ICH Q2(R1) Analytical Method Validation: The Definitive Guide for Pharmaceutical Professionals
This guide provides a comprehensive overview of ICH Q2(R1) analytical method validation, a critical process for ensuring the quality, safety, and efficacy of pharmaceuticals.
ICH Q2(R1) Analytical Method Validation: The Definitive Guide for Pharmaceutical Professionals
Abstract
This guide provides a comprehensive overview of ICH Q2(R1) analytical method validation, a critical process for ensuring the quality, safety, and efficacy of pharmaceuticals. Tailored for researchers, scientists, and drug development professionals, it covers the foundational principles, methodological application of key validation parameters, and practical troubleshooting strategies. The content also addresses the evolving regulatory landscape, comparing ICH Q2(R1) with the modernized Q2(R2) and Q14 guidelines to offer a complete perspective on analytical procedure lifecycle management for both chemical and biological drugs.
Understanding ICH Q2(R1): The Foundation of Analytical Method Validation
Historical Development of ICH Q2(R1)
The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," represents a cornerstone of global pharmaceutical regulation. Its development began in the 1990s to address conflicting technical requirements for pharmaceutical registration across major regions [1]. The guideline originated as two separate documents: ICH Q2A ("Text on Validation of Analytical Procedures"), finalized in October 1994, and ICH Q2B ("Validation of Analytical Procedures: Methodology"), finalized in 1996 [1] [2].
In November 2005, these two documents were unified into a single, comprehensive guideline renamed ICH Q2(R1) without changes to their original technical content [3] [2]. This harmonized document was subsequently adopted by regulatory authorities worldwide, including the U.S. Food and Drug Administration (FDA), the European Commission (EC), and Japan's Ministry of Health, Labour and Welfare (MHLW/PMDA) [4]. In September 2021, the FDA reissued the combined Q2(R1) guidance, confirming its ongoing regulatory status while the scientific community anticipates the finalization of its successor, ICH Q2(R2) [5].
Harmonization Objectives and Regulatory Impact
The primary harmonization goal of ICH Q2(R1) was to establish a uniform framework for validating analytical procedures used in pharmaceutical development and quality control [4]. Before its implementation, pharmaceutical companies faced significant challenges in meeting divergent regulatory expectations from different regions, leading to redundant testing, increased costs, and delays in product approvals [1].
ICH Q2(R1) successfully created a common language and standardized set of requirements for analytical procedure validation that regulatory authorities in the United States, European Union, Japan, and other adopting regions (such as Canada) would accept [4] [1]. This harmonization eliminated the need for companies to conduct multiple validations for the same product in different jurisdictions, streamlining the drug registration process and facilitating global market access [6].
The guideline achieved this by providing clear recommendations on the validation characteristics that must be evaluated for different types of analytical procedures, along with the specific data that should be presented in registration applications [4]. This ensured that analytical methods used to assess drug substances and products would generate reliable, reproducible results that accurately reflected product quality, safety, and efficacy, regardless of where the testing was performed [7].
Core Principles and Validation Parameters
Scope and Application
ICH Q2(R1) applies to the four most common types of analytical procedures used in pharmaceutical analysis [2]:
- Identification Tests: Methods intended to ensure the identity of an analyte in a sample, typically through comparison to a reference standard [2].
- Quantitative Tests for Impurities' Content: Procedures to measure the amount of impurities present in a sample [2].
- Limit Tests for the Control of Impurities: Methods to determine whether impurities exceed a specified limit [2].
- Quantitative Tests of the Active Moisty: Assays to measure the active component in drug substance or drug product samples [2].
Key Validation Characteristics
The guideline defines specific validation characteristics that must be demonstrated based on the type of analytical procedure. The table below summarizes these requirements:
Table 1: Validation Characteristics for Different Analytical Procedures per ICH Q2(R1)
| Validation Characteristic | Identification | Testing for Impurities | Assay | |
|---|---|---|---|---|
| Quantitative | Limit | |||
| Accuracy | - | Yes | - | Yes |
| Precision | - | Yes | - | Yes |
| Specificity | Yes | Yes | Yes | Yes |
| Detection Limit | - | - | Yes | - |
| Quantitation Limit | - | Yes | - | - |
| Linearity | - | Yes | - | Yes |
| Range | - | Yes | - | Yes |
| Robustness | Yes | Yes | Yes | Yes |
Source: Adapted from ICH Q2(R1) guidance [2]
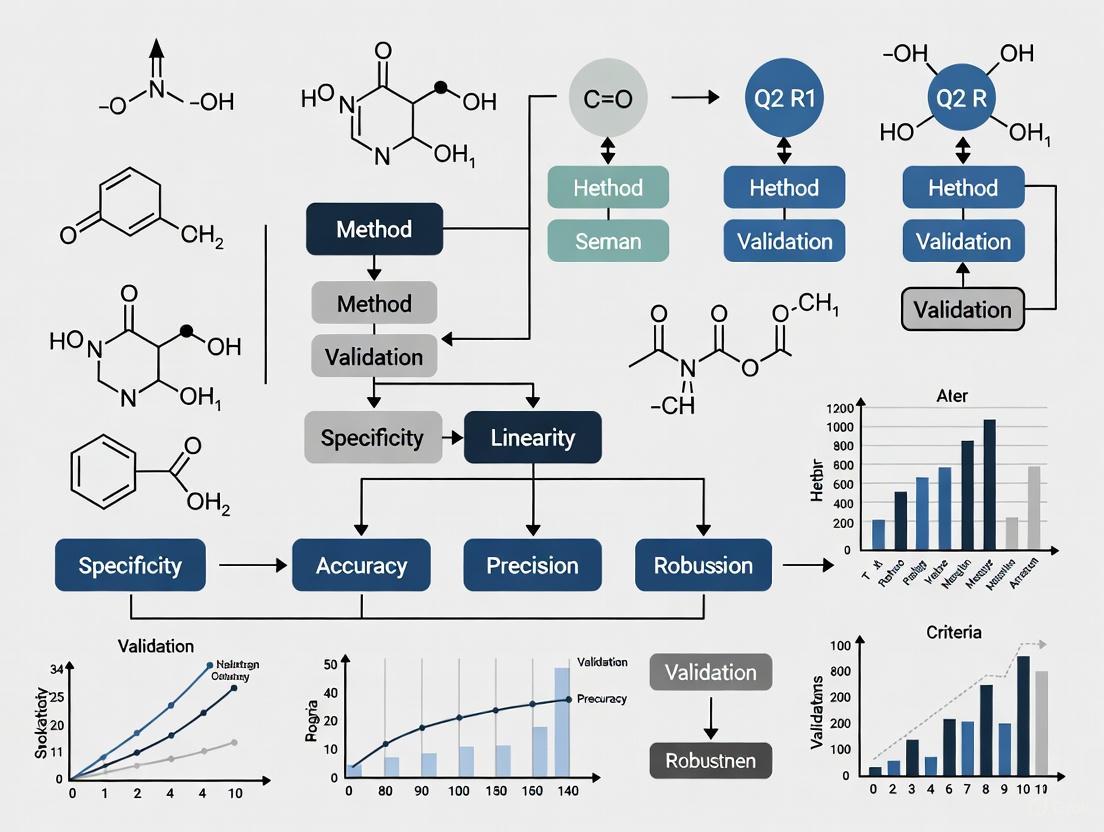
The following diagram illustrates the logical relationship between the analytical procedure lifecycle and its core validation components as conceptualized under ICH Q2(R1):
Detailed Methodologies for Core Validation Parameters
Accuracy
Accuracy demonstrates the closeness of agreement between the measured value and a reference value [2]. Recommended methodologies include:
- Spiked Recovery Studies: For drug substance analysis, compare measured values against known amounts of reference standards. For drug products, use the placebo formulation spiked with known quantities of the analyte [2].
- Comparison to Reference Method: Evaluate results against those obtained from a well-characterized independent procedure [2].
- Acceptance Criteria: Typically requires minimum of 9 determinations across a minimum of 3 concentration levels covering the specified range [2].
Precision
Precision expresses the closeness of agreement between a series of measurements from multiple sampling under prescribed conditions [2]. It should be investigated at three levels:
- Repeatability (Intra-assay Precision): Assess precision under the same operating conditions over a short time interval using at least 9 determinations covering the specified range or 6 determinations at 100% of the test concentration [2].
- Intermediate Precision: Evaluate within-laboratory variations due to different days, different analysts, different equipment, etc. [2].
- Reproducibility: Assess precision between laboratories, typically applied during technology transfer or standardization of methodology [2].
Specificity
Specificity is the ability to assess unequivocally the analyte in the presence of components that may be expected to be present [2]. Methodology includes:
- For Identification: Ensure identity of an analyte through comparison with reference standard using techniques like spectroscopy or chromatographic behavior [2].
- For Assay and Impurity Tests: Demonstrate complete separation of analyte from impurities, degradation products, or matrix components using chromatographic peak purity tests or orthogonal methods [2].
Detection Limit (DL) and Quantitation Limit (QL)
Detection Limit Methodologies:
- Visual Evaluation: Determine lowest concentration detectable by instrumental or visual examination [2].
- Signal-to-Noise Approach: Apply signal-to-noise ratio between 3:1 or 2:1 [2].
- Standard Deviation Method: Calculate based on standard deviation of response and slope of calibration curve: DL = 3.3σ/S [2].
Quantitation Limit Methodologies:
Linearity and Range
- Linearity: Demonstrate ability to obtain test results directly proportional to analyte concentration within a given range. Typically requires minimum of 5 concentrations with correlation coefficients, y-intercept, and slope of regression line reported [2].
- Range: Establish interval between upper and lower concentrations demonstrating suitable level of accuracy, precision, and linearity. Specific ranges depend on application (e.g., for assay of drug substance/drug product: 80-120% of test concentration) [2].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents and Materials for ICH Q2(R1) Validation
| Item | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Reference Standards | Serves as primary benchmark for identity, purity, and potency assessments [2]. | Well-characterized identity, certified purity, documented stability, traceable source [2]. |
| High-Purity Reagents | Used in mobile phases, sample preparation, and system suitability testing [2]. | Appropriate grade (HPLC, ACS), low impurity levels, minimal interference background [2]. |
| Placebo Formulation | Evaluates specificity by confirming absence of interference with analyte detection [2]. | Representative of final product composition without active ingredient, consistent with manufacturing process [2]. |
| System Suitability Solutions | Verifies chromatographic system resolution, efficiency, and reproducibility before validation runs [2]. | Stable composition, produces characteristic retention times and peak shapes, sensitive to system variations [2]. |
Evolution Beyond ICH Q2(R1) and Current Status
While ICH Q2(R1) remains the current implemented standard, the ICH has recognized limitations in addressing modern analytical techniques such as Near-IR, Raman spectroscopy, and multivariate models [1] [8]. This has led to the development of revised guidelines:
- ICH Q2(R2): Expands validation guidance to include modern analytical procedures and provides more detailed methodology with specific annexes for techniques like quantitative LC/MS and binding assays [6] [8].
- ICH Q14: Introduces a systematic approach to analytical procedure development, incorporating Quality by Design (QbD) principles and the Analytical Procedure Lifecycle concept [6].
These new guidelines promote a more holistic approach where validation begins with clear definition of the Analytical Target Profile (ATP) and continues through ongoing performance verification, representing a significant evolution beyond the foundation established by ICH Q2(R1) [6].
Defining Analytical Procedure Validation and Its Critical Importance
In the pharmaceutical industry, analytical procedure validation is the formal, documented process of demonstrating that an analytical method is suitable for its intended purpose, providing a high degree of assurance that it will consistently yield reliable and accurate results [7]. This process establishes, through laboratory studies, that the method's performance characteristics meet the requirements for its specific analytical application, ensuring reliability during normal use [9]. Validation serves as definitive evidence that the analytical procedure attains the necessary levels of precision, accuracy, and reliability required for assessing the identity, strength, quality, purity, and potency of drug substances and products [10].
The International Council for Harmonisation (ICH) guideline Q2(R1), titled "Validation of Analytical Procedures: Text and Methodology," serves as the primary global standard for this activity [5] [3]. First finalized and later harmonized in 2005, ICH Q2(R1) combines the principles of two earlier documents (Q2A and Q2B) to provide a comprehensive framework for the validation of analytical methods used in regulatory submissions [5] [2]. For pharmaceutical manufacturers, validation is not merely a regulatory formality but a fundamental requirement for compliance with Good Laboratory Practices (GLP) and Current Good Manufacturing Practices (cGMP) [7]. It is a critical component of the overall validation process that ensures the safety and efficacy of pharmaceutical products reaching patients [10].
The Regulatory Framework: ICH Q2(R1)
Scope and Objective
The ICH Q2(R1) guideline provides a harmonized framework for validating analytical procedures, with its core objective being to demonstrate that a procedure is suitable for its intended purpose [2]. This guideline primarily addresses the validation of the four most common types of analytical procedures encountered in pharmaceutical analysis:
- Identification Tests: Methods intended to ensure the identity of an analyte in a sample, typically achieved by comparing a property of the sample (such as spectrum, chromatographic behavior, or chemical reactivity) to that of a reference standard [2].
- Quantitative Tests for Impurities: Procedures designed to accurately measure the content of impurities in a sample, reflecting the purity characteristics of the material [2].
- Limit Tests for Impurities: Methods that determine whether an impurity is above or below a specified limit, without necessarily providing an exact quantitative value [2].
- Assay Procedures: Quantitative measurements of the major component(s) in a drug substance or drug product, which also apply to assays for the active moiety or other selected components in the final product [2].
The guidance outlines the fundamental validation parameters that must be evaluated for each type of procedure, recognizing that different parameters may be applicable depending on the method's intended use [2].
The Validation Lifecycle and Recent Evolution
While ICH Q2(R1) has served as the cornerstone for analytical method validation for nearly two decades, the regulatory landscape is evolving. Recent updates have introduced a more comprehensive lifecycle approach to analytical procedures [6]. The simultaneous introduction of ICH Q2(R2) and the new ICH Q14 guideline represents a significant modernization, shifting from a prescriptive, "check-the-box" approach to a more scientific, risk-based model [6] [11].
This evolution addresses the increasing complexity of biopharmaceutical products and the need for more flexible, science-based approaches to method validation [6]. The new guidelines emphasize that analytical procedure validation is not a one-time event but a continuous process that begins with method development and continues throughout the method's entire operational life [6] [11]. This shift requires organizations to implement systems for ongoing method evaluation and improvement, integrating quality control and method optimization as continuous activities [6].
Core Validation Parameters and Methodologies
The validation process involves the systematic evaluation of specific performance characteristics as defined in ICH Q2(R1). The following parameters are considered fundamental to demonstrating a method's suitability.
Specificity
Specificity is the ability of a method to assess the analyte unequivocally in the presence of other components that may be expected to be present, such as impurities, degradation products, or matrix components [7] [2]. This parameter ensures that the analytical procedure can accurately measure the analyte without interference from other substances.
- Methodology for Identification: Specificity is demonstrated by the ability to discriminate between compounds in the sample or by comparison to known reference materials [9].
- Methodology for Assay and Impurity Tests: Specificity can be shown by resolving the two most closely eluted compounds, typically the major component and a closely eluted impurity [9]. For chromatographic methods, peak purity assessment using photodiode-array (PDA) detection or mass spectrometry (MS) is recommended to demonstrate that a peak's response is due to a single component with no co-elutions [9].
Accuracy
Accuracy expresses the closeness of agreement between the value accepted as a conventional true value or an accepted reference value and the value found [2]. It is sometimes termed "trueness" and measures the exactness of the analytical method.
- Methodology for Drug Substance: Accuracy is typically assessed by comparison with a standard reference material or by comparison to a second, well-characterized method [9].
- Methodology for Drug Product: Accuracy is evaluated by analyzing synthetic mixtures spiked with known quantities of components [9]. For impurity quantification, accuracy is determined by analyzing samples spiked with known amounts of impurities [9].
- Recommended Data: The guidelines recommend collecting data from a minimum of nine determinations over at least three concentration levels covering the specified range (e.g., three concentrations, three replicates each) [9]. Results should be reported as the percentage recovery of the known, added amount, or as the difference between the mean and true value with confidence intervals [9].
Precision
Precision expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [2]. Precision should be considered at three levels, as outlined in the table below.
Table 1: Levels of Precision Evaluation in Analytical Method Validation
| Precision Level | Description | Experimental Approach | Data Reporting |
|---|---|---|---|
| Repeatability | Precision under the same operating conditions over a short time interval (intra-assay precision) [2]. | A minimum of nine determinations covering the specified range (three concentrations, three repetitions) or at least six determinations at 100% of test concentration [9]. | Typically reported as % RSD (Relative Standard Deviation) [9]. |
| Intermediate Precision | Within-laboratory variations: different days, analysts, equipment, etc. [2]. | Experimental design where effects of individual variables (e.g., different analysts, instruments, days) are monitored [9]. | % RSD and statistical comparison (e.g., Student's t-test) of results under varied conditions [9]. |
| Reproducibility | Precision between laboratories (collaborative studies) [2]. | Analysis of the same samples by multiple laboratories, often for technology transfer or compendial method standardization [9]. | Standard deviation, % RSD, and confidence intervals between laboratories [9]. |
Detection Limit (LOD) and Quantitation Limit (LOQ)
- Detection Limit (LOD): The lowest amount of analyte in a sample that can be detected but not necessarily quantitated as an exact value [2].
- Quantitation Limit (LOQ): The lowest amount of analyte in a sample that can be quantitatively determined with suitable precision and accuracy [2]. This parameter is particularly critical for determining impurities and degradation products.
Methodologies for Determination:
- Visual Evaluation: Can be used for non-instrumental and instrumental methods [2].
- Signal-to-Noise Ratio: Typically 3:1 for LOD and 10:1 for LOQ in chromatographic methods [9].
- Standard Deviation of Response and Slope: Based on the formula: LOD = 3.3(SD/S) and LOQ = 10(SD/S), where SD is the standard deviation of response and S is the slope of the calibration curve [9].
Linearity and Range
- Linearity: The ability of the method to obtain test results that are directly proportional to the concentration (amount) of analyte in the sample within a given range [2].
- Range: The interval between the upper and lower concentrations of analyte (inclusive) that have been demonstrated to be determined with acceptable precision, accuracy, and linearity using the method as written [9].
Methodology: Linearity is typically demonstrated using a minimum of five concentration levels across the specified range [9]. Data should be reported with the equation for the calibration curve line, the coefficient of determination (r²), residuals, and the calibration curve itself [9].
Robustness
Robustness measures the capacity of a method to remain unaffected by small, deliberate variations in method parameters (e.g., pH, mobile phase composition, temperature, flow rate) and provides an indication of its reliability during normal usage [9] [11].
Methodology: Robustness is evaluated by deliberately introducing small changes to method parameters and monitoring the resulting effect on the method's performance [9]. The experimental design should identify critical parameters that may require tight control in the method instructions to ensure reproducibility [9].
The following workflow diagram illustrates the strategic process and key decision points in analytical method validation according to regulatory standards:
Experimental Protocols for Key Validation Parameters
Protocol for Accuracy Assessment
Objective: To demonstrate that the analytical method provides results that are close to the true value.
Materials and Reagents:
- Reference standard of known purity
- Placebo formulation (excluding active ingredient)
- Appropriate solvents and reagents as per method
Procedure:
- Prepare a minimum of nine samples over three concentration levels (e.g., 80%, 100%, 120% of target concentration) with three replicates at each level.
- For drug substance, compare results against a certified reference standard.
- For drug product, prepare samples by spiking placebo with known quantities of the active ingredient.
- Analyze all samples using the analytical method under validation.
- Calculate the percentage recovery for each sample using the formula: Recovery (%) = (Measured Concentration / Theoretical Concentration) × 100.
Acceptance Criteria: The mean recovery should be within specified limits (e.g., 98-102% for drug substance, 97-103% for drug product) with appropriate precision (%RSD) [9].
Protocol for Precision Evaluation
Objective: To demonstrate the degree of scatter in results under prescribed conditions.
Materials and Reagents:
- Homogeneous sample of drug substance or product
- Reference standard
- Appropriate solvents and reagents
Procedure for Repeatability:
- Prepare six independent sample preparations at 100% of test concentration.
- Analyze all six preparations under the same operating conditions.
- Calculate the mean, standard deviation, and %RSD of the results.
Procedure for Intermediate Precision:
- Perform the analysis on different days, with different analysts, or using different instruments.
- Follow the same procedure as for repeatability but under varied conditions.
- Analyze a minimum of three concentration levels with three replicates each.
- Compare results from both sets of data using statistical tests (e.g., Student's t-test).
Acceptance Criteria: %RSD for repeatability should typically be ≤ 2% for assay of drug substance, and ≤ 3% for drug product. Results from intermediate precision should show no significant difference between operators or instruments [9].
Protocol for Linearity and Range Determination
Objective: To establish that the method provides results proportional to analyte concentration.
