatability studies | Comparison to reference materials |
| Correctable via | Averaging multiple measurements | Calibration, correction factors |
Mathematical Models for Combining Uncertainty Components
Several mathematical models exist for combining random and systematic errors, each developed for specific purposes with different underlying assumptions [68]. The most common models include:
Linear Model: Also known as the total error approach, this model combines uncertainty components linearly: TE = |bias| + z × σ, where TE is total error, bias is the systematic error component, σ is the random error component (standard deviation or coefficient of variation), and z is the probability factor [68] [1]. This approach provides a conservative estimate of the combined uncertainty.
Squared Model: This model combines uncertainty components in quadrature (square root of the sum of squares), following the principles of the Guide to Uncertainty in Measurements (GUM) [68]. The squared model includes two sub-models: the classical statistical variance model and the GUM model for estimating measurement uncertainty.
Clinical Outcome Model: A combined model developed for estimating analytical quality specifications according to the clinical consequences of errors, considering the medical impact of measurement uncertainty [68] [1].
Detailed Model Formulations
The transformation of bias into imprecision differs considerably across models, leading to substantially different results and consequences for uncertainty estimation [68]. The linear model (total error approach) is often preferred in pharmaceutical quality control environments where specifications must account for worst-case scenarios, while the squared model (GUM approach) follows international metrological standards and typically provides smaller uncertainty estimates [68] [66].
For the linear model, the constant z is typically chosen based on the desired confidence level. For approximately 95% confidence, z = 2 is commonly used [1]. In the squared model, the combined standard uncertainty (uc) is calculated as the square root of the sum of the variances of the individual components: uc = √(urandom² + usystematic²) [1]. The expanded uncertainty (U) is then calculated by multiplying the combined standard uncertainty by a coverage factor (k), typically k=2 for approximately 95% confidence: U = k × uc [1] [66].
Table 2: Mathematical Models for Combining Random and Systematic Errors
| Model Type | Formula | Application Context | Key Assumptions | ||
|---|---|---|---|---|---|
| Linear (Total Error) | TE = | bias | + z × σ [68] | Pharmaceutical quality control, specification setting | Conservative approach, assumes worst-case combination |
| Squared (GUM) | uc = √(urandom² + usystematic²) [68] [1] | Metrology, international standards | Uncertainty components are independent and normally distributed | ||
| Clinical Outcome | Customized based on clinical tolerance [68] | Medical testing, diagnostic applications | Error significance depends on medical decision points |
Experimental Protocols for Uncertainty Component Estimation
Quantifying Random Error (Precision)
Random error is quantified through precision studies, which should encompass both repeatability and intermediate precision as recommended by ICH guidelines [3]. The experimental protocol involves:
Repeatability (Intra-assay Precision): Perform a minimum of six replicate determinations at 100% of the test concentration or nine determinations across three concentration levels covering the specified range (e.g., three concentrations with three replicates each) [3]. Results are typically reported as % relative standard deviation (%RSD), with acceptance criteria often set at ≤2% for chromatographic methods [2].
Intermediate Precision: Demonstrate the agreement between results from within-laboratory variations due to random events, such as different days, analysts, or equipment [3]. An experimental design should be implemented so that the effects of individual variables can be monitored. This is typically generated by two analysts who prepare and analyze replicate sample preparations using different HPLC systems, with results reported as %RSD [3].
The standard deviation for repeatability (Sr) can be calculated using the formula: Sr = √[Σ(Xdi - X̄d)² / D(n-1)], where Xdi represents individual replicate results per day, X̄d is the average of all results for day d, D is the total number of days, and n is the total number of replicates per day [1].
Quantifying Systematic Error (Bias)
Systematic error is assessed through accuracy and trueness studies using several methodological approaches:
Recovery Studies: Fortify known amounts of analyte into real samples and aim for 95-105% recovery [2]. The data should be collected from a minimum of nine determinations over a minimum of three concentration levels covering the specified range, reported as the percent recovery of the known, added amount [3].
Comparison to Reference Materials: Analyze certified reference materials (CRMs) or quality control materials with assigned values [1]. The verification interval can be calculated as X ± 2.821√(Sx² + Sa²), where X is the mean of the tested reference material, Sx is the standard deviation of the tested reference material, and Sa is the uncertainty of the assigned reference material [1].
Method Comparison Studies: Compare results with those from a reference method using linear regression analysis (Y = a + bX), where the y-intercept (a) indicates constant systematic error and the slope (b) indicates proportional systematic error [1].
Systematic error is detected by linear regression analysis, with the y-intercept of the linear regression curve indicating constant error while the slope indicates proportional error [1].
Workflow for Combined Uncertainty Calculation
The following diagram illustrates the systematic workflow for calculating combined uncertainty in single-laboratory method validation:
Uncertainty Calculation Workflow
Advanced Applications in Pharmaceutical Method Validation
Uncertainty Based on Current Information (UBCI) Model
A significant advancement in uncertainty estimation for pharmaceutical analysis is the Uncertainty Based on Current Information (UBCI) model, which provides real-time assessment of method performance characteristics using information extracted from individual chromatograms [69]. This approach recognizes that method execution always occurs under specific circumstances, and uncertainty about generated results must account for both operational conditions and hardware performance [69].
