Protocols for Assessing Nutrient Bioavailability: From Foundational Concepts to Advanced Predictive Models
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the established and emerging protocols for assessing nutrient bioavailability.
Protocols for Assessing Nutrient Bioavailability: From Foundational Concepts to Advanced Predictive Models
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the established and emerging protocols for assessing nutrient bioavailability. It covers the foundational principles defining bioavailability and bioaccessibility, explores the full spectrum of in vivo and in vitro methodologies, and addresses critical troubleshooting factors such as anti-nutrients and food matrix effects. Furthermore, it details the development and validation of predictive algorithms for iron, zinc, and vitamins, enabling a comparative analysis of method efficacy and translation to clinical and biomedical research outcomes.
Defining Bioavailability: Core Principles and Influencing Factors
What is Nutrient Bioavailability? A Review of Key Definitions (Bioavailability vs. Bioaccessibility)
In nutritional science, simply consuming a nutrient does not guarantee its utilization by the body. The concepts of bioaccessibility and bioavailability are critical for understanding the journey of a dietary compound from ingestion to its final physiological use. These terms are foundational for researchers designing experiments, developing functional foods, and formulating drugs or supplements.
The sequential relationship from ingestion to physiological effect can be defined as follows [1] [2]:
- Bioaccessibility refers to the fraction of a compound that is released from its food matrix into the gastrointestinal lumen and thus becomes accessible for intestinal absorption. This process involves digestion in the mouth, stomach, and intestinal lumen, making the nutrient available for uptake by intestinal epithelial cells [1].
- Bioavailability is the proportion of an ingested nutrient that is absorbed, becomes available for physiological functions, and is stored or utilized by the body [3] [4]. From a pharmacological perspective, it can be defined as the rate and extent to an administered drug or bioactive compound that reaches the systemic circulation [1] [5].
It is crucial to distinguish this from bioactivity, which represents the specific biological effect or physiological activity exerted by the absorbed compound or its metabolites at the target tissue [2].
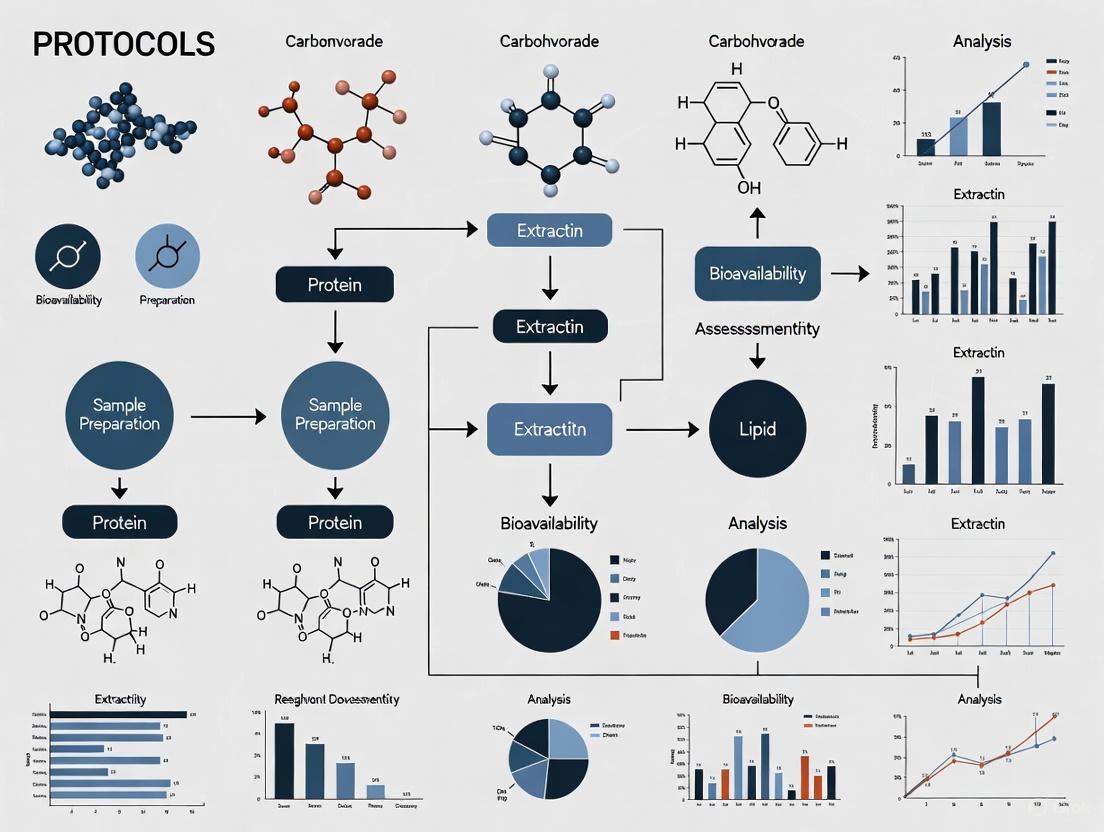
The following diagram illustrates the complete pathway from food ingestion to physiological effect, highlighting the key stages of bioaccessibility and bioavailability.
Quantitative Bioavailability Data for Key Nutrients
The bioavailability of micronutrients varies significantly depending on their food source, chemical form, and interactions with other dietary components. The table below summarizes the bioavailability ranges for selected vitamins and minerals from common food sources, based on in vivo human studies.
Table 1: Bioavailability of Selected Micronutrients from Whole Foods [4] [6]
| Nutrient | Food Source | Bioavailability Range | Key Influencing Factors |
|---|---|---|---|
| Iron (Heme) | Red Meat, Poultry, Fish | 10% - 40% | Iron status of the individual; minimally affected by dietary factors [6]. |
| Iron (Non-Heme) | Plant Foods (e.g., Spinach, Legumes) | 2% - 20% | Strongly inhibited by phytate and polyphenols; enhanced by vitamin C and meat [6]. |
| Calcium | Dairy Products (e.g., Milk, Cheese) | ~40% (varies with age) | Enhanced by vitamin D, casein phosphopeptides, lactose; inhibited by sulfur-containing proteins (increases urinary loss) [4]. |
| Zinc | Cereals, Legumes, Meat | Varies widely | Primarily inhibited by dietary phytate; absorption efficiency is higher from animal sources [6]. |
| Vitamin A (Retinol) | Animal Liver, Dairy, Eggs | 70% - 90% | Efficiently absorbed as pre-formed vitamin A [6]. |
| Vitamin A (Provitamin A Carotenoids) | Orange & Green Vegetables (e.g., Carrots, Spinach) | 10% - 80% | Enhanced by dietary fat; reduced by inefficient bioconversion in the gut [6]. |
| Folate | Leafy Greens, Legumes, Fortified Foods | ~50% (varies with form) | Synthetic folic acid is more bioavailable than natural food folates [6]. |
Methodologies for Assessing Bioaccessibility and Bioavailability
A multi-faceted approach is required to fully evaluate the bioavailability of nutrients, ranging from simulated in vitro digestion to sophisticated in vivo human trials.
In VitroDigestion and Bioaccessibility Models
In vitro models simulate human physiological conditions to predict the bioaccessibility of food components, offering a high-throughput, ethical, and cost-effective alternative to human studies [2]. The INFOGEST network has developed a widely adopted, standardized static protocol that simulates the oral, gastric, and intestinal phases of digestion [2].
- Oral Phase: Food is macerated and mixed with simulated salivary fluid (SSF) containing electrolytes and α-amylase.
- Gastric Phase: The oral bolus is mixed with simulated gastric fluid (SGF) containing pepsin and gastric lipase. The pH is adjusted to 3.0 and incubated at 37°C with shaking.
- Intestinal Phase: The gastric chyme is mixed with simulated intestinal fluid (SIF) containing pancreatic enzymes and bile salts. The pH is adjusted to 7.0 and incubated at 37°C with shaking.
The resulting chyme is centrifuged to obtain the soluble fraction, which represents the bioaccessible component of the nutrient, ready for absorption studies or further chemical analysis [2].
In VivoBioavailability and Absorption Techniques in Humans
While in vitro models are excellent for predicting bioaccessibility, bioavailability determination in humans is considered the "gold standard" [2]. Several sophisticated techniques are employed.
- Plasma Concentration Curves (AUC): This pharmacological method involves measuring the plasma or serum concentration of a nutrient over time after ingestion. The Area Under the Curve (AUC) is calculated and often compared to the AUC after an intravenous dose to determine Absolute Bioavailability [5].
- Use of Isotopic Tracers: The use of stable or radioactive isotopes has greatly improved the accuracy of in vivo nutrient bioavailability studies [4]. The extrinsic tag method, where an isotope is mixed with a food, has been validated against intrinsic tagging (where the food is biosynthetically labeled) for many minerals, showing homogeneous mixing with the native mineral pool in the food [3]. This allows for precise tracking of absorption and utilization.
- Functional Endpoint Measurements: Bioavailability can be estimated by measuring a functional or biochemical endpoint that reflects the absorption and utilization of the nutrient. For example, the change in blood hemoglobin concentration after consumption of an iron source in iron-deficient subjects can serve as a functional measure of iron bioavailability [3].
The following workflow outlines a comprehensive, multi-model research approach for determining nutrient bioavailability, integrating both in vitro and in vivo methods.
The Scientist's Toolkit: Key Reagents and Materials
Successful experimentation in bioavailability research requires a specific set of reagents and model systems. The following table details essential materials for setting up key experiments, particularly in vitro digestion and absorption studies.
Table 2: Essential Research Reagents for Bioavailability Studies
| Reagent / Material | Function / Application | Examples / Specifications |
|---|---|---|
| Simulated Digestive Fluids | To mimic the ionic composition and pH of salivary, gastric, and intestinal secretions. | KCl, KH₂PO₄, NaHCO₃, NaCl, MgCl₂(H₂O)₆, (NH₄)₂CO₃; prepared per INFOGEST protocol [2]. |
| Digestive Enzymes | To catalyze the breakdown of macronutrients (starch, proteins, fats) during in vitro digestion. | α-Amylase (oral), Pepsin (gastric), Pancreatin (intestinal mix), Gastric Lipase [2]. |
| Bile Salts | To emulsify lipids and form mixed micelles, which are crucial for the bioaccessibility of lipophilic compounds. | Porcine bile extracts or synthetic salts like sodium taurocholate [1] [2]. |
| Intestinal Cell Models | To study cellular uptake, metabolism, and transepithelial transport of bioaccessible nutrients. | Caco-2 cell line (human colonic adenocarcinoma), HT-29 (goblet cells), co-cultures, or primary-derived enteroids [2]. |
| Isotopic Tracers | To accurately track and quantify the absorption, distribution, and metabolism of specific nutrients in vivo. | Stable isotopes (e.g., ⁵⁷Fe, ⁶⁷Zn) or radioisotopes (e.g., ⁴⁷Ca, ¹⁴C); used in extrinsic/intrinsic tagging [3] [4]. |
| Transwell Inserts | To create a compartmentalized system (apical and basolateral) for studying transepithelial transport in cell monolayers. | Permeable supports (e.g., polycarbonate, polyester) with a pore size of 0.4–3.0 μm [2]. |
The LADME framework is a foundational pharmacokinetic model that describes the sequential processes a compound undergoes within an organism. Originally developed for pharmaceuticals, this framework is increasingly critical for understanding the fate of bioactive food compounds and nutrients, where it describes the journey from ingestion to elimination [7]. The acronym LADME stands for Liberation, Absorption, Distribution, Metabolism, and Elimination [8]. For nutrition researchers, this framework provides a systematic approach to quantify the bioavailability of nutrients—defined as the proportion of an ingested nutrient that is absorbed, transported, and delivered to target tissues in a form that can be utilized in metabolic functions or stored [9]. Understanding these processes is essential for moving beyond simply measuring the total nutrient content in foods and toward predicting their actual physiological impact, which is a key goal in modern nutritional science [10].
The LADME Process: A Detailed Breakdown for Nutrient Bioavailability
The five components of the LADME framework represent interlinked processes that determine the ultimate bioefficacy of a nutrient.
Liberation: This initial step involves the release of the nutrient from its food matrix. The process is influenced by food structure, processing methods, and mastication. For instance, nutrients entrapped in plant cellular structures or complexed with antagonists like phytates may not be fully liberated during digestion [9] [11]. Techniques such as mechanical processing, fermentation, or enzymatic treatments are often employed in research to enhance nutrient liberation [11].
Absorption: Absorption refers to the movement of nutrients from the gastrointestinal tract into the bloodstream or lymphatic system [8]. This stage is highly dependent on the chemical form of the nutrient (e.g., heme vs. non-heme iron), the presence of other dietary components (enhancers like vitamin C for iron or inhibitors like phytates for minerals), and host factors including gut health and microbiota [9] [12]. The absorption site varies; for example, fat-soluble vitamins are absorbed via the lymphatic system, while most water-soluble vitamins and minerals are absorbed directly into the portal blood [7].
Distribution: Once absorbed, nutrients are distributed via the circulatory system to various tissues and organs. The extent of distribution is influenced by the nutrient's ability to bind to plasma proteins, its lipophilicity, and the body's specific demands at the time. For instance, calcium may be directed to bone tissues, while iron is complexed with transferrin for delivery to the bone marrow and other tissues [7] [9].
Metabolism: Nutrients can undergo metabolic transformations, which can either activate them into more bioactive forms or deactivate them for excretion. A key example is the conversion of provitamin A carotenoids into active retinol or the hydroxylation of vitamin D into its active form, calcifediol [9] [12]. Nutrient metabolism can occur in the liver (first-pass metabolism) or in peripheral tissues and can be influenced by an individual's genetic makeup and nutritional status [7].
Elimination: The final process is the elimination of the nutrient or its metabolites from the body. This primarily occurs via renal (urine) or biliary (feces) excretion [8]. The rate of elimination determines the half-life and residence time of a nutrient in the body, impacting its long-term availability for physiological functions. Balance studies, which measure the difference between ingestion and excretion, are a common method for studying the elimination and overall absorption of nutrients [9].
It is crucial to note that these processes are not discrete sequential events but often occur simultaneously, especially with complex meals or sustained-release formulations [8].
Key Pharmacokinetic Parameters in LADME Studies
The following table summarizes the key quantitative parameters used to evaluate each stage of the LADME framework in nutritional research.
Table 1: Key Quantitative Parameters for Assessing Nutrient Bioavailability via the LADME Framework
| LADME Stage | Key Pharmacokinetic Parameters | Nutritional Application Example |
|---|---|---|
| Liberation | Liberation efficiency, bioaccessibility percentage | Percentage of a carotenoid released from its food matrix during in vitro digestion. |
| Absorption | Fraction absorbed (Famax, Tmax, AUC | Area Under the Curve (AUC) for plasma retinol after consuming β-carotene. |
| Distribution | Apparent Volume of Distribution (Vd), plasma protein binding | Distribution of vitamin E to adipose tissue and cell membranes. |
| Metabolism | Metabolic conversion rate, bioefficacy | Conversion rate of provitamin A carotenoids to retinol [12]. |
| Elimination | Elimination half-life (t1/2), clearance (CL) | Renal clearance of water-soluble B vitamins. |
Experimental Protocols for Assessing LADME Stages
A robust understanding of nutrient bioavailability requires integrated methodologies. The following workflow outlines a multi-technique approach, from simulated digestion to human trials.
Protocol 1: Bioaccessibility and Liberation Assessment
This protocol determines the fraction of a nutrient that is released from the food matrix into the digestive chyme (bioaccessibility), which is the first step toward bioavailability [9].
- Objective: To simulate the gastrointestinal liberation of a target nutrient from a food sample.
- Materials:
- Food Sample: Homogenized test food.
- Simulated Fluids: Simulated salivary fluid (SSF), gastric fluid (SGF), and intestinal fluid (SIF), prepared according to standardized recipes (e.g., INFOGEST).
- Digestive Enzymes: α-amylase, pepsin, pancreatin, and bile extracts.
- Equipment: Water bath or shaking incubator maintaining 37°C, pH meter, centrifuge.
- Methodology:
- Oral Phase: Mix 5 g of food sample with 4 mL of SSF and 1 mL of α-amylase solution. Incubate for 2 minutes at 37°C with constant agitation.
- Gastric Phase: Adjust the pH to 3.0, add 8 mL of SGF and 1 mL of pepsin solution. Incubate for 2 hours at 37°C with agitation.
- Intestinal Phase: Adjust the pH to 7.0, add 8 mL of SIF, 1 mL of pancreatin solution, and 4 mL of bile salts solution. Incubate for 2 hours at 37°C with agitation.
- Centrifugation: Centrifuge the final chyme at high speed (e.g., 10,000 × g, 30 minutes, 4°C) to separate the aqueous micellar phase (containing the liberated nutrient) from the solid residue.
- Analysis: Quantify the target nutrient in the aqueous phase using appropriate analytical techniques (e.g., HPLC for vitamins, ICP-MS for minerals). Calculate bioaccessibility as: (Nutrient in aqueous phase / Total nutrient in food sample) × 100.
Protocol 2: Mineral Absorption Using Stable Isotopes
This method provides a direct and highly accurate measurement of absorption for minerals like iron, zinc, and calcium in human subjects.
- Objective: To determine the true absorption of a mineral by tracking a stable isotope tracer.
- Materials:
- Stable Isotopes: e.g., 57Fe or 70Zn.
- Test Meals: Precisely formulated meals containing the isotope tracer.
- Sample Collection Tubes: For blood and fecal samples.
- Analytical Equipment: Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
- Methodology:
- Administration: Administer a test meal containing a precisely weighed amount of a stable isotope of the mineral (e.g., 57Fe) to a human participant after an overnight fast.
- Sample Collection: Collect complete fecal samples for a period of 8-14 days post-administration to ensure complete excretion of the unabsorbed isotope.
- Sample Preparation: Acid-digest the fecal samples to mineralize all organic matter and bring the mineral into solution.
- Isotopic Analysis: Analyze the isotopic composition of the prepared samples using ICP-MS. The instrument differentiates between the administered stable isotope and the natural isotopes present in the body.
- Calculation: Calculate the fraction of the isotope that was absorbed based on the amount not recovered in the feces: Absorption (%) = [1 - (Isotope recovered in feces / Isotope administered)] × 100.
Protocol 3: Algorithm-Based Bioavailability Estimation for Iron and Zinc
For population-level studies, algorithms that account for dietary enhancers and inhibitors provide a practical estimate of bioavailability [12].
- Objective: To estimate the total absorbed iron and zinc from a whole diet.
- Materials:
- Dietary Intake Data: Detailed food consumption records from participants.
- Comprehensive Food Composition Database: Must include data on the target nutrients, their chemical forms (e.g., heme vs. non-heme iron), and key modulators (phytates, vitamin C, etc.).
- Computational Tool: Software for implementing the algorithms (e.g., R, Python, or Excel).
- Methodology:
- Data Compilation: From the dietary records, calculate the total daily intakes of:
- Apply Algorithm for Non-Heme Iron Absorption:
- Use an algorithm such as: Non-heme Iron Absorption (%) = k × (SF^0.8) × (1 + α × C) × (1 + β × TMF) / ((1 + γ × T) × (1 + δ × P) × (1 + ε × Ca)) [12], where SF is serum ferritin, C is vitamin C, TMF is total meat/fish, T is tea/coffee, P is phytate, and Ca is calcium. Constants (k, α, β, γ, δ, ε) are derived from the literature.
- Apply Algorithm for Zinc Absorption:
- Use the equation: Total Absorbed Zinc (TAZ, mmol) = Total Dietary Zinc (TDZ, mmol) / [1 + (0.5 × Total Dietary Phytates (TDP, mmol))] [12].
- Calculate Total Absorption: For iron, sum the absorbed heme and non-heme iron. The results represent the estimated amount of mineral available for metabolic processes.
The Scientist's Toolkit: Key Reagents and Materials
Successful execution of bioavailability research requires specific reagents and tools. The following table details essential items for a laboratory focused on nutrient LADME.
Table 2: Essential Research Reagents and Materials for Nutrient Bioavailability Studies
| Item Name | Specification / Example | Primary Function in LADME Research |
|---|---|---|
| Simulated Digestive Fluids | INFOGEST standardized SSF, SGF, SIF | To mimic human gastrointestinal conditions for in vitro liberation (L) and absorption (A) studies [9]. |
| Caco-2 Cell Line | Human colon adenocarcinoma cell line | A well-established in vitro model of the intestinal epithelium for studying nutrient transport and absorption (A) [7]. |
| Stable Isotopes | 57Fe, 44Ca, 70Zn | Non-radioactive tracers to precisely track mineral absorption, distribution, and elimination in humans and animals [12]. |
| Phytase Enzymes | From microbial sources (e.g., Aspergillus niger) | Used in processing or in vitro models to hydrolyze phytate, an absorption inhibitor, thereby enhancing mineral bioavailability [9] [11]. |
| Permeation Enhancers | Medium-Chain Triglycerides (MCTs), chitosan | Compounds used in formulations to improve the absorption (A) of poorly absorbed nutrients by increasing intestinal permeability [9]. |
| Encapsulation Materials | Maltodextrin, chitosan, alginate, liposomes | Used for nanoencapsulation to protect sensitive nutrients from metabolism (M) and enhance their stability and absorption [11]. |
Advanced Applications and Current Research Trends
The application of the LADME framework is evolving with new technologies and a deeper understanding of individual variability. Advanced techniques are being deployed to overcome bioavailability challenges.
Table 3: Strategies for Enhancing Nutrient Bioavailability Across the LADME Framework
| LADME Stage | Challenge | Enhancement Strategy | Research Example |
|---|---|---|---|
| Liberation | Nutrient entrapment in plant cell walls. | Mechanical processing (e.g., fine milling), fermentation. | Fermentation by lactic acid bacteria degrades phytates in cereals, liberating bound minerals [11]. |
| Absorption | Low solubility or dietary inhibitors. | Nanoencapsulation, use of absorption enhancers (e.g., vitamin C with iron). | Lipid-based nanoencapsulation improves solubility and absorption of fat-soluble vitamins [9] [11]. |
| Distribution & Metabolism | Rapid metabolism or poor conversion. | Using precursor forms or more bioavailable chemical forms. | Calcifediol (25-hydroxyvitamin D) is more bioavailable than cholecalciferol (vitamin D3) [9]. |
| Overall Bioefficacy | Host-specific factors (genetics, microbiome). | Personalized nutrition based on genotyping and microbiome analysis. | Formulating diets based on individual genetic profiles affecting nutrient metabolism [11]. |
Furthermore, there is a strong push to integrate bioavailability data into public health tools. The International Life Sciences Institute (ILSI) U.S. and Canada recently published a framework for estimating nutrient absorption, aiming to incorporate bioavailability algorithms into nutrient databases, food labels, and dietary assessment tools [10] [13]. This transition from total nutrient content to "usable nutrient intake" represents the ultimate application of LADME research, enabling more accurate dietary recommendations and effective public health interventions.
The assessment of nutrient bioavailability is a critical component of nutritional science and food research. While dietary factors are often emphasized, host-related factors—including genetics, health status, and life stage—fundamentally determine how individuals absorb and utilize nutrients from foods. Understanding these variables is essential for developing accurate research protocols and interpreting experimental outcomes in human studies. This application note provides detailed methodologies for investigating these host-related factors within the context of nutrient bioavailability research, offering researchers a standardized framework to account for intrinsic human variability.
Genetic Factors Influencing Nutrient Absorption
Key Genetic Variants and Mechanisms
Genetic variations introduce significant inter-individual variability in nutrient absorption and metabolism. These differences primarily occur through polymorphisms that affect digestive enzymes, transport proteins, and metabolic pathways.
Table 1: Key Genetic Variants Affecting Nutrient Bioavailability
| Gene | Nutrient Affected | Impact of Variation | Research Implications |
|---|---|---|---|
| TAS2R38 | Phenylthiocarbamide (in brassica vegetables) | Alters taste perception; influences food preference and consumption [14] | Requires dietary preference screening in study participants |
| LCT | Lactose | Determines lactase persistence or non-persistence [14] | Necessitates genotype screening for dairy-based nutrient studies |
| BCO1 | Carotenoids (β-carotene, lutein, zeaxanthin) | SNPs (rs6564851-C, rs6420424-A) significantly impact circulating carotenoid levels [15] | Critical for studies on fat-soluble vitamin bioavailability |
| FLG | Multiple nutrients | Loss-of-function mutations affect skin and gut barriers; alter nutrient absorption [16] | Important for studies on barrier function and nutrient absorption |
| FTO | Lipids | Intronic variant affects IRX3/IRX5 expression; alters adipocyte metabolism [16] | Relevant for lipid metabolism and energy balance studies |
Experimental Protocol: Genotyping for Nutrient Absorption Studies
Objective: To identify and control for genetic variants that significantly impact nutrient bioavailability in human intervention studies.