Materials and Reagents:
- Reference standard
- Appropriate solvents and reagents
Procedure:
- Prepare a minimum of five standard solutions covering the specified range (e.g., 50%, 75%, 100%, 125%, 150% of target concentration).
- Analyze each concentration in triplicate.
- Plot the mean response against concentration.
- Perform linear regression analysis to calculate the correlation coefficient, y-intercept, and slope of the line.
Acceptance Criteria: The correlation coefficient (r) should typically be ≥ 0.999 for assay methods. The y-intercept should not be significantly different from zero, and the residuals should be randomly distributed [9].
The Scientist's Toolkit: Essential Materials and Reagents
Successful analytical method validation requires specific, high-quality materials and reagents. The following table details essential components of the validation toolkit.
Table 2: Essential Research Reagent Solutions and Materials for Analytical Method Validation
| Material/Reagent | Function and Importance in Validation | Key Quality Considerations |
|---|---|---|
| Reference Standards | Certified reference materials of known purity and identity serve as the benchmark for accuracy determination [9]. | Must be of certified purity and properly characterized; traceable to national or international standards. |
| Chromatographic Columns | Essential for separation-based methods (HPLC, GC); critical for achieving specificity and resolution [10]. | Multiple columns from different lots should be tested to demonstrate robustness and column-to-column reproducibility. |
| High-Purity Solvents & Reagents | Used for preparation of mobile phases, standard and sample solutions; impurities can interfere with analysis [10]. | HPLC or LC-MS grade solvents minimize background noise and interference, especially important for LOD/LOQ determination. |
| Mass Spectrometry Reference Compounds | For mass-dependent detectors; used for calibration and ensuring accurate mass measurement [9]. | Should be appropriate for the mass range being analyzed and compatible with the ionization technique used. |
| System Suitability Standards | Specific test mixtures used to verify that the total analytical system is adequate for the intended analysis [9]. | Must contain components that test critical method parameters (resolution, efficiency, tailing). |
| Placebo Formulation | For drug product methods; used in accuracy studies to assess interference from excipients [9]. | Should contain all formulation components except the active ingredient, representing the complete sample matrix. |
Critical Importance in Pharmaceutical Development
Analytical procedure validation plays an indispensable role in ensuring pharmaceutical product quality, safety, and efficacy through several critical dimensions:
Ensuring Regulatory Compliance and Product Quality
Validation is a mandatory requirement for regulatory submissions such as New Drug Applications (NDAs) and Abbreviated New Drug Applications (ANDAs) [11]. Regulatory bodies including the FDA, European Medicines Agency (EMA), and other global authorities require comprehensive validation data to support the identity, potency, quality, and purity of pharmaceutical substances and products [10] [11]. Without proper validation, regulatory submissions face substantial delays or rejection, potentially preventing products from reaching the market [10].
The process provides documented evidence that analytical methods can consistently generate reliable data for critical quality decisions, including batch release, stability studies, and shelf-life determination [7] [9]. This documented evidence is essential during regulatory inspections and audits, demonstrating a commitment to quality and compliance [6].
Protecting Patient Safety
Perhaps the most crucial aspect of analytical procedure validation is its role in safeguarding patient health [10]. Validated methods ensure that:
- Drugs contain the correct amount of active ingredient, ensuring proper dosing and therapeutic efficacy [7].
- Impurities and degradation products are properly identified and controlled within safe limits [2].
- Products maintain their identity, purity, and quality throughout their shelf life [7].
The thorough assessment of specificity, accuracy, and precision provides assurance that analytical results truly reflect the quality attributes of the product, preventing the release of substandard or potentially harmful medications to the market [10].
Supporting Robust Quality Control Systems
Well-validated analytical methods form the foundation of effective quality control systems in pharmaceutical manufacturing [10]. They provide the necessary tools for:
- Raw Material Testing: Ensuring the quality of incoming materials before they enter the manufacturing process [7].
- In-Process Controls: Monitoring critical parameters during manufacturing to ensure process consistency [7].
- Finished Product Testing: Verifying that the final product meets all established specifications before release [7].
- Stability Studies: Monitoring product quality over time to establish appropriate storage conditions and expiration dates [12].
The robustness evaluation within validation ensures that methods remain reliable despite minor variations in laboratory conditions, equipment, or analysts, contributing to the overall robustness of the quality control system [9].
Analytical procedure validation stands as a cornerstone practice in pharmaceutical development and manufacturing, providing the critical evidence that analytical methods are fit for their intended purpose. The ICH Q2(R1) guideline, while recently complemented by updated standards, continues to provide the fundamental framework for demonstrating method suitability through the assessment of specificity, accuracy, precision, and other key parameters.
The critical importance of validation extends far beyond mere regulatory compliance, serving as an essential safeguard for patient safety and a fundamental component of effective pharmaceutical quality systems. As the industry continues to evolve with increasingly complex molecules and advanced analytical technologies, the principles of method validation remain constant in their purpose: to ensure that analytical data driving critical quality decisions are reliable, accurate, and reproducible.
The ongoing evolution toward a lifecycle approach with ICH Q2(R2) and Q14 further strengthens this foundation, emphasizing that method quality is built through systematic development, thorough validation, and continuous monitoring throughout the method's operational life. For researchers, scientists, and drug development professionals, understanding and implementing these validation principles remains non-negotiable for ensuring product quality and, ultimately, patient safety.
In the pharmaceutical industry, the validation of analytical procedures is a fundamental regulatory requirement to ensure the quality, safety, and efficacy of drug substances and products. The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," serves as the primary global standard for this critical activity [11]. It provides a harmonized framework for validating analytical methods, ensuring that data generated are reliable and reproducible for regulatory submissions and quality control [3] [7].
Analytical method validation provides documented evidence that a specific analytical procedure is suitable for its intended use, consistently producing results that accurately reflect the quality of the material being tested [13] [7]. According to ICH Q2(R1), analytical procedures are predominantly categorized into three major types, each addressing a fundamental aspect of pharmaceutical quality as defined by the identity, purity, and content of a medicinal product [14]. This article provides an in-depth technical guide to these three core types—identification tests, impurity tests, and assays—detailing their purposes, validation requirements, and practical methodologies within the framework of ICH Q2(R1).
The Three Primary Analytical Procedure Categories
The three categories of analytical procedures directly correspond to the core tenets of pharmaceutical quality as outlined in the definition of the German Medicines Act (AMG) and other international regulations: identity, purity, and content [14]. Simply put, they answer the following critical questions:
- Does it contain what is declared? (Identity)
- Does it exclusively contain what is declared? (Purity)
- Does it contain as much as is declared? (Content) [14]
The table below summarizes the key characteristics of these analytical procedure categories.
Table 1: Overview of Primary Analytical Procedure Categories per ICH Q2(R1)
| Procedure Category | Primary Objective | Key Validation Parameters* | Example Techniques |
|---|---|---|---|
| Identification Tests | To verify the identity of an analyte in a sample [14]. | Specificity [14] [13] | Color reactions, FTIR, Peptide Mapping, PCR [14] |
| Impurity Tests | To detect and quantify or limit impurities and degradation products [14]. | Specificity, Accuracy, Precision (Quantitative); Specificity, LOD, LOQ (Limit Test) [13] | HPLC, GC, Limit tests for arsenic or residual solvents [14] [13] |
| Assays | To quantify the analyte or measure its potency in a sample [14]. | Specificity, Linearity, Accuracy, Precision [14] [13] | HPLC/UV-Vis Assay, Bioassays, Potency Tests [14] |
*Note: This list includes the most critical parameters; other parameters may be required based on the specific procedure [13].
Identification Tests
Purpose and Principle
Identification tests are performed to confirm the identity of an active pharmaceutical ingredient (API) or other analyte in a given sample [14]. This is a fundamental regulatory requirement to prove that a drug product contains the correct substance claimed to have healing properties [14]. The core principle involves comparing a property of the analyte in the sample to that of a authenticated reference standard [14].
Key Validation Parameter: Specificity
The paramount validation parameter for an identification test is specificity (sometimes referred to as selectivity) [14] [13]. The method must demonstrate its ability to unequivocally discriminate between the analyte of interest and other closely related substances that might be present, such as impurities, degradation products, or excipients [14] [13]. A non-specific method can lead to false positives or negatives, compromising patient safety and product efficacy.
Experimental Protocols and Techniques
The choice of technique depends on the complexity of the molecule and the required level of discrimination.
- For Small Molecules: Techniques like color reactions (as listed in pharmacopoeias), Fourier-Transform Infrared (FTIR) spectroscopy, or melting point determination are commonly used due to their simplicity and speed [14].
- For Biologics: More sophisticated techniques are necessary. Peptide mapping provides a unique "fingerprint" for a protein based on its specific cleavage pattern [14]. Capillary isoelectric focusing (cIEF) can identify a known monoclonal antibody charge variant among a pool of others [14]. Techniques like Western Blotting or immunofluorescence use specific antibodies to bind and identify target proteins or viruses [14]. Polymerase Chain Reaction (PCR) is a highly specific identity test for nucleic acid-containing pharmaceuticals, as specific primers amplify only a defined gene sequence unique to the target [14].
Impurity Tests
Purpose and Principle
Impurity tests are designed to establish the purity profile of a drug substance or product by detecting, and often quantifying, impurities and degradation products [14]. The objective is to demonstrate that all impurities are controlled below levels considered safe for the patient [14]. These procedures can be either quantitative, providing a precise measurement of impurity content, or limit tests, which simply demonstrate that an impurity is below a specified acceptable threshold [14].
Key Validation Parameters
The validation parameters required depend on whether the test is quantitative or a limit test.
- For Quantitative Impurity Tests: Key parameters include specificity (to ensure separation from the main analyte and other impurities), accuracy (to ensure the measured value is close to the true amount), precision, LOQ (the lowest level that can be accurately quantified), and linearity across the expected range [14] [13].
- For Limit Tests: The focus is on specificity and the LOD (the lowest level at which the impurity can be detected) [14] [13].
Experimental Protocols and Techniques
- Quantitative Tests: Chromatographic techniques like High-Performance Liquid Chromatography (HPLC) are the gold standard for quantifying impurities. The method is validated to ensure it can resolve and accurately measure known and potential unknown impurities.
- Limit Tests: These are often used for common, potentially toxic contaminants. Examples include colorimetric or photometric methods that show a visible color change when the impurity concentration exceeds the limit [14]. Pharmacopoeias such as the European Pharmacopoeia (Ph. Eur.) include limit tests for substances like methanol, formaldehyde, and arsenic [14].
Assays
Purpose and Principle
Assays are analytical procedures used for the quantification of the major analyte in a sample [14]. This category can be divided into two main aspects:
- Content Determination: Measures the amount of the active pharmaceutical ingredient present in the drug product [14].
- Potency Testing: Measures the biological or functional activity of the API, which is critical for complex molecules like biologics where the amount does not directly correlate with therapeutic effect [14].
Key Validation Parameters
For a typical content assay, the key validation parameters as per ICH Q2(R1) include specificity, linearity, accuracy, and precision [14] [13]. The method must be proven to accurately and reproducibly measure the analyte across the specified range without interference.
Experimental Protocols and Techniques
- Content Assays: Techniques like HPLC with UV-Vis detection are widely used for small molecules [14]. For proteins, a simple UV absorption measurement at 280 nm is often sufficient for content determination [14].
- Potency Assays (Bioassays): These are essential for biologics. They are often cell-based or biochemical assays that measure a specific biological response. An example is a clot lysis assay for tissue plasminogen activator (tPA), which directly measures the enzyme's functional activity [14]. For live viral vaccines, a plaque-forming unit (PFU) virus titration is used, which quantifies the amount of infectious virus, thereby reflecting its potency [14].
It is important to note that a single method may lack full specificity. The ICH Q2(R2) guideline notes that a lack of specificity in one procedure (e.g., a PFU assay that cannot distinguish between virus strains) can be compensated by other supporting procedures (e.g., a specific identification test using antibodies) [14].
The Method Validation Lifecycle and Experimental Protocols
The following diagram illustrates the interconnected stages of the analytical procedure lifecycle, from initial design through to ongoing performance verification, as informed by modern regulatory thinking [15].
Core Validation Parameters and Protocols
The validation process involves conducting specific experiments to demonstrate that the analytical procedure meets predefined acceptance criteria for a set of core performance characteristics [11] [13]. The parameters required depend on the type of analytical procedure, as summarized in the table below.
Table 2: Validation Parameters for Different Analytical Procedure Types (based on ICH Q2(R1))
| Validation Parameter | Definition | Identification | Impurity Test (Quantitative) | Assay (Content) |
|---|---|---|---|---|
| Accuracy | Closeness of results to the true value [13]. | - | Yes [13] | Yes [13] |
| Precision (Repeatability, Intermediate Precision) | Closeness of repeated individual measurements [13]. | - | Yes [13] | Yes [13] |
| Specificity | Ability to assess analyte unequivocally in the presence of potential interferents [13]. | Yes [14] [13] | Yes [13] | Yes [13] |
| Linearity | Ability to obtain results proportional to analyte concentration [13]. | - | Yes [13] | Yes [13] |
| Range | Interval between upper and lower analyte levels demonstrating suitability [13]. | - | Yes [13] | Yes [13] |
| LOD | Lowest amount of analyte that can be detected [13]. | - | Yes [13] | - |
| LOQ | Lowest amount of analyte that can be quantified [13]. | - | Yes [13] | - |
Accuracy
- Protocol: Accuracy is typically established by analyzing a sample of known concentration (e.g., a reference standard) and calculating the percent recovery of the measured value. Alternatively, the method of standard addition ("spiking") is used, where a placebo is spiked with a known, precise amount of the analyte, and the recovery is calculated [13]. This should be performed across the specified range of the procedure, often at a minimum of three concentration levels with multiple replicates each [13].
Precision
Precision has three tiers:
- Repeatability (Intra-assay Precision): Assesses precision under the same operating conditions over a short time interval. Protocol: A minimum of nine determinations covering the specified range (e.g., three concentrations/three replicates each) or a minimum of six determinations at 100% of the test concentration [13].
- Intermediate Precision: Expresses within-laboratory variations (e.g., different days, different analysts, different equipment) [13].
- Reproducibility: Expresses precision between laboratories, often assessed during method transfer [13]. Precision is measured by the scatter of individual results and expressed as the relative standard deviation (RSD) [13].
Specificity
- Protocol: For chromatographic assays, specificity is demonstrated by injecting samples containing potential interferents (impurities, degradation products forced through stress studies, excipients) and showing that the analyte peak is pure and unaffected (e.g., with peak purity tools) and that interferents are baseline separated [13].
Linearity and Range
- Protocol: Linearity is assessed by preparing a series of samples where the analyte concentration spans the claimed range of the procedure. A minimum of five concentrations is recommended [13]. The data is evaluated by appropriate statistical methods, such as linear regression analysis, and the correlation coefficient, y-intercept, and slope of the regression line are reported [13]. The range is derived from these linearity studies [13].
Essential Research Reagents and Materials
The integrity of analytical method validation is contingent upon the quality of the materials used. The following table details key reagent solutions and their critical functions.
Table 3: Essential Research Reagent Solutions for Analytical Method Validation
| Reagent / Material | Function and Importance in Validation |
|---|---|
| Reference Standard | An authenticated substance of known purity and identity used as a benchmark for all quantitative and qualitative measurements (e.g., for calibration, identification, potency tests) [14]. |
| Placebo Formulation | A mixture of all excipients without the active ingredient. Critical for specificity testing and for accuracy studies via the standard addition (spiking) method [13]. |
| System Suitability Test (SST) Solutions | Specific mixtures containing the analyte and key impurities used to verify that the chromatographic system (or other instrumentation) is performing adequately at the time of the test [13]. |
| Forced Degradation Samples | Samples of the drug substance and product that have been intentionally stressed under various conditions (e.g., heat, light, acid, base, oxidation). Used to demonstrate the stability-indicating properties and specificity of the method [13]. |
| Certified Mobile Phases and Reagents | High-purity solvents, buffers, and other chemical reagents are essential for achieving the required specificity, sensitivity (LOD/LOQ), and robustness, as variations can significantly impact method performance [13]. |
Within the rigorous framework of ICH Q2(R1), the categorization of analytical procedures into identification, impurity testing, and assays forms the bedrock of pharmaceutical quality control. Each category serves a distinct and vital purpose in verifying the identity, purity, and strength of a drug product, thereby directly ensuring patient safety and product efficacy. A thorough understanding of the specific validation parameters required for each procedure type, coupled with the execution of robust experimental protocols, is non-negotiable for regulatory compliance. As the industry evolves, the principles outlined in ICH Q2(R1) continue to provide a stable foundation, even as newer guidelines like ICH Q2(R2) and ICH Q14 introduce enhanced, lifecycle-based approaches for analytical procedures [11] [6]. For researchers and drug development professionals, mastering these core analytical procedure types is an essential competency for successfully bringing safe and effective medicines to market.
In the highly regulated pharmaceutical landscape, demonstrating that an analytical method is suitable for its intended purpose is not merely a best practice—it is a fundamental regulatory requirement. This process, formally known as analytical method validation, provides documented evidence that the method consistently produces reliable, accurate, and reproducible results that are fit for their intended use in supporting the identity, strength, quality, purity, and potency of drug substances and products [16] [17]. The International Council for Harmonisation (ICH) guideline Q2(R1), "Validation of Analytical Procedures," serves as the internationally recognized standard for this critical activity, outlining the scientific framework and specific performance parameters that must be evaluated [6] [18]. Validation confirms that a method's performance characteristics meet the requirements for its analytical application, thereby providing assurance of reliability during normal use and forming the foundation of quality in the analytical laboratory [17].
The importance of this demonstration cannot be overstated. A flawed or unsuitable analytical method can lead to questionable results, potentially compromising patient safety, leading to costly product recalls, and causing significant delays in regulatory approval [16]. For researchers, scientists, and drug development professionals, a thorough understanding and execution of method validation according to ICH Q2(R1) is therefore indispensable. It is the crucial link between raw laboratory data and evidence-based, regulatory-ready decisions, ensuring that every test result generated can be trusted to reflect the true quality of the pharmaceutical product.
Core Principles of ICH Q2(R1) Method Validation
The ICH Q2(R1) guideline establishes a comprehensive framework for validating analytical methods. Its core principle is that the validation effort must be commensurate with the method's purpose and the stage of product development [16]. The guideline systematically categorizes the validation requirements based on the type of analytical procedure (e.g., identification, impurity testing, or assay), and defines the key performance parameters that must be evaluated to prove a method's suitability [18].
Distinguishing Validation from Verification and Qualification
A critical first step is understanding the distinction between validation, verification, and qualification, as these terms are often misused. Each serves a distinct purpose within the pharmaceutical quality system:
- Validation: A formal, comprehensive process that demonstrates a method's suitability for its intended use through extensive laboratory studies. It is typically required for methods used in the routine quality control testing of drug substances, raw materials, or finished products for release and stability testing [16].
- Verification: A more limited process performed to confirm that a previously validated method works as expected in a new laboratory setting, with its specific analysts, equipment, and environmental conditions. This is often applicable when adopting a compendial method (e.g., from the USP) [16].
- Qualification: An early-stage evaluation of an analytical method's performance, often used during early development phases (preclinical or Phase I). It provides preliminary data showing the method is likely reliable before committing to a full validation [16].
For the purposes of this guide, the focus is on the full validation required for methods supporting commercial products and critical decision-making.
The Validation Lifecycle and Regulatory Context
Method validation is not an isolated event but part of a broader validation lifecycle. This lifecycle begins with qualified instrumentation and validated software, proceeds through method development and validation, and is maintained through system suitability tests and ongoing performance verification [17]. Regulatory authorities, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), require full validation for methods that support decision-making for the finished product, and they expect compliance with guidelines such as ICH Q2(R1) [16] [6]. Furthermore, the recent introduction of ICH Q14 on Analytical Procedure Development and the update of ICH Q2(R1) to Q2(R2) emphasize a more structured, lifecycle approach, incorporating Quality by Design (QbD) principles and continuous validation processes [6].
Key Validation Parameters and Experimental Protocols
The demonstration of method suitability is achieved through the experimental assessment of specific performance characteristics. The following sections detail the key validation parameters outlined in ICH Q2(R1), their definitions, and the standard experimental protocols for their determination.
Specificity
Definition: Specificity is the ability of the method to assess the analyte unequivocally in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [18].
Experimental Protocol:
- Analyze Blank and Placebo: Inject the sample matrix or formulation placebo without the analyte to demonstrate the absence of interfering signals at the retention time of the analyte and other critical peaks.
- Analyze Spiked Samples: Spike the placebo or matrix with the analyte at the target concentration to confirm that the response is due solely to the analyte.
- Stress Testing (Forced Degradation): Subject the sample to stress conditions (e.g., acid/base, oxidative, thermal, photolytic) to generate degradation products. Analyze the stressed sample to demonstrate that the analyte peak is pure and resolved from degradation peaks, and that the method can detect the degradants. This is often assessed using a diode array detector (DAD) to check for peak purity [18].