The UBCI model expresses performance characteristics as a function of signal and noise levels, hardware specifications, and software settings, providing an opportunity for "live validation" of test results [69]. This dynamic assessment addresses the limitation of historical validation data, which may not fully reflect current experimental conditions due to hardware differences or changes in analyst skill levels over time [69]. Implementation of UBCI can streamline qualification and validation studies by providing concurrent assessment of measurement uncertainty, potentially mitigating challenges associated with conventional method validation [69].
Lifecycle Management and Revalidation Triggers
Uncertainty estimation is not a one-time exercise but requires ongoing management throughout the method lifecycle [2]. A robust uncertainty management plan should include:
- Periodic Reviews: Schedule annual check-ins or tie reviews to major instrument service events [2].
- Change Control: Revalidate impacted parameters when introducing new lots of critical reagents, software upgrades, or shifts in key SOP steps [2].
- Control Charts: Implement statistical control charts (e.g., X̄-R charts) to monitor ongoing performance and detect subtle drifts before they trigger formal revalidation [2].
- Method Transfer Protocols: When shifting validated methods between labs or instruments, draft transfer plans comparing critical parameters and confirm equivalency through parallel testing [2].
The following diagram illustrates the relationship between different uncertainty components and their combined contribution to the final measurement result:
Uncertainty Components Relationship
Essential Research Reagents and Materials for Uncertainty Studies
Table 3: Essential Research Reagents and Materials for Uncertainty Estimation Studies
| Reagent/Material | Function in Uncertainty Studies | Application Examples |
|---|---|---|
| Certified Reference Materials (CRMs) | Provide traceable standards with assigned values and uncertainties for systematic error quantification [1] [66] | Accuracy determination, method validation, calibration verification |
| Quality Control Materials | Monitor method performance over time, contributing to precision estimates [1] | Daily quality control, precision monitoring, trend analysis |
| High-Purity Analytical Standards | Enable preparation of calibration standards for linearity studies and detection limit determination [70] | Calibration curve preparation, LOD/LOQ studies, linearity assessment |
| Matrix-Matched Calibration Standards | Account for matrix effects that contribute to method uncertainty [70] | Recovery studies, accuracy assessment in complex matrices |
| Internal Standards | Correct for analytical variability, reducing random error components [70] | GC-MS and LC-MS analyses, normalization of instrument response |
The integration of random and systematic error components provides a comprehensive framework for estimating measurement uncertainty in single-laboratory method validation. By implementing systematic protocols for precision and accuracy determination, selecting appropriate mathematical models for error combination, and maintaining ongoing surveillance of method performance throughout its lifecycle, researchers and drug development professionals can ensure the reliability and fitness-for-purpose of their analytical methods. The advancing methodology in uncertainty estimation, including dynamic approaches like UBCI, continues to enhance our ability to provide meaningful uncertainty statements that support robust decision-making in pharmaceutical development and quality control.
Leveraging Reference Methods and Certified Reference Materials for Bias Assessment
In the framework of single-laboratory method validation (SLV), the assessment of bias—the difference between the expected test result and an accepted reference value—is a fundamental requirement for establishing method accuracy [1]. Bias represents a systematic error that can compromise the reliability of analytical data, leading to incorrect scientific conclusions and decisions in drug development [1]. Within the SLV context, where resources for full multi-laboratory collaborative trials may be limited, Certified Reference Materials (CRMs) and validated reference methods provide a practical foundation for conducting this critical assessment [71] [72].
Bias can manifest as either constant or proportional error [1]. Constant bias is unaffected by analyte concentration, while proportional bias changes with concentration levels, making its detection dependent on assessing multiple points across the method's range [1]. The primary objective of bias assessment is to quantify this deviation and ensure it falls within the total allowable error (TEa) based on medical or analytical requirements [1]. This guide details the strategic use of reference methods and CRMs to perform rigorous, defensible bias evaluation within a single-laboratory setting.
Theoretical Foundations of Bias and Analytical Accuracy
Distinguishing Between Types of Measurement Error
Understanding the distinction between random and systematic error is crucial for effective bias assessment.
- Random Error: This error varies unpredictably between repeated measurements and is quantified as imprecision through parameters like standard deviation (SD) and coefficient of variation (CV) [1]. It causes a scatter of results around the mean value but does not represent a consistent directional shift.
- Systematic Error (Bias): This represents a consistent directional deviation from the true value and is the focal point of bias assessment. It can be further categorized as:
- Constant Bias: The magnitude of error remains consistent regardless of analyte concentration, often identified by a non-zero y-intercept in regression analysis [1].
- Proportional Bias: The magnitude of error changes in proportion to the analyte concentration, detectable as a slope deviation from 1 in regression analysis [1].
Systematic errors typically arise from calibration problems, such as impure or unstable calibration materials, improper standard preparation, or inadequate calibration procedures [1]. Unlike random errors, which can be reduced through repeated measurements, systematic errors require correction of their fundamental causes to eliminate their effect [1].