Materials:
- DNA extraction kit (validated for human biospecimens)
- Pre-designed TaqMan SNP Genotyping Assays or equivalent
- Quantitative PCR system with allelic discrimination capability
- EDTA-treated whole blood or saliva samples
- Laboratory automation equipment for high-throughput processing
Procedure:
- Participant Selection and Stratification:
- Recruit sufficient participants to ensure statistical power for subgroup analysis (typically n≥50 per genotype group)
- Include ancestry and ethnicity matching to control for population-specific allele frequencies [16]
DNA Extraction and Quality Control:
- Extract genomic DNA from whole blood or saliva following manufacturer protocols
- Quantify DNA concentration using spectrophotometry (A260/A280 ratio of 1.8-2.0 acceptable)
- Normalize all samples to working concentration of 5-10 ng/μL
Genotyping Analysis:
- Perform real-time PCR with allele-specific probes
- Include positive controls for all three possible genotypes (homozygous reference, heterozygous, homozygous variant) in each run
- Run duplicate samples to ensure genotype concordance >99%
Data Analysis:
- Cluster plot analysis to assign genotypes
- Calculate Hardy-Weinberg equilibrium p-values for quality control (p>0.05 acceptable)
- Stratify nutrient absorption data by genotype for statistical comparison
Applications: This protocol is particularly valuable for studies investigating carotenoids, lipids, and minerals where known genetic variants explain significant portions of inter-individual variability in response to interventions.
Health Status and Physiological Factors
Impact of Health Conditions on Absorption
Health status significantly modulates nutrient absorption through multiple mechanisms, including alterations in gastrointestinal environment, inflammatory responses, and metabolic demands.
Table 2: Health Status Factors Affecting Nutrient Bioavailability
| Health Factor | Impact on Absorption | Research Considerations |
|---|---|---|
| Infections | Decreased food intake, impaired nutrient absorption, nutrient wastage, sequestration [17] | Requires health screening; acute infections may necessitate study postponement |
| Gastric Acid Reduction | Reduced bioavailability of micronutrients, especially iron and B12 [18] | Document medication use (PPIs, H2 blockers); consider age-related decline |
| Inflammatory Bowel Disease | Malabsorption of multiple nutrients due to mucosal damage | Exclusion criterion or separate stratification group |
| Obesity | Altered lipid metabolism, potential micronutrient deficiencies | Record BMI and body composition; may require separate cohort design |
| Helicobacter pylori Infection | Impaired iron and B12 absorption through gastric changes | Screen for infection status in mineral studies |
Experimental Protocol: Assessing Health Status in Bioavailability Studies
Objective: To systematically evaluate and document health status factors that may confound nutrient absorption measurements.
Materials:
- Standardized health screening questionnaire
- Basic metabolic panel reagents
- C-reactive protein (CRP) assay
- Hemoglobin and ferritin measurement systems
- Stool antigen tests for H. pylori (if applicable)
Procedure:
- Comprehensive Health Screening:
- Administer detailed medical history questionnaire covering gastrointestinal conditions, chronic diseases, and surgical history
- Document all prescription and over-the-counter medications, particularly acid-reducing agents and anti-inflammatories
- Record recent (within 2 weeks) symptoms of infection or illness
Biomarker Analysis:
- Collect fasting blood samples for CRP (inflammatory marker), complete blood count, and basic metabolic panel
- For mineral studies, include iron status markers (ferritin, transferrin saturation)
- For fat-soluble nutrient studies, include liver function tests
Statistical Control:
- Include health status covariates in statistical models analyzing nutrient absorption data
- Consider exclusion criteria for values outside normal ranges that may indicate subclinical conditions
- For studies focusing on specific health conditions, recruit homogeneous patient groups with matched controls
Life Stage Considerations
Life Stage Impact on Nutrient Requirements
Physiological changes across the lifespan significantly alter nutrient absorption capacity and requirements. These changes must be accounted for in study design and data interpretation.
Key Life Stage Considerations:
- Aging: Gradual decline in gastric acid production reduces micronutrient bioavailability; older adults show 40% reduction in nutrient absorption efficiency compared to younger individuals [18] [17]
- Pregnancy: Enhanced calcium absorption (approximately 2-fold increase) to support fetal skeletal development; increased zinc absorption tendencies [17]
- Lactation: Altered mineral homeostasis with renal conservation and bone resorption mechanisms [17]
- Infancy/Childhood: Rapidly changing gut maturation and enzyme expression patterns
Experimental Protocol: Life Stage Stratification in Absorption Studies
Objective: To account for physiological differences in nutrient absorption across life stages through appropriate study design and data analysis.
Materials:
- Age-appropriate dosing and sampling protocols
- Pregnancy tests for women of childbearing potential
- Additional safety monitoring for vulnerable populations
Procedure:
- Study Group Design:
- Define specific age ranges for study cohorts (e.g., young adults: 18-35y, older adults: 65-80y)
- For studies including older adults, document medication use that may affect GI function
- For women of childbearing age, conduct pregnancy testing and standardize testing to similar menstrual cycle phases when possible
Protocol Adaptations:
- For elderly participants, consider longer absorption periods to account for slowed GI transit
- For pregnancy studies, carefully time interventions to specific trimesters with obstetric oversight
- For pediatric studies, implement age-appropriate dosing (weight-based) and sampling volumes
Data Interpretation:
- Analyze results stratified by life stage group
- Include age as a continuous variable in regression models examining absorption kinetics
- Compare study populations to reference values for specific age groups
Integrated Experimental Workflow
The investigation of host-related factors in nutrient bioavailability requires a systematic approach that integrates genetic, health, and life stage assessments. The following workflow provides a visual representation of this integrated protocol:
Diagram: Integrated Workflow for Assessing Host Factors in Bioavailability. This workflow systematically integrates assessment of genetic, health, and life stage factors throughout the study design.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Host Factor Analysis
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Genotyping Assays | TaqMan SNP Genotyping Assays, Illumina Infinium arrays | Identification of genetic variants affecting nutrient metabolism [15] [16] | Select population-specific variants; verify assay validation for human genomes |
| DNA Extraction Kits | QIAamp DNA Blood Mini Kit, PureLink Genomic DNA kits | High-quality DNA extraction from blood, saliva, or buccal cells | Assess yield and purity; ensure compatibility with downstream applications |
| Inflammatory Markers | CRP ELISA kits, cytokine panels, leukocyte differentiation kits | Quantification of systemic inflammation affecting nutrient utilization [17] | Establish normal ranges for study population; control for acute inflammation |
| Metabolic Panels | Automated clinical chemistry analyzers, enzyme activity assays | Assessment of organ function and nutrient status [17] | Standardize sampling conditions (fasting, time of day) |
| Nutrient Biomarker Assays | HPLC systems, mass spectrometers, immunoassays | Quantification of nutrient and metabolite concentrations in biological samples [1] | Validate for specific sample matrices; establish detection limits |
| Microbiome Analysis | 16S rRNA sequencing kits, metagenomic sequencing services | Characterization of gut microbiota composition affecting nutrient processing [15] | Standardize sample collection and storage to preserve microbial DNA |
Host-related factors including genetic variation, health status, and life stage constitute fundamental determinants of nutrient bioavailability that must be rigorously controlled in nutritional research. The protocols outlined herein provide researchers with standardized methodologies to account for these variables, thereby enhancing the accuracy, reproducibility, and biological relevance of nutrient absorption studies. By implementing these comprehensive assessment strategies, researchers can advance the development of personalized nutrition approaches and strengthen the scientific basis for dietary recommendations tailored to individual physiological needs.
The food matrix is defined as the integrated physicochemical domain that contains and/or interacts with specific constituents of a food, providing functionalities and behaviors that are different from those exhibited by the components in isolation or a free state [19] [20]. This concept has fundamentally shifted the understanding of nutritional quality, moving beyond simple proximate composition analysis to consider how the complex organization of food components influences nutrient bioavailability—the fraction of an ingested nutrient that becomes available for use and storage in the body [4]. The matrix effect demonstrates that foods are not merely ideal systems with equally distributed components, but rather intricate, multicomponent systems where macro- and microconstituents interact through various molecular forces including hydrogen bonding, coordination forces, electrostatic interactions, π-π stacking, and hydrophobic reactions [20].
Understanding the diet-related factors that enhance or inhibit nutrient bioavailability is crucial for developing effective dietary recommendations, nutritional therapies, and fortified food products [21]. The journey of a nutrient from ingestion to utilization involves multiple biological processes: it must first be released from the food matrix (a concept referred to as bioaccessibility), then absorbed through the gut lining into the bloodstream, and finally utilized by cells [21] [22]. At each of these stages, specific dietary factors can either facilitate or hinder the process, creating a complex network of interactions that ultimately determines the nutritional value of a food. This document provides detailed protocols and application notes for assessing these critical interactions within the context of food bioavailability research.
Key Enhancers and Inhibitors of Nutrient Bioavailability
The following sections provide a detailed overview of the major dietary factors that influence the bioavailability of micronutrients, with specific emphasis on the underlying mechanisms and practical implications for research and food design.
Major Bioavailability Enhancers
Table 1: Key Dietary Bioavailability Enhancers and Their Mechanisms of Action
| Enhancer | Target Nutrient(s) | Mechanism of Action | Food Sources |
|---|---|---|---|
| Vitamin C | Non-heme iron | Reduces ferric iron (Fe³⁺) to more absorbable ferrous (Fe²⁺) form; chelates iron to maintain solubility in intestinal lumen [21] [22]. | Citrus fruits, bell peppers, broccoli, strawberries |
| Milk Proteins (Casein, Whey) | Calcium, Minerals | Phosphopeptides from casein hydrolysis bind calcium, protecting it from precipitation by anions like phosphates; slow release enhances passive diffusion [4]. | Milk, yogurt, cheese |
| Lactose | Calcium | Widens paracellular spaces in enteric cell lining; may function as prebiotic to stimulate calcium absorption in colon [4]. | Milk, dairy products |
| Organic Acids | Various minerals | Acidic environment enhances mineral solubility; chelation effects improve absorption [21]. | Fermented foods, citrus fruits |
| Vitamin D | Calcium | Regulates active transport of calcium at low and moderate intake levels; enhances calcium absorption efficiency [4]. | Fortified dairy, fatty fish, egg yolks |
| Certain Amino Acids | Minerals | L-lysine and L-arginine bind minerals, making them readily released during digestion [4]. | Animal proteins, legumes |
Vitamin C stands as one of the most potent enhancers of non-heme iron absorption, particularly relevant for plant-based diets where iron bioavailability is typically lower [22]. The mechanism involves both chemical reduction of iron to its more absorbable form and chelation to maintain solubility throughout the digestive process. Research indicates that simultaneous consumption of vitamin C-rich foods with iron-rich plant sources can significantly improve iron status, a critical consideration for populations at risk of deficiency [21].
Dairy matrices present a fascinating case of natural enhancement, where multiple components work synergistically to improve calcium bioavailability. The combined action of casein-derived phosphopeptides, whey proteins, lactose, and vitamin D creates a highly efficient calcium delivery system that explains why dairy products remain the most effective source for bone health [4]. This synergistic effect underscores the importance of studying whole foods rather than isolated nutrients, as the net benefit exceeds what would be predicted from individual components alone.
Major Bioavailability Inhibitors
Table 2: Key Dietary Bioavailability Inhibitors and Their Mechanisms of Action
| Inhibitor | Target Nutrient(s) | Mechanism of Action | Food Sources |
|---|---|---|---|
| Phytates (Phytic Acid) | Zinc, Iron, Calcium, Magnesium | Forms insoluble complexes with minerals in the intestinal lumen, preventing absorption [21] [20]. | Whole grains, legumes, nuts, seeds |
| Oxalates | Calcium | Binds calcium to form insoluble calcium oxalate crystals [20]. | Spinach, rhubarb, beets, nuts |
| Polyphenols (Tannins) | Iron, Zinc | Forms insoluble complexes with minerals; inhibits digestive enzymes [22] [20]. | Tea, coffee, red wine, certain legumes |
| Dietary Fiber | Various minerals | Physically traps minerals; increases intestinal transit time; may bind minerals directly [20]. | Whole grains, fruits, vegetables |
| Calcium | Iron, Zinc | Competitive inhibition for transport proteins; particularly affects non-heme iron [4]. | Dairy products, fortified foods |
| Sulfur-containing Proteins | Calcium | Induces hypercalciuria (increased urinary calcium excretion) [4]. | Animal proteins, eggs |
Phytates represent one of the most significant inhibitors of mineral absorption, particularly for zinc and iron. These compounds, which serve as phosphorus storage in seeds and grains, have strong chelating properties that form stable complexes with di- and trivalent minerals, rendering them unavailable for absorption [21]. The negative impact of phytates is particularly pronounced in populations relying heavily on whole grain and legume-based diets, highlighting the importance of food processing techniques such as fermentation, soaking, and germination that can reduce phytate content.
The interaction between different minerals presents another complex inhibitory mechanism. Calcium, for instance, has been shown to inhibit the absorption of both iron and zinc when consumed simultaneously, likely through competition for shared transport mechanisms [4]. This interaction has important implications for meal planning and fortification strategies, as the addition of calcium to iron-fortified products may inadvertently reduce iron bioavailability. Similarly, the presence of multiple inhibitors in the same meal can have cumulative effects, substantially reducing the overall mineral bioavailability from plant-based foods [20].
Diagram 1: Bioavailability Pathway with Key Enhancers and Inhibitors. This workflow illustrates the sequential stages of nutrient bioavailability and points where major enhancers and inhibitors exert their effects.
Experimental Protocols for Assessing Bioavailability
This section provides detailed methodologies for evaluating the impact of diet-related factors on nutrient bioavailability, with specific protocols designed for research applications.
Protocol 1: In Vitro Simulation of Gastrointestinal Digestion
Purpose: To simulate the human digestive process for evaluating nutrient bioaccessibility from complex food matrices under controlled laboratory conditions [4] [20].
Principle: This protocol recreates the sequential physiological conditions of the mouth, stomach, and small intestine to measure the fraction of nutrients released from the food matrix during digestion (bioaccessibility). The method is particularly valuable for rapid screening of multiple food matrix interactions and the effects of processing conditions on nutrient release.
Materials and Reagents:
- Simulated Salivary Fluid (SSF): Contains α-amylase in appropriate buffer
- Simulated Gastric Fluid (SGF): Contains pepsin in acidified saline (pH 3.0)
- Simulated Intestinal Fluid (SIF): Contains pancreatin and bile extracts in neutral buffer
- pH-Stat Titrator: For maintaining precise pH control during intestinal phase
- Water Bath or Incubator: Maintained at 37°C with continuous agitation
- Centrifuge and Ultracentrifuge: For separation of aqueous fraction (micellar phase)
- Dialysis Membranes: Molecular weight cut-off 12-14 kDa for fractionation
- Analytical Equipment: HPLC, ICP-MS, or spectrophotometric systems for nutrient quantification
Procedure:
- Sample Preparation: Homogenize test food material to standardized particle size (typically 2-5 mm). Precisely weigh 5-10 g samples in digestion vessels.
Oral Phase: Add SSF to sample at 1:1 ratio (w/v). Incubate for 2 minutes at 37°C with continuous agitation (100 rpm).
Gastric Phase: Adjust mixture to pH 3.0 using 1M HCl. Add SGF containing pepsin (2000 U/mL final concentration). Incubate for 2 hours at 37°C with continuous agitation.
Intestinal Phase: Adjust mixture to pH 7.0 using 1M NaHCO₃. Add SIF containing pancreatin (100 U/mL trypsin activity) and bile extracts (10 mM final concentration). Incubate for 2 hours at 37°C while maintaining pH at 7.0 using pH-stat titration.
Bioaccessible Fraction Collection: Centrifuge intestinal digest at 5000 × g for 30 minutes at 4°C. Collect supernatant representing the bioaccessible fraction. For additional fractionation, ultracentrifuge at 100,000 × g for 1 hour to isolate the micellar phase.
Analysis: Quantify target nutrients in the bioaccessible fraction using appropriate analytical methods (HPLC for vitamins, ICP-MS for minerals).
Data Interpretation: Calculate bioaccessibility as: (Nutrient content in bioaccessible fraction / Total nutrient content in original sample) × 100. Compare values across different food matrices or processing conditions to determine the impact of enhancers/inhibitors.
Protocol 2: Stable Isotope Studies for Human Bioavailability Assessment
Purpose: To precisely measure the absorption and metabolic utilization of nutrients in human subjects using stable isotope tracers [4].
Principle: This approach uses nutrients labeled with non-radioactive stable isotopes (²H, ¹³C, ¹⁵N, etc.) to trace the fate of specific nutrients from ingestion through absorption, distribution, and excretion. The method provides the most accurate assessment of true bioavailability in humans and is considered the gold standard for bioavailability research.
Materials and Reagents:
- Stable Isotope-Labeled Nutrients: Specifically synthesized with ¹³C, ²H, ⁵⁷Fe, ⁶⁷Zn, etc.
- Medical-Grade Supplement Vehicles: Such as gelatin capsules or sterile solutions
- Blood Collection Equipment: Vacutainer tubes (EDTA, heparin)
- Urine/Stool Collection Containers: Pre-weighed, acid-washed containers
- Mass Spectrometry Equipment: ICP-MS for mineral isotopes, GC-IRMS or LC-IRMS for organic nutrients
- Anthropometric Equipment: For subject screening and monitoring
Procedure:
- Subject Selection and Preparation: Recruit healthy volunteers based on inclusion/exclusion criteria. Provide standardized lead-in diet for 3-7 days before study to normalize nutrient status. Obtain informed consent following institutional ethics committee approval.
Isotope Administration: After an overnight fast, administer precisely weighed stable isotope-labeled nutrient (e.g., ⁵⁷Fe, ²H-folate) with a test meal containing the enhancer/inhibitor of interest. Use cross-over design with washout period when comparing multiple test conditions.
Sample Collection: Collect baseline blood, urine, and stool samples before isotope administration. Continue serial blood sampling at predetermined intervals (30 min, 1, 2, 4, 6, 8, 24 hours). Collect complete urine and stool for 5-7 days post-administration.
Sample Processing: Process blood samples to separate plasma, serum, and erythrocytes. Precisely weigh and homogenize stool samples. Acid-digest samples for mineral analysis or extract for vitamin analysis as appropriate.
Isotope Ratio Analysis: Determine isotope ratios in biological samples using appropriate mass spectrometric techniques:
- ICP-MS: For mineral isotopes (Fe, Zn, Ca, etc.)
- GC-IRMS: For ¹³C-labeled vitamins and organic nutrients
- LC-IRMS: For polar compounds and certain vitamins
Kinetic Modeling: Apply compartmental modeling to isotope appearance curves in blood to calculate absorption parameters. Use fecal monitoring or dual-isotope method to determine total absorption.
Data Interpretation: Calculate bioavailability as the fraction of administered isotope that appears in circulation or is retained in the body. Compare isotopic enrichment patterns between test conditions to quantify the effects of specific enhancers or inhibitors.
Research Reagent Solutions and Essential Materials
Table 3: Essential Research Reagents for Bioavailability Studies
| Reagent/Material | Specifications | Research Application | Key Considerations |
|---|---|---|---|
| Stable Isotopes | ⁵⁷Fe, ⁶⁷Zn, ⁴⁴Ca, ¹³C-labeled vitamins | Human tracer studies for precise absorption measurement [4] | Purity >98%; chemical form identical to native nutrient; sterile preparation for human use |
| Digestive Enzymes | Porcine or recombinant pepsin, pancreatin, α-amylase | In vitro simulation of gastrointestinal digestion [20] | Activity standardization; lot-to-lot consistency; minimal endogenous nutrient contamination |
| Simulated Gastrointestinal Fluids | SSF, SGF, SIF following standardized recipes | In vitro bioaccessibility assessment [20] | pH stability; ionic composition matching human physiology; sterile filtration |
| Caco-2 Cell Line | Human colon adenocarcinoma cells, passages 30-45 | Intestinal absorption studies and transport mechanisms [20] | Proper differentiation (21 days); TEER measurement for monolayer integrity; mycoplasma testing |
| Dialyzation Membranes | Regenerated cellulose, MWCO 12-14 kDa | Fractionation of bioaccessible nutrients in vitro [20] | Pre-treatment to remove contaminants; compatibility with target analytes; lot consistency |
| Reference Materials | Certified food matrices with known nutrient composition | Method validation and quality control [22] | Matrix-matched to samples; certified values for target nutrients; stability documentation |
The systematic investigation of diet-related factors affecting nutrient bioavailability reveals the profound complexity of food as a biological delivery system rather than merely a collection of individual nutrients. The protocols and application notes provided here offer researchers standardized approaches to quantify these critical interactions, with particular relevance for developing evidence-based dietary recommendations, optimizing food fortification strategies, and designing functional foods targeted to specific population needs.
Future research directions should focus on expanding our understanding of food matrix interactions beyond the traditional vitamin and mineral considerations to include bioactive phytochemicals, the role of the gut microbiome in nutrient utilization, and the development of sophisticated in silico models that can predict bioavailability based on food composition and matrix properties. The integration of these approaches will ultimately enable more personalized nutritional recommendations and the development of food products with optimized nutrient delivery capabilities.
Diagram 2: Comprehensive Research Workflow for Bioavailability Studies. This diagram outlines an integrated approach to investigating enhancers and inhibitors, combining in vitro screening with mechanistic studies and human validation.
A Guide to In Vivo, In Vitro, and In Silico Assessment Methods
The quantitative assessment of nutrient bioavailability in humans requires sophisticated methodologies that can trace metabolic pathways in vivo without disrupting normal physiology. Stable and radioactive isotopes serve as powerful tracers for this purpose, providing the gold standard for understanding the dynamic aspects of human metabolism including nutrient absorption, distribution, and utilization [23]. These tracer techniques allow researchers to move beyond static concentration measurements to kinetic analyses that reveal how nutrients are processed within the human body [23]. The fundamental principle involves administering an isotope-labeled compound and tracking its movement through biological systems, enabling precise measurement of metabolic flux rates, pool sizes, and turnover times [23].
Unlike in vitro methods that merely estimate bio-accessibility, isotopic tracer studies in humans provide direct evidence of bioavailability, defined as the proportion of a nutrient that is absorbed and becomes available for physiological functions [24]. This approach is particularly valuable for assessing nutrients from plant-based foods, where anti-nutrients such as phytic acid and tannins can significantly limit mineral absorption [24]. As plant-based diets gain prominence for health and sustainability reasons, understanding the bioavailability of their nutrients becomes increasingly important for addressing global malnutrition challenges [25].
Fundamental Isotope Concepts for Metabolic Tracers
Stable versus Radioactive Isotopes
Isotopes are variants of a single element that differ in the number of neutrons in their nuclei, resulting in different atomic masses but identical chemical properties [26]. For metabolic research, isotopes are categorized as either stable or radioactive:
- Stable isotopes do not emit radiation, are naturally occurring, and have constant atomic masses over time [27] [26]. Examples include deuterium (²H), carbon-13 (¹³C), nitrogen-15 (¹⁵N), and oxygen-18 (¹⁸O) [23].
- Radioactive isotopes (radioisotopes) spontaneously decay with emission of radiation and have defined half-lives [27] [26]. While useful for certain applications, safety concerns have limited their use in human studies, particularly in vulnerable populations [23].
The selection between stable and radioactive isotopes depends on the research question, target population, and detection capabilities. Gold-197 represents the only stable isotope of gold, while radioactive gold isotopes such as gold-195 (half-life: 186.01 days) and gold-198 (half-life: 2.69 days) exist but are not typically used in nutrient bioavailability studies [28].
Metabolic Tracer Principles
A metabolic isotope tracer is a molecule where one or more atoms have been replaced with an uncommon isotope, making it chemically and functionally identical to the naturally occurring molecule (tracee) but distinguishable by mass or radioactivity [23]. The core requirement is that the tracer must participate in biological processes identically to the tracee while remaining detectable throughout the metabolic pathway of interest.