Accuracy
Definition: Accuracy expresses the closeness of agreement between the value found and the value accepted as a true or reference value. It is typically reported as percent recovery [18].
Experimental Protocol:
- Prepare a reference standard of the analyte with known, high purity.
- Spike the placebo or matrix with the analyte at a minimum of three concentration levels covering the specified range (e.g., 80%, 100%, 120% of the target concentration).
- Perform a minimum of nine determinations (e.g., three replicates at each of the three levels).
- Calculate the percent recovery for each measurement and determine the mean recovery across all levels. Acceptance criteria are typically 98-102% for assay methods [18].
Precision
Definition: Precision expresses the closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions. It is considered at three levels: repeatability, intermediate precision, and reproducibility [18].
Experimental Protocol:
- Repeatability (Intra-assay Precision):
- Assay a minimum of six independent preparations of a homogeneous sample at 100% of the test concentration.
- Calculate the relative standard deviation (RSD). Acceptance criteria for assay methods are typically an RSD of less than 2% [18].
- Intermediate Precision:
- Demonstrate the method's reliability under variations within the same laboratory.
- Perform the analysis on different days, with different analysts, and using different equipment.
- Compare the results from both sets of data; no significant variation should be observed.
- Reproducibility: Reproducibility is assessed when method transfer occurs between laboratories, such as during a collaborative study [18].
Detection Limit (LOD) and Quantitation Limit (LOQ)
Definitions:
- LOD: The lowest concentration of an analyte that can be detected, but not necessarily quantified, under the stated experimental conditions.
- LOQ: The lowest concentration of an analyte that can be quantified with acceptable accuracy and precision [18].
Experimental Protocol (Calculation Methods):
- Signal-to-Noise Ratio: Typically applied to chromatographic methods. A ratio of 3:1 is generally accepted for LOD, and 10:1 for LOQ [18].
- Standard Deviation of the Response and Slope:
- LOD can be calculated as (3.3 \times \sigma / S), where (\sigma) is the standard deviation of the response (y-intercept) and (S) is the slope of the calibration curve.
- LOQ can be calculated as (10 \times \sigma / S) [18].
Linearity and Range
Definitions:
- Linearity: The ability of the method to obtain test results that are directly proportional to the concentration of the analyte within a given range.
- Range: The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the method has suitable levels of accuracy, precision, and linearity [18].
Experimental Protocol:
- Prepare a minimum of five concentrations spanning the intended range (e.g., 50%, 75%, 100%, 125%, 150%).
- Analyze each concentration in triplicate.
- Plot the response versus the concentration and perform linear regression analysis.
- The correlation coefficient (r) should be not less than 0.995. The y-intercept should be not significantly different from zero, and the residuals should be randomly scattered [18].
Robustness
Definition: The robustness of a method is a measure of its capacity to remain unaffected by small, deliberate variations in method parameters, and provides an indication of its reliability during normal usage [18].
Experimental Protocol:
- Deliberately introduce small changes to critical method parameters. For an HPLC method, this could include:
- Variations in mobile phase pH (±0.2 units)
- Variations in column temperature (±5°C)
- Variations in flow rate (±10%)
- Different columns (from different lots or suppliers)
- Analyze a standard and a sample under each varied condition.
- Evaluate the impact on critical results such as resolution, tailing factor, and assay value. The method should perform acceptably under all tested conditions.
The table below summarizes the key validation parameters, their experimental objectives, and typical acceptance criteria for a quantitative assay method, providing a clear overview for protocol design and reporting.
Table 1: Summary of Key ICH Q2(R1) Validation Parameters and Criteria
| Validation Parameter | Objective | Typical Experimental Approach | Typical Acceptance Criteria (for Assay) |
|---|---|---|---|
| Specificity | To prove the method measures only the analyte. | Compare blank, placebo, and analyte; perform forced degradation studies. | No interference from placebo, impurities, or degradants at the analyte retention time. Peak purity confirmed. |
| Accuracy | To determine the closeness to the true value. | Spike and recover analyte from placebo/matrix at 3 levels with 9 determinations. | Mean recovery of 98–102% [18]. |
| Precision | To determine the degree of scatter in the data. | Analyze 6 samples at 100% test concentration. | RSD < 2% for repeatability [18]. |
| Linearity | To demonstrate proportional response to concentration. | Analyze a minimum of 5 concentrations across the range. | Correlation coefficient (r) ≥ 0.995 [18]. |
| Range | To confirm accuracy, precision, and linearity across the operating range. | The interval from the LOQ to 120% of the test concentration for assay. | Meets accuracy and precision criteria across the specified range [18]. |
| LOD | To determine the lowest detectable amount. | Signal-to-Noise ratio or based on standard deviation of the response and the slope. | Signal-to-Noise ratio ~ 3:1 [18]. |
| LOQ | To determine the lowest quantifiable amount with accuracy and precision. | Signal-to-Noise ratio or based on standard deviation of the response and the slope. | Signal-to-Noise ratio ~ 10:1. At LOQ, accuracy and precision should be demonstrated [18]. |
| Robustness | To assess the method's resistance to deliberate parameter changes. | Vary critical parameters (pH, temperature, flow rate, column). | System suitability criteria are met; no significant impact on results. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful execution of validation protocols relies on the use of high-quality, well-characterized materials. The following table details key reagents and their critical functions in ensuring the integrity of the validation study.
Table 2: Key Research Reagent Solutions for Method Validation
| Reagent / Material | Function in Validation |
|---|---|
| Reference Standard | A substance of established quality, purity, and identity used as a benchmark for assessing the performance of the analytical method and for quantifying the analyte [18]. |
| High-Purity Solvents | Used for preparation of mobile phases, sample solutions, and standards. Purity is critical to prevent baseline noise, ghost peaks, or unintended chemical interactions. |
| Placebo / Blank Matrix | The formulation or biological matrix without the active analyte. It is essential for demonstrating specificity by proving the absence of interfering signals and for conducting accuracy (recovery) studies [18]. |
| Characterized Impurities and Degradation Products | Isolated and identified impurities and forced degradation products are used to challenge the method's specificity, ensuring it can separate and resolve the analyte from other related substances. |
| System Suitability Test Solutions | A stable, well-characterized mixture of the analyte and critical impurities, or a standard, used to verify that the chromatographic system is adequate for the intended analysis before and during the validation runs [17] [18]. |
Method Validation Workflow and Relationship Diagram
The following diagram illustrates the logical sequence and relationships between the core activities in the analytical method validation lifecycle, from initial preparation through to ongoing verification.
Analytical Method Validation Workflow
Demonstrating that an analytical method is suitable for its intended purpose through rigorous validation, as dictated by the core principles of ICH Q2(R1), is a non-negotiable pillar of pharmaceutical development and quality control. It is a deliberate, science-based process that transforms a laboratory procedure from a theoretical concept into a trusted tool for critical decision-making. By systematically evaluating the parameters of specificity, accuracy, precision, and the others outlined herein, scientists generate the documented evidence required by regulators and, more importantly, build the confidence that their methods will reliably safeguard patient health. As the industry evolves with the adoption of ICH Q14 and Q2(R2), the principles of a structured, lifecycle approach and enhanced method development will further strengthen this foundation, ensuring that analytical methods continue to meet the challenges of modern, complex therapeutics [6].
In the global pharmaceutical industry, the validation of analytical methods is a regulatory imperative to ensure the safety, quality, and efficacy of drug products. The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," provides the foundational scientific framework for this process. Its adoption and interpretation by regulatory agencies worldwide, particularly the U.S. Food and Drug Administration (FDA), form a complex landscape that researchers and drug development professionals must navigate. This guide examines the precise relationship between the ICH Q2(R1) standard and FDA regulations, detailing how this global guideline is implemented under U.S. regulatory oversight and providing explicit experimental protocols for compliance.
The ICH Q2(R1) and FDA Regulatory Nexus
The ICH Q2(R1) guideline establishes the core validation parameters and methodologies accepted by its member regions, including the United States, the European Union, and Japan. The FDA integrates this guideline directly into its regulatory expectations for drug applications. While ICH Q2(R1) provides the scientific and methodological basis, the FDA enforces it through its own guidance documents and inspectional activities. A critical understanding for any applicant is that the FDA views method validation not as a one-time event but as an activity spanning the entire method lifecycle, from initial development and validation to ongoing verification and monitoring during the product's market life [19] [20].
For instance, the FDA's own guidance documents, such as those for specific product categories like tobacco products, reinforce the need for fully validated and verified analytical test methods in application submissions, which is fully consistent with the principles of ICH Q2(R1) [21]. The selection of the appropriate validation guideline is not arbitrary; it is determined by the product's target market. Using a guideline misaligned with the regulatory region, such as submitting data based solely on EMA expectations to the FDA, can result in rejected applications, costly revalidation, and significant product launch delays [19].
Table 1: Core Regulatory Bodies and Their Guidance Alignment with ICH Q2(R1)
| Regulatory Body | Regional Focus | Primary Guidance | Key Emphasis in Validation |
|---|---|---|---|
| FDA | United States | ICH Q2(R1) and supporting FDA-specific guidances | Lifecycle validation, risk management, data integrity for regulatory submissions [21] [19]. |
| EMA | European Union | ICH Q2(R1) | Scientific rigor, compliance with EU regulatory directives. |
| PMDA | Japan | ICH Q2(R1) | Alignment with Japanese Pharmacopoeia and national standards. |
The following diagram illustrates the interconnected regulatory and scientific workflow for method validation, from foundational guidelines to ongoing process control.
Structured Comparison of Validation Parameters
Adherence to ICH Q2(R1) requires the systematic testing of specific analytical performance parameters. The following tables provide a structured overview of these core parameters and the standard experimental protocols for assessing them, offering a clear, comparable format essential for laboratory execution and regulatory documentation.
Table 2: Core Validation Parameters as Defined by ICH Q2(R1) and Regulatory Expectations
| Validation Parameter | ICH Q2(R1) Definition | Regulatory Purpose & Objective |
|---|---|---|
| Accuracy | The closeness of agreement between a conventionally accepted true value and the value found. | To demonstrate that the method provides results that are unbiased and reflect the true value of the analyte, crucial for patient safety and dosing. |
| Precision (Repeatability & Intermediate Precision) | The closeness of agreement between a series of measurements. | To ensure the method produces consistent results under normal operating conditions, across different days, analysts, and equipment. |
| Specificity | The ability to assess the analyte unequivocally in the presence of components that may be expected to be present. | To prove the method can distinguish and quantify the analyte from impurities, degradants, or matrix components. |
| Linearity | The ability of the method to obtain test results proportional to the concentration of the analyte. | To establish that the method's response is directly proportional to analyte concentration across a specified range. |
| Range | The interval between the upper and lower concentrations of analyte for which it has been demonstrated that the method has suitable precision, accuracy, and linearity. | To define the concentrations over which the method is fit for purpose, ensuring it covers all intended applications. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters. | To identify critical method parameters and ensure reliability during routine use, such as in different laboratories. |
Table 3: Standard Experimental Protocols for Key Validation Parameters
| Parameter | Recommended Experimental Methodology | Typical Acceptance Criteria |
|---|---|---|
| Accuracy | Analyze a minimum of 9 determinations across a minimum of 3 concentration levels (e.g., 80%, 100%, 120% of target) in the presence of the sample matrix. Report % recovery of the known added amount or comparison to a reference method. | Mean Recovery: 98.0% - 102.0% RSD < 2.0% |
| Precision (Repeatability) | Perform a minimum of 6 independent preparations at 100% of the test concentration and analyze under the same operating conditions over a short interval of time. | RSD ≤ 1.0% for drug substance; RSD ≤ 2.0% for drug product (varies by product) |
| Linearity | Prepare and analyze a minimum of 5 concentration levels (e.g., 50%, 75%, 100%, 125%, 150% of target). Plot response vs. concentration and calculate regression statistics (slope, intercept, correlation coefficient). | Correlation Coefficient (r) ≥ 0.999 |
| Robustness | Deliberately vary method parameters (e.g., column temperature ±2°C, flow rate ±10%, mobile phase pH ±0.2 units) in a systematic, pre-planned design (e.g., Design of Experiments). Evaluate impact on system suitability criteria. | All results meet system suitability requirements; resolution of critical pairs > 2.0. |
Advanced Monitoring: Statistical Process Control (SPC) in the Method Lifecycle
The FDA's lifecycle approach to method validation necessitates robust ongoing monitoring strategies post-approval. Statistical Process Control (SPC) is a powerful methodology for this purpose, enabling scientists to monitor a method's performance over time and distinguish between inherent, common-cause variation and assignable, special-cause variation that requires investigation [22] [20].
SPC is most effectively implemented using control charts, which are graphical tools that plot process data (e.g., results from system suitability tests or quality control standards) against statistically derived control limits. The most common charts for continuous data in the laboratory are the Individual Moving Range (I-MR) chart and the X-bar & R chart [20]. Decision rules, such as the Western Electric Rules, are applied to these charts to detect non-random patterns that indicate a process may be going out of control. These rules include a single point outside the 3-sigma control limits, or two out of three consecutive points beyond the 2-sigma warning limits [20].
Table 4: Essential Research Reagent Solutions and Materials for Method Validation
| Item / Reagent Solution | Critical Function in Validation Experiments |
|---|---|
| Reference Standard (High-Purity) | Serves as the benchmark for quantifying the analyte; its certified purity and stability are foundational for accuracy, linearity, and specificity studies. |
| System Suitability Test (SST) Solutions | A mixture of key analytes and potential interferents used to verify that the chromatographic or analytical system is performing adequately at the start of, during, and at the end of a sequence. |
| Placebo/Blank Matrix | The drug product formulation without the active ingredient; critical for demonstrating specificity by proving the absence of interference at the retention time of the analyte. |
| Forced Degradation Samples | Samples of the drug substance or product subjected to stress conditions (heat, light, acid, base, oxidation); used to validate the method's ability to separate and quantify the analyte from its degradation products (Specificity). |
| Mobile Phase/Buffer Components | High-purity solvents and salts used to create the eluent system; their quality and precise preparation are vital for robustness, reproducibility, and consistent retention times. |
The integration of SPC within a modern quality management system is visualized in the following diagram, highlighting its role in maintaining a state of control.
The ICH Q2(R1) guideline provides the indispensable technical and scientific foundation for analytical method validation. Its adoption by the FDA and other major regulatory bodies creates a harmonized, though not identical, global standard. For researchers and drug development professionals, success hinges on a dual understanding: a deep mastery of the experimental protocols defined by ICH Q2(R1) and a strategic awareness of how these protocols are applied and monitored within the FDA's rigorous, lifecycle-oriented regulatory framework. By integrating robust initial validation with data-driven monitoring tools like SPC, organizations can ensure both compliance and continuous quality assurance throughout a product's market life.
Implementing Q2(R1): A Step-by-Step Guide to Validation Parameters
Within the framework of the ICH Q2(R2) guideline on analytical procedure validation, specificity stands as a foundational parameter, critical for ensuring the reliability of identity, assay, and impurity tests methods [23]. It is the quality that demonstrates that an analytical procedure can unambiguously assess the analyte of interest when other components are present in the sample matrix. In the context of drug development, this means proving that a method can accurately measure the active pharmaceutical ingredient (API) and distinguish it from excipients, impurities, degradation products, or other potential interferents. A specific method provides confidence that the reported result is truly representative of the analyte and is not biased by the presence of other substances, thereby forming the bedrock of product quality, safety, and efficacy assessments.
This technical guide provides an in-depth exploration of specificity, detailing its regulatory context, experimental methodologies, and data interpretation strategies to equip scientists with the knowledge to robustly validate their analytical procedures.
Core Definition and Regulatory Significance
Specificity is defined as the ability to assess unequivocally the analyte in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [9]. It takes into account the degree of interference from other active ingredients, excipients, impurities, and degradation products. For a chromatographic method, this ensures that a peak's response is due to a single component, with no peak co-elutions [9].
The significance of specificity is directly tied to the purpose of the analytical procedure:
- For Identification: Specificity must be able to discriminate between compounds of closely related structures which are likely to be present.
- For Purity Tests: The method must demonstrate that it can separate and accurately quantify all specified impurities and degradation products from the API and from each other.
- For Assay (Content/Potency): The method must be shown to be unaffected by the presence of impurities, excipients, or other matrix components.
The International Council for Harmonisation (ICH) guideline Q2(R2), which came into effect in 2023, provides the harmonized framework for validating analytical procedures for the pharmaceutical industry [23]. Compliance with this guideline is essential for regulatory submissions within ICH member regions, including the European Medicines Agency (EMA).
Experimental Design for Specificity Assessment
A well-designed specificity experiment challenges the analytical method with samples containing all potential interferents to prove its discriminatory power.
Sample Types for Specificity Challenges
To conclusively demonstrate specificity, a set of deliberately challenged samples must be analyzed and compared to a reference standard of the pure analyte.
Key Experimental Protocols
Forced Degradation Studies
Forced degradation (or stress testing) is a critical part of specificity validation for stability-indicating methods. The goal is to generate representative samples containing degradation products.
- Protocol: Separate portions of the drug substance or product are subjected to various stress conditions.
- Acidic/Basic Hydrolysis: Treat with a defined concentration (e.g., 0.1-1 M) of HCl or NaOH for a specified time and temperature (e.g., at 60°C for several hours or days).
- Oxidative Degradation: Treat with an oxidizing agent (e.g., 0.1-3% hydrogen peroxide) under controlled conditions.
- Thermal Degradation: Expose the solid drug substance or product to elevated temperatures (e.g., 70-105°C).
- Photolytic Degradation: Expose to UV and visible light as per ICH Q1B conditions.
- Analysis: The stressed samples are analyzed, and the chromatograms are examined for the formation of degradation products. The method should successfully resolve the main analyte peak from all degradation peaks. Peak purity testing (discussed in Section 4) is essential for these samples.
Resolution of Critical Pair
This test directly challenges the method's ability to separate the most difficult-to-separate components.
- Protocol: Prepare a mixture containing the analyte and a closely eluting impurity or degradation product. Alternatively, a mixture of the drug product with all known impurities can be used. The analysis should demonstrate baseline separation (Resolution, Rs > 1.5) between the analyte and this critical pair [9].
Analytical Techniques and Peak Purity Assessment
While traditional chromatography parameters are necessary, modern guidance emphasizes advanced techniques for unequivocal specificity demonstration.
The Scientist's Toolkit: Essential Technologies
Table 1: Key Technologies for Specificity Assessment
| Technology / Reagent | Primary Function in Specificity Assessment |
|---|---|
| High-Performance Liquid Chromatography (HPLC) | The primary separation platform for resolving analytes from interferents. |
| Photodiode-Array (PDA) Detector | Collects full spectra across a peak; the primary tool for confirming peak homogeneity/purity by spectral comparison [9]. |
| Mass Spectrometry (MS) Detector | Provides unequivocal peak purity information, exact mass, and structural data; highly effective for identifying unknown degradants [9]. |
| Chemical Reference Standards | Pure substances of the analyte and known impurities used to confirm identity and retention time. |
| Stressed/Degraded Samples | Artificially generated samples containing potential interferents to challenge the method's discriminatory power. |
Peak Purity Assessment
This is a definitive test to prove that a chromatographic peak corresponds to a single chemical entity, with no hidden co-eluting compounds.
- Using a PDA Detector: Modern PDA detectors collect spectra across a range of wavelengths at every point during a peak's elution. Software algorithms then compare these spectra. A pure peak will show a high degree of spectral similarity throughout, while a peak with a co-eluting impurity will show spectral variations [9].
- Using Mass Spectrometry: MS detection is a more powerful technique for peak purity. It can detect co-eluting compounds based on differences in mass-to-charge ratio, even if they have identical UV spectra. The combination of both PDA and MS on a single instrument provides valuable orthogonal information for a comprehensive specificity assessment [9].
It is important to note the limitations of PDA-based purity testing, including a lack of UV response from potential interferents and limitations in distinguishing compounds with very similar spectra, especially at low relative concentrations [9].
Data Analysis, Acceptance Criteria, and Comparison of Methods
Key Parameters and Acceptance Criteria
The data generated from specificity experiments must be evaluated against predefined, scientifically justified acceptance criteria.
Table 2: Specificity Parameters and Typical Acceptance Criteria
| Analytical Procedure | Parameter | Typical Acceptance Criteria |
|---|---|---|
| All Procedures | Peak Purity | The peak is determined to be pure by PDA or MS (i.e., no co-elution detected) [9]. |
| Chromatographic Assay/Impurity Test | Resolution (Rs) | Baseline separation between analyte and closest eluting peak; Rs ≥ 1.5 [9]. |
| Assay (Drug Product) | Interference from Placebo | No interference (peak area < reporting threshold) from placebo at the retention time of the analyte peak. |
| Impurity Test | Separation of Impurities | All specified impurities are resolved from each other and from the main analyte. |
Comparison of Methods for Comprehensive Validation
The ICH Q2(R2) guideline emphasizes that validation should be a structured process, with specificity being one critical component among others. As outlined in the Comparison of Methods Experiment, assessing the systematic error or inaccuracy of a method is another key validation activity [24]. While specificity ensures the signal is correct, a comparison of methods (often against a well-characterized reference method) quantifies the overall systematic error.
