Macronutrient Malabsorption in Research Populations: Mechanisms, Assessment, and Translational Applications
This article provides a comprehensive resource for researchers and drug development professionals navigating the complexities of macronutrient malabsorption.
Macronutrient Malabsorption in Research Populations: Mechanisms, Assessment, and Translational Applications
Abstract
This article provides a comprehensive resource for researchers and drug development professionals navigating the complexities of macronutrient malabsorption. It synthesizes current evidence on the pathophysiology of impaired digestion and absorption of fats, proteins, and carbohydrates across diverse research populations, including those with environmental enteropathy, inflammatory bowel disease, and pancreatic insufficiency. We detail a battery of established and emerging functional tests—from breath analyses to direct invasive procedures—evaluating their applicability, limitations, and standardization in research settings. The scope extends to troubleshooting common methodological pitfalls, optimizing nutritional status in study cohorts, and validating novel biomarkers against histological and clinical endpoints. Finally, we present a framework for the comparative analysis of malabsorption syndromes to inform the development of targeted nutritional and pharmacologic interventions, aiming to bridge the gap between basic science and clinical application.
Deconstructing Macronutrient Malabsorption: Pathophysiological Mechanisms and Research Populations
Technical Support Center
Welcome to the technical support center for research on macronutrient malabsorption. This resource provides troubleshooting guidance for experiments based on the Three-Phase Model of Nutrient Assimilation, designed to help you pinpoint the phase of disruption.
Troubleshooting Guides
Guide 1: Investigating Luminal Phase Disruption
- Q: We are observing inconsistent digestion of a lipid emulsion in our in vitro gut model. What could be the cause?
- A: Inconsistent luminal digestion often stems from variable enzyme activity or suboptimal physicochemical conditions.
- Checkpoints:
- Enzyme Activity: Assay the activity of your pancreatic lipase and colipase preparation. Ensure it is fresh and has not been subjected to freeze-thaw cycles that degrade activity.
- pH & Bile Salts: Verify the pH of your simulated intestinal fluid is consistently maintained at 6.5-7.0. Confirm the critical micellar concentration (CMC) of your bile salt mixture is being achieved and that the composition (e.g., taurocholate vs. glycocholate ratio) is physiologically relevant.
- Substrate Preparation: Ensure the lipid emulsion is homogenous and stable. Sonication time and power should be standardized.
Guide 2: Investigating Mucosal Phase Disruption
- Q: Our Caco-2 cell monolayer assays show high transepithelial electrical resistance (TEER) but unexpectedly low uptake of a glucose analog. What should we investigate?
- A: High TEER confirms barrier integrity, so the issue is likely with specific transport mechanisms, not paracellular leakage.
- Checkpoints:
- Transporter Expression: Confirm the expression and membrane localization of key transporters (e.g., SGLT1 for glucose) via Western blot or immunofluorescence. Passage number can affect differentiation and transporter profile.
- Competitive Inhibition: Check your assay buffer for compounds that might competitively inhibit your target transporter (e.g., phlorizin for SGLT1).
- Cellular Viability & Metabolism: Use an MTT or similar assay to rule out general cytotoxicity from your test compound that may be impairing active transport processes non-specifically.
Guide 3: Investigating Post-Absorptive Phase Disruption
- Q: In our rodent model, we detect nutrients in the portal blood but see no corresponding change in peripheral tissue (e.g., muscle) biomarkers of anabolism. Where is the blockage?
- A: The nutrient is absorbed but not utilized, indicating a post-absorptive defect.
- Checkpoints:
- Hepatic First-Pass Metabolism: The liver may be sequestering or metabolizing the nutrient before it reaches systemic circulation. Measure arterial vs. portal nutrient concentrations.
- Signaling Pathways: Analyze key anabolic signaling pathways in the target tissue (e.g., the Insulin/IGF-1 → PI3K/Akt pathway for protein synthesis). Phospho-specific antibodies can detect activation status.
- Systemic Hormones: Measure plasma levels of insulin, glucagon, and incretins (e.g., GLP-1). Dysregulation here can prevent nutrient partitioning to tissues.
Frequently Asked Questions (FAQs)
Q: What is the best biomarker to confirm a luminal phase defect for proteins?
- A: Fecal nitrogen or specific undigested protein fragments (measured via mass spectrometry) are direct markers. A rise in breath hydrogen after a protein meal can also indicate bacterial fermentation of undigested protein in the colon.
Q: How can we differentiate between a mucosal and a post-absorptive defect for carbohydrates?
- A: A combined oral glucose tolerance test (OGTT) with serum insulin measurement is key. A flat blood glucose curve with low insulin suggests a mucosal defect (impaired absorption). A rising blood glucose curve with low or absent insulin suggests a post-absorptive defect (pancreatic beta-cell dysfunction).
Q: Our drug candidate is intended to enhance fat absorption. Which phase-specific assays are most relevant for preclinical validation?
- A:
- Luminal: In vitro lipolysis model measuring fatty acid release over time.
- Mucosal: Caco-2 cell uptake assay for bile acid-micellized fatty acids.
- Post-Absorptive: In vivo study measuring post-prandial plasma triglycerides, chylomicron levels, and tissue-specific fatty acid uptake.
- A:
Experimental Data & Protocols
Table 1: Key Biomarkers for Phase-Specific Disruption in Macronutrient Malabsorption
| Phase | Macronutrient | Key Biomarkers of Disruption | Normal Range (Exemplary) | Disrupted Range |
|---|---|---|---|---|
| Luminal | Lipids | Fecal Fat Excretion | <7 g/24h | >7 g/24h |
| Proteins | Fecal Nitrogen | <2.0 g/24h | >2.5 g/24h | |
| Carbohydrates | Breath H2 | <20 ppm rise from baseline | >20 ppm rise | |
| Mucosal | All | D-Xylose Blood Test (5h) | >20 mg/dL | <20 mg/dL |
| Lipids | Serum Beta-Carotene | 50-250 µg/dL | Low | |
| Post-Absorptive | Proteins | Plasma Amino Acid Ratio (Val/Gly) | Stable Post-Prandial Rise | Blunted Response |
| Carbohydrates | Oral GTT (2h Glucose) | <140 mg/dL | Impaired |
Protocol 1: In Vitro Lipolysis Model to Assess Luminal Phase
- Prepare Simulated Intestinal Fluid (SIF): 150 mM NaCl, 5 mM Tris, 1.4 mM CaCl2, 3 mM NaTDC, 0.75 mM PC, pH 7.5.
- Add Substrate: Introduce your lipid formulation (e.g., 5 mg triglyceride) to the SIF.
- Initiate Digestion: Add pancreatic lipase/colipase solution (e.g., 1000 U/mL) to the mixture.
- Maintain pH: Use a pH-stat titrator to automatically add NaOH, maintaining pH 7.5. The volume of NaOH consumed is proportional to fatty acids released.
- Sample & Analyze: Take samples at timed intervals. Stop the reaction and quantify liberated fatty acids via gas chromatography or a colorimetric assay.
Protocol 2: Differentiated Caco-2 Cell Monolayer Uptake Assay
- Culture: Seed Caco-2 cells on Transwell inserts at high density. Culture for 21 days, changing media every 2-3 days. Monitor TEER until >500 Ω·cm².
- Prepare Uptake Buffer: Hank's Balanced Salt Solution (HBSS) with 10 mM HEPES, pH 7.4.
- Uptake Experiment: Aspirate culture media. Wash cells with uptake buffer. Add the test compound (e.g., C13-glucose) in buffer to the apical chamber.
- Incubate: Incubate at 37°C for a defined time (e.g., 15-60 min).
- Terminate & Quantify: Remove the apical solution and wash the monolayer with ice-cold buffer. Lyse the cells and analyze the lysate for transported compound using LC-MS/MS or a scintillation counter for radiolabeled compounds.
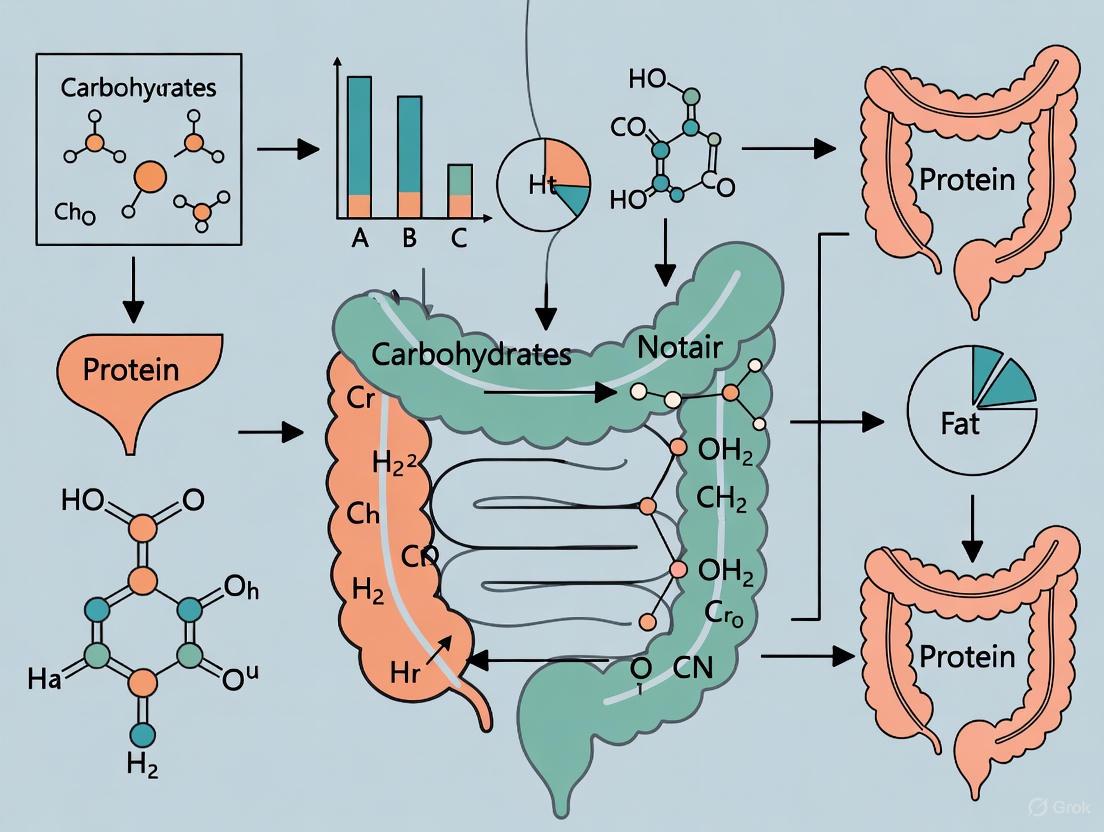
Pathway and Workflow Visualizations
Diagram: Luminal Digestion & Disruption
Diagram: Mucosal Uptake & Disruption
Diagram: Post-Absorptive Processing & Disruption
Diagram: Phase Disruption Diagnostic Workflow
The Scientist's Toolkit
Table 2: Research Reagent Solutions for Macronutrient Absorption Studies
| Reagent / Material | Function / Application |
|---|---|
| Porcine Pancreatin | A crude extract containing lipases, proteases, and amylases for simulating luminal digestion in in vitro models. |
| Taurocholic Acid Sodium Salt | A primary bile salt used to achieve physiologically relevant micelle formation for lipid solubilization. |
| Caco-2 Cell Line | A human colon adenocarcinoma cell line that spontaneously differentiates into enterocyte-like cells, forming a polarized monolayer for mucosal uptake and transport studies. |
| Transwell Permeable Supports | Inserts with a porous membrane used to culture Caco-2 cells, allowing separate access to apical and basolateral compartments. |
| D-[U-¹⁴C] Glucose | Radiolabeled glucose tracer used to quantitatively track carbohydrate uptake and transport in cellular and tissue models. |
| Electric Cell-Substrate Impedance Sensing (ECIS) | A real-time, label-free method to monitor cell barrier integrity (TEER) and cell behavior in culture. |
| Phospho-Akt (Ser473) Antibody | A key reagent for assessing activation of the PI3K/Akt pathway, a central regulator of post-absorptive nutrient utilization and anabolism. |
| Luminex Multiplex Assay Panels | For simultaneous measurement of multiple hormones (insulin, GLP-1, glucagon) from small volume plasma/serum samples to assess systemic post-absorptive signaling. |
FAQs: Core Concepts and Phenotype Differentiation
Q1: What is the fundamental difference between global and selective malabsorption in a research context?
A1: Global malabsorption involves the impaired absorption of almost all nutrients across multiple classes (fats, proteins, carbohydrates, vitamins, and minerals), typically resulting from conditions causing widespread mucosal damage or a significant reduction in absorptive surface area. In contrast, selective malabsorption is the isolated or specific malabsorption of a single nutrient or a limited array of nutrients, often due to a defect in a specific transporter, enzyme, or receptor [1] [2]. For example, celiac disease often presents as global malabsorption, while lactose intolerance, caused by lactase deficiency, is a classic example of selective carbohydrate malabsorption [3] [1].
Q2: What are the primary pathophysiological mechanisms a researcher should consider when modeling these phenotypes?
A2: Malabsorption can be categorized based on the disruption of one of the three phases of nutrient assimilation [3] [4] [5]:
- Luminal Phase (Maldigestion): Defective hydrolysis of nutrients. Causes include exocrine pancreatic insufficiency (e.g., chronic pancreatitis, cystic fibrosis), insufficient bile salt synthesis or secretion, and small intestinal bacterial overgrowth (SIBO) which deconjugates bile salts [3] [5] [6].
- Mucosal Phase (Malabsorption): Defects at the brush border membrane or within the enterocyte. This includes disorders like celiac disease and other enteropathies that damage the mucosa, congenital deficiencies of brush border enzymes (e.g., lactase), and specific defects in nutrient transporters [7] [3] [6].
- Post-Absorptive (Transport) Phase: Impairment in the delivery of absorbed nutrients via the lymphatic system or circulation. Conditions include intestinal lymphangiectasia, lymphoma, and abetalipoproteinemia [3] [6].
Q3: Which non-invasive functional tests are most suitable for phenotyping research populations, particularly in pediatric or field settings?
A3: Breath tests are increasingly favored for their non-invasive nature. Key examples include [7] [8]:
- Hydrogen Breath Tests: Used to diagnose specific carbohydrate intolerances (e.g., lactose, fructose) and Small Intestinal Bacterial Overgrowth (SIBO).
- ¹³C-Labeled Substrate Breath Tests: Can measure the absorption of carbohydrates (e.g., ¹³C-starch, ¹³C-sucrose), fats (e.g., ¹³C-mixed triglyceride), and proteins (using labeled dipeptides like benzoyl-L-tyrosyl-L-1-¹³C-alanine). These tests show promise for detecting subclinical malabsorption in conditions like environmental enteric dysfunction [8].
Troubleshooting Guides for Experimental Challenges
Challenge 1: Differentiating between pancreatic and mucosal causes of fat malabsorption in an animal model.
- Step 1 - Confirm Fat Malabsorption: Quantify fecal fat using a 72-hour stool collection while the subject is on a controlled diet (≥100 g fat/day). Fecal fat excretion >7 g/day confirms steatorrhea [4].
- Step 2 - Functional Testing:
- Direct Pancreatic Function: Measure fecal levels of pancreatic enzymes. Low fecal elastase or chymotrypsin is indicative of exocrine pancreatic insufficiency [4].
- Assess Mucosal Integrity/Absorption: The D-xylose absorption test can be used. Normal D-xylose absorption in the presence of steatorrhea points toward a pancreatic cause, whereas an abnormal result suggests mucosal disease [4].
- Step 3 - Histological Confirmation: A small intestinal biopsy remains the gold standard for identifying mucosal abnormalities such as villous atrophy, intraepithelial lymphocytes, or other enteropathies [7] [4].
Challenge 2: Inconsistent results from breath tests in a longitudinal cohort study.
- Potential Cause 1: Lack of standardized test protocols and subject preparation.
- Solution: Strictly control pre-test conditions: overnight fasting, avoidance of antibiotics and prokinetics before testing, use of standardized test meals, and consistent physical activity during the test [8].
- Potential Cause 2: Variable gastric emptying or small intestinal transit time.
- Solution: Consider dual-label isotope tests that can account for transit time or use study designs that allow each subject to serve as their own control.
- Potential Cause 3: Establishing appropriate, population-specific normative cut-off values.
- Solution: Conduct pilot studies to establish baseline values for your specific research population rather than relying on published values from different demographic or health groups [8].
Table 1: Characteristics of Global vs. Selective Malabsorption Phenotypes
| Feature | Global Malabsorption | Selective Malabsorption |
|---|---|---|
| Definition | Impaired absorption of multiple nutrients [1] | Impaired absorption of a single or limited nutrients [1] |
| Common Causes | Celiac disease, Crohn's disease, extensive mucosal damage, Short Bowel Syndrome [7] [3] [2] | Lactose intolerance (lactase deficiency), Pernicious anemia (B12), Abetalipoproteinemia [3] [1] [2] |
| Key Lab Findings | Steatorrhea, weight loss, deficiencies in iron (microcytic anemia), B12/folate (macrocytic anemia), vitamins A, D, E, K, hypoalbuminemia, hypocalcemia [4] [9] [2] | Findings specific to the deficient nutrient (e.g., iron deficiency anemia; osteoporosis from vitamin D malabsorption) [4] [2] |
| Primary Research Focus | Restoring mucosal integrity, nutritional support, managing underlying inflammatory disease [7] | Enzyme replacement, dietary modification, targeted nutrient delivery [9] |
Table 2: Key Functional Tests for Macronutrient Malabsorption Assessment
| Nutrient | Test Method | Experimental Protocol Summary | Interpretation & Key Considerations |
|---|---|---|---|
| Fat | 72-hour Fecal Fat Measurement [4] | 1. Subject consumes a controlled diet with 100g fat/day for 3 days.2. Collect all stool for 72 hours.3. Analyze total stool fat content. | Abnormal: >7g fat/24h. Gold standard but cumbersome. High values (≥40g/day) suggest pancreatic or severe mucosal disease. |
| Fat | ¹³C-Mixed Triglyceride Breath Test [8] | 1. Administer a test meal containing ¹³C-labeled mixed triglyceride.2. Collect breath samples at baseline and at regular intervals for up to 6 hours.3. Measure ¹³CO₂ enrichment. | Non-invasive proxy for pancreatic lipase activity. Requires standardization and population-specific cut-offs. |
| Carbohydrate | Hydrogen/Methane Breath Test [8] [9] | 1. After an overnight fast, administer a load of the specific carbohydrate (e.g., 25-50g lactose).2. Measure breath H₂/CH₄ at baseline and every 15-30 minutes for 2-5 hours. | A rise in H₂ ≥20 ppm from baseline indicates malabsorption. False negatives occur in non-H₂ producers; assess with lactulose. |
| Protein | Fecal Nitrogen [4] | Measure nitrogen content in a 72-hour stool collection. | Technically difficult and rarely used in clinical practice; research tool. |
| Protein | ¹³C-Dipeptide Breath Test [8] | Administer a labeled dipeptide (e.g., Benzoyl-L-tyrosyl-L-1-¹³C-alanine) and measure ¹³CO₂ in breath over time. | Non-invasive research method to assess peptide absorption and mucosal function. |
Experimental Protocols for Key Assessments
Protocol 1: D-Xylose Absorption Test for Mucosal Integrity Principle: D-xylose is a pentose sugar absorbed via passive diffusion that does not require pancreatic enzymes for digestion. Its absorption serves as a marker of proximal small intestinal mucosal integrity [4]. Procedure:
- The subject fasts overnight.
- A 25g dose of D-xylose is dissolved in 250-500 mL of water and administered orally.
- Blood is drawn at 1 hour post-administration. Alternatively, all urine is collected over a 5-hour period.
- Serum D-xylose or total urinary D-xylose excretion is measured. Interpretation:
- Abnormal: 1-hour serum level <20 mg/dL (1.33 mmol/L) or 5-hour urinary excretion <4 g [4].
- A normal result in the presence of steatorrhea suggests pancreatic insufficiency, while an abnormal result indicates mucosal disease or SIBO (as bacteria metabolize the D-xylose) [4].
Protocol 2: Serum Biomarkers for Nutritional Deficiencies in Malabsorption Research Principle: Widespread or specific nutrient malabsorption leads to measurable deficiencies in blood, serving as surrogate markers for the condition's severity and scope [4] [2]. Procedure:
- Collect a fasting blood sample from research subjects.
- Analyze for the following key biomarkers:
- Complete Blood Count (CBC) with indices: To detect microcytic (iron deficiency) or macrocytic (B12/folate deficiency) anemia [4] [2].
- Iron Studies (Ferritin), Vitamin B12, Folate: To confirm and specify deficiencies.
- Fat-Soluble Vitamins (A, D, E): Commonly low in fat malabsorption.
- Albumin, Prealbumin: Markers of protein-calorie nutrition and chronic deficiency.
- Calcium, Magnesium, Phosphate: May be low due to malabsorption or vitamin D deficiency.
- Prothrombin Time (PT): Prolonged in vitamin K deficiency [4] [9].
Diagnostic Pathway and Research Reagent Solutions
Diagram Title: Research Diagnostic Pathway for Malabsorption Phenotypes
Table 3: Research Reagent Solutions for Malabsorption Studies
| Reagent / Material | Primary Function in Research |
|---|---|
| ¹³C-Labeled Substrates (e.g., Mixed Triglyceride, Sucrose, Dipeptides) | Non-invasive probes for assessing the digestive and absorptive capacity of specific macronutrients via breath tests [8]. |
| D-Xylose | A carbohydrate probe used to assess the integrity of the small intestinal mucosa independently of pancreatic function [4]. |
| Hydrogen/Methane Breath Test Kits (Lactulose, Lactose, Fructose) | Diagnostic kits for detecting carbohydrate malabsorption and small intestinal bacterial overgrowth (SIBO) by measuring bacterial fermentation gases [8] [9]. |
| Fecal Fat Analysis Kits (Acid Steatocrit, Near-Infrared Reflectance Analysis - NIRA) | Quantitative and semi-quantitative methods for confirming steatorrhea in study subjects, with varying levels of practicality and precision [4]. |
| ELISA/Kits for Serological Markers (Anti-tTG, Anti-EMA for Celiac Disease) | Essential for screening and identifying specific etiologies of mucosal damage within study cohorts [7] [2]. |
| Endoscopy & Biopsy Forceps | Tools for obtaining gold-standard histopathological samples from the small intestinal mucosa to confirm and classify enteropathies [7] [4]. |
Pathophysiology and Key Etiologies of Fat Malabsorption
Fat malabsorption, or steatorrhea, occurs when the digestive system fails to properly process and absorb dietary fats. Normal fat absorption is a complex process that can be disrupted at several key stages: the luminal phase (digestion), the mucosal phase (absorption), and the post-absorptive phase (transport) [3] [4].
The table below summarizes the primary etiologies of fat malabsorption, categorized by the physiological phase they disrupt.
Table 1: Major Etiologies of Fat Malabsorption
| Physiological Phase | Underlying Mechanism | Specific Conditions |
|---|---|---|
| Luminal Phase (Digestion) [3] [10] | Impaired hydrolysis of triglycerides due to insufficient pancreatic enzyme activity or an unfavorable luminal environment. | Exocrine Pancreatic Insufficiency (EPI) from Chronic Pancreatitis, Cystic Fibrosis, Pancreatic Tumors, or Pancreatic Resection [3] [11] [10]. |
| Reduced bile acid synthesis or secretion, critical for micelle formation [3]. | Cholestatic Liver Disease, Cirrhosis, Small Intestinal Bacterial Overgrowth (SIBO) causing bile acid deconjugation [3] [4]. | |
| Mucosal Phase (Absorption) [3] | Damage to the intestinal mucosa, reducing the functional surface area for absorption. | Celiac Disease, Crohn's Disease, Environmental Enteropathy [3] [12]. |
| Post-Absorptive Phase (Transport) [3] | Defective packaging or transport of absorbed lipids via the lymphatic system. | Abetalipoproteinemia, Intestinal Lymphangiectasia [3]. |
Troubleshooting Guides & FAQs
Guide 1: Investigating Suspected Fat Malabsorption in a Pre-Clinical Model
Problem: An animal model presents with weight loss and diarrhea following a surgical procedure or dietary challenge. You suspect fat malabsorption.
Objective: Systematically identify the phase of fat absorption that is impaired.
Table 2: Troubleshooting Workflow for Fat Malabsorption
| Step | Investigation | Methodology / Assay | Interpretation of Key Results |
|---|---|---|---|
| 1. Confirm Steatorrhea | Quantitative Fecal Fat Analysis [4] | 72-hour stool collection while subject is on a controlled, high-fat diet (≥100 g/day). Measure total fecal fat. | Fecal fat >7 g/day confirms steatorrhea [4]. |
| 2. Localize the Defect | Differentiate Pancreatic vs. Mucosal Cause [4] | Fecal Elastase-1 (FE-1) Test [11] [13]. | Low FE-1 suggests Exocrine Pancreatic Insufficiency (EPI). Normal FE-1 points toward a mucosal or post-absorptive defect [4]. |
| 3. Identify Specific Etiology | Evaluate Mucosal Integrity & Function | Serum Blood Tests: Vitamin B12, Folate, Ferritin, Albumin [4]. | Microcytic anemia (iron deficiency) suggests proximal mucosal disease (e.g., Celiac). Low B12 can indicate terminal ileal disease or SIBO [4]. |
| Small Bowel Biopsy [4] | Histology can reveal villous atrophy (Celiac), lymphangiectasia, or other mucosal pathologies [3]. | ||
| Test for Carbohydrate Malabsorption | 13C-Substrate Breath Tests (e.g., 13C-Sucrose) [12]. | Abnormal results indicate generalized mucosal dysfunction, as seen in Environmental Enteropathy [12]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the most reliable non-invasive tests to differentiate pancreatic from intestinal causes of fat malabsorption in human studies?
The Fecal Elastase-1 (FE-1) test is the most widely used and reliable non-invasive test for this purpose. It is a simple, single-stool sample test that does not require discontinuation of pancreatic enzyme replacement therapy (PERT). A concentration of <200 μg/g is indicative of Exocrine Pancreatic Insufficiency (EPI), while a value of <15 μg/g demonstrates high sensitivity and specificity for severe EPI. A normal FE-1 value in the presence of steatorrhea strongly suggests a mucosal or post-absorptive etiology [11] [4] [13].
FAQ 2: Beyond classic pancreatic diseases, what other conditions should researchers consider as potential causes of EPI?
EPI can result from both pancreatic and non-pancreatic disorders. Key non-pancreatic causes include:
- Diabetes Mellitus
- Celiac Disease
- Inflammatory Bowel Disease (IBD)
- Post-Gastrointestinal Surgery (e.g., Gastrectomy): Disrupts neurohormonal signaling and causes pancreaticocibal asynchrony [11] [13].
- Advanced Age [11].
FAQ 3: In the context of environmental enteropathy (EE), which macronutrients are most likely to be malabsorbed, and what tests are suitable for field studies?
Available evidence suggests that lactose and fat malabsorption are more likely to occur in EE [12]. For field studies in pediatric populations, non-invasive 13C-breath tests are particularly suitable. These include the 13C-mixed triglyceride breath test for fat malabsorption and the 13C-sucrose or 13C-lactose breath tests for carbohydrate malabsorption. These tests are well-tolerated and provide a functional readout of digestive and absorptive capacity [12].
Experimental Protocols & The Scientist's Toolkit
Detailed Protocol: Fecal Fat Quantification (72-Hour Collection)
Principle: This is the gold-standard method to objectively confirm steatorrhea by directly measuring the amount of fat excreted in stool over a precise period while the subject consumes a standardized high-fat diet [4].
Materials:
- Pre-weighed, sealed, and labeled stool collection containers.
- Metabolic cage or dedicated collection system.