The tracer-to-tracee ratio (TTR) represents the fundamental measurement in these studies, typically determined using mass spectrometry techniques [23]. For stable isotopes, the natural abundance of heavier isotopes must be accounted for in calculations; for example, approximately 6.6% of naturally occurring glucose contains at least one carbon-13 atom due to its 1.1% natural abundance [23].
Table 1: Stable Isotopes Commonly Used in Bioavailability Research
| Stable Isotope | Natural Abundance | Applications in Nutrition Research |
|---|---|---|
| Carbon-13 (¹³C) | ~1.1% [23] | Breath tests for carbohydrate metabolism, amino acid kinetics, fatty acid metabolism [29] |
| Deuterium (²H) | ~0.015% | Energy expenditure studies, water turnover [29] |
| Nitrogen-15 (¹⁵N) | ~0.4% | Protein turnover, amino acid metabolism [23] |
| Oxygen-18 (¹⁸O) | ~0.2% | Energy expenditure, water turnover (with deuterium) [29] |
| Calcium-42, -44, -46 | Varying abundances | Calcium absorption, bone turnover studies, osteoporosis research [29] |
| Iron-54, -57, -58 | Varying abundances | Iron metabolism, absorption studies, anemia interventions [29] |
Experimental Protocols for Isotope Tracer Studies
General Study Design and Setup
Isotope tracer studies in humans follow standardized protocols to ensure reproducible and interpretable results. The basic design involves administering one or more isotope tracers and collecting biological samples at predetermined time points to track the tracer's appearance, distribution, and disappearance [23].
Subject Preparation: Participants are typically studied after an overnight fast to establish baseline metabolic conditions. For nutrient bioavailability studies, the isotope-labeled nutrient may be administered with a test meal to evaluate absorption under realistic dietary conditions. The tracer dose is carefully calculated based on body weight, natural abundance of the isotope, and detection sensitivity of analytical instruments.
Tracer Administration: Isotope tracers can be administered via multiple routes depending on the research question:
- Intravenous infusion: Provides direct access to systemic circulation for quantifying production, disappearance, and clearance rates [23]
- Oral administration: Essential for assessing absorption and first-pass metabolism of nutrients
- Combined protocols: Simultaneous intravenous and oral tracers (e.g., dual calcium isotopes) can differentiate between absorption and endogenous secretion [29]
Sample Collection: Blood samples are most commonly collected, but urine, breath, saliva, and tissue biopsies may also be obtained depending on the metabolic pathway under investigation. Sampling frequency ranges from minutes to hours or days, determined by the kinetics of the traced metabolite [23].
Protocol for Stable Isotope Tracer Infusion Study
The following protocol outlines a standardized approach for conducting stable isotope tracer infusion studies in human subjects:
- Pre-Study Preparation
- Secure ethical approval and informed consent
- Screen participants for eligibility based on study objectives
- Prepare isotope tracer solutions ensuring pharmaceutical grade purity and sterility
- Calibrate infusion pumps and prepare sampling equipment
- Baseline Sample Collection
- Collect pre-dose blood, urine, or other samples to determine background isotopic enrichment
- Record baseline physiological parameters (weight, height, vital signs)
- Tracer Administration
- For intravenous studies: Insert venous catheter for tracer infusion and a separate catheter for blood sampling to avoid contamination
- Prime the infusion tubing with tracer solution to ensure immediate delivery
- Initiate tracer infusion at a constant rate using a calibrated pump
- For oral administration: Administer the isotope tracer with or without a test meal under standardized conditions
- Sample Collection During Tracer Administration
- Collect biological samples at predetermined time points during the infusion period
- Process samples appropriately for subsequent analysis (e.g., plasma separation, storage at -80°C)
- Record exact sampling times relative to the start of tracer administration
- Sample Analysis
- Extract the analyte of interest from biological samples
- Derivatize if necessary for gas chromatography mass spectrometry (GC/MS) analysis
- Measure isotopic enrichment using GC/MS or liquid chromatography mass spectrometry (LC/MS)
- Calculate tracer-to-tracee ratios (TTR) or mole percent excess (MPE) [23]
- Kinetic Calculations
- Apply appropriate mathematical models to calculate metabolic kinetics based on isotopic enrichment patterns
- Common parameters include rate of appearance (Ra), fractional synthesis rate (FSR), and clearance rate [23]
Figure 1: Experimental workflow for human isotope tracer studies
Specialized Protocol: Dual Isotope Method for Mineral Absorption
The dual isotope method provides a comprehensive approach for assessing mineral bioavailability, particularly useful for minerals like calcium, iron, and zinc:
Isotope Selection: Choose two stable isotopes of the same mineral with different masses (e.g., calcium-42 and calcium-44) [29]
Administration:
- Administer one isotope orally with the test meal
- Simultaneously administer the second isotope intravenously
- Use precise dosing based on participant weight and isotope enrichment
Sample Collection: Collect blood samples at 0, 30, 60, 120, 240, and 360 minutes post-administration, and 24-hour urine collections for several days
Analysis:
- Separate minerals from biological matrices using chemical extraction
- Analyze isotopic ratios using inductively coupled plasma mass spectrometry (ICP-MS)
- Correct for natural abundance and spectral interferences
- Calculation:
- Calculate fractional absorption from the ratio of oral and intravenous isotopes in urine or blood
- Determine endogenous excretion and compartmental distribution
Analytical Methodologies for Isotope Detection
Mass Spectrometry Techniques
Mass spectrometry represents the cornerstone technology for detecting stable isotopes in biological samples due to its high sensitivity, specificity, and precision [23]. The two primary approaches are:
Gas Chromatography-Mass Spectrometry (GC/MS): This technique combines separation of complex mixtures by gas chromatography with mass detection. Samples must be volatile or chemically derivatized to increase volatility for GC analysis [23]. Within the mass spectrometer, ionization occurs typically through electron impact or chemical impact ionization, followed by separation of ions based on mass-to-charge ratio (m/z) in the mass analyzer [23]. The abundance of specific ions is detected, allowing calculation of isotopic enrichment.
Liquid Chromatography-Mass Spectrometry (LC/MS): This approach uses liquid chromatography for separation, making it suitable for compounds that are not easily volatilized. LC/MS has become increasingly popular for analyzing larger molecules, polar compounds, and thermally labile substances without requiring derivatization.
The selection of specific ion fragments for monitoring is critical for accurate enrichment measurements. Ions should be unique to the analyte of interest and contain the atoms that were isotopically labeled [23].
Nuclear Magnetic Resonance (NMR) Spectroscopy
While mass spectrometry detects mass differences between isotopes, NMR spectroscopy exploits the magnetic properties of certain nuclei, such as carbon-13. NMR provides complementary structural information about metabolites and can track the position-specific incorporation of isotopes within molecules. This is particularly valuable for understanding metabolic pathways where the position of the labeled atom provides information about specific enzymatic reactions.
Table 2: Comparison of Analytical Techniques for Isotope Detection
| Technique | Principles | Applications in Bioavailability | Advantages | Limitations |
|---|---|---|---|---|
| GC/MS | Separation by volatility, detection by mass | Amino acid kinetics, carbohydrate metabolism, fatty acid oxidation | High sensitivity, well-established methods | Requires volatile compounds or derivatization |
| LC/MS | Separation by polarity, detection by mass | Protein turnover, vitamin metabolism, complex lipids | No derivatization needed, handles polar compounds | More complex ionization, potential matrix effects |
| ICP-MS | Ionization in plasma, elemental detection | Mineral absorption studies (Ca, Fe, Zn, Se) | Excellent for elemental analysis, very low detection limits | Does not distinguish molecular forms without separation |
| NMR | Magnetic properties of nuclei | Metabolic pathway mapping, position-specific isotope tracing | Non-destructive, provides structural information | Lower sensitivity than MS, requires higher isotope enrichment |
Applications in Nutrient Bioavailability Research
Mineral Bioavailability Studies
Isotopic tracers have revolutionized our understanding of mineral absorption and metabolism, providing critical data for establishing dietary requirements and developing fortification strategies:
Calcium Metabolism: Stable calcium isotopes (e.g., calcium-42, -44, -46, -48) enable precise measurement of calcium absorption, endogenous excretion, and bone turnover [29]. Using simultaneous oral and intravenous administration of different calcium isotopes, researchers can investigate how various factors such as age, pregnancy, lactation, and dietary composition affect calcium bioavailability [29]. This approach has been particularly valuable in osteoporosis research, revealing how nutritional calcium influences bone remodeling and calcium balance under different physiological conditions [29].
Iron Bioavailability: Stable iron isotopes (iron-54, -57, -58) provide a safe method for studying iron absorption in vulnerable populations, including children and pregnant women [29]. These studies have elucidated how dietary inhibitors (phytic acid, polyphenols) and enhancers (ascorbic acid, meat factors) influence non-heme iron absorption [24]. The double isotope technique, using two different iron isotopes administered with and without a test meal, allows for within-subject comparisons of iron bioavailability from different dietary sources or processing methods.
Zinc and Other Trace Minerals: Similar approaches using stable isotopes have been applied to zinc, copper, selenium, and other essential trace minerals, generating critical data on their absorption kinetics and metabolic utilization [29].
Macronutrient Metabolism
Stable isotopes provide unique insights into the dynamic aspects of macronutrient metabolism:
Protein Turnover: Amino acids labeled with nitrogen-15, carbon-13, or deuterium allow quantification of whole-body protein turnover and tissue-specific protein synthesis and breakdown rates [23]. These techniques have revealed how dietary protein quality, physical activity, aging, and disease states influence protein metabolism. The fundamental approach involves administering a labeled amino acid and measuring its incorporation into body proteins or appearance as oxidation products.
Carbohydrate Metabolism: Glucose labeled with carbon-13 or deuterium enables investigation of glucose production, disposal, and oxidation [23]. These studies have advanced our understanding of metabolic adaptations in conditions such as diabetes, obesity, and intensive exercise. For example, the use of [1-¹³C]glucose in conjunction with NMR spectroscopy can track glycogen synthesis rates in human liver and muscle [29].
Lipid Metabolism: Fatty acids labeled with carbon-13 or deuterium allow tracing of fatty acid oxidation, incorporation into different lipid fractions, and measurement of lipid kinetics. These approaches have elucidated how dietary fatty acids are partitioned between storage and oxidation, and how this partitioning is altered in metabolic disorders.
Figure 2: Metabolic pathways traced using isotope-labeled nutrients
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of isotope tracer studies requires specialized reagents and materials designed to maintain isotopic integrity and ensure accurate measurements:
Table 3: Essential Research Reagents for Isotope Tracer Studies
| Reagent/Material | Specifications | Application in Research |
|---|---|---|
| Stable Isotope Tracers | Pharmaceutical grade, >98% isotopic purity, sterile and pyrogen-free for human administration | Metabolic tracing of specific nutrients [29] |
| Isotope-Labeled Compounds | Position-specific labeling (e.g., [1-¹³C]glucose, 6,6-²H₂-glucose) with known chemical and isotopic purity | Pathway-specific metabolic studies [23] |
| Calibrated Infusion Pumps | Precision pumps with minimal pulsation, calibrated for accurate delivery rates | Controlled administration of isotope tracers [23] |
| Sample Collection Equipment | Evacuated blood collection tubes, catheters, urine containers | Biological sample acquisition without contamination |
| Derivatization Reagents | HPLC or GC grade reagents for sample preparation (e.g., pentaacetate derivative for glucose) | Preparing samples for GC/MS analysis [23] |
| Mass Spectrometry Standards | Certified reference materials with known isotopic composition | Instrument calibration and quality control [23] |
| Solid Phase Extraction Cartridges | Specific chemistries for analyte isolation (C18, ion exchange, mixed mode) | Sample cleanup and concentration before analysis |
| Isotope Ratio Standards | International measurement standards for specific elements | Accurate quantification of isotopic enrichment |
Data Analysis and Kinetic Modeling
The transformation of isotopic enrichment data into meaningful biological parameters requires appropriate mathematical models that describe the system's behavior:
Basic Kinetic Parameters
The fundamental parameters derived from isotope tracer studies include:
- Rate of Appearance (Ra): The entry rate of a substance into the circulation, calculated from the tracer dilution principle during constant tracer infusion [23]
- Fractional Synthesis Rate (FSR): The fraction of a pool that is synthesized per unit time, determined from the incorporation of labeled precursors into products [23]
- Clearance Rate: The volume of plasma completely cleared of a substance per unit time
- Compartmental Masses: The sizes of different metabolic pools within the body
Compartmental Modeling
Compartmental models represent the body as a series of interconnected pools (compartments) between which the traced substance moves. These models range from simple one-compartment systems to complex multi-compartment structures that more accurately represent biological reality. The model structure is determined by the sampling strategy, with more frequent sampling and multiple sampling sites enabling more complex model configurations.
Steady-State versus Non-Steady-State Models
The simplest kinetic analyses assume metabolic steady state, where production rates equal disposal rates, and pool sizes remain constant. However, many nutritional interventions and physiological states involve non-steady-state conditions, requiring more sophisticated modeling approaches that can account for changing pool sizes and flux rates.
Stable and radioactive isotope methodologies represent the gold standard for assessing nutrient bioavailability in human studies, providing unprecedented insights into the dynamic aspects of human metabolism. These techniques enable researchers to move beyond static measurements to kinetic analyses that reveal how nutrients are absorbed, distributed, metabolized, and excreted. The continued refinement of isotopic methods, coupled with advances in analytical technologies and modeling approaches, will further enhance our understanding of nutrient requirements and metabolism across different physiological states and population groups.
As the field progresses, the integration of isotopic tracer methodology with other 'omics' technologies (genomics, proteomics, metabolomics) promises to provide even more comprehensive understanding of the complex relationships between diet, metabolism, and health. These advances will support the development of more personalized nutritional recommendations and targeted interventions to address global malnutrition challenges.
Animal models serve as indispensable tools in bioavailability research, providing complex living systems to study the absorption, distribution, metabolism, and excretion (ADME) of nutrients and bioactive food compounds. Bioavailability represents the fraction of an ingested nutrient that is absorbed and becomes available for physiological functions or storage, while bioaccessibility refers to the amount of an ingested nutrient that is released from the food matrix and becomes potentially available for absorption [1] [30]. These concepts are fundamental to nutritional sciences and drug development, as they determine the efficacy of dietary components and pharmaceuticals.
The selection of appropriate animal models is crucial for generating translatable data in bioavailability studies. Researchers must consider anatomical, physiological, and metabolic similarities between animal species and humans, alongside practical considerations such as cost, lifespan, and ethical justifications [31]. This document provides a comprehensive framework for the application of animal models in bioavailability research, addressing their suitability, methodological protocols, limitations, and ethical considerations within the context of a broader thesis on nutritional assessment protocols.
Suitability of Different Animal Models
The choice of animal model significantly influences the validity and translational potential of bioavailability research findings. Different models offer distinct advantages and limitations based on their physiological resemblance to humans, handling characteristics, and ethical considerations.
Table 1: Comparative Analysis of Animal Models in Bioavailability Research
| Animal Model | Key Advantages | Major Limitations | Common Applications in Bioavailability |
|---|---|---|---|
| Mouse (Mus musculus) | Short lifespan enabling generational studies; cost-effective; extensive genomic tools [31] [32] | Small size limits blood and tissue sampling; significant metabolic differences from humans [31] | Preliminary screening of nutrient absorption; genetic studies using transgenic models [33] |
| Rat (Rattus norvegicus) | Larger size than mice for easier sampling; well-established physiological data; cost-effective [31] | Not ideal for inflammation studies; limited genetic diversity in inbred strains [31] | Mineral (iron, zinc, calcium) bioavailability; polyphenol and phytochemical metabolism [31] |
| Guinea Pig (Cavia porcellus) | Similar cholesterol metabolism to humans; suitable for asthma and tuberculosis research [31] | High phenotypic variations; limited infectious disease models for some pathogens [31] | Vitamin C bioavailability studies (as they require dietary Vitamin C like humans) [31] |
| Zebrafish (Danio rerio) | High regenerative capacity; rapid development; transparent embryos for visualization [31] | Less physiological resemblance to humans; small size [31] | Early-stage nutrient uptake studies; genetic screening of metabolic pathways [31] |
| Non-Human Primates | Close phylogenetic relationship to humans; similar genetic, biochemical, and psychological activities [31] | Significant ethical constraints; high cost; long maturity period; specialized housing needs [31] | Critical translational studies for vaccines and complex drug metabolism [31] |
Criteria for Model Selection
Choosing an appropriate animal model requires systematic evaluation of several factors:
- Physiological and Pathophysiological Resemblance: The model should replicate key aspects of human digestion, absorption, and metabolism relevant to the nutrient or compound under investigation [31]. For instance, pigs share remarkable similarities with humans in gastrointestinal anatomy and function, making them valuable for certain bioavailability studies.
- Genetic Considerations: Transgenic animal models, produced by incorporating genetic information directly into embryos via foreign DNA injection or retroviral vectors, enable researchers to study specific metabolic pathways or humanized physiological processes [31] [33].
- Practical Constraints: Factors such as animal availability, size, lifespan, housing requirements, and cost must align with research objectives and resources [31]. Small rodents are often preferred for initial screening due to their cost-effectiveness and short reproductive cycles, while larger animals may be necessary for advanced stages of research.
- Ethical Compliance: The principle of the 3Rs (Replacement, Reduction, Refinement) must guide model selection, prioritizing species with lower neurophysiological capacity when scientifically justified [34] [32] [35].
Limitations and Challenges in Translation
Despite their utility, animal models present significant challenges that can compromise the translatability of research findings to human contexts.
Biological and Methodological Constraints
- Species-Specific Variations: Fundamental differences in genetics, gut microbiota, digestive physiology, and metabolic pathways between animals and humans can lead to divergent outcomes in bioavailability studies [36]. For example, a compound that shows promise in animal models may not be beneficial in humans due to these variations [36].
- Artificial Disease Induction: Many models rely on artificially induced disease states (e.g., chemically induced diabetes or fibrosis) that may not accurately replicate the natural progression or complexity of human conditions [36] [37]. The Streptozotocin (STZ)-induced diabetes model, while producing clinical features resembling human diabetes, faces challenges due to the physiochemical properties and toxicities of STZ that can cause animal mortality [31].
- Genetic Homogeneity: Laboratory animals are often inbred, resulting in genetic uniformity that fails to represent the diversity of human populations [31] [36]. This limitation is particularly relevant for nutritional studies, where inter-individual variability in bioavailability is common due to genetic polymorphisms, gut microbiome composition, and environmental factors [1] [33].
Historical Failures in Translation
Several notable cases highlight the limitations of animal models in predicting human responses:
- Thalidomide: In the 1950s, animal testing failed to predict the severe birth defects caused by thalidomide in humans, as the species used (particularly mice) were less sensitive to the drug's teratogenic effects [36].
- TGN1412 Therapeutic Antibody: A potentially fatal immune response in humans was not predicted by prior testing in non-human primates, despite their close evolutionary relationship to humans [36].
- Monoclonal Antibodies for Cancer: Preclinical trials of monoclonal antibodies (mAbs) in animal models are required for clinical application, yet mAbs are often less adapted to animal studies, creating translational challenges [31].
These cases underscore the critical need for careful interpretation of animal data and the development of more human-relevant models.
Ethical Considerations and Evolving Standards
The use of animals in research involves significant ethical considerations that have evolved into structured frameworks and regulations.
The 3Rs Principle and Ethical Oversight
The foundational framework for ethical animal research is the 3Rs principle:
- Replacement: Use of non-animal alternatives (e.g., in vitro models, computer simulations) whenever scientifically feasible [31] [34] [35]. This includes emerging technologies such as organ-on-a-chip systems and advanced computer modeling [34] [35].
- Reduction: Minimizing the number of animals used while maintaining statistical validity, achieved through improved experimental design, sharing of data and resources, and use of advanced imaging techniques that allow longitudinal studies in the same animals [31] [32] [35].
- Refinement: Modifying procedures to minimize pain, suffering, and distress, and enhancing animal welfare throughout their lifetime [31] [34] [32]. This includes improved housing conditions, better anesthesia and analgesia protocols, and humane endpoints.
All animal research protocols must receive approval from institutional animal care and use committees or ethics committees, which evaluate the justification for animal use and ensure compliance with the 3Rs [34] [32].
Evolving Ethical Standards (2024-2025)
Current trends in animal research ethics include several significant developments:
- Integration of Advanced Alternatives: Increased adoption of organoid technology, sophisticated in silico (computer-based) modeling, and 3D-bioprinted tissues to reduce reliance on animal models [35].
- Enhanced Transparency: Movement toward mandatory pre-registration of animal studies to combat publication bias and improve research quality [35].
- Global Harmonization: Efforts to standardize ethical standards across international borders to ensure consistent animal welfare protections in collaborative research [35].
- Advanced Non-Invasive Imaging: Use of technologies that enable longitudinal monitoring of the same animals, reducing overall animal numbers while collecting comprehensive data [35].
The ethical decision-making process for animal research can be visualized as a sequential workflow:
Experimental Protocols for Bioavailability Assessment
This section outlines standardized protocols for assessing nutrient bioavailability using animal models, with emphasis on methodological rigor and translational relevance.
Protocol 1: Mineral Bioavailability Using Dialyzability Assay
The dialyzability method estimates mineral bioaccessibility by measuring the fraction that becomes soluble and dialyzable during simulated gastrointestinal digestion [30].
Materials and Reagents:
- Pepsin (from porcine stomach): For gastric protein digestion
- Pancreatin: Provides pancreatic enzymes (amylase, lipase, proteases)
- Bile salts: Emulsifiers that facilitate lipid digestion and micelle formation
- Dialysis tubing: With appropriate molecular weight cutoff (typically 6-8 kDa)
- Atomic Absorption Spectrophotometry (AAS) or ICP-AES: For mineral quantification
Procedure:
- Sample Preparation: Homogenize the test food material and weigh duplicate samples.
- Gastric Phase: Add pepsin solution (e.g., 0.2 g in 10 mL of 0.1M HCl) to adjust pH to 2.0. Incubate at 37°C for 1-2 hours with continuous agitation.
- Intestinal Phase: Neutralize the gastric digest to pH 5.5-6.0, then add pancreatin-bile extract mixture (e.g., 0.15 g pancreatin and 0.75 g bile extract in 25 mL of 0.1M NaHCO₃). Adjust final pH to 6.5-7.0.
- Dialysis: Place the intestinal digest in dialysis tubing and incubate at 37°C for 30-120 minutes.
- Analysis: Collect the dialysate and analyze mineral content using appropriate analytical methods (AAS, ICP-AES).
- Calculation: Calculate dialyzability as (mineral content in dialysate / total mineral content in test sample) × 100.
Validation Notes: This method has been applied to study bioaccessibility of calcium, zinc, iron, and magnesium. It provides a useful screening tool but may not fully predict in vivo bioavailability due to the absence of absorptive cellular mechanisms [30].
Protocol 2: Cellular Bioavailability Using Caco-2 Cell Model
The Caco-2 cell model, derived from human colonic adenocarcinoma, exhibits enterocyte-like differentiation and is widely used to study nutrient uptake and transport [30].
Materials and Reagents:
- Caco-2 cells: Human epithelial colorectal adenocarcinoma cells (ATCC HTB-37)
- Transwell inserts: Permeable supports for cell culture and transport studies
- Dulbecco's Modified Eagle Medium (DMEM): Cell culture medium with high glucose
- Fetal Bovine Serum (FBS): Serum supplement for cell culture media
- Hanks' Balanced Salt Solution (HBSS): For transport assays
- Enzyme inhibitors: To protect cells from digestive enzymes
Procedure:
- Cell Culture: Maintain Caco-2 cells in DMEM with 10% FBS, 1% non-essential amino acids, and 1% penicillin-streptomycin at 37°C in 5% CO₂.
- Seeding: Seed cells on Transwell inserts at high density (e.g., 1×10⁵ cells/insert) and culture for 14-21 days to allow differentiation and tight junction formation.
- Transepithelial Electrical Resistance (TEER) Monitoring: Measure TEER regularly using an epithelial voltohmmeter to confirm monolayer integrity.
- Sample Preparation: Subject test material to in vitro gastrointestinal digestion as described in Protocol 1.
- Bioavailability Assay: Apply the digested sample to the apical compartment. Incubate at 37°C for specified time periods.