- Purpose: To estimate inaccuracy by analyzing patient samples (or representative test samples) by both the new (test) method and a comparative method [24].
- Statistical Analysis: For methods with a wide analytical range, linear regression statistics (slope, y-intercept) are calculated. The systematic error (SE) at a critical medical decision concentration (Xc) is determined as: Yc = a + bXc, then SE = Yc - Xc [24]. This provides a quantitative measure of the method's accuracy, which complements the qualitative assurance provided by specificity.
Specificity is a non-negotiable attribute of a validated analytical method, serving as the primary defense against analytical interference that could compromise data integrity and patient safety. A robust demonstration of specificity requires a holistic approach, combining traditional chromatographic resolution with modern peak purity assessment tools like PDA and MS. By designing rigorous experiments that include forced degradation studies and the analysis of spiked samples, and by adhering to the structured framework of ICH Q2(R2), scientists can provide the documented evidence required to prove that their method unambiguously measures what it is intended to measure, thereby ensuring the quality, safety, and efficacy of pharmaceutical products throughout their lifecycle.
In the pharmaceutical sciences, the reliability of any analytical result is paramount, directly impacting drug safety, efficacy, and quality. Within the framework of the International Council for Harmonisation (ICH) Q2(R1) guideline, "Validation of Analytical Procedures: Text and Methodology," accuracy and precision emerge as two fundamental pillars that establish the trueness and reliability of results [5] [3]. These parameters are not isolated concepts but are integral components of a holistic validation process that ensures an analytical method is fit for its intended purpose [25] [11]. Accuracy is defined as the closeness of agreement between a test result and an accepted reference value, essentially measuring the trueness of the method [25] [9]. Precision, on the other hand, expresses the closeness of agreement (degree of scatter) between a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions, thereby quantifying the reliability of the method [9] [26]. Together, they provide the foundational confidence that analytical data generated for regulatory submissions, such as those required by the U.S. Food and Drug Administration (FDA), are trustworthy and meaningful [5] [11]. This guide provides an in-depth technical exploration of these critical characteristics, detailing their definitions, experimental protocols, and role in ensuring data integrity within the ICH Q2(R1) paradigm.
Theoretical Foundations: Defining the Core Concepts
Accuracy (Trueness)
Accuracy, often referred to as "trueness," is a measure of systematic error. It provides an answer to the fundamental question: "Is the method measuring the correct value?" According to ICH Q2(R1), accuracy should be established across the specified range of the analytical procedure [5] [9]. For drug substance analysis, accuracy is typically demonstrated by comparing the results to the analysis of a standard reference material or by comparison to a second, well-characterized method [9]. For the assay of drug products, accuracy is evaluated through the analysis of synthetic mixtures spiked with known quantities of components [9]. In the context of quantifying impurities, accuracy is determined by analyzing samples spiked with known amounts of impurities [9]. A common technique for determining accuracy in complex matrices is the spike recovery method, where the amount of a target compound is determined as a percentage of the theoretical amount present in the matrix [26]. The percentage recovery is calculated as (Measured Concentration / Known Concentration) * 100%, with results close to 100% indicating high accuracy [9] [26].
Precision (Reliability)
Precision, a measure of random error, characterizes the reproducibility of measurements. It addresses the question: "Can the method produce the same result consistently?" The ICH guideline mandates that precision should be considered at three levels: repeatability, intermediate precision, and reproducibility [9].
- Repeatability (intra-assay precision) refers to the precision under the same operating conditions over a short interval of time [9]. It is assessed using a minimum of nine determinations covering the specified range (e.g., three concentrations and three replicates each) or a minimum of six determinations at 100% of the test concentration [9]. Results are typically reported as the relative standard deviation (RSD) or coefficient of variation (%CV) [9].
- Intermediate precision expresses within-laboratory variations, such as different days, different analysts, or different equipment [9]. An experimental design is used to monitor the effects of these individual variables, and results are often subjected to statistical testing (e.g., Student's t-test) to examine differences [9].
- Reproducibility represents the precision between different laboratories, typically assessed during collaborative studies [9]. While critical for method standardization, it is not always required for routine method validation [9].
Table 1: Summary of Precision Measures in Analytical Method Validation
| Precision Measure | Conditions of Assessment | Typical Experimental Design | Reporting Metric |
|---|---|---|---|
| Repeatability | Same analyst, same equipment, short time interval | ≥9 determinations over specified range or ≥6 at 100% | % RSD |
| Intermediate Precision | Different days, different analysts, different equipment | Replicate sample preparations by two analysts | % RSD & statistical comparison of means |
| Reproducibility | Different laboratories | Collaborative studies between labs | % RSD & confidence intervals |
The Interrelationship: Accuracy vs. Precision
The relationship between accuracy and precision is best understood visually, as they are independent but complementary concepts. A method can be precise but not accurate, accurate but not precise, neither, or both. The ideal analytical procedure demonstrates high levels of both accuracy and precision, ensuring results are both correct and consistent. The following diagram illustrates these fundamental relationships.
Experimental Protocols for Establishing Accuracy and Precision
Standard Experimental Protocol for Accuracy
The ICH Q2(R1) guideline and related literature provide a clear framework for demonstrating accuracy [9] [26]. The following workflow outlines the standard protocol for conducting an accuracy study, typically through a spike recovery experiment.
Detailed Methodology:
- Sample Preparation: Accuracy is typically assessed using a minimum of nine determinations over a minimum of three concentration levels covering the specified range (e.g., 80%, 100%, and 120% of the target concentration) with three replicates per level [9] [26].
- Analysis: The prepared samples are analyzed using the complete analytical procedure, including all sample preparation steps, to account for potential losses during extraction, filtration, or other manipulations [26].
- Calculation: The recovery for each sample is calculated. When the analyte is naturally present in the matrix (e.g., in a crude botanical), the recovery is calculated using the formula:
Recovery % = [(Found Amount - Native Amount) / Added Amount] * 100%[26]. - Data Reporting: Data should be reported as the percent recovery of the known, added amount for each concentration level, or as the difference between the mean and the true value along with confidence intervals (e.g., ±1 standard deviation) [9].
Standard Experimental Protocol for Precision
The evaluation of precision, particularly repeatability and intermediate precision, follows a structured approach involving replication under varying conditions. The following workflow details the key steps.
Detailed Methodology:
Repeatability (Intra-assay Precision):
- A homogeneous sample is prepared and analyzed multiple times. The ICH guideline suggests a minimum of nine determinations covering the specified range (three concentrations/three replicates each) or a minimum of six determinations at 100% of the test concentration [9].
- All analyses are performed by the same analyst, using the same equipment and reagents, within a short time frame [9].
- The standard deviation (SD) and relative standard deviation (%RSD) of the results are calculated. The %RSD is calculated as
(Standard Deviation / Mean) * 100%[9].
Intermediate Precision:
- The degree of intermediate precision should be established based on the circumstances under which the method is intended to be used. A common approach involves two different analysts each preparing and analyzing replicate sample preparations on different days or using different HPLC systems [9].
- Each analyst uses their own standards and solutions. The results from all analyses are pooled, and the overall %RSD is calculated to reflect the method's performance under normal laboratory variations [9].
- The results from the different analysts can be subjected to statistical testing (e.g., a Student's t-test) to examine if there is a significant difference in the mean values obtained [9].
Table 2: Experimental Design and Acceptance Criteria for Accuracy and Precision
| Validation Parameter | Experimental Design | Recommended Acceptance Criteria |
|---|---|---|
| Accuracy | 9 determinations over 3 concentration levels (3 reps each) [9]. | Data reported as % recovery. Acceptance criteria are method-specific but must be justified [9] [26]. |
| Precision (Repeatability) | 6 determinations at 100% test concentration or 9 determinations over specified range [9]. | Reported as %RSD; acceptance criteria depend on analyte and level but must be justified [9]. |
The Scientist's Toolkit: Essential Reagents and Materials
The following table details key research reagents and materials essential for conducting robust accuracy and precision studies, along with their critical functions.
Table 3: Key Research Reagent Solutions and Materials for Method Validation
| Reagent / Material | Function / Purpose | Critical Considerations |
|---|---|---|
| Certified Reference Standard | Serves as the benchmark for identity and purity to establish calibration curves and calculate recovery [26]. | Purity must be verified; certificate of analysis should be obtained. Assumed purity is a source of inaccuracy [26]. |
| High-Purity Solvents & Reagents | Used for mobile phase preparation, sample extraction, and dilution. | Impurities can cause high background noise, interfering with detection and quantification, affecting both accuracy and precision [9]. |
| Placebo / Blank Matrix | The drug product formulation without the active ingredient(s). Used to prepare spiked samples for accuracy studies [9]. | Must be truly representative of the sample matrix without containing the analyte to avoid false positive signals [25]. |
| Chromatographic Column | The stationary phase for separation in HPLC or UPLC analyses. | Column selectivity is critical for specificity; different column lots or brands can affect retention time and resolution, impacting precision and accuracy [9]. |
| System Suitability Standards | A reference preparation used to verify that the chromatographic system is adequate for the intended analysis [9]. | Typically a mixture of key analytes; system performance parameters (e.g., tailing factor, theoretical plates, %RSD) must meet pre-set criteria before validation runs [9]. |
Regulatory Context and Evolving Standards
Adherence to ICH Q2(R1) is a foundational requirement for regulatory submissions across global jurisdictions, including the FDA and the European Medicines Agency [5] [11] [27]. The principles outlined in this guideline ensure that analytical methods for assessing the identity, strength, quality, purity, and potency of drug substances and products are thoroughly validated [5] [11]. It is crucial for scientists to be aware that the regulatory landscape is evolving. The recent finalization of ICH Q2(R2) and the introduction of ICH Q14 on "Analytical Procedure Development" signify a modernized, lifecycle approach to analytical methods [6] [11].
These updated guidelines emphasize a more scientific, risk-based approach, encouraging the use of an Analytical Target Profile (ATP) which prospectively defines the required performance criteria of a method, including accuracy and precision [6] [11]. They also enhance requirements for validation, mandating more detailed statistical methods and linking the method's range directly to its ATP [6]. While the core definitions of accuracy and precision remain, the context of their application is becoming more integrated with method development and lifecycle management, moving beyond a one-time validation exercise [6] [11]. This evolution aims to ensure that methods remain robust, reliable, and continuously suitable for their intended use throughout their operational life, thereby supporting the consistent quality and safety of pharmaceutical products [6].
Within the framework of ICH Q2(R1) analytical method validation, linearity and range are fundamental performance characteristics that establish the reliability of an analytical procedure [28] [29]. Linearity is defined as the ability of a method to elicit test results that are directly proportional to the concentration of the analyte in a sample within a given range [30] [12]. The range is the interval between the upper and lower concentration levels of the analyte for which suitable levels of precision, accuracy, and linearity have been demonstrated [28] [30].
For researchers and drug development professionals, demonstrating these parameters provides documented evidence that an analytical method is fit for its intended purpose, a requirement for regulatory submissions to agencies like the FDA and EMA [31] [12]. This guide details the experimental protocols and evaluation criteria for establishing linearity and range in compliance with ICH Q2(R1).
Regulatory Definitions and Importance
Core Principles under ICH Q2(R1)
ICH Q2(R1) harmonizes the definitions and validation requirements for analytical procedures, ensuring consistency and reliability in the assessment of drug substances and products [29].
- Linearity demonstrates a direct proportional relationship between analyte concentration and instrument response [29]. This is a cornerstone for quantitative methods, as it confirms that the method can accurately measure the analyte across the intended concentrations.
- Range is directly derived from linearity studies and defines the specific concentration interval over which the method is validated [30]. The validated range must encompass all expected sample concentrations and is contingent upon the method's intended application, such as assay or impurity testing [28].
Role in Analytical Method Lifecycle
The demonstration of linearity and a defined range is not a one-time exercise but a critical part of the analytical procedure lifecycle [30] [12]. A properly established range ensures that the method will produce reliable data during quality control testing, stability studies, and clinical trial sample analysis [31]. Regulatory authorities mandate this validation to ensure the continued quality, safety, and efficacy of pharmaceutical products [29].
Establishing Linearity: Experimental Design and Protocol
Preparation of Linearity Standards
A robust linearity experiment begins with careful preparation of standard solutions.
- Number of Concentration Levels: A minimum of five, and preferably more, distinct concentration levels are recommended [32] [33] [28].
- Concentration Range: The standards should be prepared from independent stock solutions to bracket the expected concentration range. A common practice is to prepare standards from 50% to 150% of the target analyte concentration [33]. For an assay of a drug substance or product, ICH Q2(R1) suggests a typical range of 80-120% of the target concentration [28].
- Matrix Considerations: Whenever possible, standards should be prepared in a blank matrix that matches the sample matrix to account for potential matrix effects [33]. For drug product analysis, this may involve spiking a placebo formulation.
Experimental Methodology
The following step-by-step protocol ensures a comprehensive assessment of linearity.
Step 1: Preparation. Prepare a minimum of five standard solutions at different concentrations, evenly spaced across the intended range. Each concentration level should be analyzed in triplicate to assess variability [33]. Step 2: Analysis. Analyze the standard solutions in a random order to prevent systematic bias from instrument drift [33]. Step 3: Data Recording. Record the instrumental response (e.g., peak area, absorbance) for each injection.
The workflow for the linearity experiment is systematic and can be visualized as follows:
Statistical Evaluation and Data Analysis
Regression Analysis and Acceptance Criteria
Once the data is collected, statistical analysis is performed to evaluate the linear relationship.
- Regression Model: A least squares regression line is fitted to the data, establishing the equation
y = a + bx, whereyis the response,xis the concentration,bis the slope, andais the y-intercept [34]. - Correlation Coefficient (r): The correlation coefficient should be reported. However, a high
rvalue close to 1.0 alone is not sufficient proof of linearity [34]. - Coefficient of Determination (r²): A more commonly used metric is r². For chromatographic methods, an r² value of ≥ 0.995 is often required, while for bioanalytical methods, ≥ 0.990 may be acceptable [33] [28]. The intercept should be statistically insignificant from zero [34].
Table 1: Key Statistical Parameters for Linearity Assessment
| Parameter | Description | Typical Acceptance Criteria |
|---|---|---|
| Correlation Coefficient (r) | Measures the strength of the linear relationship. | > 0.998 (or as per protocol) [34] |
| Coefficient of Determination (r²) | Proportion of variance in response explained by concentration. | ≥ 0.995 (for HPLC) [33] [12] |
| Y-Intercept | The value of y when x is zero. | Should not be statistically different from zero [34] |
| Slope | The rate of change of response with concentration. | Should be statistically significant [34] |
Analysis of Residuals
A critical step often overlooked is the visual inspection of residual plots [33] [34]. Residuals are the differences between the observed response and the response predicted by the regression line.
- A random scatter of residuals around zero indicates a good fit for the linear model.
- A recognizable pattern (e.g., U-shaped curve) in the residual plot indicates non-linearity, suggesting a more complex model may be needed [34].
Troubleshooting Non-Linearity
Common issues and their solutions include:
- Heteroscedasticity: When the variance of residuals increases with concentration, it violates the assumption of equal variance. Solution: Use weighted least squares regression (e.g., 1/x or 1/x²) to assign more importance to less variable points [34].
- Matrix Effects: Interference from the sample matrix can cause non-linearity. Solution: Use a matched blank matrix for preparing standards or employ a standard addition method [33].
- Detector Saturation: At high concentrations, the instrument response may plateau. Solution: Dilute samples to remain within the linear dynamic range of the detector [33].
Defining the Validated Range
The range is determined from the linearity data and is the interval where the method meets acceptable criteria for precision, accuracy, and linearity [30].
Table 2: Typical Ranges for Different Analytical Procedures (as per ICH)
| Analytical Procedure | Recommended Range |
|---|---|
| Assay of Drug Substance/Product | 80% - 120% of the target concentration [28] |
| Impurity Testing | From reporting threshold to 120% of the specification [28] |
| Content Uniformity | 70% - 130% of the test concentration [30] |
| Dissolution Testing | ±20% over the specified range (e.g., Q+20%) [28] |
The relationship between the established linearity and the final validated range is a critical decision point, as shown in the logic below:
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for Linearity and Range Studies
| Item | Function in Experiment |
|---|---|
| Certified Reference Standard | Provides the analyte of known purity and identity for preparing standard solutions with accurate concentrations [33]. |
| Blank Matrix | The analyte-free base material (e.g., placebo for drug product, biological fluid for bioanalysis) used to prepare standards and account for matrix effects [33] [34]. |
| High-Purity Solvents & Reagents | Used for preparing mobile phases, standard solutions, and sample dilutions to prevent interference and background noise [31]. |
| Volumetric Glassware | Certified Class A pipettes, flasks, and volumetric cylinders ensure accurate and precise measurement of volumes during standard preparation [33]. |
| Quality Control (QC) Samples | Independent samples at known concentrations (low, mid, high within the range) used to verify the accuracy and precision of the calibration model [34]. |
The rigorous demonstration of linearity and range is a non-negotiable element of analytical method validation under ICH Q2(R1). By following a structured experimental protocol involving a minimum of five concentration levels, employing appropriate statistical analysis including residual evaluation, and defining the range where precision, accuracy, and linearity are assured, scientists can generate reliable and defensible data. This process ensures that analytical methods used in pharmaceutical development and quality control are truly fit for purpose, thereby supporting the safety, efficacy, and quality of medicines for patients.
Within the framework of analytical method validation, the establishment of sensitivity thresholds is a fundamental requirement for ensuring the reliability of data used in drug development and quality control. For professionals working under the ICH Q2(R1) guideline, the Limit of Detection (LOD) and Limit of Quantitation (LOQ) are critical parameters that define the operational boundaries of an analytical procedure [23] [11] [3]. The LOD represents the lowest amount of analyte that can be detected but not necessarily quantified, while the LOQ is the lowest concentration that can be determined with acceptable accuracy and precision [35] [36] [37]. Properly determining these limits is essential for methods intended to detect and measure low levels of impurities, degradation products, or active ingredients in pharmaceutical substances and products, ensuring they are "fit for purpose" [38] [11].
The following diagram illustrates the statistical relationship between the blank, LOD, and LOQ, and their associated error rates.
Defining the Fundamental Parameters
Limit of Blank (LoB)
The Limit of Blank (LoB) is a foundational concept for understanding detection capabilities. It is defined as the highest apparent analyte concentration expected to be found when replicates of a blank sample containing no analyte are tested [38]. In practice, even a blank sample can produce an analytical signal that might be misinterpreted as a low concentration of analyte. The LoB establishes the threshold above which a signal is considered statistically different from the background noise [38].
Calculation Formula:
LoB = mean_blank + 1.645(SD_blank) [38]
This formula assumes a Gaussian distribution of the raw analytical signals from blank samples. The LoB is set to exceed 95% of the observed blank values, meaning that only 5% of blank measurements (false positives or Type I errors) will exceed this limit due to random variation [38].
Limit of Detection (LOD)
The Limit of Detection (LOD) is the lowest analyte concentration that can be reliably distinguished from the LoB and at which detection is feasible [38]. It is important to note that the LOD is a detection limit, not a quantification limit; at this concentration, the analyte can be identified as present, but without guaranteed precision or accuracy of the measured value [35] [37].
Calculation Formula (per CLSI EP17):
LOD = LoB + 1.645(SD_low concentration sample) [38]
This calculation utilizes both the measured LoB and test replicates of a sample containing a low concentration of analyte. Assuming a Gaussian distribution, this ensures that 95% of values from a sample at the LOD concentration will exceed the LoB, limiting false negatives (Type II errors) to 5% [38].
Limit of Quantitation (LOQ)
The Limit of Quantitation (LOQ), also known as the Lower Limit of Quantitation (LLOQ), is the lowest concentration at which the analyte can not only be reliably detected but also quantified with acceptable accuracy and precision [38] [36]. The LOQ represents a higher threshold of performance where predefined goals for bias and imprecision are met, making it suitable for reporting quantitative results [35] [36].
Table 1: Key Characteristics of LoB, LOD, and LOQ
| Parameter | Definition | Primary Focus | Typical Statistical Basis |
|---|---|---|---|
| LoB | Highest concentration expected from a blank sample | Distinguishing noise from potential signal | mean_blank + 1.645(SD_blank) [38] |
| LOD | Lowest concentration reliably distinguished from LoB | Detecting the presence of the analyte | LoB + 1.645(SD_low concentration sample) or 3.3σ/S [38] [35] |
| LOQ | Lowest concentration quantified with acceptable accuracy and precision | Providing a reliable numerical result | 10σ/S or concentration yielding ≤20% CV [35] [36] |
Experimental Protocols for Determination
The determination of LOD and LOQ requires a structured experimental approach. The following workflow outlines a comprehensive protocol for establishing these limits, incorporating data from blank, low-concentration, and calibration curve experiments.
