Portable vs. Laboratory Allergen Detection: A 2025 Comparative Analysis for Biomedical Research
This article provides a comparative analysis for researchers and drug development professionals on the evolving landscape of food allergen detection.
Portable vs. Laboratory Allergen Detection: A 2025 Comparative Analysis for Biomedical Research
Abstract
This article provides a comparative analysis for researchers and drug development professionals on the evolving landscape of food allergen detection. It explores the foundational principles of both portable devices and established laboratory methods like ELISA and PCR. The analysis covers methodological applications, troubleshooting for complex food matrices, and a critical validation of performance metrics including sensitivity, specificity, and throughput. Synthesizing current market data and technological trends, it concludes with strategic insights on selecting the appropriate method based on research intent and outlines future directions driven by AI, biosensors, and multiplexing technologies.
Understanding the Landscape: Core Technologies in Allergen Detection
Food allergies represent a significant and growing international health problem, affecting approximately 2% of adults and 5-8% of children worldwide [1]. For these individuals, exposure to even trace amounts of allergens can trigger reactions ranging from hives and digestive issues to life-threatening anaphylactic shock [1]. This public health concern is compounded by the economic burden of allergen management, including healthcare costs, product recalls, and regulatory compliance. Accurate allergen detection is therefore a critical component of food safety, serving to protect consumers and manage economic risks.
The field of allergen analysis is currently divided between traditional laboratory-based methods and emerging portable detection technologies. Laboratory methods like ELISA (Enzyme-Linked Immunosorbent Assay) and PCR (Polymerase Chain Reaction) have long been the gold standard, offering high sensitivity and reliability for quality control and regulatory purposes [2] [3]. However, these methods are time-consuming, require trained personnel and specialized equipment, and are generally unsuitable for real-time, on-the-spot testing [3] [1].
In response to these limitations, a new generation of portable food allergen sensors is emerging. These devices are designed to provide rapid, on-site detection, empowering consumers to verify the safety of their food instantly [3]. This guide provides an objective comparison of the performance characteristics, methodologies, and appropriate applications of portable allergen detection devices versus established laboratory methods, framed within the context of ongoing research and technological advancement.
Performance Comparison: Portable Sensors vs. Laboratory Methods
The following table summarizes the key performance metrics of traditional laboratory methods versus emerging portable detection technologies.
Table 1: Performance Comparison of Allergen Detection Methods
| Feature | Traditional Laboratory Methods | Portable Detection Devices |
|---|---|---|
| Primary Examples | ELISA, PCR, Mass Spectrometry [2] [3] | Smartphone-based assays, Handheld electrochemical sensors [3] [1] |
| Detection Principle | Antibody-Antigen binding (ELISA), DNA amplification (PCR), Protein-specific peptide detection (MS) [2] [3] [1] | Electrochemical, Optical (colorimetry, fluorescence), often with antibodies or aptamers [3] |
| Throughput | High (can process many samples simultaneously) | Low to Medium (single or multiplexed tests) |
| Time to Result | Hours to days [3] | Minutes [3] |
| Sensitivity | Very High (e.g., Mass Spectrometry: as low as 0.01 ng/mL) [2] | Variable; can be high, but often lower than lab methods [3] |
| Quantification | Fully Quantitative | Mostly Semi-Quantitative or Qualitative |
| User Skill Requirement | Requires trained technicians | Designed for consumer or front-line staff use |
| Key Advantage | High accuracy, sensitivity, and reliability for compliance | Speed, portability, and ease of use for point-of-care |
| Key Limitation | Time-consuming, expensive, not portable | Limited multiplexing, sensitivity can be affected by food matrix [3] |
Experimental Protocols and Methodologies
Laboratory-Based Methods
A. Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA is a widely used immunochemical method for detecting allergenic proteins. The workflow involves extracting proteins from a food sample and incubating them in wells coated with allergen-specific antibodies. After washing, a second antibody linked to an enzyme is added. A substrate is then introduced, and the enzyme catalyzes a reaction that produces a color change, measured spectrophotometrically, which is proportional to the allergen concentration [3] [1]. While highly sensitive, ELISA can struggle to detect denatured proteins found in cooked foods, and antibody cross-reactivity may lead to false positives [3].
B. Mass Spectrometry (MS)-Based Methods
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) is a powerful proteomic technique. The protocol involves:
- Extraction and Digestion: Proteins are extracted from the food matrix and digested with an enzyme (e.g., trypsin) to generate specific peptide fragments.
- Chromatographic Separation: The peptide mixture is separated by liquid chromatography.
- Mass Analysis & Quantification: Peptides are ionized and identified by their mass-to-charge ratio. Unique proteotypic peptides (e.g., Ara h 3 and Ara h 6 for peanut, Bos d 5 for milk) serve as biomarkers for absolute quantification of specific allergenic proteins [2] [4]. This method offers high specificity and the ability to multiplex, detecting multiple allergens in a single run [2].
Portable Sensor Technologies
A. Electrochemical Sensor Protocol
Handheld sensors, similar to glucometers, use disposable test strips. The experimental process is:
- Sample Preparation: A small, dissolved food sample is applied to the disposable strip.
- Biorecognition: The strip contains a biorecognition element (e.g., an antibody, aptamer, or Molecularly Imprinted Polymer (MIP)) that binds specifically to the target allergen.
- Signal Transduction: This binding event causes a change in electrical properties (current, potential, or impedance).
- Readout: The handheld reader processes this change and provides a digital output (e.g., ppm) within minutes [3]. MIPs are noted for their durability and resistance to heat and acidity, making them suitable for complex food matrices [3].
B. Smartphone-Based Optical Detection Protocol
This approach leverages a smartphone's camera and processing power:
- Assay Execution: The user performs a lateral flow immunoassay (LFIA) or uses a microfluidic chip, following the device instructions.
- Image Capture: The smartphone camera captures an image of the test strip or chip.
- Data Processing: A dedicated app analyzes color intensity or fluorescence patterns.
- Result Delivery: The app interprets the signal, providing a clear "detected/not detected" result or a semi-quantitative concentration, sometimes with geo-tagging capabilities for data mapping [1].
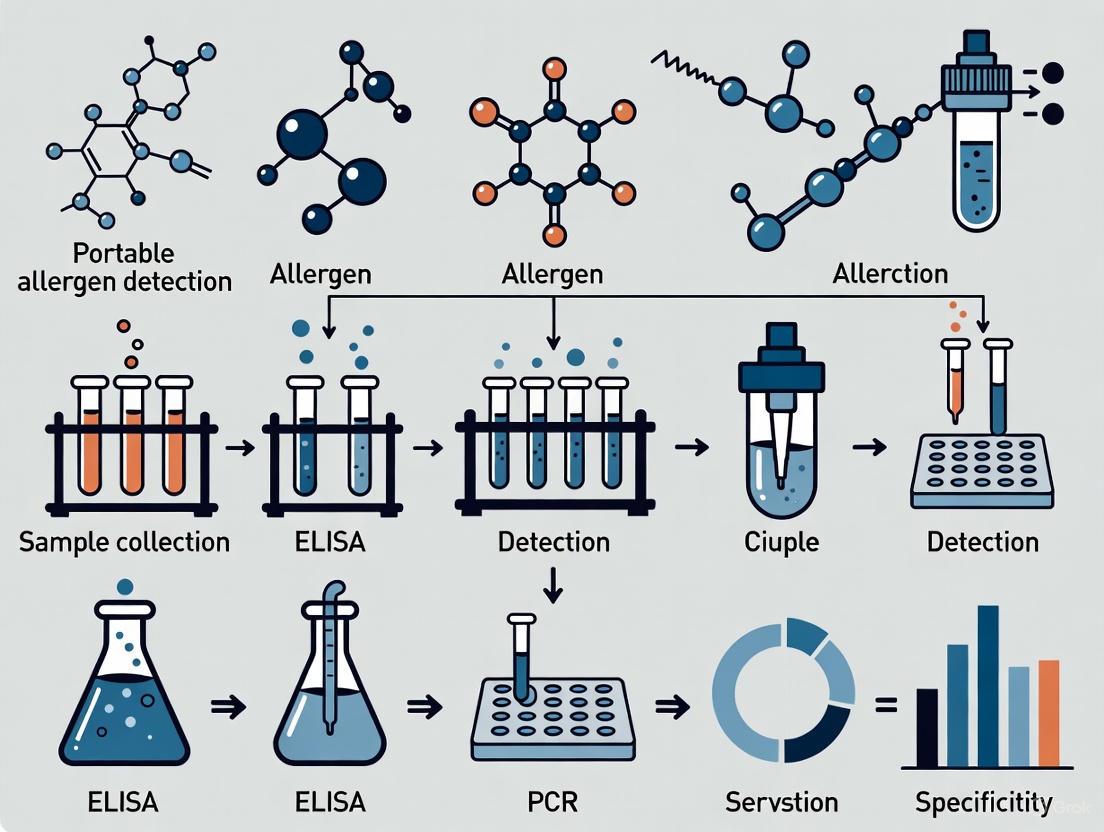
Diagram 1: Method Workflow Comparison
The Scientist's Toolkit: Key Research Reagents & Materials
Successful allergen detection, whether in a lab or a portable format, relies on specific, high-quality reagents. The following table details essential components and their functions.
Table 2: Essential Research Reagents for Allergen Detection
| Reagent/Material | Function in Detection | Application Context |
|---|---|---|
| Allergen-Specific Antibodies | Biorecognition element that binds specifically to target allergenic proteins (e.g., Ara h 1, Bos d 5). | Core component of ELISA, lateral flow devices, and some biosensors [3] [1]. |
| Aptamers | Synthetic single-stranded DNA or RNA oligonucleotides that bind targets with high specificity and affinity. | Used as more stable, cost-effective alternatives to antibodies in some modern biosensors [3]. |
| Molecularly Imprinted Polymers (MIPs) | Synthetic polymers with cavities tailored to fit specific allergen molecules; robust and stable. | Bioreceptor in electrochemical sensors for challenging environments (e.g., cooked foods) [3]. |
| Proteotypic Peptides | Unique peptide sequences that serve as biomarkers for a specific protein in a mass spectrometry assay. | Essential for the development of targeted, quantitative LC-MS/MS methods for specific allergens [2] [4]. |
| Certified Reference Materials (CRMs) | Materials with certified values for allergen/protein content, used for method validation and calibration. | Critical for ensuring accuracy, traceability, and harmonization of measurements across labs; a key focus of programs like the NIST Food Protein Allergen Program [4]. |
| LOINC/NPU Codes | Standardized codes for identifying laboratory tests and results in a universal, unambiguous way. | Used for data harmonization and interoperability, as seen in the CLSI ILA37 database for allergen-specific IgE testing [5]. |
Discussion and Future Directions
The comparison reveals that portable devices and laboratory methods serve complementary roles. Laboratory methods remain indispensable for regulatory compliance, method validation, and quantitative analysis where ultimate accuracy is required. In contrast, portable devices excel in providing rapid, on-the-spot screening for consumers, restaurants, and manufacturing line checks, putting analytical power directly into the hands of users [3].
Future innovation is focused on overcoming current limitations. Research is advancing towards:
- Multiplexing: Developing portable devices that can simultaneously test for multiple allergens from a single sample [3] [1].
- Enhanced Sensitivity: Incorporating nanomaterials like graphene and gold nanoparticles to improve detection limits [3].
- Improved Bioreceptors: Engineering more stable and cost-effective elements like peptide aptamers and nanobodies [3].
- Data Integration: Leveraging Artificial Intelligence (AI) to improve signal interpretation and using the Internet of Things (IoT) to create real-time allergen exposure maps [2] [3].
Diagram 2: Future Technology Directions
In conclusion, the choice between portable and laboratory methods is not a matter of superiority but of application. Researchers and industry professionals must select the appropriate tool based on the required balance between speed, sensitivity, precision, and context of use. The ongoing convergence of these technologies—driven by advancements in materials science, genomics, and data analytics—promises a future with more transparent, reliable, and accessible allergen management systems.
In the context of increasing global food allergies, reliable detection of allergens is crucial for protecting public health. For researchers developing portable allergen detection devices, a deep understanding of established laboratory gold standards is foundational. These traditional methods—Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and Mass Spectrometry (MS)—set the benchmark for sensitivity, specificity, and reliability against which new technologies are measured. This guide provides a detailed, objective comparison of these three core techniques, framing their principles, performance data, and experimental protocols within the needs of modern scientific and development professionals.
Core Principles and Experimental Workflows
The following workflows diagram the standard experimental procedures for each method, highlighting key preparatory and analytical steps.
ELISA Workflow
Diagram Title: ELISA Sandwich Assay Procedure
The Enzyme-Linked Immunosorbent Assay (ELISA) is an antibody-based technique that detects target proteins. In the common sandwich format shown above, a capture antibody immobilized on a plate binds the target allergen. A second enzyme-conjugated detection antibody then binds to the captured allergen. A substrate is added, and the enzyme catalyzes a reaction, producing a color change measured via absorbance. The intensity is proportional to the allergen concentration [6] [7].
PCR Workflow
Diagram Title: Polymerase Chain Reaction (PCR) Process
The Polymerase Chain Reaction (PCR) is a DNA-based method that amplifies specific nucleic acid sequences for detection. The process involves repeated thermal cycles of denaturation, primer annealing, and enzyme-driven extension to exponentially copy a target DNA region. In real-time PCR, fluorescent probes allow for simultaneous amplification and quantification, enabling the detection of allergen-specific DNA from ingredients [8] [9].
Mass Spectrometry Workflow
Diagram Title: LC-MS/MS Protein Analysis Workflow
Mass Spectrometry (MS), particularly Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS), identifies and quantifies proteins by analyzing their peptide fragments. Proteins are digested into peptides, separated by liquid chromatography, ionized, and then analyzed based on their mass-to-charge ratio. The first mass analyzer selects specific peptide ions, which are then fragmented, and a second mass analyzer measures the fragments, generating a "fingerprint" for highly specific identification [6] [10].
Performance Comparison and Experimental Data
The following table summarizes the key performance characteristics of ELISA, PCR, and Mass Spectrometry, drawing from direct comparative studies and evaluations of each technology.
| Performance Metric | ELISA | PCR | Mass Spectrometry |
|---|---|---|---|
| Analytical Target | Protein [8] | DNA [8] | Protein/Peptide [6] |
| Sensitivity (Example) | Pork: 10.0% w/w; Beef: 1.00% w/w [8] | Pork: 0.10% w/w; Beef: 0.50% w/w [8] | Detection limits as low as 0.01 ng/mL for specific allergens [2] |
| Specificity | High (Relies on antibody affinity) [7] | High (Determined by primer design) [8] | Very High (Identifies proteotypic peptides) [2] |
| Multiplexing Capability | Low (Typically one protein per assay) [10] | Moderate with specialized design | High (Can detect many proteins simultaneously) [2] |
| Throughput | Medium to High (96-well plate format) [10] | Medium to High (96-well plate format) | Low to Medium (One sample at a time; scale-up possible) [10] |
| Quantification | Relative or Absolute [10] | Relative or Absolute [10] | Relative or Absolute [10] |
| Sample Input Volume | ~100 µL [10] | Varies (Small amount of DNA) | ~150 µL (highly concentrated) [10] |
| Key Advantage | Cost-effective, regulatory approved, high sensitivity for proteins [7] | Excellent sensitivity, works in processed foods where protein is denatured [8] [7] | Unmatched specificity, can detect multiple allergens in one run, high precision [6] [2] |
| Key Limitation | Can be affected by food processing that denatures protein targets [7] | Detects DNA, not the allergenic protein itself; can be inhibited by food matrices [8] | High cost, requires specialized equipment and trained operators [6] [10] |
Detailed Experimental Protocols
Protocol: Sandwich ELISA for Allergen Detection
This protocol is adapted from procedures used for detecting allergens like peanuts or milk proteins [7].
- Coating: Dilute the capture antibody in a coating buffer (e.g., carbonate-bicarbonate buffer, pH 9.6). Add 100 µL per well to a 96-well microplate. Seal the plate and incubate overnight at 4°C.
- Washing: Aspirate the contents of the wells and wash three times with a wash buffer (e.g., PBS containing 0.05% Tween 20). Blot the plate on absorbent paper to remove residual buffer.
- Blocking: Add 200 µL of blocking buffer (e.g., 1-5% BSA or non-fat dry milk in PBS) to each well. Incubate for 1-2 hours at room temperature. Wash as in step 2.
- Sample & Standard Incubation: Prepare a dilution series of the allergen standard. Extract and prepare food samples in an appropriate extraction buffer. Add 100 µL of standards, samples, and controls (blank) to assigned wells. Incubate for 1-2 hours at room temperature. Wash thoroughly.
- Detection Antibody Incubation: Add 100 µL of the enzyme-conjugated detection antibody (e.g., Horseradish Peroxidase conjugate) diluted in assay buffer to each well. Incubate for 1-2 hours at room temperature. Wash thoroughly.
- Signal Development: Add 100 µL of substrate solution (e.g., TMB for HRP) to each well. Incubate in the dark for 15-30 minutes until color develops.
- Reaction Stopping: Add 50 µL of stop solution (e.g., 1M sulfuric acid) to each well. The color will change from blue to yellow.
- Measurement: Measure the absorbance of each well at 450 nm using a microplate reader within 30 minutes. Plot the standard curve and calculate the allergen concentration in the samples.
Protocol: Real-Time PCR for Meat Species Identification
This protocol is based on a comparative study detecting beef and pork in processed meat products [8].
- DNA Extraction: Use a commercial DNA extraction kit suitable for food matrices. From the homogenized sample, extract genomic DNA following the manufacturer's instructions. Quantify the DNA purity and concentration using a spectrophotometer.
- PCR Reaction Setup: Prepare a master mix for each sample containing:
- SensiFAST Probe No-ROX Mix (or equivalent): 10 µL
- Species-Specific Forward Primer (e.g., for pork): 0.7 µL
- Species-Specific Reverse Primer: 0.7 µL
- Species-Specific TaqMan Probe (with a fluorescent dye, e.g., FAM): 0.2 µL
- Nuclease-Free Water: 6.4 µL
- Total Volume: 18 µL per reaction
- Sample Addition: Add 2 µL of template DNA (or non-template control water) to each PCR tube/strip containing the 18 µL master mix, for a final reaction volume of 20 µL.
- Real-Time PCR Amplification: Place the samples in a real-time PCR instrument and run the following program:
- Initial Denaturation: 95°C for 10 minutes (1 cycle)
- Amplification (40 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 1 minute (with fluorescence data collection)
- Data Analysis: Set the cycle threshold (Ct) manually or allow the instrument software to set it. A sample is considered positive if it produces a Ct value below a predetermined cutoff (e.g., Ct < 40). The Ct value is inversely proportional to the amount of target DNA in the original sample.
Protocol: LC-MS/MS for Allergen-Specific Peptide Detection
This protocol outlines the core steps for detecting allergenic proteins via their proteotypic peptides, as used in high-precision applications [6] [2].
- Protein Extraction and Digestion: Weigh a homogenized food sample. Extract proteins using an appropriate buffer (e.g., urea or SDS-based). Reduce disulfide bonds with dithiothreitol (DTT) and alkylate with iodoacetamide (IAA). Digest the proteins into peptides using a proteolytic enzyme, most commonly trypsin, overnight at 37°C.
- Peptide Clean-up: Desalt the digested peptide mixture using a solid-phase extraction (SPE) cartridge (e.g., C18 resin) to remove interfering salts and buffers. Elute peptides in a solvent compatible with LC-MS/MS (e.g., acetonitrile with 0.1% formic acid) and dry down in a vacuum concentrator.
- Liquid Chromatography (LC): Reconstitute the dried peptides in a mobile phase (e.g., water with 0.1% formic acid). Inject the sample onto a reverse-phase C18 LC column. Separate the peptides using a gradient of increasing organic solvent (e.g., acetonitrile) over time.
- Tandem Mass Spectrometry (MS/MS):
- Ionization: The eluting peptides are ionized via Electrospray Ionization (ESI).
- MS1 Survey Scan: The mass spectrometer performs a full scan to measure the mass-to-charge (m/z) ratios of all intact peptide ions entering the instrument.
- Selection and Fragmentation: The instrument automatically selects the most abundant peptide ions (precursor ions) from the MS1 scan and fragments them using an inert gas (like nitrogen or argon) in a collision cell—a process known as Collision-Induced Dissociation (CID).
- MS2 Fragment Scan: The mass spectrometer then performs a second scan to measure the m/z ratios of the resulting fragment ions.
- Data Analysis: The MS2 fragmentation spectra are searched against a protein database containing the sequences of known allergenic proteins (e.g., Ara h 1 from peanut, Bos d 5 from milk) using specialized software (e.g., MaxQuant, Skyline). The identification of allergen-specific peptides is confirmed by matching the observed fragment ions to the theoretical fragmentation pattern.