- Sampling: Collect samples from both apical and basolateral compartments at predetermined time points.
- Analysis: Quantify nutrient or compound of interest in both compartments using HPLC, MS, or other appropriate analytical methods.
- Calculation: Determine apparent permeability coefficient (Papp) using the formula: Papp = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the membrane surface area, and C₀ is the initial concentration.
Validation Notes: The Caco-2 model allows study of uptake, transport, and interactions between nutrients at the absorption site. However, it lacks the complexity of in vivo systems, including hormonal regulation, blood flow, and enteric nervous system input [30].
Protocol 3: In Vivo Nutrient Absorption and Metabolism
This protocol outlines a comprehensive approach for assessing nutrient bioavailability in rodent models.
Materials and Reagents:
- Animal model: Typically rats or mice of specific pathogen-free status
- Metabolic cages: For separate collection of urine, feces, and possible expired air
- Test compound: Isotopically labeled nutrients (e.g., ¹³C, ¹⁵N, ²H) for precise tracing
- Anesthesia: Ketamine/xylazine or isoflurane for blood collection and tissue sampling
- Anticoagulants: Heparin or EDTA for blood collection
- Tissue homogenization buffers: Phosphate-buffered saline or specific lysis buffers
Procedure:
- Acclimatization: House animals in controlled conditions with free access to standardized diet and water for at least 7 days prior to experimentation.
- Experimental Diet: Formulate diets with precise nutrient composition, incorporating the test compound (preferably isotopically labeled for accurate tracing).
- Dosing: Administer test compound via oral gavage or incorporate into diet. For kinetic studies, fast animals overnight prior to dosing.
- Sample Collection:
- Blood: Collect at multiple time points via tail vein, orbital sinus, or cardiac puncture under anesthesia.
- Urine and Feces: Collect over specified periods (e.g., 0-24h, 24-48h) using metabolic cages.
- Tissues: Euthanize animals at predetermined time points and collect relevant tissues (liver, kidney, intestine, etc.).
- Sample Analysis:
- Plasma/Serum: Separate via centrifugation and analyze for nutrient and metabolite concentrations using HPLC-MS, GC-MS, or ELISA.
- Tissues: Homogenize and extract for nutrient and metabolite analysis.
- Feces: Analyze for excreted test compound and metabolites.
- Pharmacokinetic Analysis: Calculate bioavailability using non-compartmental analysis: F = (AUCₒᵣₐₗ × Dᵢᵥ)/(AUCᵢᵥ × Dₒᵣₐₗ) × 100, where AUC is area under the concentration-time curve and D is dose.
Validation Notes: This approach provides the most comprehensive assessment of bioavailability but requires significant resources and raises ethical considerations regarding animal use. Isotopic labeling provides the most accurate quantification of absorption and metabolism [1] [30].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Materials for Bioavailability Studies
| Category | Specific Items | Function/Application | Examples/Notes |
|---|---|---|---|
| Digestive Enzymes | Pepsin, Pancreatin, Bile salts | Simulate gastrointestinal digestion in vitro | Porcine-derived enzymes most common; concentration and activity must be standardized [30] |
| Cell Cultures | Caco-2 cells, HT-29 cells, Enteroids | Intestinal absorption models | Caco-2 requires 14-21 days for full differentiation; enteroids provide more physiologically relevant but complex models [30] |
| Analytical Instruments | HPLC, LC-MS/MS, AAS, ICP-MS | Quantification of nutrients and metabolites | Mass spectrometry methods offer highest sensitivity and specificity for compound quantification [30] |
| Isotopic Tracers | ¹³C, ¹⁵N, ²H-labeled compounds | Precise tracking of nutrient fate | Allow discrimination between administered dose and endogenous pools; essential for accurate bioavailability determination [1] |
| Animal Models | Rodents (mice, rats), Non-human primates | In vivo absorption and metabolism studies | Choice depends on research question, budget, and ethical considerations; transgenic models available for specific pathways [31] [33] |
| Specialized Equipment | Metabolic cages, Transwell inserts, TIM system | Specialized experimental setups | Metabolic cages allow separate collection of urine and feces; TIM system simulates human gastrointestinal dynamics [30] |
Integrated Approaches and Future Directions
The limitations of individual models have spurred the development of integrated approaches that combine multiple methods to enhance predictive accuracy.
Complementary Methodologies
- In Silico Treatment (IST) Framework: This computational approach analyzes gene expression data from both humans and animal models to quantify how closely animal models align with human conditions [37]. IST simulates changes observed in animals onto human data, providing a quantitative measure of translatability and assisting in optimal model selection for specific research questions [37].
- Multi-omics Integration: Combining genomics, transcriptomics, metabolomics, and metagenomics data from both animal and human studies helps identify conserved pathways and species-specific differences that affect nutrient bioavailability [33].
- Sophisticated In Vitro Systems: The TNO Intestinal Model (TIM) is a computer-controlled system that simulates human digestive parameters including body temperature, digestive secretions, peristalsis, and transit times [30]. When coupled with cellular models, it provides a powerful tool for studying bioaccessibility and bioavailability.
The relationship between different bioavailability assessment methods and their applications can be visualized as follows:
Emerging Technologies and Future Perspectives
The field of bioavailability research is rapidly evolving with several promising developments:
- Organ-on-a-Chip Technology: Microfluidic devices containing human cells that simulate organ-level functionality, offering more physiologically relevant models for nutrient absorption and metabolism [34] [35].
- 3D-Bioprinted Tissues: Engineered tissues that replicate the complex structure and function of human intestinal epithelium, including villi and crypt structures [35].
- Gut Microbiome Integration: Advanced co-culture systems that incorporate human gut microbiota to better simulate the complex interactions between nutrients, host cells, and microorganisms [1] [33].
- Precision Nutrition Approaches: Recognition that bioavailability varies significantly between individuals due to genetic polymorphisms, gut microbiome composition, and other factors, driving the development of personalized assessment models [33].
These innovations promise to enhance the predictive accuracy of bioavailability assessment while reducing reliance on animal models through the principles of the 3Rs.
The bioavailability of nutrients, defined as the proportion of an ingested nutrient that is absorbed and becomes available for normal physiological functions, is a critical determinant of the nutritional value of foods [4] [38]. Research in this field requires robust methods to predict how food matrices behave during digestion and release their components for intestinal absorption. In vivo studies involving human or animal subjects, while valuable, are often hampered by ethical concerns, high costs, significant inter-individual variability, and practical limitations [39] [40]. Consequently, in vitro digestion models have become indispensable tools for the rapid screening of foods and delivery systems, allowing researchers to study digestibility, nutrient release, and bioaccessibility under controlled, reproducible conditions [39] [41].
This article provides Application Notes and Protocols for employing these models within the context of a research thesis focused on assessing nutrient bioavailability. It covers the principles of the widely adopted standardized static method (INFOGEST), introduces more advanced dynamic systems, and presents detailed experimental protocols suitable for researchers and scientists in food science, nutrition, and pharmaceutical development.
In vitro digestion models are laboratory systems that simulate the physiological conditions of the human gastrointestinal (GI) tract. They can be broadly categorized into static and dynamic models [40] [42]. Static models are single-compartment systems that simulate digestion in a batch process, with fixed conditions of pH, enzyme concentrations, and incubation times for each GI compartment (oral, gastric, intestinal). In contrast, dynamic models are multi-compartmental systems that incorporate the gradual changes and physical forces (e.g., peristalsis, gastric emptying) characteristic of human digestion [43].
The choice of model depends on the research question. While dynamic models offer a more physiologically realistic simulation, static models are valuable for high-throughput screening due to their simplicity, reproducibility, and low cost [39] [42]. A significant advancement in the field was the development of the INFOGEST standard static protocol, which has harmonized experimental conditions across laboratories, enabling direct comparison of results worldwide [44].
Table 1: Classification and Characteristics of Major In Vitro Digestion Models.
| Model Type | Key Features | Advantages | Limitations | Primary Applications |
|---|---|---|---|---|
| Static (e.g., INFOGEST) | Fixed pH, incubation time, and enzyme activity per phase; single compartment [44]. | Simple, cost-effective, high reproducibility, suitable for rapid screening, low reagent volume [40] [42]. | Over-simplified, does not simulate dynamic physiological processes [42]. | End-point bioaccessibility studies; digestibility of macronutrients; screening emulsion-based delivery systems [39] [44]. |
| Semi-Dynamic | Incorporates key dynamics in the gastric phase (gradual acidification, enzyme addition, gastric emptying) while keeping the intestinal phase static [42]. | Better approximation of gastric digestion than static models; more affordable and simpler than full dynamic systems [42]. | Intestinal phase remains static; may not replicate full GI complexity. | Studying gastric breakdown kinetics; testing expensive drugs or nano-engineered materials [42]. |
| Dynamic (e.g., TIM, DGM, HGS) | Multi-compartmental; simulates peristalsis, continuous flow, real-time pH adjustment, and gastric emptying [43]. | Closer mimicry of in vivo conditions; allows for time-resolved analysis [42] [43]. | Complex, expensive, requires large volumes of reagents, time-consuming [42]. | Mechanistic studies on food disintegration; validating static model findings; pharmaceutical development [43]. |
The INFOGEST Standardized Static Protocol: A Detailed Methodology
The INFOGEST protocol is a consensus static method that simulates the oral, gastric, and intestinal phases of digestion [44]. The following is a detailed application note for its use in assessing the bioaccessibility of nutrients from a food sample.
Research Reagent Solutions
Table 2: Essential Reagents for the INFOGEST In Vitro Digestion Protocol.
| Reagent / Enzyme | Simulated Fluid | Typical Concentration / Activity | Physiological Function |
|---|---|---|---|
| α-Amylase | Simulated Salivary Fluid (SSF) | 75 U/mL in oral phase [44] | Initiates starch hydrolysis in the mouth [41]. |
| Pepsin | Simulated Gastric Fluid (SGF) | 2000 U/mL in gastric phase [44] | Primary protease in the stomach, breaks down proteins [41]. |
| Pancreatin | Simulated Intestinal Fluid (SIF) | Trypsin activity 100 U/mL in intestinal phase [44] | Enzyme mixture containing proteases, lipases, and amylases for small intestinal digestion [44]. |
| Bile Salts | SIF | 10 mM in intestinal phase [44] | Emulsifies lipids, facilitating lipolysis and formation of mixed micelles for lipid absorption [39]. |
| Calcium Chloride (CaCl₂) | SSF, SGF, SIF | 0.75 mM in gastric phase, 0.3 mM in intestinal phase [45] | Cofactor for several enzymes; impacts emulsion stability and lipid digestion [45]. |
Step-by-Step Experimental Protocol
Pre-digestion Sample Preparation:
- For solid foods, homogenize and standardize the particle size. A common approach is to use a sieve to obtain a particle size of <2 mm [41].
- For emulsions, characterize the initial droplet size and ζ-potential.
Workflow Overview:
Phase 1: Oral Digestion
- Incubation: Mix the food sample with Simulated Salivary Fluid (SSF) in a 1:1 ratio (e.g., 5 g food + 5 mL SSF).
- Conditions: Adjust pH to 7.0 using 1M HCl or 1M NaOH.
- Enzyme: Add human salivary α-amylase to a final activity of 75 U/mL in the final mixture.
- Time: Incubate in a shaking water bath at 37°C for 2 minutes to simulate the short oral residence time [44].
Phase 2: Gastric Digestion
- Initiation: Combine the entire oral bolus with an equal volume of Simulated Gastric Fluid (SGF).
- Conditions: Adjust the pH of the mixture to 3.0.
- Enzyme: Add porcine pepsin to a final activity of 2000 U/mL in the final mixture.
- Time: Incubate at 37°C with continuous agitation for 2 hours to simulate a typical gastric residence time [44].
Phase 3: Intestinal Digestion
- Initiation: Transfer the entire gastric chyme to a new vessel. Add an equal volume of Simulated Intestinal Fluid (SIF).
- Conditions: Adjust the pH to 7.0.
- Enzymes & Bile: Add pancreatin (trypsin activity at 100 U/mL in the final mixture) and bile salts (final concentration of 10 mM).
- Time: Incubate at 37°C with continuous agitation for 2 hours [44].
Termination and Analysis:
- To stop the enzymatic reaction, immediately place the intestinal digest on ice or use specific enzyme inhibitors.
- Centrifuge the digest (e.g., at 40,000 x g for 1 hour at 4°C) to separate the aqueous phase (containing bioaccessible compounds) from the solid residue and oil droplets.
- Analyze the aqueous phase (the bioaccessible fraction) for nutrients of interest (e.g., peptides, fatty acids, carotenoids, minerals) using appropriate analytical methods (HPLC, GC, spectrophotometry).
Advanced Model: Semi-Dynamic Gastric Digestion
For a more realistic simulation of gastric processing, a semi-dynamic approach can be adopted, as proposed by the INFOGEST network [42]. This model focuses on incorporating dynamics during the gastric phase.
Protocol for Semi-Dynamic Gastric Digestion
Principle: This method simulates the gradual acidification of the stomach and the controlled emptying of gastric contents into the intestine, rather than using a single pH adjustment and batch incubation.
Workflow for Semi-Dynamic Gastric Phase:
Key Steps:
- After the oral phase, the bolus is introduced into the gastric compartment at an initial pH of ~5.0, mimicking the dilution and buffering capacity of the meal [41].
- The pH is gradually decreased to 2.0 over a period of 90 minutes using a pH-stat titrator or a syringe pump delivering HCl, simulating the secretion of gastric acid.
- Simulated gastric fluid (with pepsin) is added gradually throughout the gastric phase.
- Gastric emptying is simulated by transferring small volumes of gastric chyme (e.g., corresponding to an energy delivery rate of 2-4 kcal/min) to the intestinal compartment at regular intervals [42].
- The intestinal phase is then typically conducted as a static incubation, as described in Section 3.2.
Table 3: Quantitative Parameters for Simulating Gastric Conditions in a Semi-Dynamic Model.
| Parameter | Simulated Physiological Condition | In Vitro Model Value | Justification |
|---|---|---|---|
| Initial Gastric pH | Increase in gastric pH after meal ingestion [41]. | Start at pH 5.0 | Mimics the buffering capacity of food. |
| Final Gastric pH | Fasting state gastric acidity [41]. | pH 2.0 after 1.5-2 h | Simulates the restoration of acidic conditions. |
| Gastric Emptying Rate | Caloric emptying from the human stomach [42]. | 2 - 4 kcal/min | A physiologically relevant rate for many meals. |
| Gastric Contractions | Antral contraction waves for mixing and grinding [43]. | Several Newton force [41] | Simulates physical forces that breakdown food particles. |
Data Interpretation and Application in Nutrient Bioavailability Research
Data from in vitro digestion models are used to calculate bioaccessibility, defined as the fraction of a nutrient that is released from the food matrix and is available for intestinal absorption [38] [22].
Calculation:
% Bioaccessibility = (Amount of nutrient in the bioaccessible fraction / Total amount of nutrient in the original food) × 100
Linking to Broader Thesis Research:
- The bioaccessible fraction obtained from the in vitro digestion can be further applied to cell culture models (e.g., Caco-2 cells simulating the intestinal epithelium) to study uptake and transport, providing a more comprehensive assessment of bioavailability [45].
- In vitro digestion results can be correlated with in vivo data from animal or human studies to validate the model's predictive power. For instance, the lipid digestion profile obtained using the pH-stat method has shown good correlation with in vivo feeding studies [45].
- This integrated approach allows for the screening of various food structures (e.g., emulsions, gels) and formulations to design foods that control the rate and extent of nutrient digestion, which is crucial for applications in satiety control and targeted nutrient delivery [39] [41].
Predictive algorithms are revolutionizing the assessment of nutrient bioavailability, moving scientific inquiry beyond static chemical composition tables toward dynamic, systems-level understanding. Within the context of food and nutritional sciences, these mathematical models integrate multifaceted data on food composition, gastrointestinal digestion, host physiology, and genetic factors to predict the fraction of iron, zinc, and protein that is absorbed and utilized by the body. The shift from traditional, resource-intensive in vivo studies toward in silico and integrated approaches addresses a critical need for precision, efficiency, and scalability in research and development [46] [47]. This document outlines key predictive modeling approaches and provides detailed application protocols for researchers investigating the bioavailability of these essential nutrients, framing them within a comprehensive thesis on bioavailability assessment protocols.
Different mathematical frameworks are employed to predict nutrient bioavailability, each with distinct strengths, limitations, and applications. The choice of model depends on the research objective, whether it is optimizing population-level diets, understanding absorption mechanisms, or predicting outcomes for novel food ingredients.
Table 1: Comparison of Key Predictive Modeling Approaches for Nutrient Bioavailability
| Model Type | Primary Application | Key Features | Advantages | Limitations |
|---|---|---|---|---|
| Linear Programming (LP) | Diet optimization to meet nutrient requirements at minimal cost or deviation from habitual intake [48]. | Uses linear equations to define constraints (e.g., nutrient requirements, food intake limits) and an objective function. | Computationally efficient; widely used for formulating food-based recommendations. | Cannot natively handle nonlinear processes like iron and zinc absorption; may identify "problem nutrients" like iron and zinc that local diets cannot adequately meet [49] [48]. |
| Nonlinear Programming (NLP) & Piecewise Linear Approximation (PLA) | Modeling nonheme iron and zinc absorption, which follows nonlinear saturation kinetics [49]. | NLP solves nonlinear equations directly; PLA approximates them with a series of linear segments. | Improves accuracy of diet models for absorbable iron and zinc; PLA can find accurate solutions efficiently [49]. | Computationally intensive; NLP may hit time limits or fail to find optimal solutions, especially in mixed-integer models [49]. |
| AI/Machine Learning (ML) | Predicting complex, nonlinear relationships between food composition, matrix effects, processing, and bioavailability [47] [50]. | Learns patterns from large datasets using algorithms like Random Forest, Deep Learning, and Natural Language Processing. | Capable of modeling highly complex interactions; can integrate multi-omics data for precision nutrition [47] [15]. | Requires large, high-quality datasets; models can be "black boxes" lacking explainability [47] [50]. |
| In Silico Digestion Models | Predicting protein digestibility and the release of peptides/amino acids [51]. | Simulates gastrointestinal conditions and enzymatic cleavage using computational bioinformatics. | Rapid, cost-effective, and reduces need for in vivo testing; useful for novel protein safety screening [51]. | Does not fully capture complex physiological factors (e.g., protein folding, dynamic gut environment); requires validation [51]. |
| Flux Balance Analysis (FBA) | Modeling metabolic fluxes in plants or gut microbes to understand nutrient synthesis and utilization [52]. | A constraint-based method that analyzes flow of metabolites through a biological network. | Provides a system-wide view of metabolism without requiring detailed kinetic parameters. | Lacks temporal dynamics and regulatory information; results are sensitive to model constraints [52]. |
Model Selection Workflow: A decision flow for selecting a predictive modeling approach based on the research objective.
Experimental Protocols
Protocol 1: Modeling Nonheme Iron and Zinc Absorption Using Nonlinear Programming and Piecewise Linear Approximation
Objective: To accurately model the absorption of nonheme iron and zinc from a diet or meal plan using nonlinear absorption equations and solve the diet model using Nonlinear Programming (NLP) or Piecewise Linear Approximation (PLA) [49].
Background: The absorption of nonheme iron and zinc is not linear but follows a saturable, nonlinear trajectory dependent on dietary composition and body status. Standard Linear Programming (LP) is insufficient for this task, requiring more advanced mathematical techniques [49].
Materials and Reagents
- Dietary Data: Food consumption data from national surveys (e.g., NHANES) or experimental diets.
- Food Composition Database: A detailed database containing total iron, zinc, and absorption modifiers (e.g., phytate, ascorbic acid, animal protein).
- Software: Optimization software capable of NLP and MILP (e.g., GAMS, MATLAB, Python with SciPy/Pyomo). Standard LP software can be used for PLA.
Methodology
Step 1: Define the Absorption Equations
- For nonheme iron, use a published equation that incorporates the effect of dietary modifiers. A common form is a logistic or saturation-type equation where the absorption fraction is a function of phytate, ascorbic acid, and other enhancers/inhibitors.
- For zinc, use an equation that similarly accounts for the inhibitory effect of dietary phytate on absorption, often derived from saturation kinetics models.
Step 2: Develop the Diet Optimization Model
- Decision Variables: Amounts of each food item in the optimized diet.
- Objective Function: Minimize total diet cost or minimize deviation from the observed diet, while maximizing absorbable iron and/or zinc.
- Constraints:
- Nutrient Constraints: Ensure the diet meets requirements for other key nutrients (protein, calcium, etc.).
- Food Group Constraints: Define acceptable intake ranges for food groups based on cultural or practical consumption patterns.
- Energy Constraint: Set total energy intake to a fixed level or within a specific range.
- Nonlinear Absorption Constraint: Integrate the equations from Step 1 as constraints to calculate total absorbable iron and zinc.
Step 3: Implement the Solver (NLP vs. PLA)
- Nonlinear Programming (NLP) Approach: Input the full nonlinear model into an NLP solver. Set convergence tolerances and, if necessary, a time limit (e.g., 1 hour).
- Piecewise Linear Approximation (PLA) Approach:
- Discretize the range of possible intake for key absorption modifiers (e.g., phytate).
- For each segment, linearize the absorption equation.
- Use binary variables to activate only the linear segment corresponding to the phytate level in the solution.
- Solve the resulting Mixed-Integer Linear Programming (MILP) model.
Step 4: Model Validation and Analysis
- Run the model for various scenarios (e.g., different population groups, cost constraints).
- Compare the solution quality (value of the objective function) and computational time between NLP and PLA.
- Validate the predicted absorbable mineral values against clinical data if available.
Protocol 2: AI-Enhanced Prediction of Nutrient Bioavailability
Objective: To develop a machine learning model that predicts the bioavailability of iron, zinc, or protein from food composition and processing data [47] [50].
Background: AI can identify complex, non-linear patterns in multifaceted datasets that are difficult to model with traditional equations. This is particularly useful for predicting the bioavailability of nutrients from novel foods or complex matrices.
Materials and Reagents
- Dataset: A curated dataset containing features such as:
- Food Composition: Proximate analysis, vitamin/mineral content, antinutritional factors (phytate, tannins).
- Food Matrix Properties: Protein structure, carbohydrate type, lipid profile, dietary fiber.
- Processing Conditions: Temperature, time, pH, fermentation.
- Host Factors (if available): Genetic variants (e.g., BCO1 for carotenoids), gut microbiota data.
- Bioavailability Label: The target variable, obtained from in vivo, in vitro, or clinical studies.
- Software: Python (with scikit-learn, TensorFlow/PyTorch, pandas) or R.
Methodology
Step 1: Data Preprocessing and Feature Engineering
- Handle Missing Data: Use imputation strategies (mean/median, k-nearest neighbors) or remove features/instances with excessive missingness.
- Feature Scaling: Normalize or standardize numerical features.
- Categorical Encoding: Use one-hot encoding for categorical variables like food category.
- Feature Selection: Use correlation analysis and feature importance scores to select the most predictive features and reduce overfitting.
Step 2: Model Selection and Training
- Split the dataset into training (e.g., 70%), validation (e.g., 15%), and test (e.g., 15%) sets.
- Train and compare multiple algorithms:
- Random Forest: Robust for small-to-medium datasets and provides feature importance.
- Gradient Boosting Machines (e.g., XGBoost): Often high performance on tabular data.
- Neural Networks: For very large and complex datasets.
- Use the validation set for hyperparameter tuning via grid or random search.
Step 3: Model Validation and Interpretation
- Performance Metrics: Evaluate the final model on the held-out test set using R², Mean Absolute Error (MAE), and Root Mean Squared Error (RMSE).
- Model Interpretation: Use techniques like SHAP (SHapley Additive exPlanations) to interpret model predictions and identify which features most drive bioavailability outcomes.
Protocol 3: In Silico Assessment of Protein Digestibility
Objective: To computationally predict the digestibility of a novel or modified protein using bioinformatics tools that simulate gastrointestinal proteolysis [51].
Background: Protein digestibility is a key determinant of its nutritional quality and safety. In silico models simulate the action of digestive proteases (e.g., pepsin, trypsin) on a protein's amino acid sequence, predicting its breakdown and potential resistance to digestion—a characteristic of some allergens.