Sample Preparation and Analysis
Sample Types:
- Blank Sample: A sample of the matrix devoid of the analyte (e.g., a placebo formulation or a zero-level calibrator) [38].
- Low-Concentration Sample: A sample with the analyte present at a concentration near the expected LOD/LOQ. This can be prepared by diluting the lowest non-negative calibrator or by spiking the matrix with a known, low amount of analyte [38].
- Calibration Standards: For the calibration curve method, prepare a series of standards in the range of the expected LOD/LOQ [35].
Replication:
Calculation Methodologies
Based on Blank and Low-Concentration Sample Standard Deviation
This method, detailed in the CLSI EP17 guideline, is empirical and directly compares analytical responses [38].
- LoB Calculation: Analyze multiple replicates (n ≥ 20) of the blank sample. Calculate the mean and standard deviation (SD_blank).
LoB = mean_blank + 1.645(SD_blank)[38]. - LOD Calculation: Analyze multiple replicates (n ≥ 20) of a low-concentration sample. Calculate the mean and standard deviation (SD_low).
LOD = LoB + 1.645(SD_low concentration sample)[38]. - Verification: The provisional LOD should be verified. If more than 5% of measurements from a sample at the LOD concentration fall below the LoB, the LOD must be re-estimated using a sample of higher concentration [38].
Based on Calibration Curve and Standard Deviation of Response
This approach, referenced in ICH guidelines, uses the standard error of the regression and the slope of the calibration curve [35] [36].
- Calibration Curve: Construct a calibration curve using samples with analyte concentrations in the range of the expected LOD/LOQ.
- Determine Standard Deviation (σ): The standard deviation (σ) can be estimated as:
- Calculate LOD and LOQ:
Based on Signal-to-Noise Ratio
This method is applicable primarily to instrumental techniques that exhibit baseline noise, such as chromatography [35] [36].
- Measurement: Compare measured signals from known low-concentration samples with those of a blank sample.
- Acceptance Criteria:
Table 2: Comparison of LOD and LOQ Determination Methods
| Method | Approach | Typical Application | Key Formulas |
|---|---|---|---|
| Blank & Low-Concentration SD | Empirical measurement of sample responses | General use, especially in clinical chemistry | LOD = LoB + 1.645(SD_low) [38] |
| Calibration Curve & SD of Response | Statistical analysis of regression data | Instrumental analyses, common in pharmaceutical analysis | LOD = 3.3σ/S, LOQ = 10σ/S [35] [36] |
| Signal-to-Noise Ratio | Direct comparison of analyte signal to background noise | Chromatography (HPLC, GC) and other instrumental methods | LOD: S/N ≈ 3:1, LOQ: S/N ≈ 10:1 [35] [36] |
Establishing Acceptance Criteria for LOQ
For the LOQ, it is not sufficient to merely calculate a value. The concentration must be experimentally confirmed to meet predefined performance goals for accuracy and precision [36].
- Prepare and Analyze: Prepare at least five replicates of a sample at the calculated LOQ concentration.
- Evaluate Precision and Accuracy:
- Confirmation: If these criteria are met, the LOQ is confirmed. If not, a higher concentration must be tested until the criteria are satisfied [36].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting robust LOD and LOQ studies.
Table 3: Essential Reagents and Materials for LOD/LOQ Studies
| Item | Function / Purpose | Critical Considerations |
|---|---|---|
| Blank Matrix | A sample material without the analyte used to establish the baseline signal and LoB. | Must be commutable with real patient or test samples to accurately reflect analytical noise [38]. |
| Authentic Analyte Standard | A material of known purity and identity used to prepare low-concentration samples and calibration standards. | High purity is critical for accurate preparation of known concentrations for spiking [38]. |
| Calibration Standards | A series of samples with known analyte concentrations used to construct the calibration curve. | Should cover the range from below the expected LOQ to above it to ensure a reliable curve fit [35]. |
| Quality Control (QC) Samples at LOD/LOQ | Independent samples spiked at or near the LOD and LOQ concentrations. | Used to verify the calculated limits; crucial for demonstrating method performance [36]. |
| Appropriate Solvents and Diluents | For dissolving, diluting, and preparing sample and standard solutions. | Must be compatible with the analyte and matrix, and not interfere with the detection system. |
The accurate determination of the Limit of Detection and Limit of Quantitation is a non-negotiable component of analytical method validation under ICH Q2(R1). By understanding the distinct definitions of LoB, LOD, and LOQ and implementing the detailed experimental protocols outlined—whether based on standard deviation of blank and low-concentration samples, calibration curve data, or signal-to-noise ratios—scientists can establish defensible sensitivity thresholds. The confirmation of the LOQ with predefined accuracy and precision criteria (typically ≤20% bias and imprecision) ensures that the analytical method is truly "fit for purpose," providing reliable data for critical decisions in pharmaceutical development and quality assurance. This rigorous approach guarantees that methods can reliably detect and quantify trace levels of analytes, thereby supporting drug safety and efficacy.
Within the framework of the ICH Q2(R1) guideline for analytical procedure validation, robustness and system suitability serve as critical pillars ensuring that methods remain reliable and fit-for-purpose under normal conditions of use. Robustness is formally defined as "a measure of [an analytical procedure's] capacity to remain unaffected by small, but deliberate variations in method parameters" [12]. It provides an indication of the method's inherent reliability during routine use. Closely related is system suitability testing (SST), which verifies that the analytical system—comprising the instrument, reagents, samples, and data processing—is functioning correctly at the time of analysis [2].
These elements are not isolated validation parameters but are fundamentally interconnected with other performance characteristics. A method that demonstrates poor robustness will likely exhibit variable precision, accuracy, and specificity when transferred between laboratories, instruments, or analysts [39]. For pharmaceutical scientists and drug development professionals, establishing robustness and implementing rigorous system suitability testing forms the foundation of a robust analytical control strategy, ensuring data integrity and regulatory compliance throughout the product lifecycle [12].
Experimental Determination of Method Robustness
Protocol Design and Parameter Selection
The experimental assessment of robustness requires a structured approach to evaluate the impact of deliberate, slight variations in method parameters on analytical results. The selection of which parameters to investigate should be science- and risk-based, focusing on those factors that experience or prior knowledge suggests could influence the method's output [39].
A standard robustness testing protocol involves varying one parameter at a time while keeping all others constant and measuring the effect on defined outcomes, such as resolution, tailing factor, or assay result. The typical experimental workflow for a robustness study, particularly for chromatographic methods, is systematically outlined below.
Diagram 1: Experimental workflow for robustness testing.
Key Parameters and Assessment Criteria
The parameters investigated vary significantly depending on the analytical technique. For chromatographic methods, common factors include variations in mobile phase pH and composition, column temperature, flow rate, and detection wavelength [39]. For other methods, parameters could include extraction time, solvent strength, or sample stability. The effects of these variations are measured against predefined, quantitative acceptance criteria that align with the method's intended purpose.
Table 1: Typical Parameters and Acceptance Criteria for Robustness Evaluation in Chromatographic Methods
| Parameter Category | Specific Examples of Variations | Typical Measured Outcomes | Example Acceptance Criteria |
|---|---|---|---|
| Mobile Phase | pH ± 0.1-0.2 units, organic ratio ± 1-2%, buffer concentration ± 10% | Resolution, Tailing Factor, Retention Time, Assay Result | Resolution > 1.5; Tailing Factor ≤ 2.0 [39] |
| Chromatographic Column | Different column batches or brands, equivalent L# stationary phases | Resolution, Retention Time, Peak Shape | Retention time variability < 2% RSD [39] |
| Instrumental | Flow rate ± 0.1 mL/min, column temperature ± 2-5°C, detection wavelength ± 2-3 nm | Peak Area, Retention Time, Signal-to-Noise | Assay result within 98.0-102.0% of target [39] |
| Sample Preparation | Extraction time ± 10%, solvent volume ± 5%, centrifugation speed ± 10% | Recovery, Precision, Assay Result | Recovery 98-102%; RSD < 2% [39] |
System Suitability Testing: The Analytical Gatekeeper
Definition and Regulatory Basis
System suitability testing is defined as "a series of tests to show that the analytical system is performing up to the standard defined by the method validation at the time of the analysis" [2]. It is a mandatory verification step performed prior to, and sometimes during, each analytical run to ensure that the complete analytical system—the instrument, reagents, column, and operator—is functioning correctly and can produce reliable data [39]. Its regulatory basis is firmly established in ICH Q2(R1) and pharmacopeial chapters like USP <1225> [40].
The primary function of SST is to serve as a final quality gate, providing confidence that the validated performance characteristics of the method, such as specificity, precision, and sensitivity, are being met during routine use. A system suitability test is therefore a diagnostic tool, and analytical runs are only considered valid if all SST criteria are met before proceeding with sample analysis.
Core System Suitability Parameters
The parameters monitored in system suitability testing are chosen to verify the critical performance aspects of the analytical system. While the specific requirements depend on the type of method, chromatographic procedures have well-established standard parameters.
Table 2: Core System Suitability Parameters for Chromatographic Methods
| SST Parameter | Definition and Purpose | Typical Acceptance Criteria |
|---|---|---|
| Theoretical Plates (N) | Measure of column efficiency and peak sharpness. | N > 2000 [39] |
| Tailing Factor (T) | Measure of peak symmetry; indicates potential adsorption issues. | T ≤ 2.0 [39] |
| Resolution (Rs) | Ability to separate two adjacent peaks; critical for specificity. | Rs > 1.5 between critical pair [39] |
| Repeatability (Precision) | Injected 5 or 6 replicates of a standard to verify short-term precision of the system. | %RSD ≤ 1.0-2.0% for assay [39] |
| Signal-to-Noise Ratio (S/N) | For quantitative methods, verifies the method's sensitivity is acceptable. | S/N ≥ 10 for the quantitation limit [39] |
The logical relationship between the various components of an analytical procedure and how they are secured through validation and verified via system suitability is summarized in the following framework.
Diagram 2: The role of robustness and SST in the analytical control strategy.
The Scientist's Toolkit: Essential Reagents and Materials
The execution of robust analytical methods and meaningful system suitability tests depends on the quality and consistency of key reagents and materials. The following table details essential items for ensuring method resilience and performance.
Table 3: Key Research Reagent Solutions for Robustness and System Suitability
| Item | Function and Importance |
|---|---|
| Reference Standards | High-purity, well-characterized substances used to prepare system suitability test solutions and calibration standards; their quality is fundamental to accuracy [39]. |
| Chromatographic Columns | Multiple batches or equivalent columns from different suppliers are critical for robustness studies to ensure method performance is not column-specific [39]. |
| System Suitability Test Mixtures | Solutions containing all critical analytes (e.g., API, known impurities) at specified levels to verify resolution, precision, and other SST parameters before sample analysis [39]. |
| Qualified Reagents and Solvents | Mobile phase components, extraction solvents, and buffers; their specified purity and quality (e.g., HPLC-grade) prevent introduction of interference or noise [39]. |
Robustness and system suitability are not merely regulatory checkboxes but are fundamental to the practical success and longevity of an analytical procedure. A thoroughly investigated robustness profile provides scientists with a clear understanding of a method's operational limits, facilitating effective troubleshooting and informed risk management. System suitability testing then translates this validated potential into verified performance for every analytical run. Together, they form an indispensable partnership that protects data integrity, ensures regulatory compliance, and ultimately guarantees that analytical methods consistently deliver results that are reliable, reproducible, and fit for their intended purpose in drug development and quality control.
Beyond the Protocol: Troubleshooting and Optimizing Your Validated Methods
Common Validation Pitfalls and How to Avoid Them
Analytical method validation is a critical, documented process that proves a laboratory procedure consistently produces reliable, accurate, and reproducible results, ensuring compliance with regulatory frameworks like ICH Q2(R1) and safeguarding pharmaceutical quality and patient safety [41]. However, this process is inherently complex, and common pitfalls can compromise the reliability of methods, delay regulatory approvals, and trigger costly audits [42] [41]. This guide, framed within the context of ICH Q2(R1) research, explores these frequent errors across key validation parameters and provides actionable strategies to avoid them, equipping researchers and drug development professionals with the knowledge to ensure robust and compliant analytical methods.
Core Validation Parameters and Associated Pitfalls
The following table summarizes the primary validation characteristics as outlined in ICH Q2(R1) and the common mistakes associated with each [42] [43] [41].
| Validation Parameter | Common Pitfalls | Consequences |
|---|---|---|
| Specificity/Selectivity | Not investigating all potential interferences (e.g., from complex sample matrices, solvents, buffers); not considering sample changes over time (e.g., degradation) [42]. | Inability to unequivocally evaluate the analyte; unreliable results during stability studies [42]. |
| Accuracy | Not evaluating accuracy in the presence of sample matrix components; performing replicate measurements instead of replicate sample preparations [43]. | Bias (systematic error) is missed or underestimated, leading to inaccurate quantification of the analyte, especially in complex biologics [43] [44]. |
| Precision | Insufficient sample size or improper application of statistical methods [41]. | High statistical uncertainty and reduced confidence in the repeatability and intermediate precision of the method [41]. |
| Linearity & Range | Testing linearity in solution without a study of reconstituted samples; too few data points [41] [45]. | Failure to identify a matrix effect; inability to define the range where the method provides linear results with suitable accuracy and precision [45]. |
| Robustness | Using test conditions that don't reflect routine operations; not identifying key method parameters through a systematic approach [41] [44]. | Method failures when minor, intentional variations occur in method parameters (e.g., flow rate, temperature) during transfer or routine use [41]. |
| General | Not setting appropriate, method-specific acceptance criteria; poor documentation [42] [41]. | Validation failure due to unjustified criteria; red flags during audits and regulatory reviews [42] [41]. |
In-Depth Analysis of Specificity and Accuracy Pitfalls
Specificity A critical mistake is failing to consider how samples may change over time, particularly in stability programs. For a method to be stability-indicating, it must be proven to accurately quantify the analyte and any potential degradation products. This often requires forced degradation studies as part of validation to demonstrate the method can separate all components of interest [42]. Furthermore, a thorough review of all potential interferences from the sample matrix and sample preparation reagents is essential [42].
Accuracy A fundamental error is failing to evaluate accuracy with samples that are as close as possible to the real test samples. The "pseudo-samples" used must contain all the sample matrix components. If the accuracy experiments use an unrepresentative matrix, a significant source of bias may be overlooked [43]. For impurities analysis in solid samples, this can be challenging, but preparing accuracy samples by spiking known amounts of impurities into the sample matrix, though not ideal, is often the only practical approach [43].
Detailed Experimental Protocols for Key Validation Experiments
Protocol for Specificity and Forced Degradation Studies
The objective of this experiment is to demonstrate that the analytical procedure can unequivocally quantify the analyte without interference from placebo, impurities, or degradation products [42] [45].
Methodology:
- Sample Preparation:
- Prepare and analyze a blank (e.g., solvent).
- Prepare and analyze a placebo (mixture of excipients without the active analyte).
- Prepare and analyze a standard of the analyte.
- Prepare and analyze a finished product (analyte with placebo).
- Forced Degradation: Subject the analyte and finished product to stress conditions (e.g., acid/base hydrolysis, oxidative stress, thermal stress, photolytic stress) to generate degradation products. The extent of degradation should be sufficient to simulate potential long-term changes [42].
Analysis: Analyze all prepared samples using the analytical procedure.
Data Evaluation and Acceptance Criteria:
- The blank and placebo chromatograms (or other relevant signals) should show no significant interference at the retention time (or equivalent) of the analyte peak.
- For the forced degradation samples, check that the analyte peak is pure and that all degradation products are baseline separated from the analyte peak and from each other. The method should be able to accurately quantify the analyte in the presence of these degradation products.
This workflow for specificity testing, including forced degradation, can be visualized as follows:
Protocol for Accuracy Evaluation
The objective is to determine the closeness of agreement between the value found and a value accepted as a true or reference value, thereby measuring the bias of the method [43] [45].
Methodology:
- Sample Preparation:
- Prepare a minimum of 9 determinations over a minimum of 3 concentration levels covering the specified range of the method (e.g., 80%, 100%, 120% of the target concentration) [43] [45].
- The samples must be "pseudo-samples" that are identical to real samples. For a drug product, this means spiking known amounts of the analyte into the placebo mixture [43].
- Each determination should be a separate preparation to capture the full variability of the method (e.g., 9 separate weighings into 9 separate volumetric flasks) [43].
Analysis: Analyze all prepared samples using the analytical procedure.
Data Evaluation and Acceptance Criteria:
- Calculate the recovery (%) for each determination: (Measured Concentration / Theoretical Concentration) × 100.
- Calculate the mean recovery and the relative standard deviation (RSD) for each concentration level and overall.
- The acceptance criteria must be set based on the method's intended use and product specification. For example, for a drug substance assay with a specification of 98.0-102.0%, the mean recovery should typically be between 98.0% and 102.0% with a suitable RSD [43].
The Scientist's Toolkit: Essential Reagent Solutions
The following table details key reagents and materials critical for successful method development and validation, explaining their function in the process.
| Item | Function in Validation |
|---|---|
| Well-Characterized Reference Standard | Serves as the accepted reference value for trueness/accuracy studies. Its purity and stability are foundational for all quantitative measurements [44]. |
| Representative Placebo/Blank Matrix | Critical for specificity testing. It must match the composition of the real product (without analyte) to prove the method does not measure interferences [45]. |
| Forced Degradation Reagents | Reagents like hydrochloric acid, sodium hydroxide, and hydrogen peroxide are used in forced degradation studies to intentionally stress the product and validate that the method is stability-indicating [42]. |
| High-Purity Solvents & Buffers | Used for mobile phases and sample preparation. Their purity and consistency are vital for achieving robust and reproducible chromatography, directly impacting precision and robustness [42] [41]. |
| Critical System Suitability Standards/ Mixtures | A prepared mixture used to verify that the chromatographic system is performing adequately before and during validation experiments. It typically tests for parameters like resolution, tailing factor, and repeatability [41]. |
The Lifecycle of an Analytical Method
The traditional view of validation as a one-time event is evolving. Modern regulatory thinking, reflected in new guidelines like ICH Q2(R2) and ICH Q14, emphasizes a lifecycle approach [6]. This involves continuous validation and assessment from method development through retirement, integrating principles of Quality by Design (QbD) and risk management from the outset [6]. The following diagram illustrates this holistic lifecycle, connecting development, validation, and ongoing monitoring.
Adopting this lifecycle mindset, where knowledge of the method's performance is continuously monitored and used to ensure ongoing reliability, is crucial for maintaining compliance in a dynamic regulatory environment [6] [45].
Navigating the complexities of analytical method validation requires a meticulous, science-driven approach that moves beyond simply ticking regulatory boxes. By understanding common pitfalls in specificity, accuracy, and other parameters—and implementing the detailed experimental protocols and lifecycle management strategies outlined in this guide—scientists and drug development professionals can significantly enhance the robustness and regulatory compliance of their analytical procedures. Ultimately, this diligence ensures the generation of reliable data, which is fundamental to guaranteeing product quality, efficacy, and patient safety.
Addressing Variability in Precision and Accuracy Studies
Within the framework of the International Council for Harmonisation (ICH) Q2(R1) guideline, the validation of analytical procedures ensures the quality, safety, and efficacy of pharmaceuticals [7]. Precision and accuracy stand as two fundamental validation parameters, providing documented evidence that an analytical method is reliable and fit for its intended purpose [9]. Accuracy refers to the closeness of agreement between a test result and an accepted reference value (or true value), while precision measures the closeness of agreement among a series of measurements obtained from multiple sampling of the same homogeneous sample under prescribed conditions [9] [18]. In simpler terms, accuracy indicates how close you are to the true value, and precision indicates how reproducible your results are.
Understanding, controlling, and minimizing variability in these studies is paramount. Variability, if unaccounted for, can compromise the reliability of analytical results, leading to incorrect decisions regarding drug quality. This guide provides a detailed examination of the sources of variability in precision and accuracy studies and offers robust experimental protocols and statistical tools to address them, ensuring compliance with regulatory standards and the generation of trustworthy data.
Fundamental Concepts: Precision, Accuracy, and Their Interplay
Precision and accuracy are distinct yet interrelated concepts. A method can be precise (producing tightly clustered results) without being accurate (the cluster is far from the true value), and vice versa. The ideal analytical method is both accurate and precise.
Deconstructing Precision: A Tiered Approach
Precision is evaluated at three tiers, each designed to assess different sources of variability [9] [18]:
Repeatability (Intra-assay Precision): This assesses precision under the same operating conditions over a short interval of time. It represents the smallest variability the method can achieve and is typically determined through a minimum of nine determinations covering the specified range (e.g., three concentrations, three replicates each) or a minimum of six determinations at 100% of the test concentration [9]. Results are reported as % Relative Standard Deviation (%RSD).