Research Reagent Solutions
The table below lists key reagents and materials essential for implementing the described laboratory methods.
| Reagent/Material | Function | Primary Application |
|---|---|---|
| Capture & Detection Antibodies | Specifically bind to the target allergen protein for immobilization and signal generation. | ELISA |
| Microtiter Plates (96-well) | Solid surface for immobilizing capture antibodies and conducting the assay. | ELISA |
| Enzyme Substrate (e.g., TMB) | Chromogenic compound that produces a measurable color change when catalyzed by the detection enzyme. | ELISA |
| Species-Specific Primers & Probes | Short oligonucleotides that bind to and facilitate the amplification/detection of unique DNA sequences. | PCR |
| Taq DNA Polymerase | Heat-stable enzyme that synthesizes new DNA strands during the PCR amplification process. | PCR |
| dNTPs | Deoxynucleotide triphosphates (A, T, C, G); the building blocks for DNA synthesis. | PCR |
| Trypsin | Proteolytic enzyme that digests proteins into smaller peptides for mass spectrometry analysis. | Mass Spectrometry |
| C18 Solid-Phase Extraction Cartridge | Used to desalt and concentrate peptide mixtures prior to LC-MS/MS analysis. | Mass Spectrometry |
| LC Column (e.g., C18) | Chromatographically separates peptides by hydrophobicity before they enter the mass spectrometer. | Mass Spectrometry |
ELISA, PCR, and Mass Spectrometry each offer distinct advantages as laboratory gold standards for allergen detection. ELISA remains the workhorse for routine, high-throughput protein detection due to its cost-effectiveness and regulatory acceptance. PCR provides exceptional sensitivity for DNA, proving valuable when proteins are denatured or for confirming results. Mass Spectrometry offers unrivalled specificity and multiplexing capabilities by directly identifying protein biomarkers, making it a powerful tool for method validation and complex matrices.
For researchers developing portable devices, this comparison highlights critical trade-offs. The ideal portable technology would combine the simplicity and low cost of ELISA, the high sensitivity of PCR, and the definitive specificity of MS. Understanding the principles and performance boundaries of these established methods is key to innovating the next generation of rapid, on-site allergen tests that meet the rigorous demands of food safety and public health.
The increasing global prevalence of food allergies has intensified the need for reliable, rapid detection methods that can be deployed beyond traditional laboratory settings [6]. While conventional techniques like Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) provide highly sensitive and specific results, they require costly equipment, well-trained technicians, and several hours to complete, making them unsuitable for on-site testing [6]. In response, portable biosensors and lateral flow devices have emerged as powerful alternatives that offer rapid, user-friendly, and cost-effective detection of food allergens, enabling point-of-care testing in supply chain settings, restaurants, and even at home [6] [11]. This guide objectively compares the operational principles and performance of these rapid methods against established laboratory techniques, providing researchers and scientists with critical experimental data and protocols for informed methodological selection.
Technology Comparison: Operational Principles and Performance Metrics
Fundamental Principles of Conventional Laboratory Methods
Immunoassays (ELISA): This method relies on the specific binding between an allergen (antigen) and its antibody. The detection is typically achieved through an enzyme-linked antibody that produces a colored product when its substrate is added, with color intensity proportional to the allergen concentration [6]. Nucleic Acid-Based Methods (PCR): PCR amplifies specific DNA sequences unique to allergenic foods, making it highly specific and sensitive. It is particularly useful for detecting allergens in processed foods where protein structures may be denatured [6]. Chromatographic Methods (LC-MS/MS): This technique separates and identifies allergenic proteins based on their mass-to-charge ratio after proteolytic digestion, providing high specificity and the ability to detect multiple allergens simultaneously (multiplexing) [6] [2].
Fundamental Principles of Portable Rapid Methods
Portable Biosensors: These devices consist of a bio-recognition element (e.g., antibody, aptamer, enzyme) that specifically interacts with the target allergen and a transducer that converts this biological interaction into a quantifiable signal [6]. Transduction mechanisms include electrochemical (measuring electrical changes), optical (detecting colorimetric, fluorescent, or SERS signals), and piezoelectric (measuring mass changes) principles [6]. Lateral Flow Devices (LFDs): Also known as lateral flow immunoassays (LFIAs), these paper-based platforms utilize capillary action to move the sample across various zones where the target allergen is captured between labeled and immobilized antibodies, producing a visible test line typically within 5-30 minutes [12] [13]. They can operate in sandwich format (for larger analytes) or competitive format (for small molecules) [14].
Table 1: Comparative Analysis of Allergen Detection Technologies
| Technology | Detection Principle | Detection Time | Sensitivity | Multiplexing Capability | Primary Applications |
|---|---|---|---|---|---|
| ELISA | Antibody-antigen interaction with enzyme-mediated color development | 2-4 hours | ppm to ppb range | Low | Laboratory quantification of specific allergens |
| PCR | Amplification of allergen-specific DNA sequences | 3-6 hours | ppb level | Medium | Laboratory detection, especially for processed foods |
| LC-MS/MS | Separation and identification based on mass-to-charge ratio | Several hours | ppt to ppb range | High | Laboratory reference method, multiplex detection |
| Portable Biosensors | Bio-recognition coupled with electrochemical/optical transduction | Minutes | ppb to ppt range | Medium to High | On-site screening, quality control |
| Lateral Flow Devices | Capillary flow with immunochromatographic detection | 5-30 minutes | ppm to ppb range | Low to Medium | Rapid screening, point-of-care testing |
Table 2: Experimental Performance Data for Allergen Detection in Food Matrices
| Allergen Target | Detection Method | Reported LOD | Matrix | Assay Time | Reference |
|---|---|---|---|---|---|
| Total Hazelnut Protein | Passive Flow-through Immunoassay | 1 ppm | Food matrix | <10 minutes | [11] |
| Total Peanut Protein | Passive Flow-through Immunoassay | 5 ppm | Food matrix | <10 minutes | [11] |
| Total Hazelnut Protein | Active Flow-through Immunoassay | 0.5 ppm | Food matrix | <10 minutes | [11] |
| Total Peanut Protein | Active Flow-through Immunoassay | 1 ppm | Food matrix | <10 minutes | [11] |
| Total Hazelnut Protein | Optimized Lateral Flow Immunoassay | 0.5 ppm | Food matrix | <10 minutes | [11] |
| Total Peanut Protein | Optimized Lateral Flow Immunoassay | 0.5 ppm | Food matrix | <10 minutes | [11] |
| Various Allergens | Electrochemical Biosensing | ppb level | Various foods | Minutes | [6] |
| Various Allergens | SERS Biosensing | ppt to ppb level | Various foods | Minutes | [6] |
Experimental Protocols and Methodological Details
Protocol for Lateral Flow Immunoassay Development
1. Antibody Selection and Characterization: Select high-affinity monoclonal or polyclonal antibodies specific to the target allergen. Characterize binding kinetics using surface plasmon resonance (SPR) to identify antibodies with fast association rates, which is crucial for rapid assays [11]. 2. Conjugate Pad Preparation: Conjugate gold nanoparticles (typically 20-40 nm) or other labels (e.g., latex beads, carbon nanoparticles) to the detection antibody. Optimize the pH and antibody concentration for maximum conjugation efficiency. The conjugate is then sprayed onto the glass fiber pad and dried [11] [12]. 3. Membrane Biofunctionalization: Dispense the capture antibody and control antibody onto the nitrocellulose membrane at the test and control lines, respectively. The membrane's capillary flow rate (typically 120-150 s/4 cm) should be optimized to balance assay speed and sensitivity [11] [12]. 4. Assembly and Cassetting: The sample pad, conjugate pad, nitrocellulose membrane, and absorbent pad are overlapped approximately 2 mm and assembled onto a plastic backing card. The card is then cut into individual strips and housed in plastic cassettes [13].
Protocol for Enhanced Sensitivity Using Electrophoretic LFDs
1. Device Fabrication: Create a portable, 3D-printed electrophoretic device equipped with electrodes and a power source (battery-operated) [15]. 2. Assay Operation: Apply the sample to the LFD strip and initiate an electric field to control fluid movement. The electrophoretic force enables iterative incubation and washing steps directly on the nitrocellulose strip, overcoming mass transport limitations of conventional capillary flow [15]. 3. Signal Detection and Quantification: After optimization of parameters (Joule heating, buffer evaporation, and electroosmotic flow), the accumulated gold nanoparticles at the test line are measured visually or using a portable reader. This approach has demonstrated a 367-fold improvement in sensitivity for human lactate dehydrogenase detection compared to conventional LFIAs [15].
Protocol for Biosensor-Based Allergen Detection
1. Recognition Element Immobilization: Immobilize bio-recognition elements (antibodies, aptamers, or molecularly imprinted polymers) onto the transducer surface. Proper orientation and density are crucial for maintaining binding affinity [6]. 2. Sample Introduction and Incubation: Apply the prepared food sample to the biosensor chamber. Incubation time varies (typically 5-20 minutes) depending on the assay format and desired sensitivity [6]. 3. Signal Transduction and Readout: Measure the signal generated from the allergen-biorecognition element interaction. For electrochemical biosensors, this may involve measuring changes in current (amperometric), potential (potentiometric), or impedance (impedimetric). For optical biosensors, changes in color, fluorescence, or surface plasmon resonance are measured [6]. 4. Data Processing: Convert the signal into allergen concentration using pre-established calibration curves. Smartphone-based readers can facilitate this process for point-of-care applications [6] [11].
Operational Principles and Signaling Pathways: Visual Representations
Lateral Flow Device Operational Workflow
Biosensor Signal Transduction Pathways
Research Reagent Solutions and Essential Materials
Table 3: Key Research Reagents and Materials for Portable Allergen Detection Development
| Reagent/Material | Function | Examples/Specifications |
|---|---|---|
| Capture & Detection Antibodies | Specific recognition of target allergens | High-affinity monoclonal/polyclonal antibodies; characterized by SPR for kinetic parameters [11] |
| Gold Nanoparticles | Signal generation in LFDs | 20-40 nm spherical particles; functionalized with antibodies via passive adsorption or covalent binding [12] [13] |
| Nitrocellulose Membranes | Porous matrix for capillary flow & test/control lines | Various pore sizes (5-15 μm) and flow rates (120-150 s/4 cm recommended) [11] [12] |
| Aptamers | Synthetic recognition elements | Single-stranded DNA/RNA molecules with high specificity and stability; alternative to antibodies [6] [12] |
| Sample Pads | Initial sample application and filtration | Glass fiber or cellulose with pretreatment buffers to control flow and pH [12] [13] |
| Nanozymes | Signal amplification | Enzyme-mimicking nanoparticles (e.g., Pt nanoparticles) for catalytic signal enhancement [12] |
| SERS Substrates | Enhanced spectroscopic detection | Noble metal nanoparticles (Au/Ag) with roughened surfaces for plasmonic enhancement [6] [12] |
| Electrochemical Transducers | Signal conversion in biosensors | Screen-printed electrodes (carbon, gold) functionalized with recognition elements [6] |
Portable biosensors and lateral flow devices represent a paradigm shift in food allergen detection, offering rapid, cost-effective, and user-friendly alternatives to conventional laboratory methods. While these rapid methods generally provide slightly lower sensitivity than sophisticated techniques like LC-MS/MS, their performance continues to improve through innovative engineering approaches such as electrophoretic flow control, advanced nanomaterial labels, and signal amplification strategies [6] [15]. The future of portable allergen detection lies in the integration of artificial intelligence for data interpretation, multiplexing capabilities for simultaneous detection of multiple allergens, enhanced connectivity through smartphone integration, and the development of increasingly robust and sensitive platforms that can handle complex food matrices with minimal sample preparation [2] [16] [13]. For researchers and drug development professionals, selecting the appropriate method involves balancing the need for sensitivity, specificity, speed, and practicality based on the specific application requirements.
The increasing global prevalence of food allergies has positioned allergen detection as a critical frontier in food safety and public health. For researchers and drug development professionals, the landscape is divided between highly accurate, established laboratory methods and a new generation of portable devices promising rapid, on-site analysis. This guide provides an objective comparison of these technologies, focusing on their operational principles, performance metrics, and suitability for various research and development applications. Understanding the dynamics between these methods is crucial for navigating a market propelled by stringent regulatory frameworks and growing consumer awareness, which collectively drive innovation and demand for more precise and accessible testing solutions [17] [18].
The United States food allergen testing market is experiencing significant growth, projected to expand from US$ 245.63 million in 2024 to US$ 451.58 million by 2033, with a compound annual growth rate (CAGR) of 7.00%. [17] [18] This expansion is underpinned by several interconnected drivers:
- Stringent Regulatory Frameworks: Agencies like the U.S. FDA are strengthening allergen compliance norms, emphasizing cross-contact prevention, robust supply-chain management, and clear advisory labeling. These regulations compel manufacturers to adopt advanced testing to avoid recalls and legal liabilities. [17] [18]
- Rising Consumer Awareness: Food allergies now affect an estimated 33 million Americans, with one in thirteen children impacted. Heightened public awareness, fueled by advocacy and social media, pressures brands to prioritize transparency and rigorous allergen screening. [17] [18]
- Technological Innovation: Advancements are enhancing the speed, sensitivity, and accuracy of detection methods. For instance, the 2024 launch of the SENSIStrip Gluten PowerLine test exemplifies progress in reducing false negatives and improving reliability across diverse food matrices. [17]
- Shift in Food Consumption Patterns: The growing demand for processed, packaged, and "free-from" foods increases the risk of cross-contamination, making routine allergen testing an essential component of quality assurance. [18]
Comparison of Allergen Detection Methods
The choice between laboratory-based and portable methods depends on the specific requirements of the analysis, such as sensitivity, throughput, and context of use. The table below summarizes the core technologies in the researcher's toolkit.
Table 1: Core Allergen Detection Technologies for Research and Development
| Method Category | Technology | Principle of Detection | Key Performance Attributes | Best Use Cases in R&D |
|---|---|---|---|---|
| Laboratory-Based | ELISA (Enzyme-Linked Immunosorbent Assay) | Targets specific allergenic proteins using antibodies. [19] | Quantitative; high sensitivity and specificity for target proteins. [19] | Protein-specific quantitation, cleaning validation, clinical relevance studies. [19] |
| Laboratory-Based | PCR (Polymerase Chain Reaction) | Detects unique DNA sequences of the allergenic source. [19] | Qualitative; high species specificity; not directly measures protein. [19] | Identifying allergenic source in complex matrices where protein is denatured. [19] |
| Laboratory-Based | LC-MS/MS (Liquid Chromatography Tandem Mass Spectrometry) | Detects proteotypic peptides after protein digestion. [2] | Highly sensitive and specific; multiplexing capability; quantitative. [2] | High-precision protein quantification, complex matrices, method development. [19] |
| Portable | Smartphone-based iSPR (Imaging Surface Plasmon Resonance) | Measures refractive index changes from allergen-antibody binding. [20] | High sensitivity (LODs ~0.04–0.53 µg/mL for hazelnut); portable; real-time. [20] | On-site screening, rapid prototype testing, field-deployable diagnostics. [20] |
| Portable | Rapid Lateral Flow Devices (RLFD) | Immuno-chromatographic assay with antibody-coated strips. [19] | Semi-quantitative/qualitative; very fast results; ease of use. [19] | Environmental swab verification, rinse water testing, preliminary screening. [19] |
Performance Data and Experimental Comparison
Quantitative Performance Benchmarking
A 2023 study directly compared a portable smartphone-based imaging Surface Plasmon Resonance (iSPR) biosensor against a conventional benchtop SPR system for detecting hazelnut allergen in plant-based milks. [20] The results demonstrate the capabilities of emerging portable technologies.
Table 2: Analytical Performance of Smartphone iSPR vs. Benchtop SPR for Hazelnut Allergen Detection
| Plant-Based Milk Matrix | Smartphone iSPR Limit of Detection (LOD) (µg/mL) | Correlation with Benchtop SPR (R²) |
|---|---|---|
| Soy | 0.53 | 0.950 – 0.991 |
| Oat | 0.16 | 0.950 – 0.991 |
| Rice | 0.14 | 0.950 – 0.991 |
| Coconut | 0.06 | 0.950 – 0.991 |
| Almond | 0.04 | 0.950 – 0.991 |
The smartphone iSPR showed a strong correlation with the conventional system, achieving detection limits for total hazelnut protein as low as 0.04 µg/mL in almond milk, confirming its viability for sensitive, on-site analysis. [20]
Experimental Protocol: Smartphone iSPR for Allergen Detection
The following workflow details the experimental methodology cited from the 2023 Talanta study, which can serve as a prototype for validating portable biosensors. [20]
1. Biosensor Functionalization:
- The gold surface of the microfluidic SPR chip is activated.
- A specific monoclonal or polyclonal antibody against the target allergenic protein (e.g., hazelnut protein) is immobilized onto the chip surface.
2. Sample Preparation:
- Food samples (e.g., plant-based milks) are diluted (e.g., 10x) in an appropriate running buffer to reduce matrix interference.
- Samples are spiked with known concentrations of the target allergen to create a standard curve for quantification.
3. Analysis Setup:
- The functionalized chip is integrated into the 3D-printed portable device.
- The smartphone is positioned to image the SPR reaction in real-time.
4. Measurement and Data Acquisition:
- The sample solution is injected over the chip surface.
- As allergens bind to the immobilized antibodies, the local refractive index changes, causing a shift in the SPR angle.
- The smartphone camera captures these changes in real-time, generating sensorgrams.
5. Data Processing:
- A dedicated smartphone application processes the video or images to quantify the SPR shift.
- The signal is correlated to allergen concentration using the pre-established standard curve.
Diagram 1: Smartphone iSPR experimental workflow.
Critical Considerations for Method Validation
Robust experimental design must account for factors that can compromise result accuracy. Key validation protocols include: [19]
- Spike Recovery Tests: A known allergen quantity is added to a test sample. The measured result versus the known value determines recovery percentage, confirming the method's accuracy in a specific food matrix. [19]
- Cross-Reactivity Checks: The assay is tested against biologically similar substances to ensure it does not generate false positives (e.g., a walnut test should not react with pecans). [19]
- Positive Control Testing: A sample containing the allergen as a deliberate ingredient is analyzed to verify the test can detect the allergen when it is present, guarding against false negatives. This is especially critical for processed allergens, like cooked egg, where protein denaturation can hinder detection by some ELISA kits. [19]
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful experimentation in allergen detection requires a suite of specialized reagents and materials. The following table details key components for setting up immunoassays like ELISA or SPR biosensors.
Table 3: Essential Research Reagent Solutions for Allergen Detection Immunoassays
| Research Reagent / Material | Function and Importance in Experimental Protocol |
|---|---|
| Specific Antibodies (Monoclonal/Polyclonal) | Core recognition element that binds specifically to the target allergenic protein (e.g., against Ara h 1 in peanuts). Critical for assay specificity. [2] |
| Purified Allergen Standards | Highly characterized native or recombinant allergenic proteins. Essential for creating calibration curves, determining LOD/LOQ, and conducting spike recovery experiments. [21] |
| Microfluidic SPR Chip | The transducer surface in an SPR biosensor. Its functionalization with antibodies is the foundation for label-free, real-time detection of binding events. [20] |
| Blocking Buffers (e.g., BSA) | Solutions used to cover unused binding sites on the sensor or well surfaces after antibody coating. Prevents non-specific binding, which is a major source of false positives. |
| Sensor Chip Coupling Reagents | Chemical agents (e.g., EDC/NHS) that activate carboxylated dextran surfaces on SPR chips to facilitate the covalent immobilization of antibodies. [20] |
Technology Positioning and Future Research Directions
The relative positioning of these technologies within the research and development ecosystem can be visualized based on their operational complexity and analytical information depth.
Diagram 2: Technology positioning map.
Emerging research is focused on integrating artificial intelligence and non-destructive diagnostics. AI models are being developed to predict the allergenicity of new ingredients before they enter the supply chain, while technologies like Hyperspectral Imaging (HSI) and Fourier Transform Infrared (FTIR) spectroscopy, combined with machine learning, allow for non-destructive, real-time allergen detection without altering the food's integrity. [2] Furthermore, mass spectrometry is advancing with its ability to detect proteotypic peptides across complex food matrices, offering unparalleled precision for multi-allergen detection. [2] These innovations point toward a future of smarter, faster, and more integrated allergen detection systems, shaping the next generation of portable and laboratory-based tools.
Methodology in Practice: Deploying Detection Technologies from Lab to Field
In the evolving landscape of diagnostic and food safety research, the demand for high-throughput, accurate detection methods is paramount. For scientists developing portable allergen detection devices, understanding the capabilities and limitations of established laboratory methods provides a crucial performance baseline. Among these, Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) represent two foundational technologies. ELISA is renowned for its direct quantification of protein allergens, while PCR offers exceptional sensitivity in detecting allergen-encoding DNA sequences. This guide objectively compares the performance, protocols, and applications of ELISA and PCR within high-throughput screening environments, synthesizing experimental data to inform the development of next-generation portable detection systems. The quantitative data and workflows presented here serve as a reference point for evaluating the performance of emerging field-deployable technologies against established laboratory standards.
Performance Comparison: ELISA vs. PCR
The choice between ELISA and PCR is often dictated by the specific requirements of the detection scenario, including the nature of the sample, the required sensitivity, and whether qualitative or quantitative data is needed. The table below summarizes a direct comparison based on key performance parameters.
Table 1: Direct comparison of ELISA and PCR for detection applications.
| Parameter | ELISA | PCR |
|---|---|---|
| Target Molecule | Proteins (e.g., allergenic proteins) [22] | DNA (from the allergenic species) [22] |
| Throughput | High (can be automated for 96 or 384-well plates) | High, with capabilities for multiplexing (detecting multiple allergens simultaneously) [22] |
| Quantification | Direct and highly accurate quantification of proteins [22] | Primarily qualitative; can be semi-quantitative [22] |
| Sensitivity | High (e.g., detects gluten at 20 mg/kg as per Codex Alimentarius) [23] | Very High (detects trace DNA) [22] |
| Specificity | High, dependent on antibody affinity | High, dependent on primer design [23] |
| Best For | Detecting allergens in raw ingredients and less processed foods where protein structure is intact [22] | Detecting allergens in complex, highly processed foods where proteins may be denatured but DNA remains stable [22] [23] |
| Sample Processing | Protein extraction | DNA extraction [22] |
| Time to Result | Several hours | Several hours (though high-speed microfluidic PCR can reduce this to minutes) [24] |
| Cost-Effectiveness | Established, relatively cost-effective for protein detection | Higher cost for DNA-based detection, but offers high-throughput multiplexing [22] |
Supporting Experimental Data
Independent comparative studies reinforce these characteristics. A 2025 study evaluating an in-house ELISA for SARS-CoV-2 antibody detection demonstrated its substantial agreement with commercial chemiluminescent assays (Elecsys CLIA), with a positive percent agreement (PPA) of 81.7% and a negative percent agreement (NPA) of 80.1%. The overall concordance was 80.8%, with a kappa coefficient of κ=0.61 (95% CI 0.55–0.67), indicating good reliability for serosurveillance [25]. This showcases ELISA's robustness in quantitative protein detection.