Materials and Reagents
- Protein Sequence: The primary amino acid sequence of the target protein in FASTA format.
- Software/Tools:
- PeptideCutter (ExPASy): Predicts potential protease cleavage sites.
- BIOPEP-UWM Database: Contains profiles of proteolytic enzyme activities.
- Molecular Docking Software (e.g., AutoDock Vina): To predict interactions between resistant peptides and human transporters or receptors.
Methodology
Step 1: Define Proteolysis Conditions
- Select the relevant digestive enzymes (e.g., pepsin at pH 1.3 and 2.0, trypsin, chymotrypsin).
- Set enzyme-specific cleavage rules (e.g., pepsin cleaves N-terminal of Phe, Leu, Trp).
Step 2: Perform In Silico Digestion
- Input the protein sequence into a tool like PeptideCutter.
- Run the analysis for the selected suite of enzymes.
- The output will be a list of potential cleavage sites and the resulting peptide fragments.
Step 3: Analyze Results
- Calculate the theoretical digestibility based on the number of cleavage sites and the size of the resulting peptides.
- Identify large, resistant peptide fragments (>9 amino acids) that may have allergenic or bioactive potential.
- For resistant peptides, use docking studies to predict affinity for human intestinal transporters (e.g., hPEPT1) [51].
Step 4: Validation
- Correlate in silico predictions with in vitro digestibility assays (e.g., using the INFOGEST standardized protocol) to validate and refine the model.
Nutrient Absorption Pathway: Key transporters and modifiers for iron, zinc, and protein/peptide absorption in the enterocyte.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Bioavailability Modeling
| Item Name | Function/Application | Key Considerations |
|---|---|---|
| Caco-2 Cell Line | An in vitro model of the human intestinal epithelium used to study and validate the absorption of iron, zinc, and peptides [53]. | Differentiate for 14-21 days to form tight junctions and express relevant transporters. Often used to calibrate and validate in silico and AI models. |
| TIM-1 (TNO Gastrointestinal Model) | A dynamic, computer-controlled in vitro system that simulates the stomach and small intestine [51]. | Provides highly controlled, reproducible data on nutrient bioaccessibility under simulated human physiological conditions. Used for generating training data for AI models. |
| Pepsin (from Porcine Gastric Mucosa) & Pancreatin | Essential enzymes for in vitro protein digestibility assays and INFOGEST simulated digestion protocols [51]. | Enzyme activity and purity must be standardized to ensure reproducible results between laboratories. |
| Phytic Acid (Sodium Salt) | A key antinutritional factor used in in vitro and in vivo studies to standardize the inhibitory effect on iron and zinc absorption [53]. | Used to create calibration curves for dose-response studies in mineral absorption models. |
| Optifood / NutVal Software | Linear programming software packages specifically designed for diet optimization and identifying nutrient gaps in populations [48]. | Used to formulate Food-Based Recommendations (FBRs) and identify "problem nutrients" like iron and zinc. |
| GastroPlus (Simulations Plus) | A PBPK (Physiologically Based Pharmacokinetic) modeling platform that can be adapted to simulate nutrient and peptide absorption in the GI tract [51]. | A sophisticated tool for predicting internal exposure; its digital TIM-1 module can simulate GI behavior. |
| BIOPEP-UWM Database | A database of bioactive peptides and profiles of proteolytic enzymes, used for in silico protein digestion prediction [51]. | Critical for predicting potential cleavage sites and the release of bioactive peptides during digestion. |
Overcoming Bioavailability Challenges: Anti-Nutrients, Matrix Effects, and Processing
Anti-nutritional factors (ANFs) are naturally occurring compounds in plant-based foods that can interfere with the digestion, absorption, and utilization of nutrients [54]. While research confirms that whole plant foods are associated with reduced risk of chronic diseases, the presence of ANFs represents a critical consideration in nutritional science and food research [55]. For researchers investigating nutrient bioavailability, understanding these compounds is paramount, as they can significantly impact the fraction of nutrients that become available for use and storage in the body [3] [4]. This application note provides a structured framework for identifying, quantifying, and mitigating four major anti-nutrients—phytates, oxalates, tannins, and lectins—within the context of bioavailability research protocols.
The dual nature of many anti-nutrients adds complexity to their study. While traditionally viewed as detrimental due to their mineral-binding and enzyme-inhibiting properties, many also demonstrate potential beneficial effects at appropriate concentrations, including antioxidant, anti-carcinogenic, and cardioprotective activities [55] [56]. This paradox necessitates precise analytical approaches that can differentiate between concentration-dependent effects and inform processing strategies that maximize nutritional quality while preserving potential health-promoting properties.
Anti-Nutrient Profiles and Analytical Considerations
Characteristic Profiles of Key Anti-Nutrients
Table 1: Profile of Major Anti-Nutrients in Plant Foods
| Anti-Nutrient | Primary Food Sources | Main Nutritional Concerns | Potential Beneficial Effects |
|---|---|---|---|
| Phytates | Legumes, cereal grains, nuts, seeds (soybeans: 1.15–3.23% raffinose) [54] [57] | Inhibits absorption of Fe, Zn, Ca, Mg; reduces protein digestibility [55] [54] | Antioxidant via iron chelation; anti-neoplastic effects; reduces risk of kidney stones [55] [58] [56] |
| Oxalates | Spinach (900–1000 mg/100g raw), Swiss chard, rhubarb, beetroot, nuts [55] [58] | Binds Ca, Mg; may inhibit calcium absorption; contributes to kidney stone formation [55] [58] | Plant calcium regulation; insect resistance [58] |
| Tannins | Tea, cocoa, grapes, berries, apples, stone fruits, nuts, beans, whole grains [55] [54] | Inhibits iron absorption; negatively impacts iron stores; reduces protein digestibility [55] [54] | Antioxidant; anti-inflammatory; antimicrobial; cardiovascular protection [54] [56] |
| Lectins | Legumes (raw soybeans: highest activity), cereal grains, seeds, nuts [55] [54] | Alters gut function; induces intestinal hyperplasia; reduces nutrient absorption [55] | Plant defense mechanism; potential antimicrobial and antitumor properties [56] |
Quantitative Assessment of Anti-Nutrient Concentrations
Table 2: Anti-Nutrient Concentration Ranges and Reduction Potentials
| Anti-Nutrient | Representative Concentration in Raw Sources | Effective Reduction Methods | Maximum Reduction Efficiency |
|---|---|---|---|
| Phytates | Defatted soy flour: 1.15–3.23% raffinose [57] | Soaking, germination, fermentation, enzymatic treatment [54] | Up to 95% through combined processing [54] |
| Oxalates | Raw spinach: 900–1000 mg/100g [58] | Boiling (70–80% reduction), soaking, pairing with calcium [55] [58] | 70–80% through boiling [58] |
| Tannins | Varies by cultivar and growing conditions [55] | Cooking, peeling skins, fermentation, germination [55] [54] | Significant reduction through processing [54] |
| Lectins | Raw Canadian legumes: soybeans (692.8 HU/mg), common beans (87.69–88.59 HU/mg) [55] | Boiling (93.77–99.81% reduction), autoclaving, fermentation [55] | 99.81% through boiling for 1 hour at 95°C [55] |
Experimental Protocols for Anti-Nutrient Analysis
Protocol 1: Phytate Quantification and Mineral Bioavailability Assessment
Principle: Phytate (myo-inositol hexakisphosphate) chelates divalent and trivalent cations, reducing mineral bioavailability. This protocol quantifies phytate content and assesses its impact on mineral absorption.
Materials:
- Sample: Finely ground legume or cereal flour
- Reagents: Phytic acid standard, Wade reagent (0.03% FeCl₃·6H₂O and 0.3% sulfosalicylic acid in distilled water), anion-exchange resin (AG 1-X4)
- Equipment: Spectrophotometer, centrifuge, water bath, shaker
Procedure:
- Extraction: Extract 1g sample with 20mL of 2.4% HCl for 2 hours with continuous shaking at room temperature.
- Purification: Centrifuge at 10,000 × g for 15 minutes. Collect supernatant and adjust pH to 3.5–4.0 with NaOH.
- Column Separation: Load onto anion-exchange column pre-equilibrated with 0.5M NaCl. Elute phytate with 0.7M NaCl and collect eluate.
- Colorimetric Determination: Mix 1mL eluate with 1mL Wade reagent. Incubate at room temperature for 10 minutes. Centrifuge at 5000 × g for 10 minutes.
- Measurement: Measure absorbance of supernatant at 500nm. Calculate phytate concentration from standard curve.
- Bioavailability Assessment: For mineral bioavailability, employ Caco-2 cell models or in vivo studies with stable isotopes to determine fractional absorption of iron, zinc, and calcium in presence of quantified phytate [3] [4].
Validation: Include certified reference materials where available. For intra-assay precision, maintain CV < 10%.
Protocol 2: Oxalate Analysis via HPLC and Kidney Stone Risk Assessment
Principle: Oxalic acid forms insoluble salts with calcium, reducing calcium bioavailability and potentially forming kidney stones. This protocol quantifies soluble and total oxalates.
Materials:
- Sample: Homogenized plant material
- Reagents: Oxalic acid standard, 2N HCl, 0.2N NaOH, amyl alcohol, ethylene glycol, sulfuric acid, chromotropic acid
- Equipment: HPLC with UV detector, hot water bath, centrifuge
Procedure:
- Soluble Oxalate Extraction: Extract 0.5g sample with 20mL deionized water at 80°C for 15 minutes. Centrifuge at 10,000 × g for 20 minutes. Collect supernatant.
- Total Oxalate Extraction: For total oxalate, extract residue from step 1 with 20mL 2N HCl at 80°C for 15 minutes. Centrifuge and collect supernatant.
- Derivatization (Alternative Method): Mix extract with chromotropic acid in sulfuric acid. Heat at 100°C for 30 minutes. Cool and measure absorbance at 490nm.
- HPLC Analysis (Preferred): Separate on C18 column with 10mM KH₂PO₄ buffer (pH 2.5) as mobile phase. Detect at 210nm.
- Bioavailability Assessment: Assess calcium bioavailability using in vitro digestion models coupled with Caco-2 cells, or measure urinary oxalate excretion in human trials to evaluate kidney stone risk [3] [58].
Validation: Spike recovery should be 85–115%. Limit of quantification typically 0.5–1.0 mg/100g.
Experimental Workflow for Anti-Nutrient Research
Diagram 1: Comprehensive workflow for anti-nutrient research integrating identification, bioavailability assessment, and mitigation strategies.
Mitigation Strategies and Bioavailability Enhancement
Processing Techniques for Anti-Nutrient Reduction
Table 3: Optimization Parameters for Anti-Nutrient Reduction Methods
| Processing Method | Key Anti-Nutrients Affected | Optimal Conditions | Mechanism of Action | Impact on Nutrient Bioavailability |
|---|---|---|---|---|
| Thermal Processing | Lectins, trypsin inhibitors, goitrogens [55] [54] | Boiling (>95°C, >10 min), autoclaving (121°C, 15-20 psi) [55] | Protein denaturation, structural degradation [55] | Increases protein digestibility and mineral bioavailability [54] |
| Soaking & Germination | Phytates, tannins, oxalates [54] [57] | Soaking (12-18h, 25-40°C), germination (24-72h) [54] | Leaching, enzymatic activation (phytase) [54] | Increases mineral bioavailability (Fe, Zn, Ca) [54] [57] |
| Fermentation | Phytates, tannins, lectins [55] [54] | Natural (24-72h) or starter culture fermentation [55] | Microbial enzymatic degradation [55] [54] | Enhances mineral absorption and protein digestibility [54] |
| Extrusion Cooking | Lectins, trypsin inhibitors, phytates [57] | High temperature, pressure, and shear force [57] | Thermal degradation and structural disruption [57] | Improves starch and protein digestibility [57] |
Strategic Food Combining for Bioavailability Enhancement
Research demonstrates that the overall meal composition significantly influences the net bioavailability of nutrients from anti-nutrient containing foods [3] [4]. Strategic food combining can mitigate negative effects:
- Vitamin C with Plant Iron: Ascorbic acid reduces ferric iron (Fe³⁺) to the more absorbable ferrous form (Fe²⁺) and can form a chelate with iron that remains soluble in the intestinal lumen, counteracting the inhibitory effects of phytates and tannins [3].
- Calcium with Oxalate: Consuming calcium-rich foods with high-oxalate foods allows binding to occur in the gut, forming insoluble calcium oxalate that is excreted in feces rather than being absorbed and potentially forming kidney stones [58].
- Food Matrix Considerations: The dairy matrix enhances calcium bioavailability through components like casein phosphopeptides, lactose, and vitamin D that facilitate both passive and active absorption mechanisms [4].
Research Reagent Solutions for Bioavailability Studies
Table 4: Essential Research Reagents for Anti-Nutrient and Bioavailability Studies
| Reagent/Chemical | Application in ANF Research | Specific Function | Research Considerations |
|---|---|---|---|
| Phytase Enzymes | Phytate degradation studies | Hydrolyzes phytic acid to lower inositol phosphates | Varying pH and temperature optima; microbial vs. plant sources [54] |
| Stable Isotopes (⁵⁷Fe, ⁶⁷Zn, ⁴⁴Ca) | Mineral absorption studies | Tracers for quantifying mineral bioavailability | Requires ICP-MS detection; enables extrinsic tagging method validation [3] [4] |
| Anion Exchange Resins (AG 1-X4) | Phytate purification | Selective binding of inositol phosphates | Capacity varies with cross-linkage; requires pH optimization [54] |
| Caco-2 Cell Line | Intestinal absorption models | Human intestinal epithelium model for nutrient transport | Requires 21-day differentiation; validated for iron and zinc uptake studies [3] |
| Wade Reagent (FeCl₃ + sulfosalicylic acid) | Phytate quantification | Forms colored complex with phytate for spectrophotometric detection | Interference from other phosphates; specific for phytate [54] |
| Simulated Gastrointestinal Fluids | In vitro digestion models | Mimics gastric and intestinal phases of digestion | Standardized protocols (INFOGEST) improve inter-lab comparability [3] |
Advanced Research Applications and Future Directions
Biomarker Development for Bioavailability Assessment
The development of nutritional biomarkers represents a cutting-edge approach to objectively assess nutrient bioavailability and status, overcoming limitations of traditional dietary assessment methods [59]. Promising biomarkers relevant to anti-nutrient research include:
- Alkylresorcinols: As biomarkers of whole-grain intake, these can help correlate phytate exposure with mineral status [59].
- Homocysteine: Functional biomarker of folate status, potentially affected by dietary tannins that may impact folate bioavailability [59].
- Nitrogen in 24h urine: Validated biomarker of protein intake, useful for assessing impact of protease inhibitors on protein utilization [59].
Genetic and Biotechnological Approaches
Emerging genetic technologies offer promising approaches to reduce anti-nutrients at the source:
- RNA interference (RNAi) and CRISPR-Cas9 gene editing technologies are being explored to develop crop varieties with reduced anti-nutrient content [57].
- Multi-omics approaches (genomics, transcriptomics, proteomics, metabolomics) help understand anti-nutrient biosynthesis and accumulation patterns in crops [57] [56].
- Molecular breeding strategies aim to develop low-phytate, low-oxalate, and low-lectin varieties while maintaining agronomic performance and stress resistance [57].
These approaches must balance anti-nutrient reduction with preservation of beneficial compounds and plant defense mechanisms, requiring comprehensive metabolic profiling.
The systematic investigation of anti-nutrients is fundamental to advancing our understanding of nutrient bioavailability. This application note provides researchers with standardized protocols for quantifying phytates, oxalates, tannins, and lectins, while offering evidence-based mitigation strategies to enhance the nutritional quality of plant foods. The integrated approach—combining traditional processing methods with modern analytical techniques and emerging biotechnologies—represents the future of anti-nutrient research. As the field progresses, the development of robust biomarkers and predictive models will further enhance our ability to optimize nutrient bioavailability from complex foods, contributing to the development of nutrition-sensitive agricultural practices and dietary recommendations that maximize health benefits while minimizing potential adverse effects of anti-nutrients.
The bioavailability of essential nutrients in food is profoundly influenced by the processing and preparation methods applied before consumption. These techniques directly impact the release of macronutrients and micronutrients from the food matrix, a critical consideration for research aimed at combating global malnutrition and optimizing dietary formulations [60]. This document provides detailed application notes and experimental protocols for assessing how cooking, fermentation, and sprouting modulate nutrient bioavailability, with a specific focus on overcoming antinutritional factors (ANFs) inherent in plant-based foods [61] [60]. The framework supports research on developing sustainable, nutritionally complete food products by leveraging traditional and modern food processing technologies.
Application Notes: Mechanisms of Nutrient Enhancement
Key Processes and Their Impact on Nutrient Bioavailability
Table 1: Impact of Processing Methods on Nutrient Bioavailability and Antinutritional Factors
| Processing Method | Key Nutritional Enhancements | Reduction in Antinutritional Factors | Underlying Mechanisms |
|---|---|---|---|
| Thermal Processing (Cooking) | Increased protein digestibility; Gelatinization of starch [60]. | Reduction of protease inhibitors (e.g., trypsin), lectins, and some phytates [61]. | Denaturation of protein complexes; Thermal degradation of heat-labile ANFs; Disruption of cell wall structures. |
| Fermentation (Microbial) | Increased free amino acids and bioactive peptides; Synthesis of B vitamins (riboflavin, niacin, B12); Improved mineral bioavailability [60]. | Significant reduction of phytates, tannins, and oxalates [60]. | Microbial enzyme activity (e.g., phytases, proteases); Production of organic acids that solubilize minerals; Pre-digestion of macronutrients. |
| Sprouting (Germination) | Increased essential amino acids (e.g., lysine); Elevated levels of total phenols and dietary fiber; Enhanced antioxidant capacity [62] [63]. | Reduction of phytates and enzyme inhibitors [61]. | Activation of endogenous enzymes (e.g., phytase, α-amylase); Metabolic conversion of stored nutrients into more bioavailable forms. |
Targeted Nutrient Enhancement Protocols
Different processing methods can be tailored to enhance the bioavailability of specific nutrients, which is crucial for addressing particular deficiency states.
Table 2: Targeting Specific Nutrient Enhancements Through Processing
| Target Nutrient | Recommended Processing Method | Research Evidence & Protocol Focus |
|---|---|---|
| Iron (Non-Heme) | Fermentation; Sprouting; Use of acidulants (e.g., amchur, lime) [64]. | Focus: Assess reduction of phytate and tannin content. Evidence: Germinating and de-hulling legumes significantly increased iron bioavailability in vitro [61]. |
| Zinc | Fermentation; Sprouting [64]. | Focus: Measure phytate degradation and zinc solubility. Evidence: Fermentation with lactic acid bacteria (LAB) reduces phytate-zinc complexes, improving bioaccessibility [60]. |
| Calcium | Thermal Processing; Sprouting; De-hulling [61]. | Focus: Evaluate reduction of oxalates and phytates. Evidence: Germinating and de-hulling cowpeas, lentils, or chickpeas significantly increased calcium bioavailability in vitro [61]. |
| Plant-Based Proteins | Fermentation; Thermal Processing [60]. | Focus: Monitor protein digestibility and essential amino acid profile. Evidence: Fermentation with specific LAB strains increases protein digestibility and free amino acid content in various matrices [60]. |
| β-Carotene (Provitamin A) | Thermal Processing; Use of enhancers (e.g., oils, Allium spices) [64]. | Focus: Assess isomerization and release from the food matrix. Evidence: Food acidulants and β-carotene-rich vegetables can enhance the bioavailability of β-carotene from combined foods [64]. |
Experimental Protocols for Assessing Bioavailability
The following protocols provide standardized methodologies for evaluating the efficacy of processing techniques in a research setting.
Protocol: In Vitro Protein Digestibility Assay
1.0 Objective: To determine the impact of processing (e.g., fermentation, cooking) on the digestibility of protein in plant-based matrices.
2.0 Principle: This simulated gastrointestinal digestion protocol measures the degree of protein hydrolysis by proteolytic enzymes under controlled conditions, predicting in vivo protein digestibility [60].
3.0 Materials and Reagents:
- Test Sample: Processed (fermented/cooked) and unprocessed (control) plant flour.
- Enzymes: Pepsin (from porcine gastric mucosa, ≥250 U/mg), Pancreatin (from porcine pancreas).
- Buffers: Simulated Gastric Fluid (SGF, 0.1 M HCl, pH 2.0), Simulated Intestinal Fluid (SIF, 0.1 M KH₂PO₄, pH 7.0).
- Equipment: Water bath/shaker, pH meter, centrifuge, spectrophotometer, and glassware.
4.0 Procedure:
- Sample Preparation: Mill samples to a uniform particle size. Precisely weigh 1.0 g of sample into a digestion vessel.
- Gastric Phase: Add 15 mL of SGF and 1.0 mL of pepsin solution (10 mg/mL in SGF). Incubate at 37°C for 2 hours with constant agitation.
- Intestinal Phase: Adjust pH to 7.0 using 0.5 M NaOH. Add 10 mL of SIF and 2.5 mL of pancreatin solution (10 mg/mL in SIF). Incubate at 37°C for a further 4 hours with constant agitation.
- Reaction Termination: Place vessels in a boiling water bath for 10 minutes to denature enzymes.
- Centrifugation: Centrifuge the digestate at 10,000 × g for 15 minutes.
- Analysis: Analyze the supernatant for:
- NH₂-Termini: Using the O-phthaldialdehyde (OPA) method.
- Total Nitrogen: Using the Kjeldahl or Dumas method.
5.0 Data Analysis:
Calculate In Vitro Protein Digestibility (IVPD) using the formula:
IVPD (%) = (Soluble Protein in Digestate / Total Protein in Sample) × 100
Compare IVPD values between processed and unprocessed controls. Statistical analysis (e.g., t-test, ANOVA) should be performed to confirm significance.
Protocol: Phytate Reduction via Fermentation
1.0 Objective: To quantify the reduction of phytic acid in cereal or legume substrates through controlled lactic acid bacteria (LAB) fermentation.
2.0 Principle: Selected LAB strains with intrinsic phytase activity hydrolyze phytic acid (myo-inositol hexakisphosphate) into lower inositol phosphates, thereby chelating fewer minerals and improving their bioavailability [60].
3.0 Materials and Reagents:
- Microbial Strains: Lactobacillus plantarum, Lactobacillus rossiae, or other phytase-producing LAB.
- Growth Media: de Man, Rogosa and Sharpe (MRS) broth and agar.
- Substrate: Whole grain or legume flour slurry (10-20% w/v in water).
- Analytical: Phytic Acid (IP6) Assay Kit (e.g., Megazyme), or reagents for colorimetric Wade reagent method.
4.0 Procedure:
- Starter Culture Preparation: Inoculate LAB strain into MRS broth and incubate at 37°C for 18-24 hours to achieve late log phase (≈10⁹ CFU/mL).
- Fermentation Setup: Inoculate the sterile substrate slurry with the starter culture at 2% (v/v). Maintain under anaerobic conditions at 37°C for 24-72 hours. Include an uninoculated control.
- Sampling: Aseptically withdraw samples at 0, 24, 48, and 72 hours.
- Phytate Extraction: Homogenize samples, centrifuge, and use the supernatant for phytate analysis as per the selected assay kit's protocol.
- Quantification: Measure phytate content spectrophotometrically and calculate concentration against a standard curve.
5.0 Data Analysis:
Calculate the percentage reduction of phytic acid:
Reduction (%) = [(Phytate_initial - Phytate_final) / Phytate_initial] × 100
Correlate phytate reduction with increases in soluble minerals (e.g., iron, zinc) measured via ICP-MS.
Protocol: Mineral Bioaccessibility Assessment
1.0 Objective: To evaluate the bioaccessibility of iron, zinc, and calcium from processed food samples using a simulated gastrointestinal digestion model.
2.0 Principle: This protocol simulates human digestion to release minerals from the food matrix into a soluble form, which represents the fraction available for intestinal absorption (i.e., the bioaccessible fraction) [61] [64].
3.0 Materials and Reagents:
- Enzymes: Pepsin, Pancreatin, Bile salts (e.g., porcine bile extract).
- Buffers: SGF (pH 2.0), SIF (pH 7.0).
- Equipment: Metabolic shaker, pH meter, centrifuge with ultracentrifuge capability (e.g., 100,000 × g), Inductively Coupled Plasma Mass Spectrometry (ICP-MS) or Atomic Absorption Spectrometer (AAS).