The Role of Reference Materials in Metrological Traceability
Certified Reference Materials (CRMs) provide the crucial link that establishes metrological traceability in chemical measurements [71]. A CRM is defined as a "reference material characterized by a metrologically valid procedure for one or more specified properties, accompanied by an RM certificate that provides the value of the specified property, its associated uncertainty, and a statement of metrological traceability" [71].
In practice, CRMs serve as verification tools that help laboratories demonstrate the trueness of their measurements by comparing their results against a certified value with known uncertainty [71] [72]. This is particularly valuable in SLV, where a laboratory must independently verify its method performance without extensive interlaboratory comparisons.
Certified Reference Materials: Selection and Application
Types of Reference Materials and Their Appropriate Use
The terminology for reference materials follows international standards to ensure precise communication and application:
- Reference Material (RM): A "material, sufficiently homogeneous and stable for one or more specified properties, which has been established to be fit for its intended use in a measurement process" [71].
- Certified Reference Material (CRM): A subclass of RMs with properties certified by a metrologically valid procedure, accompanied by documentation that provides the certified value, its associated uncertainty, and a statement of metrological traceability [71].
For bias assessment, matrix-based CRMs are particularly valuable as they account for analytical challenges such as extraction efficiency and interfering compounds that may be present in real samples [71]. While an exact matrix-matched CRM is ideal, the limited availability of such materials means that analysts must often use CRMs that represent similar analytical challenges rather than identical matrices [71].
Strategic Implementation of CRMs for Bias Assessment
The process for using CRMs to assess bias involves a structured experimental approach:
- CRM Selection: Identify a CRM with a matrix similar to routine test samples and with analyte concentrations relevant to the method's measuring range [71]. The certified value should have uncertainty statements that meet the laboratory's requirements.
- Experimental Design: Analyze the CRM a minimum of six times across multiple independent assay runs to account for random variation [2] [3]. These analyses should be performed by different analysts on different days whenever possible to incorporate realistic laboratory variation into the assessment.
- Calculation of Bias: Calculate the percentage difference between the mean value obtained by the laboratory and the certified value using the formula for trueness assessment (Equation 4, Table 1) [1].
- Statistical Evaluation: Compare the calculated bias against predefined acceptance criteria, typically derived from the total allowable error (TEa) based on clinical or analytical requirements [1]. The verification interval should account for both the uncertainty of the tested reference material and the certified value's uncertainty.
Table 1: Key Equations for Bias and Uncertainty Assessment
| Parameter | Equation Number | Formula | Application |
|---|---|---|---|
| Systematic Error (Regression) | 2 | (Y = a + bX)(a = \frac{(\sum y)(\sum x^2) - (\sum y)(\sum xy)}{n(\sum x^2) - (\sum x)^2})(b = \frac{n(\sum xy) - (\sum x)(\sum y)}{n(\sum x^2) - (\sum x)^2}) | Constant error (y-intercept), proportional error (slope) [1] |
| Trueness (Bias) Verification | 4 | Verification interval = (X \pm 2.821\sqrt{Sx^2 + Sa^2}) | Compare result vs. certified value, accounting for uncertainty [1] |
| Measurement Uncertainty | 8C | (Uc = \sqrt{Us^2 + U_B^2}) | Combine imprecision (random) and bias (systematic) uncertainty [1] |
CRM Bias Assessment Workflow
Reference Method Comparison for Bias Assessment
Establishing Comparative Experiments
When suitable CRMs are unavailable or limited, bias assessment can be performed through comparison with a validated reference method [3] [11]. This approach involves analyzing a set of patient samples or test materials covering the analytical measurement range using both the new test method and the established reference method.
The experimental design should include:
- A minimum of 40 samples distributed across the reportable range, with concentrations that cover low, medium, and high levels [1].
- Samples should represent the typical matrix encountered in routine testing, preferably patient specimens rather than spiked samples whenever possible.
- Analysis should be performed within a timeframe that ensures sample stability, typically with both methods analyzing each sample in duplicate within the same analytical run or within closely timed runs.
Statistical Analysis of Method Comparison Data
The data from method comparison studies should be analyzed using both regression statistics and difference plots (Bland-Altman plots):
- Linear Regression: Provides information about both constant (intercept) and proportional (slope) bias [1]. The ideal scenario is a slope of 1 and an intercept of 0, indicating no proportional or constant bias between methods.
- Bland-Altman Plot: Visualizes the difference between methods against their average, helping identify concentration-dependent bias and outliers [1].
The standard error of estimate (Sy/x) represents the random error around the regression line and is calculated using Equation 1 from Table 1 [1]. A higher Sy/x indicates greater scatter and higher random error in the measurement comparison.
Table 2: Method Validation Parameters for Bias Assessment
| Parameter | Definition | Acceptance Criteria Examples | Role in Bias Assessment |
|---|---|---|---|
| Accuracy | Closeness of agreement between measured value and true value [3] [11] | 95-105% recovery of known amount [2] | Direct measure of bias through recovery studies |
| Precision | Closeness of agreement between independent measurements [3] | %RSD ≤2% for repeatability [2] | Must be established before meaningful bias assessment |
| Specificity | Ability to measure analyte accurately in presence of interferences [3] | Resolution of closely eluted compounds [3] | Ensures bias is not caused by interfering substances |
| Linearity | Ability to obtain results proportional to analyte concentration [3] [11] | r² ≥ 0.99 [2] [11] | Assesses proportional bias across analytical range |
Integrated Experimental Protocols for Comprehensive Bias Evaluation
Protocol 1: CRM-Based Bias Assessment
This protocol provides a detailed methodology for using Certified Reference Materials to quantify methodological bias:
Materials and Reagents:
- Certified Reference Material with documented uncertainty
- Appropriate calibrators and quality controls
- All necessary solvents and reagents of documented purity
Experimental Procedure:
- Allow the CRM to equilibrate to room temperature and homogenize according to manufacturer instructions.