Similarly, a 2020 comparison of eight commercial serological assays for SARS-CoV-2 highlighted that while a good correlation exists between different methods, discrepancies can occur, particularly in individuals with low antibody levels. This underscores the importance of understanding the limits of detection and the potential for false negatives in certain populations, a consideration that directly translates to allergen detection research [26].
Method Selection Guide
Selecting the appropriate method is critical for accurate results. The following flowchart provides a logical workflow for deciding between ELISA, PCR, or other methods based on the sample and research question.
Figure 1: A decision workflow for selecting appropriate detection methods based on sample type and requirements. LFA is included as a common portable alternative for context [22].
Experimental Protocols in Practice
To ensure reproducibility and provide a clear understanding of laboratory standards, detailed protocols for ELISA and PCR are outlined below. These methodologies form the benchmark against which portable devices are often validated.
Detailed ELISA Protocol for Protein Detection
The following protocol, adapted from serology and allergen testing research, describes an indirect ELISA for detecting specific antibodies or proteins [25] [23].
Principle: A capture antibody (or antigen) is immobilized on a solid phase. The sample containing the target protein is added. A secondary enzyme-conjugated detection antibody is then used, which produces a measurable signal upon substrate addition [22].
Materials:
- Microtiter Plates: 96-well plates for high-throughput analysis [25].
- Coating Antigen/Antibody: The purified protein (e.g., recombinant RBD of a spike protein) or capture antibody [25].
- Blocking Buffer: 4% skimmed milk in PBS with 0.1% Tween-20 to prevent non-specific binding [25].
- Washing Buffer: Phosphate-buffered saline (PBS) with 0.1% Tween-20 (PBST) [25].
- Detection Antibody: Enzyme-linked (e.g., Horseradish Peroxidase, HRP) antibody specific to the target [25] [27].
- Substrate Solution: TMB (3,3',5,5'-Tetramethylbenzidine) for HRP, which produces a blue color [27].
- Stop Solution: Acidic solution to halt the enzyme reaction [27].
- Plate Reader: Spectrophotometer for measuring absorbance at a specific wavelength (e.g., 450 nm) [22].
Step-by-Step Workflow:
Figure 2: The key steps in an indirect ELISA protocol for detecting a specific protein or antibody [25] [27].
Detailed PCR Protocol for Nucleic Acid Detection
This protocol describes a standard real-time PCR (qPCR) procedure for detecting specific DNA sequences, common in food allergen analysis [22] [23].
Principle: Target DNA sequences are amplified exponentially through thermal cycling. In qPCR, the accumulation of amplified DNA is measured in real-time using fluorescent dyes, allowing for quantification [22].
Materials:
- Thermal Cycler: Instrument for precise temperature cycling, with fluorescence detection for qPCR [24].
- PCR Reagents Mix: Contains DNA polymerase (e.g., Taq polymerase), dNTPs, and MgCl₂ in an appropriate buffer [22].
- Primers: Short, specific nucleotide sequences designed to flank the target DNA region [22].
- Probes/Dye: Fluorescent probe (e.g., TaqMan) or intercalating dye (e.g., SYBR Green) for detection in qPCR [23].
- DNA Template: Extracted and purified DNA from the sample [22].
Step-by-Step Workflow:
Figure 3: The standard workflow for a PCR assay, highlighting the cyclical nature of amplification [22] [23].
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of ELISA and PCR workflows relies on a suite of specialized reagents and instruments. The following table details key materials and their functions in these assays.
Table 2: Essential reagents and equipment for ELISA and PCR workflows.
| Category | Item | Primary Function in Assay |
|---|---|---|
| ELISA-Specific | Microtiter Plates | Solid-phase surface for immobilizing the capture molecule [25]. |
| Coating Antigen/Antibody | The initial protein that specifically captures the target from the sample [25]. | |
| Enzyme-Conjugated Antibody | Produces a measurable signal (color, light) upon reacting with its substrate [25] [27]. | |
| TMB Substrate | Chromogenic substrate for HRP enzyme, changes color in presence of the target [27]. | |
| PCR-Specific | Thermostable DNA Polymerase | Enzyme that synthesizes new DNA strands at high temperatures [22]. |
| Primers | Short DNA sequences that define the start and end of the target DNA region to be amplified [22]. | |
| dNTPs | The building blocks (nucleotides) for synthesizing new DNA strands [22]. | |
| Fluorescent Probe/Dye | Allows for real-time detection and quantification of amplified DNA in qPCR [23]. | |
| General/Core | Plate Reader (Spectrophotometer) | Measures the absorbance of the final solution in ELISA wells for quantification [22]. |
| Thermal Cycler | Precisely controls temperature cycles for DNA amplification in PCR [24]. | |
| Blocking Buffer (e.g., BSA, Milk) | Prevents non-specific binding of proteins to the plate in ELISA [25]. |
Future Directions and Integrated Approaches
The future of detection lies in leveraging the strengths of different technologies. Integrated approaches using both ELISA and PCR are increasingly used to overcome the limitations of a single method, especially in complex food matrices or for verifying allergen-free claims [22]. For instance, PCR can first screen for the presence of allergenic species DNA, with ELISA providing subsequent confirmation and quantification of the actual allergenic protein [22].
Emerging technologies are also shaping the field. Biosensors, combined with microfluidics, offer promise for on-site detection with advantages in rapidity and sensitivity [23]. Furthermore, Artificial Intelligence (AI) and machine learning are being integrated into high-throughput screening platforms to analyze massive datasets, optimize assay design, and improve pattern recognition for more accurate diagnostics [28]. The ongoing development of high-speed microfluidic PCR systems, accelerated during the COVID-19 pandemic, aims to reduce analysis time from hours to minutes, blurring the lines between laboratory and point-of-care testing [24]. These advancements provide a exciting roadmap for the evolution of portable allergen detection devices.
The growing global burden of allergic diseases, which now affect over 25% of the population in many developed nations, has intensified the need for accurate, accessible diagnostic tools [29] [30]. Traditional laboratory-based methods for allergen detection, including enzyme-linked immunosorbent assays (ELISAs) and ImmunoCAP systems, have long served as the gold standard for specific IgE detection and allergen quantification in food products [31] [32]. However, these methods require centralized laboratories, specialized equipment, and trained personnel, creating significant barriers to rapid diagnosis and point-of-care testing. In response to these limitations, portable detection platforms combining lateral flow assays (LFAs) with smartphone-based detection have emerged as transformative technologies that bridge the gap between laboratory accuracy and field-deployable testing.
The fundamental appeal of these integrated systems lies in their ability to meet WHO ASSURED criteria (Affordable, Sensitive, Specific, User-friendly, Rapid and Robust, Equipment-free, and Deliverable to end-users) while incorporating advanced digital capabilities [33]. Smartphone integration addresses one of the most significant limitations of conventional LFAs: the subjective interpretation of results. Studies demonstrate that AI algorithms integrated with smartphone readers have reduced interpretation errors by 40% in low-contrast conditions, substantially improving diagnostic reliability [33]. Furthermore, the integration of digital connectivity enables real-time data analysis, geotracking of allergen exposures, and remote consultation capabilities that enhance both clinical diagnostics and public health surveillance.
Performance Comparison: Portable vs. Laboratory Methods
The analytical and clinical performance of smartphone-integrated LFA systems must be rigorously evaluated against established laboratory methods to determine their appropriate applications and limitations. The following tables summarize key performance metrics based on current validation studies and market analyses.
Table 1: Analytical Performance Comparison of Allergen Detection Platforms
| Parameter | Smartphone-LFA Systems | Laboratory ELISA | Laboratory ImmunoCAP |
|---|---|---|---|
| Limit of Detection | 0.01 pg/mL (nanoparticle-enhanced) [33] | 0.1-1 ng/mL [31] | 0.1 kUA/L [32] |
| Assay Time | 5-30 minutes [34] [32] | 2-4 hours [31] | 3-4 hours [32] |
| Multiplexing Capability | Up to 20 allergens simultaneously (15% of new products) [34] [35] | Typically single-plex | Limited multiplexing |
| Sample Volume | 10-100 μL [14] [32] | 50-200 μL | 50-100 μL |
| Quantification | Semi-quantitative with smartphone readers [34] [33] | Fully quantitative | Fully quantitative |
| Cost per Test | $5-25 [34] | $25-100 | $50-150 |
Table 2: Clinical Performance of Representative Portable Allergy Tests
| Test System | Sensitivity | Specificity | Concordance with Lab Methods | Allergens Detected |
|---|---|---|---|---|
| FastCheckPOC 20 | 43.3% overall; 79.8% for grass pollen [32] | 92.1% overall [32] | Variable by allergen class | 20 allergens |
| Smartphone-Nano LFA | 92% (modeled estimate) [33] | 98% (modeled estimate) [33] | 92% with gold-standard assays [33] | Customizable |
| Conventional LFA | 76% (literature report) [32] | 80% (literature report) [32] | 70-85% depending on analyte [34] | Variable |
Performance data reveal that while smartphone-integrated systems approach laboratory-level sensitivity for some applications, significant variability exists between different platforms and allergen targets. The FastCheckPOC 20 device demonstrates notably higher sensitivity for inhalation allergens (79.8% for grass pollen) compared to food allergens, highlighting how protein characteristics impact test performance [32]. Meanwhile, advancements in nanoparticle-enhanced LFAs have achieved detection limits as low as 0.01 pg/mL – a 100-fold improvement over conventional LFAs – suggesting the potential for future platforms to rival laboratory sensitivity [33].
Lateral flow assays operate on capillary action principles, where a liquid sample migrates through a series of porous membranes containing biorecognition elements that generate a visible signal in the presence of target analytes [14] [33]. The two primary LFA formats used in allergen detection are sandwich assays (for larger targets with multiple epitopes) and competitive assays (for small molecules and single-epitope targets) [14]. Understanding these fundamental mechanisms is essential for selecting appropriate platforms for specific allergen targets.
Smartphone Integration and Detection Modalities
Smartphone-integrated LFA systems employ multiple detection modalities that transform simple colorimetric tests into quantitative analytical tools. The primary detection methods include:
- Colorimetric Analysis: Smartphone cameras capture test line intensity, with proprietary algorithms converting pixel density to analyte concentration. This approach has demonstrated 98% specificity in real-world surveillance applications [33].
- Fluorescent Detection: Using quantum dots or fluorescent nanoparticles, these systems provide enhanced sensitivity with detection limits up to 100-fold lower than colorimetric methods, though they require additional illumination components [33].
- Surface-Enhanced Raman Spectroscopy (SERS): Noble metal nanoparticles functionalized with recognition elements provide unique spectral fingerprints for target analytes, enabling highly specific multiplex detection [33].
The integration of artificial intelligence has been particularly transformative, with machine learning algorithms now capable of distinguishing faint test lines in suboptimal lighting conditions and automatically validating control line functionality to reduce invalid results [33]. Furthermore, cloud connectivity enables the aggregation of population-level data, creating opportunities for mapping allergen prevalence and identifying emerging sensitization patterns.
Experimental Protocols: Validation Methodologies for Portable Systems
Robust validation against established laboratory methods is essential when evaluating smartphone-LFA systems. The following protocols outline standardized approaches for performance verification.
Protocol 1: Comparative Sensitivity and Specificity Analysis
This protocol evaluates the clinical performance of a smartphone-LFA system against laboratory reference methods for specific IgE detection [32] [30].
Materials and Reagents:
- Serum samples from characterized allergic and non-allergic donors
- Smartphone-LFA system and associated reagents
- Reference laboratory equipment (e.g., ImmunoCAP, ELISA)
- Standardized allergen extracts
- Data collection forms and statistical analysis software
Procedure:
- Collect serum samples from 150-200 participants representing diverse allergen sensitivities and demographic characteristics [32] [30].
- Divide each sample for parallel testing with the smartphone-LFA system and reference laboratory method.
- Perform all tests according to manufacturer specifications, ensuring blinded analysis.
- For smartphone-LFA systems, capture both visual and algorithm-interpreted results.
- Compare results using statistical measures including sensitivity, specificity, positive predictive value, negative predictive value, and overall agreement.
- Conduct subgroup analyses based on allergen class, patient age, and symptom severity [32].
Data Interpretation: Calculate Cohen's kappa coefficient to assess agreement beyond chance. ROC analysis determines optimal cutoff values. For the FastCheckPOC 20 system, this approach revealed 43.3% overall sensitivity and 92.1% specificity compared to ALEX2 microarray testing [32].
Protocol 2: Limit of Detection and Quantification Assessment
This protocol establishes the analytical sensitivity of smartphone-LFA systems for allergen detection in food matrices [31] [36].
Materials and Reagents:
- Purified allergen standards (e.g., Ara h 1 for peanut, Bos d 5 for milk)
- Appropriate food matrices (naturally allergen-free)
- Smartphone-LFA system with calibration standards
- Sample preparation equipment (blenders, centrifuges, filters)
- Reference method (ELISA or mass spectrometry)
Procedure:
- Prepare serial dilutions of purified allergen standards in appropriate matrices covering the expected detection range.
- Spike allergen-free food samples with known allergen concentrations for recovery studies.
- Process samples through the smartphone-LFA system according to established protocols.
- Analyze each concentration in triplicate across multiple lots of test devices.
- Compare results with reference laboratory methods using matched samples.
- Determine limit of detection (LOD) as the lowest concentration detectable above background and limit of quantification (LOQ) as the lowest concentration measurable with ≤20% coefficient of variation.
Data Interpretation: Nanoparticle-enhanced LFAs have achieved LODs as low as 0.01 pg/mL for some targets, representing a 100-fold improvement over conventional LFAs [33]. However, performance varies significantly across food matrices, emphasizing the need for matrix-specific validation.
Research Reagent Solutions and Essential Materials
Successful implementation of smartphone-LFA systems requires specific reagents and materials optimized for portable detection platforms.
Table 3: Essential Research Reagents for Smartphone-Integrated Allergen Detection
| Reagent/Material | Function | Performance Considerations |
|---|---|---|
| Nitroc cellulose Membranes | Porous substrate for capillary flow and bioreceptor immobilization | Pore size (5-15 μm) affects flow rate and test line resolution [14] |
| Colloidal Gold Nanoparticles | Colorimetric labels for visual detection | 20-40 nm diameter optimizes color intensity and conjugation efficiency [33] |
| Quantum Dots | Fluorescent labels for enhanced sensitivity | Emission wavelengths should match smartphone camera filters; 5-10 nm diameter [33] |
| Mono clonal Antibodies | Target recognition elements for sandwich assays | Must recognize different epitopes than detection antibodies; high affinity (KD < 10⁻⁸ M) [14] |
| Recombinant Allergens | Positive controls and calibration standards | Should represent immunodominant epitopes; purity >95% [36] |
| Blocking Buffers | Prevent non-specific binding | Typically contain proteins (BSA, casein) and surfactants (Tween-20) [14] |
| Conjugation Buffers | Optimize antibody-nanoparticle coupling | pH 8-9 with minimal salt content preserves antibody binding capacity [14] |
Applications and Implementation Considerations
The implementation of smartphone-integrated LFA systems spans multiple domains, each with distinct requirements and validation criteria.
Clinical Diagnostic Applications
In clinical settings, these systems enable rapid specific IgE testing with 30-minute turnaround times compared to 3-4 hours for laboratory methods [32]. However, performance varies significantly by allergen class, with inhalation allergens typically showing higher sensitivity (79.8% for grass pollen) than food allergens [32]. This variability necessitates careful test selection based on clinical presentation and prevalence of specific allergens in the target population.
Recent studies implementing these systems in primary care settings demonstrate particular utility for ruling out sensitization due to high specificity (92.1% for FCP20), though low overall sensitivity (43.3%) limits their utility as standalone screening tools [32]. The integration of smartphone-based decision support algorithms has shown promise in improving appropriate test utilization and interpretation by non-specialists.
Food Safety and Environmental Monitoring
In food safety applications, smartphone-LFA systems provide rapid detection of allergenic contaminants with sensitivity approaching 0.1 ppm for major allergens like peanut and milk [31] [36]. The ability to perform on-site testing without specialized laboratory facilities enables food manufacturers to conduct frequent environmental monitoring and verify sanitation protocols.
Multiplex systems capable of simultaneously detecting multiple allergens in a single test are particularly valuable for food manufacturing facilities handling multiple allergenic ingredients. Approximately 15% of new LFA products now incorporate multiplexing capabilities, though competitive assay formats remain challenging for multiplex detection due to complex signal interpretation [34] [35].
Smartphone-integrated lateral flow assays represent a significant advancement in portable allergen detection, offering a compelling balance between performance characteristics and practical utility. While these systems have not yet achieved parity with laboratory methods for all performance parameters, their 98% specificity in real-world applications, rapid turnaround time, and connectivity features position them as valuable tools for specific use cases [33].
The future trajectory of this technology points toward enhanced sensitivity through novel nanomaterials, expanded multiplexing capabilities leveraging CRISPR-based detection, and improved connectivity through 5G and cloud-based analytics [33]. Additionally, the emergence of sustainable manufacturing approaches using biodegradable materials addresses environmental concerns while maintaining performance [35]. For researchers and clinicians, these advancements promise increasingly sophisticated portable platforms that may eventually achieve laboratory-level performance while retaining the practical advantages of point-of-care testing.
For the present, optimal implementation requires careful matching of technology capabilities to specific application requirements, with laboratory confirmation remaining essential for cases where portable systems demonstrate limited sensitivity. As validation datasets expand and technology evolves, smartphone-integrated LFA systems are poised to play an increasingly central role in decentralized allergen detection across clinical, food safety, and environmental monitoring applications.
The management of allergens is a critical public health challenge, with accurate detection serving as the cornerstone for protecting susceptible individuals. While traditional laboratory methods like enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR) have long been the gold standard, a new generation of portable detection devices is emerging. These technologies promise rapid, on-site analysis, potentially transforming practices in clinical diagnostics, food manufacturing, and food service. This guide provides an objective comparison of these portable technologies against established laboratory methods, framing the analysis within the broader thesis that while field-deployable devices offer significant advantages in speed and convenience, their performance must be carefully evaluated against application-specific requirements.
Performance Comparison of Allergen Detection Methods
The following tables summarize the key operational characteristics and performance data of various detection methods, highlighting the trade-offs between laboratory-based and portable platforms.
Table 1: Comparison of Core Allergen Detection Technologies
| Method | Format | Detection Mechanism | Time-to-Result | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Lateral Flow Device (LFD) [37] | Portable, Immunoassay | Visual colorimetric line | < 20 minutes | Ideal for quick spot-checks; minimal training required | Qualitative/Semi-quantitative (yes/no); lower sensitivity than ELISA |
| Electrochemical Sensor [38] | Portable, Biosensor | Electrochemical signal from MIP | Rapid (specific time not given) | High accuracy in complex foods; consumer-friendly potential | Emerging technology; limited commercial availability |
| ELISA [37] | Laboratory, Immunoassay | Colorimetric readout via plate reader | Several hours | High sensitivity and quantification; robust and established | Requires lab equipment and trained technicians |
| LC-MS/MS [6] | Laboratory, Mass Spectrometry | Mass-to-charge ratio of allergen peptides | Several hours | High selectivity and throughput; detects multiple allergens | Costly equipment; complex sample preparation |
Table 2: Experimental Performance Data of Portable vs. Laboratory Methods
| Technology (Study) | Sensitivity | Specificity | Comparative Laboratory Method | Notes / Context |
|---|---|---|---|---|
| FastCheckPOC (FCP20) [32] | 43.3% (Overall) | 92.1% (Overall) | ALEX2 Multiplex Assay | Utility limited by low overall sensitivity, but useful for exclusion. |
| FastCheckPOC (FCP20) [32] | 79.8% (Grass Pollen) | Not specified | ALEX2 Multiplex Assay | Performance varies significantly by allergen type. |
| Electrochemical Sensor (Allergy Amulet) [38] | Correctly identified presence/absence in 42 foods | Not specified | Commercial LFD & Immunoassay | Effective in diverse, complex food matrices. |
Clinical Point-of-Care Deployment
The deployment of point-of-care (POC) tests in primary care settings aims to streamline the diagnosis of allergic sensitization, providing rapid results that can guide clinical decision-making during a patient's visit.
Experimental Protocol: Evaluating a POC Test
A recent 2025 cross-sectional study evaluated the performance of the FastCheckPOC 20 Atopy (FCP20), a lateral flow POC test, against the laboratory multiplex assay Allergy Explorer 2 (ALEX2) [32].
- Participant Recruitment and Sample Collection: 215 participants were recruited. Venous blood was drawn from each participant, and the sample was left to clot for 15-30 minutes [32].