4.0 Procedure:
- Gastric Digestion: Subject 2 g of sample to gastric digestion as described in Protocol 3.1.
- Intestinal Digestion: Adjust pH to 7.0, add pancreatin and bile salts (final conc. 2-4 mg/mL), and incubate for 2 hours at 37°C.
- Collection of Bioaccessible Fraction: Centrifuge the final digestate at 10,000 × g for 1 hour at 4°C. For a more refined estimate of the absorbable fraction, ultracentrifuge the supernatant at 100,000 × g for 1 hour.
- Mineral Analysis: Digest the soluble (bioaccessible) fraction with concentrated nitric acid and analyze for target mineral concentrations using ICP-MS or AAS. Analyze the original food sample for total mineral content.
5.0 Data Analysis:
Calculate the Bioaccessible Fraction:
Bioaccessibility (%) = (Mineral Content in Soluble Fraction / Total Mineral Content in Sample) × 100
Figure 1: Experimental workflow for assessing mineral bioaccessibility using a simulated gastrointestinal model.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Bioavailability Research
| Item | Function/Application | Research Context |
|---|---|---|
| Pepsin (from porcine gastric mucosa) | Proteolytic enzyme for simulated gastric digestion phase. | Critical for IVPD assays and mineral bioaccessibility studies to mimic stomach proteolysis [60]. |
| Pancreatin (from porcine pancreas) | Mixture of digestive enzymes (amylase, protease, lipase) for simulated intestinal digestion. | Used in the intestinal phase of in vitro digestion models to simulate pancreatic activity [60]. |
| Phytic Acid (Sodium Salt) & Assay Kits | Standard for quantification and calibration; kits for high-throughput analysis of phytate. | Essential for monitoring the reduction of this potent antinutrient during fermentation and sprouting studies [60]. |
| Lactic Acid Bacteria (LAB) Starters | Defined microbial cultures (e.g., Lactobacillus spp., Lactococcus spp.) for controlled fermentation. | Used to inoculate substrates, ensuring reproducible fermentation and specific metabolic outcomes (e.g., phytate degradation) [65] [60]. |
| Bile Salts (Porcine) | Emulsifying agents for lipid digestion and micelle formation in the small intestine. | Added during the intestinal phase to simulate the role of bile in solubilizing lipophilic compounds and minerals [61]. |
| ICP-MS Standard Solutions | Calibration standards for precise and accurate quantification of mineral elements. | Required for the analysis of total and bioaccessible mineral content (Fe, Zn, Ca) in digestate fractions [61]. |
The strategic application of cooking, fermentation, and sprouting presents a powerful, natural approach to enhancing the nutritional quality of plant-based foods. The protocols outlined herein provide a standardized framework for researchers to quantitatively assess the impact of these processing methods on critical parameters such as protein digestibility, phytate content, and mineral bioaccessibility. By leveraging these methodologies, the scientific community can generate robust data to develop optimized, nutrient-dense food products, contributing to improved public health and sustainable food systems. Future research should focus on integrating multi-omics approaches to fully elucidate the molecular mechanisms behind these enhancements and optimize processing conditions for specific food matrices.
The concept of nutrient bioavailability, defined as the fraction of an ingested nutrient that is absorbed and utilized in the body, is fundamental to nutritional science and the development of effective food-based interventions [3]. Beyond merely quantifying the amount of a nutrient in a food matrix, understanding bioavailability is crucial for linking dietary intake to physiological outcomes and health benefits [22]. The absorption and utilization of micronutrients can be significantly influenced by interactions with other food components within a meal, leading to either synergistic or antagonistic effects [4]. This application note focuses on the well-established synergy between vitamin C and non-heme iron, providing researchers with detailed protocols to assess this interaction within a broader framework of bioavailability research.
Theoretical Framework: The Vitamin C and Iron Synergy
Mechanism of Action
The enhancing effect of vitamin C (ascorbic acid) on iron bioavailability is primarily targeted at non-heme iron, the inorganic form found in plant-based foods. The mechanism is twofold [66]:
- Reduction and Chelation: Vitamin C creates an acidic environment in the stomach, facilitating the reduction of ferric iron (Fe³⁺) to the more soluble ferrous (Fe²⁺) form. It subsequently binds to the iron, forming a soluble iron-ascorbate chelate. This complex remains stable in the alkaline environment of the duodenum, preventing precipitation and making the iron more readily available for absorption by the intestinal enterocytes [66].
- Overcoming Dietary Inhibitors: This synergistic action is particularly beneficial in plant-based diets where non-heme iron predominates and its absorption can be inhibited by dietary compounds such as phytates (found in grains and legumes) and polyphenols (found in tea and coffee) [66] [67].
Experimental Evidence and Health Implications
Clinical studies substantiate that the co-administration of vitamin C with iron supplements substantially improves treatment outcomes for individuals with iron deficiency anemia [66]. This increased absorption efficiency means that lower doses of supplemental iron may be used to achieve the desired therapeutic effect, potentially reducing the adverse gastrointestinal side effects often associated with high-dose iron intake [66]. The resulting improvement in iron status supports critical bodily functions, including efficient oxygen transport for reduced fatigue and the proliferation of immune cells for a stronger immune response [66].
Quantitative Data on Bioavailability Synergies
Table 1: Documented Synergistic Effects on Micronutrient Bioavailability
| Target Nutrient | Synergistic Compound/Food | Documented Effect | Proposed Mechanism |
|---|---|---|---|
| Iron (Non-Heme) | Vitamin C (Ascorbic Acid) | Significantly enhances absorption; improves anemia treatment outcomes [66] [67]. | Reduction of Fe³⁺ to Fe²⁺; formation of a soluble chelate to prevent precipitation [66]. |
| Vitamin A | Dietary Fat | Fat is found to be synergistic for vitamin A absorption [67]. | Solubilization and incorporation of the fat-soluble vitamin into mixed micelles for absorption. |
| Calcium | Vitamin D, Casein Phosphopeptides, Lactose | Enhances passive and active absorption; improves bone mineralization [4]. | Vitamin D regulates active transport; peptides prevent precipitation; lactose may act as a prebiotic [4]. |
| Zinc | Protein, Red Wine (explored) | Protein has been explored for enhancing zinc absorption [67]. | Amino acids (e.g., histidine) may chelate zinc, facilitating its absorption via separate pathways. |
Experimental Protocols for Assessing Bioavailability
A critical appraisal of bioavailability requires a clear differentiation of terms: bioaccessibility (the fraction released from the food matrix into the gut), absorption (the fraction that crosses the intestinal epithelium), and bioavailability (the fraction that is absorbed and utilized for physiological functions) [22]. The following protocols provide methodologies for key experiments in this field.
Protocol: In Vitro Assessment of Iron Bioaccessibility
This protocol simulates human gastrointestinal digestion to estimate the fraction of iron released from a food matrix (bioaccessibility), which is a prerequisite for absorption.
1. Research Reagent Solutions:
- Simulated Gastric Fluid (SGF): Prepare a solution containing pepsin in 0.1 M HCl, pH adjusted to 2.0.
- Simulated Intestinal Fluid (SIF): Prepare a solution containing pancreatin and bile salts in 0.1 M NaHCO₃, pH adjusted to 7.0.
- Standard Solutions: Prepare ferrous and ferric iron standards for calibration curves.
- Colorimetric Reagent: e.g., Ferrozine or Bathophenanthroline disulfonic acid for iron quantification.
2. Methodology:
- Step 1: Gastric Phase. Weigh a homogenized test food sample. Add SGF and incubate for 1-2 hours at 37°C under continuous agitation.
- Step 2: Intestinal Phase. Raise the pH to 7.0 using NaHCO₃, add SIF, and incubate for a further 2 hours at 37°C.
- Step 3: Digesta Collection. Centrifuge the final digestate to separate the soluble fraction (containing bioaccessible iron) from the solid residue.
- Step 4: Iron Quantification. Analyze the soluble fraction using a validated method such as Inductively Coupled Plasma Optical Emission Spectrometry (ICP-OES) or a colorimetric assay. Compare results from test samples (e.g., food alone) with samples containing the synergistic combination (e.g., food + vitamin C source).
Protocol: In Vivo Assessment Using an Extrinsic Tag Method
The extrinsic tag method is a validated in vivo technique for measuring the relative bioavailability of minerals, such as iron, from different food sources in human subjects [3].
1. Research Reagent Solutions:
- Stable Isotope Tracer: A solution of ⁵⁷Fe or ⁵⁸Fe (as ferrous sulfate or other soluble salt) of high isotopic purity.
- Reference Dose: A solution of a different iron isotope (e.g., ⁵⁴Fe) in a highly bioavailable form (e.g., ferrous ascorbate) for normalization.
2. Methodology:
- Step 1: Study Design. Obtain ethical approval and informed consent. A crossover design is often used where subjects serve as their own controls.
- Step 2: Dosing. The test meal (e.g., a plant-based meal high in non-heme iron) is extrinsically tagged by thoroughly mixing a known amount of the stable isotope tracer (⁵⁷Fe) into the meal immediately before consumption. On a separate occasion, a reference dose (⁵⁴Fe) is administered.
- Step 3: Sample Collection. Collect baseline blood samples. Subsequent blood samples are collected over 10-14 days post-administration.
- Step 4: Isotopic Analysis. Isolate iron from the blood samples and analyze the isotopic enrichment using Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
- Step 5: Calculation of Bioavailability. Calculate the fractional absorption of the extrinsic tag from the test meal and the reference dose. The relative bioavailability is expressed as the ratio of absorption from the test meal to absorption from the reference dose.
The Scientist's Toolkit: Reagents & Materials
Table 2: Essential Research Reagents for Bioavailability Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Stable Isotopes (e.g., ⁵⁷Fe, ⁵⁸Fe) | Safe, non-radioactive tracers for quantifying mineral absorption and kinetics in human studies [3]. | Extrinsic tag method for measuring iron bioavailability from a test meal. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that differentiates into enterocyte-like cells, used as an in vitro model of the intestinal epithelium. | Assessing iron uptake and transport in the presence/absence of vitamin C. |
| Pepsin & Pancreatin | Digestive enzymes used to simulate gastric and intestinal phases of digestion in in vitro models. | Preparing simulated gastrointestinal fluids for bioaccessibility studies. |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Highly sensitive analytical technique for elemental and isotopic analysis. | Quantifying isotopic enrichment in blood samples from stable isotope studies. |
| Colorimetric Assay Kits (e.g., for Iron) | Accessible method for quantifying specific nutrient concentrations in solutions. | Measuring iron concentration in the soluble fraction of in vitro digestas. |
Visualizing Experimental Workflows
Experimental Workflow for Bioavailability Research
Vitamin C and Iron Absorption Mechanism
The efficacy of nutraceuticals and bioactive compounds is fundamentally constrained by challenges such as poor solubility, chemical instability during digestion, and low bioavailability [68] [69]. Nanotechnology-based delivery systems present a transformative approach to overcoming these barriers. By engineering materials at the nanoscale (1-100 nm), these systems enhance the surface area-to-volume ratio, enabling improved encapsulation, protection, and targeted release of active compounds [68] [70]. This document provides detailed application notes and experimental protocols for formulating and evaluating nano-enabled delivery systems, designed for use within a broader research framework assessing nutrient bioavailability in foods.
Key Nanotechnology Delivery Systems: Properties and Applications
Nanocarriers are designed to address specific challenges associated with different bioactive compounds. The selection of an appropriate system depends on the physicochemical nature of the compound (e.g., hydrophilicity vs. lipophilicity) and the desired release profile [70] [69].
Table 1: Overview of Major Nanotechnology-Based Delivery Systems
| Delivery System | Key Components | Typical Size Range | Target Bioactives | Key Advantages |
|---|---|---|---|---|
| Nanoemulsions [68] | Oil, Water, Emulsifier (e.g., phospholipids, polysorbates) | 20-200 nm | Lipophilic compounds (e.g., vitamins A, D, E, carotenoids) [69] | Ease of fabrication, enhances solubility and stability of lipophilics [68] |
| Nanoliposomes [68] | Phospholipids (e.g., lecithin) | 50-100 nm | Both hydrophilic & lipophilic compounds | Biocompatible, ability to encapsulate a wide range of molecules [68] |
| Solid Lipid Nanoparticles (SLNs) [69] | Solid lipids (e.g., triglycerides, waxes), Surfactants | 50-300 nm | Lipophilic compounds, hydrophobic vitamins [69] | Improved stability over liposomes, controlled release [69] |
| Biopolymer Nanoparticles [68] | Proteins (e.g., zein, whey), Polysaccharides (e.g., chitosan, alginate) | 50-200 nm | Polyphenols, flavonoids, vitamins [68] [71] | Use of food-grade, biodegradable materials; tunable release [68] |
Experimental Protocols for Formulation and Assessment
Protocol: Fabrication of Oil-in-Water (O/W) Nanoemulsions for Lipophilic Bioactives
This protocol describes the preparation of a nanoemulsion for encapsulating a model lipophilic nutrient, Vitamin E (α-tocopherol), using high-pressure homogenization [68].
I. Research Reagent Solutions & Essential Materials
Table 2: Key Materials for Nanoemulsion Formulation
| Item | Function/Explanation |
|---|---|
| Medium-Chain Triglyceride (MCT) Oil | Lipid phase; serves as the solvent for the lipophilic bioactive. |
| Vitamin E (α-Tocopherol) | Model lipophilic bioactive compound. |
| Food-Grade Emulsifier (e.g., Tween 80, Lecithin) | Stabilizes oil droplets in water, prevents coalescence. |
| Deionized Water | Aqueous continuous phase. |
| High-Pressure Homogenizer | Equipment used to apply intense shear forces, reducing droplet size to nanoscale. |
II. Step-by-Step Methodology:
- Oil Phase Preparation: Dissolve 1.0 g of Vitamin E in 9.0 g of MCT oil. Add 2.0 g of Tween 80 to this mixture and stir gently until the emulsifier is fully dissolved.
- Aqueous Phase Preparation: In a separate beaker, measure 88.0 g of deionized water. Heat the water to 40°C to facilitate emulsification.
- Coarse Emulsion Formation: Slowly add the oil phase to the aqueous phase while using a high-shear mixer (e.g., Ultra-Turrax) at 10,000 rpm for 3 minutes. This creates a coarse macroemulsion.
- Nanoemulsion Formation: Pass the coarse emulsion through a high-pressure homogenizer for 5 cycles at a pressure of 100 MPa. Maintain the sample collection vessel in an ice bath to dissipate heat.
- Characterization: Analyze the resulting nanoemulsion for droplet size, polydispersity index (PDI), and zeta-potential using dynamic light scattering (DLS). Store the nanoemulsion at 4°C for further studies.
The following workflow outlines the fabrication and characterization process:
Protocol: In Vitro Bioavailability Assessment Using the Simulated Gastrointestinal Model
This protocol outlines a standardized in vitro method to simulate the digestion process and estimate the bioaccessibility of the nano-encapsulated bioactive, a key indicator of potential bioavailability [4].
I. Research Reagent Solutions & Essential Materials
Table 3: Key Materials for In Vitro Digestion Assay
| Item | Function/Explanation |
|---|---|
| Simulated Gastric Fluid (SGF) | Contains pepsin, NaCl, HCl; mimics stomach conditions. |
| Simulated Intestinal Fluid (SIF) | Contains pancreatin, bile salts, NaHCO₃; mimics small intestine. |
| Pepsin (from porcine gastric mucosa) | Proteolytic enzyme for gastric digestion. |
| Pancreatin (from porcine pancreas) | Enzyme mixture (amylase, protease, lipase) for intestinal digestion. |
| Bile Salts (e.g., sodium taurocholate) | Emulsifies fats, facilitating lipolysis. |
| pH Meter & Controller | Critical for maintaining correct pH in each digestion phase. |
II. Step-by-Step Methodology:
- Oral Phase (Optional): Mix 5 mL of nanoemulsion with 5 mL of simulated salivary fluid (pH 6.8) and incubate at 37°C for 2 minutes with constant agitation.
- Gastric Phase: Adjust the pH of the mixture from step 1 to 2.5 using 1M HCl. Add pepsin to a final concentration of 2000 U/mL. Incubate at 37°C for 60 minutes in a shaking water bath.
- Intestinal Phase: Raise the pH of the gastric chyme to 6.5-7.0 using 1M NaHCO₃. Add pancreatin (final concentration 100 U/mL of trypsin activity) and bile salts (final concentration 10 mM). Incubate at 37°C for 120 minutes with constant agitation.
- Bioaccessibility Determination: After intestinal digestion, centrifuge the final digest (e.g., 10,000 x g, 30 minutes) to separate the aqueous phase (micellar fraction). The bioactive compound contained in this micellar fraction is considered bioaccessible. Quantify the amount of bioactive in this fraction using HPLC-UV and calculate the bioaccessibility percentage using the formula:
- % Bioaccessibility = (Amount in micellar fraction / Total amount in initial sample) × 100
The sequential stages of the in vitro digestion model are summarized below:
The Scientist's Toolkit: Essential Research Reagents
A curated list of critical materials required for R&D in nanotechnology-based nutrient delivery is provided below.
Table 4: Essential Research Reagent Solutions for Nano-Delivery Systems
| Category / Item | Specific Examples | Function in Formulation & Assessment |
|---|---|---|
| Lipid Materials | Medium/Long-chain triglycerides (MCT, LCT), Glyceryl monostearate, Phospholipids (Lecithin) | Form the core matrix of lipid NPs and emulsions; solubilize lipophilic bioactives [68] [69]. |
| Biopolymer Materials | Proteins: Zein, Whey, Casein; Polysaccharides: Chitosan, Alginate, Pectin | Form biodegradable polymer NPs for encapsulation; stabilize emulsions; enable controlled release [68] [71]. |
| Surfactants / Emulsifiers | Polysorbates (Tween), Sorbitan esters (Span), Sodium dodecyl sulfate (SDS) | Stabilize interfaces in emulsions and NPs; reduce surface tension to achieve nanoscale droplets [68]. |
| Digestion Enzymes & Salts | Pepsin, Pancreatin, Pancreatic lipase, Bile salts (e.g., sodium glycodeoxycholate) | Critical components of simulated gastrointestinal fluids for in vitro bioavailability assays [4]. |
| Characterization Instruments | Dynamic Light Scatterer (DLS), HPLC-UV/FLD, Transmission Electron Microscope (TEM) | Measure particle size/zeta-potential (DLS), quantify bioactive content (HPLC), visualize morphology (TEM) [70]. |
Validating Methods and Comparing Bioavailability Across Nutrients and Foods
Within the critical field of nutrient bioavailability research, accurate predictive equations are indispensable for translating scientific knowledge into practical dietary recommendations and public health policy. The adequacy of nutrient intake depends not only on the total amount consumed but also on the fraction absorbed and utilized by the body [46]. Current nutrient intake recommendations, nutritional assessments, and food labeling predominantly rely on estimated total nutrient content in foods and dietary supplements, creating a significant gap between reported consumption and actual physiological utilization [46] [72]. This document establishes comprehensive application notes and experimental protocols for developing, validating, and translating predictive algorithms that estimate nutrient absorption and bioavailability, providing researchers with a standardized framework to enhance the accuracy and applicability of their predictive models.
Foundational Framework for Equation Development
The development of robust predictive equations requires a structured, multi-stage approach that systematically addresses the complex factors influencing nutrient absorption. The following four-step framework provides a methodological foundation for researchers developing predictive algorithms for nutrient bioavailability.
Four-Step Development Framework
Step 1: Identify Key Influencing Factors - Comprehensively identify and document the biological, food matrix, compositional, and host-specific factors that influence the bioavailability of the target nutrient or bioactive compound. This includes factors such as dietary inhibitors and enhancers, food processing methods, nutrient chemical form, and individual physiological variations [46] [72].
Step 2: Conduct Comprehensive Literature Review - Perform a systematic review of high-quality human studies to gather empirical data on the identified factors. This review should prioritize human intervention studies that provide quantitative measures of absorption and utilization, forming the essential database for equation construction [46].
Step 3: Construct Predictive Equations - Develop mathematical equations based on the insights gained from the literature review. This typically involves statistical modeling techniques such as regression analysis (linear, logistic, or multivariate) to establish relationships between predictor variables (influencing factors) and outcome variables (bioavailability measures) [46] [73].
Step 4: Validate and Translate - Rigorously validate the predictive equations using independent datasets not used in model development. This critical step assesses real-world performance and ensures the model's reliability before translation into practical applications such as dietary guidelines or clinical recommendations [46].
The workflow for this framework can be visualized as follows:
Performance Metrics and Validation Protocols
Quantitative Validation Metrics
Validating predictive equations requires multiple performance metrics to assess different aspects of model accuracy. The table below summarizes the key metrics used in evaluating predictive model performance, drawing from established validation methodologies in physiological and nutritional research [74] [73].
Table 1: Key Performance Metrics for Validating Predictive Equations
| Metric | Calculation | Interpretation | Application in Bioavailability |
|---|---|---|---|
| Root Mean Square Error (RMSE) | $\sqrt{\frac{\sum{i=1}^{n}(yi - \hat{y}_i)^2}{n}}$ | Measures average magnitude of prediction error; lower values indicate better accuracy | Quantifies average error in predicting absorption percentages [74] |
| R-squared (R²) | $1 - \frac{\sum{i=1}^{n}(yi - \hat{y}i)^2}{\sum{i=1}^{n}(y_i - \bar{y})^2}$ | Proportion of variance in dependent variable explained by model; higher values (closer to 1) indicate better fit | Assesses how well influencing factors explain variability in bioavailability [73] |
| Mean Absolute Error (MAE) | $\frac{\sum{i=1}^{n}|yi - \hat{y}_i|}{n}$ | Average absolute difference between predicted and observed values; less sensitive to outliers than RMSE | Useful when extreme prediction errors are not disproportionately penalized |
| Concordance Correlation Coefficient | $\frac{2\rho\sigmay\sigma{\hat{y}}}{\sigmay^2 + \sigma{\hat{y}}^2 + (\muy - \mu{\hat{y}})^2}$ | Measures agreement between predicted and measured values, accounting for systematic differences | Assesses both precision and accuracy in predicting bioavailability measures |
Experimental Validation Protocol
The following protocol provides a detailed methodology for validating predictive equations for nutrient bioavailability, adapted from established research practices [74] [46].
Protocol 1: External Validation of Bioavailability Prediction Equations
Objective: To independently validate the performance of a predictive equation for nutrient bioavailability using data not used in model development.
Materials:
- Independent validation dataset (n ≥ 50 recommended)
- Statistical software (R, Python, MATLAB, or equivalent)
- Laboratory equipment for bioavailability assessment (as required by specific nutrient)
Procedure:
- Dataset Preparation: Compile an independent validation dataset comprising:
- Measured bioavailability values from controlled human studies
- Corresponding values for all predictor variables included in the equation
- Ensure dataset represents the target population and conditions
Prediction Generation: Apply the predictive equation to generate estimated bioavailability values for all observations in the validation dataset.
Performance Calculation: Calculate validation metrics including:
- Root Mean Square Error (RMSE)
- R-squared (R²)
- Mean Absolute Error (MAE)
- Concordance Correlation Coefficient
Calibration Assessment: Generate a calibration plot of predicted versus measured values and evaluate:
- Linearity of relationship (slope and intercept)
- Presence of systematic bias
- Homogeneity of variance
Clinical Significance Evaluation: Determine whether prediction errors are clinically/nutritionally significant in magnitude.
Acceptance Criteria: For satisfactory validation, models should demonstrate:
- RMSE < 15% of the range of observed values
- R² > 0.60 in external validation
- No systematic bias in calibration plot
- Prediction errors below thresholds for clinical significance
Recalibration Methods and Procedures
Even well-developed predictive equations often require recalibration when applied to new populations or conditions. Recalibration involves adjusting the model's intercept or coefficients to improve alignment with new data while preserving the underlying relationships identified in the original model [74].
Recalibration Protocol
Protocol 2: Equation Recalibration for New Populations
Objective: To recalibrate an existing predictive equation to improve its accuracy for a specific population or set of conditions.
Materials:
- Target population dataset (n ≥ 100 recommended)
- Original predictive equation
- Statistical software with regression capabilities
Procedure:
- Data Collection: Assemble a dataset from the target population including:
- Measured bioavailability values
- Values for all predictor variables in the original equation
Performance Assessment: Apply the original equation and calculate baseline performance metrics (as in Protocol 1).