- Controlled diet with precisely measured fat content (≥100 g/day).
- Solvents and laboratory equipment for fat extraction (e.g., gravimetric analysis or near-infrared reflectance analysis).
Procedure:
- Diet Standardization: For 3 days prior to and throughout the 72-hour collection period, provide the subject with a controlled diet containing exactly 100 grams of fat per day.
- Stool Collection: Collect all stool produced over a continuous 72-hour period. Ensure immediate storage of collected samples at -20°C to prevent fat degradation and water loss.
- Homogenization and Analysis: Pool and thoroughly homogenize the entire 72-hour stool sample. Take a representative aliquot for fat analysis.
- Fat Extraction & Calculation: Perform fat extraction using a standard method (e.g., van de Kamer method). Calculate total fat content and express the result as grams of fat excreted per 24 hours.
- Interpretation: Fat excretion of >7 grams/24 hours is diagnostic of steatorrhea. Severe malabsorption (≥40 g/day) is often seen in pancreatic insufficiency or severe mucosal disease [4].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Investigating Fat Malabsorption
| Reagent / Material | Primary Function in Research | Specific Application Example |
|---|---|---|
| Fecal Elastase-1 (FE-1) ELISA Kit | To quantitatively measure pancreatic elastase levels in stool samples as a marker of exocrine pancreatic function [11] [13]. | Diagnosing and stratifying the severity of Exocrine Pancreatic Insufficiency (EPI) in animal models or human subjects. |
| 13C-Labeled Substrates (Mixed Triglyceride, Sucrose, Lactose) | To act as tracer molecules for non-invasive breath tests that assess digestive and absorptive function [12]. | Evaluating fat (13C-MTG) or carbohydrate (13C-sucrose) malabsorption in functional studies, especially in pediatric or field research settings. |
| D-Xylose | To assess the integrity of the small intestinal mucosa independently of pancreatic function [4]. | Differentiating between mucosal disease (abnormal D-xylose absorption) and pancreatic disease (normal D-xylose absorption) in the presence of steatorrhea. |
| Pancreatic Enzyme Replacement Therapy (PERT) | To provide exogenous digestive enzymes (lipase, protease, amylase) and rescue fat malabsorption in experimental models [11]. | Conducting therapeutic intervention studies to confirm an EPI diagnosis and evaluate the efficacy of new treatments. |
Diagnostic and Pathophysiological Visualizations
Diagram 1: Diagnostic decision tree for fat malabsorption.
Diagram 2: Key pathophysiological phases of fat absorption.
FAQs and Troubleshooting Guide
Q1: Why do my hydrogen breath test results show high hydrogen levels, yet the volunteer reports no gastrointestinal symptoms?
A: This is a common finding and underscores the crucial difference between malabsorption and intolerance [14]. Malabsorption is a biochemical phenomenon confirmed by diagnostic tests, while intolerance is the clinical manifestation of symptoms [14]. A significant proportion of individuals (up to 50% for fructose and sorbitol) are asymptomatic "malabsorbers" [14]. Symptom development depends on factors beyond bacterial gas production, including:
- Colonic Microbiome Composition: The specific bacterial species present and their metabolic pathways (e.g., hydrogen vs. methane production) influence symptoms [14].
- Visceral Hypersensitivity: Some individuals have a heightened sensitivity to gut distension from gas and osmotic load [14].
- Intestinal Motility: Rapid transit may exacerbate diarrhea, while slower transit could increase fermentation time and gas-related symptoms [3].
Q2: How can I distinguish between SIBO and a primary enzyme deficiency as the cause of carbohydrate malabsorption in my study participants?
A: Differentiation is critical for directing appropriate therapy. The clinical presentation can overlap, but key diagnostic features can help distinguish them [3]:
- Pattern on Hydrogen Breath Test: SIBO often produces an early peak (e.g., within 60-90 minutes) in hydrogen concentration as the substrate is fermented prematurely in the small intestine. A primary deficiency typically shows a later peak as the carbohydrate reaches the colon [3].
- Response to a Lactulose Breath Test: Lactulose is not absorbed in the small intestine. A double peak (small intestinal and colonic) on the lactulose test is suggestive of SIBO [3].
- Underlying Risk Factors: A history of abdominal surgery, motility disorders, or proton pump inhibitor use supports a SIBO diagnosis [3].
- Broad Symptom Profile: SIBO can cause fat malabsorption (steatorrhea) and vitamin B12 deficiency due to bacterial consumption, which is not typical of isolated enzyme deficiencies [3].
Q3: What are the primary limitations of the hydrogen breath test, and how can I mitigate them in my research protocol?
A: The hydrogen breath test, while non-invasive, has several limitations that must be controlled for in rigorous research [14] [15]:
- Non-Hydrogen Producers: An estimated 2-20% of the population has a microbiome that produces little to no hydrogen, leading to false-negative results. Mitigation: Include a concomitant lactulose challenge to confirm the presence of hydrogen-producing bacteria. Consider measuring methane (CH4) in addition to hydrogen, as some individuals are methanogenic producers [14].
- False-Positive Results: These can occur due to small intestinal bacterial overgrowth (SIBO) or orocecal transit time that is excessively rapid or slow. Mitigation: A standardized pre-test diet (low-fermentable carbohydrates for 24 hours) and an overnight fast are essential to reduce baseline hydrogen levels [15].
- Lack of Standardization: Test dose, formulation, and duration can vary. Mitigation: Adhere to published consensus guidelines (e.g., Rome Consensus Conference) for dosage (e.g., 25g fructose, 50g lactose) and test duration (typically 3-4 hours) [15].
Q4: Our dietary intervention for fructose malabsorption is failing. Could other FODMAPs be influencing the results?
A: Absolutely. A common pitfall in dietary intervention studies is focusing on a single sugar in isolation. The gut absorbs and ferments multiple carbohydrates simultaneously, and they interact [14] [16]. For example, the presence of glucose enhances fructose absorption via the GLUT2 transporter, while sorbitol competitively inhibits the GLUT5 transporter, thereby exacerbating fructose malabsorption [14]. A successful dietary intervention must account for the total "fermentable load" and consider a comprehensive low-FODMAP approach, at least initially, to establish a baseline response.
Key Experimental Protocol: Hydrogen/Methane Breath Test
The hydrogen breath test is the primary non-invasive method for detecting carbohydrate malabsorption [14] [15].
Detailed Methodology:
Pre-Test Preparation:
- Volunteers must fast for a minimum of 12 hours prior to testing (water is permitted) [15].
- Avoid antibiotics, probiotics, and laxatives for at least 4 weeks before the test [14].
- No smoking or vigorous exercise on the test day, as this can affect gut motility and hydrogen production.
- A low-fermentable carbohydrate dinner is recommended the night before.
Baseline Breath Sample:
- Collect a baseline (time 0) end-expiratory breath sample using a standardized breath bag or hand-held analyzer to measure fasting hydrogen and methane levels.
Test Substrate Administration:
- Administer the test sugar dissolved in 250 mL of water. Common research doses are:
- Note: For fructose malabsorption testing, simultaneous measurement of blood glucose is recommended to rule out hereditary fructose intolerance, which can cause dangerous hypoglycemia [14].
Post-Ingestion Sampling:
- Collect subsequent breath samples every 15-30 minutes for a period of 3 to 4 hours [15].
- Volunteers should record the onset of any symptoms (bloating, pain, diarrhea) and their severity on a standardized scale at each time point.
Interpretation of Results:
- Positive for Malabsorption: An increase in hydrogen of > 20 parts per million (ppm) over the baseline value at any time point is considered diagnostic of malabsorption [15].
- Methane Production: An increase in methane of > 10 ppm over baseline is also considered significant [14].
- Clinical Correlation: A positive test must be correlated with the volunteer's symptom log to diagnose carbohydrate intolerance.
Quantitative Data on Carbohydrate Malabsorption
The prevalence of carbohydrate malabsorption varies significantly by type of sugar, dose, and population ethnicity [14].
Table 1: Prevalence of Carbohydrate Malabsorption in Response to Test Doses
| Sugar | Test Dose | Prevalence of Malabsorption | Key Population Notes |
|---|---|---|---|
| Lactose | 50 g | 70% - 100% in parts of Asia, Africa, Southern Europe [14] | Prevalence follows a north-south gradient in Europe; <10% in Scandinavia [14]. |
| Fructose | 25 g in 250 mL water | ~40% [14] | Dose-dependent; rate increases with higher doses [14]. |
| 50 g in 250 mL water | 60% - 70% [14] | ||
| Sorbitol | 10 g | Up to 100% [14] | Poorly absorbed by passive diffusion in most individuals [14]. |
Table 2: Comparison of Primary Carbohydrate Malabsorption Disorders
| Disorder | Defective Mechanism | Primary Site of Dysfunction | Key Diagnostic Method |
|---|---|---|---|
| Lactose Intolerance | Deficiency of lactase enzyme (LPH) [15] | Small intestinal brush border [3] | Hydrogen breath test, Lactose tolerance test [15] |
| Fructose Malabsorption | Deficiency/ dysfunction of GLUT5 transporter [14] | Small intestinal enterocyte membrane [3] | Hydrogen breath test with concurrent blood glucose measurement [14] |
| Sucrase-Isomaltase Deficiency | Deficiency of sucrase-isomaltase (SI) complex [3] | Small intestinal brush border [3] | Breath test or enzymatic assay from intestinal biopsy [3] |
Pathway and Workflow Visualizations
Carbohydrate Digestion & Malabsorption Pathway
Diagnostic Workflow for Malabsorption
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Carbohydrate Malabsorption Research
| Research Reagent / Material | Function / Application in Research |
|---|---|
| Lactulose | A non-absorbable disaccharide used as a positive control in breath testing to confirm the presence of hydrogen-producing colonic bacteria and to assess orocecal transit time [14]. |
| 13C-Labeled Substrates (e.g., 13C-lactose, 13C-sucrose) | Stable isotope-labeled compounds used in 13C-breath tests. The measurement of 13CO2 in breath provides an alternative, non-radioactive method to assess carbohydrate digestion and absorption [8]. |
| Test Carbohydrates (Pharmaceutical Grade) | High-purity lactose, fructose, sorbitol, and glucose are essential for standardized oral challenges and hydrogen breath tests to ensure consistent and reproducible dosing [14] [15]. |
| Hydrogen & Methane Breath Analyzer | A gas chromatograph or specialized handheld device for the quantitative, high-frequency measurement of hydrogen (H2) and methane (CH4) concentrations in end-expiratory breath samples [14]. |
| Standardized Symptom Questionnaires | Validated instruments (e.g., visual analogue scales, Likert scales) for the quantitative and systematic recording of abdominal pain, bloating, flatulence, and stool consistency during challenge tests to correlate with biochemical findings [15]. |
| Modular Diet Components | Pre-defined, chemically controlled meals or formula diets (e.g., low-FODMAP, lactose-free, fructose-restricted) for conducting controlled dietary intervention studies to assess the efficacy of elimination diets [14]. |
Protein Malabsorption and Amino Acid Transport Dysfunction
Frequently Asked Questions (FAQs)
Q1: What are the primary clinical signs that suggest a patient or research model is experiencing protein malabsorption?
Initial signs often resemble general indigestion, including abdominal bloating, gas, and diarrhea [9]. Over time, symptoms progress to those of protein undernutrition and amino acid deficiency, such as unintentional weight loss, muscle wasting (sarcopenia), edema (swelling due to fluid), and easy bruising [9]. Laboratory findings may include hypoalbuminemia (low serum albumin) and generalized malnutrition [17] [18].
Q2: What are the main mechanisms that lead to protein malabsorption?
The causes can be organized by the phase of digestion and absorption they disrupt:
- Luminal Phase (Impaired Digestion): Defects in the initial breakdown of proteins. Causes include Exocrine Pancreatic Insufficiency (EPI) (deficiency of proteases like trypsin) from chronic pancreatitis, cystic fibrosis, or pancreatic resection [3] [18]. Inactivation of pancreatic enzymes from gastric hypersecretion (e.g., Zollinger-Ellison syndrome) is another cause [18].
- Mucosal Phase (Impaired Absorption): Defects at the level of the small intestinal lining. This includes damage to the mucosal surface from celiac disease, Crohn's disease, or infectious enteropathies, which reduces the absorptive surface area [9] [3]. It also encompasses specific defects in amino acid transporter systems themselves [19] [18].
- Post-Absorptive Phase (Impaired Transport): Obstruction of the lymphatic system (e.g., intestinal lymphangiectasia, lymphoma) can impair the transport of absorbed nutrients, leading to protein-losing enteropathy [3] [18].
Q3: What are some specific genetic disorders of amino acid transport, and which transporters do they affect?
Several inherited disorders are linked to specific amino acid transporter defects. The table below summarizes key examples [19].
Table 1: Inherited Disorders of Amino Acid Transport
| Disorder Name | Gene / Transporter | SLC Family | Main Clinical Manifestations |
|---|---|---|---|
| Lysinuric Protein Intolerance | SLC7A7 (y+LAT-1) | SLC7 | Inability to digest proteins, diarrhea, vomiting, hyperammonemia after meals. |
| Hartnup Disorder | SLC6A19 (B⁰AT1) | SLC6 | Pellagra-like photosensitive rash, cerebellar ataxia, aminoaciduria. |
| Cystinuria | SLC3A1 (rBAT) & SLC7A9 (b⁰⁺AT) | SLC3 / SLC7 | Formation of cystine stones in the kidneys. |
| Iminoglycinuria | SLC6A20 (SIT1) or SLC36A2 (PAT2) | SLC6 / SLC36 | Typically benign, excessive glycine and proline in urine. |
Q4: How is amino acid transport across the Blood-Brain Barrier (BBB) relevant to neurological disorders?
The BBB tightly regulates the brain's environment. Amino acid transporters at the BBB are essential for providing precursors for neurotransmitters and antioxidants. Dysfunction of these transporters is linked to abnormalities in amino acid levels, which have been implicated in the pathophysiology of conditions like schizophrenia, autism spectrum disorder, and Huntington's disease. For instance, a deficiency in L-Cysteine transport can limit the production of the critical antioxidant glutathione, leading to oxidative stress in the central nervous system [20].
Q5: What is the role of SLC7 transporters in metabolic disease and diabetes pathophysiology?
The SLC7 family, particularly LAT1 (SLC7A5), transports large neutral amino acids (LNAAs) like branched-chain amino acids (BCAAs). Alterations in the expression or function of these transporters are implicated in insulin resistance and Type 2 Diabetes (T2D). Elevated plasma BCAA levels, a common finding in T2D, are thought to arise from and contribute to dysregulated mTOR signaling, a key pathway in insulin action [21]. This can lead to impaired glucose uptake in skeletal muscle cells [21].
Experimental Protocols & Methodologies
Protocol for Diagnosing Protein Malabsorption in a Clinical Research Setting
Aim: To systematically identify and confirm protein malabsorption and differentiate its causes in a study population.
Methodology:
- Initial Screening:
- Blood Tests:
- Stool Tests:
- Fecal Fat Content (72-hour collection): Since fat malabsorption frequently accompanies protein malabsorption, this is a key test. Healthy individuals excrete <7g fat per day on a 100g fat diet [17].
- Fecal Elastase or Chymotrypsin: Low levels indicate Exocrine Pancreatic Insufficiency (EPI) as a likely cause [17].
Functional and Mucosal Integrity Tests:
- D-Xylose Test: This test assesses mucosal integrity. Abnormal absorption suggests a mucosal problem rather than a pancreatic one [17].
- Breath Tests:
- Hydrogen Breath Test: Used to diagnose carbohydrate malabsorption (e.g., lactose intolerance) and small intestinal bacterial overgrowth (SIBO), which can contribute to general malabsorption [9] [17].
- ¹³C-Di-peptide Breath Test: An emerging, non-invasive method to directly assess protein/peptide absorption. The test uses a synthetic dipeptide labeled with ¹³C (e.g., Benzoyl-L-tyrosyl-L-1-¹³C-alanine). Upon absorption and metabolism, ¹³CO₂ is exhaled and measured, with lower levels indicating malabsorption [8].
Definitive Diagnosis:
- Upper Endoscopy with Duodenal Biopsy: The gold standard for diagnosing mucosal diseases. Histologic examination of biopsied tissue can confirm celiac disease, tropical sprue, Whipple's disease, and other infiltrative or inflammatory conditions [17].
The following workflow diagram illustrates the diagnostic pathway for protein malabsorption.
Protocol for Investigating Amino Acid Transporter Function in Cell Models
Aim: To characterize the function and kinetics of a specific amino acid transporter in a cultured cell line.
Methodology:
- Cell Culture: Use an appropriate cell model (e.g., Caco-2 for intestinal transport, HEK293 for heterologous expression). Culture cells to confluence on multi-well plates or permeable filter supports (for transepithelial transport studies).
- Uptake Assay:
- Prepare an uptake buffer containing a radiolabeled (e.g., ¹⁴C, ³H) or stable isotope-labeled amino acid of interest.
- Wash cells with a pre-warmed buffer.
- Initiate uptake by adding the labeled amino acid solution to the cells for a defined time (e.g., 1-10 minutes). Incubate at 37°C.
- Include control conditions with an excess of unlabeled amino acid to measure non-specific transport and determine carrier-mediated uptake.
- Terminate the reaction by rapid removal of the uptake solution and washing with an ice-cold buffer.
- Quantification:
- For radiolabeled amino acids, lyse the cells and measure the accumulated radioactivity using a scintillation counter.
- For stable isotopes, use mass spectrometry to quantify the accumulated label.
- Kinetic Analysis: Repeat the uptake assay with a range of amino acid concentrations. Plot the uptake rate (V) against substrate concentration ([S]) and fit the data to the Michaelis-Menten equation (V = Vₘₐₓ * [S] / (Kₘ + [S])) to determine the transporter's affinity (Kₘ) and maximum transport capacity (Vₘₐₓ).
Research Reagent Solutions
This table lists key reagents and tools used in the study of amino acid transporters and protein absorption.
Table 2: Essential Research Reagents for Amino Acid Transport Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Stable Isotope-Labeled Amino Acids (e.g., ¹³C, ¹⁵N) | Tracing amino acid uptake, metabolism, and flux in vitro and in vivo. | ¹³C-dipeptide breath test in human subjects [8]; kinetic uptake assays in cell culture. |
| Radiolabeled Amino Acids (e.g., ³H, ¹⁴C) | High-sensitivity detection for quantitative measurement of transporter kinetics. | Classic cell-based uptake assays to determine Kₘ and Vₘₐₓ. |
| Specific Transporter Inhibitors | Pharmacologically blocking specific transporter systems to elucidate function. | Using BCH (2-aminobicyclo[2.2.1]heptane-2-carboxylic acid) to inhibit System L (LAT1/SLC7A5) transport. |
| cDNA Plasmids for SLC Transporters | Heterologous expression of transporters in model cell lines (e.g., HEK293, Xenopus oocytes). | Functional characterization of a wild-type vs. mutant transporter gene [19]. |
| Anti-SLC Transporter Antibodies | Detecting protein expression, localization, and quantification via Western Blot, Immunofluorescence. | Confirming plasma membrane localization of LAT1 in cancer cell lines. |
| Permeable Filter Supports (e.g., Transwell) | Modeling polarized epithelial transport and barrier function. | Measuring transepithelial flux of amino acids across a Caco-2 cell monolayer. |
Signaling Pathways & Metabolic Context
Amino acid transporters are not just conduits for nutrients; they are critical signaling nodes. The SLC7 family, particularly the SLC3A2-SLC7A5 heterodimer (LAT1), transports branched-chain amino acids (BCAAs) like leucine, which activate the mTORC1 signaling pathway. This pathway is a central regulator of cell growth, proliferation, and metabolism. The following diagram illustrates this key signaling relationship and its implication in insulin resistance.
Troubleshooting Guides and FAQs
Q: What are the key differences in intestinal permeability assessment methods between EE, IBD, and celiac disease models?
A: Intestinal permeability assessment requires method optimization for each condition:
Lactulose-Mannitol Test Issues:
- False positives in EE: Address by controlling for tropical enteropathy confounding factors
- IBD variability: Time testing relative to flare activity
- Celiac specificity: Combine with gluten challenge protocols
Ussing Chamber Technical Problems:
- Tissue viability maintenance during transport
- Mounting orientation consistency
- Solution osmolarity calibration
Q: How do I optimize organoid cultures from different disease biopsies?
A: Disease-specific optimization is critical:
Environmental Enteropathy:
- Problem: Poor crypt survival from malnourished tissue
- Solution: Pre-condition with lipid-enriched media for 48 hours
IBD-derived Organoids:
- Problem: Inflammatory cytokine interference
- Solution: Add TNF-α inhibitors during initial establishment
Post-surgical Tissue:
- Problem: Fibrotic tissue contamination
- Solution: Implement longer collagenase digestion (90 minutes)
Table 1: Macronutrient Absorption Markers in Disease Populations
| Disease State | Fecal Fat (g/24h) | D-Xylose Absorption (g/5h) | Serum Albumin (g/dL) | Citrulline (μmol/L) |
|---|---|---|---|---|
| Healthy Controls | <7 | >4.5 | 3.5-5.0 | 30-45 |
| Environmental Enteropathy | 8-15 | 2.5-4.0 | 2.8-3.5 | 15-28 |
| Active IBD | 10-25 | 1.8-3.5 | 2.5-3.8 | 10-25 |
| Celiac Disease (Untreated) | 9-18 | 2.0-3.8 | 2.9-3.9 | 18-30 |
| Post-Surgical (Short Bowel) | 15-40 | 1.0-2.5 | 2.2-3.2 | 8-20 |
Table 2: Barrier Function Parameters Across Conditions
| Parameter | Normal Range | EE | IBD | Celiac | Post-Surgical |
|---|---|---|---|---|---|
| TEER (Ω·cm²) | >50 | 25-40 | 20-35 | 30-45 | 15-30 |
| FITC-Dextran Flux (μg/ml) | <0.5 | 0.8-2.5 | 1.2-4.0 | 0.9-2.8 | 1.5-5.0 |
| Zonulin (ng/ml) | <50 | 65-120 | 80-200 | 70-150 | 60-110 |
Experimental Protocols
Protocol 1: Dual-Sugar Absorption Test for Field Studies
Purpose: Assess intestinal permeability in resource-limited settings Materials:
- Lactulose and mannitol solutions
- Urine collection containers
- HPLC system with refractive index detector
Procedure:
- Administer oral dose (5g lactulose + 2g mannitol in 100ml water)
- Collect urine over 5-hour period
- Preserve with thymol crystals
- Analyze sugar concentrations via HPLC
- Calculate L:M ratio (normal <0.03)
Troubleshooting:
- Incomplete urine collection: Use para-aminobenzoic acid as recovery marker
- Bacterial degradation: Add chlorhexidine to collection containers
Protocol 2: Ex Vivo Mucosal Healing Assay
Purpose: Quantify epithelial repair mechanisms Materials:
- IBD patient-derived colonoids
- Electric cell-substrate impedance sensing (ECIS) system
- Wounding electrodes
Procedure:
- Seed colonoids in ECIS arrays (20,000 cells/well)
- Grow to confluence (TER >1000 Ω)
- Apply wounding pulse (30 seconds, 3000 μA)
- Monitor resistance recovery every 5 minutes for 48 hours
- Calculate healing rate from recovery curve slope
Pathway Diagrams
Title: Nutrient Absorption Disruption Pathway
Title: Tight Junction Regulation Pathway
The Scientist's Toolkit
Table 3: Essential Research Reagents
| Reagent | Function | Application |
|---|---|---|
| FITC-dextran 4kDa | Paracellular permeability tracer | Barrier function assays |
| Human zonulin ELISA | Tight junction regulator quantification | EE and celiac research |
| Citrulline assay kit | Enterocyte mass marker | Absorption capacity assessment |
| Ussing chamber system | Electrophysiology measurement | Transepithelial resistance |
| Organoid culture matrix | 3D growth support | Patient-derived models |
| Cytokine multiplex panel | Inflammatory profile | IBD mechanism studies |
| Stable isotope nutrients | Metabolic trafficking | Absorption pathway mapping |
Troubleshooting Common SIBO Research Challenges
FAQ 1: How can I distinguish between SIBO and other malabsorption syndromes in a research setting?
SIBO presents a diagnostic challenge due to symptom overlap with other malabsorption syndromes. The key is to identify the unique etiological factors and diagnostic patterns of SIBO. Table 1 outlines the primary diagnostic approaches and their research considerations [22] [23].
Table 1: Diagnostic Methods for SIBO in Research Populations
| Method | Procedure | Research Advantages | Research Limitations |
|---|---|---|---|
| Jejunal Aspirate & Culture | Endoscopic collection of small intestinal fluid with quantitative culture (>10³ CFU/mL diagnostic) | Considered historical gold standard; allows bacterial identification | Invasive, expensive, risk of oropharyngeal contamination, poorly reproducible [22] |
| Glucose Breath Test | Oral administration of 50-75g glucose solution with breath hydrogen/methane measurement | High specificity (less colonic fermentation) | May miss distal SIBO (false negatives); sensitivity 20-93%, specificity 45-86% [22] [24] |
| Lactulose Breath Test | Oral administration of 10g lactulose solution with breath hydrogen/methane measurement | Identifies SIBO throughout entire small intestine | Potential for false positives from rapid transit; sensitivity 17-68%, specificity 44-86% [22] [24] |
| Supportive Laboratory Findings | Measurement of B12, folate, fat-soluble vitamins, nutritional markers | Non-invasive, indicates functional consequences | Non-specific; can be normal in early disease [22] [25] |
FAQ 2: What are the most common confounding variables in SIBO comorbidity research, and how can they be controlled?
Several confounding variables can complicate SIBO research. Motility disorders (diabetes, scleroderma), anatomical abnormalities (small intestinal diverticula, surgical blind loops), and medications (PPIs, narcotics) strongly associate with SIBO [22] [25] [26]. Control strategies include: (1) Detailed participant stratification based on comorbid conditions; (2) Standardized medication documentation and analysis; (3) Pre-study fasting and dietary controls to minimize test variability [24].
FAQ 3: Why might SIBO treatment protocols fail in research populations with significant comorbidities?
Treatment failure often stems from unaddressed underlying mechanisms. Key reasons include: (1) Persistent dysmotility not managed with prokinetics; (2) Anatomical defects requiring surgical intervention; (3) Biofilm formation requiring sequential or combination therapies; (4) Methane-dominant SIBO (IMO) requiring different antibiotic regimens [22]. Complex comorbidities like scleroderma, Crohn's disease, and immunodeficiency disorders often require simultaneous management of the underlying condition for successful SIBO eradication [22] [25].
Essential Experimental Protocols for SIBO Research
Hydrogen/Methane Breath Testing Protocol
Principle: Bacterial fermentation of carbohydrates produces hydrogen and methane gases, which are absorbed and exhaled [24].
Materials: Breath test kit (collection tubes, labels), substrate (lactulose or glucose), timing device, breath analyzer.
Procedure:
- Pre-Test Preparation (4 weeks prior): Complete any antibiotic courses [24].
- One Week Pre-Test: Discontinue prokinetics and laxatives if tolerated (consult physician) [24].
- 24-Hour Prep Diet: Avoid complex carbohydrates and fermentable foods. Consume only plain meat, fish, eggs, white rice, clear fluids [24] [27].
- 12-Hour Fast: Overnight fast with only water permitted [24] [27].
- Test Day: Avoid smoking and physical activity [24].
- Baseline Sample: Collect initial breath sample.
- Substrate Ingestion: Drink sugar solution (10g lactulose or 50-75g glucose).
- Timed Sampling: Collect breath samples every 20 minutes for 3 hours (total 10 samples) [27].
- Sample Analysis: Measure hydrogen and methane concentrations.
Interpretation: Positive test defined as (1) Rise in hydrogen ≥20 ppm from baseline within 90 minutes, OR (2) Methane level ≥10 ppm at any point [22].