- Prepare the CRM according to the standard operating procedure of the method being validated.
- Analyze the CRM in six independent replicates over at least three different analytical runs by two different analysts if possible.
- Include appropriate calibration curves and quality control samples in each run as per routine laboratory protocol.
- Record all results with appropriate metadata including date, analyst, instrument, and reagent lots.
Data Analysis:
- Calculate the mean and standard deviation of the results.
- Determine the percentage bias using the formula: [(Mean Result - Certified Value) / Certified Value] × 100.
- Calculate the verification interval using Equation 4 (Table 1) to account for measurement uncertainty [1].
- Verify that the certified value falls within the verification interval, indicating no significant bias.
Acceptance Criteria:
- The calculated bias should be less than the established total allowable error (TEa) for the analyte.
- The certified value should fall within the verification interval calculated from the laboratory's results.
Protocol 2: Reference Method Comparison for Bias Assessment
This protocol outlines the procedure for evaluating bias through comparison with a validated reference method:
Materials and Reagents:
- 40 patient samples covering the analytical measurement range
- All reagents and materials for both test method and reference method
- Calibrators and quality controls for both methods
Experimental Procedure:
- Select and aliquot patient samples to ensure concentration distribution across the reportable range.
- Analyze all samples using both the test method and reference method in random order to avoid systematic bias.
- Perform all analyses within the stability period of the samples.
- Ensure both methods are operated by competent analysts following established protocols.
- Record all results with appropriate identification to maintain sample-to-method correspondence.
Data Analysis:
- Perform linear regression analysis with the reference method as the independent variable (x) and the test method as the dependent variable (y).
- Calculate the slope and y-intercept with their confidence intervals.
- Generate a Bland-Altman plot by graphing the difference between methods against their average values.
- Calculate the standard error of estimate (Sy/x) using Equation 1 (Table 1) [1].
Acceptance Criteria:
- The slope confidence interval should include 1.0, indicating no proportional bias.
- The y-intercept confidence interval should include 0, indicating no constant bias.
- The Bland-Altman plot should show no obvious concentration-dependent trend in differences.
Bias Assessment Strategy Selection
Research Reagent Solutions for Bias Assessment
Table 3: Essential Research Reagents for Bias Assessment
| Reagent Solution | Technical Function | Application Context |
|---|---|---|
| Matrix-Matched CRMs | Provides matrix-specific certified values for trueness verification [71] | Quantifying bias in complex sample matrices (e.g., food, botanicals, biological fluids) |
| Calibrator CRMs | Pure substance CRMs with documented purity and uncertainty [71] | Establishing metrological traceability in calibration curves |
| Stable Isotope-Labeled Internal Standards | Compensates for analyte loss and matrix effects in MS-based methods [72] | Improving accuracy in mass spectrometric analyses |
| Spiked Matrix Materials | Laboratory-prepared materials with known added analyte [11] | Assessing recovery and bias when CRMs are unavailable |
| Method Comparison Panels | Well-characterized patient sample panels | Evaluating bias relative to reference methods across clinical range |
Documentation and Compliance in Bias Assessment
Essential Documentation Elements
Comprehensive documentation is critical for demonstrating the validity of bias assessment in SLV. The following elements should be included in the validation report:
- Reference Material Certification: Provide complete documentation of CRM certificates, including certified values, uncertainties, and traceability statements [71].
- Experimental Design: Document the number of replicates, analysis sequence, personnel involved, and instrumentation used [2].
- Raw Data: Maintain all primary data, including chromatograms, spectra, or instrumental readouts with appropriate metadata [2].
- Statistical Analysis: Include all calculations, regression analyses, and graphical representations with clear interpretation [2] [1].
- Acceptance Criteria Justification: Provide rationale for selected acceptance criteria based on regulatory guidance, clinical requirements, or analytical state-of-the-art [1].
Managing Measurement Uncertainty
Bias assessment directly contributes to the estimation of measurement uncertainty, a key requirement for accredited laboratories [1]. The combined standard uncertainty (Uc) incorporates both random (imprecision) and systematic (bias) components using Equation 8C (Table 1) [1]. Properly evaluated bias, along with its uncertainty, should be incorporated into the overall measurement uncertainty budget for the validated method.
Effective bias assessment using Certified Reference Materials and reference methods forms the cornerstone of reliable single-laboratory method validation. Through the strategic application of the protocols and principles outlined in this guide, researchers and drug development professionals can produce defensible data with established metrological traceability. The rigorous assessment and documentation of bias not only fulfills regulatory and accreditation requirements but also strengthens the scientific validity of research outcomes, ultimately supporting the development of safe and effective pharmaceutical products.