Intermediate Precision: This evaluates the impact of within-laboratory variations, such as different days, different analysts, or different equipment, on the analytical results. A well-designed study, where these factors are deliberately varied, demonstrates the method's robustness in a single laboratory [9].
Reproducibility: This represents the precision between different laboratories, such as during collaborative studies for method standardization. It is the most comprehensive measure of precision, assessing the method's performance across the global scientific community [9].
Quantifying Accuracy
Accuracy is established across the specified range of the analytical procedure [9]. For drug substances, it can be determined by comparing results to a standard reference material or a second, well-characterized method. For drug products, accuracy is typically evaluated by analyzing synthetic mixtures spiked with known quantities of components [9]. The ICH guideline recommends that data be collected from a minimum of nine determinations over a minimum of three concentration levels (e.g., 50%, 100%, 150%) covering the specified range [9]. Data are reported as the percent recovery of the known, added amount, or as the difference between the mean and the true value along with confidence intervals [46] [9].
The Emerging Concept of Total Analytical Error (TAE)
An advanced approach to addressing variability is the consideration of Total Analytical Error (TAE). TAE combines both accuracy (bias) and precision (imprecision) into a single metric, providing a more holistic view of the method's performance [47]. The concept is expressed as: TE ≈ |Bias| + 2 * SD where SD is the standard deviation representing precision [47]. This approach ensures that the combined impact of inaccuracy and imprecision does not exceed a predefined acceptance limit, which can be particularly useful for setting justified validation criteria. The recently implemented ICH Q2(R2) guideline acknowledges this approach as an alternative to the separate evaluation of accuracy and precision [47].
The following workflow outlines the strategic process for evaluating these parameters and managing variability.
Experimental Protocols for Assessing Precision and Accuracy
A meticulously designed experimental protocol is the first line of defense against uncontrolled variability.
Protocol for Precision Studies
The following table summarizes the key design elements for a comprehensive precision study.
Table 1: Experimental Design for Tiered Precision Evaluation
| Precision Tier | Objective | Minimum Experimental Design | Primary Output & Acceptance |
|---|---|---|---|
| Repeatability | Assess the basic method variability under identical conditions. | - Nine determinations across three concentration levels (e.g., 50%, 100%, 150%) in triplicate, or - Six determinations at 100% test concentration. | % RSD. Typically, RSD < 2% for assay methods [18]. |
| Intermediate Precision | Evaluate impact of intra-lab variations (e.g., analyst, day, instrument). | - Two analysts, each preparing replicates on different days using different HPLC systems (if available). | % RSD and statistical comparison (e.g., Student's t-test) of means. No significant difference between analysts. |
| Reproducibility | Determine method performance across different laboratories. | - Collaborative study involving multiple laboratories following the same, standardized protocol. | % RSD and % difference in mean values between labs. Criteria set prior to study. |
Protocol for Accuracy Studies
The accuracy protocol involves a spike and recovery experiment, which is calculated using the formula: Accuracy (%) = (Calculated Concentration / True Concentration) × 100 [46].
Table 2: Experimental Design for Accuracy Evaluation via Spike/Recovery
| Step | Description | Key Considerations |
|---|---|---|
| 1. Sample Preparation | Prepare samples spiked with known amounts of analyte at a minimum of three concentration levels (e.g., 50%, 100%, 150% of the target or specification limit). Use a minimum of nine determinations (e.g., triplicates at each level) [9]. | The sample matrix should be representative of the actual test samples (e.g., drug product placebo). |
| 2. Analysis & Calculation | Analyze the prepared samples and record the instrument response (e.g., peak area). Calculate the concentration of the analyte found using a pre-established calibration curve (y = mx + c) [46]. | The calibration curve must be generated independently from the accuracy samples. |
| 3. % Recovery Calculation | For each spiked sample, calculate the percent recovery using the formula above. | Report the individual recovery values, the mean recovery, and the %RSD for each concentration level. |
| 4. Acceptance Criteria | Compare the mean recovery against pre-defined acceptance criteria. For assay methods of drug substances and products, recovery is often expected to be within 98-102% [18]. | Criteria should be justified based on the method's intended use and the complexity of the matrix. |
Case Study: Accuracy Determination for a Related Substance
Consider a drug substance with a specification for an isomer impurity of NMT 1.0%. The sample concentration is 1.0 mg/mL (1000 mcg/mL). The target concentrations for accuracy are calculated as follows [46]:
- 50% Level: 1000 mcg/mL × (0.5/100) = 5 mcg/mL
- 100% Level: 1000 mcg/mL × (1.0/100) = 10 mcg/mL
- 150% Level: 1000 mcg/mL × (1.5/100) = 15 mcg/mL
After preparing and injecting these solutions, the concentration is calculated from the measured response (y) using the linear equation (x = (y - c)/m). The accuracy is then determined. For instance, a true concentration of 5.2 mcg/mL yielding a calculated concentration of 5.0 mcg/mL gives an accuracy of (5.0/5.2) × 100 = 96.2% [46]. The average deviation from 100% recovery should be within justified limits (e.g., less than 2%) [46].
The Scientist's Toolkit: Essential Reagents and Materials
The following table lists key reagents and materials critical for successfully executing precision and accuracy studies, along with their specific functions.
Table 3: Key Research Reagent Solutions for Validation Studies
| Reagent/Material | Function in Precision/Accuracy Studies |
|---|---|
| High-Purity Reference Standard | Serves as the accepted reference with a defined purity, essential for preparing known concentrations to evaluate accuracy and for constructing calibration curves. |
| Placebo Matrix | Mimics the composition of the drug product without the active ingredient. Used to prepare spiked samples for accuracy studies to assess matrix interference. |
| Certified Volumetric Glassware | Ensures precise and accurate measurement of volumes during sample and standard preparation, directly impacting the accuracy and precision of results. |
| Chromatographic Mobile Phase Components | High-purity solvents and buffers are crucial for maintaining stable chromatographic performance (retention time, peak shape), which affects the precision of analyte measurement. |
| System Suitability Test Solutions | A standardized solution used to verify that the chromatographic system is performing adequately before and during the analytical run, a prerequisite for reliable precision data. |
Statistical Analysis and Data Interpretation
Proper statistical analysis transforms raw data into meaningful evidence of method validity.
Analyzing Precision Data
Precision is most commonly expressed as the % Relative Standard Deviation (%RSD), also known as the coefficient of variation (CV). It is calculated as: %RSD = (Standard Deviation / Mean) × 100
A lower %RSD indicates higher precision. For assay methods, %RSD values below 2% are often expected for repeatability [18]. For intermediate precision, the results from different analysts or days are compared using statistical tests like the Student's t-test to determine if there is a significant difference between the means obtained under different conditions [9].
Interpreting Accuracy Data
Accuracy data is summarized by reporting the mean percent recovery at each concentration level. The overall accuracy of the method is confirmed if the mean recoveries at all levels fall within the pre-defined acceptance criteria (e.g., 98-102% for assay) [18]. The precision of the recovery values (as %RSD) should also be reported to demonstrate the consistency of the measurements.
Advanced Tool: Total Analytical Error (TAE) Analysis
For a more comprehensive assessment, the Total Analytical Error can be evaluated. A practical way to implement this is by calculating a β-expectation tolerance interval for the relative accuracy. If this interval, which accounts for both bias and variability, falls entirely within the acceptance limits for accuracy, the method is considered valid [47]. This approach provides a high degree of confidence that future results will meet quality standards.
The relationship between precision, accuracy, and the combined TAE is visualized in the following diagram.
Effectively addressing variability in precision and accuracy studies is a cornerstone of robust analytical method validation under ICH Q2(R1). By implementing a tiered approach to precision, employing rigorous spike/recovery experiments for accuracy, and utilizing advanced statistical concepts like Total Analytical Error, scientists can thoroughly characterize method performance. This systematic and scientific approach ensures the generation of reliable, high-quality data, which is fundamental to the development and control of safe and effective pharmaceutical products. As regulatory science evolves with the adoption of ICH Q2(R2), these principles of understanding and controlling variability remain more critical than ever.
Strategies for Verifying Compendial (e.g., USP) Methods
Within the framework of ICH Q2(R1) analytical method validation research, the verification of compendial methods represents a distinct and critical regulatory requirement. Unlike full method validation, which establishes the performance characteristics of a newly developed procedure, verification is the process that demonstrates a compendial method is suitable for use with a specific drug substance or product under actual conditions of use [48]. The United States Pharmacopeia (USP) General Chapter <1226> Verification of Compendial Procedures provides the primary guidance for this practice, requiring laboratories to demonstrate that the compendial method works as intended in their hands and with their specific sample matrix [49]. This process is fundamentally rooted in the principles of ICH Q2(R1), applying its core validation parameters to confirm method suitability without the need for complete re-validation.
The regulatory landscape for method verification is evolving. A proposed revision to USP <1225> aims to align it more closely with the modern lifecycle approach inspired by ICH Q14 and the updated ICH Q2(R2) [50] [51]. This shift emphasizes "fitness for purpose" as the overarching goal, focusing on whether the method generates reliable reportable results that support confident decision-making for batch release and compliance [51]. Consequently, verification strategies must now consider not just a one-time demonstration of suitability, but also the method's performance throughout its operational life.
Regulatory Foundation and Key Concepts
Distinguishing Between Validation, Verification, and Qualification
A clear understanding of terminology is essential for implementing the correct strategy. The terms validation, verification, and qualification are often used interchangeably, but they serve different purposes within the analytical lifecycle [48].
- Validation: A comprehensive process performed for non-compendial methods to establish that their performance characteristics meet the intended analytical applications. This is a full exercise conducted per ICH Q2(R1) or similar guidelines [40] [48].
- Verification: The specific process for compendial methods (e.g., USP, Ph. Eur.) to demonstrate they are suitable for testing a specific material under actual conditions of use in a given laboratory [49] [48]. It is not a re-validation, but a confirmation of suitability.
- Qualification: A term sometimes used in early development stages (e.g., Phase I clinical trials) where a full validation may not be possible or prudent because the manufacturing process is not yet locked. The term "validation" is often reserved for later-stage (Phase III and commercial) products [48].
The following table summarizes the core concepts and relevant guidelines governing compendial method verification.
Table 1: Regulatory Guidelines and Core Concepts for Compendial Method Verification
| Concept/Guideline | Description | Primary Application |
|---|---|---|
| USP <1226> | Provides guidance on verifying compendial procedures to confirm their suitability for use with a specific material under actual conditions of use [49]. | Verification of USP methods. |
| ICH Q2(R1) | Provides the foundational validation parameters (accuracy, precision, specificity, etc.) that are applied during verification [7] [40]. | Underpins the parameters assessed during verification. |
| Fitness for Purpose | An overarching principle that the verification strategy should ensure the method is fit for its intended use and capable of generating reliable reportable results [50] [51]. | Strategic goal for all verification activities. |
| Reportable Result | The final analytical result (e.g., mean of replicates) reported and used for quality decisions. Verification should focus on this output, not just individual measurements [51]. | The definitive output of the analytical procedure. |
The Role of ICH Q2(R1) Parameters in Verification
While verification is not as extensive as validation, it relies on the same core performance characteristics defined in ICH Q2(R1). The depth of assessment for each parameter is justified by the method's history of use and the specific sample matrix.
- Specificity/Mandatory Forced Degradation: Verification must confirm that the method is specific for the analyte in the presence of excipients and potential impurities. For stability-indicating methods, this includes forced degradation studies to demonstrate that the method can accurately measure the analyte and resolve it from degradation products [52].
- Accuracy and Precision: Accuracy (closeness to the true value) is typically assessed through spike recovery experiments, with acceptance criteria often set at 80-120% for impurities. Precision, encompassing repeatability, demonstrates the reliability of the method under normal operating conditions [7] [52].
- Linearity and Range: The linearity of the method (its ability to obtain results proportional to analyte concentration) should be verified over the specified range. For assay methods, a correlation coefficient (≥0.9999) is often expected, while ≥0.9995 may be acceptable for impurities [52].
Designing a Verification Protocol: Methodologies and Experiments
A robust verification protocol is a pre-approved plan that defines the experiments, acceptance criteria, and methodologies. The design should be risk-based, focusing on parameters most likely to be affected by the sample matrix.
Specificity and Selectivity Assessment
For compendial methods, the key specificity challenge is demonstrating that the sample matrix does not interfere with the detection and accurate quantification of the analyte.
- Experimental Protocol: Prepare and analyze a placebo/blank sample (containing all excipients but no API), the API alone, and the finished product. Compare the chromatograms or profiles to ensure the analyte peak is free from interference from placebo components at the retention time of the analyte [7].
- For Stability-Indicating Methods: Conduct forced degradation studies on the drug product under stress conditions (e.g., acid, base, oxidation, thermal, photolytic). The method should effectively separate degradation products from the main analyte, demonstrating its ability to accurately measure stability [52]. For advanced techniques like LC-MS/MS, specificity assessments may also need to rule out cross-signal contributions between monitored compounds, which can impact accuracy at ultra-trace levels, such as in nitrosamine testing [53].
Accuracy (Recovery) Studies
Accuracy verification confirms that the method provides a truthful result for the specific product being tested.
- Experimental Protocol: Spike the API into the placebo matrix at multiple concentration levels (e.g., 80%, 100%, 120% of the target concentration) in triplicate. Process and analyze these samples according to the compendial method. Calculate the percentage recovery for each level and the overall average recovery.
- Acceptance Criteria: Acceptance criteria are based on ICH Q2(R1) principles and the method's purpose. For an assay, a mean recovery of 98.0-102.0% is typical. For impurities, a wider range of 80-120% is often applied [52].
Precision Evaluation
Precision verification demonstrates the method's reliability under normal operating conditions. The focus is typically on repeatability.
- Experimental Protocol: Prepare and analyze multiple homogeneous samples (e.g., six preparations at 100% of the test concentration) under the same operating conditions, by the same analyst, using the same equipment within a short timescale. The %RSD (Relative Standard Deviation) of the results is calculated.
- Acceptance Criteria: Acceptance criteria for repeatability are typically stringent. For an assay of a drug product, an RSD of ≤1.0% is commonly expected, though the specific compendial method may provide guidance [52].
Table 2: Summary of Key Verification Experiments and Typical Acceptance Criteria
| Performance Characteristic | Recommended Experiment | Typical Acceptance Criteria (Examples) |
|---|---|---|
| Specificity | Analysis of placebo, API, and product; forced degradation. | No interference from placebo or degradation products; peak purity index ≥0.99 [52]. |
| Accuracy | Spike recovery at 3 levels in triplicate (80%, 100%, 120%). | Assay: Mean recovery 98.0-102.0%; Impurities: 80-120% [7] [52]. |
| Precision (Repeatability) | Six preparations at 100% test concentration. | Assay: RSD ≤1.0% [52]. |
| Linearity | Minimum of 5 concentrations across the specified range. | Assay: Correlation coefficient (r) ≥0.999 [52]. |
| Robustness | Deliberate, small variations in method parameters (e.g., pH, temperature, flow rate). | System suitability criteria are met despite variations; no significant impact on reportable result. |
The Verification Workflow
The following diagram illustrates the logical workflow for planning and executing a compendial method verification, from initial assessment to final documentation.
Verification Workflow
The Scientist's Toolkit: Essential Materials and Reagents
Successful execution of a verification protocol depends on the use of well-characterized materials and reagents.
Table 3: Key Research Reagent Solutions for Verification
| Item | Function in Verification | Critical Considerations |
|---|---|---|
| Well-Characterized Reference Standard | Serves as the benchmark for identity, potency, and purity for preparing known concentrations for accuracy, linearity, and precision studies. | Purity and traceability are paramount. Must be obtained from a certified source (e.g., USP). |
| Placebo/Blank Matrix | Used in specificity experiments to demonstrate no interference from excipients and in accuracy studies for spike recovery. | Should be representative of the final drug product formulation, minus the Active Pharmaceutical Ingredient (API). |
| Forced Degradation Reagents | Used to intentionally degrade the sample to validate the specificity of stability-indicating methods. | Includes acid (e.g., HCl), base (e.g., NaOH), oxidant (e.g., H₂O₂), and exposure to heat and light [52]. |
| High-Purity Solvents and Mobile Phase Components | Used to prepare mobile phases, diluents, and solutions as per the compendial method. | Purity and grade must meet compendial specifications. Variations can impact robustness and system suitability. |
Verifying compendial methods is a regulatory mandate that ensures the reliability of analytical data used to make critical decisions about product quality. By applying the principles of ICH Q2(R1) within a risk-based framework, scientists can design efficient and effective verification protocols. The evolving regulatory landscape, with its increased emphasis on the analytical procedure lifecycle and fitness for purpose, encourages a more holistic view of verification. This view sees it not as a one-time checkbox activity, but as the initial stage in an ongoing commitment to ensuring that analytical methods remain capable of generating reliable reportable results throughout their use. A well-executed verification strategy, therefore, forms the foundation of data integrity and product quality in pharmaceutical development and manufacturing.
Developing a Comprehensive Validation Protocol and Acceptance Criteria
The International Council for Harmonisation (ICH) Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," provides the foundational international framework for validating analytical methods in the pharmaceutical industry. This guideline harmonizes the requirements for demonstrating that an analytical procedure is suitable for its intended purpose, ensuring the reliability, accuracy, and consistency of data used to assess the quality, safety, and efficacy of drug substances and products [3] [11]. Originally established in 1994 and later unified in 2005, ICH Q2(R1) combines the principles from the earlier Q2A (text) and Q2B (methodology) documents [5] [3]. Regulatory authorities across the globe, including the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), have adopted this guideline, making compliance mandatory for market authorization applications [5] [27].
The validation process defined by ICH Q2(R1) is not merely a regulatory formality but a critical scientific exercise that confirms an analytical method consistently produces reliable results when applied to the analysis of pharmaceutical compounds. The guideline systematically outlines the key validation parameters that must be evaluated, the experimental methodologies required, and the acceptance criteria that must be met based on the type of analytical procedure being validated—whether for identification, assay, impurity testing, or other specific applications [18] [12]. By providing this structured approach, ICH Q2(R1) ensures that analytical methods can reliably measure the identity, potency, purity, and quality of drug products throughout their lifecycle.
It is important to note that while ICH Q2(R1) remains the current standard for this discussion, the ICH has recently finalized a revised version, ICH Q2(R2), which modernizes the framework to accommodate advanced analytical technologies and aligns with the new ICH Q14 guideline on analytical procedure development [12] [54] [6]. These updates emphasize a science- and risk-based approach, along with analytical procedure lifecycle management. However, the core principles established in ICH Q2(R1) continue to underpin the revised guidance and remain essential knowledge for any professional in pharmaceutical development [6] [11].
Core Validation Parameters and Acceptance Criteria
The ICH Q2(R1) guideline defines a set of fundamental validation characteristics that must be assessed to demonstrate an analytical procedure is fit-for-purpose. The specific parameters required depend on the type of analytical procedure (e.g., identification, assay, impurity testing). The table below summarizes these core parameters, their definitions, and typical acceptance criteria for quantitative assays.
Table 1: Core Validation Parameters and Acceptance Criteria per ICH Q2(R1)
| Validation Parameter | Definition | Typical Acceptance Criteria for Assays |
|---|---|---|
| Specificity | The ability to assess the analyte unequivocally in the presence of components that may be expected to be present, such as impurities, degradation products, and matrix components [18] [12]. | The method should successfully discriminate between the analyte and all potential interferents, such as degradation products, impurities, and excipients [18]. |
| Accuracy | The closeness of agreement between the value which is accepted as a conventional true value or an accepted reference value and the value found [18] [12]. | Expressed as percent recovery. Typically requires a minimum of 9 determinations across a minimum of 3 concentration levels covering the specified range [18]. |
| Precision | The closeness of agreement between a series of measurements obtained from multiple sampling of the same homogeneous sample under the prescribed conditions [18]. | Repeatability (Intra-assay): RSD typically < 2% for assay methods, using a minimum of 6 determinations at 100% of the test concentration.Intermediate Precision: Consistency of results within a laboratory (different days, analysts, equipment) [18] [12]. |
| Linearity | The ability of the method to obtain test results that are directly proportional to the concentration of the analyte in a given range [18] [11]. | A correlation coefficient (r) of at least 0.995 is generally expected for the linear regression curve [18]. |
| Range | The interval between the upper and lower concentrations of analyte for which the method has demonstrated suitable levels of linearity, accuracy, and precision [18] [54]. | For assay of a drug product, typically 80-120% of the test concentration [18] [54]. |
| Detection Limit (LOD) | The lowest amount of analyte in a sample that can be detected, but not necessarily quantitated, under the stated experimental conditions [18]. | Typically based on a signal-to-noise ratio of 3:1 [18]. |
| Quantitation Limit (LOQ) | The lowest amount of analyte in a sample that can be quantitatively determined with suitable precision and accuracy under the stated experimental conditions [18]. | Typically based on a signal-to-noise ratio of 10:1. At the LOQ, the method should demonstrate an acceptable accuracy and precision (e.g., RSD < 5%) [18]. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters (e.g., pH, mobile phase composition, temperature) [18] [12]. | The method should maintain acceptable performance when operational parameters are deliberately varied. Evidence that the method is reliable during normal usage [18] [54]. |
For impurity methods, the range is expected to extend from the quantitation limit to a level above the specified impurity limit (e.g., 120% of the specification) [54]. The validation protocol must pre-define all acceptance criteria based on the procedure's intended use and the stage of product development, with appropriate scientific justification [12] [11].