Jejunal Aspirate Culture Protocol
Principle: Direct quantification of bacterial load in small intestinal contents [22].
Materials: Sterile endoscope, protected specimen brush or aspiration catheter, anaerobic and aerobic transport media, culture plates.
Procedure:
- Pre-Procedure: Overnight fast with clear liquids only.
- Endoscopic Collection: Advance endoscope to distal duodenum/proximal jejunum.
- Aspiration: Use sterile catheter to collect 2-3mL of intestinal fluid.
- Transport: Immediately place sample in anaerobic transport media.
- Processing: Serial dilutions and culture on selective media.
- Quantification: Count colony-forming units after 48-72 hours incubation.
Interpretation: >10³ CFU/mL indicates SIBO. >10⁵ CFU/mL confirms diagnosis [22] [26].
SIBO and Systemic Inflammation: Pathophysiological Pathways
The relationship between SIBO and systemic inflammation involves multiple interconnected pathways that contribute to macronutrient malabsorption. The following diagram illustrates these key mechanisms:
Key Pathophysiological Mechanisms:
Direct Mucosal Injury: Bacterial endotoxins and metabolites damage epithelial tight junctions, increasing intestinal permeability and allowing bacterial translocation into systemic circulation [22] [26].
Nutrient Competition and Malabsorption: Bacteria compete for nutrients, particularly vitamin B12, iron, and thiamine, leading to deficiencies despite adequate intake [22] [28].
Metabolic Consequences: Bacterial deconjugation of bile salts impairs micelle formation, causing fat malabsorption and steatorrhea. Carbohydrate fermentation produces excess gas and osmotic diarrhea [22] [25].
Inflammatory Cascade Activation: Bacterial translocation triggers immune responses with increased pro-inflammatory cytokines (TNF-α, IL-6, IL-8), contributing to systemic inflammation [26].
Research Reagent Solutions for SIBO Investigation
Table 2: Essential Research Reagents for SIBO and Malabsorption Studies
| Reagent/Category | Specific Examples | Research Application | Considerations for Comorbid Populations |
|---|---|---|---|
| Breath Test Substrates | Lactulose, Glucose | Non-invasive SIBO diagnosis | Lactulose detects distal SIBO; glucose has higher specificity but may miss distal SIBO [24] |
| Culture Media | MacConkey agar, Blood agar, Selective anaerobic media | Bacterial quantification from aspirates | Essential for antibiotic sensitivity testing; anaerobic culture crucial [22] |
| Antibiotic Agents | Rifaximin, Neomycin, Metronidazole, Ciprofloxacin | SIBO eradication studies | Rifaximin (1650mg/day) for hydrogen; combo therapy for methane; consider resistance patterns [22] |
| Nutritional Assays | Vitamin B12, folate, fat-soluble vitamins (A,D,E,K), iron studies | Assessment of malabsorption | SIBO typically shows low B12 but elevated folate; multiple deficiencies indicate severity [22] [25] |
| Inflammatory Markers | Cytokine panels (TNF-α, IL-6, IL-8), fecal calprotectin, intestinal fatty-acid binding protein (I-FABP) | Quantification of systemic inflammation | Limited evidence for fecal calprotectin in SIBO; novel biomarkers needed [23] |
| Motility Assessment | Lactulose hydrogen breath test for orocecal transit time, SmartPill | Evaluation of underlying dysmotility | Critical for comorbid conditions like diabetes and scleroderma [22] [26] |
Advanced Research Considerations for Complex Comorbidities
FAQ 4: How do SIBO research approaches differ between hydrogen-dominant and methane-dominant variants?
Methane-dominant SIBO (also termed Intestinal Methanogen Overgrowth) represents a distinct research entity with different treatment responses and clinical implications [22]. Table 3 highlights these critical differences.
Table 3: Comparative Analysis of SIBO Variants in Research Populations
| Characteristic | Hydrogen-Dominant SIBO | Methane-Dominant SIBO |
|---|---|---|
| Primary Gas | Hydrogen (H₂) | Methane (CH₄) |
| Microbial Origin | Facultative anaerobes (E. coli, Klebsiella) | Archaea (Methanobrevibacter smithii) |
| Breath Test Threshold | ≥20 ppm H₂ rise from baseline | ≥10 ppm CH₄ at any time point [22] |
| Dominant Symptoms | Diarrhea, abdominal pain, bloating | Constipation, bloating, gas retention |
| First-Line Treatment | Rifaximin 1650mg/day for 14 days | Rifaximin 1650mg/day + Neomycin 1000mg/day for 14 days [22] |
| Research Implications | More responsive to single antibiotic therapy | Requires combination therapy; higher relapse rates |
FAQ 5: What specialized methodologies are needed for SIBO research in populations with neuropsychiatric comorbidities?
Emerging research indicates complex gut-brain axis interactions in SIBO. Patients with psychiatric disorders show altered tryptophan metabolism through the kynurenine pathway, potentially contributing to neurological symptoms [29]. Essential methodologies include: (1) Mass spectrometry for tryptophan metabolite quantification; (2) Intestinal permeability assessment (lactulose-mannitol test); (3) Fecal microbiome analysis with 16S rRNA sequencing; (4) Standardized neuropsychiatric assessments integrated with GI evaluation [29].
The intricate relationship between thyroid disorders and SIBO further complicates research in this area, as hypothyroidism can impair motility while SIBO may affect thyroid hormone conversion, creating a bidirectional relationship that requires careful stratification in study design [29].
A Researcher's Toolkit: Functional Tests for Assessing Macronutrient Digestion and Absorption
Frequently Asked Questions (FAQs) for Researchers
Q1: What is the specific clinical and research utility of the 72-hour fecal fat test?
The 72-hour quantitative fecal fat test is historically considered a gold standard for objectively confirming the presence of steatorrhea (excess fat in stool) in a research setting [30] [31]. It provides a quantitative measure of fat malabsorption. However, leading guidelines strongly caution against its use for differential diagnosis, such as distinguishing between pancreatic and intestinal causes of malabsorption [30] [32]. Its role in modern research is often limited to validating the efficacy of new therapeutic interventions, such as pancreatic enzyme replacement therapies, or as a benchmark for validating newer, less invasive diagnostic methods [32].
Q2: What are the primary limitations that affect its reliability in clinical studies?
The test's reliability is compromised by several significant challenges:
- Stringent Pre-Analytical Requirements: The test is highly sensitive to dietary fat intake (typically requiring 100-150 grams per day), complete stool collection, and avoidance of interfering substances [30] [33]. Even minor deviations can invalidate results.
- Patient Burden and Compliance: The 72-hour collection period is cumbersome for participants, leading to potential non-compliance and incomplete collections, which skews results [30] [34].
- Lack of Etiological Specificity: A positive test confirms malabsorption but does not provide information on the underlying mechanism or disease cause [30] [31].
Q3: What are the recommended alternative or complementary assays for investigating macronutrient malabsorption?
Given the challenges of the 72-hour collection, researchers are exploring several alternative techniques, particularly for studies in vulnerable populations like children [12] [8]. The table below summarizes key investigational methods.
Table 1: Investigational Assays for Macronutrient Malabsorption
| Macronutrient | Investigation Method | Function Tested | Key Advantages & Status |
|---|---|---|---|
| Fat | ¹³C-Mixed Triglyceride Breath Test | Global fat digestion and absorption [12] [8] | Non-invasive; potential for use in pediatric studies [12] [8]. |
| Carbohydrates | ¹³C-Starch/Sucrose/Lactose Breath Tests | Carbohydrate digestion and absorption [12] [8] | Non-invasive; can probe specific digestive pathways [12] [8]. |
| Protein | Benzoyl-L-tyrosyl-L-1-¹³C-alanine Breath Test | Dipeptide absorption [12] [8] | Non-invasive; assesses functional peptide transport [12] [8]. |
| Pancreatic Function | Fecal Elastase-1 | Pancreatic exocrine output [30] | Single stool sample; high negative predictive value for pancreatic insufficiency [30]. |
Q4: How should fecal fat results be interpreted in a pediatric research population?
Interpretation in pediatric populations requires special consideration. Reference values for timed collections are not firmly established for patients under 18 years of age [33] [32]. For random stool samples, results are often reported as a percentage of fat, with a typical reference value of 0-19% for all ages [32]. Furthermore, results may be reported as a Coefficient of Fat Absorption (CFA), which calculates the percentage of ingested fat that was absorbed, providing a more normalized metric for inter-individual comparison [32].
Experimental Protocol: 72-Hour Quantitative Fecal Fat Collection
This protocol outlines the standardized methodology for the 72-hour fecal fat test, based on guidelines from major reference laboratories [33] [32].
Pre-Collection Phase (Patient Preparation)
- Duration: 3 days prior to and throughout the 72-hour stool collection period.
- Controlled Diet: Participants must consume a fat-controlled diet of 100-150 grams of fat per day [33] [32]. Dietary intake records are crucial for accurate interpretation [30].
- Prohibited Substances:
- Laxatives, particularly mineral oil and castor oil [33] [32].
- Synthetic fat substitutes (e.g., Olestra) or fat-blocking nutritional supplements (e.g., Orlistat) [30] [33].
- Diaper rash ointments or creams, which can falsely elevate results [34] [33]. Petroleum jelly or cornstarch are acceptable alternatives [34].
- Other Considerations: Discontinue pancreatic enzyme replacement therapy if applicable (under medical supervision) [30]. A 48-hour waiting period is required after procedures using barium contrast [33].
Collection Phase
- Duration: A full, continuous 72-hour period.
- Supplies: Use approved, single-use stool collection containers provided by the laboratory. These are often designed to comply with shipping safety regulations [33].
- Procedure:
- Collect all stool passed during the 72-hour window.
- Use a wooden tongue depressor or plastic spoon to transfer stool to the container.
- Avoid contamination with urine, toilet water, or toilet paper [34] [31].
- Close the lid tightly after each use. If multiple containers are needed, label them sequentially (e.g., "1 of 3").
- Storage: Keep the specimen container refrigerated or on ice in a cooler during the collection period [34] [32].
- Specimen Submission: The entire collection must be submitted to the lab. The total weight of the collection must be documented.
Analytical Phase
- Methodology: The preferred method at many core laboratories is Nuclear Magnetic Resonance (NMR) Spectroscopy [32].
- Process: The homogenized stool sample is weighed, dried, and analyzed by NMR to determine the percentage of fat. This value is converted to grams of fat excreted per 24-hour period [32].
Data Interpretation and Troubleshooting
Reference Values and Interpretation
Table 2: Reference Values for 72-Hour Fecal Fat Test
| Population | Specimen Type | Reference Range | Interpretation of Abnormal Result |
|---|---|---|---|
| Adults (≥18 years) | 72-hour Timed | < 7 g fat/24 hours [32] | >7 g/24h is suggestive of malabsorption, provided dietary compliance [30] [32]. |
| Pediatrics (& All Ages) | Random | 0-19% fat [32] | >19% fat is abnormal. A timed collection should be performed for confirmation. |
Common Experimental Pitfalls and Solutions
Table 3: Troubleshooting Guide for the 72-Hour Fecal Fat Test
| Problem | Potential Impact on Results | Corrective Action / Prevention |
|---|---|---|
| Inadequate Dietary Fat Intake | Falsely low result; failure to challenge absorptive capacity [30]. | Provide participants with detailed dietary instructions and a food diary to ensure consistent 100-150 g/day intake. |
| Incomplete Stool Collection | Falsely low result; underestimation of total fat excretion [30]. | Provide clear verbal and written collection instructions. Emphasize the need to collect every stool. |
| Use of Prohibited Medications/Ointments | Falsely elevated results [30] [33]. | Provide a comprehensive list of prohibited substances and verify compliance during the collection period. |
| Specimen Contamination (Urine, Water) | Analytically interference; invalid results [34] [31]. | Instruct on proper use of collection devices like a "toilet hat" or plastic wrap. |
The Researcher's Toolkit: Essential Materials
Table 4: Key Research Reagent Solutions for 72-Hour Fecal Fat Testing
| Item | Function / Utility in the Experiment |
|---|---|
| Stool Collection Kit (72-Hour) | A specialized container, often provided by reference labs (e.g., Mayo T291), is required for safe specimen containment and shipping [33]. |
| Fat-Controlled Diet Protocol | Standardized dietary guidelines and recording sheets are critical to ensure a consistent fat challenge, which is fundamental to test validity [30] [32]. |
| Nuclear Magnetic Resonance (NMR) Spectrometer | The analytical instrument used for quantitative fat measurement in homogenized stool samples at reference laboratories [32]. |
| Proprietary Stool Stabilizers | Some specialized collection kits may include stabilizers to preserve specimen integrity during storage and transport. |
Experimental and Diagnostic Pathways
The following diagram illustrates the logical workflow for a researcher or clinician investigating malabsorption, highlighting the role of the 72-hour fecal fat test alongside modern alternatives.
Malabsorption Diagnostic Workflow
Technical Support Center
FAQs & Troubleshooting Guides
General Breath Test Principles
- Q: What is the fundamental principle behind a 13C-breath test?
- A: A 13C-labeled substrate (carbohydrate, fat, or protein) is orally administered. If the substrate is properly digested, absorbed, and metabolized, the 13C-isotope is ultimately oxidized in the liver, producing 13CO2. This 13CO2 is excreted via the lungs and can be measured in breath samples over time. A reduced or delayed 13CO2 recovery indicates malabsorption or impaired metabolic function.
Substrate-Specific Issues
Carbohydrates (e.g., 13C-Spirulina platensis, 13C-Starch)
- Q: We are observing low 13CO2 recovery with a 13C-starch test. What could be the cause?
- A: Low recovery suggests carbohydrate malabsorption. Key troubleshooting steps:
- Confirm Pancreatic Function: Rule out pancreatic exocrine insufficiency (PEI) as a cause of inadequate amylase secretion. Correlate with a 13C-mixed triglyceride breath test.
- Check for Small Intestinal Bacterial Overgrowth (SIBO): SIBO can cause premature fermentation of carbohydrates in the small intestine, diverting the 13C from oxidative metabolism and reducing 13CO2 recovery. A positive hydrogen/methane breath test can confirm this.
- Verify Substrate Preparation: Ensure the substrate was prepared and administered correctly, as per the experimental protocol.
- A: Low recovery suggests carbohydrate malabsorption. Key troubleshooting steps:
Lipids (e.g., 13C-Mixed Triglyceride (MTG), 13C-Octanoic Acid)
- Q: Our 13C-MTG breath test results are highly variable between subjects. How can we improve consistency?
- A: Variability often stems from the test meal composition.
- Standardize the Test Meal: Use a high-fat, standardized meal (see Experimental Protocols below) to ensure consistent stimulation of pancreatic lipase and biliary secretion.
- Control Gastric Emptying: The 13C-MTG test is influenced by gastric emptying rates. Consider co-administering a 13C-octanoic acid capsule (a marker for gastric emptying) in a separate test to normalize results.
- Subject Preparation: Ensure subjects fasted for the recommended 12 hours and abstained from alcohol and strenuous exercise prior to testing.
- A: Variability often stems from the test meal composition.
Proteins (e.g., 13C-Leucine, 13C-Lysine)
- Q: What does a delayed peak in 13CO2 excretion during a 13C-leucine breath test indicate?
- A: A delayed time to peak (Tmax) typically indicates impaired gastric emptying, as the substrate must reach the small intestine for absorption. A reduced cumulative recovery (%CD) suggests impaired protein digestion (e.g., pepsin or pancreatic protease deficiency) or impaired hepatic metabolism (e.g., liver dysfunction).
Analytical Troubleshooting
- Q: The Isotope Ratio Mass Spectrometer (IRMS) is giving unstable baseline readings. What should we check?
- A:
- Gas Purity: Ensure the reference CO2 gas supply is pure and not depleted.
- Leak Check: Perform a full system leak check, including the breath sample inlet system.
- Contamination: Clean the sample introduction needle and check for contaminants in the breath collection bags or tubes.
- A:
Quantitative Data Summary
Table 1: Common 13C-Labeled Substrates for Macronutrient Absorption Studies
| Macronutrient | Exemplary Substrate | Targeted Dysfunction | Key Pharmacokinetic Parameter | Normal Range (Example) |
|---|---|---|---|---|
| Carbohydrate | 13C-Spirulina platensis | Generalized Malabsorption | Cumulative % Dose Recovered (CDR) | > 14% (over 6 hours) |
| Lipid | 13C-Mixed Triglyceride | Pancreatic Exocrine Insufficiency (PEI) | Cumulative % Dose Recovered (CDR) | > 29% (over 6 hours) |
| Protein | 13C-Leucine | Gastric Emptying / Metabolic Rate | Time to Peak (Tmax) / %CD | Tmax: 60-120 mins |
Experimental Protocols
Protocol 1: 13C-Mixed Triglyceride (MTG) Breath Test for Pancreatic Exocrine Insufficiency
- Subject Preparation: Overnight fast (12 hours). No smoking or strenuous exercise on test day.
- Test Meal: Administer a standardized test meal (e.g., 60g white bread, 20g butter, 200mL whole milk) containing 250mg of 13C-MTG.
- Baseline Breath Sample: Collect a baseline breath sample in a suitable container (e.g., Exetainer tube) before substrate administration.
- Post-Dose Sampling: Collect breath samples at 30, 60, 90, 120, 150, 180, 240, 300, and 360 minutes after the test meal.
- Sample Analysis: Analyze breath samples via Isotope Ratio Mass Spectrometry (IRMS) to determine the 13CO2/12CO2 ratio.
- Data Calculation: Calculate the percentage of 13C dose recovered per hour (%DR/h) and the cumulative recovery (%CDR) over 6 hours.
Protocol 2: 13C-Spirulina platensis Breath Test for Carbohydrate Malabsorption
- Subject Preparation: As per Protocol 1.
- Substrate Administration: Administer 100mg of 13C-Spirulina platensis (or equivalent 13C-labeled carbohydrate) with 150mL of water.
- Breath Sampling: Collect baseline and post-dose breath samples at 30, 60, 90, 120, 150, 180, 210, 240, 300, and 360 minutes.
- Sample Analysis: Analyze via IRMS.
- Data Calculation: Calculate the cumulative %CDR over 6 hours. A lower value indicates malabsorption.
Visualizations
13C Breath Test Workflow
13C-MTG Metabolic Pathway
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions
| Item | Function / Application |
|---|---|
| 13C-Labeled Substrates | The core tracer for the breath test (e.g., 13C-MTG for fat, 13C-Spirulina for carbs). |
| Standardized Test Meal | Ensures consistent and physiological stimulation of digestive processes (e.g., for lipid tests). |
| Breath Collection Bags/Tubes | Vacuum-evacuated containers (e.g., Exetainer) for stable, long-term storage of breath samples. |
| Isotope Ratio Mass Spectrometer (IRMS) | The gold-standard analytical instrument for high-precision measurement of 13CO2/12CO2 ratios. |
| Reference CO2 Gas | A calibrated, high-purity CO2 standard gas required for accurate IRMS calibration. |
| Software for Kinetic Analysis | Used to calculate key parameters like Cumulative % Dose Recovered (CDR) and Time to Peak (Tmax). |
Frequently Asked Questions (FAQs)
What is the primary clinical and research application of the secretin-stimulated ePFT? The secretin-stimulated ePFT is considered the definitive method for assessing exocrine pancreatic function. Its primary application is the diagnosis of early chronic pancreatitis, especially in cases where imaging tests are normal, and for determining a pancreatic cause for unexplained chronic diarrhea [35]. It is a sensitive tool for detecting functional deficiencies before structural damage becomes apparent.
How does ePFT compare to other diagnostic tests for Exocrine Pancreatic Insufficiency (EPI)? ePFT is considered the most accurate test for assessing pancreatic exocrine function but is limited to specialized centers [36]. In clinical practice, less invasive tests are often used first. The fecal elastase test is commonly recommended as an initial test, though it may be less sensitive for mild EPI [37] [38]. The 72-hour fecal fat test quantitatively measures fat malabsorption but is cumbersome for patients [38] [36].
What are the common technical challenges when collecting pancreatic secretions? A key challenge is ensuring proper tube placement in the duodenum to allow for uncontaminated, sequential collection of pancreatic juice. Secretions are typically collected at set intervals (e.g., every 15 minutes for 60 minutes) following secretin injection [35]. Fluid collection must be meticulous to avoid loss of sample, which can compromise the bicarbonate measurement.
What does an abnormal bicarbonate concentration indicate? The bicarbonate concentration in the collected pancreatic secretions is the primary outcome measure. An adequate production and secretion of bicarbonate implies intact pancreatic function. A low bicarbonate output, particularly when progressively lower concentrations are seen over the collection period, is indicative of impaired exocrine function and supports a diagnosis of chronic pancreatitis [35].
Troubleshooting Guide for Direct Pancreatic Function Testing
| Problem Area | Specific Issue | Potential Cause | Solution |
|---|---|---|---|
| Pre-procedure | Patient has contraindications to endoscopy. | Severe cardiopulmonary comorbidities, uncooperative patient. | Complete a thorough pre-procedural risk assessment. Consider alternative tests like fecal elastase or imaging. |
| Secretin Administration | Suboptimal pancreatic stimulation. | Incorrect secretin dosing; compromised secretin potency. | Use synthetic human secretin at the validated dose. Ensure proper storage and handling of the reagent. |
| Sample Collection | Low sample volume or failed collection. | Duodenal tube displacement or blockage; incorrect timing. | Verify tube position under imaging. Adhere strictly to collection timepoints (e.g., 0, 15, 30, 45, 60 minutes). |
| Sample Analysis | Erratic or implausible bicarbonate results. | Sample contamination with gastric juice; degradation of sample. | Ensure tube is positioned post-ampulla. Process samples promptly according to laboratory protocols. |
| Data Interpretation | Discordance between ePFT results and clinical picture. | Early/mild disease with borderline results; non-pancreatic causes of malabsorption. | Interpret results within the full clinical context, including imaging and nutritional status [37]. |
Comparative Analysis of Pancreatic Function and Malabsorption Diagnostics
The following table summarizes key quantitative and functional characteristics of major tests used in the assessment of pancreatic function and macronutrient malabsorption.
Table 1: Diagnostic Tests for Pancreatic Function and Fat Malabsorption
| Test Name | Primary Measured Analyte | Normal Value / Diagnostic Threshold | Key Performance Characteristics | Advantages & Limitations |
|---|---|---|---|---|
| Direct Pancreatic Function Test (ePFT) [35] | Bicarbonate concentration in duodenal aspirate | Not explicitly stated in results; low output indicates impairment. | Considered the most accurate assessment of exocrine function. | Advantage: Definitive gold-standard. Limitation: Invasive, limited availability, requires specialized expertise. |
| Fecal Elastase (FEL-1) [37] | Human pancreatic elastase in stool | - Normal: >200 µg/g- Moderate PEI: 100-200 µg/g- Severe PEI: <100 µg/g | Sensitivity: 25-65% (mild PEI) to 82-100% (severe PEI). Specificity: >90% in most studies. | Advantage: Non-invasive, specific to pancreatic enzyme, unaffected by enzyme replacement therapy. Limitation: Less sensitive for mild PEI, false positives with watery diarrhea. |
| 72-Hour Fecal Fat Test [38] [36] | Fat content in stool | Quantitative measure of fat absorption; high levels indicate steatorrhea. | Directly measures fat malabsorption, a functional consequence of severe PEI. | Advantage: Quantitative gold standard for steatorrhea. Limitation: Cumbersome for patients, requires high-fat diet, unpleasent sample handling. |
| Serum Nutritional Markers [37] | Fat-soluble vitamins (A, E, D), magnesium, proteins | Low levels can support diagnosis of malabsorption. | Low vitamin E is consistently reported in PEI; other markers are non-specific. | Advantage: Supports assessment of nutritional status. Limitation: Not diagnostic for PEI in isolation; can be abnormal in other malabsorption syndromes. |
The Scientist's Toolkit: Key Reagents & Materials for Secretin-ePFT
Table 2: Essential Research Reagents and Materials for Secretin-Stimulated ePFT
| Item | Function in the ePFT Protocol |
|---|---|
| Synthetic Human Secretin | Hormone administered intravenously to stimulate the pancreas to secrete fluid and bicarbonate-rich enzymes [35]. |
| Endoscope | A flexible tube with a camera used to access the duodenum and correctly position the collection tube distal to the ampulla of Vater. |
| Duodenal Aspiration Tube | A specialized tube used to collect pancreatic juices directly from the duodenum after secretin stimulation. |
| Collection Vials | Sterile, pre-labeled vials for collecting duodenal aspirate at sequential time points (e.g., every 15 minutes). |
| Blood Analyzer / Blood Gas Machine | An automated laboratory instrument capable of rapidly and accurately measuring the bicarbonate concentration in the collected fluid samples. |
Experimental Protocol: Secretin-Stimulated Direct Pancreatic Function Test
Objective: To quantitatively assess exocrine pancreatic function by measuring bicarbonate concentration in duodenal secretions following intravenous secretin stimulation.
Methodology:
- Patient Preparation: The patient is sedated. An endoscope is passed through the stomach and into the duodenum [35].
- Tube Placement: A collection tube is positioned in the small bowel at the location of the ampulla to allow for uncontaminated collection of pancreatic secretions [35].
- Secretin Stimulation: Synthetic human secretin is administered intravenously as a bolus [35].
- Sample Collection: Pancreatic juice is aspirated via the collection tube and sampled at sequential time intervals. The standard protocol involves collection at 15-minute intervals for a total of 60 minutes [35].
- Sample Analysis: The bicarbonate concentration (measured in mmol/L) is determined for each collected sample using a standard clinical laboratory method, such as a blood gas analyzer.
- Data Interpretation: The peak bicarbonate concentration and/or the trend in concentrations over the collection period is analyzed. A low and/or progressively declining bicarbonate output is diagnostic of exocrine pancreatic insufficiency.
Secretin-ePFT Procedural Workflow
Frequently Asked Questions (FAQs)
Q1: What is the fundamental principle behind an oral tolerance test? An oral tolerance test is a functional assay that provides a global readout of intestinal brush border enzyme (hydrolysis) and transporter activity (absorption), and subsequent metabolization of substrates [12]. In the context of macronutrient malabsorption research, it helps identify impaired digestive and absorptive capacity by measuring the body's systemic response to an orally administered nutrient load.
Q2: How does a carbohydrate tolerance test specifically assess hydrolase and transporter activity? When a carbohydrate like lactose or sucrose is ingested, it must first be broken down by brush border enzymes (e.g., lactase, sucrase) into monosaccharides before specific transporters (e.g., SGLT1 for glucose) can absorb them [12]. An abnormal rise in blood glucose after an oral load indicates a failure in this chain of events, pointing to potential deficiencies in hydrolase activity or transporter function [12].
Q3: What are the key advantages of using breath tests over blood-based tolerance tests? Breath tests, such as the (^{13}\text{C})-starch or (^{13}\text{C})-sucrose breath test, are non-invasive and can provide a more direct measure of complete digestion and absorption [12]. They detect the exhalation of (^{13}\text{CO}_2) after a labeled substrate is ingested, absorbed, and metabolized. This makes them particularly suitable for vulnerable populations, like children in studies on environmental enteropathy [12].
Q4: In a research context, what can an abnormal oral tolerance test result indicate? An abnormal result suggests sub-optimal digestion and absorption (malabsorption) of the tested macronutrient [12]. In conditions like environmental enteropathy (EE), this malabsorption is a critical link to functional outcomes such as linear growth faltering and impaired cognition, making the test a valuable tool for quantifying gut functional capacity beyond histopathology [12].
Q5: Why is proper patient preparation critical for a valid oral tolerance test? Multiple factors can significantly impact test results. Patients must consume a diet with at least 150 grams of carbohydrates per day for 3 days prior to the test to ensure their metabolic systems are primed. They must also fast, avoid strenuous exercise, and maintain normal activity levels to prevent confounding variables that affect glucose metabolism or gastric emptying [39] [40] [41].