Establishing Method Equivalency and Preparing for Successful Tech Transfer
Method transfer and equivalency establishment are critical pharmaceutical quality assurance processes, ensuring that analytical methods produce equivalent results when transferred from a sending laboratory (transferring unit) to a receiving laboratory (receiving unit). The fundamental goal is to guarantee that the receiving laboratory can reproduce the same results as the transferring laboratory, thereby ensuring the quality, safety, and efficacy of medicines despite differences in personnel, equipment, and environmental conditions [73]. Health regulators frequently require these processes for external testing sites and stability studies [73].
Within the broader context of Single-Laboratory Validation (SLV) research, method transfer acts as a practical extension. SLV establishes method validity within one laboratory, while method transfer verifies this validity across multiple laboratories. The Interstate Shellfish Sanitation Conference (ISSC) emphasizes this relationship by providing specific SLV protocols for submitting methods for approval, demonstrating how foundational SLV research supports subsequent multi-laboratory application [42]. The growing adoption of Digital Validation Tools (DVTs), used by 58% of organizations in 2025, is enhancing this process by centralizing data, streamlining workflows, and supporting continuous audit readiness [74].
Core Approaches to Analytical Method Transfer
Regulatory guidelines, such as those outlined in USP 〈1224〉, recognize three primary approaches for transferring analytical methods. The selection depends on the method's development and validation status, the receiving laboratory's involvement, and the specific project requirements [73] [75].
Table 1: Approaches for Analytical Method Transfer
| Approach | Description | Best Use Cases |
|---|---|---|
| Comparative Transfer [73] [75] | A predetermined number of samples are analyzed by both the sending and receiving units. Results are compared using acceptance criteria derived from method validation data, often from intermediate precision or reproducibility studies. | Methods already validated at the transferring laboratory or by a third party [73] [75]. |
| Co-validation [73] [75] | The receiving unit participates as part of the validation team during the method's initial validation. This includes the receiving laboratory in reproducibility testing from the outset. | Methods transferred from a development site to a commercial site before full validation is complete [73] [75]. |
| Revalidationor Partial Revalidation [73] [75] | The method undergoes a full or partial revalidation at the receiving unit. Partial revalidation evaluates only the parameters affected by the transfer, with accuracy and precision being typical. | The original sending lab is not involved, or the original validation was not performed according to ICH requirements and requires supplementation [73] [75]. |
In specific, justified cases, a formal method transfer can be waived. Common waivers apply to compendial methods (which require verification but not formal transfer), transfers of general methods (e.g., weighing) to familiar labs, and scenarios where the personnel responsible for the method move to the new site [75].
Designing the Transfer Experiment and Protocol
A successful transfer hinges on a meticulously designed and documented protocol. This document, typically drafted by the transferring laboratory, serves as the project's blueprint and must be agreed upon by all parties [75].
Key Protocol Components
A comprehensive method transfer protocol should include the following elements [75]:
- Objective and Scope: Clearly defines the purpose and boundaries of the transfer.
- Responsibilities: Outlines the requirements and duties of both the sending and receiving units.
- Materials and Instruments: Specifies all equipment, reagents, and reference standards to be used.
- Analytical Procedure: Provides the detailed, step-by-step method.
- Experimental Design: Describes the number of samples, replicates, and the statistical approach for comparison.
- Acceptance Criteria: Defines the pre-defined, justified criteria for determining a successful transfer.
Defining Statistical Acceptance Criteria
Acceptance criteria should be based on the method's validation data, particularly reproducibility, and must respect ICH requirements [75]. While criteria are method-specific, some typical examples are used in the industry.
Table 2: Typical Acceptance Criteria for Method Transfer
| Test | Typical Acceptance Criteria |
|---|---|
| Identification | Positive (or negative) identification is obtained at the receiving site [75]. |
| Assay | The absolute difference between the results from the two sites is not more than (NMT) 2-3% [75]. |
| Related Substances | Criteria vary by impurity level. For low levels, recovery of 80-120% for spiked impurities may be used. For impurities above 0.5%, an absolute difference requirement is typical [75]. |
| Dissolution | Absolute difference in mean results is NMT 10% at time points when <85% is dissolved, and NMT 5% when >85% is dissolved [75]. |
The following workflow diagram outlines the key stages of the transfer process, from initiation to final reporting.
Experimental Protocols for Key Validation Parameters
The experimental design for a method transfer must demonstrate that the receiving laboratory can meet the method's performance characteristics. The ISSC Single Laboratory Validation (SLV) protocol requires analyses to determine several key parameters, providing a robust framework for establishing equivalency [76].
Accuracy and Precision (Trueness)
Objective: To demonstrate that the receiving laboratory's results are both accurate (close to the true value) and precise (repeatable).
Methodology:
- Analysis of Spiked Samples: Prepare a series of samples spiked with known concentrations of the analyte as required by the SLV protocol [76].
- Joint Testing: Both laboratories analyze a predetermined number of samples from homogeneous lots. A common approach is for each lab to analyze a minimum of six sample determinations from a single batch [75].