Recalibration Approach Selection:
- Intercept-Only Adjustment: Regress measured values against the original predicted values with no intercept to estimate a new intercept term
- Slope and Intercept Adjustment: Regress measured values against original predicted values to estimate new slope and intercept parameters
- Full Coefficient Re-estimation: Re-estimate all equation coefficients using the new dataset while retaining the original variable structure
Model Refitting: Implement the selected recalibration approach to generate revised regression coefficients.
Validation: Assess performance of the recalibrated equation using cross-validation or an independent holdout dataset.
Interpretation: The recalibration process typically significantly reduces RMSE values. For example, in validation of VO₂max prediction equations, recalibration decreased RMSE values from a range of 4.2-20.4 mL·kg⁻¹·min⁻¹ to 3.9-4.2 mL·kg⁻¹·min⁻¹ [74].
The relationship between original and recalibrated models can be visualized as follows:
Translation to Clinical and Regulatory Applications
Assessing Predictive Utility for Health Outcomes
The ultimate validation of any predictive equation lies in its ability to forecast clinically relevant endpoints. This assessment involves evaluating whether predicted values maintain the same relationship with health outcomes as directly measured values [74].
Table 2: Translation Assessment Framework for Bioavailability Equations
| Assessment Level | Methodology | Interpretation | Regulatory Significance |
|---|---|---|---|
| Association with Health Outcomes | Cox proportional hazards models or logistic regression assessing relationship between predicted values and clinical endpoints | Determines if predictive values show similar hazard ratios/odds ratios as measured values | Evidence for use in public health recommendations and dietary guidelines |
| Robustness to Covariate Adjustment | Multivariable models adjusting for demographic and clinical characteristics | Assesses whether predictive values maintain independent association with outcomes after adjustment | Indicates whether equation captures unique biological information beyond basic demographics |
| Classification Accuracy | Analysis of sensitivity, specificity, and correct classification rates for identifying deficient/sufficient status | Evaluates clinical utility for identifying individuals or populations at risk | Supports use in screening and targeted intervention programs |
Implementation Protocol
Protocol 3: Translation to Clinical and Public Health Practice
Objective: To assess the suitability of a validated predictive equation for implementation in clinical or public health settings.
Materials:
- Dataset with health outcome measures
- Measured and predicted bioavailability values
- Statistical software for survival analysis and risk prediction
Procedure:
- Outcome Association Analysis:
- Fit Cox proportional hazards models with measured bioavailability values as predictor
- Fit identical models with predicted bioavailability values as predictor
- Compare hazard ratios and confidence intervals between models
Covariate Adjustment Assessment:
- Adjust models for relevant demographic and clinical covariates
- Determine whether predicted values maintain statistical significance after adjustment
- Assess magnitude of attenuation in effect size
Risk Stratification Accuracy:
- Establish clinical cutpoints for deficiency/insufficiency based on measured values
- Calculate sensitivity, specificity, and area under ROC curve for predicted values
- Determine positive and negative predictive values in target population
Interpretation: Successful translation is demonstrated when predicted values show similar associations with health outcomes as measured values, though some attenuation is expected. For example, in cardiorespiratory fitness research, predicted VO₂max values yielded similar mortality hazard estimates as measured values in unadjusted models, though they were less robust to covariate adjustment [74].
The Scientist's Toolkit: Research Reagent Solutions
The experimental validation of nutrient bioavailability prediction equations requires specific methodological approaches and analytical tools. The following table details key "research reagents" – methodological components and their functions – in this field.
Table 3: Essential Methodological Components for Bioavailability Research
| Methodological Component | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Stable Isotope Tracers | Allow precise tracking of nutrient absorption, distribution, and utilization without radioactivity | Iron, zinc, vitamin A bioavailability studies | Requires mass spectrometry detection; provides highly accurate absorption measures [46] |
| Caco-2 Cell Models | In vitro system simulating human intestinal absorption for preliminary screening | Bioavailability of minerals, carotenoids, and other micronutrients | Correlates with human data for some nutrients but not all; useful for mechanistic studies |
| High-Performance Liquid Chromatography (HPLC) | Separation and quantification of specific nutrient forms and metabolites | Measurement of vitamin isomers, carotenoid profiles, folate forms | Enables specific chemical form analysis critical for bioavailability assessment |
| Regression Modeling | Statistical technique for developing mathematical relationships between predictors and outcomes | Constructing prediction equations based on dietary and host factors | Multiple approaches (linear, logistic, multivariate) depending on outcome variable type [73] |
| Cross-Validation | Resampling procedure for assessing how model results will generalize to independent data | Preventing overfitting during equation development | Particularly important with limited datasets; provides robust performance estimates |
The validation of predictive equations for nutrient bioavailability represents a critical bridge between nutritional science and its practical application in public health and clinical medicine. By implementing the structured frameworks, detailed protocols, and rigorous validation methodologies outlined in these application notes, researchers can develop more accurate, reliable, and translatable predictive models. This systematic approach to equation development, validation, and implementation will ultimately enhance the evidence base for dietary recommendations, food labeling policies, and clinical nutritional practice, ensuring that predictions of nutrient bioavailability reflect physiological reality and contribute meaningfully to improving human health through optimal nutrition.
Iron bioavailability, representing the fraction of ingested iron absorbed and utilized for physiological functions, varies significantly between its two dietary forms: heme and non-heme iron. This disparity is a critical consideration in nutritional science, public health, and food technology research. Heme iron, derived from hemoglobin and myoglobin in animal tissues, demonstrates high and relatively consistent absorption rates between 15-35% [75] [76]. In contrast, non-heme iron from plant sources exhibits more variable absorption (1-10%) that is strongly influenced by dietary composition and gastrointestinal conditions [75] [77]. Understanding these differences and the methodologies to quantify them is essential for developing effective strategies to combat iron deficiency anemia, which remains the most widespread nutritional deficiency globally [78].
This case study examines the fundamental distinctions in absorption mechanisms, key influencing factors, and specialized protocols for assessing iron bioavailability from diverse food sources, providing a framework for researchers investigating nutrient bioavailability.
Biochemical Fundamentals of Iron Absorption
Chemical Forms and Absorption Pathways
The divergent absorption pathways for heme and non-heme iron stem from their distinct chemical properties. Heme iron (Fe²⁺ within a protoporphyrin ring) is absorbed as an intact metalloporphyrin complex via specific heme carrier proteins on duodenal enterocytes, protected from dietary inhibitors [75] [78]. Non-heme iron (primarily Fe³⁺) must undergo solubilization and reduction before transport, making it vulnerable to chemical interactions within the gastrointestinal lumen [75].
The absorption of non-heme iron is particularly dependent on luminal conditions. Gastric acid solubility of ferric iron (Fe³⁺) is crucial, with the brush border membrane enzyme duodenal cytochrome B (Dcytb) reducing it to the more soluble ferrous form (Fe²⁺) for transport via divalent metal transporter 1 (DMT1) [75]. This process is highly sensitive to dietary factors and gastrointestinal pH, explaining why proton pump inhibitor use can significantly impair non-heme iron absorption [75].
Intracellular Iron Handling and Systemic Regulation
Following absorption, both iron pools merge into a common intracellular pathway. Iron can be stored as ferritin within the enterocyte or exported into circulation via ferroportin [75] [78]. The basolateral export requires oxidation back to Fe³⁺ by hephaestin for binding to transferrin, the primary plasma transport protein [75].
Systemic iron homeostasis is regulated principally by hepcidin, a hepatic hormone that controls ferroportin internalization and degradation. Recent research indicates that habitual dietary patterns influence this regulatory axis; vegans demonstrated significantly lower hepcidin levels correlated with enhanced non-heme iron absorption in a 2025 controlled trial [79] [80]. This adaptation suggests physiological compensation for lower non-heme iron bioavailability in plant-based diets.
Quantitative Comparison of Heme vs. Non-Heme Iron
Table 1: Characteristics of Heme and Non-Heme Iron
| Parameter | Heme Iron | Non-Heme Iron |
|---|---|---|
| Chemical Form | Iron incorporated into protoporphyrin IX ring (Fe²⁺) | Ionic iron (primarily Fe³⁺) |
| Dietary Sources | Animal flesh: meat, poultry, seafood, organ meats | Plant foods: grains, legumes, nuts, leafy greens; also in animal flesh and fortified foods |
| Absorption Mechanism | Endocytosis via heme carrier protein (HCP1) | Reduction by Dcytb followed by DMT1 transport |
| Typical Absorption Rate | 15-35% [75] | 1-10% (highly variable) [77] |
| Contribution to Total Iron Intake | 10-15% (Western diets) [81] | 85-90% (Western diets) [81] |
| Influence of Dietary Factors | Relatively unaffected by inhibitors | Strongly inhibited by phytates, polyphenols, calcium |
| Influence of Enhancers | Minimal enhancement effect | Significantly enhanced by vitamin C, organic acids |
Table 2: Dietary Factors Influencing Non-Heme Iron Bioavailability
| Factor | Effect on Absorption | Mechanism | Common Dietary Sources |
|---|---|---|---|
| Inhibitors | |||
| Phytates (phytic acid) | Potent inhibition [81] [78] | Forms insoluble complexes with iron | Whole grains, legumes, nuts, seeds |
| Polyphenols | Significant inhibition [81] [75] | Chelates iron, forming insoluble complexes | Tea, coffee, red wine, herbs, certain grains |
| Calcium | Inhibits both heme and non-heme iron [81] [75] | Competes for absorption transporters | Dairy products, fortified foods, supplements |
| Enhancers | |||
| Ascorbic Acid (Vitamin C) | Powerful enhancement [81] [75] [78] | Reduces Fe³⁺ to Fe²⁺, forms absorbable complexes | Citrus fruits, bell peppers, strawberries, broccoli |
| Muscle Tissue ("Meat Factor") | Enhances non-heme absorption [81] | Mechanism not fully understood; cysteine-containing peptides proposed | Meat, fish, poultry |
| Organic Acids (citric, lactic, malic) | Moderate enhancement [81] | Chelates iron, maintaining solubility | Various fruits and vegetables |
Research Protocol: Caco-2 Cell Bioassay for Iron Bioavailability
The Caco-2 cell model represents a validated in vitro method for assessing iron bioavailability from complex food matrices, combining simulated human digestion with cellular uptake measurement [82]. This protocol is particularly valuable for screening biofortified foods, evaluating dietary interventions, and studying absorption mechanisms without human trials.
Principle and Experimental Workflow
The assay simulates gastrointestinal digestion of test foods, followed by measurement of iron uptake using human intestinal epithelial cells (Caco-2 line). Differentiated Caco-2 cells form polarized monolayers expressing intestinal transport proteins, including DMT1 and ferroportin. Bioavailability is quantified via intracellular ferritin formation, a marker for iron uptake and utilization [82].
Materials and Reagents
Table 3: Essential Research Reagents for Caco-2 Iron Bioavailability Assay
| Reagent/Cell Line | Specification/Function | Application Notes |
|---|---|---|
| Caco-2 cells | Human colorectal adenocarcinoma line (HTB-37) | Differentiates into enterocyte-like cells; use passages 10-15 for consistency [82] |
| Cell Culture Medium | DMEM with 25 mM HEPES (pH 7.2), 10% FBS, 1% antibiotic-antimycotic | Standard growth medium; switch to MEM for differentiation [82] |
| Collagen-coated plates | 6-well plates (9.66 cm²/well) | Enhances cell attachment and monolayer formation [82] |
| Digestion enzymes | Porcine pepsin (gastric phase), pancreatin-bile extract (intestinal phase) | Simulate human gastrointestinal conditions [82] |
| Dialysis membranes | Acid-washed, molecular weight cutoff 12-14 kDa | Separates bioaccessible iron for cellular uptake [82] |
| Cation exchange resin | e.g., Chelex 100 | Removes contaminant iron from pancreatin-bile solution [82] |
| Ferritin immunoassay | Species-specific ELISA/EIA kit | Quantifies cellular iron uptake via ferritin formation [82] |
Step-by-Step Procedure
Sample Preparation
- Obtain 100-150 g of test food material to ensure representative sampling [82]
- Rinse with distilled-deionized water to remove soil contaminants
- Process using non-contaminating equipment (stainless steel recommended)
- Lyophilize and grind to homogeneous powder using standard coffee grinder
- Use 0.5 g lyophilized sample per replicate (avoids dialysis membrane clogging)
Caco-2 Cell Culture
- Culture stock Caco-2 cells in T225 flasks at 37°C, 5% CO₂ [82]
- Seed at 30,000 cells/cm² for maintenance, passage every 7-10 days
- For experiments: seed collagen-coated 6-well plates at 50,000 cells/cm²
- Differentiate for 12 days, changing medium every 48 hours
- On day 12: replace with Minimum Essential Medium (MEM) with supplements
- On day 13 (assay day): replace with 1 mL fresh MEM (pH 7.0)
In Vitro Digestion
- Prepare pepsin solution: 0.145 g in 50 mL 0.1 M HCl [82]
- Prepare pancreatin-bile solution: 0.35 g pancreatin + 2.1 g bile extract in 175 mL 0.1 M NaHCO₃
- Treat pancreatin-bile solution with cation exchange resin to remove contaminant iron
- Gastric phase: Incubate sample with 10 mL physiological saline (pH 2) + 0.5 mL pepsin solution for 1 hour at 37°C with gentle rocking
- Intestinal phase: Adjust pH to 5.5-6.0 with 1 M NaHCO₃, add 2.5 mL pancreatin-bile solution
Iron Uptake Measurement
- Insert acid-washed dialysis membrane rings into 6-well plates
- Add digestive mixture to apical chamber
- Incubate 2 hours at 37°C, 5% CO₂
- Harvest cells for ferritin analysis via ELISA
- Normalize ferritin to total cellular protein
- Calculate iron bioavailability relative to iron content of original sample
Quality Control Considerations
- Include iron standards (e.g., FeSO₄) as reference in each assay run
- Maintain consistent passage number (10-15) to minimize phenotypic drift
- Verify monolayer integrity and differentiation status
- Process samples in triplicate to account for biological variability
- Include blank digestions to correct for background iron contamination
Molecular Regulation of Iron Absorption
Iron absorption is regulated at multiple levels, from systemic hormonal control to cellular transport mechanisms. The key regulator is hepcidin, a liver-derived peptide hormone that controls ferroportin-mediated iron efflux from enterocytes and macrophages [75] [80]. During iron deficiency or increased demand, hepcidin production decreases, allowing ferroportin to remain active on basolateral membranes and enhance iron absorption into circulation.
Recent Research Findings and Adaptations
A 2025 controlled trial demonstrated that vegans exhibit significantly higher non-heme iron absorption compared to omnivores, with serum iron area under the curve (AUC) of 1002.8 ± 143.9 µmol/L/h versus 853 ± 268.2 µmol/L/h following pistachio consumption [79] [80]. This enhanced absorption correlated with lower hepcidin levels (β = -0.5, p = 0.03), suggesting a physiological adaptation to plant-based diets that improves iron utilization efficiency.
This finding challenges the conventional paradigm that vegetarians and vegans are inherently at higher risk for iron deficiency solely due to non-heme iron's lower bioavailability. Instead, it indicates that long-term dietary patterns induce regulatory adaptations that may compensate for differences in iron forms [79] [80]. However, population studies continue to show that female adolescents and women of childbearing age remain vulnerable groups, with Polish data indicating inadequate iron intake in menstruating adolescents regardless of dietary pattern [77].
The comparison of heme versus non-heme iron absorption reveals a complex interplay between chemical form, dietary context, and physiological adaptation. While heme iron demonstrates consistently higher bioavailability, the human body exhibits remarkable adaptability to plant-based iron sources through regulatory mechanisms like hepcidin modulation. The Caco-2 cell bioassay provides researchers with a robust, reproducible method for evaluating iron bioavailability from diverse food sources, particularly valuable for screening biofortified crops and functional foods. Future research should focus on longitudinal studies of iron status in diverse populations and refine in vitro models to better predict human absorption, supporting development of effective strategies to address global iron deficiency.
Within nutritional sciences and food research, accurately assessing nutrient bioavailability—the fraction of an ingested nutrient that is absorbed, becomes available for physiological functions, and is utilized by the body—is paramount for developing effective dietary guidelines, functional foods, and therapeutic nutrition [30] [3]. The choice of methodology for these assessments presents a significant trade-off between the physiological precision of in vivo models and the high throughput, cost-effectiveness, and ethical advantages of in vitro systems [83]. Researchers and drug development professionals must navigate this methodological landscape to select the most appropriate tools for their specific context of use. This application note provides a detailed comparison of these approaches, framed within the broader thesis of optimizing protocols for assessing nutrient bioavailability, and includes standardized experimental procedures to enhance reproducibility and data comparability across studies.
Defining the Key Concepts: Bioavailability vs. Bioaccessibility
A critical first step in methodology selection is understanding the distinct phases of nutrient assimilation.
- Bioavailability is a comprehensive term defined as the amount of an ingested nutrient that is absorbed and available for physiological functions [30] [24]. It encompasses the entire journey of a nutrient: digestion, release from the food matrix, absorption by intestinal cells, transport to systemic circulation, metabolism, and eventual utilization by tissues [30] [84].
- Bioaccessibility, in contrast, is a subset of bioavailability. It refers specifically to the amount of an ingested nutrient that is released from the food matrix during digestion and is therefore potentially available for absorption [30] [84]. It is dependent on digestion and release from the food matrix but does not include the steps of cellular absorption and metabolism [30].
In vitro methods are generally capable of measuring bioaccessibility or specific components of absorption, whereas in vivo studies are required to determine true, systemic bioavailability [30] [84].
Comparative Analysis: In Vivo vs. In Vitro Methodologies
The following table summarizes the core characteristics, advantages, and limitations of in vivo and in vitro approaches for bioavailability assessment.
Table 1: Comprehensive Comparison of In Vivo and In Vitro Bioavailability Assessment Methods
| Aspect | In Vivo Methods | In Vitro Methods |
|---|---|---|
| Definition | Studies conducted within a living organism, such as humans, rodents, or swine. | Studies conducted outside a living organism, simulating biological processes in a controlled environment. |
| Primary Measured Endpoint | Systemic bioavailability; absorption and utilization for physiological functions [3]. | Bioaccessibility; nutrient release from the matrix, and sometimes uptake/transport [30]. |
| Key Advantages | High physiological relevance; accounts for complete host physiology, including immune system, metabolism, and endocrine signaling [83] [3]. | High throughput; rapid, cost-effective, enable screening of many samples [30] [85]. |
| Inherent Limitations | Low throughput; time-consuming, expensive, and involve ethical constraints [85]. | Limited physiological correlation; absence of systemic feedback, nervous system, and endocrine signals [83]. |
| Data Output | Quantitative absorption data; provides a direct measure of the fraction of nutrient absorbed and utilized [3]. | Reproducibility and control; offer better control of experimental variables and ease of sampling [30] [84]. |
| Regulatory Status | Often required for nutrient content claim substantiation in various jurisdictions (e.g., PDCAAS in North America) [85]. | Primarily used as a screening or research tool; not yet widely accepted for regulatory claims, though this is evolving [85] [84]. |
| Host Factor Consideration | Can incorporate host factors like nutrient status, age, genotype, and health status [30]. | Cannot factor in host factors that influence nutrient absorption [30]. |
The Decision Pathway for Method Selection
The choice between in vivo and in vitro methodologies depends on the research question's stage and goal. The following workflow diagram outlines a logical decision-making process for selecting the appropriate methodology.
Diagram Title: Methodology Selection Workflow
Detailed Experimental Protocols
Protocol 1: Static In Vitro Digestion for Bioaccessibility
This protocol outlines a standardized static digestion method suitable for high-throughput screening of nutrient bioaccessibility from food matrices, based on the INFOGEST framework [24] [84].
1. Principle: To simulate the sequential gastric and intestinal phases of human digestion in a static system, enabling the measurement of the fraction of a nutrient released from the food matrix (i.e., bioaccessible) [30] [84].
2. Applications: Studying effects of food matrix, processing, and ingredient interactions on mineral (e.g., iron, zinc), vitamin, and carotenoid bioaccessibility [30] [24].
3. Materials and Reagents:
- Simulated Gastric Fluid (SGF): Prepare with pepsin (e.g., from porcine stomach mucosa) and adjust to pH 2.0-3.0 using HCl to simulate adult gastric conditions [30].
- Simulated Intestinal Fluid (SIF): Prepare with pancreatin (containing amylase, lipase, proteases) and bile salts. Adjust to pH 6.5-7.0 using NaHCO₃ [30].
- Water Bath or Incubator: Maintained at 37°C with continuous agitation to simulate body temperature and peristalsis [30].
- Centrifuge: For separating soluble (bioaccessible) fraction from undigested residue.
4. Step-by-Step Procedure:
1. Sample Preparation: Homogenize the test food to a consistent particle size.
2. Gastric Phase: Mix the food sample with SGF and incubate at 37°C for a defined period (e.g., 1-2 hours) with continuous shaking.
3. Intestinal Phase: Adjust the gastric chyme to pH ~6-7 using NaHCO₃ solution. Add SIF and incubate for another 2 hours at 37°C with shaking.
4. Termination & Separation: Centrifuge the final intestinal digest (e.g., at 10,000 × g, 30 min, 4°C). The supernatant contains the mixed micelles and soluble fraction.
5. Analysis: Quantify the nutrient of interest in the supernatant using appropriate analytical techniques (e.g., HPLC, ICP-MS, AAS). Calculate bioaccessibility as:
Bioaccessibility (%) = (Mass of nutrient in supernatant / Total mass of nutrient in test sample) × 100 [84].
Protocol 2: Caco-2 Cell Model for Nutrient Absorption
This protocol describes the use of the human intestinal Caco-2 cell line to model nutrient uptake and transport, a key component of bioavailability [30].
1. Principle: Caco-2 cells, derived from a human colon carcinoma, spontaneously differentiate into enterocyte-like cells when cultured on permeable supports. They form tight junctions and express brush border enzymes and transporters, making them a valuable model for studying intestinal absorption [30] [86].
2. Applications: Investigation of nutrient uptake kinetics, transporter mechanisms, and the effects of inhibitors/enhancers on mineral (e.g., iron, selenium) and organic compound (e.g., polyphenols) absorption [30] [86] [24].
3. Materials and Reagents:
- Caco-2 Cells: Human colon adenocarcinoma cell line (available from cell banks like ATCC).
- Transwell Inserts: Permeable supports with a porous membrane (e.g., 0.4 μm or 3.0 μm pore size) to allow for separate access to apical and basolateral compartments [30].
- Cell Culture Medium: Dulbecco's Modified Eagle Medium (DMEM) supplemented with fetal bovine serum (FBS), non-essential amino acids, and antibiotics.
- In Vitro Digest: The sample to be tested, prepared via the in vitro digestion protocol (Section 4.1). Note: The digest must be treated (e.g., via dialysis membrane or heat inactivation) to protect cells from digestive enzymes [30].