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting Guide for Oral Tolerance Tests
| Problem & Phenomenon | Potential Root Cause | Proposed Solution |
|---|---|---|
| High Intra-Assay Variability: Inconsistent results between duplicate tests on the same subject. | Variable gastric emptying rates; Uncontrolled diet or activity prior to test [42] [40]. | Strictly standardize pre-test protocol: enforce 3-day carbohydrate diet, overnight fast, and minimal activity. Schedule all tests for the morning [40] [41]. |
| Flat Blood Glucose Response Curve: No significant rise in blood glucose after carbohydrate load. | Severe hydrolase/transporter deficiency; Delayed gastric emptying; Laboratory error in sample handling [12]. | Verify functionality of glucose assay. Correlate with clinical symptoms (e.g., diarrhea). Consider using a breath test for a more sensitive measure [12]. |
| Unexpected Hypoglycemic Episode: Blood glucose drops significantly below fasting level during test. | Reactive hypoglycemia; Excessive insulin response [39] [41]. | Ensure patient safety with continuous monitoring. Extend the testing period to capture the hypoglycemic trend and investigate insulin secretion dynamics [39]. |
| Nausea/Vomiting Post-Dose: Subject cannot tolerate the test solution. | High osmolarity and sweetness of the concentrated glucose solution [39] [41]. | Use commercially available, more palatable formulations. Ensure the solution is chilled. Advise the subject to drink it steadily over 3-5 minutes, not chug it [40]. |
Standard Experimental Protocol: The 2-Hour Oral Glucose Tolerance Test (OGTT)
The following protocol is adapted for research purposes to assess carbohydrate digestion and absorption.
1. Principle: The OGTT evaluates the efficiency with which the body processes a standardized oral glucose load. It relies on the normal function of intestinal hydrolases and transporters for monosaccharide absorption, followed by systemic disposal of glucose into tissues [42] [40].
2. Reagents and Equipment:
- Glucose Load: 75 g of anhydrous glucose for adults [40]. For children, 1.75 g per kg of body weight, up to a maximum of 75 g [40].
- Solvent: 250-300 mL of water [40].
- Collection Tubes: Fluoride-oxalate tubes to inhibit glycolysis in blood samples [40].
- Analyzer: Automated clinical chemistry analyzer using the hexokinase method for precise plasma glucose measurement [40].
3. Step-by-Step Procedure:
- Pre-Test Preparation: Instruct the subject to maintain an unrestricted diet (≥150 g of carbohydrates daily) and normal physical activity for at least 3 days prior to the test [40].
- Overnight Fast: Confirm a 10- to 16-hour fast before the test. Water is permitted [40].
- Baseline Blood Draw (T=0 min): Perform a venipuncture to collect a baseline fasting blood sample. Centrifuge and separate plasma within 60 minutes of collection [40].
- Administration of Glucose Load: Have the subject drink the prepared glucose solution within 5 minutes. Note the start time [39] [40].
- Post-Load Blood Draws: Collect subsequent blood samples at precisely 30, 60, and 120 minutes after the complete ingestion of the solution. Adhere to the same sample processing protocol [42] [40].
- Subject Monitoring: The subject must remain seated and refrain from smoking or eating throughout the test period [40].
4. Data Interpretation: Interpret the 2-hour plasma glucose value against standard criteria [40] [41]:
| 2-Hour Plasma Glucose Level | Interpretation |
|---|---|
| < 140 mg/dL (7.8 mmol/L) | Normal Glucose Tolerance |
| 140 - 199 mg/dL (7.8 - 11.0 mmol/L) | Impaired Glucose Tolerance (Prediabetes) |
| ≥ 200 mg/dL (11.1 mmol/L) | Provisional Diabetes Diagnosis |
Note: A single abnormal test is not diagnostic. The test should be repeated on a separate day for confirmation [40].
Visualizing the Test Workflow and Data Interpretation
The following diagram illustrates the logical workflow and physiological principles of the oral carbohydrate tolerance test.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials for Oral Tolerance Research
| Research Reagent / Material | Function in Experiment |
|---|---|
| (^{13}\text{C})-Labeled Substrates (e.g., (^{13}\text{C})-Starch, (^{13}\text{C})-Sucrose) | Non-invasive tracer for breath tests; allows for precise measurement of macronutrient-specific digestion, absorption, and oxidation [12]. |
| Enzymatic Glucose Assay Kits (Hexokinase Method) | Gold-standard method for precise and specific quantification of plasma glucose concentrations in collected samples [40]. |
| Sodium Fluoride/Potassium Oxalate Blood Collection Tubes | Preserves blood glucose concentration by inhibiting glycolysis in white blood cells during sample storage and transport [40]. |
| Standardized Macronutrient Loads (e.g., 75g Glucose, Mixed-Meal Drinks) | Provides a consistent and reproducible challenge to the digestive system, enabling comparative studies across subjects and populations [42] [40] [43]. |
| C-Peptide & Insulin Immunoassays | Differentiates endogenous insulin production from exogenous insulin; provides insight into pancreatic β-cell function in response to the nutrient load [43]. |
This technical support center provides essential guidance for researchers investigating macronutrient malabsorption. The analysis of citrulline (marker of functional enterocyte mass), intestinal fatty acid-binding protein (I-FABP, marker of enterocyte damage), and calprotectin (marker of neutrophilic inflammation) provides critical insights into intestinal health and function. Proper handling of these biomarkers is crucial for obtaining reliable data in clinical and preclinical studies.
Citrulline
Research Significance & Application
Citrulline, a non-protein amino acid produced almost exclusively by enterocytes, serves as a reliable plasma marker for functional enterocyte mass. In macronutrient malabsorption studies, reduced citrulline levels indicate diminished intestinal absorptive capacity, helping researchers quantify the severity of intestinal failure and monitor responses to nutritional interventions.
Troubleshooting & FAQs
Q: What causes unexpectedly low citrulline levels in plasma samples from subjects with confirmed normal intestinal function? A: Pre-analytical factors are the most common cause:
- Sample Hemolysis: Erythrocytes contain arginase which converts citrulline to arginine. Visibly hemolyzed samples should be discarded.
- Improper Sample Processing: Plasma must be separated from cells within 1 hour of collection via centrifugation at 1500-2000×g for 10 minutes at 4°C. Use EDTA or heparin tubes; avoid citrate.
- Repeated Freeze-Thaw Cycles: Analyze samples within 3 freeze-thaw cycles. Aliquot samples to avoid repeated cycling.
Q: Our citrulline ELISA shows a high coefficient of variation between replicates. What could be wrong? A: This typically indicates an assay-specific issue:
- Plate Washer Malfunction: Check for clogged aspirator needles or improperly calibrated dispenser heads. Ensure thorough washing without introducing air bubbles.
- Inconsistent Incubation Times or Temperatures: Use a calibrated thermal plate sealer and timer. Avoid stacking plates during incubations.
- Antibody Degradation: Check expiration dates. Ensure the detection antibody is stored away from light and has not been subjected to temperature fluctuations.
Q: How should we interpret stable citrulline levels in an intervention study for malabsorption? A: A stable plasma citrulline concentration (reference range: ~20-40 μmol/L in healthy adults) suggests:
- Preservation of Enterocyte Mass: The intervention may have prevented further enterocyte loss.
- Lack of Regeneration: The treatment did not stimulate significant mucosal healing.
- Confounding Factors: Consider renal function, as citrulline is cleared by the kidneys. Measure plasma creatinine concurrently.
Research Reagent Solutions
| Item | Function & Application |
|---|---|
| L-Citrulline ELISA Kit | Quantifies citrulline concentration in plasma, serum, and cell culture supernatants via competitive immunoassay. |
| Citrulline Deuterated Internal Standard | Essential for accurate quantification and recovery calculations in LC-MS/MS methods. |
| Amino Acid Analysis Sample Prep Kit | Provides pre-column derivatization reagents for HPLC-based separation and detection. |
| Protein Precipitation Plates | For deproteinizing plasma samples prior to LC-MS/MS analysis to reduce matrix effects. |
Experimental Protocol: Plasma Citrulline Measurement by ELISA
- Sample Collection: Draw venous blood into EDTA tubes. Invert gently 8-10 times.
- Plasma Separation: Centrifuge at 2,000×g for 15 minutes at 4°C within 30 minutes of collection.
- Aliquoting: Transfer supernatant (plasma) to polypropylene tubes. Store at -80°C if not analyzed immediately.
- ELISA Procedure:
- Thaw samples on ice and centrifuge at 10,000×g for 5 minutes.
- Prepare standards, controls, and samples as per kit instructions.
- Add 50 μL of standard or sample to appropriate wells.
- Add 50 μL of Biotinylated Citrulline Detector Antibody to each well. Incubate 45 minutes at 37°C.
- Aspirate and wash 3 times with 350 μL wash buffer.
- Add 100 μL of HRP-Streptavidin Conjugate. Incubate 30 minutes at 37°C.
- Aspirate and wash 5 times.
- Add 90 μL of TMB Substrate. Incubate 15-20 minutes at 37°C in the dark.
- Add 50 μL of Stop Solution. Read absorbance at 450 nm within 10 minutes.
Citrulline Metabolism & Assessment Workflow
Workflow for Citrulline Assessment
I-FABP
Research Significance & Application
Intestinal Fatty Acid-Binding Protein (I-FABP) is a cytosolic protein abundant in mature enterocytes. Upon enterocyte damage or necrosis, I-FABP is rapidly released into the circulation, making it a highly sensitive and specific early marker for acute intestinal epithelial injury. In macronutrient malabsorption syndromes, elevated I-FABP indicates ongoing mucosal damage.
Troubleshooting & FAQs
Q: Why are I-FABP levels sometimes undetectable in patients with confirmed intestinal ischemia? A: Timing is critical due to I-FABP's short half-life (~11 minutes):
- Delayed Sampling: I-FABP peaks within 1-2 hours post-injury. Sample multiple time points if onset is uncertain.
- Sample Type: Use plasma (EDTA) over serum. Serum preparation can lead to platelet degranulation and proteolysis.
- Assay Sensitivity: Confirm the lower detection limit of your ELISA kit (typically ~10-20 pg/mL). Consider a high-sensitivity assay if needed.
Q: We observe high background signal in our I-FABP ELISA. How can we reduce it? A: High background often stems from interference or washing issues:
- Inadequate Washing: Ensure all wells are filled with wash buffer and allowed to soak for 30 seconds before aspiration. Manually inspect wells post-wash.
- Heterophile Antibody Interference: Re-analyze samples using a diluent containing blocking agents for heterophile antibodies or use a proprietary interference blocker.
- Contaminated Reagents: Prepare fresh wash buffer and ensure TMB substrate is not contaminated with oxidants.
Q: How do we differentiate I-FABP elevation due to intestinal ischemia from other causes like celiac disease? A: Context and additional markers are key:
- Magnitude of Elevation: Ischemic insults often cause a massive, acute spike (>500 pg/mL), while chronic conditions like celiac may show moderate, persistent elevation.
- Marker Panels: Combine with D-lactate (for bacterial translocation) and citrulline (for functional mass). Ischemia typically shows high I-FABP and D-lactate with low citrulline.
- Clinical Correlation: Correlate with imaging and patient symptoms.
Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Human I-FABP ELISA Kit | Measures I-FABP concentration in plasma/serum for detecting acute intestinal injury. |
| Recombinant I-FABP Protein | Used as a standard for ELISA calibration and for spike-and-recovery experiments. |
| Protease Inhibitor Cocktail | Added to plasma immediately after collection to prevent in vitro degradation of I-FABP. |
| Heterophile Antibody Blocking Tubes | Pre-treatment tubes to minimize false positive results from interfering antibodies. |
Experimental Protocol: Plasma I-FABP Measurement by ELISA
- Sample Collection & Stabilization: Collect blood in EDTA tubes pre-loaded with a broad-spectrum protease inhibitor cocktail. Mix gently.
- Rapid Processing: Centrifuge at 1,500×g for 10 minutes at 4°C within 30 minutes. Delay compromises stability.
- Aliquoting: Aliquot plasma into low-protein-binding tubes. Freeze at -80°C. Avoid freeze-thaw cycles.
- ELISA Procedure:
- Equilibrate all components to room temperature for 30 minutes.
- Prepare standards and samples. Dilute samples 1:2 if above the standard curve range.
- Add 100 μL of standard or sample to the appropriate wells. Cover and incubate 60 minutes at room temperature on a plate shaker (300 rpm).
- Aspirate and wash each well 4 times with 400 μL of 1x Wash Buffer.
- Add 100 μL of Biotinylated Anti-I-FABP Antibody to each well. Incubate 60 minutes at room temperature with shaking.
- Aspirate and wash 4 times.
- Add 100 μL of HRP-Streptavidin Solution. Incubate 30 minutes at room temperature protected from light.
- Aspirate and wash 4 times.
- Add 100 μL of TMB Substrate. Incubate 10 minutes at room temperature in the dark.
- Add 100 μL of Stop Solution. Read absorbance at 450 nm with a correction at 570 nm or 620 nm.
I-FABP Release and Detection Pathway
I-FABP Release and Detection Pathway
Calprotectin
Research Significance & Application
Calprotectin (S100A8/S100A9 heterodimer) is a neutrophil-derived protein that constitutes about 60% of cytosolic proteins in neutrophils. Fecal calprotectin is a robust marker for neutrophilic inflammation in the intestinal tract. It is used to differentiate inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS) and to monitor disease activity and response to therapy in macronutrient malabsorption associated with gut inflammation.
Troubleshooting & FAQs
Q: Fecal calprotectin levels vary widely between samples from the same subject collected on consecutive days. Is this normal? A: Some biological variation is normal, but high variability suggests a pre-analytical issue:
- Inhomogeneous Stool Sample: Fecal matter is heterogeneous. Take multiple aliquots from different parts of the stool and homogenize thoroughly before extraction.
- Hydration Status: Concentrations are weight/weight. Diarrhea can artificially lower values, while constipation can increase them. Use an extraction buffer with a defined ratio.
- Sample Timing: For disease monitoring, collect samples at the same time of day and under similar dietary conditions.
Q: Our fecal extract is too viscous to pipette accurately for the ELISA. How can we resolve this? A: Viscosity is typically due to incomplete homogenization or mucin content.
- Enhanced Homogenization: Use a vortex mixer with a tube adapter for at least 15 minutes. Alternatively, use a mechanical homogenizer (e.g., bead beater).
- Centrifugation Clarification: After extraction, centrifuge the sample at 10,000×g for 10 minutes. Carefully pipette the supernatant for analysis.
- Filter Clarification: Pass the supernatant through a 0.8 μm syringe filter (low protein binding). Check kit instructions to ensure this is permissible.
Q: How do we interpret a high fecal calprotectin level in an asymptomatic research subject? A: Elevated fecal calprotectin (>50-60 μg/g) indicates subclinical intestinal inflammation.
- Confirm the Result: Repeat the test with a new sample to rule out pre-analytical error.
- Exclude NSAID Use: Document NSAID/medication use, a common cause of elevated calprotectin in asymptomatic individuals.
- Consider Other Causes: Potential causes include subclinical IBD, microscopic colitis, or neoplasia. Further clinical evaluation may be warranted.
Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Fecal Calprotectin ELISA Kit | Quantifies calprotectin in fecal extracts to assess intestinal inflammation. |
| Fecal Sample Extraction Buffer | Standardized buffer for homogenizing stool samples at a fixed dilution (e.g., 1:50). |
| Sample Homogenizer (Bead Beater) | Ensures complete and consistent disruption of solid stool samples for accurate extraction. |
| Low-Protein-Bind Tubes & Tips | Prevents analyte loss due to adhesion to plastic surfaces during sample handling. |
Experimental Protocol: Fecal Calprotectin Measurement by ELISA
- Sample Collection: Collect stool in a clean, dry container. Sample can be stored at 2-8°C for up to 3 days or frozen at -20°C for long-term storage.
- Homogenate Preparation:
- Weigh 50-100 mg of feces.
- Add the corresponding volume of extraction buffer to achieve a 1:50 dilution (e.g., add 4.95 mL buffer to 100 mg stool).
- Vortex vigorously for 15-30 minutes until a homogenous suspension is achieved.
- Clarification: Centrifuge the homogenate at 10,000×g for 10 minutes at room temperature.
- Supernatant Collection: Carefully collect the supernatant for analysis. If the supernatant is still turbid, perform a second centrifugation or filtration.
- ELISA Procedure:
- Pipette 50 μL of standard, control, or clarified supernatant into the appropriate wells.
- Add 50 μL of Enzyme Conjugate to each well. Mix gently by tapping the plate frame. Incubate 60 minutes at room temperature (20-25°C).
- Empty the plate contents and wash each well 5 times with 400 μL of 1x Wash Solution.
- Add 100 μL of TMB Substrate Solution to each well. Incubate 30 minutes at room temperature in the dark.
- Add 100 μL of Stop Solution to each well. Read the absorbance at 450 nm within 30 minutes.
Fecal Calprotectin Analysis Workflow
Fecal Calprotectin Analysis Workflow
| Biomarker | Sample Type | Healthy Reference Range | Clinically Significant Cut-off | Primary Clinical Interpretation | Stability & Handling Notes |
|---|---|---|---|---|---|
| Citrulline | Plasma (EDTA) | 20 - 40 μmol/L | < 20 μmol/L | Indicator of functional enterocyte mass. Low levels suggest intestinal failure. | Separate plasma within 1 hr; stable at -80°C; avoid hemolysis. |
| I-FABP | Plasma (EDTA) | < 200 pg/mL | > 500 pg/mL | Marker of acute enterocyte damage. Elevated in ischemia, NEC, etc. | Very short half-life (~11 min). Process immediately with protease inhibitors. |
| Calprotectin | Feces | < 50 μg/g | > 100 μg/g | Marker of neutrophilic inflammation in the gut. Differentiates IBD from IBS. | Homogenize thoroughly. Stable at room temp for 3 days; long-term at -20°C. |
FAQs: Troubleshooting Experimental Challenges in Malabsorption Research
FAQ 1: A patient's duodenal biopsy shows villous atrophy, but their celiac disease serology is negative. What are the next steps?
When serologic testing for celiac disease is negative despite villous atrophy, a detailed and systematic evaluation is required [44]. You should not assume the finding is non-specific. The Paris Consensus provides a framework for diagnosing these seronegative enteropathies, splitting them into two main groups: celiac disease with negative serology and non-celiac enteropathies [44]. The differential diagnosis is broad and includes:
- Autoimmune Enteropathy
- Common Variable Immunodeficiency
- Tropical Sprue
- Giardiasis
- Drug-Induced Enteropathy (e.g., caused by medications like NSAIDs) [45]
- Crohn's Disease
- HIV Enteropathy
- Environmental Enteropathy (EE) [12]
- Idiopathic Villous Atrophy [44]
The diagnostic workflow should include a thorough medication review, careful assessment of the medical history for systemic conditions and infections, and further targeted testing based on clinical clues [44]. For a confirmed diagnosis of seronegative celiac disease, it is essential to exclude other causes, confirm the presence of a permissive HLA haplotype (DQ2.5, DQ2.2, DQ8, or DQ7.5), and document histologic improvement after several months on a gluten-free diet [44].
FAQ 2: What is the proper biopsy protocol for confirming celiac disease and ruling out mimickers?
An accurate diagnosis relies on a correct endoscopic biopsy protocol. For suspected celiac disease, guidelines recommend taking four to six biopsies from the duodenal bulb and at least four biopsies from the distal duodenum [46]. It is critical to ensure that biopsies are performed when there are abnormalities of the duodenal mucosa, and not when findings are minor or non-specific [46]. The characteristic histologic features of celiac disease include [45]:
- Intraepithelial lymphocytosis
- Crypt hyperplasia
- Villous atrophy (partial to total)
- A chronic inflammatory cell infiltrate in the lamina propria
The modified Marsh-Oberhuber classification is often used to classify these histologic features [45]. Be aware that findings such as mucosal erosions, neutrophilic infiltrates, and loss of goblet cells are uncharacteristic of celiac disease and should prompt a search for alternative diagnoses [45].
FAQ 3: How can we functionally measure macronutrient malabsorption in research populations, particularly in children?
Assessing digestive and absorptive capacity is key to understanding conditions like Environmental Enteropathy (EE). A battery of tests is available, with non-invasive breath tests being particularly suitable for pediatric populations [12] [8].
The table below summarizes key tests for measuring macronutrient malabsorption:
Table 1: Tests for Measuring Macronutrient Malabsorption in Research
| Macronutrient | Test Name | Function Tested | Key Advantages | Considerations |
|---|---|---|---|---|
| Carbohydrate | ¹³C-Sucrose Breath Test (SBT) | Sucrose digestion by brush border enzymes, absorption, and metabolism [12]. | Non-invasive; can detect subclinical malabsorption. | Requires a separate ¹³C-glucose test for normalization; protocol standardization in children is needed [12]. |
| Carbohydrate | ¹³C-Starch Breath Test | Starch digestion by salivary/pancreatic amylase, absorption, and metabolism [12]. | Non-invasive; probes pancreatic and mucosal function. | Normative cut-offs for children are not fully established [12]. |
| Fat | ¹³C-Mixed Triglyceride Breath Test | Fat digestion (lipase activity) and absorption [12] [8]. | Non-invasive; avoids radioactive isotopes. | Results can be influenced by gastric emptying and transit time. |
| Protein | Benzoyl-L-tyrosyl-L-1-¹³C-alanine Breath Test | Dipeptide digestion and absorption at the brush border membrane [12] [8]. | Non-invasive; tests functional peptide transport. | Less commonly used than carbohydrate and fat tests; requires protocol validation. |
| Pancreatic Function | Endoscopic Pancreatic Function Test (ePFT) | Direct measurement of pancreatic bicarbonate and enzyme output after stimulation [12]. | Considered a criterion standard for exocrine pancreatic function. | Invasive, expensive, and technically challenging; not ideal for all studies [12]. |
FAQ 4: What are the common clinical and histologic mimickers of celiac disease that can confound research data?
Many conditions can mimic celiac disease both clinically and histologically. A major challenge in serologically negative enteropathy is distinguishing between these entities [45].
- Clinical Mimickers: Irritable Bowel Syndrome (IBS) and Small Intestinal Bacterial Overgrowth (SIBO) can present with diarrhea, bloating, and abdominal pain that mirrors celiac disease [45]. Inflammatory Bowel Disease (IBD), particularly Crohn's disease, can also cause similar symptoms and malabsorption [45].
- Histologic Mimickers: Several conditions can cause increased intraepithelial lymphocytes or villous atrophy. These include the entities listed in FAQ 1, such as autoimmune enteropathy, tropical sprue, and certain infections [45] [44]. Medications are a particularly important mimicker and should be considered in all patients with a serologically negative enteropathy [45].
Experimental Protocols for Key Investigations
Protocol 1: Standardized Duodenal Biopsy for Suspected Enteropathy
Objective: To obtain adequate tissue samples for a definitive histopathological diagnosis of villous atrophy and its causes.
Methodology:
- Patient Preparation: Standard patient preparation for an upper gastrointestinal endoscopy is required.
- Biopsy Locations:
- Take four to six biopsies from the duodenal bulb.
- Take at least four biopsies from the distal duodenum (second, third, or fourth portion) [46].
- Handling: Place biopsy specimens immediately in formalin-filled containers, ensuring they are properly labeled with the location.
- Clinical Information: Provide the pathologist with complete clinical information, including celiac serology results, medication history, and reason for the endoscopy [46].
Troubleshooting:
- Inconclusive Histology: If histology is inconclusive and clinical suspicion remains high, review the case considering non-celiac enteropathies and repeat endoscopy with a systematic biopsy protocol may be necessary after a treatment trial (e.g., gluten-free diet for suspected seronegative celiac) [44].
- Patchy Involvement: The number of biopsies is critical because villous atrophy can be patchy.
Protocol 2: Non-Invasive Assessment of Carbohydrate Malabsorption using ¹³C-Sucrose Breath Test
Objective: To quantify sucrose digestion and absorption capacity in research subjects, useful for evaluating Environmental Enteropathy (EE) [12] [8].
Methodology:
- Subject Preparation: Subjects must fast overnight (typically 8-12 hours). In children under 2 years, a shorter fasting duration may be necessary to ensure compliance [12].
- Test Meal: Administer a standardized test meal or solution containing ¹³C-labeled sucrose.
- Breath Sample Collection:
- Collect a baseline breath sample before ingestion of the test meal.
- Collect subsequent breath samples at regular intervals (e.g., every 15-30 minutes) for up to 2-4 hours.
- Analysis: Analyze the ¹³C enrichment in the breath samples using Isotope Ratio Mass Spectrometry (IRMS).
- Normalization: To account for individual differences in substrate oxidation, conduct a separate ¹³C-glucose breath test on a different day. The results from the sucrose test are normalized using the Coefficient of Glucose Oxidation (CGO%) [12].
Troubleshooting:
- High Inter-subject Variability: Ensure strict adherence to the pre-test diet (e.g., avoiding fiber-rich foods the day before) and control physical activity during the test [12].
- Unclear Cut-offs: Establish lab-specific normative values from control subjects, as universal cut-offs are not yet fully standardized [12].
Diagnostic Pathways & Research Workflows
The following diagram illustrates the diagnostic workflow for a patient with villous atrophy, guiding researchers through the critical decision points.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagents for Investigating Macronutrient Malabsorption
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Intrinsically ¹³C-Labeled Substrates | Serve as tracers to track the digestion, absorption, and metabolism of specific macronutrients without radioactivity. | ¹³C-sucrose, ¹³C-starch, and ¹³C-mixed triglycerides are used in breath tests to measure carbohydrate and fat malabsorption [12] [47]. |
| Intrinsically ¹⁵N/²H-Labeled Protein | Allows for precise quantification of protein digestion, absorption, and subsequent colonic fermentation. | Labeled eggs (e.g., with ¹⁵N-leucine, ²H₅-phenylalanine) are used in test meals to study protein metabolism and malabsorption [47]. |
| Isotope Ratio Mass Spectrometry (IRMS) | Precisely measures the ratio of stable isotopes (e.g., ¹³C/¹²C) in biological samples with high accuracy. | Analyzing the ¹³C enrichment in breath samples collected during a ¹³C-sucrose breath test [47]. |
| Anti-Tissue Transglutaminase (TTG) IgA ELISA Kits | Standardized serological assay for the initial screening and diagnosis of celiac disease. | Used to classify patient cohorts into seropositive and seronegative enteropathy groups [44]. |
| HLA-DQ2/DQ8 Genotyping Kits | Determine the genetic predisposition to celiac disease. The absence of these haplotypes effectively rules out the disease [45]. | Used in the diagnostic work-up of seronegative villous atrophy to rule in or out celiac disease [44]. |
Troubleshooting Guides & FAQs
Frequently Asked Questions
What is the primary consideration when selecting a test battery for macronutrient absorption studies? The foremost consideration is aligning the test with the specific research question and the macronutrient of interest. A single, non-invasive test is often insufficient to fully characterize malabsorption. Therefore, a battery of tests is typically required to probe the digestion and absorption of carbohydrates, proteins, and fats separately. The choice depends on whether you need to assess pancreatic digestive function or intestinal brush border membrane absorptive capacity [12] [8].
Which non-invasive tests are most suitable for pediatric populations or field studies? Breath tests are particularly suitable for these populations due to their non-invasive nature. Tests using 13C-labeled substrates, such as 13C-starch, 13C-sucrose, 13C-lactose for carbohydrates, 13C-mixed triglyceride for fat, and benzoyl-L-tyrosyl-L-1-13C-alanine for dipeptide absorption, show significant promise. They are relatively easy to perform, with testing times varying from 1.5 to 6 hours, which helps in maintaining participant compliance [12] [8].