- Data Analysis: Calculate the mean, standard deviation (SD), and relative standard deviation (RSD) for results from each laboratory. Compare the mean values between laboratories for accuracy/trueness and the RSD for precision. The absolute difference between the mean values is often evaluated against pre-defined criteria (e.g., NMT 2-3% for an assay) [75].
Specificity
Objective: To prove that the method can unequivocally assess the analyte in the presence of other components, such as impurities or matrix elements.
Methodology:
- For chromatographic methods, analyze blank samples (placebos) and samples containing the analyte. Demonstrate that the analyte peak is pure and free from interference from other peaks at the retention time of the analyte.
- This is a critical parameter for methods transferred for testing complex matrices, such as in the harmonization project for DSP toxins in different shellfish species [76].
Limit of Detection (LOD) and Limit of Quantitation (LOQ)
Objective: To verify the lowest levels of analyte that can be detected and reliably quantified by the receiving laboratory.
Methodology:
- Based on the SLV protocol, the receiving laboratory performs analyses on samples with progressively lower analyte concentrations.
- LOD is typically determined as the concentration that gives a signal-to-noise ratio of 3:1.
- LOQ is typically determined as the concentration that gives a signal-to-noise ratio of 10:1 and can be quantified with acceptable precision and accuracy (e.g., RSD < 20% and recovery of 80-120%).
Linearity and Range
Objective: To verify that the receiving laboratory's analytical procedure produces results that are directly proportional to analyte concentration within a specified range.
Methodology:
- Prepare and analyze a minimum of five concentrations across the specified range of the method (e.g., 50% to 150% of the target concentration).
- Plot the response against the concentration and perform linear regression analysis. The correlation coefficient (r), y-intercept, and slope of the line are evaluated against pre-defined acceptance criteria.
Ruggedness
Objective: To evaluate the method's reliability under normal, but varied, conditions of operation, such as different analysts, days, or equipment.
Methodology:
- The transfer itself is a ruggedness test, as it involves different laboratories with different analysts and equipment.
- The comparison of results from the sending and receiving units, often using criteria from validation studies on intermediate precision, directly assesses the method's ruggedness [75].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method transfer relies on high-quality, well-characterized materials. The following table details key reagents and their critical functions in ensuring a smooth and successful process.
Table 3: Essential Materials for Analytical Method Transfer
| Item | Function & Importance |
|---|---|
| Certified Reference Standards | Well-characterized materials used to calibrate instruments and validate method accuracy. Their quality and traceability are paramount for generating comparable data [75]. |
| Characterized Reagents | Reagents with known purity and performance specifications. Sharing sources and batches between labs minimizes a major source of variability [75]. |
| Stable, Homogeneous Sample Lots | Uniform sample materials are essential for a meaningful comparison. Using a single, homogeneous lot for all testing at both sites is a best practice [75]. |
| System Suitability Test (SST) Materials | Specific preparations used to verify that the chromatographic or other analytical system is operating correctly before and during analysis. SST criteria must be consistently met by both labs [73]. |
Critical Success Factors and Common Challenges
Beyond the technical protocol, several managerial and communication-focused factors are crucial for success.
- Proactive Communication and Knowledge Transfer: Open communication is the most important non-technical factor [75]. This begins with introducing the teams and establishing a direct line between analytical experts. The sending laboratory must share all relevant data and, crucially, the tacit "silent knowledge" not found in written procedures, such as practical tips and troubleshooting experience [75].
- Building Method Robustness: The success of the transfer depends on consistent results. The transferring laboratory must develop robust analytical methods that account for variables like instrument differences and operator skill [73]. A collaborative process, including joint review of method requirements and instrumentation, helps build this robustness [73].
- Clear, Unambiguous Documentation: Documentation must use clear language that allows for only a single interpretation [73]. Highly detailed procedures and strict parameters help generate consistent results regardless of the scientist's technical skill level, preventing subjective interpretation of instructions [73].
- Risk-Based Approach: A successful transfer involves identifying factors that could affect results (e.g., infrastructure, method complexity, skill sets) and planning how to mitigate them [73]. The sending laboratory should share any prior risk assessments to guide the receiving laboratory's preparations.
Establishing method equivalency through a well-executed technology transfer is a foundational activity in regulated industries. It bridges the gap between single-laboratory validation and the reliable application of analytical methods across the global supply chain. By selecting the appropriate transfer strategy, executing a rigorous experimental protocol based on SLV principles, and fostering robust collaboration and communication between laboratories, organizations can ensure the continued quality of their products and maintain a state of audit readiness in an increasingly complex regulatory landscape.
Conclusion
Single Laboratory Validation is not a one-time exercise but a fundamental component of a sustainable quality culture. Mastering the fundamentals of SLV, from rigorous planning and execution to thorough statistical analysis and troubleshooting, empowers laboratories to generate reliable, defensible data. This directly translates to robust product development, regulatory compliance, and ultimately, ensured patient safety. The future of SLV will continue to evolve with regulatory expectations, increasingly integrating lifecycle management and digital data integrity tools. A solid foundation in these principles positions scientists and laboratories to adapt and excel, turning analytical data into a trusted asset for biomedical and clinical research.