4. Step-by-Step Procedure: 1. Cell Culture: Seed Caco-2 cells at high density on Transwell inserts and culture for 14-21 days to allow for full differentiation. Monitor transepithelial electrical resistance (TEER) to confirm the formation of tight junctions. 2. Sample Application: Apply the in vitro digest (after enzyme inactivation) to the apical compartment. The basolateral compartment contains transport medium (e.g., serum-free culture medium). 3. Incubation: Incubate the cell system at 37°C in a 5% CO₂ atmosphere for a defined period (e.g., 2-24 hours). 4. Sample Collection: Collect samples from the basolateral compartment at designated time points to measure transported nutrient. 5. Analysis: Quantify the nutrient that has been transported to the basolateral side using analytical methods (HPLC, ICP-MS). Uptake can also be measured by analyzing nutrient content in the cell monolayer after washing [30] [86].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents and Materials for Bioavailability Research
| Research Reagent/Material | Function in Experiment |
|---|---|
| Pepsin (porcine) | Simulates gastric proteolysis in in vitro digestion models, breaking down proteins in the food matrix [30]. |
| Pancreatin & Bile Salts | Simulates intestinal digestion. Pancreatin provides key enzymes (amylase, lipase, proteases), while bile salts emulsify lipids, crucial for micelle formation and solubilization of hydrophobic nutrients [30]. |
| Caco-2 Cell Line | A human cell line that models the intestinal epithelium; used for studying uptake, transport, and competition of nutrients at the site of absorption [30] [86]. |
| Transwell Inserts | Permeable supports for growing cell monolayers; enable separate access to apical (intestinal lumen) and basolateral (blood side) compartments for transport studies [30]. |
| Dialyzability Setup | Dialysis tubing or hollow-fibre systems used to separate low molecular weight, soluble compounds after digestion, representing the bioaccessible fraction [30] [24]. |
| Atomic Absorption Spectrophotometry (AAS)/ICP-MS | Highly sensitive analytical techniques for the quantitative detection and speciation of minerals and trace elements (e.g., Fe, Zn, Se) in digests, cells, and fluids [30] [86]. |
The strategic choice between in vivo precision and in vitro throughput is not a matter of selecting a superior method, but of aligning the methodology with the research objective. In vitro models offer an unparalleled, ethically favorable tool for high-throughput screening, mechanistic studies, and the rational design of functional foods during early development. However, their predictive power is maximized only when validated against in vivo data [84]. For definitive quantitative absorption data and regulatory substantiation, in vivo studies remain indispensable. A synergistic approach, leveraging the strengths of both methodologies in a tiered testing strategy, represents the most efficient and scientifically robust path forward for advancing research in nutrient bioavailability.
Nutrient bioavailability is defined as the fraction of a nutrient in a food that is absorbed and utilized by the body [3]. For sustainable diet models, which often rely heavily on plant-based sources, understanding and accurately assessing bioavailability is not merely an academic exercise but a fundamental requirement for validating nutritional adequacy. The presence of inhibitors and enhancers within food matrices, coupled with individual physiological factors, means that the total nutrient content of a food is a poor predictor of its nutritional value [3] [4] [87]. This document provides detailed application notes and protocols for researchers to integrate robust bioavailability assessment into the evaluation of sustainable diets, moving beyond static food composition data to a dynamic, physiologically relevant model.
Core Concepts and Key Interactions
The bioavailability of a nutrient is governed by a complex interplay of food composition, processing, and host factors. The following table summarizes major enhancers and inhibitors for key nutrients, with particular relevance to plant-forward, sustainable diets.
Table 1: Key Dietary Factors Affecting Nutrient Bioavailability
| Nutrient | Enhancers | Inhibitors | Key Considerations for Sustainable Diets |
|---|---|---|---|
| Non-Heme Iron (Plant-based) | Vitamin C (ascorbic acid) [87] [88] | Phytates (whole grains, legumes), Polyphenols/Tannins (tea, coffee), Oxalates (spinach, rhubarb) [87] [88] | Vitamin C-rich fruits/vegetables can be strategically paired with iron-rich plants. |
| Calcium | Vitamin D, Lactose (in milk), Certain amino acids (L-lysine, L-arginine) [4] | Oxalates (spinach, rhubarb), Phytates, Sulfur-containing proteins (can increase urinary loss) [4] [87] | Bioavailability from low-oxalate vegetables (e.g., kale) is superior to high-oxalate sources (e.g., spinach). |
| Zinc | Organic acids (e.g., citric acid) [3] | Phytates (strong inhibitor) [3] [87] | Processing methods like fermentation and sprouting can reduce phytate content. |
| Fat-Soluble Vitamins (A, D, E, K) | Dietary fats [87] | Very low-fat meals [87] | Sustainable diets must ensure adequate healthy fat intake to utilize these vitamins. |
| Vitamin B9 (Folate) | Not applicable | Various natural forms (folates) have different stability and bioavailability compared to synthetic folic acid [22]. |
The relationship between a sustainable diet, its composition, and the ultimate nutritional adequacy is a multi-step process, summarized in the workflow below:
Diagram 1: Bioavailability in Sustainable Diet Assessment
Methodologies for Assessing Bioavailability
A tiered approach, combining in vitro screening with validated in vivo methods, provides a robust framework for assessing bioavailability.
In Vitro Digestion Models
In vitro simulations of human digestion offer a high-throughput, cost-effective screen for relative bioavailability.
Table 2: Key Components of a Static In Vitro Digestion Model
| Phase | Key Parameters | Simulated Conditions | Common Reagents |
|---|---|---|---|
| Oral | Incubation: 2 min, pH 6.8-7.2 | Chewing, α-amylase activity | α-Amylase, Mucin, Electrolytes |
| Gastric | Incubation: 2 hours, pH 2.0-3.0 (adjusted with HCl) | Stomach acid, Pepsin digestion | Pepsin, HCl, Electrolytes |
| Intestinal | Incubation: 2 hours, pH 7.0-7.5 (adjusted with NaHCO₃) | Pancreatic & bile secretion, Nutrient absorption | Pancreatin, Bile salts, NaHCO₃ |
Protocol 1: Static In Vitro Digestion for Mineral Bioavailability
- Sample Preparation: Homogenize test food. Weigh 1-2 g into a digestion vessel.
- Oral Phase: Add simulated salivary fluid (SSF) containing α-amylase. Incubate at 37°C for 2 minutes with constant agitation.
- Gastric Phase: Add simulated gastric fluid (SGF) containing pepsin. Adjust pH to 3.0 with HCl. Incubate at 37°C for 2 hours.
- Intestinal Phase: Add simulated intestinal fluid (SIF) containing pancreatin and bile salts. Adjust pH to 7.0-7.5 with NaHCO₃. Incubate at 37°C for 2 hours.
- Bioaccessibility Analysis: Centrifuge the final chyme. The bioaccessible fraction is the amount of nutrient recovered in the supernatant, measurable via ICP-MS (for minerals) or HPLC (for vitamins). This fraction represents the portion solubilized and available for absorption [4] [89].
In Vivo Methodologies
In vivo studies in humans remain the gold standard for determining true bioavailability.
Protocol 2: Stable Isotope Studies for Mineral Absorption This method is considered definitive for measuring absorption of minerals like iron, zinc, and calcium in humans [3] [4].
- Isotope Administration:
- Intrinsic Labeling: Grow plants hydroponically in a nutrient solution enriched with a stable isotope (e.g., ⁵⁸Fe, ⁶⁷Zn). This incorporates the isotope into the plant tissue, representing the native food form.
- Extrinsic Labeling: For pre-existing foods, mix a highly purified stable isotope of the mineral directly with the test meal. This method is valid if the extrinsic tag exchanges completely with the intrinsic mineral pool in the food [3].
- Subject Administration: Administer the labeled test meal to human volunteers after an overnight fast. Blood samples are collected at baseline and at predetermined intervals.
- Sample Analysis: Isolate the mineral from blood or fecal samples (for fecal monitoring). Analyze isotopic enrichment using Inductively Coupled Plasma Mass Spectrometry (ICP-MS).
- Calculation: Calculate absorption based on the appearance of the tracer in the blood (plasma or erythrocytes, e.g., for iron incorporation into red blood cells) or its disappearance from the feces [3] [4].
Protocol 3: Postprandial Kinetic Studies for Vitamins and Bioactives This protocol assesses the absorption and metabolism of vitamins (e.g., C, B2, B9) and phenolic compounds [89] [22].
- Study Design: A single-dose, cross-over design is typical. Subjects fast overnight before consuming the test meal.
- Blood Collection: Collect blood samples at baseline (t=0) and at frequent intervals postprandially (e.g., 0.5, 1, 2, 4, 6, 8, 24 hours).
- Plasma Analysis: Isolate plasma. Deproteinize samples and analyze for the target nutrient and its metabolites using High-Performance Liquid Chromatography coupled with tandem Mass Spectrometry (HPLC-MS/MS).
- Pharmacokinetic Analysis: Calculate key parameters: Area Under the Curve (AUC), which reflects total systemic exposure; Cmax (maximum concentration); and Tmax (time to reach Cmax) [90] [89].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Bioavailability Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| Stable Isotopes (e.g., ⁵⁸Fe, ⁴⁴Ca, ²H-Folate) | Tracers for studying absorption, metabolism, and retention in human subjects without radioactivity [3] [4]. | Gold-standard for measuring mineral absorption in vivo (Protocol 2). |
| Simulated Digestive Fluids (Salivary, Gastric, Intestinal) | Standardized mixtures of enzymes, salts, and buffers to replicate human GI conditions in vitro [4]. | Core component of in vitro digestion models (Protocol 1). |
| HPLC-MS/MS Systems | High-sensitivity identification and quantification of nutrients and their metabolites in complex biological samples like plasma and urine [89] [22]. | Analyzing postprandial plasma concentrations of vitamins and polyphenols (Protocol 3). |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Ultra-sensitive elemental analysis for quantifying mineral concentrations and isotopic ratios in food and biological samples [4]. | Measuring mineral concentration in in vitro supernatants and isotopic enrichment in blood/feces. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that, upon differentiation, exhibits enterocyte-like properties. Used to model intestinal absorption and transport [3]. | Studying transport mechanisms and uptake of nutrients after in vitro digestion. |
A Framework for Predictive Modeling
To translate research findings into practical tools for diet evaluation, a structured framework for developing predictive algorithms is essential. The International Life Sciences Institute (ILSI) has proposed a four-step process [91] [13]:
Diagram 2: Predictive Bioavailability Algorithm Framework
This framework aims to create equations that adjust total nutrient content based on the presence of known enhancers and inhibitors, providing a more accurate estimate of absorbable nutrient intake for sustainable diet modeling [13]. As a proof of concept, an open-access calcium bioavailability algorithm is being developed for integration into nutrient-tracking platforms [13].
Conclusion
The accurate assessment of nutrient bioavailability is paramount for setting valid dietary recommendations, formulating effective fortified foods and supplements, and evaluating the true nutritional value of diets, especially in the context of shifts towards more plant-based and sustainable eating patterns. A multi-faceted approach that intelligently combines in vivo, in vitro, and in silico methods is essential for a complete picture. Future directions must focus on refining and validating predictive models for a wider range of nutrients, incorporating individual host factors like genetics and gut microbiota into bioavailability estimates, and standardizing protocols to improve inter-study comparability. These advances will directly enhance the efficacy of clinical nutritional interventions and inform the development of next-generation, precision nutrition solutions in biomedical research.
References
- 1. Bioavailability of bioactive food compounds: a challenging journey to bioefficacy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575927/]
- 2. Trust your gut: Bioavailability and bioaccessibility of dietary compounds - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8787780/]
- 3. sciencedirect.com/topics/medicine-and-dentistry/ nutrient - bioavailability [https://www.sciencedirect.com/topics/medicine-and-dentistry/nutrient-bioavailability]
- 4. Bioavailability of Micronutrients From Nutrient-Dense Whole Foods: Zooming in on Dairy, Vegetables, and Fruits - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7393990/]
- 5. - Wikipedia Bioavailability [https://en.wikipedia.org/wiki/Bioavailability]
- 6. Nutritional assessment ‑ Food Composition [https://nutritionalassessment.org/bioavailability/index.html]
- 7. of bioactive Bioavailability compounds: a challenging journey to... food [https://pubmed.ncbi.nlm.nih.gov/22897361/]
- 8. Section 1 - LADME Scheme [https://www.rxkinetics.com/pktutorial/1_2.html]
- 9. Frontiers | Micronutrient Bioavailability: Concepts, Influencing Factors, and Strategies for Improvement [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1646750/abstract]
- 10. A New Approach to Understanding Nutrient Intake: An ILSI US & Canada Framework [https://www.prnewswire.com/news-releases/a-new-approach-to-understanding-nutrient-intake-an-ilsi-us--canada-framework-302619857.html]
- 11. Enhancing Nutrient : FRL's Advanced Techniques Bioavailability [https://www.foodresearchlab.com/insights/what-science-can-do/enhancing-nutrient-bioavailability-frls-advanced-techniques/]
- 12. Integrating nutrient bioavailability and co-production links when identifying sustainable diets: How low should we reduce meat consumption? | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0191767]
- 13. A New Approach to Understanding Nutrient Intake: An ILSI US... [https://finance.yahoo.com/news/approach-understanding-nutrient-intake-ilsi-191700589.html]
- 14. Impacting Nutritional Requirement Genetic Factors [https://www.news-medical.net/health/Genetic-Factors-Impacting-Nutritional-Requirement.aspx]
- 15. Frontiers | Editorial: Precision nutrition and nutrients: making the promise a reality [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1553149/full]
- 16. Gene–environment interactions and their impact on human health | Genes & Immunity [https://www.nature.com/articles/s41435-022-00192-6]
- 17. 6 Contextual Factors : Host , Diet/Environment, and Health Status [https://nap.nationalacademies.org/read/25023/chapter/7]
- 18. Are you absorbing the nutrients you eat? - MSU Extension [https://www.canr.msu.edu/news/are_you_absorbing_the_nutrients_you_eat]
- 19. The food matrix: implications in processing, nutrition and health - PubMed [https://pubmed.ncbi.nlm.nih.gov/30040431/]
- 20. Food Matrix: Implications for Nutritional Quality | SpringerLink [https://link.springer.com/chapter/10.1007/978-981-19-4590-8_3]
- 21. The Science of Bioavailability in Micronutrients [https://www.numberanalytics.com/blog/science-bioavailability-micronutrients]
- 22. of vitamins C, B2 and B9 (Folate) in Bioavailability and... nutrition [https://fppn.biomedcentral.com/articles/10.1186/s43014-025-00330-3]
- 23. Applications of stable , nonradioactive isotope tracers in in ... vivo [https://www.nature.com/articles/emm201597?error=cookies_not_supported&code=4a5015b0-2160-4fc6-8cbc-d1cf8fbbe92c]
- 24. Frontiers | A Narrative Review: In-vitro Methods for Assessing... [https://www.frontiersin.org/journals/sustainable-food-systems/articles/10.3389/fsufs.2021.727533/full]
- 25. Biofortified and bioavailable: The gold for... - GOV.UK standard [https://www.gov.uk/research-for-development-outputs/biofortified-and-bioavailable-the-gold-standard-for-plant-based-diets]
- 26. Geochemistry: Stable and Radioactive Isotopes – Isobar Science [https://isobarscience.com/geochemistry/]
- 27. 2. Radioactive and Stable Isotopes [https://www.isotopesmatter.com/lessons/2_1.html]
- 28. Isotopes of gold - Wikipedia [https://en.wikipedia.org/wiki/Isotopes_of_gold]
- 29. 2 ENRICHED STABLE | ISOTOPES for Medicine and the... Isotopes [https://nap.nationalacademies.org/read/4818/chapter/4]
- 30. Application of in vitro bioaccessibility and bioavailability methods for calcium, carotenoids, folate, iron, magnesium, polyphenols, zinc, and vitamins B6, B12, D, and E - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3429087/]
- 31. Role of animal in biomedical models : a review - PMC research [https://pmc.ncbi.nlm.nih.gov/articles/PMC9247923/]
- 32. Notes for The role and ethical of considerations in... animal research [https://www.revisiondojo.com/ib/ib-psychology/ib-psychology-the-value-of-animal-models-in-research-to-provide-insig-30435/notes]
- 33. W5002: Nutrient Bioavailability--Phytonutrients and Beyond – NIMSS [https://nimss.org/projects/view/mrp/outline/19012]
- 34. The Ethics of Animal in Preclinical Testing Models [https://www.news-medical.net/life-sciences/The-Ethics-of-Animal-Models-in-Preclinical-Testing.aspx]
- 35. : Evolving Standards for 2024- Animal Research Ethics 2025 [https://editverse.com/animal-research-ethics-evolving-standards-for-2024-2025/]
- 36. of Limitations | National Anti-Vivisection SocietyTBD Animal Research [https://navs.org/insight/limitations-of-the-animal-model/]
- 37. and In Silico Treatment: Bridging Animal Gaps Models Research [https://scisimple.com/en/articles/2025-09-12-animal-models-and-in-silico-treatment-bridging-research-gaps--a37ldnd]
- 38. sciencedirect.com/topics/ food -science/ nutrient - bioavailability [https://www.sciencedirect.com/topics/food-science/nutrient-bioavailability]
- 39. Review of in for vitro of... digestion models rapid screening [https://pubs.rsc.org/en/content/articlehtml/2010/fo/c0fo00111b]
- 40. A review of in - vitro digestibility models on diverse foods in various... [https://link.springer.com/article/10.1007/s44187-025-00454-y]
- 41. A Review on In Vitro Evaluation of Chemical and Physical Digestion for Controlling Gastric Digestion of Food - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027026/]
- 42. A miniaturised semi-dynamic in-vitro model of human digestion | Scientific Reports [https://www.nature.com/articles/s41598-024-54612-w]
- 43. Frontiers | Progress and challenges in designing dynamic in vitro gastric models to study food digestion [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1399534/full]
- 44. A standardised static in vitro digestion method suitable for food - an international consensus - PubMed [https://pubmed.ncbi.nlm.nih.gov/24803111/]
- 45. Review of in for vitro of... digestion models rapid screening [https://www.semanticscholar.org/paper/Review-of-in-vitro-digestion-models-for-rapid-of-Mcclements-Li/02a29e8cf2fbb51d190476ed4e538a61dd9e939b]
- 46. Framework for Developing Prediction Equations ... [https://pubmed.ncbi.nlm.nih.gov/40683371/]
- 47. Artificial intelligence-enhanced bioavailability studies [https://www.sciencedirect.com/science/article/abs/pii/S0924224425003395]
- 48. The use of linear programming approach in diet optimization ... [https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-025-22414-y]
- 49. Diet optimization: modeling iron and zinc absorption by ... [https://www.sciencedirect.com/science/article/pii/S000291652500379X]
- 50. Artificial Intelligence-Enabled Ingredient Substitution in ... [https://www.mdpi.com/2304-8158/14/22/3919]
- 51. In silico analyses as a tool for regulatory assessment of ... [https://www.sciencedirect.com/science/article/abs/pii/S2468111325000325]
- 52. Multiscale Mathematical Modeling in Systems Biology [https://www.mdpi.com/2223-7747/14/3/470]
- 53. Dietary Zn—Recent Advances in Studies on Its ... [https://www.mdpi.com/1420-3049/30/13/2742]
- 54. Plant food anti-nutritional factors and their reduction strategies: an overview | Food Production, Processing and Nutrition | Full Text [https://fppn.biomedcentral.com/articles/10.1186/s43014-020-0020-5]
- 55. Is There Such a Thing as “ Anti - Nutrients ”? A Narrative Review of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7600777/]
- 56. A review on anti-nutritional factors: unraveling the natural gateways to human health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10501406/]
- 57. Innovative genetic approaches to minimize anti-nutritional compounds in staple crops for future food security [https://www.abrinternationaljournal.org/articles/innovative-genetic-approaches-to-minimize-antinutritional-compounds-in-staple-crops-for-future-food-security-110321.html]
- 58. - Anti Explained: Nutrients , Oxalates And ‘Toxic’ Vegetables Lectins [https://www.forbes.com/sites/christopherthompson/2025/10/08/anti-nutrients-explained-oxalates-lectins-and-toxic-vegetables/]
- 59. Biomarkers of Nutrition and Health: New Tools for New Approaches - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6567133/]
- 60. Harnessing Microbes for Sustainable Development: Food Fermentation as a Tool for Improving the Nutritional Quality of Alternative Protein Sources - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7230334/]
- 61. for Plant-based Diets: Managing Nutrition Intake and... Nutrient [https://khni.kerry.com/news/plant-based/nutrition-for-plant-based-diets-managing-nutrient-intake-and-bioavailability/]
- 62. Plant sprout foods: Biological activities, health benefits, and bioavailability - PubMed [https://pubmed.ncbi.nlm.nih.gov/34050545/]
- 63. The nutritional profile of chia seeds and sprouts: tailoring germination practices for enhancing health benefits-a comprehensive review - PubMed [https://pubmed.ncbi.nlm.nih.gov/38622873/]
- 64. of Micronutrients from Plant Foods: An Update Bioavailability [https://pubmed.ncbi.nlm.nih.gov/25748063/]
- 65. Microbial Fermentation in Food: Impact on Functional Properties and Nutritional Enhancement—A Review of Recent Developments [https://www.mdpi.com/2311-5637/11/1/15]
- 66. and Iron : Vitamin Mechanism of Action C Synergistic [https://www.linkedin.com/pulse/iron-vitamin-c-synergistic-mechanism-action-amit-katoch-qdcjf]
- 67. Food synergies for improving bioavailability of micronutrients from... [https://pubmed.ncbi.nlm.nih.gov/28867091/]
- 68. -based Delivery Nanotechnology for Enhanced... Systems [https://www.foodandnutritionjournal.org/vol13nospl-issue-phytonutrients-2025/nanotechnology-based-delivery-systems-for-enhanced-bioavailability-of-antioxidant-compounds-in-fruits-and-vegetables/]
- 69. : A novel tool to enhance the Nanotechnology of... bioavailability [https://pmc.ncbi.nlm.nih.gov/articles/PMC8194941/]
- 70. Nanoscale Nutrient Delivery Systems for Food Applications: Improving... [https://pubmed.ncbi.nlm.nih.gov/26073042/]
- 71. -Based Nutraceuticals, Nutrigenomics... | SpringerLink Nanomaterials [https://link.springer.com/chapter/10.1007/978-981-99-5045-4_6]
- 72. Perspective: Framework for Developing Prediction Equations for Estimating the Absorption and Bioavailability of Nutrients from Foods [https://hsrc.himmelfarb.gwu.edu/gwhpubs/7571/]
- 73. Modeling Techniques- A Comprehensive Guide [ Predictive ] 2025 [https://www.projectpro.io/article/predictive-modelling-techniques/598]
- 74. , Recalibration, and Validation of Published... Predictive Accuracy [https://pubmed.ncbi.nlm.nih.gov/36069964/]
- 75. Biochemistry, Iron Absorption - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK448204/]
- 76. • The Nutrition Iron Source [https://nutritionsource.hsph.harvard.edu/iron/]
- 77. Analysis of Heme and Non-Heme Iron Intake and Iron Dietary Sources in Adolescent Menstruating Females in a National Polish Sample - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6567869/]
- 78. Factors Affecting Iron Absorption and Mitigation Mechanisms: A review [https://www.agriscigroup.us/articles/IJASFT-4-133.php]
- 79. Dietary Adaptation of Non - Heme in Vegans... Iron Absorption [https://pubmed.ncbi.nlm.nih.gov/40320969/]
- 80. Dietary Adaptation of Non‐Heme Iron Absorption in Vegans: A Controlled Trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189169/]
- 81. How to Increase the Absorption of Iron from Foods [https://www.healthline.com/nutrition/increase-iron-absorption]
- 82. Caco-2 Cell Bioassay: An In Vitro Method for Measuring Iron ... [https://www.jove.com/t/30422/caco-2-cell-bioassay-an-vitro-method-for-measuring-iron]
- 83. From in vitro Experiments to in vivo and Clinical Studies; Pros and Cons - PubMed [https://pubmed.ncbi.nlm.nih.gov/26778084/]
- 84. Validation of in vitro bioaccessibility assays — a key aspect in the rational design of functional foods towards tailored bioavailability - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2214799321000436]
- 85. In vitro protein digestibility to replace in vivo digestibility for purposes of nutrient content claim substantiation in North America's context - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11157434/]
- 86. of Nine Bioselenocompounds Bioavailability ... Comparison In Vitro [https://pmc.ncbi.nlm.nih.gov/articles/PMC5372522/]
- 87. Interactions and Nutrient | Intro to Bioavailability Class Notes Nutrition [https://fiveable.me/introduction-nutrition/unit-4/nutrient-interactions-bioavailability/study-guide/WGUStQhrXAChaO86]
- 88. Maximizing Nutrient Absorption [https://www.numberanalytics.com/blog/maximizing-nutrient-absorption-bioavailability]
- 89. Recent Analytical Approaches for the Study of Bioavailability and Metabolism of Bioactive Phenolic Compounds - PubMed [https://pubmed.ncbi.nlm.nih.gov/35164041/]
- 90. Relative Bioavailability, Food Effect, and Bioequivalence Studies to Assess a New Zanubrutinib 160-mg Tablet: Results From 2 Phase 1 Studies in Healthy Volunteers - PubMed [https://pubmed.ncbi.nlm.nih.gov/40900302/]
- 91. Algorithms to Estimate Bioavailability of Nutrients from Foods [https://ilsi.org/publication/algorithms-to-estimate-bioavailability-of-nutrients-from-foods/]