A breath test yielded a negative result, but I suspect malabsorption. What should I check? First, verify the experimental controls. A negative result could indicate a problem with the protocol rather than the absence of malabsorption. Ensure you have included appropriate positive and negative controls. Second, check all equipment and reagents. Confirm that the 13C-labeled substrates have been stored correctly and have not expired. Finally, consider repeating the experiment if it is not cost-prohibitive, as simple errors in substrate administration or sample handling can occur [48].
My experimental results show high variability across participants. How can I improve consistency? High variability can stem from a lack of protocol standardization. To improve consistency:
- Standardize pretest conditions: Implement a strict fasting period appropriate for the population (e.g., shorter fasting for young children).
- Use standardized test meals: Ensure the composition and administration of test substrates are identical for all participants.
- Control for background diet: Be aware that the previous day's diet, especially if it contains foods with a high natural abundance of 13C (like corn or sugarcane), can dilute the body’s 13C pool and affect results [12] [8].
Troubleshooting Common Experimental Issues
Problem: Unexpectedly low or absent signal in a 13C-breath test.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Expired or improperly stored reagents | Check storage temperature and expiration dates of labeled substrates. | Use new, properly stored batches of reagents. |
| Insufficient substrate dosage | Review literature for age- and weight-appropriate dosages. | Re-run the experiment with an optimized, validated dose. |
| Protocol not suited to population | Evaluate if the test duration or fasting period is too long for the study population (e.g., young children). | Modify the protocol to shorten test time or fasting as needed [12]. |
| Equipment malfunction | Run a calibration test or use a known standard to verify equipment function. | Service or calibrate the analytical instrument (e.g., mass spectrometer). |
Problem: Inconsistent results between test runs under seemingly identical conditions.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Uncontrolled variables | Document all experimental conditions meticulously. Change only one variable at a time between runs to isolate the cause [48]. | Implement a standardized checklist for all experimental procedures. |
| Participant non-compliance | Use questionnaires or interviews to verify adherence to pre-test instructions (e.g., fasting). | Improve participant education and communication before the test. |
| Subclinical degree of malabsorption | The test might be detecting mild or variable impairment. | Increase sample size or use a more sensitive test as a confirmatory measure. |
Experimental Protocols for Key Macronutrient Absorption Tests
The following table summarizes key non-invasive tests for assessing macronutrient malabsorption, which are vital for creating a comprehensive test battery [12] [8].
Table 1: Battery of Non-Invasive Tests for Macronutrient Malabsorption
| Macronutrient | Test Name | Function Tested | Protocol Overview | Key Indicators & Normal Values |
|---|---|---|---|---|
| Carbohydrate | 13C-Sucrose Breath Test (SBT) | Global readout of sucrase-isomaltase activity (hydrolysis) and absorption. | Administer 13C-sucrose orally. Collect breath samples at baseline and regular intervals for several hours. | Cumulative percentage of 13C dose recovered (cPDR). Normal values for children are not firmly established and are lab-specific [12]. |
| Carbohydrate | 13C-Starch Breath Test | Global readout of starch digestion by salivary/pancreatic amylase and absorption. | Administer 13C-starch orally. Collect breath samples over time. Often paired with a 13C-glucose test for normalization. | cPDR. A study in healthy children reported a median cPDR of ~35% (range 18-52%) [12]. |
| Fat | 13C-Mixed Triglyceride Breath Test | Assesses pancreatic lipase activity and fat absorption. | Administer a triglyceride substrate labeled with 13C. Measure 13CO2 in breath over time. | cPDR. Lower recovery indicates fat malabsorption, potentially due to exocrine pancreatic insufficiency [12] [8]. |
| Protein | Dipeptide Absorption Test (Bz-Tyr-Ala) | Tests mucosal dipeptide absorptive capacity. | Administer the synthetic dipeptide benzoyl-L-tyrosyl-L-1-13C-alanine. Monitor 13CO2 in breath. | cPDR. Reduced recovery suggests impairment in the peptide transporter function in the intestine [12] [8]. |
Research Workflow and Signaling Pathways
The following diagram illustrates the logical workflow for designing a study protocol and selecting the appropriate test battery for macronutrient malabsorption research.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Materials for Malabsorption Studies
| Item | Function / Role in Experiment |
|---|---|
| 13C-Labeled Substrates (e.g., 13C-sucrose, 13C-starch, 13C-MTG) | The core reagents used in breath tests. They are metabolically "visible" tracers. After ingestion, digestion, and absorption, their oxidation produces 13CO2, which is measured in breath [12] [8]. |
| Standardized Test Meals | Ensure that the vehicle and composition for administering the labeled substrate are consistent across all participants, reducing variability in gastric emptying and absorption. |
| Positive & Negative Control Samples | Essential for verifying test accuracy. Positive controls confirm the test can detect malabsorption, while negative controls ensure specificity. |
| Breath Collection Kits (e.g., airtight bags, vacutainers) | Allow for the non-invasive, serial collection of breath samples from participants at specific time points for later isotope analysis. |
| Isope Ratio Mass Spectrometer (IRMS) | The analytical instrument that precisely measures the ratio of 13CO2 to 12CO2 in breath samples, providing the quantitative data for the test. |
Overcoming Research Hurdles: Standardization, Nutritional Confounders, and Data Interpretation
Addressing the Lack of Standardization in Pediatric and Adult Test Protocols
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: Why can't we simply use adult test protocols for pediatric populations? Children are not miniature adults. Significant differences exist in pharmacokinetics, pharmacodynamics, and immune system development between children and adults, and these factors vary considerably across different pediatric age groups [49]. Using adult protocols can lead to overtesting, misinterpretation of results, and a failure to identify pediatric-specific pathogens [49]. For example, Clostridium difficile testing is not recommended in infants under 12 months because about half are asymptomatically colonized, and a positive test could mislead clinicians from the true cause of diarrhea [49].
Q2: What are the main consequences of inadequate reporting standards in child health research? Poor reporting makes it difficult for clinicians to make wise decisions for pediatric patients and for systematic reviews to perform age-specific subgroup analyses [50]. This ultimately affects the ability of decision-makers to create effective policies and programs for specific pediatric age groups [50]. A 2023 study found that available reporting standards for child health are few, methodologically weak, and poorly implemented [50].
Q3: What non-invasive tests are suitable for measuring macronutrient malabsorption in children? Breath tests are promising, non-invasive tools. The following are particularly relevant for investigating malabsorption in conditions like Environmental Enteropathy (EE) [8] [12]:
- 13C-starch breath test: Measures starch digestion.
- 13C-sucrose breath test: Assesses sucrose digestion.
- 13C-lactose breath test: Identifies lactose malabsorption.
- 13C-mixed triglyceride breath test: Evaluates fat absorption.
- Benzoyl-L-tyrosyl-L-1-13C-alanine breath test: Tests dipeptide absorption [8] [12].
Q4: Are there established guidelines for designing pediatric clinical trials? Yes, the StaR (Standards for Research) Child Health initiative has developed evidence-based guidelines to improve the design, conduct, and reporting of pediatric clinical trials [51]. These standards address child-specific issues like recruitment and consent, selection of outcome measures, and defining appropriate age groups [51].
Troubleshooting Common Experimental Issues
Problem: Inconsistent yield from pediatric blood culture samples.
- Root Cause: Use of adult blood culture bottles with a minimum required volume (e.g., 10 mL) that is impractical to draw from small children, leading to underfilled bottles and reduced bacterial recovery [49].
- Solution: Implement pediatric blood collection bottles, which require a minimum of only 1 mL of blood [49].
- Important Consideration: Ongoing education for nurses and phlebotomists is critical. The volume of blood drawn should be appropriate to the patient's size, and the practice of collecting a minimal 1 mL sample should not be universally applied to larger pediatric patients [49].
Problem: High rate of asymptomatic bacteriuria reporting in pediatric urine cultures.
- Root Cause: Culturing all urine specimens regardless of urinalysis (UA) findings, similar to adult protocols. In pediatric patients, a negative UA makes a true urinary tract infection very unlikely [49].
- Solution: Implement an algorithmic approach. First, perform a UA to check for pyuria (white blood cells in urine). Only proceed to culture if the UA is positive, unless the patient is immunocompromised [49].
- Exception: This algorithm may not be appropriate for immunocompromised patients (e.g., oncology) who may not elicit a sufficient immune response to produce pyuria [49].
Problem: Lack of standardized age groups for pediatric trial analysis.
- Root Cause: Historically, age groupings have been arbitrary, making it difficult to compare or pool data across different studies [51].
- Solution: The StaR Child Health standard recommends considering the use of age groupings proposed by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and to pool data with other studies of the same age group when possible [51].
Experimental Protocols for Macronutrient Malabsorption
Protocol 1: 13C-Sucrose Breath Test (SBT) for Sucrose Malabsorption
- Principle: This test provides a global readout of sucrose digestion by the brush-border enzyme sucrase-isomaltase and subsequent absorption. A patient ingests a stable isotope (13C)-labeled sucrose substrate, and the 13CO2 in their breath is measured over time. Reduced 13CO2 excretion indicates malabsorption [12].
- Detailed Methodology:
- Patient Preparation: The patient must fast overnight (duration as per standardized protocol for the child's age).
- Baseline Breath Sample: Collect one or more baseline breath samples before substrate administration.
- Substrate Administration: Administer a test meal containing a defined dose of 13C-sucrose.
- Breath Sample Collection: Collect breath samples at regular intervals (e.g., every 15-30 minutes) for a test duration of 1.5 to 6 hours [8].
- Analysis: Measure the 13C/12C isotope ratio in the breath samples using isotope ratio mass spectrometry.
- Data Expression: Calculate the cumulative percentage of the 13C dose recovered over time (cPDR). Results are compared against established normal values for the patient's age group [12].
Protocol 2: 13C-Mixed Triglyceride Breath Test for Fat Malabsorption
- Principle: This test detects exocrine pancreatic insufficiency. A 13C-labeled mixed triglyceride is ingested. Normal pancreatic lipase activity releases 13C-fatty acids, which are absorbed and metabolized, producing 13CO2. Low levels of 13CO2 in breath suggest impaired fat digestion [12].
- Detailed Methodology:
- Patient Preparation: The patient must fast overnight.
- Baseline Breath Sample: Collect a baseline breath sample.
- Substrate Administration: Administer a test meal containing a known quantity of 13C-mixed triglyceride.
- Breath Sample Collection: Collect breath samples at regular intervals over a period of 4-6 hours.
- Analysis: Analyze the 13C enrichment in breath samples via isotope ratio mass spectrometry.
- Interpretation: The results, often expressed as the cumulative % dose recovered or a specific time-point value, are compared to age-specific normative data. Lower values indicate fat malabsorption [8] [12].
Data Presentation
Table 1: Evidence Gaps in Pediatric Clinical Microbiology Protocols
| Testing Area | Specific Challenge | Consequence of Using Adult Protocols | Potential Pediatric-Specific Solution |
|---|---|---|---|
| Blood Cultures | Optimal blood volume for culture | Underfilled adult bottles → low bacterial yield | Use pediatric bottles & continuous staff education on volume [49] |
| Urinalysis & Culture | Significance of bacteria in urine | High reporting of asymptomatic bacteriuria | Implement UA-based algorithmic culture to reduce unnecessary treatment [49] |
| C. difficile Testing | Asymptomatic colonization in infants | Misdiagnosis and distraction from true cause of diarrhea | Reject specimens from patients <12 months (per AAP guideline) [49] |
Table 2: Key Recommendations from StaR Child Health Guidelines
| Standard Area | Core Recommendation | Application in Trial Design |
|---|---|---|
| Consent & Recruitment | Seek to approach all eligible patients; recognize a child's objection to participation. | Ensure equitable recruitment strategies and have clear protocols for child assent [51]. |
| Containing Risk of Bias | Use appropriate randomization and blinding; pre-specify all outcomes and analyses. | Register the trial before initiation and report according to CONSORT guidelines [51]. |
| Sample Sizes | Always perform sample size calculations in consultation with a statistician. | Use standard methods when information is available from the pediatric population of interest [51]. |
| Age Groups | Consider the effect of developmental changes; use standardized age groupings (e.g., NICHD). | Pool data with other studies of the same age group to perform age-specific analyses [51]. |
Research Reagent Solutions
Table 3: Essential Reagents for Macronutrient Malabsorption Breath Tests
| Reagent | Function in Experiment | Key Consideration |
|---|---|---|
| 13C-Sucrose | Stable isotope-labeled substrate to probe sucrase-isomaltase activity and monosaccharide absorption. | Requires a standardized, age-appropriate dose and a palatable test meal for pediatric compliance [12]. |
| 13C-Mixed Triglyceride | Stable isotope-labeled substrate to probe the efficiency of pancreatic lipase-mediated fat digestion. | The test meal's fat content must be controlled, as it influences gastric emptying and absorption [8] [12]. |
| Benzoyl-L-tyrosyl-L-1-13C-alanine | A synthetic dipeptide used to assess peptide transport function across the intestinal brush border. | Helps diagnose protein malabsorption, which is less studied than carbohydrate or fat malabsorption [8]. |
| Breath Collection Bags/Containers | For the non-invasive collection of exhaled breath samples at multiple time points. | Must be airtight and designed for easy use by children to ensure sample integrity and compliance [8]. |
Experimental and Conceptual Workflows
Mitigating the Impact of Baseline Nutritional Status on Study Outcomes
Technical Support Center: FAQs & Troubleshooting Guides
Frequently Asked Questions (FAQs)
FAQ 1: Why is assessing baseline nutritional status critical in clinical research populations?
Evaluating a participant's baseline nutritional status is vital because malnutrition is an independent predictor of mortality and can significantly confound study outcomes [52]. Nutritional status reflects the body's functional capacity and protein-energy reserves, which are essential for responding to disease and treatment. In research, a poor nutritional status, often identified by high CONUT (CONtrolling NUTritional) scores, is strongly linked to increased complications, mortality, and intubation rates, especially in critically ill populations [52]. Failure to account for this can introduce significant bias and mask the true effect of an intervention.
FAQ 2: What are the common mechanisms of macronutrient malabsorption I should consider in my study design?
Macronutrient malabsorption can occur through several mechanisms, often categorized by the phase of absorption that is impaired [10]:
- Luminal Phase (Digestion): Defective intraluminal hydrolysis of nutrients. This is commonly caused by exocrine pancreatic insufficiency (reducing lipase, protease, and amylase output), insufficient bile salt secretion, or defects in gastric acid and pepsin secretion [10].
- Mucosal Phase (Absorption): Defective uptake by the intestinal mucosa. Conditions like Environmental Enteric Dysfunction (EED) or celiac disease damage the intestinal lining, impairing the function of brush border enzymes and transporters [12].
- Post-Absorptive Phase: Impairments in the processing and transport of absorbed nutrients via the lymphatic and portal systems.
FAQ 3: Which non-invasive tests can I use to detect macronutrient malabsorption in field studies or sensitive populations?
Breath tests are promising, non-invasive tools for measuring digestive and absorptive capacity [12].
- ^13C-Sucrose Breath Test (SBT): Assesses sucrase-isomaltase activity at the intestinal brush border.
- ^13C-Starch Breath Test: Evaluates the completeness of starch digestion by salivary and pancreatic amylase.
- ^13C-Mixed Triglyceride Breath Test: Measures lipolysis by pancreatic lipase, indicating fat digestion.
- Benzoyl-L-tyrosyl-L-1-^13C-alanine Test: A dipeptide test that can probe mucosal absorptive function.
These tests work by measuring the exhalation of ^13CO₂ after ingestion of a ^13C-labeled substrate, which indicates the substrate's digestion, absorption, and subsequent metabolism [12].
Troubleshooting Guides
Problem 1: Unexpectedly High Mortality or Complication Rates in Study Cohort
- Identify the Problem: A higher-than-anticipated rate of death, intubation, or other severe outcomes is observed, potentially skewing the primary endpoint analysis [52].
- Diagnose the Cause: This is often linked to unaccounted-for patient vulnerability. A key variable to investigate is baseline nutritional status. As demonstrated in ICU studies, a high CONUT score (≥5) is a significant independent risk factor for mortality, even after correcting for other covariates like age and comorbidity burden [52] [53].
- Implement a Solution:
- Retrospectively analyze existing data using a validated nutritional scoring system like the CONUT score.
- Prospectively stratify randomization and analysis by nutritional risk groups (e.g., low vs. high CONUT score) to isolate the intervention's effect from the impact of malnutrition [52].
- Adjust statistical models for nutritional status as a covariate.
Problem 2: Suspected Micronutrient or Macronutrient Malabsorption Affecting Biomarker Levels
- Identify the Problem: Biomarkers related to vitamin status, protein levels (e.g., albumin), or immune function (e.g., lymphocyte count) are consistently lower than expected, suggesting poor absorption rather than a primary deficiency [52] [10].
- Diagnose the Cause: Malabsorption can be caused by subclinical conditions like Environmental Enteric Dysfunction (EED), which is prevalent in settings with poor sanitation and is characterized by villous atrophy and inflammation [12]. This can lead to fat, lactose, and carbohydrate malabsorption.
- Implement a Solution:
- Incorporate functional tests like the ^13C-labeled breath tests mentioned above to quantify the degree of malabsorption [12].
- Use a combination of biomarkers. The CONUT score, for example, uses serum albumin (protein reserve), total cholesterol (caloric depletion), and total lymphocyte count (immunological status) to provide a integrated picture of nutritional status [52].
- Consider pathogen screening and measures of intestinal inflammation (e.g., fecal calprotectin, myeloperoxidase) to diagnose EED where biopsy is not feasible [12].
Methodologies and Data Presentation
Table 1: The CONUT Nutritional Assessment Score [52]
This table details the scoring system used to calculate the CONUT score, a tool for identifying patients at nutritional risk.
| Parameter | Score 0 | Score 1 | Score 2 | Score 3 | Score 4 |
|---|---|---|---|---|---|
| Serum Albumin (g/dL) | ≥3.5 | 3.0–3.49 | 2.5–2.9 | <2.5 | |
| Total Cholesterol (mg/dL) | ≥180 | 140–179 | 100–139 | <100 | |
| Total Lymphocyte (count/mm³) | ≥1600 | 1200–1599 | 800–1199 | <800 | |
| Interpretation: Total Score: 0-1 (Normal), 2-4 (Mild), 5-8 (Moderate), 9-12 (Severe) malnutrition. |
Table 2: Functional Tests for Macronutrient Malabsorption [12]
This table summarizes non-invasive tests suitable for assessing digestive and absorptive function in research populations.
| Test Target | Test Method | Function Probed | Key Advantage |
|---|---|---|---|
| Fat Digestion | ^13C-Mixed Triglyceride Breath Test | Pancreatic lipase activity | Non-invasive; suitable for children and field studies |
| Carbohydrate Absorption | ^13C-Sucrose Breath Test (SBT) | Sucrase-isomaltase (brush border) activity | Probes mucosal health without biopsy |
| Carbohydrate Digestion | ^13C-Starch Breath Test | Salivary & pancreatic amylase function | Assesses global starch digestion |
| Mucosal Function | Benzoyl-L-tyrosyl-L-1-^13C-alanine Test | Dipeptide absorption | Tests intestinal peptide transport |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Assessing Nutritional Status and Malabsorption
| Reagent / Material | Function in Research |
|---|---|
| CONUT Score Components | Provides a rapid, automated nutritional risk screening using routine lab data (albumin, cholesterol, lymphocytes) [52]. |
| ^13C-Labeled Substrates (e.g., mixed triglyceride, sucrose, starch) | The core reagent for non-invasive breath tests to quantify specific macronutrient digestion and absorption capacity [12]. |
| Serum Albumin Assay Kit | Measures protein reserves, a key component of nutritional status and a predictor of clinical outcomes [52]. |
| Lymphocyte Count Assay | Evaluates immune competence, which is compromised in malnutrition and is part of the CONUT score [52]. |
Experimental Workflow Diagrams
Flowchart for Integrating Nutritional Status in Research
Generalized Troubleshooting Workflow
Optimizing Pancreatic Enzyme Replacement Therapy (PERT) in Study Cohorts
Troubleshooting Guides & FAQs
Frequently Asked Questions from a Research Perspective
Q1: What is the evidence-based minimum effective dosage of lipase for a main meal in post-pancreatectomy patients? A1: A systematic review of randomized controlled trials indicates that an effective dosage should consist of at least 40,000 PhEur units of lipase per main meal to treat exocrine pancreatic insufficiency (EPI) following pancreatoduodenectomy [54].
Q2: How should researchers standardize the timing of PERT administration in study protocols to maximize nutrient digestion? A2: Research protocols should stipulate that PERT capsules are taken with the first bite of food to ensure the enzymes move through the digestive system concurrently with the meal. Dosing should be spread throughout the meal, with one capsule at the start, another halfway through, and a final one at the end for optimal mixing with the chyme [55].
Q3: What are the critical methodological pitfalls in assessing PERT adherence and efficacy in a cohort study? A3: A significant pitfall is not adjusting the enzyme dose for dietary fat intake. Prescribing PERT adjusted to a fixed ratio of lipase units per gram of dietary fat intake is more appropriate than a fixed dose per meal, as fat intake can vary significantly between meals. One study found that despite a recommendation of 40,000 units per meal, the actual ratio of lipase to dietary fat varied widely, from 2,521 to 4,441 units/gram fat across different meals [54].
Q4: In a study population with dietary restrictions (e.g., Kosher, Halal, vegetarian), how should the porcine origin of standard PERT be managed? A4: Currently, all first-line PERT products are derived from pork. For participants with religious restrictions, it is documented that special dispensation has been granted by religious organizations, as these are essential medicines. For participants who remain unwilling, researchers should consult with their healthcare provider regarding the feasibility of plant-based enzyme replacement therapy, though this is not a like-for-like replacement [56] [55].
Q5: What are the key nutritional outcome measures, beyond weight change, for evaluating PERT efficacy in a clinical trial? A5: Beyond simple body weight, key nutritional endpoints should include:
- Prognostic Nutritional Index (PNI): Calculated from serum albumin and lymphocyte count [57].
- Patient-Generated Subjective Global Assessment (PG-SGA) Score: A validated tool for nutritional status in cancer patients [57].
- Stool Characteristics: Reduction in steatorrhea (fatty, oily stools) is a direct marker of improved fat absorption [55] [58].
Experimental Protocols & Methodologies
Protocol 1: Establishing an EPI Diagnosis in a Research Cohort
Objective: To consistently identify participants with Exocrine Pancreatic Insufficiency for inclusion in a PERT intervention study.
Methodology:
- Clinical Symptom Screening: Recruit subjects presenting with at least one of the following symptoms of malabsorption [55] [58]:
- Steatorrhea (fatty, oily, foul-smelling stool that floats)
- Unexplained weight loss
- Abdominal bloating and pain
- Increased gas and flatulence
- Confirmatory Diagnostic Testing: Confirm EPI in symptomatic subjects using one of these objective measures [57]:
- Fecal Elastase-1 Test (FE-1): A value of ≤200 μg/g of stool is considered diagnostic for EPI.
- Direct Pancreatic Function Test: The gold standard, though more invasive.
Protocol 2: Dosing and Administration of PERT in a Clinical Study
Objective: To ensure standardized and effective administration of pancreatic enzyme replacement therapy.
Methodology:
- Determining Initial Dose:
- Administration Procedure:
- Instruct participants to swallow capsules whole with a cold or room-temperature liquid. Hot liquids can denature the enzymes [56] [55].
- Capsules must be taken with the first mouthful of food and the dose spread throughout the meal [55].
- For participants with dysphagia, capsules can be opened, and the intact granules mixed with a small amount of acidic soft food (e.g., applesauce, yogurt) and swallowed immediately without chewing [56] [55].
- Dose Titration:
Data Presentation: Efficacy of PERT
Table 1: Impact of PERT on Nutritional and Survival Outcomes in Advanced Pancreatic Cancer
Data derived from a retrospective cohort study of 501 patients with advanced PDAC and EPI [57].
| Outcome Measure | PERT Group (n=188) | Non-PERT Group (n=313) | P-value |
|---|---|---|---|
| Weight Change (kg) over ~8 weeks | -1.5 kg | -2.5 kg | 0.04 |
| Change in Prognostic Nutritional Index (PNI) | -1.9 | -3.0 | 0.01 |
| Change in PG-SGA Score | -8.4 | -6.0 | 0.02 |
| Median Overall Survival (Months) | 17.1 | 12.5 | 0.001 |
Table 2: PERT Dosing and Dietary Fat Integration
Data on PERT dosing adequacy and its relationship to meal fat content from a prospective observational study [54].
| Parameter | Findings | Research Implication |
|---|---|---|
| Recommended Min. Dose | ≥40,000 PhEur lipase units/main meal | A standard baseline for study protocols. |
| Adherence to Recommendation | 52% of patients (15/29) | Highlights a common point of protocol non-adherence. |
| Lipase-to-Fat Ratio (Dinner) | 2,521 ± 1,770 units/gram fat | Suggests dosing based on fat intake (e.g., 2,500-4,500 units/g fat) may be more precise than fixed dosing. |
| Lipase-to-Fat Ratio (Breakfast) | 4,441 ± 6,936 units/gram fat | Indicates high variability in fat intake per meal, reinforcing the need for meal-specific dosing. |
Experimental Workflow Visualization
Research Workflow for PERT Intervention Studies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for PERT Research
| Item / Reagent | Function in Research | Example Brands / Types |
|---|---|---|
| Pancreatic Enzyme Supplements | The primary intervention; replaces missing digestive enzymes (lipase, protease, amylase). | Creon, Nutrizym, Pancrease, Pancrex, Zenpep [56] [55] |
| Fecal Elastase-1 (FE-1) Test | Gold-standard non-invasive test for objectively confirming EPI diagnosis in study subjects. | Immunoassay-based test kits [57] |
| Patient-Generated Subjective Global Assessment (PG-SGA) | Validated patient-reported instrument for assessing nutritional status in oncology cohorts. | PG-SGA Short Form [57] |
| Dietary Fat Intake Logs / Software | Critical for calculating lipase-to-fat ratios and customizing PERT dosing in nutritional analyses. | 24-hour recall interviews, food frequency questionnaires [54] |
| Prognostic Nutritional Index (PNI) | Composite metric derived from serum albumin and lymphocyte count; an objective nutritional endpoint. | Calculated as: 10Albumin (g/dL) + 0.005Lymphocyte Count (/mm³) [57] |
Navigating Dietary Restrictions and Food Avoidance in Research Participants
Troubleshooting Guides
Participant Recruitment and Adherence Challenges
Problem: High dropout rates in populations with pre-existing dietary restrictions
- Potential Cause: Research diets conflict with established eating patterns due to sensory sensitivity or food-related anxiety [59] [60].
- Solution: Implement validated screening tools (e.g., the Nine Item Avoidant/Restrictive Food Intake Disorder (ARFID) Screen) during recruitment to identify potential conflicts. Offer dietary choices within protocol parameters to accommodate sensory preferences [61].
- Preventive Measure: Design study diets with customizable options for key sensory properties (texture, flavor) while maintaining nutritional equivalence.
Problem: Suspected macronutrient malabsorption affecting study outcomes
- Potential Cause: Underlying gastrointestinal conditions not identified during screening [62].
- Solution: Implement baseline malabsorption testing for at-risk populations. The D-xylose test can assess carbohydrate absorption, while 72-hour fecal fat collection identifies fat malabsorption [62].
- Alternative Approach: For studies where malabsorption is an exclusion criterion, utilize breath tests (e.g., hydrogen breath test for lactose intolerance) as a cost-effective screening tool [62].
Data Collection and Compliance Issues
Problem: Inaccurate dietary recall in populations with disordered eating patterns
- Potential Cause: Individuals with ARFID may underreport due to shame or lack of awareness about the significance of their restrictions [60].
- Solution: Supplement 24-hour recalls with mobile food photography to objectively document intake without reliance on memory or estimation.