References
- 1. Verification of quantitative analytical methods in medical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8199534/]
- 2. Laboratory Validation Method: From Basics to Best Practices [https://zamann-pharma.com/2025/04/29/laboratory-validation-method-from-basics-to-best-practices/]
- 3. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 4. USP <1225> Revised: Aligning Compendial Validation with ... [https://investigationsquality.com/2025/11/13/usp-1225-revised-aligning-compendial-validation-with-ich-q2r2-and-q14s-lifecycle-vision/]
- 5. ICH Q2(R1) Validation of Analytical Procedures [https://www.gmp-compliance.org/guidelines/gmp-guideline/ich-q2r1-validation-of-analytical-procedures-text-and-methodology]
- 6. 3 Key Regulatory Guidelines for Method Validation [https://altabrisagroup.com/regulatory-guidelines-for-method-validation/]
- 7. FDA Issues Final Guidance on Analytical Testing for ... [https://www.fda.gov/tobacco-products/ctp-newsroom/fda-issues-final-guidance-analytical-testing-industry-use-tobacco-product-applications]
- 8. Key Principles of USP Compendial Method Validation [https://altabrisagroup.com/usp-1225-compendial-method-validation/]
- 9. Proposed Revision of USP <1225> Published in the ... [https://www.gmp-compliance.org/gmp-news/proposed-revision-of-usp-1225-published-in-the-pharmacopeial-forum]
- 10. Method Validation vs Method Verification: Which is Better ... [https://www.labmanager.com/method-validation-vs-method-verification-which-is-better-for-use-in-laboratories-33982]
- 11. Introduction to Analytical Method Validation [https://lab-training.com/introduction-to-analytical-method-validation/]
- 12. Glossary of Terms Related to Chromatographic Method ... [https://www.chromatographyonline.com/view/glossary-terms-related-chromatographic-method-validation]
- 13. Method Validation and Robustness | LCGC International [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 14. What are the differences and key steps in Analytical ... [https://resources.eirgenix.com/blog/method_dev_qual_validation]
- 15. The Importance of Method Selection in Determining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4785475/]
- 16. Flawed records, flawed outcomes: why data integrity is key ... [https://mbihealth.com/insights/article/flawed-records-flawed-outcomes/]
- 17. Data Accuracy vs. Data Integrity: Similarities and Differences [https://www.ibm.com/think/topics/data-accuracy-vs-data-integrity]
- 18. Data Integrity vs Data Validity: Proving They Are Different [https://atlan.com/data-integrity-vs-data-validity/]
- 19. Patient Safety & Pharmacovigilance [https://www.sanofi.com/en/patients/patient-engagement/patient-safety-at-sanofi]
- 20. Pharmacovigilance as a tool for safety and monitoring [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636760/]
- 21. Harmonised guidelines for single-laboratory validation [https://www.oiv.int/index.php/standards/compendium-of-international-methods-of-wine-and-must-analysis/annex-e/annex-e-laboratory-quality-assurance/harmonised-guidelines-for-single-laboratory-validation]
- 22. Method validation and method verification - Introduction - ISO [https://committee.iso.org/sites/tc34sc9/home/essential-information/content-left-area/validation-of-methods/method-validation-and-method-ver.html]
- 23. Single Laboratory Validation [https://pathologyuncertainty.com/single-laboratory-validation/]
- 24. Single Lot vs. Full Validation of Minimum Sterilization Dose [https://www.steris-ast.com/resources/techtips/radiation-dose-setting-single-lot-vs-full-validation-of-minimum-sterilization-dose]
- 25. Laboratory Validation Method: From Basics to Best Practices [https://www.linkedin.com/pulse/laboratory-validation-method-from-basics-best-practices-4e44f]
- 26. The Fitness for Purpose of Analytical Methods (2025) [https://www.eurachem.org/index.php/3-publications/guides/144-gdmv2014]
- 27. Analytical Method Validation: Back to Basics, Part I [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 28. Laboratory Method Validation - Foundational Course [https://pharmuni.com/courses/43/laboratory-method-validation-foundational-course]
- 29. New edition of CLSI EP46: best practices for determining ... [https://www.westgard.com/essays/guest-essay/paulo-pereira-ep46.html]
- 30. Analytical performance evaluation of intelligent quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12162070/]
- 31. 2025 IFCC Recommendations for IQC [https://www.westgard.com/essays/quality-requirements-and-standards/ifcc-iqc-2025.html]
- 32. The QA/QC Blueprint: Ensuring Trust, Compliance, and ... [https://www.labmanager.com/the-qa-qc-blueprint-ensuring-trust-compliance-and-reproducibility-in-the-modern-laboratory-34423]
- 33. Quality services frequently asked questions [https://www.theiia.org/en/group-services/quality-assurance/quality-services/faq/]
- 34. 2025 Great Global QC Survey Results: The whole world [https://www.westgard.com/qc-applications/basic-qc-practices/2025-global-qc-survey.html]
- 35. Determination and Validation of a Single Laboratory ... [https://www.chromatographyonline.com/view/determination-and-validation-single-laboratory-method-coenzyme-q10-ubiquinone-uhplc]
- 36. Specimen integrity: How errors occur and the role ... [https://www.cardinalhealth.com/en/product-solutions/medical/laboratory-products/specimen-collection/specimen-integrity-resources/specimen-integrity-how-errors-occur.html]