- Serum Separation: The blood sample was centrifuged at 1,500 × g for 10 minutes. The resulting serum was divided into two aliquots: one for immediate POC testing and one for laboratory analysis [32].
- POC Testing (FCP20): The serum aliquot for the FCP20 test was used immediately. The sample was diluted with a provided diluent, applied to the test cassette, followed by the sequential addition of washing solutions and a buffer solution. The test results were optically evaluated after 30 minutes. A result was classified as positive for levels 2-5, corresponding to CAP class 2 and above [32].
- Laboratory Testing (ALEX2): The second serum aliquot was stored at -20°C. The frozen samples were shipped on dry ice to a central laboratory, where the ALEX2 test was performed according to the manufacturer's instructions. This test provides a comprehensive sensitization profile [32].
- Data Analysis: Results from the FCP20 and ALEX2 were compared. Dichotomous data (positive/negative) were used to calculate the overall sensitivity and specificity of the FCP20, using the ALEX2 as the reference standard [32].
Technology Comparison and Workflow
The diagram below illustrates the procedural differences between conducting a POC test in a clinical setting and sending a sample to a central laboratory.
Food Manufacturing & Dining Safety Deployment
In food safety, the priority is to prevent allergen cross-contact and verify the effectiveness of cleaning protocols to protect consumers and comply with labeling regulations.
Experimental Protocol: Sensor Testing in Complex Foods
A 2021 study demonstrated a rapid electrochemical sensor using molecularly imprinted polymers (MIPs) for detecting a soy allergen tracer (genistein) in complex food products [38].
- Sample Preparation: For solid foods, 1 g of sample was homogenized into a fine powder using a mortar and pestle for 5 minutes. The powder was mixed with 10 mL of buffer solution and stirred for 15 minutes. For liquid foods, 1 g was mixed directly with 10 mL of buffer [38].
- Sensor Preparation: Template-extracted MIP electrodes were equilibrated in a clean buffer solution for 5 minutes before measurement [38].
- Sample Incubation and Measurement: The prepared electrode was incubated with 100 µL of the sample solution for 1 minute. It was then subjected to differential pulse voltammetry (DPV) measurements using a potentiostat. The critical DPV parameters were: scan rate of 50 mV/s, pulse width of 50 ms, and amplitude of 50 mV [38].
- Result Interpretation: A positive response was confirmed by the presence of an oxidation peak at approximately 0.60 V (vs Ag/AgCl reference electrode) and an imprinting factor (MIP signal/NIP signal) above 1.3 [38].
- Confirmatory Analysis: Results were confirmed using a commercial Soy Protein LFD kit, following the manufacturer's protocol, which involved extracting the sample in a specific buffer and incubating in the LFD for 11 minutes [38].
Comparative Analysis of Food Safety Tools
The following diagram outlines the decision-making process for allergen testing in a food production environment, comparing different tools.
The Scientist's Toolkit: Key Research Reagents and Materials
The development and validation of novel allergen detection methods rely on a specific set of reagents and materials. The following table details key components used in the featured experiments.
Table 3: Essential Research Reagents for Allergen Detection Development
| Reagent / Material | Function / Role in Research | Example from Literature |
|---|---|---|
| Monoclonal/Polyclonal Antibodies | Bio-recognition element in immunoassays (ELISA, LFD) that specifically binds to target allergenic protein. | Used in commercial LFDs and ELISA kits for allergen detection [37]. |
| Molecularly Imprinted Polymer (MIP) | Synthetic polymer with cavities complementary to a specific allergen molecule; serves as an antibody mimic in biosensors. | Used as the recognition element in an electrochemical sensor for soy allergen detection [38]. |
| Allergen Extracts & purified proteins | Positive controls for assay development and validation; used to determine sensitivity and specificity. | Aerosolized proteins from mites, dander, and pollen used in UV light inactivation studies [39]. |
| Screen-Printed Electrodes (SPE) | Disposable electrochemical cells used for portable biosensor development; enable miniaturization. | Carbon ItalSens IS-C SPEs were used in the development of the soy allergen electrochemical sensor [38]. |
| Sample Diluent / Extraction Buffer | Liquid medium used to extract allergens from complex samples and prepare them for analysis. | 3M extraction buffer used for LFD analysis; PBS buffer used for electrochemical sensor testing [38]. |
The landscape of allergen detection is diversifying, with portable devices now addressing needs that were once the exclusive domain of central laboratories. Lateral Flow Devices offer unparalleled speed for routine monitoring in food production, while emerging electrochemical biosensors show strong potential for accurate, consumer-facing applications. In the clinic, POC tests can aid in initial screening but are currently best suited for ruling out sensitization due to variable sensitivity. The choice between these technologies is not a matter of superiority but of context. Researchers and professionals must base their selection on a clear understanding of the required detection limits, the need for quantification, the complexity of the sample matrix, and the trade-off between the rapidity of a field result and the comprehensive data provided by a laboratory test. Future advancements will likely focus on improving the sensitivity and multiplexing capabilities of portable devices to narrow this performance gap further.
Food allergies represent a significant and growing global health concern, affecting an estimated 2-5% of adults and 6-8% of children worldwide [38]. For allergic individuals, strict avoidance of trigger foods remains the only effective prevention strategy, as no definitive treatments currently exist [6] [40]. This reality places tremendous importance on reliable detection methodologies that can identify allergenic contaminants throughout the food supply chain. The emergence of sophisticated non-destructive technologies, particularly those integrating artificial intelligence (AI) and hyperspectral imaging (HSI), represents a paradigm shift from conventional laboratory-bound methods toward rapid, on-site, and intelligent detection platforms [40] [41].
The regulatory landscape has identified key allergens requiring mandatory declaration, with the "Big Nine" – wheat (gluten), peanuts, egg, shellfish, milk, tree nuts, fish, sesame, and soybeans – responsible for the majority of severe reactions [40]. Traditional detection methods, including enzyme-linked immunosorbent assays (ELISA), polymerase chain reaction (PCR), and liquid chromatography-tandem mass spectrometry (LC-MS/MS), have provided the analytical foundation for allergen detection for decades [6] [42]. However, these methods present significant limitations for modern food industry needs, including lengthy analysis times, destructive sample preparation, requirements for specialized laboratory facilities and trained technicians, and limited suitability for real-time monitoring [6] [40] [38].
This comprehensive analysis compares established laboratory methodologies with emerging portable and non-destructive technologies, focusing on their operational parameters, performance characteristics, and practical applicability within research and industrial contexts.
Conventional Allergen Detection Methods: Established but Limited
Traditional allergen detection techniques can be broadly categorized into immunoassays, DNA-based methods, and mass spectrometry, each with distinct mechanisms and applications.
Performance Analysis of Conventional Methods
Table 1: Comparison of Conventional Laboratory-Based Allergen Detection Methods
| Method Type | Detection Principle | Key Advantages | Significant Limitations | Sensitivity Range | Analysis Time |
|---|---|---|---|---|---|
| ELISA/Immunoassays [6] [38] | Antibody-antigen binding | High specificity, commercially available kits | Antibody instability, cross-reactivity issues, protein denaturation effects | ppm to ppb levels | 1-4 hours |
| PCR (DNA-Based) [6] [40] | Amplification of species-specific DNA sequences | High sensitivity, detects processed foods | Indirect (detects DNA, not protein), false negatives from processing | ~0.1% celery (1000 mg/kg) [42] | 2-6 hours |
| LC-MS/MS [6] [43] | Separation and mass analysis of proteins/peptides | High selectivity and accuracy, multiplexing capability | Costly equipment, complex sample prep, requires expertise | High ppm to ppb | Several hours |
| Western Blot [6] | Protein separation and antibody detection | Confirms protein identity and size | Semi-quantitative, low throughput, technical complexity | Variable | 6-24 hours |
Experimental Protocols for Traditional Methods
Typical ELISA Protocol for Allergen Detection [1]:
- Sample Extraction: 1g of solid food is homogenized and extracted with appropriate buffer (e.g., PBS) for 15 minutes
- Coating: Microplate wells are coated with capture antibody specific to target allergen
- Blocking: Non-specific binding sites are blocked with protein buffers (e.g., BSA)
- Incubation: Sample extract is added and allergen binds to capture antibody
- Detection: Enzyme-conjugated detection antibody is added, followed by substrate addition
- Measurement: Color development is measured spectrophotometrically
- Quantification: Concentration determined against standard curve
Typical PCR Protocol for Allergen Detection [6] [42]:
- DNA Extraction: Isolation and purification of DNA from food matrix
- Primer Design: Selection of species-specific primers (e.g., mannitol dehydrogenase for celery)
- Amplification: Thermal cycling with fluorescence detection (real-time PCR)
- Analysis: Cycle threshold (Ct) values compared to standards for quantification
While these conventional methods provide the reference standards for allergen detection with proven sensitivity and specificity, their limitations in speed, portability, and operational complexity have driven the development of emerging technologies [6] [38].
Emerging Non-Destructive Technologies and Portable Platforms
The integration of biosensing technologies with portable analytical devices represents the most promising advancement for rapid, on-site allergen detection, moving analysis from centralized laboratories to point-of-need settings [6] [40].
Hyperspectral Imaging and AI-Enhanced Platforms
Hyperspectral imaging captures spatial and spectral information across hundreds of contiguous bands, enabling the detection of subtle chemical signatures associated with allergenic proteins [44] [41]. When combined with AI algorithms, these systems can identify and quantify allergens without destructive sample preparation.
Key Technology Providers:
- Specim: Cameras capturing broad spectrum (visible to thermal) with real-time data analysis software [44]
- Headwall Photonics: Hyperspectral systems with precision optical components for industrial inspection [44]
- Resonon: Pika cameras covering UV to SWIR ranges for airborne and benchtop configurations [44]
- FlyPix AI: Platform processing satellite, aerial, and drone imagery with AI detection algorithms [44]
Portable Biosensing Platforms
Table 2: Emerging Portable and Non-Destructive Allergen Detection Platforms
| Platform/Technology | Detection Principle | Key Features | Reported Performance | Analysis Time | User Level |
|---|---|---|---|---|---|
| iTube Smartphone Platform [45] | Colorimetric assay with smartphone analysis | 40g attachment, automated image processing, spatio-temporal mapping | Quantification 1-25 ppm peanut, R=0.99 calibration | ~20 min total (inc. prep) | Consumer/Research |
| Electrochemical Sensor (MIP-based) [38] | Molecularly imprinted polymers with electrochemical detection | Tested in 42 complex food products, 300+ ingredients | Correct presence/absence in all samples vs LFD confirmation | Minutes (post extraction) | Professional |
| Lateral Flow Devices (LFDs) [6] [38] | Immuno-chromatographic strip | Simple operation, minimal equipment | Lower accuracy vs lab methods, viscosity-dependent | 10-15 minutes | Consumer/Industry |
| AI-Enabled HSI/FTIR [41] [46] | Spectral signature analysis with machine learning | Non-destructive, real-time capability, multi-allergen potential | Research phase, promising quantification accuracy | Near real-time | Industry/Research |
Experimental Protocols for Emerging Methods
iTube Smartphone Detection Protocol [45]:
- Sample Preparation: 5g food sample ground and mixed with hot water (50-60°C) and extraction solvent
- Assay Activation: 3 drops sample solution added to test tube with control
- Incubation: 10-minute incubation period
- Chemical Development: Sequential addition of conjugate, substrate, and stop solutions with washing steps (~10 minutes)
- Measurement: Test tubes inserted into smartphone attachment (650nm LED illumination)
- Analysis: Custom application captures transmission images and calculates allergen concentration based on relative absorbance: A = log₁₀(Icontrol/Itest)
Electrochemical Sensor (MIP-based) Protocol [38]:
- Sensor Preparation: Molecularly imprinted polymer electrodes fabricated using electrophysmerization
- Template Extraction: Removal of original allergen tracer molecules from polymer matrix
- Sample Preparation: 1g food homogenized with 10mL buffer solution (15 min extraction)
- Measurement: Template-extracted MIP electrodes incubated with 100μL sample solution (1 min)
- Detection: Differential pulse voltammetry measurements performed
- Interpretation: Positive response indicated by oxidation peak at 0.60V vs Ag/AgCl and imprinting factor >1.3
Comparative Performance Analysis: Experimental Data
Rigorous evaluation of emerging technologies against established methods provides critical performance insights for researchers and industry professionals.
Table 3: Comparative Experimental Performance Data Across Methodologies
| Methodology | Target Allergen | Food Matrix | Sensitivity | Accuracy vs Reference | Key Limitations Observed |
|---|---|---|---|---|---|
| MIP Electrochemical Sensor [38] | Soy (genistein) | 42 complex foods (meats, sauces, confectionery) | Clinically relevant levels | 100% correct presence/absence vs LFD | Requires sample extraction step |
| iTube Platform [45] | Peanut | Commercial cookies | 1-25 ppm range | Accurate quantification, R=0.99 | ~20 min sample preparation needed |
| Conventional ELISA [6] [38] | Multiple | Various matrices | ppm to ppb | Reference standard | Protein denaturation effects, cross-reactivity |
| Lateral Flow Devices [38] | Soy | Complex foods | Variable | Lower than MIP sensors | Accuracy affected by food viscosity |
| Hyperspectral Imaging + AI [41] [46] | Research phase | Tomato quality (model) | High for attributes | Promising for non-destructive use | Limited allergen-specific validation |
Technology Integration Pathways
The most significant advancement in allergen detection emerges from integrating multiple technologies into unified systems. The combination of biosensors with portable devices (e.g., LFAs, microfluidic chips) creates powerful platforms for reliable on-site detection [6]. Furthermore, the coupling of these systems with smartphones enables automated, intelligent detection with connectivity features for result sharing and spatio-temporal mapping [45] [1].
Diagram: Integrated Allergen Detection Platform Architecture. Emerging systems combine multiple technologies to achieve portable, sensitive detection with connectivity features.
Research Reagent Solutions and Essential Materials
Successful implementation of allergen detection methodologies requires specific reagents and materials tailored to each technological approach.
Table 4: Essential Research Reagents and Materials for Allergen Detection
| Reagent/Material | Function/Purpose | Example Applications | Technology Category |
|---|---|---|---|
| Molecularly Imprinted Polymers (MIPs) [38] | Synthetic recognition elements for specific allergens | Electrochemical sensor development | Biosensors |
| Monoclonal/Polyclonal Antibodies [6] [1] | Specific binding to allergenic proteins | ELISA, Lateral Flow Immunoassays | Immunoassays |
| Genistein (Soy Tracer) [38] | Marker molecule for soy allergen detection | MIP sensor development | Biosensors |
| Ortho-Phenylenediamine (o-PD) [38] | Electrophysmerization monomer for MIP formation | Sensor fabrication | Electrochemical |
| Screen-Printed Electrodes (SPEs) [38] | Disposable electrochemical platforms | Portable sensor systems | Electrochemical |
| LED Illumination (650nm) [45] | Matched wavelength for colorimetric assays | Smartphone-based detection | Optical |
| Hyperspectral Cameras (UV-SWIR) [44] [46] | Capture spectral signatures across wavelengths | Non-destructive material analysis | HSI |
| Food Extraction Buffers [43] | Solubilize allergenic proteins from food matrix | Sample preparation for multiple methods | Sample Preparation |
Future Perspectives and Research Directions
Despite significant advances, several challenges remain in the widespread implementation of emerging allergen detection technologies. Current biosensing strategies often remain at the theoretical stage, with limited real-world validation across diverse food matrices [6]. Sample preparation complexity continues to present barriers to truly rapid detection, and the high cost of implementation for some advanced systems (e.g., HSI) limits accessibility [6] [40].
Future research priorities should focus on:
- Development of simplified sample pretreatment procedures to minimize preparation time [6]
- Multi-allergen detection platforms capable of simultaneous detection of multiple allergens from a single sample [6] [1]
- Miniaturization and cost reduction of HSI systems and associated AI analytics [40] [46]
- Comprehensive validation studies across diverse food matrices and processing conditions [6] [43]
- Integration with food processing systems for real-time monitoring during manufacturing [41]
The integration of AI with sensor technologies represents perhaps the most promising direction, enabling pattern recognition capabilities for minute levels of biological and chemical constituents in foods through interactions with light and sensors [40] [41]. As these technologies evolve, they promise to increase the accessibility of testing tools across the food supply chain, driving greater assurance and safety for allergic consumers [41].
The integration of AI, hyperspectral imaging, and non-destructive diagnostics represents a transformative advancement in food allergen detection methodology. While conventional laboratory techniques like ELISA, PCR, and LC-MS/MS provide essential reference methods with high sensitivity and specificity, their limitations in speed, portability, and operational complexity restrict their utility for rapid, on-site detection scenarios.
Emerging portable biosensing platforms, smartphone-based analyzers, and AI-enhanced hyperspectral imaging systems demonstrate increasingly competitive performance characteristics while offering distinct advantages in operational flexibility, analysis time, and user accessibility. The experimental data from platforms such as the iTube smartphone system and MIP-based electrochemical sensors confirm their viability for accurate allergen detection in complex food matrices, with performance metrics approaching those of established laboratory methods.
For researchers and drug development professionals, the evolving landscape of allergen detection technologies offers multiple pathways for application-specific solutions. Traditional methods remain essential for reference measurements and validation studies, while emerging non-destructive platforms provide unprecedented capabilities for real-time monitoring, field studies, and point-of-need testing. The continued integration of AI algorithms with advanced sensor technologies promises to further bridge the performance gap between laboratory and portable methods, ultimately enhancing food safety and quality of life for allergic individuals worldwide.
Navigating Technical Hurdles: Optimization Strategies for Accurate Detection
Matrix interference in complex and processed food samples presents a significant challenge for the accurate detection of food allergens, impacting the reliability of both portable devices and laboratory methods. The immune response to allergenic proteins can be severe, and with the prevalence of food allergies rising, the demand for robust detection techniques has never been greater [23] [40]. Food processing can denature protein structures, mask epitopes, and introduce compounds that interfere with analytical signals, complicating detection [23]. This guide objectively compares the performance of various allergen detection platforms, focusing on their respective strategies to overcome matrix interference, and is situated within a broader thesis comparing portable and laboratory-based allergen detection systems.
Comparative Performance of Allergen Detection Methods
The following table summarizes the core characteristics, advantages, and limitations of major allergen detection method categories when applied to complex food matrices.
Table 1: Comparison of Allergen Detection Methods for Complex and Processed Foods
| Method Category | Key Principle | Suitability for Processed Foods | Key Limitations | Reported Sensitivity |
|---|---|---|---|---|
| Immunoassays (ELISA) | Antibody-antigen binding to detect allergenic proteins [23]. | Moderate; processing can denature protein epitopes, leading to false negatives [23]. | Susceptible to protein denaturation from heat/processing; antibody cross-reactivity [23]. | Adopted by Codex for gluten with a threshold of 20 mg/kg [23]. |
| PCR (DNA-based) | Amplification of species-specific DNA sequences [23]. | High; DNA is more stable than proteins under harsh processing conditions [23]. | Indirect; does not detect the allergenic protein itself. Correlation between DNA and protein can vary [23]. | Official method in Germany; Japan uses it with a 10 μg/g threshold [23]. |
| Mass Spectrometry (MS) | Detection and quantification of target allergen peptides [23]. | High; can detect and quantify specific allergen markers even in processed matrices [23]. | Requires extensive sample preparation; high equipment cost and operational expertise [23]. | Enables multi-allergen detection; used for precise quantification (e.g., in surimi) [23]. |
| Biosensors | Biological recognition element (antibody, aptamer) coupled to a transducer [23]. | Varies; emerging designs aim for direct analysis of complex samples [23]. | Sensitivity can be affected by non-specific binding in complex food samples [23]. | High sensitivity demonstrated for tropomyosin, β-lactoglobulin [23]. |
Experimental Protocols for Key Methods
Protocol: Enzyme-Linked Immunosorbent Assay (ELISA)
ELISA is a widely used laboratory immunoassay for protein-based allergen detection. The following protocol is adapted from methodologies cited in the literature [23].
- Coating: Coat the wells of a microtiter plate with a capture antibody specific to the target allergen (e.g., anti-Ara h 1 for peanut) in a suitable coating buffer (e.g., carbonate-bicarbonate). Incubate overnight at 4°C.
- Blocking: Empty the wells and block any remaining protein-binding sites with a blocking agent (e.g., 1-5% Bovine Serum Albumin or non-fat dry milk in PBS-Tween) to prevent non-specific binding. Incubate for 1-2 hours at room temperature.
- Sample Addition: Add the processed food sample extract (ground and dissolved in appropriate extraction buffer) and a series of allergen standards of known concentration to the wells. Incubate to allow the target allergen to bind to the capture antibody.
- Detection Antibody Addition: Add a detection antibody, which is also specific to the target allergen but conjugated to an enzyme such as Horseradish Peroxidase (HRP). Incubate.
- Substrate Addition: After washing, add a chromogenic enzyme substrate (e.g., TMB). The enzyme catalyzes a reaction that produces a colored product.
- Signal Measurement: Stop the reaction with a stop solution (e.g., sulfuric acid) and measure the absorbance of the solution in each well with a plate reader. The absorbance is proportional to the allergen concentration in the sample.
Protocol: Real-Time Polymerase Chain Reaction (qPCR)
qPCR is an official nucleic acid-based method used for detecting allergen DNA, particularly useful in highly processed foods where proteins may be denatured [23].
- DNA Extraction: Isolate total DNA from the processed food sample using a commercial kit designed for complex matrices. This may involve steps for cell lysis, RNAse treatment, and DNA purification.
- Primer/Probe Design: Design and synthesize sequence-specific primers and a fluorescently labeled probe (e.g., TaqMan) for a target gene unique to the allergenic food source (e.g., a specific parvalbumin gene for fish).