Experimental Protocols for Key Validation Tests
Specificity
Objective: To demonstrate that the method can unequivocally distinguish and quantify the target analyte from other components, proving a lack of interference.
Methodology:
- Analyze a blank sample: The sample matrix (e.g., placebo or sample solvent) should show no interference at the retention time or spectral location of the analyte.
- Analyze samples spiked with potential interferents: These include known impurities, degradation products (generated from forced degradation studies), and excipients. The chromatogram or spectrum should show baseline separation between the analyte and all interferents.
- For stability-indicating methods: Perform forced degradation studies on the drug substance or product under various stress conditions (e.g., acid/base hydrolysis, oxidation, thermal, and photolytic stress). The method must be able to separate the analyte peak from all degradation peaks, demonstrating its ability to accurately measure the analyte in the presence of degradation products [18] [54].
Accuracy
Objective: To determine the closeness of the measured value to the true value of the analyte.
Methodology:
- Preparation: Prepare a minimum of 9 determinations over at least 3 concentration levels (e.g., 80%, 100%, 120%) covering the entire specified range. Each determination involves analyzing a sample of known concentration, typically prepared by spiking the analyte into a placebo or blank matrix.
- Analysis: Analyze the samples using the validated method.
- Calculation: Calculate the percent recovery for each determination using the formula:
(Measured Concentration / Known Concentration) * 100. Alternatively, the accuracy can be expressed as the difference (bias) between the mean value and the accepted true value. - Reporting: The mean recovery and the relative standard deviation (RSD) of the recovery values are reported and assessed against pre-defined acceptance criteria [18] [12].
Precision
Precision is evaluated at two levels: repeatability and intermediate precision.
A. Repeatability (Intra-assay Precision) Objective: To assess the precision under the same operating conditions over a short interval of time. Methodology: Perform a minimum of 6 determinations at 100% of the test concentration. Calculate the Relative Standard Deviation (RSD or %CV) of the results. The RSD should typically be less than 2% for assay methods [18] [12].
B. Intermediate Precision Objective: To evaluate the impact of random variations within the same laboratory, such as different analysts, different days, and different equipment. Methodology: The same homogeneous sample is analyzed multiple times using the same method but with deliberate changes in operational factors. The results from both sets (e.g., Analyst 1 on Day 1 vs. Analyst 2 on Day 2) are compared statistically. The RSD for the combined data set is calculated and evaluated against pre-defined criteria [18] [12].
Linearity and Range
Objective: To demonstrate a proportional relationship between the analyte concentration and the instrumental response, and to define the concentration range over which this relationship holds with acceptable accuracy, precision, and linearity.
Methodology:
- Preparation: Prepare a minimum of 5 standard solutions at different concentrations spanning the intended range (e.g., 50%, 75%, 100%, 125%, 150% for impurity methods, or 80%, 90%, 100%, 110%, 120% for assay methods).
- Analysis: Analyze each standard solution.
- Data Analysis: Plot the instrumental response (e.g., peak area) against the concentration. Perform linear regression analysis on the data to calculate the correlation coefficient (r), slope, and y-intercept.
- Acceptance: The correlation coefficient is typically required to be ≥ 0.995. The range is confirmed as the interval where linearity, accuracy, and precision all meet the acceptance criteria [18] [54].
Robustness
Objective: To evaluate the method's reliability when subjected to small, deliberate variations in method parameters.
Methodology:
- Identification of Factors: Identify critical method parameters that could vary during routine use (e.g., mobile phase pH ± 0.2 units, flow rate ± 10%, column temperature ± 5°C, different columns from the same supplier).
- Experimental Design: Use a structured experimental design (e.g., a Plackett-Burman or factorial design) to systematically vary these parameters.
- Analysis: Analyze a standard or sample under each set of varied conditions.
- Evaluation: Monitor the impact on critical performance attributes such as resolution, tailing factor, and efficiency. The method is considered robust if these attributes remain within specified acceptance criteria despite the variations [18].
The Validation Workflow and System Suitability
The overall process of method validation follows a logical sequence, from initial planning to final reporting, as illustrated in the workflow below.
Diagram 1: Analytical Method Validation Workflow
The Role of System Suitability Testing
While not a validation parameter per se, system suitability testing is a critical ongoing verification step that ensures the analytical system is functioning correctly at the time of analysis. These tests are based on the concept that the equipment, electronics, analytical operations, and samples constitute an integral system that can be evaluated for performance [18].
System suitability tests are performed before and during the analysis of validation samples and are defined in the method procedure. They involve injecting a standard or a standard preparation a specified number of times and calculating key parameters against pre-defined acceptance criteria. The following table details the essential reagents and materials required for a typical HPLC method validation, which directly supports the execution of these tests and the overall validation.
Table 2: Essential Research Reagent Solutions for HPLC Method Validation
| Item | Function |
|---|---|
| Reference Standard | A highly characterized substance of known purity used as the benchmark for quantifying the analyte and establishing the calibration curve [54]. |
| Mobile Phase | The solvent mixture that moves the analyte through the chromatographic column. Its composition, pH, and buffer strength are critical for separation and retention time [18]. |
| Chromatographic Column | The stationary phase that separates the components of a mixture based on their chemical interactions. Column selectivity and efficiency are vital for specificity [18]. |
| System Suitability Test Solution | A preparation containing the analyte and key interferents used to verify that the chromatographic system has adequate resolution, efficiency, and precision before the run [18]. |
The relationship between method validation, system suitability, and the control strategy is foundational to a successful analytical procedure, as shown below.
Diagram 2: Relationship between Validation, Suitability, and Control
The ICH Q2(R1) guideline provides a robust, harmonized framework for analytical method validation that is critical for ensuring the quality and safety of pharmaceutical products. A comprehensive validation protocol, built upon the core parameters of specificity, accuracy, precision, linearity, range, LOD, LOQ, and robustness, generates defensible scientific evidence that an analytical procedure is fit for its intended purpose. By meticulously designing experiments, pre-defining scientifically justified acceptance criteria, and integrating system suitability controls, researchers and drug development professionals can build a foundation of data integrity and quality that meets rigorous global regulatory standards. As the industry evolves, the principles of ICH Q2(R1) continue to serve as the cornerstone for analytical quality, even as they are enhanced by the modernized, lifecycle approaches of ICH Q2(R2) and Q14.
Maintaining Data Integrity and Documentation for Regulatory Scrutiny
The ICH Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," provides the foundational framework for validating analytical methods in the pharmaceutical industry. This harmonized standard, adopted by regulatory bodies including the U.S. Food and Drug Administration (FDA), outlines the essential validation parameters required to demonstrate that an analytical procedure is suitable for its intended purpose [5] [3] [11]. Originally established as two separate guidelines (Q2A and Q2B), they were unified into Q2(R1) in November 2005, and the FDA issued this as a final Level 2 guidance in September 2021 [5].
Within this framework, data integrity is paramount. It ensures that all data generated during method validation and routine analysis are complete, consistent, and accurate, thereby forming the bedrock of reliable scientific evidence for regulatory submissions [55] [10]. Proper documentation provides the auditable trail that regulatory agencies scrutinize to verify that a method consistently produces results that can be trusted to assess the identity, potency, quality, and purity of drug substances and products [11] [10]. Adherence to ICH Q2(R1) is not merely a regulatory formality but a critical component in ensuring patient safety and product efficacy [12].
Core Validation Parameters of ICH Q2(R1)
The ICH Q2(R1) guideline defines a set of key validation characteristics that must be evaluated based on the type of analytical procedure. The following table summarizes these core parameters, their definitions, and typical methodological approaches for assessment [18] [11] [55].
Table 1: Core Validation Parameters as per ICH Q2(R1)
| Parameter | Definition | Typical Experimental Methodology |
|---|---|---|
| Specificity | The ability to assess the analyte unequivocally in the presence of components that may be expected to be present [18]. | Analysis of samples with and without potential interferents (degradation products, impurities, matrix components) to demonstrate separation and lack of interference [18]. |
| Accuracy | The closeness of agreement between the value which is accepted as a true value or an accepted reference value and the value found [18] [55]. | Comparison of results to a known reference standard; recovery studies of known amounts of analyte spiked into the matrix across the specified range (at least 9 determinations across 3 concentration levels) [18] [55]. |
| Precision | The degree of agreement among individual test results when the procedure is applied repeatedly to multiple samplings of a homogeneous sample [55]. | Repeatability: Multiple measurements under identical conditions.Intermediate Precision: Variations within the same lab (different days, analysts, equipment).Expressed as % Relative Standard Deviation (%RSD), with ≤ 2% often acceptable for assays [18] [11]. |
| Linearity | The ability of the method to obtain test results directly proportional to the concentration of the analyte within a given range [11]. | Analysis of at least 5 concentrations across the specified range. Demonstrated via correlation coefficient (r), typically requiring at least 0.995, and evaluation of the y-intercept and slope of the regression line [18]. |
| Range | The interval between the upper and lower concentrations of analyte for which linearity, accuracy, and precision have been demonstrated [11]. | Defined based on the intended application of the method (e.g., 80-120% of test concentration for assay, from reporting threshold to 120% of specification for impurities) [18]. |
| Detection Limit (LOD) | The lowest amount of analyte in a sample that can be detected, but not necessarily quantified [11]. | Signal-to-noise ratio (typically 3:1) or based on the standard deviation of the response and the slope of the calibration curve (e.g., 3.3σ/slope) [18]. |
| Quantitation Limit (LOQ) | The lowest amount of analyte in a sample that can be quantitatively determined with suitable precision and accuracy [11]. | Signal-to-noise ratio (typically 10:1) or based on the standard deviation of the response and the slope of the calibration curve (e.g., 10σ/slope) [18]. |
| Robustness | A measure of the method's capacity to remain unaffected by small, deliberate variations in method parameters [18] [11]. | Deliberate variations in operational parameters (e.g., pH, mobile phase composition, temperature, flow rate) to evaluate the method's reliability [18]. |
Experimental Protocols for Key Validation Experiments
Protocol for Demonstrating Accuracy and Precision
The validation of accuracy and precision is often integrated into a single experimental study to provide a comprehensive view of the method's reliability [54].
- Experimental Design:
- Sample Analysis:
- Analyze all samples using the validated analytical procedure. For intermediate precision, repeat the study on a different day, with a different analyst, or using different equipment, as applicable [18].
- Data Analysis:
- Accuracy: Calculate the percent recovery for each sample by comparing the measured value to the known theoretical value. The mean recovery at each level should be within predefined acceptance criteria [18] [54].
- Precision: Calculate the % Relative Standard Deviation (%RSD) for the replicate measurements at each concentration level and across the entire study. For assay methods, an RSD of ≤ 2% is commonly accepted for precision [18].
Protocol for Specificity and Robustness
Specificity ensures the method is measuring only the intended analyte [18].
- Methodology: Inject and analyze the following solutions individually:
- Blank: The sample matrix without the analyte.
- Placebo/Matrix: Formulation components or sample matrix without the analyte.
- Standard: The analyte of interest.
- Stressed/Spliced Sample: Samples subjected to stress conditions (e.g., heat, light, acid/base) to generate degradants, or samples spiked with potential interferents like known impurities [18] [54].
- Acceptance Criteria: The chromatogram or signal for the blank and placebo should show no interference at the retention time or location of the analyte. The analyte peak should be pure and baseline resolved from any degradation products or impurities [18].
Robustness evaluates the method's resilience to parameter variations [18].
- Methodology: Deliberately introduce small, intentional changes to method parameters one at a time (e.g., mobile phase pH ± 0.2 units, flow rate ± 10%, column temperature ± 2°C). Analyze a standard and a sample preparation under each modified condition [18].
- Acceptance Criteria: System suitability criteria (e.g., resolution, tailing factor, %RSD of replicates) should be met under all varied conditions, demonstrating that the method performance remains acceptable [18].
The Method Validation Workflow
The following diagram illustrates the logical workflow for a successful analytical method validation, from initial planning through to ongoing monitoring, integrating both ICH Q2(R1) parameters and data integrity principles.
The Scientist's Toolkit: Essential Research Reagent Solutions
A successful method validation relies on high-quality, well-characterized materials. The following table details key reagents and their critical functions in ensuring reliable and compliant analytical results.
Table 2: Essential Reagents and Materials for Method Validation
| Item | Critical Function in Validation |
|---|---|
| Reference Standards | Certified, high-purity materials used to prepare known concentrations for accuracy, linearity, and precision studies. They provide the benchmark for all quantitative measurements [55]. |
| System Suitability Test (SST) Solutions | A specific mixture of analytes and/or impurities used to verify that the chromatographic or analytical system is performing adequately before and during sample analysis [18]. |
| Stressed/Spliced Samples | Samples intentionally degraded (e.g., by heat, light, acid/base) or spiked with known impurities to critically challenge and demonstrate the method's specificity [18] [54]. |
| High-Purity Solvents and Reagents | Essential for minimizing background interference and noise, which is crucial for accurately determining Limits of Detection (LOD) and Quantitation (LOQ) and for achieving the required specificity [10]. |
| Characterized Columns/Consumables | Using specified and well-characterized chromatographic columns, filters, and vials is vital for demonstrating the robustness and intermediate precision of the method [18]. |
Adherence to the ICH Q2(R1) guideline, coupled with an unwavering commitment to data integrity, is non-negotiable for navigating regulatory scrutiny. A method validation is only as strong as the data that supports it. This requires a science-based approach, meticulous execution of experimental protocols, and transparent documentation of all results—not just those that meet expectations [10]. By integrating these principles into a comprehensive lifecycle management strategy—from initial development and validation through ongoing monitoring via system suitability tests—organizations can ensure their analytical methods remain robust, reliable, and fully compliant, thereby safeguarding product quality and patient safety [6] [11].
ICH Q2(R1) in Context: Comparison with Q2(R2) and Future Directions
The Evolution from a One-Time Event to a Lifecycle Approach
The framework for validating analytical procedures in the pharmaceutical industry has undergone a fundamental transformation, moving from a static, one-time event to a dynamic, holistic lifecycle approach. This evolution represents a significant shift from what has been characterized as "compliance theater"—a performance of rigor that may not reflect actual method capability—toward a genuine, science-based system that ensures ongoing analytical reliability [51]. The traditional model, primarily governed by ICH Q2(R1), treated validation as a discrete activity with a fixed set of parameters to be demonstrated before method deployment. In contrast, the modern paradigm, encapsulated in emerging guidelines including ICH Q2(R2), ICH Q14, and USP <1220>, reconceptualizes validation as a continuous process embedded throughout the analytical procedure's existence [56] [51].
This shift aligns with broader trends in pharmaceutical quality systems. The FDA's 2011 process validation guidelines redefined validation as "the collection and evaluation of data, from the process design stage throughout production, which establishes scientific evidence that a process is capable of consistently delivering quality products," moving away from the 1987 definition that focused on "establishing documented evidence" at a single point [56]. Similarly, the lifecycle approach to analytical procedures emphasizes understanding, control, and ongoing verification over mere documentary proof [56]. This article explores this critical evolution, framing it within the context of ICH Q2(R1) analytical method validation guide research, and provides technical guidance for its implementation.
The Traditional Foundation: ICH Q2(R1) and Its Limitations
The ICH Q2(R1) guideline, titled "Validation of Analytical Procedures: Text and Methodology," served as the global regulatory standard for nearly a quarter-century, with its origins in the even earlier USP General Chapter <1225> [56]. This guideline provided a harmonized framework for demonstrating that an analytical procedure was suitable for its intended purpose through the assessment of a standardized set of performance characteristics. The traditional approach prescribed specific validation parameters based on the type of analytical procedure (e.g., identification, testing for impurities, assay), creating a category-based validation system [56].
However, experience over decades revealed significant limitations in this model:
- Focus on Discrete Event: ICH Q2(R1) treated validation as a one-time activity conducted prior to method deployment, with no formal requirements for ongoing monitoring of method performance during routine use [56] [51].
- Inadequate for Modern Techniques: The guideline was originally developed primarily for chromatographic procedures, particularly HPLC, and provided inadequate guidance for newer analytical technologies such as Near-Infrared (NIR) and Raman spectroscopy, especially those utilizing multivariate models [57] [56].
- Ignored Procedure Development: The guideline focused solely on validation without addressing the critical method development phase, potentially allowing poorly developed methods with inherent variability to be "validated" and subsequently generate out-of-specification (OOS) results during routine use [57].
- Terminology and Conceptual Gaps: The term "specificity" was often used to describe what was functionally "selectivity," and the guideline confused the relationship between the reportable result and the analytical response function [56].
These limitations created a situation where methods could pass validation yet still fail under routine operating conditions, contributing to regulatory observations and OOS results [57]. The fundamental shortcoming was the "comfortable fiction that validation is a discrete event rather than an ongoing commitment to analytical quality" [51].
The Lifecycle Approach: Framework and Regulatory Evolution
Core Principles and Regulatory Drivers
The lifecycle approach to analytical procedures is founded on the principle that ensuring method fitness for purpose requires continuous attention from development through retirement, not merely a one-time demonstration of performance [51]. This paradigm shift has been driven by multiple regulatory and pharmacopeial developments:
- USP General Chapter <1220>: The official introduction of "The Analytical Procedure Lifecycle" in May 2022 provided a structured three-stage framework (Procedure Design and Development, Procedure Performance Qualification, and Procedure Performance Verification) and marked a fundamental change in how analytical procedures are managed [57] [56].
- ICH Q14 "Analytical Procedure Development": This new guideline complements the revised ICH Q2(R2) by providing a structured, science- and risk-based approach to analytical procedure development, emphasizing prior knowledge, robust method design, and the Analytical Target Profile (ATP) [12].
- ICH Q2(R2) "Validation of Analytical Procedures": The revision of the traditional Q2(R1) guideline expands its scope to cover modern analytical technologies and aligns with the lifecycle approach, though it has been criticized for not fully integrating development and ongoing verification [57] [12].
- Revised USP <1225>: The proposed revision of "Validation of Compendial Procedures" incorporates lifecycle concepts such as "reportable result," "fitness for purpose," and "replication strategy," creating alignment with ICH Q2(R2) and Q14 [51].
The following diagram illustrates the core structure of the analytical procedure lifecycle management framework:
The Three-Stage Lifecycle Model
The Analytical Procedure Lifecycle, as defined in USP <1220>, consists of three interconnected stages:
Stage 1: Procedure Design and Development: This foundational stage moves beyond traditional method development by beginning with an Analytical Target Profile (ATP) - a predefined objective that explicitly states the required performance characteristics of the reportable result [57] [12]. The ATP defines "fitness for purpose" through measurable performance criteria such as precision, accuracy, and range, tailored to the method's intended use [51]. Development activities then focus on understanding critical method parameters through systematic studies and risk assessment, establishing a control strategy and design space within which the method will perform robustly [57].
Stage 2: Procedure Performance Qualification: This stage corresponds to traditional method validation but is conducted within the context of the understanding gained during Stage 1. Rather than mechanically testing all possible validation parameters, qualification focuses on demonstrating that the procedure performs as intended when operated within the established design space [57] [56]. The experiments evaluate the procedure's ability to generate reportable results that meet the ATP criteria [51].
Stage 3: Procedure Performance Verification: This ongoing stage represents the most significant departure from the traditional model. It involves continuous monitoring of the procedure's performance during routine use to ensure it remains in a state of control [57]. Trends are analyzed, and any changes within the defined design space can be made without formal revalidation [57]. This stage potentially continues for decades, throughout the method's operational lifetime, and provides real-world evidence of continued fitness for purpose [51].
Key Conceptual Innovations in the Lifecycle Approach
The Analytical Target Profile (ATP) and Reportable Result
The Analytical Target Profile represents a fundamental shift in how analytical requirements are defined. The ATP is a prospective summary of the required performance characteristics of the reportable result—the actual analytical output used for quality decisions [51]. It defines the criteria for quality throughout the procedure's lifecycle, moving beyond instrument performance to focus on the final result that impacts product quality decisions [51].
The "reportable result" concept forces validation to address what will actually be reported and used, not just individual measurements [51]. For instance, if a standard operating procedure specifies reporting the mean of duplicate sample preparations, validation must demonstrate the precision and accuracy of that mean value, not just the repeatability of individual injections [51].
Enhanced Method Development and Understanding
ICH Q14 encourages both minimal and enhanced approaches to analytical procedure development, with the enhanced approach emphasizing greater understanding and control [12]. This includes:
- Systematic Experimentation: Using structured studies, including Design of Experiments (DoE), to understand method parameters and their interactions [57].