- Protocol Adjustment: Implement the Remote Food Photography Method (RFPM) validated for eating disorder populations to reduce participant burden and increase data accuracy.
Problem: Inconsistent supplement adherence in malabsorption studies
- Potential Cause: Gastrointestinal discomfort from high-dose supplements, particularly in pancreatic insufficiency or biliary disease [62].
- Solution: Titrate dosage gradually and provide medium-chain triglyceride (MCT) oil as an alternative fat source that doesn't require pancreatic enzymes for absorption [62].
- Monitoring Protocol: Use riboflavin biomarkers in urine to verify compliance with supplemented products.
Frequently Asked Questions (FAQs)
Study Design Considerations
Q: What prevalence of ARFID should we anticipate in general population studies?
A: Recent epidemiological studies indicate ARFID affects approximately 2.84% in nonclinical populations and up to 12.0% in clinical populations. The condition affects individuals across all age groups, confirming it as an age-independent condition [61].
Q: How do we differentiate ARFID-related food avoidance from other eating disorders?
A: The key distinction is that ARFID does not involve weight or shape concerns characteristic of anorexia nervosa or bulimia nervosa. Instead, it typically presents in three primary profiles:
- Sensory sensitivity (picky eating) - strong preferences based on food characteristics
- Fear of aversive consequences - concern about choking, vomiting, or allergic reactions
- Lack of interest in food or eating [59] [60]
Assessment and Measurement
Q: What assessment tools are validated for identifying food avoidance in research participants?
A: Several validated instruments are available:
- ARFID Scale - assesses three primary dimensions of the disorder
- Children's Eating Behavior Questionnaire (CEBQ) - includes food fussiness subscale [63]
- Child Feeding Questionnaire (CFQ) - evaluates parental feeding practices that may influence child eating behaviors [63]
Q: What laboratory markers are essential for monitoring nutritional status in restriction studies?
A: The essential biomarkers include:
Table: Essential Nutritional Biomarkers for Dietary Restriction Studies
| Biomarker Category | Specific Tests | Clinical Significance |
|---|---|---|
| Macronutrient Status | Prealbumin, Transferrin | Short-term protein status assessment |
| Micronutrient Status | Ferritin, 25-OH Vitamin D, B12, Folate | Identifies common deficiencies |
| Fat Malabsorption | Fecal elastase, Fecal fat quantification | Pancreatic function assessment |
| Carbohydrate Malabsorption | Hydrogen breath testing | Identifies disaccharidase deficiencies [62] |
Methodological Considerations
Q: How can we accommodate sensory sensitivities while maintaining protocol integrity?
A: Implement these strategies:
- Sensory-matched placebos that account for texture, color, and mouthfeel
- Graded exposure protocols for introducing study foods or supplements
- Multiple formulation options (liquid, powder, solid) with equivalent nutrient profiles
- Systematic desensitization procedures administered by study dietitians [59]
Q: What ethical considerations are unique to studying populations with dietary restrictions?
A: Key considerations include:
- Therapeutic misconception - clarifying that study participation may not resolve underlying eating pathology
- Nutritional risk mitigation - implementing stopping rules based on weight loss or deficiency markers
- Disclosure protocols for identifying clinically significant ARFID symptoms that require treatment referral [61] [60]
Experimental Protocols
Protocol for Assessing Macronutrient Absorption
Objective: To quantify malabsorption of carbohydrates, fats, and proteins in research participants with dietary restrictions.
Materials:
- D-xylose solution (25g/250mL water)
- Sterile containers for blood and stool collection
- Hydrogen breath test equipment
- Laboratory equipment for biochemical analyses
Procedure:
- Participant Preparation:
- 3-day lead-in diet with standardized fat content (100g/day)
- 12-hour fast prior to testing with water permitted ad libitum
Carbohydrate Absorption Assessment:
- Administer 25g D-xylose in 250mL water
- Collect venous blood at 0, 30, 60, and 120 minutes
- Interpretation: Blood D-xylose <20mg/dL at 120 minutes suggests malabsorption [62]
Fat Absorption Assessment:
- Collect 72-hour stool specimen while maintaining 100g fat diet
- Homogenize and aliquot stool for analysis
- Interpretation: Fecal fat >7g/24h indicates steatorrhea [62]
Breath Testing Protocol:
- Baseline breath sample collection
- Administer test carbohydrate (lactose, fructose, etc.)
- Collect breath samples at 15, 30, 60, 90, and 120 minutes
- Interpretation: Hydrogen increase >20ppm indicates malabsorption [62]
Quality Control: Include positive and negative controls in each assay batch. Process samples within 2 hours of collection or store at -80°C.
Protocol for Food Rechallenge in Avoidant Populations
Objective: To systematically evaluate adverse food reactions in participants with food avoidance.
Materials:
- Blinded food challenges (active and placebo)
- Visual Analog Scales (VAS) for symptom rating
- Standardized food preparation equipment
- Emergency equipment for anaphylaxis management
Procedure:
- Single-blind, placebo-controlled food challenge:
- Prepare active and placebo materials matched for sensory properties
- Administer increasing doses at 15-20 minute intervals
- Monitor for objective and subjective adverse reactions
Symptom Assessment:
- Utilize validated scales (e.g., Food Allergy Quality of Life Questionnaires)
- Record physiological parameters (heart rate, respiratory rate)
- Document behavioral responses to food presentation [60]
Graded Exposure Protocol:
- Begin with visual exposure only
- Progress to olfactory exposure
- Advance to tactile interaction with food
- Final step: tasting and swallowing [59]
Safety Considerations: Establish stopping criteria based on symptom severity. Maintain emergency medications and equipment on-site.
Signaling Pathways and Workflows
Macronutrient Absorption Pathway
Diagram: Macronutrient Digestion and Absorption Pathway
Dietary Restriction Assessment Workflow
Diagram: Dietary Restriction Assessment Workflow
Research Reagent Solutions
Table: Essential Reagents for Dietary Restriction Research
| Reagent Category | Specific Products | Research Application | Protocol Considerations |
|---|---|---|---|
| Carbohydrate Absorption | D-xylose, Lactulose, Hydrogen breath test kits | Quantifying carbohydrate malabsorption | Administer after 12-hour fast; contraindicated in diabetes [62] |
| Fat Absorption | 72-hour fecal fat collection kits, Medium-chain triglycerides | Assessing steatorrhea and fat digestion capacity | Require standardized 100g fat diet prior to testing [62] |
| Protein Status | Prealbumin, Transferrin, Urinary nitrogen kits | Monitoring protein-energy status and turnover | Prealbumin has shorter half-life than albumin for acute changes [64] |
| Sensory Testing | Taste strips, Texture-modified foods, Olfactory stimuli | Evaluating sensory sensitivity contributions | Standardize administration; control for recent food intake [59] |
| Biomarker Analysis | ELISA kits for vitamin and mineral assays, Inflammatory markers | Objective nutritional status assessment | Process samples promptly; follow stability guidelines [64] [62] |
Standardized Data Collection Tools
For consistent assessment across studies, implement these validated instruments:
- Nutrition Knowledge Questionnaire (adapted from Abridged Nutrition for Sport Knowledge Questionnaire) [63]
- Child Feeding Questionnaire (CFQ) - assesses parental feeding practices [63]
- Food Fussiness Scale from the Child Eating Behavior Questionnaire (CEBQ) [63]
Dietary Adherence Scoring
Calculate dietary guideline adherence using a seven-component score assessing:
- Red and processed meat consumption
- Fish intake
- Dairy consumption
- Fruit and vegetable intake
- Confectionery consumption
- Beverage choices [63]
This systematic approach to navigating dietary restrictions and food avoidance in research participants will enhance data quality while maintaining ethical standards and participant safety in nutrition research.
Differentiating Malabsorption from Maldigestion in Data Analysis
Frequently Asked Questions (FAQs)
Q1: What is the core pathophysiological difference between maldigestion and malabsorption?
Maldigestion refers specifically to the inability to break down large nutrient molecules (proteins, fats, carbohydrates) into their smaller constituents within the intestinal lumen. This is often due to deficiencies in digestive enzymes or bile [1] [65].
In contrast, malabsorption is the inability to transport these properly digested nutrients across the intestinal mucosa into the bloodstream for systemic use. This typically results from damage to the intestinal mucosa or defects in specific transport systems [1] [9].
While distinct, the processes are interdependent, and the term "malabsorption" is often used clinically to encompass both disorders [3].
Q2: How can research data on stool fat content help distinguish the underlying cause?
Quantitative fecal fat analysis is a key test. The results can point toward different etiologies, though they are not definitive on their own. The following table summarizes how the degree of steatorrhea can guide differential diagnosis:
| Fat Excretion (g/24h on 100g fat diet) | Severity | Common Associated Conditions |
|---|---|---|
| 10-30 g | Mild to Moderate | Bile acid deficiency, Small Intestinal Bacterial Overgrowth (SIBO), Celiac disease [66] |
| >30-60 g | Moderate | Significant mucosal disease (e.g., Celiac disease) [66] |
| >60-100 g | Severe | Pancreatic insufficiency (e.g., Chronic Pancreatitis, Cystic Fibrosis), major bowel resection [66] |
Q3: What specific breath tests can pinpoint carbohydrate maldigestion versus malabsorption?
Breath tests are non-invasive tools to assess carbohydrate handling. The table below outlines common applications:
| Breath Test | Substrate | Primary Mechanism Assessed | Typical Diagnostic Use |
|---|---|---|---|
| Hydrogen Breath Test | Lactose, Lactulose, Glucose | Bacterial fermentation of unabsorbed carbohydrate in the colon, producing hydrogen [17] [62] | Lactose intolerance (maldigestion), SIBO, general carbohydrate malabsorption [9] |
| ¹³C-Substrate Breath Test | ¹³C-Lactose, ¹³C-Sucrose, ¹³C-Starch | Enzymatic digestion and subsequent absorption of the ¹³C-labeled substrate, with measurement of ¹³CO₂ in breath [8] | Specific disaccharidase deficiencies (maldigestion), generalized mucosal absorptive capacity [8] |
Q4: Which blood and urine biomarkers are essential for differentiating nutrient deficiencies in study populations?
Serum biomarkers can identify specific nutrient deficiencies resulting from malabsorption/maldigestion. Key biomarkers and their implications include:
- Carotene (Vitamin A precursor): Low levels are a useful screening marker for fat malabsorption as it is a fat-soluble vitamin [62].
- Vitamin B12 and Folate: Deficiencies indicate impaired absorption. B12 deficiency is associated with ileal disease/resection (malabsorption) or pernicious anemia (lack of intrinsic factor), while folate deficiency is more common in proximal small bowel diseases [17] [65].
- Iron and Calcium: Malabsorption of these minerals is often seen in duodenal and proximal jejunal diseases like Celiac disease [62].
- 25-Hydroxy Vitamin D: A low level is a sensitive marker for fat-soluble vitamin malabsorption [17].
- Prothrombin Time (PT): Prolonged PT can indicate Vitamin K deficiency, another fat-soluble vitamin malabsorption sign [17].
- D-xylose Test: This involves administering D-xylose sugar and measuring its levels in blood or urine. Abnormal absorption suggests a mucosal absorption problem, while normal absorption in the context of steatorrhea points toward pancreatic maldigestion [66] [62].
Q5: What is the definitive procedure for confirming mucosal vs. luminal causes in a research setting?
Upper endoscopy with small bowel mucosal biopsy and histologic examination is the definitive method for confirming mucosal causes of malabsorption. This procedure allows for the direct diagnosis of conditions such as Celiac disease, Whipple's disease, giardiasis, and abetalipoproteinemia [17]. For luminal causes, tests of pancreatic function (e.g., fecal elastase, secretin stimulation test) or bile acid metabolism (e.g., bile acid breath test, SeHCAT test) are required [17] [65].
Troubleshooting Guides
Guide 1: Interpreting Discrepant Fat and D-Xylose Test Results
Problem: Research data shows conflicting results between quantitative fecal fat analysis and the D-xylose absorption test.
Interpretation Framework: This discrepancy is a classic way to differentiate maldigestion from malabsorption.
- If Fecal Fat is HIGH and D-xylose is ABNORMAL: This combination suggests a mucosal malabsorption problem (e.g., Celiac disease, tropical sprue). The damaged intestine cannot absorb either fats or carbohydrates properly [66].
- If Fecal Fat is HIGH and D-xylose is NORMAL: This points toward a luminal maldigestion problem, such as pancreatic exocrine insufficiency or bile acid deficiency. The intestinal mucosa is healthy and can absorb D-xylose, but the nutrients are not properly broken down for absorption [66].
Guide 2: Diagnosing Bile Acid Malabsorption (BAM)
Problem: Study participants present with chronic watery diarrhea and evidence of fat malabsorption, but pancreatic function is normal.
Investigation Protocol:
- Clinical Context: Suspect BAM in participants with a history of ileal resection (e.g., for Crohn's disease), cholecystectomy, or radiation enteritis [17] [62].
- Pathophysiology: The ileum is the primary site for bile acid reabsorption. If diseased or removed, bile acids are not recycled, leading to:
- Reduced intraluminal bile acid concentration, impairing micelle formation and fat digestion (steatorrhea).
- Spillage of bile acids into the colon, which stimulates water and electrolyte secretion, causing secretory diarrhea [62].
- Diagnostic Tests:
- ⁷⁵Selenium HomotauroCholic Acid Test (SeHCAT): Considered the gold standard in many regions. It measures bile acid retention.
- Fecal Bile Acid Assays: Directly measure levels of bile acids in stool [65].
- Serum C4 (7α-hydroxy-4-cholesten-3-one): A marker for bile acid synthesis; high levels indicate increased synthesis to compensate for losses [3].
The diagram below illustrates the pathophysiology and consequences of bile acid malabsorption.
Guide 3: A Stepwise Algorithm for Differential Diagnosis
Follow this logical workflow to systematically analyze data and narrow down the cause of malabsorption in a research cohort.
The Scientist's Toolkit: Key Reagents & Experimental Materials
| Research Reagent / Material | Primary Function in Experimentation |
|---|---|
| ¹³C-labeled Substrates (e.g., ¹³C-Mixed Triglyceride, ¹³C-Sucrose) | Non-invasive tracers for specific nutrient digestion and absorption studies using breath tests [8] [67]. |
| Stable Isotope-labeled Proteins (e.g., ¹³C, ¹⁵N, ²H-labeled egg protein) | Intrinsic tracers to quantify protein digestion, malabsorption, and colonic fermentation in kinetic studies [67]. |
| D-Xylose | A carbohydrate probe used to assess the integrity of the intestinal mucosal absorptive capacity independent of pancreatic function [17] [66]. |
| Fecal Elastase-1 Immunoassay Kits | A non-invasive and specific method to assess pancreatic exocrine function; low levels indicate pancreatic insufficiency [17]. |
| Hydrogen Breath Test Kits (Lactulose, Lactose, Glucose) | Standardized substrates to detect carbohydrate malabsorption and small intestinal bacterial overgrowth via H₂ gas production [17] [62]. |
| Secretin | A hormone used in direct pancreatic function testing (e.g., secretin-stimulation test) to measure bicarbonate output from the pancreas [66]. |
Technical Support Center
Frequently Asked Questions (FAQs)
FAQ 1: Why is a child's age a critical variable in malabsorption research? The digestive system matures significantly after birth. Key digestive enzymes and nutrient transporters exhibit specific ontogenetic trajectories, meaning their presence and activity levels change with age and dietary exposure. For example, pancreatic amylase activity is very low at one month of life and increases with the introduction of complementary foods, reaching adult levels only around two years of age. Similarly, the activity of the lactase-phlorizin hydrolase (LPH) enzyme declines after breastfeeding ceases in many populations. Therefore, an experimental protocol that does not account for the age-specific digestive capacity of its pediatric cohort risks misinterpreting results, as a negative finding could be due to developmental immaturity rather than a pathological condition [8].
FAQ 2: What are the common methodological pitfalls when measuring fat malabsorption in infants? A primary pitfall is the assumption that fat absorption mechanisms are fully mature. In young infants, fat absorption can be less efficient due to a combination of factors: lower bile salt pool size, reduced pancreatic lipase output, and the immaturity of the intestinal lymphatic system. Furthermore, using a breath test protocol designed for adults without modification for infants can lead to errors. For instance, in children under two years, the natural abundance of 13C in breastmilk or previous day's diet can dilute the body's 13C pool, skewing the results of a 13C-mixed triglyceride breath test. Accurate measurement requires protocols tailored to the ontogenetic stage, including considerations of fasting duration and test meal composition [12] [8].
FAQ 3: How does Environmental Enteric Dysfunction (EED) confound nutrient absorption studies? Environmental Enteric Dysfunction (EED) is a subclinical condition characterized by villous atrophy and inflammation of the gut. It creates a state of generalized malabsorption by damaging the intestinal mucosa, which is the primary site for nutrient absorption. In a research setting, EED can be a major confounding variable because it can cause malabsorption of multiple macronutrients simultaneously—most notably fat and lactose. If a study is designed to investigate the absorption of a specific nutrient (e.g., a novel protein), the underlying presence of EED in the study population could lead to falsely attributed results. Screening for EED using validated biomarker panels or functional tests is essential to isolate the effect of the intervention being studied [12] [8].
FAQ 4: My study shows high variability in carbohydrate absorption results among children of the same age. What could be the cause? This is a common challenge rooted in both genetic and environmental factors. Genetically, there is natural variation in the persistence of lactase enzyme activity into childhood. Environmentally, the history of previous intestinal infections, the timing of introduction of solid foods, and the current composition of the gut microbiome can all influence the expression and activity of brush border disaccharidases. This normal biological variation must be accounted for in your experimental design by using a within-subjects design where possible, increasing sample size to capture the diversity, and carefully controlling for dietary intake and medical history in your participant selection and statistical analysis [8] [3].
Troubleshooting Guides
Problem: Inconsistent results in a pediatric breath test study.
- Potential Cause 1: Non-standardized test meals or fasting times.
- Solution: Ensure all participants receive an identical test meal with a standardized macronutrient composition. Adhere to age-appropriate fasting times; for children under two years, prolonged fasting is not recommended and requires protocol adaptation [12].
- Potential Cause 2: Uncontrolled physical activity.
- Solution: In children, uncontrolled or high levels of physical activity can lead to faster washout of the 13C isotope from the breath, altering results. Maintain a calm, controlled environment during the testing period and monitor activity levels [12].
- Potential Cause 3: Underlying subclinical enteropathy.
Problem: Failure to detect an expected growth response to a nutritional intervention.
- Potential Cause 1: The intervention did not account for age-specific nutrient requirements or absorptive capacity.
- Potential Cause 2: Systemic inflammation is diverting nutrients from growth.
- Solution: In populations with high infectious burdens or conditions like EED, systemic inflammation increases nutrient requirements and shifts nutrient utilization away from growth. Measure and control for inflammatory biomarkers (e.g., C-reactive protein) to clarify the relationship between nutrient absorption and functional outcomes like growth [12] [8].
Problem: High participant dropout rates in a longitudinal study on infant digestion.
- Potential Cause: Overly invasive or burdensome testing procedures for the age group.
Experimental Protocols & Data Presentation
Detailed Methodology: 13C-Sucrose Breath Test for Carbohydrate Absorption
Principle: A patient is administered a test meal containing 13C-labeled sucrose. If sucrose digestion (by the brush border enzyme sucrase-isomaltase) and absorption are normal, the 13C is absorbed, metabolized, and exhaled as 13CO2. Reduced exhalation of 13CO2 indicates maldigestion or malabsorption of the carbohydrate [12].
Protocol:
- Baseline Sample: After an age-appropriate fast, collect a baseline breath sample from the child in a sealed vacutainer.
- Test Meal Administration: Administer a standardized test meal containing a known quantity of 13C-sucrose (e.g., 5-10 mg/kg body weight). The meal should be consumed completely within 10 minutes.
- Post-Dose Sampling: Collect sequential breath samples at 30, 60, 90, 120, 150, and 180 minutes after ingestion.
- Sample Analysis: Analyze the breath samples using isotope ratio mass spectrometry (IRMS) to determine the 13CO2/12CO2 ratio.
- Data Calculation: Calculate the cumulative percentage of the administered 13C dose recovered in breath over time (cPDR). This value is compared to established normal ranges for the child's age group [12].
Normalization: For enhanced precision, the test can be performed on a separate day with 13C-glucose to establish an individual's Coefficient of Glucose Oxidation (CGO%), which accounts for variation in metabolic rate. The sucrose result is then normalized using this value [12].
Diagnostic Tests for Macronutrient Malabsorption
The table below summarizes key diagnostic tests, highlighting their applicability and limitations in pediatric research.
Table 1: Diagnostic Tests for Macronutrient Malabsorption in Pediatric Research
| Macronutrient | Test Name | Methodology | Key Pediatric Considerations | Primary Research Application |
|---|---|---|---|---|
| Fat | 13C-Mixed Triglyceride Breath Test [12] | Oral administration of a 13C-labeled fat; serial breath sampling to measure 13CO2. | Non-invasive and suitable for children. Normative cut-offs are lab-specific and age-dependent. | Detecting fat maldigestion (e.g., pancreatic insufficiency) and malabsorption. |
| Fat | Quantitative Fecal Fat Assessment [9] [3] | Stool collection over 72 hours with controlled fat intake; measurement of stool fat content. | Gold standard but burdensome. Accurate stool collection is difficult in infants and young children. | Validating less invasive methods; severe fat malabsorption studies. |
| Carbohydrate | 13C-Sucrose / 13C-Lactose Breath Test [12] [8] | Oral administration of 13C-labeled sugar; serial breath sampling to measure 13CO2. | Non-invasive. Can be adapted for children. Lacks standardized pediatric protocols. | Assessing specific disaccharidase deficiencies (e.g., sucrase-isomaltase, lactase). |
| Carbohydrate | Hydrogen Breath Test [9] [3] | Oral administration of a sugar; measurement of hydrogen in breath from bacterial fermentation of unabsorbed carbohydrate. | Non-invasive. A high baseline hydrogen can indicate SIBO, which is a common confounder. | Diagnosing lactose intolerance, fructose malabsorption, and SIBO. |
| Protein | Dipeptide Absorption Test (e.g., Benzoyl-L-tyrosyl-L-1-13C-alanine) [12] | Oral administration of a 13C-labeled dipeptide; serial breath sampling. | Non-invasive and a direct test of peptide transport function. Still considered a research tool. | Investigating protein malabsorption and brush border transporter function. |
Key Signaling Pathways and Workflows
The following diagram illustrates the multi-stage process of nutrient assimilation, highlighting key ontogenetic checkpoints where dysfunction can lead to malabsorption.
Figure 1: Ontogenetic Checkpoints in Nutrient Assimilation
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for Pediatric Malabsorption Research
| Item | Function / Application | Key Considerations |
|---|---|---|
| 13C-Labeled Substrates (Sucrose, Lactose, Mixed Triglycerides, Dipeptides) | Active ingredient for stable isotope breath tests to assess digestion and absorption of specific macronutrients [12]. | Purity is critical. Must be compounded into palatable, age-appropriate test meals to ensure complete consumption by children. |
| Stable Isotope Ratio Mass Spectrometer (IRMS) | Analytical instrument for highly precise measurement of the 13C/12C ratio in breath samples [12]. | Requires specialized operation and maintenance. The cornerstone technology for non-invasive, quantitative absorption studies. |
| Fecal Calprotectin ELISA Kits | To measure a biomarker of neutrophil activity in stool, used as a non-invasive proxy for intestinal inflammation [68]. | Essential for screening and controlling for confounders like Environmental Enteric Dysfunction (EED) or Inflammatory Bowel Disease (IBD). |
| Breath Sampling Kits (Vacutainers, Mouthpieces, Straws) | For the collection and storage of breath samples from participants in a hygienic and gas-tight manner. | Must be designed to be user-friendly for children of different ages to ensure sample integrity and participant compliance. |
| Standardized Formula & Test Meals | Provides a uniform nutritional base for metabolic tests, ensuring all subjects receive identical challenges. | Macronutrient composition must be precise. Palatability is a key factor in pediatric studies to avoid refusal and ensure valid results. |
Benchmarking and Validation: From Novel Biomarkers to Syndrome-Specific Profiles
Validating Non-Invasive Tests Against the Histological Gold Standard
In research on macronutrient malabsorption and metabolic liver diseases, histopathological assessment from tissue biopsies remains the scientific gold standard for diagnosis. However, the invasive nature of biopsies drives the development of non-invasive tests (NITs). Validating these NITs against histological reference standards is therefore a critical methodological step to ensure their accuracy and clinical relevance. This technical support guide provides researchers with a structured framework for this validation process, addressing common pitfalls and solutions.
Key Non-Invasive Tests and Their Histological Correlations
The table below summarizes the diagnostic performance of several well-established NITs when validated against histology in the context of Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) [69].
| Non-Invasive Test (NIT) | Components / Formula | Area Under Curve (AUC) | Optimal Cut-off | Validation Cohort |
|---|---|---|---|---|
| Framingham Steatosis Index (FSI) | Age, sex, BMI, triglycerides, hypertension, diabetes, ALT/AST ratio | 0.836 (0.826–0.847) | Determined by Youden Index [69] | NHANES (n=5,524) [69] |
| Fatty Liver Index (FLI) | BMI, waist circumference, triglycerides, GGT | 0.835 (0.825–0.845) | Determined by Youden Index [69] | NHANES (n=5,524) [69] |
| Zhejiang University Index (ZJU) | BMI, fasting plasma glucose, triglycerides, ALT/AST ratio | 0.815 (0.797–0.832) | Determined by Youden Index [69] | Health Management Center (n=2,187) [69] |
| Magnetic Resonance Elastography (MRE) | Liver Stiffness Measurement (LSM) | 0.781 – 0.977 (for fibrosis staging) | Varies by fibrosis stage [70] | Biopsy-proven MASLD (n=99) [70] |
Essential Research Reagent Solutions
The following table outlines key reagents and their critical functions for experiments involving chromogenic immunohistochemistry, a core technique for generating histological standard [71] [72].
| Reagent / Kit | Primary Function | Technical Notes & Pitfalls |
|---|---|---|
| Primary Antibodies | Specifically bind to target antigen (e.g., p53, Ki-67, cytokeratins). | Must be validated for FFPE sections. Avoid repeated freeze-thaw cycles by aliquoting with cryopreservative (e.g., 25-50% glycerol) [71]. |
| HRP-Labeled Polymer Reagents | Signal detection and amplification. | Superior sensitivity and specificity vs. older biotin-labeled techniques (e.g., ABC, LSAB), which are susceptible to endogenous biotin interference [71]. |
| Diaminobenzidine (DAB) | Chromogenic substrate producing a brown precipitate at antigen sites. | Handle in fume hood; monitor reaction time (3-20 min) under microscope to avoid over/under-staining [71] [72]. |
| Mayer's Hematoxylin | Nuclear counterstain (deep blue). | Brief incubation (e.g., 10 seconds) is typically sufficient to avoid obscuring specific staining [71]. |
| Antigen Retrieval Buffers | Unmask epitopes cross-linked by formalin fixation. | Heat-Induced Epitope Retrieval (HIER) is common. Optimization is required as it can be harsh on cryostat sections [72]. |
| Peroxidase & Avidin/Biotin Blocking Reagents | Reduce non-specific background staining. | Critical step to block endogenous enzyme activity and endogenous biotin, especially in tissues rich in these molecules [72]. |
Experimental Protocol: Chromogenic Immunostaining for Histological Standard
This protocol is optimized for formalin-fixed, paraffin-embedded (FFPE) sections, the common standard in diagnostic pathology [71] [72].
Step-by-Step Methodology:
- Deparaffinization and Rehydration: Pass FFPE sections through xylene and graded alcohols to water.
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) using an appropriate buffer (e.g., citrate, EDTA). The precise time, temperature, and pH must be optimized for each primary antibody [71].