- Reaction Setup: Prepare a qPCR reaction mix containing the extracted DNA template, primers, probe, and a master mix containing DNA polymerase, dNTPs, and buffer.
- Amplification and Detection: Run the reaction in a real-time PCR instrument. The instrument monitors the fluorescence signal during each amplification cycle. The cycle threshold (Ct) at which the fluorescence exceeds the background is recorded.
- Quantification: The Ct value is compared to a standard curve generated from samples with known amounts of the target DNA to determine the concentration in the unknown sample.
Protocol: Lateral Flow Immunoassay (LFIA)
LFIA is a rapid format used in many portable devices. Research into smartphone-linked LFIAs aims to enhance their quantitative capability for consumer use [1].
- Sample Application: Apply the liquid extract from the processed food sample to the sample pad of the lateral flow strip.
- Capillary Flow and Conjugation: The sample migrates via capillary action to the conjugate pad, where it solubilizes labeled detection antibodies (e.g., gold nanoparticles or latex beads) specific to the target allergen.
- Test and Control Lines: The complex flows onto the nitrocellulose membrane. If the target allergen is present, it binds to the detection antibodies and is captured at the test line by a second immobilized antibody, generating a visible signal. The control line captures excess labeled antibodies to validate the test.
- Signal Readout: The result is visually interpreted (qualitative) or measured with a dedicated strip reader or smartphone-based optical detector (semi-quantitative/quantitative) [1].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Allergen Detection Research
| Item | Function in Research | Example Application |
|---|---|---|
| Monoclonal/Polyclonal Antibodies | Serve as highly specific recognition elements for target allergenic proteins (e.g., Ara h 1, tropomyosin) in immunoassays and biosensors [23]. | Coating and detection antibodies in a sandwich ELISA protocol [23]. |
| DNA Primers and Probes | Designed to amplify and detect species-specific DNA sequences, providing an indirect marker for the presence of an allergenic food source [23]. | Target-specific primers for real-time PCR detection of fish (parvalbumin gene) or buckwheat [23]. |
| Aptamers | Single-stranded DNA or RNA oligonucleotides that bind to specific targets (proteins); used as synthetic, stable alternatives to antibodies in biosensors [23]. | Recognition element in an electrochemical or graphene-based biosensor for β-lactoglobulin [23]. |
| Stable Isotope-Labeled Peptides | Act as internal standards in mass spectrometry-based methods, enabling precise and accurate quantification of target allergen peptides by correcting for matrix-induced ion suppression [23]. | Quantification of multi-allergens in surimi products by LC-MS/MS [23]. |
| Gold Nanoparticles / Quantum Dots | Used as signal labels in LFIA and biosensors due to their strong optical properties, enhancing detection sensitivity [23] [1]. | Signal generation in a quantum-dot-based lateral flow immunoassay for shrimp tropomyosin [23]. |
Workflow and Signaling Pathways
Experimental Workflow for Method Selection and Validation
The following diagram illustrates a logical decision workflow for selecting and validating an allergen detection method based on the food matrix and analytical requirements.
Signaling Pathway in Immunochemical Allergen Detection
This diagram outlines the core signaling principle of immunochemical methods like ELISA and LFIA, which is the specific molecular recognition between an antibody and its target epitope on an allergenic protein.
The detection of trace-level food allergens represents a significant public health challenge, with food allergies affecting approximately 5-10% of the population in developed nations and prevalence rates rising globally [43]. For sensitized individuals, exposure to even microgram quantities of allergenic proteins can trigger reactions ranging from mild symptoms to life-threatening anaphylaxis [1] [47]. Consequently, the food industry, regulatory bodies, and researchers face mounting pressure to develop and implement detection techniques capable of identifying allergenic contaminants at levels far below established reaction thresholds. The minimum dose to induce allergic reactions (ED01) for major allergens has been documented as low as 0.03 mg for walnut, 0.05 mg for cashew, and 0.20 mg for peanut, egg, and milk [47], establishing exceptionally demanding sensitivity requirements for analytical methods.
This comparative guide examines the evolving landscape of allergen detection technologies, with particular focus on the performance relationship between portable devices and laboratory-based methods. As the field advances, techniques such as mass spectrometry, biosensors, and multiplex immunoassays are pushing detection limits to unprecedented levels, with some achieving sensitivity as low as 0.01 ng/mL for specific allergenic proteins [2]. This analysis provides researchers, scientists, and drug development professionals with experimental data and performance comparisons essential for selecting appropriate methodologies for specific applications, from industrial quality control to clinical diagnostics.
Laboratory-Based Methods: Gold Standards and Emerging Innovations
Traditional laboratory-based methods continue to serve as reference standards for allergen detection due to their proven reliability, sensitivity, and reproducibility. These techniques form the foundation upon which newer technologies are validated and benchmarked.
Established Laboratory Techniques
Immunoassays and DNA-Based Methods Enzyme-linked immunosorbent assay (ELISA) remains one of the most widely used laboratory methods for allergen detection, providing quantitative results with simple test formats and limits of detection typically in the low parts-per-million (ppm) range [48]. For gluten detection specifically, the R5 ELISA kit has received AOAC Performance Tested Method status with a limit of detection of 3 ppm (mg/kg) [48]. Polymerase chain reaction (PCR) methods offer an alternative approach targeting allergen-encoding DNA sequences, demonstrating prominent specificity and high sensitivity, particularly for allergens difficult to detect by immunoassays (e.g., celery) and for avoiding cross-reactivity with related species [48].
Mass Spectrometry Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has emerged as a powerful tool for allergen detection, offering high selectivity, throughput, and accuracy [6]. This proteomics-based approach detects proteotypic peptides across complex food matrices, providing new levels of precision compared to antibody-based methods [2]. A key advantage of mass spectrometry is its ability to simultaneously quantify specific proteins responsible for allergic responses, such as peanut (Ara h 3, Ara h 6), milk (Bos d 5), egg (Gal d 1, Gal d 2), and shellfish (Tropomyosin) [2].
Advanced Laboratory Innovations
Multiplex Microarray Technology The multiplex allergen microarray-based immunoassay represents a significant innovation in laboratory testing, enabling identification of numerous allergenic proteins with a single test [43]. This technology utilizes IgE-binding inhibition assays on multiplex allergen biochips (e.g., ISAC, FABER tests), providing a comprehensive allergen profile that captures both known and previously unidentified IgE-reactive proteins [43]. Unlike conventional methods that target preselected individual allergens, this approach offers unprecedented capability for detecting unexpected contaminations and evaluating the effectiveness of food processing procedures in reducing allergenicity.
AI-Enhanced Non-Destructive Diagnostics Emerging technologies combining hyperspectral imaging (HSI), Fourier Transform Infrared (FTIR) spectroscopy, and computer vision with machine learning are enabling non-destructive, real-time allergen detection without altering food integrity [2]. These methods allow for continuous monitoring throughout production processes and can predict allergenicity of new ingredients before they enter the supply chain, representing a paradigm shift from detection to prevention [2].
Table 1: Performance Comparison of Laboratory-Based Allergen Detection Methods
| Method | Detection Mechanism | Limit of Detection | Key Advantages | Key Limitations |
|---|---|---|---|---|
| ELISA | Antibody-antigen interaction | 3 ppm (gluten R5 ELISA) [48] | Quantitative, simple format, automated platforms available | Limited multiplexing capability, relatively poor sensitivity compared to newer methods |
| PCR | DNA amplification | Varies by allergen | High specificity, detects allergens difficult to identify by immunoassays | Indirect method (detects DNA, not protein), some processed foods contain little DNA |
| LC-MS/MS | Mass-to-charge ratio of peptides | 0.01 ng/mL for some allergens [2] | High specificity, can simultaneously quantify multiple specific proteins | Expensive equipment, requires skilled technicians, complex sample preparation |
| Multiplex Microarray | IgE-binding inhibition on biochip | Comprehensive profiling capability | Identifies multiple unknown allergens in single test, reveals complete allergen profile | Limited commercial availability, specialized interpretation required |
| AI-Enhanced Spectroscopy | Spectral analysis with machine learning | Research phase | Non-destructive, real-time monitoring, predictive capability | Early development stage, requires extensive training data |
Portable Detection Devices: Field-Deployable Solutions
The growing demand for rapid, on-site allergen detection has driven development of portable devices that offer immediate results outside laboratory environments. These systems prioritize speed, ease of use, and portability while maintaining sufficient sensitivity for practical applications.
Biosensor-Based Platforms
Technology Overview Biosensors represent a promising technological approach for portable allergen detection, utilizing transducers to transfer interactions between bio-recognition elements and targets [6]. Recent advances have yielded platforms employing colorimetric, fluorescent, electrochemical, surface enhanced Raman spectroscopy (SERS), and surface plasmon resonance (SPR) detection mechanisms [6]. The integration of these biosensing technologies with portable platforms like lateral flow assays (LFAs), microfluidic chips, and paper-based microfluidic devices has created powerful field-deployable tools for allergen monitoring.
Commercial Portable Systems The Allergy Amulet positions itself as a consumer-focused solution, claiming capability to "detect allergenic ingredients at levels lower than those known to trigger an allergic reaction in the most sensitive food-allergic individuals" with results in approximately one minute [49]. Similarly, Allergen Alert has developed a portable instrument that identifies allergens and gluten in food within minutes using smartphone application connectivity [50]. For industrial applications, companies like Hygiena and Safe Food Corporation offer portable, easy-to-use kits designed for rapid decision-making in production environments [51].
Lateral Flow and Microfluidic Devices
Lateral Flow Immunoassays Lateral flow tests (e.g., SENSIStrip) provide semi-quantitative results with high sensitivity and low limits of detection without requiring highly qualified users [48]. Recent innovations include the introduction of a "hook line" to exclude false negative interpretations of highly contaminated samples, addressing a historical limitation of LFA technology [48]. When paired with portable readers like the RapidScan ST5-W, these assays can provide quantitative evaluation in both laboratory and field settings [48].
Microfluidic Integration Microfluidic chips and paper-based microfluidic devices enable miniaturization, automation, and integration of complex assay procedures into portable formats [6]. These systems facilitate sample preparation, recognition, transduction, and signal processing within compact, self-contained platforms suitable for use in resource-limited environments [6]. The combination of microfluidics with smartphone-based detection creates particularly powerful field-deployable analytical capabilities.
Table 2: Comparison of Portable Allergen Detection Platforms
| Platform Type | Example Products | Time to Result | Sensitivity Claims | Target Users |
|---|---|---|---|---|
| Biosensor-Based | Allergen Alert, Research prototypes | Few minutes | Not specified in search results | Consumers, restaurant owners, food safety professionals |
| Lateral Flow Assays | SENSIStrip, various commercial kits | <10-20 minutes | High sensitivity, low LOD (specific values not provided) [48] | Food manufacturers, quality control staff |
| Smartphone-Integrated | Allergy Amulet, research systems | ~1 minute [49] | "Lower than those known to trigger reactions" [49] | Consumers, allergic individuals |
| Microfluidic Devices | Research prototypes | Varies by design | Research phase, promising for trace detection | Future applications: field testing, point-of-care |
Experimental Comparison: Methodologies and Performance Data
Experimental Protocols for Sensitivity Assessment
Sample Preparation Methodology Effective allergen detection requires careful sample preparation to extract allergenic proteins from complex food matrices. Protocols vary significantly based on the food type and detection method, with key considerations including:
- Extraction buffer selection: High-salt or high-pH buffers generally recover higher protein concentrations compared to low-pH buffers, as demonstrated in studies showing more IgE-reactive bands on immunoblotting [43].
- Matrix effect management: Protein interactions with matrix components can modify immunological behavior by changing conformation and epitope exposure [43]. For instance, parvalbumins purified from fish show thermostability alone but demonstrate thermal instability in natural matrices due to physical and chemical interactions [43].
- Processing impact assessment: Thermal and non-thermal processing methods can induce protein modifications (denaturation, aggregation, fragmentation, Maillard reactions) that significantly affect extractability and immunodetection [43].
Validation Procedures Method validation requires comparison against established reference materials and protocols. For immunoassays, this includes:
- Calibration with certified reference materials covering expected concentration ranges
- Cross-reactivity assessment with related and unrelated food proteins
- Robustness testing under varying environmental conditions (temperature, humidity)
- Parallel analysis with reference methods (e.g., ELISA validation against mass spectrometry)
Comparative Performance Data
Sensitivity and Detection Limits The most advanced detection technologies achieve exceptional sensitivity levels. Mass spectrometry platforms can detect specific allergenic proteins at concentrations as low as 0.01 ng/mL [2]. Multiplexed immunoassays offer similar sensitivity while maintaining the ability to simultaneously quantify multiple specific allergens in a single analysis [2]. While portable devices generally have higher detection limits than laboratory methods, leading commercial products claim sensitivity sufficient to detect allergens below clinically relevant thresholds, with the Allergy Amulet reporting capability to detect levels "lower than those known to trigger an allergic reaction in the most sensitive food-allergic individuals" [49].
Multiplexing Capability A significant advantage of emerging technologies is their capacity for multiplexed analysis. DNA-based methods typically identify only one or a few allergens per test [43], while biosensors generally offer singleplex detection unless specifically designed for multiplexing [43]. In contrast, multiplex allergen microarray-based immunoassays enable identification of numerous allergenic proteins, including previously unknown ones, in a single test [43]. This comprehensive profiling capability represents a substantial advancement for evaluating complex food products with potential multiple allergen contaminations.
Visualization of the relationship between detection technologies, showing the spectrum from portable field devices to advanced laboratory methods with increasing sensitivity and multiplexing capability.
Technical Challenges and Future Directions
Current Limitations
Sample Preparation Complexity Effective detection of trace allergens remains challenging due to complexities in sample preparation. The extraction efficiency of allergenic proteins varies significantly based on buffer composition, with high-salt buffers demonstrating superior recovery of some cell wall-bound proteins [43]. Furthermore, matrix effects can substantially impact results, as components in food extracts may modify protein conformation and epitope exposure, potentially hindering allergen recovery or masking epitopes [43]. These factors complicate both method development and comparison of results across different platforms.
Technology-Specific Constraints Each detection methodology faces distinct limitations:
- Portable devices must balance sensitivity with practical constraints of size, cost, and operational simplicity
- DNA-based methods indirectly detect allergens and cannot differentiate between active proteins and non-allergenic genetic material [43]
- Mass spectrometry requires expensive equipment and specialized technical expertise [6]
- Biosensors often remain at theoretical development stages rather than practical implementation [6]
Emerging Innovations
Next-Generation Biosensing Future developments in allergen detection focus on enhancing sensitivity, specificity, and practicality. Key research directions include:
- Dual-mode biosensing combining multiple detection mechanisms to improve reliability
- Advanced material integration incorporating nanotechnology and novel transducers to lower detection limits
- Miniaturized automation enabling complex assay procedures in field-deployable formats
- AI-powered analysis facilitating real-time interpretation and trend identification [51]
Digital Integration and Automation The integration of detection platforms with digital technologies represents a significant advancement trend. Cloud-based platforms that integrate allergen data with other quality metrics (e.g., ATP readings, microbial counts) provide visualized heat maps and trend analysis across production facilities [2]. These systems support predictive risk management and centralized dashboards for compliance auditing, ultimately reducing costs associated with rework and recalls [2]. For portable devices, smartphone connectivity enables result tracking, data analysis, and sharing capabilities that enhance usability and documentation [1] [49] [50].
Table 3: Essential Research Reagent Solutions for Allergen Detection Studies
| Reagent Category | Specific Examples | Function in Detection | Application Notes |
|---|---|---|---|
| Extraction Buffers | High-salt buffers, high-pH buffers | Protein solubilization from food matrices | Selection critically impacts extraction efficiency; high-salt buffers improve recovery of cell wall-bound proteins [43] |
| Reference Allergens | Purified native proteins (Ara h 1-9, Bos d 5, Gal d 1-2) | Assay calibration and validation | Essential for quantitative method development; provides benchmark for processed allergen detection |
| Detection Antibodies | Monoclonal (e.g., R5 antibody for gluten), polyclonal | Target recognition in immunoassays | Specificity determines cross-reactivity profile; monoclonal antibodies offer better reproducibility |
| Molecular Probes | Allergen-specific primers, aptamers | Nucleic acid or protein recognition | Aptamers offer potential alternative to antibodies with enhanced stability; primers must target appropriate marker sequences |
| Signal Amplification Systems | Enzyme-substrate pairs, nanoparticles, fluorescent tags | Signal generation and enhancement | Critical for achieving low detection limits; nanoparticle labels can significantly enhance sensitivity |
The landscape of trace-level allergen detection continues to evolve, with both laboratory-based and portable technologies achieving progressively lower detection limits. Mass spectrometry and multiplex immunoassays currently provide the highest sensitivity levels, reaching 0.01 ng/mL for specific allergenic proteins [2], while portable biosensors and lateral flow devices offer increasingly capable alternatives for rapid, on-site testing. The choice between these approaches depends fundamentally on the specific application requirements, balancing needs for sensitivity, multiplexing capability, speed, and operational simplicity.
Future advancements will likely focus on closing the performance gap between portable and laboratory methods while enhancing the connectivity, automation, and intelligence of detection platforms. Technologies incorporating artificial intelligence, cloud-based data management, and improved multiplexing capabilities will enable more comprehensive allergen management strategies moving from simple detection toward predictive prevention. For researchers and professionals, understanding the comparative strengths and limitations of each technological approach remains essential for selecting appropriate methodologies, interpreting results accurately, and developing effective allergen control strategies that protect susceptible consumers while supporting industry innovation.
Comprehensive workflow for allergen detection methodology, highlighting decision points between laboratory and portable approaches based on research objectives and practical constraints.
The increasing global prevalence of food allergies, affecting up to 10% of consumers worldwide, has intensified the need for reliable allergen detection methods [52]. While laboratory-based analytics remain the gold standard for accuracy, the growing demand for immediate, on-site results has driven innovation in portable detection devices. This shift creates a critical challenge: harmonizing the performance standards and validation protocols between these fundamentally different analytical approaches. Without global standardization, the data generated by portable devices lacks the consistency and reliability required for research, regulatory compliance, and clinical decision-making. This guide objectively compares the current landscape of portable allergen detection technologies against established laboratory methods, examining the technical and procedural gaps that impede universal protocol adoption.
Comparative Performance Analysis of Detection Platforms
The evaluation of allergen detection methods reveals significant differences in sensitivity, operational complexity, and suitable application environments. The table below summarizes the key performance metrics of various technologies.
Table 1: Performance Comparison of Allergen Detection Platforms
| Detection Platform | Detection Limit (Total Hazelnut Protein) | Detection Limit (Total Peanut Protein) | Assay Time | Format | Key Strengths |
|---|---|---|---|---|---|
| Passive Flow-Through Immunoassay [53] | 1 ppm (in matrix) | 5 ppm (in matrix) | ≤10 min | Portable | Simplicity, visual readout |
| Active Flow-Through Immunoassay [53] | 0.5 ppm (in matrix) | 1 ppm (in matrix) | ≤10 min | Portable | Improved sensitivity |
| Lateral Flow Immunoassay (LFIA) [53] | 0.5 ppm (in matrix) | 0.5 ppm (in matrix) | ≤10 min | Portable | Rapid, multiplexing potential |
| Smartphone iSPR Biosensor [20] | 0.04 - 0.53 µg/mL (in various plant-based milks) | N/R | N/R | Portable / Benchtop | Excellent sensitivity, quantitative |
| Electrochemical Sensor (MIP-based) [38] | N/R | N/R | ~6 min (inc. prep) | Portable | High accuracy in complex foods, detects tracer (genistein) |
| Conventional Benchtop SPR [20] | (Reference method) | N/R | N/R | Benchtop | Gold-standard sensitivity, full sensorgrams |
| ELISA [1] | (Varies by kit) | (Varies by kit) | Several hours | Benchtop | High sensitivity, quantitative, widely validated |
N/R: Not Reported in the cited studies.
Portable devices excel in speed and convenience, with most assays completed within 10 minutes or less, a stark contrast to the several hours required for a standard ELISA [53] [1]. However, this speed often comes with a trade-off in sensitivity. While the best portable systems like the smartphone-based imaging Surface Plasmon Resonance (iSPR) platform approach the sensitivity of benchtop methods—achieving limits of detection (LoDs) for hazelnut protein as low as 0.04 µg/mL in almond milk [20]—they remain the exception. More common rapid tests like Lateral Flow Immunoassays (LFIA) show higher, though still clinically relevant, LoDs (e.g., 0.5 ppm for peanut and hazelnut in food matrix) [53].
A critical challenge is that performance varies significantly based on the food matrix. As shown in Table 1, the smartphone iSPR's LoD for hazelnut protein varied by over an order of magnitude (0.04 to 0.53 µg/mL) across different plant-based milks [20]. This highlights a major standardization gap: a device validated in one matrix may not perform reliably in another, whereas laboratory methods include rigorous matrix-specific validations.
Detailed Experimental Protocols
To understand the root of performance disparities, it is essential to examine the fundamental experimental protocols underlying these technologies.
Laboratory-Reference Method: Surface Plasmon Resonance (SPR)
SPR is a label-free technique that detects biomolecular interactions in real-time by measuring changes in the refractive index on a sensor surface [20].
- Sample Preparation: Food samples (e.g., plant-based milks) are typically diluted 10-fold in an appropriate buffer. Complex matrices may require additional extraction, centrifugation, or filtration steps to remove particulates that could foul the sensor chip [20].