- 37. Pre-analytical pitfalls: Missing and mislabeled specimens [https://psnet.ahrq.gov/web-mm/pre-analytical-pitfalls-missing-and-mislabeled-specimens]
- 38. Effectiveness of Laboratory Practices to Reducing Patient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5701285/]
- 39. Analytical Method Validation: A Recipe for Accurate Results [https://certified-laboratories.com/blog/analytical-method-validation-a-recipe-for-accurate-results/]
- 40. 5 Common Mistakes in Defining Acceptance Criteria for MSA [https://www.roi-ally.com/index.php/en/blog/5-common-mistakes-in-defining-acceptance-criteria-for-msa]
- 41. How to Avoid Pitfalls in Acceptance Criteria [https://www.linkedin.com/advice/3/what-some-common-pitfalls-avoid-when-3c]
- 42. Single Lab Validation for Laboratory Methods | Interstate Shellfish Sanitation Conference [https://www.issc.org/single-lab-validation-laboratory-methods]
- 43. Contribution of solid–liquid–vapor interface to droplet ... [https://www.sciencedirect.com/science/article/abs/pii/S0927775722021744]
- 44. Preparation for blood tests: what can go wrong before the ... [https://australianprescriber.tg.org.au/articles/preparation-for-blood-tests-what-can-go-wrong-before-the-sample-reaches-the-lab.html]
- 45. Method Validation [https://www.eurachem.org/index.php/mnu-tsk-mv]
- 46. Sample Management: Recommendation for Best Practices ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4779093/]
- 47. Specimen Stability Considerations During Flow Cytometry ... [https://blog.td2inc.com/specimen-stability-considerations]
- 48. Study of the Stability of Various Biochemical Analytes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5015491/]
- 49. Study of specimen stability in clinical laboratories [https://jbpml.org.br/study-of-specimen-stability-in-clinical-laboratories-ensuring-quality-of-results-and-patients-safety-2/]
- 50. Compensate for or Minimize Matrix Effects? Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412464/]
- 51. A Pragmatic Approach to Managing Interferences in ICP-MS [https://www.spectroscopyonline.com/view/pragmatic-approach-managing-interferences-icp-ms]
- 52. Managing Matrix Interference in Immunoassays: Tips and ... [https://www.bio-connect.nl/news/managing-matrix-interference-in-immunoassays-tips-and-solutions/]
- 53. 14 Comparing quantitative data between individuals [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 54. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 55. Quality by Design (QBD): An approach in Analytical ... [https://www.ijpsjournal.com/article/Quality+by+Design+QBD+An+approach+in+Analytical+Method+Development]
- 56. Aspects and Implementation of Pharmaceutical Quality by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114689/]
- 57. The Application of Quality by Design to Analytical Methods [https://www.pharmtech.com/view/application-quality-design-analytical-methods]
- 58. A Beginner's Guide to Quality by Design (QbD) for HPLC ... [https://www.sepscience.com/a-beginners-guide-to-quality-by-design-qbd-for-hplc-method-development-11307]
- 59. Quality by design approach: Regulatory need [https://arabjchem.org/quality-by-design-approach-regulatory-need/]
- 60. Basic Method Validation, 3rd Edition, FAQs [https://www.westgard.com/resources/resources/bmv3edfaqs.html]
- 61. Understanding Bland Altman analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4470095/]
- 62. Understanding Diagnostic Plots for Linear Regression Analysis [http://library.virginia.edu/data/articles/diagnostic-plots]
- 63. Top 6 Visualizations for Quantitative Analysis Methods Data [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 64. Random vs. Systematic Error | Definition & Examples [https://www.scribbr.com/methodology/random-vs-systematic-error/]
- 65. Method Validation - the Real World Applications [https://www.westgard.com/qc-applications/method-validation-qc/qcapp14.html]
- 66. Uncertainty of Measurement in Quantitative Medical Testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC1934961/]
- 67. Measurements and Error Analysis [https://www.webassign.net/question_assets/unccolphysmechl1/measurements/manual.html]
- 68. Models for combining random and systematic errors. assumptions and consequences for different models - PubMed [https://pubmed.ncbi.nlm.nih.gov/11522103/]
- 69. Uncertainty Estimates of Purity Measurements Based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3497960/]
- 70. Method validation and measurement uncertainty of possible ... [https://jast-journal.springeropen.com/articles/10.1186/s40543-020-00242-6]
- 71. The Importance of Reference Materials and Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8713974/]
- 72. The Benefits of Including Certified Reference Materials in a ... [https://www.chromatographyonline.com/view/benefits-including-certified-reference-materials-collaborative-trial]
- 73. Best Practices for Transferring Analytical Methods [https://www.jmolner.com/post/transferring-analytical-methods]
- 74. Validation in Transition: Why 2025 is the Turning Point for ... [https://ispe.org/pharmaceutical-engineering/ispeak/validation-transition-why-2025-turning-point-industry]
- 75. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 76. Harmonizing Methods to Determine Diarrhetic Shellfish ... [https://coastalscience.noaa.gov/project/harmonizing-methods-to-determine-diarrhetic-shellfish-poisoning-toxins-for-improved-shellfish-safety/]