- Quench Endogenous Peroxidase: Incubate sections with peroxidase blocking reagent (e.g., 3% H₂O₂) for 5-15 minutes [72].
- Block Non-Specific Binding: Apply a serum blocking reagent for 15 minutes to reduce background staining.
- Primary Antibody Incubation: Apply the optimized dilution of primary antibody in incubation buffer (e.g., PBS with 1% BSA). Incubate as required (often overnight at 4°C for maximum specificity) [72].
- Polymer Detection: Incubate with an HRP-labeled polymer secondary reagent for 30-60 minutes. Polymer-based systems are recommended for their high sensitivity and low background [71].
- Chromogenic Development: Apply DAB chromogen solution. Monitor the development of the brown precipitate under a microscope to ensure specific signal intensity without high background, typically for 3-20 minutes [71].
- Counterstaining and Mounting: Briefly counterstain with Mayer's hematoxylin, rinse, and mount with an aqueous mounting medium.
Workflow Diagram: Chromogenic IHC Staining
This diagram visualizes the core steps and key decision points in the chromogenic IHC protocol.
Troubleshooting Guides & FAQs
Q1: Our immunostaining shows high background staining. What are the primary causes and solutions?
- Cause: Inadequate blocking of non-specific interactions.
- Solution: Ensure complete blocking of endogenous peroxidase, biotin, and hydrophobic sites. Use the recommended serum blocking reagent and avidin/biotin blocking kits. Always include a negative control (no primary antibody) to identify the source of background [72].
- Cause: Over-fixation of tissue in formalin.
- Solution: Standardize fixation time (typically 4-8 hours for immersion fixation). If over-fixation is suspected, optimize the antigen retrieval step, though this can be challenging for cryostat sections [71] [72].
Q2: We are getting false-negative immunostaining results despite known antigen presence. How can we resolve this?
- Cause: Epitope masking due to formalin cross-linking.
- Solution: Systematically optimize the antigen retrieval protocol. Test different retrieval buffers (e.g., citrate vs. EDTA), pH values, and heating conditions (time and temperature) [71].
- Cause: Loss of antigenicity due to improper antibody handling.
- Solution: Avoid repeated freezing and thawing of primary antibodies. Prepare small, single-use aliquots diluted in a stabilizing buffer containing glycerol [71].
Q3: When validating a new NIT, what statistical measures are most important for comparing it to the histological gold standard?
- Primary Metrics: Calculate the Area Under the Receiver Operating Characteristic Curve (AUC) to assess overall diagnostic accuracy. Determine the optimal cut-off value by maximizing the Youden Index (Sensitivity + Specificity - 1) [69].
- Supplementary Analysis: Perform Decision Curve Analysis (DCA) and calculate Net Reclassification Index (NRI) and Integrated Discrimination Improvement (IDI) to evaluate the clinical utility and improvement in risk prediction over existing tests [69].
Q4: How can we address inter-observer variability in the histological gold standard itself?
- Solution: Implement digital pathology tools. Artificial intelligence (AI)-based systems can quantify histological features, providing a more objective and reproducible measurement. For example, AI-based systems like AIM-MASH have demonstrated superior repeatability and reproducibility compared to manual scoring for features like inflammation and ballooning in MASLD [73].
- Solution: Use consensus reads by multiple expert pathologists to establish a robust ground truth, especially in pivotal validation studies [73].
Workflow Diagram: NIT Validation Pathway
This diagram illustrates the logical flow and key steps for rigorously validating a Non-Invasive Test.
FAQ: Troubleshooting Experimental Challenges in Malabsorption Research
Q1: In a murine model, how can I definitively distinguish between the villous blunting caused by a gluten challenge (Celiac Disease) and that caused by environmental enteropathy?
A1: Distinguishing these etiologies requires a multi-parameter assessment beyond histology alone.
- Key Differentiating Factors:
- Trigger: Gluten challenge is specific to Celiac Disease (CeD) models, while Environmental Enteric Dysfunction (EED) is induced by constant exposure to fecal pathogens or a contaminated environment [74] [75].
- Inflammatory Context: EED is characterized by a chronic, low-grade inflammatory state driven by bacterial exposure, even in the absence of overt diarrhea [74] [76]. The mucosal inflammation in CeD is a specific autoimmune response to gluten [77] [78].
- Genetic Background: CeD models typically rely on mice with a specific genetic predisposition (e.g., expressing HLA-DQ2 or DQ8) [77] [78]. EED models do not have this requirement.
- Recommended Experimental Triangulation:
- Serology: Test for anti-tTG IgA antibodies, which are highly specific for the CeD immune response [77] [78].
- Immune Profiling: Analyze the lamina propria and intraepithelial lymphocytes. A pronounced increase in CD8+ intraepithelial lymphocytes is characteristic of CeD [77] [79]. EED also shows intraepithelial lymphocytosis and a proinflammatory cytokine profile (e.g., elevated TNF-α, IFN-γ) [76].
- Functional Tests: Perform a dual-sugar absorption test (e.g., lactulose:mannitol ratio) to quantify intestinal permeability, a hallmark of EED and active CeD [74] [76].
Q2: When establishing an in vitro model of nutrient transport using intestinal organoids, what are the critical culture conditions to simulate the barrier dysfunction seen in Crohn's Disease?
A2. To mimic Crohn's Disease (CD) barrier dysfunction, focus on recapitulating its inflammatory and architectural disruption.
- Critical Culture Modifications:
- Cytokine Cocktail: Supplement the culture medium with a combination of pro-inflammatory cytokines, notably TNF-α and IFN-γ, which are elevated in CD and directly disrupt tight junction integrity [80].
- Oxygen Tension: Consider culturing under slightly hypoxic conditions or introducing elements that simulate oxidative stress, reflecting the inflammatory microenvironment in CD.
- Microbiome Components: Challenge the organoids with bacterial products (e.g., LPS) or co-culture with adherent-invasive E. coli (AIEC) strains to model the dysbiosis and pathobiont response observed in CD.
- Validation Metrics for Your Model:
- Transepithelial Electrical Resistance (TEER): Monitor for a sustained decrease in TEER, indicating loss of barrier integrity.
- Immunofluorescence: Stain for key tight junction proteins (e.g., ZO-1, occludin) and look for discontinuous or aberrant localization at the cell membrane.
- Permeability Assays: Measure the flux of fluorescently-labeled dextrans or other tracer molecules across the organoid monolayer.
Q3: Our clinical trial on a nutritional intervention for malabsorption is seeing highly variable D-xylose test results. What are the primary confounding factors, and how can we control for them?
A3. The D-xylose test, which assesses carbohydrate absorption, is notoriously sensitive to several variables.
- Primary Confounding Factors:
- Gastric Emptying Rate: Delayed gastric emptying will alter the rate of D-xylose delivery to the absorption site.
- Renal Function: Impaired kidney function can reduce D-xylose excretion, leading to falsely low plasma or urine levels independent of intestinal absorption [76].
- Intestinal Motility: Rapid transit time, common in diarrheal states, reduces contact time with the absorptive surface.
- Small Intestinal Bacterial Overgrowth (SIBO): Bacteria in the small intestine can metabolize D-xylose before it is absorbed, invalidating the test [3].
- Hydration Status: Inadequate hydration can affect urine volume and concentration, skewing urine-based results.
- Troubleshooting Protocol:
- Standardize Procedures: Ensure patients fast, are well-hydrated, and receive a standardized D-xylose dose based on body weight.
- Pre-screen Subjects: Measure serum creatinine to exclude subjects with renal impairment.
- Consider Plasma vs. Urine: Using a plasma D-xylose test (measuring blood levels at a specific time point, e.g., 1 hour post-ingestion) can avoid confounders related to incomplete urine collection.
- Rule Out SIBO: Implement a hydrogen breath test to screen for and exclude subjects with SIBO from the D-xylose analysis [3].
Comparative Data Tables for Research Populations
Table 1: Key Pathophysiological and Histological Distinctions
| Feature | Celiac Disease (CeD) | Environmental Enteropathy (EED) | Crohn's Disease (CD) |
|---|---|---|---|
| Primary Etiology | Autoimmune response to dietary gluten [77] [79] | Chronic exposure to fecal-oral contaminants [74] [75] | Dysregulated immune response to intestinal microbiota; genetic susceptibility [80] |
| Key Histological Findings | Villous atrophy, crypt hyperplasia, intraepithelial lymphocytes (IELs) [77] [79] | Villous blunting, crypt hyperplasia, chronic inflammation [81] [74] | Transmural inflammation, crypt distortion, ulceration, non-caseating granulomas [80] |
| Primary Nutrient Malabsorption | Fat, fat-soluble vitamins, iron, carbohydrates [3] [77] | Global macronutrient and micronutrient malabsorption [74] [76] | Variable; fat, vitamin B12, bile acids (in terminal ileal disease) [3] [80] |
| Systemic Inflammation | Present during active disease | Chronic, low-grade systemic inflammation [74] [76] | Prominent, driven by pro-inflammatory cytokines (e.g., TNF-α) [80] |
Table 2: Standardized Diagnostic & Research Assays
| Assay / Marker | Celiac Disease (CeD) | Environmental Enteropathy (EED) | Crohn's Disease (CD) |
|---|---|---|---|
| Serologic Biomarkers | Anti-tTG IgA, Anti-EMA IgA [77] [78] | No established serologic test; research on fecal markers (e.g., Calprotectin) [74] [76] | Elevated CRP, ASCA antibodies [80] |
| Functional Gut Barrier Test | Often abnormal (e.g., Lactulose:Mannitol) | Lactulose:Mannitol ratio (gold standard for permeability) [74] [76] | Often abnormal; used in research contexts |
| Definitive Diagnosis | Small intestinal biopsy with characteristic histology [77] [79] | No single diagnostic; composite of clinical context, permeability tests, and biomarkers [81] [75] | Clinical, endoscopic, radiologic, and histologic findings [80] |
| Research-Grade Permeability Protocol | Administer lactulose (1g) and mannitol (0.5g) per 10kg body weight; collect 5-hour urine; measure by HPLC-MS/MS. A high L:M ratio indicates increased permeability. |
Essential Signaling Pathways in Malabsorption Syndromes
CeD Gluten-Induced Immunopathology
EED Pathogenesis Cycle
The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent / Material | Primary Function in Research | Application Across Syndromes |
|---|---|---|
| Lactulose & Mannitol | Dual-sugar test solution for quantifying intestinal permeability and absorptive surface area [74] [76]. | Core functional test for EED; also used in CeD and CD research. |
| Fecal Calprotectin | Protein marker released by neutrophils; non-invasive measure of intestinal inflammation [74]. | Used to monitor inflammation in CD and EED; typically normal or mildly elevated in isolated CeD. |
| Anti-tTG IgA ELISA Kit | Serological assay to detect autoantibodies against tissue transglutaminase [77] [78]. | Gold-standard blood test for diagnosing and monitoring CeD. |
| Cytokine Panels (TNF-α, IFN-γ, IL-12, IL-17) | Multiplex assays to profile the systemic and mucosal inflammatory milieu. | Critical for differentiating Th1/Th17 responses in CD, and the pro-inflammatory state in EED and active CeD. |
| Ussing Chamber System | Ex vivo apparatus to measure transepithelial electrical resistance (TEER) and macromolecular flux. | Used to directly evaluate gut barrier function in intestinal tissues from all disease models. |
| HLA-DQ2/DQ8 Genotyping Kits | Genetic test to determine susceptibility haplotypes. | Used to stratify research populations for CeD studies and exclude non-susceptible individuals. |
The Promise of Metabolomics for Objective Nutritional Phenotyping
Frequently Asked Questions (FAQs)
1. What is the core advantage of using metabolomics for nutritional studies? Metabolomics provides functional insights into an individual's metabolic responses to diet, reflecting real-time physiological changes. Unlike genomics, which shows genetic potential, metabolomics reveals the actual biochemical activity, making it ideal for understanding personalized nutrient processing and identifying objective nutritional phenotypes, such as macronutrient malabsorption [82].
2. How can we ensure our metabolomic data is reproducible across multiple batches? Batch-to-batch variation is a major challenge in large-scale studies. Key strategies include:
- Using Labeled Internal Standards (IS): Incorporate a mix of deuterated or 13C-labeled compounds (like LPCs, sphingolipids, fatty acids, and amino acids) that cover a wide range of retention times and physicochemical properties to monitor instrument performance [83].
- Robust Quality Control (QC): Inject QC samples—prepared from a pool of all study samples—throughout the sequence to condition the system and monitor stability. These QCs are later used for data normalization [83].
- Proper Normalization: Apply post-acquisition data correction methods (e.g., QC-SVRC normalization, total useful signal) to correct for both intra- and inter-batch instrumental drift [83].
3. Which chromatographic method should I use for polar metabolites? Reversed-phase LC is the gold standard but poorly retains highly polar molecules. For comprehensive coverage of the polar metabolome (including amino acids, sugars, and short-chain organic acids), Hydrophilic Interaction Chromatography (HILIC) is the preferred method. HILIC offers higher retention for polar metabolites, enhanced MS sensitivity due to better eluent desolvation, and orthogonal selectivity compared to reversed-phase methods [84] [85].
4. Our lab is new to HILIC; what are the critical steps for sample preparation? Sample preparation is more critical for HILIC than for reversed-phase LC. Best practices include:
- Protein Precipitation: Use cold organic solvents like methanol or acetonitrile. For HILIC, the sample diluent must be compatible with the organic-rich mobile phase [85].
- Optimal Sample Diluent: Re-dissolve the final extract in a solvent with a high organic content (e.g., pure acetonitrile or a mixture of acetonitrile and isopropanol) to avoid severe peak distortion [85].
- Minimal Injection Volume: Inject less than 1% of the total column volume to prevent volume overload, which causes peak tailing [85].
5. What are common metabolic signs of fat malabsorption in metabolomic data? Fat malabsorption, often linked to bile acid dysregulation, is associated with distinct metabolite patterns. Key findings from studies on conditions like liver cirrhosis and Inflammatory Bowel Disease (IBD) include:
- A dramatic decrease in fecal bile acids and bile pigments [86].
- Strong increases in fecal fatty acids and acylcarnitines, indicating disordered fatty acid metabolism [86].
- Elevated serum levels of the bile acid precursor 7α-hydroxy-4-cholesten-3-one (C4), a promising biomarker for bile acid malabsorption [87].
Troubleshooting Guides
Issue 1: Poor Retention and Peak Shape of Polar Metabolites
Problem: Early eluting, poorly resolved peaks for polar compounds when using reversed-phase LC, leading to co-elution with matrix interferences and inaccurate data.
Solutions:
- Switch to HILIC: Implement a HILIC method to properly retain and separate polar metabolites. Start with a bare silica or amide-based HILIC column [85].
- Optimize Sample Solvent: Ensure your injected sample is dissolved in a solvent that is no more than 10-20% water. A high organic solvent content (e.g., >80% acetonitrile) is crucial for maintaining sharp peaks in HILIC [85].
- Check Mobile Phase: Use a mobile phase with a high starting concentration of organic solvent (typically acetonitrile, 90-95%) with a volatile buffer like ammonium formate or acetate [85].
Issue 2: High Technical Variation and Batch Effects in Large Studies
Problem: Signal drift and systematic errors occur when analyzing hundreds of samples across multiple batches, making it impossible to compare data directly.
Solutions:
- Implement a Detailed Batch Design: Randomize all experimental samples across batches. Include system conditioning injections (e.g., 10 initial QC injections) and interleaved QC samples throughout the run [83].
- Use a Comprehensive Internal Standard Mix: Add a cocktail of isotopically labeled internal standards at the beginning of sample preparation. This helps monitor extraction efficiency, matrix effects, and instrument performance. An example mix could contain carnitine-D3, sphingosine-D7, stearic acid-D5, LPC18:1-D7, and isoleucine-13C,15N [83].
- Apply Systematic Normalization: Use the data from the repeatedly measured QC samples in a post-processing normalization algorithm (e.g., using the
qcsvrcpackage in R) to correct for systematic drift across the entire batch [83].
Issue 3: Difficulty in Metabolite Identification
Problem: Confidently identifying metabolites from LC-MS data is a major bottleneck, especially for distinguishing between structural isomers.
Solutions:
- Leverage Orthogonal Data: Use retention time (RT) as orthogonal information to mass spectrometry data. Compare your experimental RTs to those from authentic standards analyzed on the same chromatographic system [88].
- Report Complete Metadata: When publishing or storing data, provide full chromatographic metadata to enable data reuse and RT prediction. This includes column name and dimensions, flow rate, temperature, and detailed mobile phase composition and gradient [88].
- Utilize Tandem MS and Databases: Acquire high-resolution MS/MS spectra and search against public databases (e.g., MetLin, MassBank). For isomers, use in-silico fragmentation tools and consider using ion mobility spectrometry if available [89].
Table 1: Comparison of Primary Analytical Platforms in Metabolomics
| Technique | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|
| LC-MS (Reversed-Phase) | High sensitivity & separation efficiency; excellent for lipids & semi-polar metabolites [84] [85] | Poor retention of highly polar metabolites [85] | Biomarker discovery, lipidomics, high-throughput analysis [82] |
| LC-MS (HILIC) | High retention of polar metabolites; enhanced MS sensitivity; orthogonal selectivity [84] [85] | Longer equilibration times; less predictable retention; sensitive to sample solvent [85] | Coverage of polar metabolome (amino acids, sugars, organic acids) [85] |
| NMR Spectroscopy | Highly reproducible; non-destructive; minimal sample prep; absolute quantification [84] [82] | Moderate sensitivity (μM range) [84] | Structural characterization, clinical studies requiring high reproducibility [82] |
| GC-MS | High separation efficiency; robust & reproducible; extensive spectral libraries | Requires derivatization for many metabolites; limited to volatile compounds [84] | Volatile metabolites, metabolomics of primary metabolism [84] |
Table 2: Metabolomic Signatures in Macronutrient Malabsorption
| Malabsorption Type | Key Metabolite Changes in Biofluids/Feces | Associated Biological Interpretation |
|---|---|---|
| Fat / Bile Acid Malabsorption | ↓ Fecal bile acids (e.g., deoxycholic acid, lithocholic acid) [86] | Disrupted enterohepatic circulation; reduced microbial transformation of bile acids [87] |
| ↑ Serum 7α-hydroxy-4-cholesten-3-one (C4) [87] | Compensatory increase in hepatic bile acid synthesis [87] | |
| ↑ Fecal fatty acids & acylcarnitines [86] | Incomplete fatty acid oxidation and malabsorption of lipids [86] | |
| General Malabsorption (e.g., in Liver Cirrhosis) | ↑ Fecal lysophosphatidylcholines, aromatic amino acids [86] | Gut microbiota dysbiosis and impaired intestinal barrier function [86] |
Experimental Protocols
Protocol 1: A Multi-Batch LC-MS Metabolomics Workflow for Nutritional Phenotyping
This protocol is designed for large-scale studies, such as investigating macronutrient malabsorption in a research cohort, with emphasis on robustness and reproducibility [83].
Sample Preparation:
- Protein Precipitation: Add 300 μL of cold methanol to 100 μL of plasma/serum. Vortex and incubate at -20°C for 1 hour.
- Centrifugation: Centrifuge at 14,000 x g for 15 minutes at 4°C.
- Supernatant Collection: Transfer the supernatant to a new vial.
- Internal Standard Addition: Critical Step: Add a known amount of your labeled IS mix to every sample, blank, and QC pool at the very beginning of preparation to account for procedural losses and matrix effects [83].
Quality Control (QC) Pool Preparation:
- Create a pooled QC sample by combining equal volumes of extract from all study samples. This QC represents the "average" metabolic composition of the entire cohort [83].
Batch Design and LC-MS Analysis:
- Batch Setup: Split samples into multiple analysis batches. Randomize sample injection order across batches to avoid bias.
- Worklist Sequence:
- Start with 3 no-injection runs to condition the column.
- Inject several blanks (extraction solvent).
- Perform 10-15 initial injections of the QC pool to equilibrate the system.
- Run samples in a randomized order, injecting a QC after every 5-10 experimental samples.
- End with a final QC injection and blank runs [83].
- Chromatography: Use both reversed-phase (for lipids) and HILIC (for polar metabolites) methods for comprehensive coverage [84] [85].
Protocol 2: Detecting Bile Acid Malabsorption (BAM) Signatures
This protocol outlines a targeted approach to confirm BAM, a common cause of fat malabsorption, using serum and fecal samples [87].
Sample Collection: Collect serum and fecal samples from participants and matched healthy controls. Immediately freeze at -80°C.
Biomarker Analysis:
- Serum C4 Measurement: Use a targeted LC-MS/MS method to quantify levels of 7α-hydroxy-4-cholesten-3-one (C4) in serum. Elevated C4 is a key indicator of increased bile acid synthesis secondary to malabsorption [87].
- Fecal Bile Acid Profiling: Perform untargeted or targeted LC-MS on fecal water extracts. Look for a relative decrease in secondary bile acids (e.g., deoxycholic acid) and an altered primary-to-secondary bile acid ratio, indicating microbial dysbiosis and malabsorption [86] [87].
Data Integration: Correlate serum C4 levels with fecal bile acid profiles and clinical symptoms (e.g., diarrhea, abdominal pain) to identify patients with BAM [87].
Visual Workflows and Pathways
Metabolomics Workflow for Nutritional Phenotyping
Bile Acid Metabolism & Malabsorption Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Metabolomics Studies
| Item | Function & Importance | Example Application |
|---|---|---|
| Deuterated Internal Standard Mix | Monitors instrument performance, extraction efficiency, and matrix effects. Crucial for data quality control in untargeted studies [83]. | A mix containing LPC18:1-D7, carnitine-D3, sphingosine-D7, stearic acid-D5, and isoleucine-13C,15N to cover a broad RT/mz range [83]. |
| Quality Control (QC) Pool | Conditions the LC-MS system and is used for post-acquisition data normalization to correct for instrumental drift [83]. | A pooled sample made from a small aliquot of every sample in the study, injected repeatedly throughout the batch [83]. |
| HILIC Column | Separates polar metabolites that are poorly retained by standard reversed-phase columns, expanding metabolome coverage [85]. | Using a ZIC-pHILIC or Acquity UPLC BEH Amide column to analyze amino acids, sugars, and organic acids in stool or serum [85]. |
| Volatile Buffers | Provides pH control and ion-pairing for chromatography without fouling the MS ionization source. | Using ammonium formate or ammonium acetate in mobile phases for both HILIC and reversed-phase LC-MS [85]. |
| Stable Isotope Tracers (for Fluxomics) | Enables tracking of metabolic fluxes through pathways, providing dynamic information beyond steady-state levels. | Using 13C-labeled glucose to trace its utilization in glycolysis or pentose phosphate pathway in cell models of nutrient stress. |
Correlating Functional Test Results with Long-Term Functional Outcomes (Growth, Cognition)
Troubleshooting Guide: FAQs on Malabsorption Research
FAQ 1: What are the key functional tests for macronutrient malabsorption and what long-term outcomes should I correlate them with?
Issue: A researcher is unsure which functional tests for malabsorption are most predictive of long-term growth and cognitive outcomes in a study population.
Solution: The table below summarizes core malabsorption assessments and the long-term functional outcomes they are theorized to impact.
Table 1: Key Functional Tests and Correlated Long-Term Outcomes
| Functional Test Category | Specific Test / Method | Primary Nutrient/Function Assessed | Correlated Long-Term Functional Outcome | Supporting Evidence |
|---|---|---|---|---|
| Fat Absorption | 72-hour Fecal Fat Test [62] | Dietary fats, Fat-soluble vitamins (A, D, E, K) | Growth: Weight loss, muscle wasting [9] [5].Cognition: Potential impairment due to vitamin D/A/E deficiency. | |
| Carbohydrate Absorption | Hydrogen Breath Test (e.g., Lactose) [9] [62] | Specific carbohydrates (e.g., Lactose) | Growth: Abdominal bloating and gas can lead to reduced nutritional intake and growth delays in children [9]. | |
| Protein Absorption | Serum Albumin & Total Protein [90] | Protein status | Growth: Edema, muscle wasting, frequent infections [9].Cognition: Not a primary direct correlate. | |
| General Malabsorption & Deficiencies | Complete Blood Count (CBC), Iron, B12, Vitamin D [9] [62] | Micronutrients (Iron, B12, Vitamin D) | Cognition: Anemia (weakness, lightheadedness) [9]. Vitamin B12 deficiency is linked to cognitive decline [90]. | |
| Cognitive Function (as an outcome) | Cambridge Neuropsychological Test Automated Battery (CANTAB) [91] | Visual memory, Executive function | Functional Outcome: Poor social and occupational function in remitted Major Depressive Disorder, independent of symptoms [91]. | |
| Cognitive Training (as an intervention) | ACTIVE Study Cognitive Assessments [92] | Reasoning, Memory, Speed of processing | Functional Outcome: Reasoning training led to less functional decline in self-reported Instrumental Activities of Daily Living (IADL) after 5 years [92]. |
FAQ 2: My study shows clear macronutrient malabsorption, but no significant cognitive decline is detected. What could explain this discrepancy?
Issue: A scientist observes a disconnect between laboratory-confirmed malabsorption and expected cognitive results in their longitudinal study.
Solution: Consider the following potential confounding factors and troubleshooting steps:
- Incorrect Cognitive Assay Selection: The cognitive tests used may not be sensitive to the specific domains affected by the nutrient deficiencies. For example, a deficiency in a nutrient crucial for executive function might not be detected by a test focused solely on short-term memory.
- Insufficient Follow-Up Duration: Cognitive decline due to nutritional deficits can be slow and subtle. The study's follow-up period may be too short to capture a statistically significant change [92].
- Check for Compensatory Mechanisms: Study participants may have adapted their diet subconsciously to increase intake of the malabsorbed nutrient, mitigating the cognitive impact.
- Control for Covariates: Ensure the analysis controls for key confounding variables such as baseline cognitive status, educational level, socioeconomic status, and overall energy intake [91].
- Verify Biochemical Correlates: Confirm that the malabsorption is severe enough to cause a measurable biochemical deficiency (e.g., low serum levels of vitamins) that is known to impact brain function [90].
FAQ 3: How can I design a protocol to directly link nutrient malabsorption to a specific long-term cognitive deficit?
Issue: A drug development team needs a detailed experimental protocol to establish a causal link between a specific malabsorption issue and a downstream cognitive effect for a regulatory submission.
Solution: Implement a longitudinal cohort study with the following methodology.
Experimental Protocol: Linking Fat-Soluble Vitamin Malabsorption to Executive Function Decline
1. Hypothesis: Chronic malabsorption of fat-soluble vitamins (A, D, E, K) in a research population leads to a quantifiable decline in executive function over a 24-month period.
2. Population & Grouping: - Experimental Group: Research participants with confirmed fat malabsorption (e.g., fecal fat >6g/24h on a 100g fat diet [5]). - Control Group: Matched participants without malabsorption.
3. Baseline & Follow-up Assessments (Months 0, 12, 24): - A. Malabsorption & Nutritional Status: - Functional Test: 72-hour fecal fat collection [62] [5]. - Biochemical Tests: Serum levels of Vitamin A, D (25-OH), E, and INR (for Vitamin K status) [62]. - B. Cognitive Outcome (Primary Endpoint): - Tool: Intra-Extra Dimensional Set Shift (IED) test from the CANTAB battery. - Rationale: This test specifically targets executive function and cognitive flexibility, which has been shown to be a strong predictor of real-world functional outcomes [91]. - C. Functional Outcome (Secondary Endpoint): - Tool: Self-reported Instrumental Activities of Daily Living (IADL) scale. - Rationale: To assess translation to everyday life, as used in long-term cognitive training studies [92].
4. Data Analysis: - Use linear mixed-effects models to analyze the rate of change in IED scores over time between groups. - Perform mediation analysis to determine if the effect of malabsorption on IED scores is mediated by the decrease in serum vitamin levels.