- Immobilization: A specific antibody (e.g., anti-hazelnut protein) is covalently immobilized on a dextran-coated gold sensor chip using standard amine-coupling chemistry.
- Analysis: The sample solution is flowed over the chip surface. Binding of the target allergen to the captured antibody causes a measurable shift in the resonance angle, producing a sensorgram. The response is proportional to the mass concentration of the bound analyte.
- Regeneration: The chip surface is regenerated by applying a low-pH buffer or detergent to dissociate the antigen-antibody complex, allowing for multiple analysis cycles [20].
Portable Immunoassays: Lateral Flow and Flow-Through
These assays rely on antibody-antigen binding visualized by a colored label, such as carbon nanoparticles or gold nanoparticles [53] [1].
- Sample Preparation: 1 g of solid food is homogenized (e.g., with mortar and pestle) and extracted in 10 mL of buffer with stirring. Liquid foods are mixed directly with the buffer [38].
- Assay Execution:
- Lateral Flow (LFIA): The sample extract is applied to the sample pad. It migrates laterally via capillary action, encountering labeled antibodies and then test/control lines where capture molecules are immobilized. A positive result is indicated by a visible line [53] [1].
- Flow-Through: The sample is applied to a membrane containing immobilized capture antibodies. In "active" flow, a wash step is applied to facilitate movement of the sample, while "passive" formats rely on gravity [53].
- Detection: Results are typically read visually or, for greater objectivity and quantitation, using a smartphone camera. Smartphone analysis can use device-independent color space to standardize results across different phone models [53].
Emerging Portable Technology: Molecularly Imprinted Polymer (MIP) Sensors
MIPs are synthetic polymer receptors with cavities complementary to the shape and functional groups of a target molecule, offering an alternative to biological antibodies [38].
- Sensor Preparation: The target molecule (e.g., genistein, a soy allergen tracer) is mixed with functional monomers and a cross-linker. Polymerization forms the MIP, after which the template is removed, leaving specific recognition sites [38].
- Sample Preparation: Identical to the protocol for immunoassays—homogenization and extraction of 1 g of food in 10 mL of buffer [38].
- Analysis & Detection: The extracted sample is incubated with the MIP sensor. Binding of the target analyte is measured electrochemically using techniques like Differential Pulse Voltammetry (DPV). An oxidation peak at a specific voltage (e.g., 0.60 V vs Ag/AgCl for genistein) confirms the presence of the target [38].
The following workflow diagram illustrates the procedural divergence between a standard laboratory method and a typical portable device protocol.
The Scientist's Toolkit: Key Research Reagent Solutions
The reliability of any allergen detection method hinges on the quality and consistency of its core reagents. The table below details essential materials and their critical functions in the assays previously discussed.
Table 2: Essential Research Reagents for Allergen Detection Assays
| Reagent / Material | Function in Assay | Key Considerations for Standardization |
|---|---|---|
| Capture & Detection Antibodies [53] [20] | Specific recognition and binding of target allergenic proteins (e.g., anti-hazelnut, anti-peanut). | Lot-to-lot consistency, specificity (minimal cross-reactivity), affinity, and stability are paramount. |
| Molecularly Imprinted Polymers (MIPs) [38] | Synthetic antibody mimics with cavities for specific allergen tracer binding (e.g., for genistein in soy). | Reproducibility of polymer synthesis and template extraction determines performance and reliability. |
| Gold/Carbon Nanoparticles [53] [1] | Visual or electrochemical labels for signal generation in immunoassays. | Particle size, morphology, and conjugation efficiency must be controlled for uniform signal strength. |
| Sensor Chips (SPR) [20] | Platform for antibody immobilization and biomolecular interaction analysis. | Surface chemistry (e.g., carboxymethyl dextran) must be uniform to ensure consistent antibody loading and activity. |
| Reference Allergen Standards [52] | Calibrants for quantitative analysis and method validation. | Purified protein composition and concentration must be certified and globally harmonized. |
| Extraction Buffers [38] | Medium for extracting allergenic proteins from complex food matrices. | pH, ionic strength, and detergent composition critically impact extraction efficiency and assay accuracy. |
Core Standardization Challenges
The path to global protocol harmonization is obstructed by several interconnected challenges that create variability in results and hinder direct comparison between methods.
Lack of Universal Reference Materials and Doses: There is currently no EU-harmonized system, let alone a global one, for allergen monitoring. This includes a lack of standardized reference doses (thresholds) for triggering precautionary allergen labeling (PAL) [52]. Without globally accepted allergen reference materials and defined action levels, it is impossible to uniformly validate the clinical relevance of the detection limits reported by any device, portable or laboratory-based.
Matrix Effects and Extraction Inefficiencies: Allergen detection in processed foods is complicated by protein denaturation and modification. As noted by researchers, "denaturation and/or degradation of proteins and DNA fragments during food processing, which can yield false negative responses" is a major limitation for many detection methods, including ELISA, LFIA, and PCR [38]. The efficiency of extracting allergenic proteins from diverse matrices (e.g., meats vs. sauces) is highly variable and not standardized, leading to significant inaccuracies [38].
Divergent Validation Protocols: The performance of a new portable smartphone iSPR biosensor was benchmarked against a conventional benchtop SPR system, showing good correlation (R² 0.950–0.991) [20]. However, such thorough correlation studies are not universally required. The validation criteria for a rapid test used in a restaurant setting are often less rigorous than those for a lab method certifying a "free-from" product, creating a spectrum of data quality that is difficult to reconcile.
Antibody Specificity and Epitope Recognition: Immunoassays depend on antibodies binding to specific epitopes on allergenic proteins. The major allergen in shellfish, tropomyosin, exhibits significant cross-reactivity among various shellfish types and even with mites and other arthropods [54]. This complicates diagnosis and management, as an assay may detect a protein that is immunologically cross-reactive but not from the target food source, potentially leading to false positives. Different antibody clones may recognize different epitopes, which can be affected differently by food processing, leading to inconsistent results between test kits.
The divergence between portable and laboratory allergen detection methods stems from a fundamental trade-off between the analytical rigor required for regulation and the practical need for speed and convenience in point-of-need testing. While portable devices are achieving increasingly impressive performance, as demonstrated by smartphone-based iSPR and MIP-sensors, the absence of a harmonized global framework for validation, reference materials, and action levels remains the single greatest obstacle to their reliable integration into research and quality control pipelines.
Future progress hinges on international cooperation. The recent work by the Codex Alimentarius Commission and the FAO/WHO Joint Expert Committee, which has begun reviewing allergen labeling and developing guidance on risk assessment and precautionary labeling, provides a crucial foundation [52]. Researchers, manufacturers, and regulators must build upon this to establish:
- Globally accepted reference materials for all major allergens.
- Matrix-specific validation protocols that portable devices must meet.
- Standardized units of measurement and reporting formats.
Until this harmonization is achieved, data generated by portable devices, though promising, must be interpreted with a clear understanding of the methodological constraints and standardization gaps that currently separate them from established laboratory standards.
The increasing global prevalence of allergic diseases has intensified the demand for reliable allergen detection. Researchers and clinicians face a critical choice between established laboratory methods and emerging portable technologies, a decision that hinges on a nuanced balance of analytical performance, cost, and operational practicality. Laboratory-based systems like immunoassays and mass spectrometry offer high throughput and precision but require significant capital investment and centralized operation. In contrast, novel portable devices and biosensors promise rapid, on-site analysis with lower upfront costs, though their operational scope is often more limited. This guide provides an objective comparison of these technologies, supported by experimental data, to inform selection for various research and development applications.
Comparative Analysis of Key Technologies
The following tables summarize the core characteristics, performance data, and cost-benefit profiles of major allergen detection platforms.
Table 1: Analytical Performance and Operational Scale of Allergen Detection Methods
| Technology | Principle / Mechanism | Typical Sensitivity | Typical Throughput | Optimal Operational Scale & Use Case |
|---|---|---|---|---|
| ImmunoCAP [55] [56] | Automated sandwich immunoassay on a cellulose solid phase | High (detects >0.35 KU/L) | Moderate (singleplex) | Large-scale clinical labs; Quantification of specific IgE for diagnosis and immunotherapy monitoring. |
| ELISA [7] [23] | Enzyme-linked immunosorbent assay on a microplate | High (parts per million) | High (96-well plate) | Centralized testing facilities; High-volume, routine screening of food products and ingredients. |
| LC-MS/MS [56] [23] | Liquid chromatography-tandem mass spectrometry | High (identifies multiple allergenic peptides) | High (multiplexed) | Research and reference labs; Confirmatory analysis and detection of multiple allergens in complex matrices. |
| Immunoblotting (RIDA) [55] | Multiplex enzyme immunoassay on nitrocellulose membrane | Moderate (83% sensitivity vs. ImmunoCAP) | Moderate (multiplex, 20 allergens/strip) | Medium-scale clinical screens; Cost-effective, rapid initial patient screening. |
| Portable Biosensors [57] [6] | Electrochemical, optical (e.g., colorimetric, fluorescent) transduction | Varies (Rapidly improving) | Low (single sample) | Point-of-care/field use; On-site food safety checks, environmental allergen mapping, and rapid initial assessments. |
Table 2: Comprehensive Cost-Benefit and Experimental Data Analysis
| Technology | Equipment Cost | Cost per Test | Key Performance Data from Studies | Primary Limitations |
|---|---|---|---|---|
| ImmunoCAP [55] [56] | Very High | High | Sensitivity: 83%, Specificity: 97%, Accuracy: 92% vs. Immunoblotting [55] | High cost of instrumentation and reagents; requires trained technicians. |
| ELISA [7] [23] | Medium-High | Low | Officially adopted by Codex Alimentarius for gluten; threshold: 20 mg/kg [23] | Limited multiplexing; protein denaturation in processed foods can affect accuracy. |
| LC-MS/MS [6] [56] | Very High | High | Capable of high-resolution, multi-allergen screening in a single injection [56] | Highest equipment and operational cost; requires extensive expertise. |
| Immunoblotting (RIDA) [55] | Medium | Low-Moderate | Kappa coefficient: 0.81, Correlation: 0.71 vs. ImmunoCAP [55] | Semi-quantitative; not recommended when precise IgE levels are critical. |
| Portable Biosensors [57] [6] | Low-Medium | Very Low | Can inactivate ~20-25% of airborne allergens in 30 mins using UV222 [39] | Lower throughput; sensitivity can be matrix-dependent; emerging technology. |
Experimental Protocols for Key Assays
This protocol details the experimental procedure for a multiplex immunoblotting assay (RIDA Allergy Screen), the performance of which was quantitatively compared to the ImmunoCAP reference method [55].
- Sample Preparation: Collect 5 mL of blood from patients. Separate serum by centrifugation and store at -70°C until analysis.
- Allergen Incubation: Add 250–400 µL of serum sample to each allergen-coated nitrocellulose membrane strip. Incubate the strips on a shaker at room temperature.
- Washing: Wash the strips with a dedicated washing buffer to remove unbound proteins.
- Detection Antibody Incubation: Add biotin-conjugated anti-human IgE to each strip. Incubate and wash again.
- Signal Amplification: Add streptavidin conjugated with alkaline phosphatase. Following incubation and washing, this complex binds to the biotinylated anti-IgE.
- Color Development: Add the substrate BCIP/NBT (bromochloroindolyl phosphate / Nitro blue tetrazolium). Alkaline phosphatase catalyzes a reaction that produces a colored precipitate.
- Quantification: Scan the developed membranes and use dedicated software to quantify the intensity of the color, reported as IU/mL. A value >0.35 IU/mL is considered positive.
This generalized protocol outlines the standard methodology for developing and validating biosensors for allergen detection, as reviewed in the literature.
- Sensor Fabrication: Functionalize the transducer surface (e.g., gold for electrochemical, chip for SPR, paper for lateral flow) with a bio-recognition element (antibody, aptamer, or DNA probe).
- Sample Preparation (if required): For complex food matrices, a preparation step such as extraction or dilution may be necessary.
- Assay Execution: Introduce the prepared sample to the sensor surface. The target allergen binds to the recognition element.
- Signal Transduction: Measure the physical or chemical change resulting from the binding event. This can be:
- Electrochemical: Change in current or impedance.
- Optical: Change in color, fluorescence intensity, or refractive index.
- SERS: Shift in Raman scattering intensity.
- Signal Processing/Analysis: A connected device (e.g., potentiostat, reader, smartphone) processes the signal and provides a quantitative or qualitative output.
This protocol describes the setup for a cost-effective, portable data sensing system that can be adapted for indoor environmental allergen monitoring.
- System Design: Build sensing nodes centered around Raspberry Pi computers. Connect compatible digital and analog sensors (e.g., for particulate matter, temperature, humidity).
- Node Configuration: Each sensing node runs local data collection software and has its own database.
- Data Transmission: Configure wireless communication modules on the nodes to transmit integrated data to a centralized server via WiFi or the Internet.
- Central Server Setup: Establish a central server with a web-based Graphical User Interface (GUI) to receive, store, and visualize data from all sensing nodes.
- Deployment & Calibration: Deploy the sensing nodes in target locations (e.g., households, specific rooms). The system is designed to be portable and requires only power and internet connection.
Technology Selection Workflow and Biosensor Mechanism
The following diagrams illustrate the logical decision-making process for technology selection and the fundamental working principle of a biosensor.
Biosensor Mechanism for Allergen Detection
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Allergen Detection Research
| Item | Function / Application |
|---|---|
| Nitrocellulose Membranes | Solid support for immobilizing allergens in immunoblotting assays (e.g., RIDA Allergy Screen) [55]. |
| Allergen Extracts / Proteins | Native or recombinant allergens used to coat membranes (immunoblotting), plates (ELISA), or sensor surfaces [55] [6]. |
| Specific IgE Antibodies / Anti-human IgE | Primary detection reagents in immunoassays to quantify patient-specific IgE levels [55]. |
| Biotin-Streptavidin System | Common signal amplification system; biotin-conjugated detection antibodies are bound by streptavidin-enzyme conjugates [55]. |
| Enzyme-Substrate Pairs (e.g., Alkaline Phosphatase + BCIP/NBT) | Generate a measurable colorimetric, fluorescent, or chemiluminescent signal for detection in ELISA and immunoblotting [55]. |
| Aptamers | Engineered single-stranded DNA or RNA molecules serving as synthetic recognition elements in biosensors, offering an alternative to antibodies [6] [23]. |
| Gold Nanoparticles (AuNPs) | Used as labels in lateral flow immunoassays and electrochemical biosensors for signal enhancement and visualization [6]. |
| Microfluidic Chips / Paper-based Devices | Miniaturized platforms that control fluid flow, enabling the development of portable, low-cost, and rapid analytical devices [6]. |
A Data-Driven Comparison: Validating Performance Metrics Across Platforms
The accurate detection of food allergens has become a critical public health priority, with the global allergen detection kit market projected to reach USD 1,250 million by 2025 [58]. For researchers, scientists, and drug development professionals, selecting the appropriate detection technology requires careful evaluation of performance metrics against operational requirements. Traditional laboratory-based methods like Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) have long been considered the gold standard for allergen detection, offering high sensitivity and specificity [23]. However, these methods can be time-consuming, require sophisticated laboratory equipment, and necessitate skilled personnel, limiting their use for rapid, on-site testing [6].
In response, a new generation of portable and point-of-care (POC) devices is emerging, promising rapid, on-the-spot analysis [59]. These technologies aim to bridge the gap between laboratory precision and field-based utility. This guide provides a head-to-head comparison of the sensitivity and specificity data from recent studies, objectively evaluating the performance of portable allergen detection devices against established laboratory methods. By synthesizing quantitative data and experimental protocols, this analysis aims to equip professionals with the evidence needed to make informed decisions in both research and applied settings.
Performance Metrics: A Quantitative Comparison of Technologies
Sensitivity and specificity are the cornerstone metrics for evaluating any diagnostic test. Sensitivity measures the test's ability to correctly identify the presence of an allergen (true positive rate), while specificity measures its ability to correctly identify the absence of an allergen (true negative rate) [32]. The following tables summarize the performance of various detection technologies as reported in recent literature.
Table 1: Performance Comparison of Point-of-Care (POC) vs. Laboratory Multiplex Assays
| Device / Assay Name | Technology Type | Sensitivity (%) | Specificity (%) | Key Allergens Tested | Reference Standard |
|---|---|---|---|---|---|
| FastCheckPOC 20 (FCP20) | POC (Lateral Flow Immunoassay) | 43.3 (Overall) | 92.1 (Overall) | 20 Inhalant & Food Allergens | ALEX2 Multiplex Assay [32] |
| FCP20 (Grass Pollen gx17) | POC (Lateral Flow Immunoassay) | 79.8 | N/R | Grass Pollen | ALEX2 Multiplex Assay [32] |
| FCP20 (Severe Symptom Patients) | POC (Lateral Flow Immunoassay) | >83.0 | N/R | Various | ALEX2 Multiplex Assay [32] |
| Allergy Explorer 2 (ALEX2) | Laboratory Multiplex Immunoassay | (Reference) | (Reference) | > 200 Allergens | - [32] |
| ImmunoCAP Rapid | POC (Lateral Flow Immunoassay) | ~76 (vs. ImmunoCAP) | ~80 (vs. ImmunoCAP) | Various | ImmunoCAP [32] |
| Mass Spectrometry | Laboratory Protein Detection | N/R | N/R | Peanut, Milk, Egg, Shellfish | - [2] |
| Detection Limit | (0.01 ng/mL) |
Table 2: Performance Characteristics of Core Detection Technology Platforms
| Technology Platform | Typical Sensitivity | Typical Specificity | Key Advantages | Inherent Limitations |
|---|---|---|---|---|
| Lateral Flow Assays (POC) | Variable (Low to Moderate) | Generally High | Rapid, user-friendly, low cost, portable | Lower sensitivity, semi-quantitative, limited multiplexing |
| ELISA (Lab) | High (CAC adopted for gluten) [23] | High | High throughput, quantitative, robust | Time-consuming, requires lab equipment, trained staff |
| PCR (Lab) | High (Official method in Germany/Japan) [23] | High | Detects highly processed allergens, specific | Indirect detection (DNA, not protein), complex sample prep |
| Mass Spectrometry (Lab) | Very High (e.g., 0.01 ng/mL) [2] | Very High | High precision, can detect specific protein markers | Costly, requires extensive expertise, complex data analysis |
| Biosensors (Emerging) | High (Rapidly improving) [6] | High | Potential for rapid, on-site, highly sensitive multiplex detection | Mostly in research/development stage, sample matrix interference |
The data reveals a clear performance trade-off. Laboratory-based methods such as mass spectrometry demonstrate exceptional sensitivity, with detection limits as low as 0.01 ng/mL for specific allergenic proteins like Ara h 3 (peanut) and Bos d 5 (milk) [2]. In contrast, a recent study on the POC device FastCheckPOC 20 (FCP20) showed an overall sensitivity of only 43.3%, despite a high specificity of 92.1% when compared to the laboratory-based ALEX2 multiplex system [32]. This indicates that while POC tests are highly reliable when a positive result is obtained, they may miss a significant number of true sensitizations, limiting their utility as a general screening tool.
However, POC performance is not uniform across all allergens or patient groups. For instance, the sensitivity of the FCP20 test for grass pollen (gx17) was notably higher at 79.8% [32]. Furthermore, in patients with severe clinical symptoms such as bronchial asthma or eczema, the test's sensitivity increased to over 83% [32], suggesting that POC devices may have more relevant clinical utility in certain well-defined contexts.
Experimental Protocols: Methodologies Behind the Data
A critical understanding of performance data requires insight into the experimental methodologies from which they are derived. The following section details the protocols used in key recent studies.
Protocol: Evaluating a Point-of-Care Device vs. a Multiplex Laboratory Assay
A 2025 cross-sectional study by et al. provides a robust framework for comparing a POC device with a reference laboratory method [32].
- Objective: To investigate the diagnostic accuracy (sensitivity and specificity) of the FastCheckPOC 20 Atopy (FCP20) in comparison with the multiplex assay Allergy Explorer 2 (ALEX2) system.
- Patient Cohort: 215 participants were recruited from South Tyrol, Italy. Inclusion criteria encompassed positive sensitizations to any food or aeroallergen, determined by prior skin prick tests or the presence of sIgE levels ≥0.30 kUA/L, and/or relevant allergic symptoms. Fourteen subjects (6.5%) with no ALEX2 sensitization served as negative controls.
- Sample Collection and Preparation: Venous blood was collected from each participant. The sample was left to clot for 15-30 minutes, followed by centrifugation at 1,500 × g for 10 minutes to obtain serum. Two aliquots of serum were prepared: one for immediate FCP20 testing and one stored at -20°C for batch analysis with ALEX2.
- FCP20 Analysis: The FCP20 test, a lateral flow immunoassay, was performed immediately according to the manufacturer's instructions. The test yields semi-quantitative results classified into five levels, correlated to CAP classes. For dichotomous analysis, levels 2-5 were classified as positive, and level 1 as negative.
- Reference Method (ALEX2) Analysis: The frozen serum samples were transported on dry ice to a central laboratory. The ALEX2 test, a macroarray-based multiplex immunoassay, was performed according to the manufacturer's protocols to detect specific IgE antibodies against a wide range of allergenic molecules.
- Data Analysis: Dichotomous data (positive/negative) from the FCP20 were used to calculate sensitivity, specificity, and their 95% confidence intervals in comparison with the ALEX2 results.
Protocol: Laboratory-Based Mass Spectrometry for Allergen Detection
Mass spectrometry represents the cutting edge of laboratory-based allergen detection, with protocols focused on high specificity and precision [2] [23].
- Objective: To simultaneously quantify specific allergenic proteins (e.g., Ara h 3, Ara h 6 for peanut; Bos d 5 for milk) in complex food matrices.
- Sample Preparation: Food samples are first homogenized. Proteins are then extracted using a suitable buffer. The extracted proteins are digested with an enzyme (typically trypsin) to generate specific peptide fragments. These peptides are often purified and concentrated via solid-phase extraction.
- Mass Spectrometry Analysis: The digested peptide mixture is separated by liquid chromatography (LC) and introduced into a tandem mass spectrometer (MS/MS).
- Detection and Quantification: The MS/MS instrument operates in Selected Reaction Monitoring (SRM) or Multiple Reaction Monitoring (MRM) mode. It selectively detects and quantifies pre-defined "proteotypic peptides" that are unique markers for the target allergenic protein. Quantification is achieved by comparing the signal of the target peptides to that of isotope-labeled internal standards.
- Data Analysis: The presence and quantity of the allergenic protein are determined based on the detection of its unique peptide markers and their signal intensity.
The workflow below illustrates the logical sequence and key decision points for selecting an allergen detection method based on the requirements of the analysis.
The Scientist's Toolkit: Key Research Reagents and Materials
The reliability of any allergen detection experiment hinges on the quality and appropriateness of its core components. The following table details essential research reagent solutions and their critical functions in various experimental protocols.
Table 3: Essential Research Reagents and Materials for Allergen Detection
| Reagent / Material | Function in Experiment | Example Use-Case |
|---|---|---|
| Specific IgE Antibodies | Primary recognition element in immunoassays; binds specifically to target allergenic proteins. | Used as capture/detection antibodies in ELISA [23] and LFIA [32] for identifying allergens like Gal d 1 (egg) or Ara h 1 (peanut). |
| DNA Primers & Probes | Binds to complementary DNA sequences to amplify and detect allergen-specific genetic markers. | Essential for PCR-based detection of allergen sources (e.g., fish, crustacean) in processed foods [23]. |
| Proteotypic Peptides | Synthetic, isotope-labeled peptides that serve as unambiguous references for target allergenic proteins. | Critical internal standards for absolute quantification of allergens (e.g., Bos d 5) using LC-MS/MS [2] [23]. |
| Allergen Extracts | Complex mixtures of proteins from allergenic sources (e.g., peanut, milk) used for calibration and validation. | Coating microplates in ELISA; used as positive controls and for creating standard curves [32]. |
| Enzymes (HRP, ALP) | Horseradish Peroxidase (HRP) or Alkaline Phosphatase (ALP) conjugated to antibodies for signal generation. | Conjugated to detection antibodies in ELISA; catalyzes colorimetric/chemiluminescent reaction for readout [1]. |
| Magnetic Beads | Solid phase for immobilizing antibodies or other capture agents, easily separated via magnetism. | Used in automated or semi-automated immunoassays and biosensors to concentrate allergens and improve sensitivity [6]. |
| Aptamers | Engineered single-stranded DNA or RNA molecules that bind targets with high affinity and specificity. | Emerging as synthetic recognition elements in biosensors for allergens like tropomyosin (shrimp) and β-lactoglobulin (milk) [23] [6]. |
Emerging Technologies and Future Outlook
The field of allergen detection is dynamic, with significant innovation aimed at overcoming the limitations of current POC and laboratory methods. Emerging biosensing technologies leveraging colorimetric, fluorescent, electrochemical, and Surface Enhanced Raman Spectroscopy (SERS) principles are showing great promise for achieving laboratory-level sensitivity in portable formats [6]. Furthermore, the integration of these biosensors with microfluidic chips, lateral flow assays (LFAs), and smartphone-based readout systems is creating a new class of portable analytical devices that are intelligent, connected, and accessible [1] [6]. This aligns with the growing trend of "citizen science," putting analytical power directly into the hands of consumers [1].
Artificial intelligence is also poised to transform the landscape. AI-enhanced testing and non-destructive diagnostics using methods like Hyperspectral Imaging (HSI) and Computer Vision (CV) allow for real-time allergen detection without altering the food sample [2]. AI models are even being developed to predict the allergenicity of new ingredients before they enter the supply chain [2]. As these technologies mature, the historical trade-off between the high performance of laboratory methods and the convenience of portable devices is expected to diminish, enabling faster decision-making and greater safety for allergic individuals.
For researchers and scientists in food safety and drug development, selecting an appropriate allergen detection method hinges on a critical understanding of the data output—whether quantitative or qualitative. Laboratory-based methods like Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) are established techniques that provide robust quantitative data, measuring the precise concentration of an allergenic protein or DNA [60] [23]. In contrast, a new generation of portable biosensors and lateral flow devices is increasingly deployed for rapid, on-site screening, typically delivering qualitative or semi-quantitative results that indicate the presence or absence of an allergen above a certain threshold [61] [6].
This guide provides a detailed, evidence-based comparison of these methodologies. It is structured to assist professionals in evaluating the performance, operational parameters, and suitable applications of each approach within the context of a rigorous research and development framework.
Comparative Analysis of Performance and Data Output
The core distinction between these methods lies in the nature and application of the data they generate. The following table summarizes the key performance characteristics of each method, highlighting the trade-offs between data richness and operational speed.
Table 1: Key Characteristics of Allergen Detection Methods
| Feature | Laboratory Methods (e.g., ELISA, PCR) | Portable Methods (e.g., Biosensors, LFDs) |
|---|---|---|
| Primary Data Output | Quantitative (precise concentration) [23] | Qualitative or Semi-Quantitative (presence/absence or relative level) [61] |
| Sensitivity | High (parts per million/billion) [23] | Variable; generally lower than lab methods, but improving [6] |
| Time to Result | Hours to a full day [6] | Minutes to under an hour [61] |
| Throughput | High (can process many samples simultaneously) | Low (typically single samples) |
| User Skill Level | Requires trained technicians [6] | Designed for ease-of-use with minimal training [61] |
| Environment | Controlled laboratory setting [6] | Field-deployable for on-site testing (e.g., factory, restaurant) [61] |
| Key Advantage | High accuracy, precision, and defensible data for compliance | Speed, portability, and cost-effectiveness for rapid decision-making |
Quantitative data from laboratory methods is indispensable for compliance with regulatory thresholds, dose-response studies, and validating the effectiveness of allergen removal processes in a production line [62] [60]. For instance, the Codex Alimentarius specifies a gluten threshold of 20 mg/kg, a level that requires quantitative measurement via ELISA for official verification [23].
Conversely, the qualitative output from portable devices supports risk mitigation at critical control points. A "yes/no" result is often sufficient for making immediate decisions, such as checking for cross-contamination on shared equipment before running a batch of "allergen-free" products or verifying a dish in a restaurant kitchen [61]. Emerging portable sensors are beginning to offer semi-quantitative capabilities, but their primary value remains rapid screening [6].
Experimental Protocols and Methodological Detail
Laboratory-Based Quantitative Protocol: Sandwich ELISA
The Sandwich ELISA is a widely used quantitative method for detecting specific allergenic proteins. Its reliability stems from the use of two antibodies for high specificity [23].
Table 2: Key Research Reagents for Sandwich ELISA
| Reagent/Material | Function in the Protocol |
|---|---|
| Capture Antibody | Monoclonal or polyclonal antibody immobilized on the plate to specifically bind the target allergen. |
| Blocking Buffer | (e.g., BSA or protein-free solution) Coats the well to prevent non-specific binding of other proteins. |
| Standard Solutions | Known concentrations of the purified allergen used to generate the calibration curve. |
| Detection Antibody | A second antibody that binds to a different epitope on the captured allergen. |
| Enzyme Conjugate | (e.g., Horseradish Peroxidase, HRP) Covalently linked to the detection antibody for signal generation. |
| Chromogenic Substrate | (e.g., TMB) The enzyme catalyzes a color change in this substrate, producing a measurable signal. |
Detailed Workflow:
- Plate Coating: A capture antibody specific to the target allergen (e.g., Ara h 1 for peanut) is adsorbed onto the wells of a microtiter plate [23].
- Blocking: Remaining protein-binding sites on the plate are blocked with a blocking buffer (e.g., Bovine Serum Albumin) to minimize non-specific background signal.
- Sample & Standard Incubation: Test samples and a series of standard solutions with known allergen concentrations are added to separate wells. The allergen binds to the immobilized capture antibody during incubation.
- Washing: Wells are washed thoroughly to remove unbound proteins.
- Detection Antibody Addition: A second, enzyme-linked detection antibody is added. It binds to the now-captured allergen, completing the "sandwich."
- Second Washing: Another wash removes any unbound detection antibody.
- Substrate Addition: A chromogenic substrate is added. The enzyme (e.g., HRP) conjugated to the detection antibody catalyzes a reaction, producing a colored product.
- Signal Measurement & Quantification: The reaction is stopped, and the absorbance is measured with a plate reader. The absorbance of the standards is used to create a calibration curve, from which the precise concentration of the allergen in the sample is calculated [23].
Portable Qualitative Protocol: Lateral Flow Immunoassay (LFIA)
Lateral Flow Devices (LFDs), or dipsticks, are a common format for portable, qualitative allergen testing. They are a type of immunoassay designed for single-use and visual readout [6].
Detailed Workflow:
- Sample Preparation: A small amount of food sample is homogenized in an extraction buffer to solubilize the target protein.
- Sample Application: The extract is applied to the sample pad of the strip. The solution migrates laterally via capillary action.
- Conjugation & Reaction: As the sample moves, it rehydrates and mixes with colored particles (e.g., gold nanoparticles) coated with detection antibodies specific to the allergen. If the allergen is present, it forms a complex with these antibodies.
- Capture & Signal Generation: The complex continues to flow across a nitrocellulose membrane until it reaches the test line. This line is pre-coated with immobilized antibodies that capture the allergen-antibody-particle complex, leading to a visible colored line.
- Control Verification: The sample continues to a control line, which captures excess detection antibodies to confirm the device has functioned correctly.
- Result Interpretation: The appearance of both a control line and a test line indicates a positive result. Only a control line indicates a negative result. The absence of a control line invalidates the test [6]. The result is typically read visually within minutes, providing a straightforward "yes/no" answer.
Workflow and Signaling Pathways
The fundamental difference in operational complexity between laboratory and portable methods can be visualized in their workflows. The multi-step, centralized lab process requires precise timing and specialized equipment, while the portable device workflow is streamlined for a single-step user experience in the field.
The choice between quantitative laboratory methods and qualitative portable devices is not a matter of superiority, but of application.
- For Definitive Quantification: When the research or regulatory objective requires knowing the exact concentration of an allergen—such as for establishing threshold doses, validating cleaning protocols, or meeting specific labeling laws—quantitative laboratory methods like ELISA and PCR are the unequivocal choice [60] [23]. Their high sensitivity and proven accuracy provide the defensible data necessary for these critical applications.
- For Rapid Screening and Risk Management: When the need is for speed and convenience to monitor potential allergen cross-contact at various points in the supply chain, manufacturing process, or food service environment, portable qualitative devices are highly effective [61] [6]. Their value lies in preventing issues proactively rather than quantifying them after the fact.
The field is advancing toward hybrid solutions. Research is focused on enhancing portable biosensors with multiplexing (detecting multiple allergens at once) and semi-quantitative capabilities, while laboratory methods continue to improve in speed and automation [63] [6]. For a comprehensive food safety program, the two approaches are complementary: portable devices for rapid, in-process checks and laboratory methods for final verification and compliance.
For researchers, scientists, and drug development professionals working in food safety and clinical diagnostics, the choice of analytical method is often a strategic trade-off between the need for rapid results and the requirement for definitive, comprehensive data. On one hand, the management of food allergies, which affect 2–5% of adults and 6–8% of children globally, demands timely interventions to prevent life-threatening anaphylaxis [1] [38]. On the other hand, the complex and variable nature of allergenic proteins, which can be altered by food processing, necessitates methods with significant analytical depth to avoid misdiagnosis and ensure consumer safety [43]. This guide provides a objective comparison of portable allergen detection devices and traditional laboratory methods, framing the analysis within the critical parameters of turnaround time and analytical depth to inform research and development decisions.
Allergen detection strategies can be broadly categorized into laboratory-based methods and emerging portable technologies. Each category possesses distinct operational paradigms, advantages, and limitations.
- Laboratory-Based Methods: These are established, often gold-standard techniques conducted in controlled settings. They are characterized by high sensitivity, specificity, and the ability to provide quantitative or highly definitive qualitative results. Their main drawbacks include longer turnaround times, the need for sophisticated equipment and trained personnel, and higher costs, making them less suitable for on-site, rapid-decision scenarios [6] [43] [64].
- Portable & Rapid Detection Devices: This category encompasses technologies designed for simplicity, speed, and use outside the central laboratory. The driving force behind their development is a trend toward point-of-care diagnostics (PoC) and a citizen science approach, putting analysis directly into the hands of consumers or production line staff [1]. While offering unparalleled speed and convenience, these methods can face challenges with sensitivity in complex matrices, limited multiplexing capability, and providing less comprehensive data compared to lab-based techniques [6] [38].
Table 1: Core Principle and Applications of Allergen Detection Methods
| Method Category | Core Principle | Primary Application Context |
|---|---|---|
| Immunoassay (ELISA) | Uses antibodies to specifically recognize and capture target allergenic proteins [1] [6]. | Laboratory-based quantitative detection; process validation in food industry [65] [64]. |
| Lateral Flow Devices (LFDs) | A rapid, immunoassay format where a sample flows along a strip, producing a visible line if the allergen is present [1] [64]. | Rapid screening on production lines, cleaning verification; simplest portable format [65] [64]. |
| Polymerase Chain Reaction (PCR) | Amplifies and detects DNA sequences specific to the allergenic species [6] [64]. | Laboratory detection, especially for allergens where protein-based tests are unsuitable (e.g., celery) or for hydrolyzed proteins [65] [64]. |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Identifies allergenic proteins by detecting unique peptide markers; highly specific and capable of multiplexing [66] [43] [64]. | Laboratory gold-standard for confirmatory analysis; detection of processed allergens that may escape immunoassays [64]. |
| Electrochemical Sensors | Measures electrical signals generated from the interaction between a sensing element (e.g., antibody, MIP) and the target allergen [6] [38]. | Emerging portable, consumer-friendly devices for on-site food testing [38] [67]. |
| Multiplex Allergen Microarray | Simultaneously tests a single sample for reactivity to a wide array of allergenic proteins immobilized on a solid surface [43]. | Research and clinical laboratories for comprehensive allergenicity profiling of foods or patient sera [43]. |
Comparative Performance Data: Turnaround Time vs. Analytical Capabilities
The fundamental trade-off between speed and precision is quantified in the following performance metrics. This data is critical for selecting the appropriate method based on the specific research or operational question.
Table 2: Comparative Analysis of Turnaround Time and Analytical Performance
| Method | Typical Turnaround Time | Detection Limit | Analytical Output / Key Advantage | Key Limitation |
|---|---|---|---|---|
| Lateral Flow (LFD) | ~10-15 minutes [65] | Varies by allergen (ppm range) | Qualitative (Present/Absent); rapid, portable, minimal training [64] | Qualitative only; potential for matrix interference; may miss processed allergens [38] [64] |
| Electrochemical Sensor | ~60 seconds [67] | Clinically relevant levels (e.g., for soy) [38] | Quantitative/Semi-Quantitative; rapid, portable, consumer-friendly design [38] [67] | Emerging technology; performance in extreme matrices requires further validation [38] |
| ELISA | 60 - 90 minutes [65] | Low ppm (e.g., 1-5 ppm) [66] | Quantitative; high sensitivity and specificity; widely validated [6] [64] | Susceptible to antibody cross-reactivity; processing can denature target proteins [38] |
| PCR | Several hours [6] | High sensitivity (DNA detection) | Qualitative/Multiplex; detects allergens without available ELISA; works for hydrolyzed proteins [64] | Detects DNA, not protein; processing can degrade DNA; not for low-DNA allergens (e.g., egg) [64] |
| LC-MS/MS | ~2 hours (analytical time) [66] | ~1-2 ppm [66] | Quantitative & Multiplex; high specificity; detects processed and marker peptides directly [43] [64] | High equipment cost; requires specialized expertise; sample transport to lab [6] [66] |
| Multiplex Microarray | Several hours [43] | Not specified (profiling tool) | Comprehensive profile; identifies multiple IgE-reactive proteins in a single test [43] | Complex data interpretation; primarily a profiling tool rather than a quantitative assay [43] |
Experimental Protocols for Key Methodologies
To ensure reproducibility and provide a clear understanding of operational rigor, detailed protocols for two representative methods—one rapid and one laboratory-based—are outlined below.
Protocol for Electrochemical Sensor Detection of Soy Allergen
This protocol is adapted from a study demonstrating a molecularly imprinted polymer (MIP)-based sensor tested in 42 complex food products [38].
1. Sensor Preparation:
- Screen-printed carbon electrodes are modified with a MIP specific to genistein, a soy allergen marker. The MIP is synthesized via electrophysiological of ortho-phenylenediamine (o-PD) in the presence of the genistein template [38].
2. Food Sample Preparation:
- Solid Foods: 1 g of food is homogenized into a fine powder using a mortar and pestle (5 min). The powder is mixed with 10 mL of buffer solution (e.g., 1X PBS) and stirred for 15 minutes.
- Liquid Foods: 1 g of food is mixed directly with 10 mL of buffer solution [38].
3. Measurement & Detection:
- A template-extracted MIP electrode is equilibrated in the buffer for 5 minutes.
- The electrode is incubated with 100 µL of the prepared sample solution for 1 minute.
- The electrode is subjected to Differential Pulse Voltammetry (DPV) measurements (parameters: scan rate 50 mV/s, pulse width 50 ms, amplitude 50 mV).
- A positive response is confirmed by an oxidation peak at approximately 0.60 V vs Ag/AgCl and an imprinting factor (MIP signal/NIP signal) above 1.3 [38].
4. Confirmatory Analysis (Referenced Study):
- Results were confirmed using a commercial Soy Protein LFD kit. 100 µL of liquid food sample was mixed with 900 µL of extraction buffer, vortexed, and 100 µL was applied to the LFD sample well, with results read after 11 minutes [38].
Protocol for Multiplex Allergen Microarray Immunoassay
This protocol details the innovative single point highest inhibition achievable assay (SPHIAa) used for comprehensive allergen profiling [43].
1. Food Extract Preparation:
- Food samples are homogenized and extracted using an appropriate buffer (e.g., high-salt or high-pH buffers to improve protein recovery). The extraction buffer must be optimized for the specific food matrix to ensure efficient solubilization of allergenic proteins, which may be altered or insolubilized by processing [43].
2. IgE-Binding Inhibition Assay:
- A suspension of the food extract is pre-incubated with a serum pool containing IgE antibodies from allergic patients. This incubation allows allergenic proteins in the food extract to bind to the IgE antibodies [43].
3. Microarray Incubation:
- The pre-incubated serum is then transferred to a multiplex allergen biochip (e.g., ISAC or FABER test) containing hundreds of different purified allergenic proteins immobilized in an array format. Any IgE not inhibited by the food extract will bind to its corresponding allergen on the biochip [43].
4. Detection and Analysis:
- Bound IgE is detected using a fluorescently labelled anti-human IgE antibody.
- The fluorescence signal is measured using a dedicated microarray scanner. A reduction in fluorescence signal for a specific allergenic spot on the biochip indicates that the corresponding allergen was present in the food extract and successfully inhibited IgE binding. This provides a comprehensive map of IgE-binding proteins in the food sample with a single test [43].
Diagram 1: Multiplex Allergen Microarray Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting experiments in the field of allergen detection research, as featured in the cited protocols and literature.
Table 3: Key Research Reagent Solutions for Allergen Detection
| Item | Function in Research |
|---|---|
| Allergen-Specific Antibodies (Monoclonal/Polyclonal) | Bio-recognition elements for immunoassays (ELISA, LFDs); critical for specificity and sensitivity [1] [6]. |
| Molecularly Imprinted Polymers (MIPs) | Synthetic polymer receptors with tailor-made recognition sites for specific allergenic molecules; used in electrochemical sensors as antibody alternatives [38]. |
| Screen-Printed Electrodes (SPEs) | Disposable, miniaturized electrochemical cells used as the platform for sensor modification and signal measurement in portable devices [38]. |
| Allergen Microarray Biochips (e.g., ISAC, FABER) | Solid supports with immobilized arrays of purified allergenic proteins; enable multiplexed detection of IgE reactivity in a single experiment [43]. |
| Human Sera Pool (from Allergic Individuals) | Source of specific IgE antibodies; essential for functional assays that assess the IgE-binding capacity (allergenicity) of food samples [43]. |
| Protein Extraction Buffers (e.g., High-Salt, High-pH) | Solutions designed to efficiently solubilize allergenic proteins from complex food matrices, which is critical for accurate detection post-processing [43]. |
| PCR Master Mix & Allergen-Specific Primers | Reagents for DNA amplification; used to detect the presence of allergenic species via their genetic material [6] [64]. |
| LC-MS/MS Grade Solvents and Peptide Standards | High-purity solvents for chromatographic separation and synthetic peptide standards for method development and quantification in mass spectrometry [66]. |
Emerging Technologies and Future Directions
The field of allergen detection is dynamically evolving, with research focused on bridging the gap between speed and precision. Key emerging trends include:
- Smartphone-Based Analysis: The integration of assays with smartphones as detectors leverages their powerful cameras, portability, and connectivity. This approach, centered around citizen science, aims to put robust analysis directly into the hands of consumers for on-demand testing [1].