Experimental Workflows & Pathways
Research Framework for Correlating Tests and Outcomes
This diagram outlines the logical workflow for designing a study that correlates functional malabsorption tests with long-term outcomes.
Malabsorption Impact Pathway on Cognition
This pathway visualizes the theorized mechanistic link between macronutrient malabsorption and its long-term cognitive effects.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 2: Essential Materials for Malabsorption and Functional Outcome Research
| Item / Reagent | Function in Research | Example Application |
|---|---|---|
| Cambridge Neuropsychological Test Automated Battery (CANTAB) | Computerized, non-linguistic assessment of multiple cognitive domains [91]. | Quantifying baseline and follow-up executive function (IED) and visual memory (PRM) in a study cohort [91]. |
| Hydrogen Breath Test Kit | Non-invasive diagnosis of carbohydrate malabsorption (e.g., lactose) [9] [62]. | Screening study participants for specific carbohydrate intolerances that may confound dietary intake and growth data. |
| Standardized Nutritional Formula | Provides a uniform nutrient load for challenge tests or nutritional support [93]. | Used in a controlled feeding study to standardize macronutrient intake before a 72-hour fecal fat collection. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Quantitative measurement of specific biomarkers in serum (e.g., Vitamin D, Albumin). | Objectively verifying micronutrient deficiency status correlated with malabsorption findings [90] [94]. |
| ACTIVE Study Training Materials | Standardized protocols for cognitive training interventions [92]. | Implementing a reasoning training intervention to test its effect on mitigating functional decline in a malnourished population [92]. |
Establishing Normative Cut-Offs and Defining Degrees of Malabsorption Severity
Diagnostic Criteria and Severity Classification
How are normative cut-offs established for fat malabsorption?
The quantitative measurement of fecal fat over a 72-hour stool collection while the patient consumes a standardized diet containing 100 grams of fat per day is considered the gold standard for establishing fat malabsorption [4]. Normative cut-offs are well-established in clinical practice:
Table 1: Established Normative Cut-Offs for Fat Malabsorption
| Parameter | Normal Range | Mild Malabsorption | Moderate Malabsorption | Severe Malabsorption | Measurement Method |
|---|---|---|---|---|---|
| Fecal Fat Excretion | ≤7 g/24 hours | 7-15 g/24 hours | 15-40 g/24 hours | ≥40 g/24 hours | 72-hour stool collection [4] |
| Fractional Fat Excretion | ≤7% | 7-15% | 15-40% | ≥40% | (Average g stool fat/day ÷ Average g fat consumed/day) × 100 [4] |
| Fecal Weight (ICU patients) | <350 g/day | - | - | ≥350 g/day | 24-hour collection correlating with energy malabsorption [95] |
Severe fat malabsorption (≥40 g/day) typically suggests pancreatic insufficiency or significant small-bowel mucosal disease, while milder elevations may occur in various conditions including bacterial overgrowth or bile acid deficiencies [3] [4].
What diagnostic thresholds are used for carbohydrate malabsorption?
Carbohydrate malabsorption is typically assessed through functional tests rather than quantitative excretion measurements:
Table 2: Diagnostic Thresholds for Carbohydrate Malabsorption
| Test Method | Normal Value | Malabsorption Indicator | Notes |
|---|---|---|---|
| Oral Lactose Tolerance Test | Blood glucose rise ≥20-30 mg/100mL | Rise <20 mg/100mL considered diagnostic [12] | High false positive rate due to metabolic variables [12] |
| Hydrogen Breath Test | Baseline hydrogen concentration | Rise >20 ppm above baseline | Indicates bacterial fermentation of unabsorbed carbohydrates [4] |
| 13C-Sucrose Breath Test | Varies by laboratory | Reduced cumulative 13CO2 recovery | Requires standardized protocols [8] |
How is malabsorption severity classified in research populations?
Malabsorption severity is classified through a combination of quantitative biochemical measures, functional tests, and clinical parameters:
Table 3: Comprehensive Severity Classification Framework
| Severity Level | Biochemical Markers | Functional Tests | Clinical Correlates |
|---|---|---|---|
| Mild | Fecal fat 7-15 g/day; Normal vitamins/minerals | Slightly abnormal breath tests; Normal D-xylose | Occasional diarrhea; Well-nourished |
| Moderate | Fecal fat 15-40 g/day; Mild micronutrient deficiencies | Definitely abnormal absorption tests; Reduced D-xylose | Chronic diarrhea; Weight loss <10%; Fatigue |
| Severe | Fecal fat ≥40 g/day; Multiple deficiencies | Markedly abnormal absorption tests; Low D-xylose | Steatorrhea; Weight loss >10%; Deficiency syndromes [4] |
Experimental Protocols and Methodologies
What is the standardized protocol for 72-hour fecal fat quantification?
The 72-hour fecal fat collection requires strict protocol adherence:
- Pre-test Diet: Patients consume 100+ grams of fat daily for 3 days before and throughout the collection period [4]
- Collection Period: 72-hour continuous stool collection in pre-weighed containers
- Laboratory Analysis: Homogenization of entire stool specimen followed by chemical quantification of fat content
- Calculation: Total fat excreted (g/24 hours) and fractional fat excretion (%) [4]
This method, while considered gold standard, has limitations including patient inconvenience, labor-intensive processing, and poor patient acceptance [4].
What non-invasive methods are available for macronutrient absorption studies?
Breath tests offer promising non-invasive alternatives for research populations:
13C-Mixed Triglyceride Breath Test for Fat Absorption
- Principle: Measures 13CO2 in breath after ingestion of 13C-labeled mixed triglyceride
- Protocol: Baseline fast, ingestion of labeled substrate, serial breath samples over 4-6 hours
- Advantages: Non-invasive, suitable for children and longitudinal studies [8] [12]
- Limitations: Requires mass spectrometry, lacks standardized pediatric reference values [12]
13C-Starch/Sucrose Breath Tests for Carbohydrate Absorption
- Principle: Tracks 13CO2 recovery from ingested 13C-labeled carbohydrates
- Protocol: Often combined with 13C-glucose breath test for normalization (Coefficient of Glucose Oxidation)
- Applications: Particularly relevant for environmental enteropathy research [8]
Benzoyl-L-tyrosyl-L-1-13C-alanine Dipeptide Absorption Test
- Principle: Assesses protein digestion and absorption via dipeptide absorption
- Measurement: 13CO2 recovery in breath indicates functional dipeptide transport [8]
Troubleshooting Common Experimental Challenges
How can researchers address the lack of standardized pediatric reference values?
The absence of age-specific normative data for many absorption tests presents significant research challenges. Recommended approaches include:
- Laboratory-Specific Controls: Establish internal reference ranges using healthy control populations matched for age, ethnicity, and diet [12]
- Parallel Validation: Where ethically feasible, compare non-invasive tests with gold standard measures in subset populations
- Cross-Center Collaboration: Pool data across research sites to develop larger reference databases [8]
- Age-Stratified Analysis: Report results stratified by age groups even without established norms
What factors account for inter-laboratory variability in breath test results?
Multiple technical factors contribute to variability in absorption breath testing:
- Test Meal Composition: Variable fat content significantly impacts lipid absorption tests
- Dosing Protocols: Differences in labeled substrate dosage and administration
- Sample Collection Timing: Inconsistent sampling intervals affect curve interpretation
- Analytical Variations: Differences in mass spectrometry calibration and 13CO2 measurement
- Ethnic and Dietary Factors: Population differences in gut microbiota and transit times [8]
Standardization protocols should address each of these variables to improve cross-study comparability.
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Reagents for Macronutrient Absorption Studies
| Reagent/Material | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| 13C-Labeled Substrates | Tracing nutrient absorption | 13C-mixed triglycerides (fat), 13C-starch (carbs), 13C-dipeptides (protein) | Chemical purity, metabolic equivalence to native compounds [8] |
| Breath Collection Systems | Capturing time-point samples for 13CO2 analysis | Glass tubes, foil bags, commercial collection systems | Air-tight integrity, appropriate storage conditions |
| Stool Collection Systems | Quantitative fecal analysis | Pre-weighed containers, homogenization equipment | Temperature control during collection period |
| Mass Spectrometry Standards | Instrument calibration for isotope ratio analysis | Certified 13CO2 reference gases | Regular calibration protocols |
| Enteral Nutrition Formulas | Standardized test meals | Defined macronutrient composition for challenge tests | Macronutrient stability, palatability |
Diagnostic Pathways and Research Algorithms
Breath Test Experimental Workflow
Evaluating the Efficacy of Nutritional and Pharmacologic Interventions (e.g., Teduglutide)
Troubleshooting Guides
Troubleshooting Guide: Measuring Macronutrient Malabsorption
Problem: High variability in malabsorption test results.
- Potential Cause 1: Lack of protocol standardization.
- Solution: Adhere strictly to published protocols for breath test administration, including pre-test fasting duration, test meal composition, and sampling frequency. When using tests like the 13C-starch breath test, ensure a reference test like the 13C-glucose breath test is conducted to normalize for individual differences in substrate oxidation [12].
- Potential Cause 2: Influence of gut transit time.
- Solution: Use a transit marker, such as ³H-polyethylene glycol (³H-PEG), concurrently with your malabsorption test. This allows you to correlate nutrient absorption with the speed of passage through the gastrointestinal tract [47].
- Potential Cause 3: Participant-related factors.
- Solution: For pediatric populations, control for factors that can dilute the body's 13C pool, such as the previous day's diet or breastmilk. Ensure participants avoid strenuous activity during testing, which can accelerate the washout of 13C in breath [12].
Problem: Difficulty interpreting the clinical significance of teduglutide-induced parenteral support (PS) reduction.
- Potential Cause 1: Focusing solely on a single outcome metric.
- Solution: Evaluate a composite of endpoints. A clinically significant response is typically defined as a ≥20% reduction in PS volume or calories. However, also monitor for the achievement of PS-free days and, ultimately, complete weaning from PS [96] [97]. Track nutritional status parameters (body weight, albumin, body composition) to ensure PS reduction does not compromise the patient's nutrition [97].
- Potential Cause 2: Unrealistic expectations for the timeline of effect.
- Solution: Understand that the response to teduglutide is variable and can take time. The onset of a significant PS reduction has been observed between 1 and 45 weeks in clinical practice. Manage expectations based on pooled efficacy data [97].
Troubleshooting Guide: Interpreting Outcomes in Short Bowel Syndrome (SBS) Trials
Problem: Heterogeneous treatment response in SBS patients.
- Potential Cause 1: Patient anatomy, specifically the presence or absence of colon in continuity.
- Solution: Stratify patients during randomization or adjust for this variable in your statistical analysis. Meta-analysis data shows the presence of colon in continuity is a significant predictor of both higher response rates and higher rates of complete weaning from PS [96].
- Potential Cause 2: Underlying SBS etiology.
- Solution: While not always a significant predictor, a non-significant trend suggests patients with Crohn's disease may have higher response and weaning rates. Ensure patient subgroups are sufficiently powered to detect potential differences based on etiology [96].
Frequently Asked Questions (FAQs)
FAQ 1: What are the key efficacy outcomes for teduglutide in adult SBS patients, and how do they change over time?
Pooled meta-analysis data provides the following estimates for teduglutide efficacy over time [96]:
Table: Teduglutide Efficacy Outcomes Over Time
| Time Point | Response Rate (≥20% PS Reduction) | Weaning Rate (PS Independence) |
|---|---|---|
| 6 Months | 64% | 11% |
| 1 Year | 77% | 17% |
| ≥2 Years | 82% | 21% |
FAQ 2: What non-invasive tests can measure macronutrient malabsorption in research populations?
Several breath tests are suitable, particularly for pediatric or sensitive populations [12] [8]:
- Carbohydrate Malabsorption: 13C-starch, 13C-sucrose, or 13C-lactose breath tests.
- Fat Malabsorption: 13C-mixed triglyceride breath test.
- Protein Malabsorption/Absorption: Benzoyl-L-tyrosyl-L-1-13C-alanine test for dipeptide absorption.
FAQ 3: What functional and structural biomarkers correlate with teduglutide efficacy?
Beyond PS reduction, successful teduglutide treatment is associated with:
- Functional Changes: Increased urine output (indicating improved fluid absorption) and improved stool frequency/consistency [97].
- Structural Changes: Significantly increased villus height and crypt depth on intestinal histology [97].
- Biomarker: A rise in plasma citrulline level, a marker of enterocyte mass [97].
Experimental Protocols & Data
Detailed Methodology: 13C Breath Test for Macronutrient Malabsorption
This protocol is adapted for assessing digestion and absorption in a research setting [12] [47].
1. Pre-Test Preparation:
- Participants: Fast for a specified period (e.g., 8-12 hours). Avoid high-fiber foods and alcohol for 24 hours prior to testing.
- Test Meal: Prepare a standardized meal containing the 13C-labeled substrate (e.g., 13C-starch, 13C-mixed triglyceride, or intrinsically labeled 13C-protein).
2. Test Administration:
- Baseline Sample: Collect a baseline breath sample in an Exetainer or similar container before meal ingestion [47].
- Meal Ingestion: The participant consumes the test meal within a fixed time frame.
- Sequential Sampling: Collect breath samples at regular intervals (e.g., every 15-30 minutes) for a period of 4-6 hours.
3. Sample Analysis:
- Analyze the isotopic abundance of 13CO2 in the breath samples using Isotope Ratio Mass Spectrometry (IRMS) [47].
- Calculate the cumulative percentage of the administered 13C dose recovered over time.
4. Data Interpretation:
- A lower cumulative 13C recovery indicates malabsorption of the tested macronutrient.
- Compare results against established normal values for the specific test and population [12].
Teduglutide Efficacy Data and Influencing Factors
Table: Predictors of Teduglutide Treatment Response in SBS [96]
| Predictor Variable | Impact on Response Rate (≥20% PS Reduction) | Impact on Weaning Rate (PS Independence) |
|---|---|---|
| Colon in Continuity | -17% (95% CI: -31%, -3%) | +16% (95% CI: +6%, +25%) |
| Etiology (Crohn's Disease) | +9% (95% CI: -8%, +27%) - Trend | +7% (95% CI: -14%, +28%) - Trend |
The Scientist's Toolkit: Key Research Reagents & Materials
Table: Essential Reagents for Macronutrient Malabsorption and Intervention Studies
| Research Reagent / Material | Function / Application |
|---|---|
| 13C-Labeled Substrates | Intrinsically or extrinsically labeled compounds used as tracers in breath tests to quantify carbohydrate, fat, and protein absorption [12] [47]. |
| Intrinsically Labeled Egg Protein | A precisely labeled protein source used to study protein digestion, malabsorption, and subsequent colonic fermentation in vivo [47]. |
| ³H-Polyethylene Glycol (³H-PEG) | A non-absorbable radioactive marker used to measure total gastrointestinal transit time during nutrient absorption studies [47]. |
| 14C-Glycocholic Acid | A radioactive bile acid used to assess bile acid malabsorption, which can be concurrent with fat malabsorption [47]. |
| Teduglutide | A glucagon-like peptide 2 (GLP-2) analog used as a pharmacologic intervention to enhance intestinal adaptation and absorption in Short Bowel Syndrome [96] [97]. |
| Plasma Citrulline | A biomarker measured via blood tests to assess functional enterocyte mass; levels increase with successful teduglutide treatment [97]. |
Conclusion
Advancing research on macronutrient malabsorption requires an integrated, multi-faceted approach. A deep understanding of pathophysiology must be paired with a critical and standardized application of functional tests, from classic invasive procedures to promising non-invasive breath analyses and metabolomic profiles. Future efforts must focus on validating these tools against robust clinical and histological endpoints across diverse populations, particularly in under-researched areas like environmental enteropathy. Furthermore, research must move beyond simple detection to elucidate the quantitative impact of malabsorption on functional outcomes like growth, muscle strength, and cognition. Success in this field will depend on collaborative, interdisciplinary research that bridges gastroenterology, nutrition, and immunology, ultimately leading to the development of precise diagnostic biomarkers and effective, mechanism-targeted interventions for these complex syndromes.
References
- 1. Malabsorption and Maldigestion | Concise Medical ... [https://www.lecturio.com/concepts/malabsorption-and-maldigestion/]
- 2. Malabsorption [https://en.wikipedia.org/wiki/Malabsorption]
- 3. Malabsorption Syndromes - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK553106/]
- 4. Overview of Malabsorption - Gastrointestinal Disorders [https://www.merckmanuals.com/professional/gastrointestinal-disorders/malabsorption-syndromes/overview-of-malabsorption]
- 5. Small and Large Intestine (I): Malabsorption of Nutrients [https://pmc.ncbi.nlm.nih.gov/articles/PMC8070135/]
- 6. The Malabsorption Syndrome and Its Causes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7149679/]
- 7. European Consensus on Malabsorption—UEG & SIGE, LGA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090837/]
- 8. Is there dietary macronutrient malabsorption in children ... [https://www.nature.com/articles/s41430-024-01510-z]
- 9. Malabsorption (Syndrome): Symptoms, Causes & Treatment [https://my.clevelandclinic.org/health/diseases/22722-malabsorption]
- 10. Small and Large Intestine (I): Malabsorption of Nutrients [https://www.mdpi.com/2072-6643/13/4/1254]
- 11. Etiologies of exocrine pancreatic insufficiency - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893156/]
- 12. Is there dietary macronutrient malabsorption in children ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11893463/]
- 13. Exocrine pancreatic insufficiency in long-term follow-up ... [https://www.sciencedirect.com/science/article/abs/pii/S1424390321001332]
- 14. Carbohydrate malabsorption in patients with non-specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4171253/]
- 15. Carbohydrate Intolerance - Gastrointestinal Disorders [https://www.merckmanuals.com/professional/gastrointestinal-disorders/malabsorption-syndromes/carbohydrate-intolerance]
- 16. Understanding Carbohydrate Malabsorption: Symptoms ... [https://juvia.me/blogs/journal/understanding-carbohydrate-malabsorption-symptoms-causes-and-the-role-of-juvia]
- 17. Malabsorption Workup: Approach Considerations, ... [https://emedicine.medscape.com/article/180785-workup]
- 18. Malabsorption: Background, Etiology, Pathophysiology [https://emedicine.medscape.com/article/180785-overview]
- 19. Amino Acid Transport Defects in Human Inherited Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6981491/]
- 20. Amino acid transporters in neurological disorders and ... [https://www.sciencedirect.com/science/article/pii/S0197018624000986]
- 21. SLC7 transporters at the crossroads of amino acid ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1467057/full]
- 22. Small Intestinal Bacterial Overgrowth - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK546634/]
- 23. Diagnosis and management of small intestinal bacterial ... [https://gastro.org/clinical-guidance/diagnosis-and-management-of-small-intestinal-bacterial-overgrowth-sibo/]
- 24. SIBO Test - All Your Questions Answered (2024) [https://healthpath.com/sibo/sibo-test-complete-guide/]
- 25. Small intestinal bacterial overgrowth (SIBO) - Symptoms & ... [https://www.mayoclinic.org/diseases-conditions/small-intestinal-bacterial-overgrowth/symptoms-causes/syc-20370168]
- 26. Small Intestinal Bacterial Overgrowth [https://pmc.ncbi.nlm.nih.gov/articles/PMC3099351/]
- 27. FAQ [https://sibocenter.com/faq/]
- 28. Small Intestinal Bacterial Overgrowth (SIBO) - Prevention ... [https://pubmed.ncbi.nlm.nih.gov/40296627/]
- 29. Association between small intestine bacterial overgrowth ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1438066/full]
- 30. 72 Hour Quantitative Fecal Fat [https://myadlm.org/advocacy-and-outreach/optimal-testing-guide-to-lab-test-utilization/a-f/72-hour-quantitative-fecal-fat]
- 31. Fecal Fat [https://www.testing.com/tests/fecal-fat/]
- 32. FATF - Overview: Fat, Feces [https://www.mayocliniclabs.com/test-catalog/overview/607701]
- 33. fecal fat - (f) [https://apps.sbgh.mb.ca/labmanual/test/view?seedId=99]
- 34. Fecal Fat Quantitative Test (72 Hour Collection) [https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/fecal-fat-quantitative-test-72-hour-collection]
- 35. Pancreatic Function Testing [https://stanfordhealthcare.org/medical-conditions/digestion-and-metabolic-health/chronic-pancreatitis/diagnosis/pancreatic-function-testing.html]
- 36. Exocrine Pancreatic Insufficiency (EPI) Diagnosis - EPI Tests [https://www.identifyepi.com/what-is-epi/exocrine-pancreatic-insufficiency-diagnosis]
- 37. Consensus for the management of pancreatic exocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212181/]
- 38. Testing for EPI [https://hcp.pancreaze.com/epi-and-gi-symptoms/testing-for-epi/]
- 39. Glucose Tolerance Test (GTT): What It Is, Preparation & ... [https://my.clevelandclinic.org/health/diagnostics/glucose-tolerance-test]
- 40. Glucose Tolerance Test - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK532915/]
- 41. The Oral Glucose Tolerance Test (OGTT): How to Prepare ... [https://www.chuwi.com/uploads/healthy/the-oral-glucose-tolerance-test-ogtt-how-to-prepare-and-what-to-expect-C2dqGG.html?srsltid=AfmBOooIGSZY7yHVv5IdutRqTixVUHmEQJv4Jx_3867ZfF6dma9E_-pg]
- 42. sciencedirect.com/topics/medicine-and-dentistry/ oral -glucose... [https://www.sciencedirect.com/topics/medicine-and-dentistry/oral-glucose-tolerance-test]
- 43. Quality of dietary macronutrients is associated with ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1158452/full]
- 44. Villous Atrophy: Flat Mucosa, Raised Questions [https://link.springer.com/article/10.1007/s10620-023-08218-3]
- 45. Clinical and Histologic Mimickers of Celiac Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5587842/]
- 46. Biopsies in Gastrointestinal Endoscopy: When and How [https://pmc.ncbi.nlm.nih.gov/articles/PMC5580003/]
- 47. The impact of bariatric surgery on macronutrient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9877414/]
- 48. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 49. Too few studies to steer test protocols for pediatrics [https://www.captodayonline.com/too-few-studies-to-steer-test-protocols-for-pediatrics/]
- 50. Reporting standards for child health research were few and ... [https://www.sciencedirect.com/science/article/abs/pii/S0895435623000689]
- 51. Evidence-based guidelines for pediatric clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC3566240/]
- 52. Assessment of nutritional status and clinical outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10627690/]
- 53. Nutritional status, nutritional risk, nutrition impact symptoms ... [https://www.sciencedirect.com/science/article/pii/S2667268524000615]
- 54. Pancreatic Enzyme Replacement Therapy After Pancreatoduodenectomy: Are Patients Treated Adequately? A Systematic Review Correlated with a Prospective Cohort | Medical Research Archives [https://esmed.org/MRA/mra/article/view/4017]
- 55. About Pancreatic Enzyme Replacement Therapy (PERT) [https://www.mskcc.org/cancer-care/patient-education/about-pancreatic-enzyme-replacement-therapy-pert]
- 56. Pancreatic Enzyme Replacement Therapy (PERT) [https://pancreaticcanceraction.org/get-help/ive-been-diagnosed/diet-and-nutrition-for-pancreatic-cancer/pert/]
- 57. Pancreatic enzyme replacement therapy in advanced adenocarcinoma of the pancreas improved overall survival: a retrospective, single institution study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11997656/]
- 58. All About EPI and PERT [https://www.ironwoodcrc.com/all-about-epi-and-pert/]
- 59. Sensory sensitivity and food disgust in avoidant/restrictive ... [https://www.sciencedirect.com/science/article/abs/pii/S0195666325004829]
- 60. New Study Sheds Light on Hidden Fears of Children with ... [https://psychiatry.duke.edu/news/new-study-sheds-light-hidden-fears-children-avoidant-restrictive-food-intake-disorder]
- 61. Recent insights into the epidemiology of avoidant ... [https://pubmed.ncbi.nlm.nih.gov/40956322/]
- 62. Malabsorption [https://iffgd.org/gi-disorders/malabsorption/]
- 63. Barriers to Healthy Eating and Influences on the Dietary ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198483/]
- 64. Nutrition: Macronutrient Intake, Imbalances, and Interventions [https://www.ncbi.nlm.nih.gov/books/NBK594226/]
- 65. Maldigestion and Malabsorption [https://abdominalkey.com/maldigestion-and-malabsorption/]
- 66. Malabsorption Tests [https://muschealth.org/medical-services/ddc/patients/medical-tests/function-studies/malabsorption-tests]
- 67. The impact of bariatric surgery on macronutrient ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.1028881/full]
- 68. A comprehensive review on malabsorption in pediatrics for ... [https://www.sciencedirect.com/science/article/pii/S0899900725002138]
- 69. Assessment of the diagnostic efficacy of five non-invasive ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1571487/full]
- 70. The Relationship Between Non-Invasive Tests and Digital ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524164/]
- 71. Pitfalls and Caveats in Applying Chromogenic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232789/]
- 72. Protocol for the Preparation and Chromogenic IHC ... [https://www.rndsystems.com/resources/protocols/protocol-preparation-and-chromogenic-ihc-staining-frozen-tissue-sections]
- 73. Clinical validation of an AI-based pathology tool for scoring ... [https://www.nature.com/articles/s41591-024-03301-2]
- 74. Environmental Enteropathy: Critical implications of a poorly ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3372657/]
- 75. Review Environmental Enteropathy: Elusive but Significant ... [https://www.sciencedirect.com/science/article/pii/S2352396416303395]
- 76. Environmental Enteric Dysfunction: Pathogenesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4481570/]
- 77. Celiac Disease - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK441900/]
- 78. Celiac Disease (Sprue): Background, Pathophysiology ... [https://emedicine.medscape.com/article/171805-overview]
- 79. Coeliac disease [https://en.wikipedia.org/wiki/Coeliac_disease]
- 80. Nutritional Rehabilitation in Patients with Malnutrition Due to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6950059/]
- 81. 用于评估环境性肠病和环境性肠功能障碍的肠活检 [https://www.x-mol.com/paper/1417204588910497792/t]
- 82. Metabolomics Service FAQs [https://www.arome-science.com/metabolomics-service-faqs/]
- 83. Troubleshooting in Large-Scale LC-ToF-MS Metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6918290/]
- 84. Applications of Chromatographic Methods in Metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11618781/]
- 85. The Rise of Hydrophilic Interaction Chromatography in Untargeted... [https://www.chromatographyonline.com/view/rise-hydrophilic-interaction-chromatography-untargeted-clinical-metabolomics]
- 86. Metabolomic Analyses of Faeces Reveals Malabsorption in ... [https://pubmed.ncbi.nlm.nih.gov/23384618/]
- 87. Fecal microbiota transplantation improves bile acid ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04353-y]
- 88. Critical assessment of chromatographic metadata in publicly available... [https://link.springer.com/article/10.1007/s11306-022-01956-x]
- 89. Common errors in mass spectrometry-based analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5548100/]
- 90. Malnutrition in Substance Use Disorders: A Critical Issue in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027436/]
- 91. Relationship between cognitive function and ... - BMC Psychiatry [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-024-05675-6]
- 92. Long-term Effects of Cognitive Training on Everyday ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2910591/]
- 93. A Descriptive Analysis of Macronutrient, Fatty Acid Profile ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2022.877875/full]
- 94. Nutritional deficiencies and muscle loss in adults with type ... [https://www.sciencedirect.com/science/article/pii/S2667368125000300]
- 95. Malabsorption and nutritional balance in the ICU: fecal weight ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3388706/]
- 96. Efficacy of Teduglutide for Parenteral Support Reduction in ... [https://pubmed.ncbi.nlm.nih.gov/35215445/]
- 97. Experience with teduglutide treatment for short bowel ... [https://www.sciencedirect.com/science/article/abs/pii/S0261561418312433]