- Dual-Mode Biosensing: The development of biosensors that combine multiple detection principles (e.g., colorimetric and electrochemical) in a single device enhances reliability and provides internal validation, mitigating the risk of false positives/negatives [6].
- Advanced Materials: The application of novel nanomaterials and improved MIPs continues to increase the sensitivity, stability, and affordability of biosensors, pushing the performance of portable devices closer to that of laboratory standards [6] [38].
Diagram 2: Research Focus Areas for Allergen Detection
The comparative analysis presented in this guide underscores that the dichotomy between speed and precision in allergen detection is not absolute but represents a spectrum of technological capabilities. Lateral flow devices and electrochemical sensors offer clear advantages for rapid screening and on-site verification, with turnaround times as low as one minute. In contrast, laboratory methods like ELISA, LC-MS/MS, and multiplex microarrays provide the analytical depth, quantification, and comprehensive profiling required for process validation, confirmatory analysis, and fundamental research. For researchers and drug development professionals, the optimal method is contingent on the specific question at hand—whether it is the immediate presence of an allergen or a full understanding of its immunoreactive profile. The future of the field lies in the continued convergence of these paths, driven by innovations that enhance the speed of laboratory-grade techniques and the analytical robustness of portable devices.
The global food allergen testing market, valued at USD 985.9 million in 2025, is experiencing significant growth driven by rising allergy prevalence and technological innovation [68]. This expansion coincides with a critical public health challenge: food allergies have become a worldwide health concern where strict avoidance remains the primary prevention strategy, creating an urgent need for reliable detection methods [23] [69]. While laboratory-based techniques like ELISA and PCR have established the standard for allergen detection, they present limitations for real-time, on-site testing due to their time-consuming processes, requirement for skilled personnel, and laboratory infrastructure [70] [38].
Portable allergen detection devices have emerged to bridge this gap, offering consumers and industry professionals the ability to detect allergens rapidly outside controlled laboratory settings. This case study provides a rigorous comparative analysis of leading commercial portable allergen detection technologies, evaluating their real-world performance against established laboratory benchmarks. We examine operational characteristics, analytical performance across complex food matrices, and practical limitations to determine the current viability and future trajectory of point-of-care allergen detection systems for research and clinical applications.
Comparative Analysis of Detection Technologies
Technology Performance Specifications
Table 1: Comparative analysis of major allergen detection technology platforms
| Technology | Detection Mechanism | Key Allergens Detected | Sensitivity | Analysis Time | Portability | Complex Food Matrix Performance |
|---|---|---|---|---|---|---|
| ELISA (Lab) | Antibody-antigen binding | Proteins from major allergens (peanut, soy, milk) | High (ppm range) | 1-2 hours | No | Moderate, can be affected by processing |
| PCR (Lab) | DNA amplification | Allergen-specific DNA sequences | High (ppm range) | 2-3 hours | No | Good for processed foods, but indirect |
| Lateral Flow Devices | Immuno-chromatography | Specific proteins (e.g., peanut, gluten) | Moderate | 10-15 minutes | Yes | Variable, viscosity affects accuracy [38] |
| MIP-based Sensors | Molecular imprinting | Soy (genistein tracer) | Clinically relevant levels | ~5 minutes | Yes | Excellent (validated in 42 complex foods) [38] |
| Electrochemical Biosensors | Electron transfer measurement | Peanut, shellfish, milk | Varies by design | Minutes | Yes | Improved with nanomaterials [71] |
Commercial Device Performance Metrics
Table 2: Real-world performance data of commercial portable allergen detection devices
| Device/Technology | Reported Accuracy | Detection Limit | Sample Type | Validation Scale | Key Limitations |
|---|---|---|---|---|---|
| Nima Peanut Sensor | 99.2% for ≥10 ppm peanut protein [68] | 10 ppm peanut protein | Solid and liquid foods | Manufacturer data | Single-allergen focus |
| Ally (Lactose Device) | Technology demonstrated | Lactose | Dairy products | Commercial product | Single-allergen focus [68] |
| MIP-based Sensor (Research) | 100% concordance with LFD in 42 foods [38] | Clinically relevant levels | Complex foods (42 types) | Academic study (300+ ingredients) | Currently research stage |
| 3M Soy Protein LFD | Reference method | Manufacturer specified | Liquid and solid extracts | Industry standard | Affected by food viscosity [38] |
| Gold Nanoparticle Biosensors | High (research phase) | Varies by target | Food samples | Laboratory studies | Mostly in development [71] |
Experimental Protocols and Methodologies
Standardized Laboratory Validation Protocols
Established laboratory methods provide the benchmark for evaluating portable device performance. ELISA (Enzyme-Linked Immunosorbent Assay) operates on antibody-antigen binding principles, typically requiring 1-2 hours for completion and offering high sensitivity in the parts-per-million (ppm) range [23]. PCR (Polymerase Chain Reaction) methods detect allergen-specific DNA sequences rather than proteins, demonstrating particular effectiveness for highly processed foods where protein structures may be denatured but DNA fragments remain detectable [23]. These methods employ standardized extraction buffers, controlled incubation temperatures, and calibrated instrumentation to ensure reproducible results across laboratories.
Sample preparation follows rigorous protocols: 1g of solid food is homogenized using a mortar and pestle until achieving a fine powder, then mixed with 10mL of buffer solution and stirred for 15 minutes. Liquid samples are prepared by direct mixing with buffer solution [38]. This standardized preparation ensures consistent analyte extraction and minimizes matrix effects that could interfere with detection accuracy. For protein-based detection methods like ELISA, additional steps may be required to address protein denaturation from food processing, which can potentially lead to false negatives if epitope structures are altered [23].
Portable Device Testing Methodologies
Portable devices employ streamlined protocols designed for rapid on-site analysis. For the MIP-based sensor technology, the testing protocol involves: (1) template-extracted MIP electrode equilibration in 10mL buffer solution for 5 minutes; (2) electrode removal and surface drying; (3) 1-minute incubation with 100μL of sample solution; and (4) differential pulse voltammetry measurements with specific parameters (scan rate: 50 mV/s; pulse width: 50 ms; amplitude: 50 mV) [38]. Positive responses are identified by an oxidation peak at approximately 0.60 V vs Ag/AgCl reference electrode and an imprinting factor above 1.3.
Lateral flow devices (LFDs), such as the 3M Soy Protein LFD used for confirmatory analysis in validation studies, follow manufacturer protocols: 100μL of liquid food samples are mixed with 900μL of extraction buffer and vortexed for 15 seconds. Then, 100μL of the mixture is introduced to the LFD sample well and incubated for 11 minutes before visual interpretation of results [38]. These simplified protocols enable rapid detection but may sacrifice the sensitivity and quantitative precision of laboratory methods, representing a trade-off between speed and analytical rigor.
Figure 1: Experimental workflow for MIP-based portable allergen sensors
Research Reagent Solutions and Essential Materials
Core Detection Components
Table 3: Essential research reagents and materials for allergen detection systems
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Molecularly Imprinted Polymers (MIPs) | Synthetic recognition elements | Soy allergen detection via genistein imprinting [38] |
| Gold Nanoparticles | Signal amplification, transduction | Enhanced sensitivity in biosensors for peanut allergens [71] |
| Carbon Screen-Printed Electrodes | Electrochemical sensing platform | MIP-based sensor substrate [38] |
| Monoclonal/Polyclonal Antibodies | Target capture and recognition | ELISA, lateral flow immunoassays [23] |
| Allergen-Specific Aptamers | Alternative recognition elements | Tropomyosin detection in shellfish [23] |
| ELISA Kits | Quantitative protein detection | Official gluten detection method (CAC) [23] |
| PCR Master Mixes | DNA amplification | Species-specific allergen gene detection [23] |
| Extraction Buffers | Protein/DNA recovery from matrices | Sample preparation across technologies [38] |
Emerging Nanomaterials and Their Applications
Nanoparticles attribute to nanobiosensors their enhanced properties, including high surface area-to-volume ratio and improved conductivity, which significantly boost performance for allergenic protein detection [71]. Gold nanoparticles demonstrate particular promise in biosensor applications for peanut allergens (Ara h proteins), while carbon-based nanomaterials and quantum dots offer alternative platforms with tunable electronic and optical properties. These nanomaterials facilitate the development of biosensors with improved sensitivity, selectivity, and lower detection limits, potentially overcoming limitations of traditional methods related to protein denaturation during food processing [71].
The functionalization of these nanomaterials with specific biological recognition elements (antibodies, aptamers, or imprinted polymers) creates sophisticated detection systems capable of operating in complex food matrices. For instance, graphene and quantum dots can be conjugated with aptamers specific to tropomyosin for shellfish allergen detection, representing a significant advancement over antibody-based approaches in terms of stability and production cost [23] [71].
Figure 2: Signaling pathways across different allergen detection technology platforms
Discussion: Performance Gaps and Future Directions
Analytical Challenges in Real-World Applications
Portable allergen detection devices face significant technical challenges that limit their widespread adoption as laboratory replacements. A primary limitation is the lack of standardization in testing practices across platforms, leading to inconsistencies in results and difficulties in comparing data across studies and regions [68]. This standardization gap creates confusion among researchers and manufacturers who cannot uniformly interpret testing outcomes. Additionally, these devices struggle with accurately detecting trace amounts of allergens in complex food matrices, particularly challenging for individuals with high sensitivity who react to minute quantities [68].
The sample matrix interference presents another substantial hurdle. Food viscosity and texture strongly influence the accuracy of lateral flow devices, while processed foods containing denatured proteins or fragmented DNA can yield false negatives in antibody-based and PCR methods, respectively [38]. Furthermore, antibody-based platforms demonstrate limited thermal stability and potential cross-reactivity with other food components, potentially producing false positives [38]. These technical limitations highlight the considerable performance gap that remains between portable devices and laboratory methods in terms of reliability, sensitivity, and quantitative precision.
Emerging Innovations and Research Trajectories
Future research directions focus on overcoming current limitations through technological convergence. Artificial intelligence and machine learning algorithms are being integrated with hyperspectral imaging (HSI) and Fourier Transform Infrared (FTIR) spectroscopy to enable non-destructive, real-time allergen detection without compromising food integrity [2]. These AI models show promise in predicting the allergenicity of novel ingredients before they enter the supply chain, potentially revolutionizing safety assessment protocols. Multiplexed detection platforms represent another frontier, with mass spectrometry advancements now capable of simultaneously quantifying specific allergenic proteins (e.g., Ara h 3 and Ara h 6 in peanuts, Bos d 5 in milk) at sensitivities as low as 0.01 ng/mL [2].
Nanomaterial innovations continue to drive progress, with gold, carbon, graphene, and quantum dots enabling more sensitive and selective detection platforms [71]. The integration of these nanomaterials with microfluidic systems creates opportunities for miniaturized, automated detection platforms that could eventually match laboratory sensitivity while maintaining portability. Additionally, cloud-based platforms that integrate multiple data streams (ATP readings, microbial counts, allergen detection) are emerging as comprehensive solutions for allergen control management, offering predictive risk assessment capabilities and centralized compliance documentation [2]. These converging technologies suggest a future where portable devices may eventually achieve the reliability standards currently exclusive to laboratory methods, though significant research and development investments remain necessary to bridge existing performance gaps.
Conclusion
The choice between portable and laboratory-based allergen detection is not a matter of superiority but of strategic application. Laboratory methods (ELISA, PCR) remain indispensable for their high sensitivity, quantitative precision, and regulatory compliance in controlled settings. Portable devices offer unparalleled advantages in speed, cost-effectiveness, and on-site decision-making, though they may trade off some analytical depth. The future of allergen detection lies in the convergence of these fields: the development of 'lab-on-a-chip' technologies, the integration of AI for real-time data analysis, and the advancement of multiplexed biosensors. For researchers and drug developers, this evolving toolkit enables more personalized, rapid, and accessible allergy management solutions, paving the way for next-generation diagnostics and therapies.
References
- 1. Consumer-friendly food allergen detection - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6096701/]
- 2. Innovations shaping the future of food allergen testing [https://allergenbureau.net/innovations-shaping-the-future-of-food-allergen-testing/]
- 3. Instant Allergen Detection: Portable Food Sensors Explained [https://www.azosensors.com/article.aspx?ArticleID=3215]
- 4. NIST Food Protein Allergen Program [https://www.nist.gov/programs-projects/nist-food-protein-allergen-program]
- 5. CLSI ILA37 Database for Allergens | News [https://clsi.org/about/news/clsi-announces-updates-to-the-i-la37-database-supplemental-data-for-allergen-specificity-for-ige-antibody-autoanalyzers/]
- 6. Recent progresses on emerging biosensing technologies ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224424001614]
- 7. The Growing Importance of Allergen Testing: How Certified ... [https://fsns.com/the-growing-importance-of-allergen-testing-how-certified-group-ensures-food-safety-with-elisa/]
- 8. Comparison of real-time PCR and ELISA-based methods ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713516303802]
- 9. Analytical techniques for nucleic acid and protein detection ... [https://www.nature.com/articles/s12276-025-01453-w]
- 10. Comparing Mass Spectrometry, ELISA, and Olink for ... [https://blog.genewiz.com/comparing-mass-spectrometry-elisa-and-olink-for-proteomics]
- 11. A Critical Comparison between Flow-through and Lateral ... [https://www.mdpi.com/2079-6374/9/4/143]
- 12. Lateral Flow Assay: A Summary of Recent Progress for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10526804/]
- 13. Lateral flow test engineering and lessons learned from ... [https://www.nature.com/articles/s44222-022-00007-3]
- 14. A comprehensive review of competitive lateral flow assays ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc01075b]
- 15. Portable electrophoretic lateral flow biosensing for ultra ... [https://www.sciencedirect.com/science/article/pii/S0956566325003781]
- 16. Novel Artificial Intelligence Approach For nsLTP Early ... [https://link.springer.com/article/10.1007/s12161-025-02851-6]
- 17. United States Food Allergen Testing Market Trends ... [https://vocal.media/feast/united-states-food-allergen-testing-market-trends-and-summary-2025-2033]
- 18. United States Food Allergen Testing Market Size and ... [https://www.renub.com/us-food-allergen-testing-market-p.php]
- 19. Food allergen detection choosing the right testing method [https://www.rssl.com/insights/food-consumer-goods/food-allergen-detection-choosing-the-right-testing-method/]
- 20. A portable smartphone-based imaging surface plasmon ... [https://www.sciencedirect.com/science/article/pii/S0039914023001170]
- 21. Food Allergenicity Evaluation Methods: Classification, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191692/]
- 22. Food allergen testing: should you use ELISA, PCR, or LFA ... [https://blog.invitek.com/articles/foodsafetyintegrity/food-allergen-testing-should-you-use-elisa-pcr-or-lfa-methods]
- 23. Research progress on detection methods for food allergens [https://www.sciencedirect.com/science/article/abs/pii/S0889157524009402]
- 24. A roadmap to high-speed polymerase chain reaction (PCR) [https://www.sciencedirect.com/science/article/pii/S0956566323007728]
- 25. Comparative evaluation of in-house ELISA and two ... [https://www.nature.com/articles/s41598-025-97050-y]
- 26. Comparison of eight commercial, high-throughput ... [https://pubmed.ncbi.nlm.nih.gov/32942137/]
- 27. Diagnostic Accuracy of ELISA versus Indirect ... [https://jccpractice.com/article/diagnostic-accuracy-of-elisa-versus-indirect-immunofluorescence-in-detecting-anti-nuclear-antibodies-among-suspected-connective-tissue-disorder-patients-1011/]
- 28. High Throughput Screening Market Forecast, 2025-2032 [https://www.coherentmarketinsights.com/industry-reports/high-throughput-screening-market]
- 29. Allergy Diagnostics Market Trends Analysis Report 2025- ... [https://finance.yahoo.com/news/allergy-diagnostics-market-trends-analysis-132800977.html]
- 30. Analysis of allergen positivity rates in relation to gender, ... [https://www.nature.com/articles/s41598-024-78909-y]
- 31. Top Allergen Detection Companies & How to Compare ... [https://www.linkedin.com/pulse/top-allergen-detection-companies-how-compare-them-wig2e]
- 32. Allergy diagnostic performance of FastCheckPOC 20 Atopy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592802/]
- 33. Advancements and Applications of Lateral Flow Assays ... [https://www.mdpi.com/1424-8220/25/17/5414]
- 34. US Lateral Flow Assays Market 2025 – 2034 [https://www.custommarketinsights.com/report/us-lateral-flow-assays-market/]
- 35. Lateral Flow Assay Test Market Size | Industry Trends [2034] [https://www.marketgrowthreports.com/market-reports/lateral-flow-assay-test-market-116700]
- 36. Review of Methods for the Detection of Allergens in Novel ... [https://science.food.gov.uk/article/125903-review-of-methods-for-the-detection-of-allergens-in-novel-food-alternative-proteins]
- 37. The Role of Allergen Testing in Safe Food Production [https://www.neogen.com/pt/usac/neocenter/blog/strengthening-food-safety-the-role-of-allergen-testing-in-safe-food-production/]
- 38. Rapid and accurate electrochemical sensor for food ... [https://www.nature.com/articles/s41598-021-00241-6]
- 39. A new way to fight allergies: Switch on the light [https://www.colorado.edu/today/2025/09/15/new-way-fight-allergies-switch-light]
- 40. The Magnitude and Impact of Food Allergens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11011628/]
- 41. How can AI Help With Food Allergen Detection and ... [https://allergenbureau.net/how-can-ai-help-with-food-allergen-detection-and-quantification/]
- 42. Review of allergen analytical testing methodologies [https://www.food.gov.uk/research/review-of-allergen-analytical-testing-methodologies-allergen-detection-methods-unbiased-literature-search]
- 43. Detection of Allergenic Proteins in Foodstuffs: Advantages ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8949930/]
- 44. Top Hyperspectral Imaging Tools for 2025 [https://flypix.ai/blog/hyperspectral-imaging-tools/]
- 45. A personalized food allergen testing platform on a cellphone [https://pmc.ncbi.nlm.nih.gov/articles/PMC3556560/]
- 46. Advances in Hyperspectral Imaging-Based Non ... [https://www.sciencedirect.com/science/article/pii/S2772375525007658]
- 47. Advances in Food Processing Techniques for Allergenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12651889/]
- 48. Allergens test kits [https://www.goldstandarddiagnostics.com/products/allergens.html]
- 49. Allergy Amulet [https://www.allergyamulet.com/]
- 50. bioMérieux invests in Allergen Alert, a startup resulting from its ... [https://www.biomerieux.com/us/en/who-we-are/company-news/allergen-alert-investment.html]
- 51. Top Food Allergen Detection Kit Companies & How to ... [https://www.linkedin.com/pulse/top-food-allergen-detection-kit-companies-how-compare-eamhc/]
- 52. The changing food allergen landscape in Europe calls for ... [https://www.sciencedirect.com/science/article/abs/pii/S0956713524006327]
- 53. A Critical Comparison between Flow-through and Lateral Flow... [https://pubmed.ncbi.nlm.nih.gov/31842439/]
- 54. Advances in Shellfish Allergy Therapy - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267385/]
- 55. Accuracy of immunoblotting assay for detection of specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5878026/]
- 56. Food Allergens Testing Information [https://www.thermofisher.com/us/en/home/industrial/food-beverage/food-beverage-learning-center/food-analytical-testing-information/food-allergens-testing-information.html]
- 57. Portable Device for Real-Time Allergen Detection [https://www.ai-futureschool.com/en/electronics/portable-device-for-real-time-allergen-detection.php]
- 58. Allergen Detection Kit Consumer Behavior Dynamics [https://www.datainsightsmarket.com/reports/allergen-detection-kit-987350]
- 59. Top Portable Food Allergen Sensor Companies & How to ... [https://www.linkedin.com/pulse/top-portable-food-allergen-sensor-companies-how-compare-yjlsc/]
- 60. UK FSA's review of main allergen detection methods [https://allergenbureau.net/uk-fsas-review-of-main-allergen-detection-methods/]
- 61. Portable Food Allergen Sensor in the Real World: 5 Uses ... [https://www.linkedin.com/pulse/portable-food-allergen-sensor-real-world-5-uses-qn4hf]
- 62. Food Allergen Testing Market [https://www.futuremarketinsights.com/reports/food-allergen-testing-market]
- 63. Portable Food Allergen Sensor 2025-2033 Analysis [https://www.archivemarketresearch.com/reports/portable-food-allergen-sensor-505236]
- 64. Food Allergen Analysis - Allergen Bureau [https://allergenbureau.net/food-allergens/food-allergen-analysis/]
- 65. Allergen Test Kits for Food Industry [https://www.hygiena.com/allergen-diagnostics-and-data-management]
- 66. New Rapid Test Method To Detect Milk Allergens In Food ... [https://allergenbureau.net/new-rapid-test-method-to-detect-milk-allergens-in-food-products/]
- 67. World's Fastest Consumer Food Allergen Sensor [https://tintash.com/portfolio/food-allergen-sensor/]
- 68. Food Allergen Testing Market Size and Forecast, 2025-2032 [https://www.coherentmarketinsights.com/market-insight/food-allergen-testing-market-5313]
- 69. Managing Food Allergies in Dining Establishments [https://pubmed.ncbi.nlm.nih.gov/40431476/]
- 70. How US Food Allergen Testing Works — In One Simple ... [https://www.linkedin.com/pulse/how-us-food-allergen-testing-works-one-simple-flow-r8dme/]
- 71. A Systematic Review of Food Allergy: Nanobiosensor and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7760337/]