- Risk-Based Approaches: Applying quality risk management principles to focus development and control efforts on critical parameters [56].
- Design Space Definition: Establishing the multidimensional combination of method parameters within which the procedure will perform robustly [57].
Knowledge Management and Continued Performance Verification
The lifecycle approach treats knowledge as a cumulative resource that informs all stages. Data generated during development, platform knowledge from similar methods, and experience from routine use all contribute to maintaining procedure fitness for purpose [51]. Continued performance verification uses statistical monitoring of system suitability tests and quality control sample results to provide ongoing assurance that the method remains in a state of control [57] [56].
The following table summarizes the core differences between the traditional and lifecycle approaches to analytical validation:
Table 1: Comparison of Traditional versus Lifecycle Validation Approaches
| Aspect | Traditional Approach (ICH Q2(R1)) | Lifecycle Approach (ICH Q2(R2)/Q14, USP <1220>) |
|---|---|---|
| Core Philosophy | Validation as a one-time event [51] | Validation as a continuous process throughout the procedure's life [56] [51] |
| Starting Point | Method technique or compendial method [56] | Analytical Target Profile (ATP) defining required quality of reportable result [57] [51] |
| Development Focus | Often empirical, with limited understanding of critical parameters [57] | Systematic, science- and risk-based, with established design space [12] [56] |
| Validation Strategy | Fixed validation parameters based on method category [56] | Risk-based strategy tailored to method purpose and criticality [51] |
| Post-Validation | Revalidation only when changes occur [56] | Ongoing performance verification with continuous monitoring [57] |
| Knowledge Management | Limited connection between development, validation, and routine use [51] | Cumulative knowledge throughout lifecycle informs all stages [51] |
| Regulatory Foundation | Primarily ICH Q2(R1) [56] | ICH Q2(R2), ICH Q14, USP <1220>, revised USP <1225> [12] [51] |
Implementation Framework: Experimental Protocols and Technical Requirements
Establishing the Analytical Target Profile (ATP)
The foundation of the lifecycle approach is a well-defined ATP. The protocol for establishing an ATP should include:
- Define Measurand: Precisely identify the analyte or property being measured.
- Specify Performance Requirements: Define required characteristics for the reportable result, including accuracy, precision, range, and any specific regulatory requirements.
- Link to Purpose: Explicitly connect performance requirements to the method's intended use (e.g., release testing, stability studies).
- Document Justification: Provide scientific rationale for all established criteria.
Procedure Design and Development Studies
The enhanced approach to procedure development should include systematic studies to understand method behavior:
- Risk Assessment: Conduct initial risk identification to determine potential critical method parameters.
- Experimental Design: Employ structured designs (e.g., factorial designs, response surface methodologies) to study parameter effects and interactions.
- Design Space Characterization: Define the multidimensional region where method performance meets ATP requirements.
- Control Strategy Development: Establish controls for critical method parameters to ensure robust operation.
Procedure Performance Qualification
The qualification protocol should be tailored to the ATP requirements and include:
- Accuracy and Precision: Combined evaluation using statistical intervals that account for both bias and variability simultaneously [51].
- Replication Strategy: Employ the same replication scheme that will be used for routine reportable results [51].
- Specificity/Selectivity: Demonstration of reliable measurement in the presence of expected sample matrix components.
- Range Determination: Verification that the procedure provides suitable precision, accuracy, and linearity across the specified range of the ATP.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of the lifecycle approach requires specific technical materials and reagents. The following table details key research reagent solutions and their functions in method development and validation:
Table 2: Essential Research Reagent Solutions for Analytical Lifecycle Management
| Reagent/Material | Function in Lifecycle Approach | Application Examples |
|---|---|---|
| Reference Standards | Provide benchmark for accuracy determination and system suitability testing [12] | API potency assays, impurity identification and quantification |
| Placebo/Blank Matrix | Evaluate specificity/selectivity by detecting interference from sample components [12] | Formulation analysis, biomarker assays in biological matrices |
| Forced Degradation Samples | Demonstrate stability-indicating capability and method specificity [12] | Validation of stability-indicating methods for APIs and products |
| System Suitability Test Solutions | Verify chromatographic system performance at time of analysis [12] | HPLC/UHPLC methods for potency and related substances |
| Quality Control Samples | Monitor method performance during validation and routine use [57] | Ongoing performance verification in Stage 3 of lifecycle |
Analytical Control Strategy and Data Governance
The lifecycle approach necessitates a robust analytical control strategy that extends beyond the traditional system suitability test. This strategy includes:
- Parameter Ranges: Defined operating ranges for critical method parameters based on development studies [57].
- System Suitability Tests: Scientifically justified tests that truly demonstrate the system's fitness for the intended analysis [51].
- Ongoing Monitoring Plan: Statistical tracking of quality control sample results and system suitability data to detect performance drift [57].
Data governance is integral to the lifecycle approach, ensuring that data—irrespective of format—are "recorded, processed, retained and used to ensure complete, consistent and accurate records throughout the data lifecycle" [56]. This is particularly critical given that "many of the large majority of data integrity breaches are more attributable to poor or bad practices and lack of adequate analytical controls than deliberate falsification" [56].
The following workflow diagram illustrates the continuous knowledge management process in the analytical procedure lifecycle:
The evolution from a one-time validation event to a holistic lifecycle approach represents a fundamental maturation in how the pharmaceutical industry ensures analytical quality. This shift, embodied in the emerging framework of ICH Q2(R2), ICH Q14, USP <1220>, and the revised USP <1225>, moves beyond compliance documentation toward genuine scientific understanding and control of analytical procedures [12] [51].
The lifecycle model offers a more scientifically rigorous and potentially more efficient path to ensuring ongoing analytical reliability. However, it demands greater expertise, particularly in statistical analysis and experimental design, and requires a cultural shift from treating validation as a regulatory hurdle to embracing it as an integral part of analytical quality [51]. For researchers, scientists, and drug development professionals, understanding and implementing this evolved approach is essential for developing robust, reliable analytical procedures that can consistently generate quality data throughout a product's lifecycle.
The framework encourages "falsifiable quality systems"—systems that make testable predictions about method performance that can be proven wrong through empirical observation [51]. This scientific rigor ultimately strengthens the foundation of pharmaceutical quality and ensures that analytical procedures remain truly fit for purpose throughout their operational lifetime.
Key Differences Between ICH Q2(R1) and the Modernized Q2(R2)
The International Council for Harmonisation (ICH) Q2(R1) guideline, established in 2005, has long served as the global benchmark for validating analytical procedures in the pharmaceutical industry, ensuring the reliability, accuracy, and reproducibility of methods used in drug testing [58]. The recent adoption of ICH Q2(R2) in 2023, effective from June 2024, marks a significant evolution in the regulatory landscape [59] [60]. Developed in parallel with the new ICH Q14 on analytical procedure development, Q2(R2) introduces a modernized, lifecycle approach to method validation, emphasizing risk-based principles, enhanced robustness, and integration with Analytical Quality by Design (AQbD) concepts [58] [6] [61]. This whitepaper provides an in-depth technical comparison of these two pivotal guidelines, detailing the key differences, their practical implications, and strategic recommendations for successful implementation in pharmaceutical research and development.
Background and Context of ICH Q2 Guidelines
The original ICH Q2 guideline was first finalized in 1994 (Q2A) and expanded in 1996 (Q2B), with these documents later combined in November 2005 into ICH Q2(R1), titled "Validation of Analytical Procedures: Text and Methodology" [60]. For nearly two decades, Q2(R1) provided the foundational framework for validating analytical methods, particularly for drug substances and products, outlining essential performance characteristics such as specificity, accuracy, precision, and linearity [58].
However, with significant advancements in analytical technologies and the increasing complexity of biopharmaceutical products, limitations of Q2(R1) became evident. It lacked guidance on integrating validation with method development, offered minimal focus on lifecycle management, and did not fully embrace risk-based approaches or modern tools like AQbD [58] [61]. These gaps prompted the need for revision, leading to the endorsement of Q2(R2) in March 2022 for public consultation and its final adoption in November 2023 [60]. The updated guideline represents a complete revision to include more recent applications of analytical procedures and to align content with ICH Q14 [60].
Core Conceptual Shifts: From Q2(R1) to Q2(R2)
The most fundamental shift introduced in Q2(R2) is the adoption of a lifecycle management concept for analytical procedures [58] [6]. Unlike Q2(R1), which focused primarily on the initial validation stage, Q2(R2) emphasizes continuous method performance verification throughout the entire lifecycle—from development and validation to routine use and eventual retirement [58] [61]. This approach aligns with broader pharmaceutical quality system concepts described in ICH Q8 to Q12, promoting better integration between method development, validation, and continual improvement [58].
Enhanced Integration with Risk Management and AQbD
Q2(R2) formally incorporates risk assessment as a required element and supports the integration of Analytical Quality by Design (AQbD) principles [58] [61]. The guideline encourages the use of risk management tools such as FMEA (Failure Mode and Effects Analysis) and Ishikawa diagrams to proactively identify and control method-related risks [58]. This alignment with AQbD facilitates the definition of an Analytical Target Profile (ATP) and exploration of Method Operable Design Regions (MODR), ensuring methods are designed with predefined objectives to meet quality requirements [58] [61].
Expanded Scope and Application
While Q2(R1) was primarily designed around traditional small molecule drugs and chromatographic methods, Q2(R2) broadens its applicability to various techniques including spectroscopy (NIR, Raman, NMR, MS), biological assays (ELISA, qPCR), and multivariate procedures [60] [62]. This extension is particularly valuable for supporting the validation of complex analyses such as real-time release testing (RTRT) and addressing the unique challenges posed by biologics [6] [62]. The revised guideline also allows for the use of platform analytical procedures, enabling streamlined development and validation by utilizing existing procedures across multiple products with minimal adjustments [62].
Detailed Comparison of Validation Parameters
Specificity and Selectivity
ICH Q2(R1) required specificity as the ability to assess the analyte accurately in the presence of other components [58]. ICH Q2(R2) enhances this concept by incorporating the term "selectivity," acknowledging that specificity is not always achievable across all techniques [62]. The revised guideline emphasizes demonstrating unbiased measurements and introduces "technology inherent justification," allowing specificity to be predicted through technical parameters (e.g., resolution of isotopes in MS analysis, chemical shifts in NMR), potentially reducing the need for additional experimental studies [62].
Linearity, Range, and Response
ICH Q2(R1) defined linearity as the method's ability to produce results directly proportional to analyte concentration within a given range [58]. ICH Q2(R2) introduces crucial distinctions between "reportable range" and "working range," and replaces "linearity" with the broader concept of "response" [60] [62]. The reportable range pertains to analyte concentration in the sample, while the working range focuses on analyte concentration in the test solution [62]. This change accommodates both linear and non-linear calibration models, which is particularly important for techniques like immunoassays, cell-based assays, and non-linear detectors [62].
Table 1: Comparison of Range Requirements for Assay Methods
| Guideline | Lower Range Limit | Upper Range Limit |
|---|---|---|
| ICH Q2(R1) | Not explicitly defined | Not explicitly defined |
| ICH Q2(R2) | 80% of lower specification limit | 120% of upper specification limit |
Accuracy and Precision
While both guidelines require assessment of accuracy (closeness to true value) and precision (repeatability across conditions), ICH Q2(R2) expands the recommendations for how to assess these parameters both independently and in combination [62]. The revised guideline emphasizes reporting mean percent recovery for accuracy with appropriate confidence intervals, and standard deviation or relative standard deviation for precision with suitable confidence intervals [62]. It also introduces a combined approach for assessing accuracy and precision that may involve estimating prediction, tolerance, or confidence intervals compared to relevant performance criteria [62].
Detection and Quantitation Limits
ICH Q2(R1) required determination of Limit of Detection (LOD) and Limit of Quantitation (LOQ) for relevant methods [58]. ICH Q2(R2) refines this concept by introducing the term "lower range limit", which encompasses both detection and quantitation limits [62]. The revised guideline adds a new impurity testing criterion: the lower range limit must meet or fall below the reporting threshold. Furthermore, if the lower range limit substantially exceeds the reporting limit (e.g., by 10-fold), justifications may support omitting confirmatory evaluation [62].
Robustness and System Suitability
ICH Q2(R1) treated robustness as optional with limited detail [58]. In contrast, ICH Q2(R2) makes robustness testing compulsory and integrates it with the lifecycle management approach, requiring continuous evaluation to demonstrate a method's stability against operational variation [6]. System suitability testing (SST), which was only implied in Q2(R1), is now explicitly emphasized and linked to ongoing method performance monitoring [58].
Table 2: Comprehensive Comparison of Validation Parameters
| Parameter | ICH Q2(R1) | ICH Q2(R2) | Key Differences |
|---|---|---|---|
| Specificity/Selectivity | Required | Required | Q2(R2) introduces "selectivity" and "technology inherent justification" |
| Linearity/Response | Required | Replaced by "Response" | Q2(R2) accommodates both linear and non-linear calibration models |
| Range | Required | Required with enhanced definitions | Q2(R2) distinguishes "reportable range" vs. "working range" |
| Accuracy & Precision | Required | Required with expanded guidance | Q2(R2) introduces combined assessment approaches and confidence intervals |
| LOD & LOQ | Required | Termed "Lower Range Limit" | Q2(R2) links to reporting thresholds and allows justifications for omission |
| Robustness | Optional, limited detail | Recommended, lifecycle-focused | Now compulsory and integrated with development and verification |
| System Suitability | Implied | Emphasized | Explicitly linked to method performance monitoring |
| Risk Assessment | Not addressed | Required | Encouraged to justify design and control strategies |
| Lifecycle Approach | Absent | Central concept | Promotes continuous method performance verification |
| AQbD Integration | Not addressed | Supported | Alignment with Q14 to define ATP and MODR |
Practical Implementation and Regulatory Implications
Method Validation Protocols and Procedures
The implementation of Q2(R2) requires significant changes to validation protocols and procedures. Organizations should incorporate prior knowledge and development data (as outlined in ICH Q14) as part of the validation data package [60] [62]. When using established platform analytical procedures for new purposes, reduced validation testing is possible with scientific justification [60] [62]. For the assessment of linear response, Q2(R2) advances recommendations by incorporating residual plot analysis in addition to traditional parameters like correlation coefficient [62].
Regulatory Expectations and Global Perspectives
Regulatory agencies worldwide, including the U.S. FDA, EMA, MHRA, and CDSCO, are increasingly promoting risk-based, science-driven validation strategies that emphasize ongoing method control [58]. Regulatory inspections have increasingly focused on deficiencies related to incomplete method robustness data, lack of performance verification, and inadequate change control documentation [58]. The implementation of Q2(R2) is expected to improve regulatory communication between industry and regulators, facilitate more efficient scientific and risk-based approval, and enhance post-approval change management of analytical procedures [60].
The Scientist's Toolkit: Essential Elements for Q2(R2) Implementation
Table 3: Key Research Reagent Solutions for Q2(R2) Compliance
| Tool/Reagent | Function in Validation | Q2(R2) Application |
|---|---|---|
| Reference Standards | Establish accuracy and calibration | Critical for defining reportable and working ranges |
| System Suitability Test Materials | Verify method performance before use | Required for ongoing performance verification |
| Quality Control Samples | Monitor precision over time | Essential for continued method performance verification |
| Forced Degradation Materials | Establish specificity and stability | Used in lifecycle-based robustness studies |
| Multivariate Calibration Tools | Model complex analytical responses | Required for non-linear and multivariate procedures |
Strategic Recommendations for Implementation
Education and Training Programs
Organizations should invest in comprehensive training programs to familiarize staff with the new Q2(R2) and Q14 guidelines, focusing on the lifecycle approach, risk management, and the importance of defining the ATP [6]. Training should cover the specific changes between Q2(R1) and Q2(R2), with practical examples relevant to the organization's analytical techniques and product portfolio.
Process Reevaluation and Gap Analysis
Conduct thorough assessments of existing analytical methods and validation processes to identify gaps and areas for improvement in line with the new ICH guidelines [6]. This includes evaluating current documentation practices, validation protocols, and change control procedures to ensure alignment with Q2(R2) requirements.
Implementation of Risk-Based Method Development
Adopt a proactive risk management strategy as recommended by ICH Q14, conducting thorough risk assessments during early method development stages to identify potential challenges [6]. Leverage tools such as FMEA (Failure Mode and Effects Analysis) to systematically evaluate potential risks and their impacts on method performance [58] [6].
Enhanced Documentation Practices
Strengthen documentation systems to meet Q2(R2) requirements, ensuring all phases of method development, validation, and subsequent changes are thoroughly documented [6]. Implement robust electronic record-keeping systems to facilitate data integrity, traceability, and streamlined regulatory audits.
The transition from ICH Q2(R1) to Q2(R2) represents a significant paradigm shift in analytical method validation, moving from a static checklist approach to a dynamic, science- and risk-based lifecycle management model. This evolution addresses the increasing complexity of modern pharmaceutical products and analytical technologies while promoting enhanced product quality and patient safety.
The key differentiators of Q2(R2)—including the lifecycle approach, integration with AQbD principles, expanded scope for modern techniques, and emphasis on continuous verification—provide a more robust framework for ensuring analytical methods remain fit-for-purpose throughout their operational life. While implementation requires significant effort in training, process modification, and cultural adaptation, the long-term benefits of reduced revalidation burdens, improved regulatory flexibility, and strengthened quality assurance systems justify this investment.
As the June 2024 effective date approaches, pharmaceutical companies should proactively develop implementation strategies, beginning with gap analysis and training, followed by phased integration into new and existing method validation programs. This proactive approach will ensure compliance while maximizing the benefits of this modernized regulatory framework.
The Role of ICH Q14 and the Analytical Target Profile (ATP) in Method Development
The introduction of ICH Q14 on Analytical Procedure Development and the revision of ICH Q2(R2) on Validation of Analytical Procedures represent a fundamental shift in pharmaceutical analytics. These guidelines, particularly when considered alongside the established ICH Q2(R1), move the industry away from traditional, static method validation toward a dynamic, lifecycle approach [6]. ICH Q14 establishes, for the first time, an independent regulatory framework for systematic, risk-based analytical procedure development [63]. This paradigm shift aligns analytical science with the Quality by Design (QbD) principles already established in ICH Q8 for pharmaceutical development, fostering greater robustness, flexibility, and scientific understanding [63]. Central to this new framework is the Analytical Target Profile (ATP), a foundational concept that prospectively defines the required quality characteristics of an analytical procedure to ensure it is fit for its intended purpose throughout its lifecycle [64].
Core Concepts: ATP, ICH Q14, and Their Relationship to ICH Q2(R1)
Defining the Analytical Target Profile (ATP)
The Analytical Target Profile (ATP) is a prospective summary of the quality characteristics of an analytical procedure [64]. It outlines what the procedure needs to achieve—the required level of performance—without initially constraining the specific technological or methodological approach [63]. In essence, the ATP defines "what" needs to be measured and the required quality of the result, leaving the "how" to be determined during development.
The ATP serves a parallel role for analytical procedures that the Quality Target Product Profile (QTPP) serves for drug product development. Just as the QTPP summarizes the target quality characteristics of a drug product, the ATP captures the target performance of the analytical procedure used to measure those characteristics [64]. Its implementation early in development facilitates monitoring and continual improvement and forms the foundation for the subsequent validation of the analytical procedure per ICH Q2(R2) [64].
The Scope and Objectives of ICH Q14
ICH Q14 provides a structured framework for the development of analytical procedures. It describes two complementary approaches for development [64]:
- The Minimal Approach: A more traditional approach.
- The Enhanced Approach: A systematic, science- and risk-based approach that includes the ATP, prior knowledge, risk assessment, designed experiments (e.g., DoE), and the definition of a control strategy.
The guideline aims to develop methods that are robust, efficient, and adaptable within a clearly defined method operable design region (MODR), promoting flexibility and continuous improvement throughout the analytical procedure's lifecycle [63].
The Foundation of ICH Q2(R1)
ICH Q2(R1), titled "Validation of Analytical Procedures: Text and Methodology," provides the foundational parameters for validating analytical methods [5] [3]. It outlines the key validation characteristics—such as specificity, accuracy, precision, linearity, and range—that must be considered and the experimental data required to demonstrate that a method is suitable for its intended purpose [5] [3] [6]. While ICH Q14 and Q2(R2) build upon this foundation, ICH Q2(R1) remains the core document establishing the fundamental principles of analytical method validation.
An Integrated Framework: ICH Q14 and ICH Q2(R2)
ICH Q14 and the updated ICH Q2(R2) are designed to be used together, creating a seamless continuum from method development to validation and ongoing lifecycle management [6]. The ATP is the critical link between these two guidelines; the performance characteristics and acceptance criteria defined in the ATP directly inform the validation studies required under ICH Q2(R2) [64]. This integration ensures that the procedure is developed with validation in mind, enhancing robustness and regulatory flexibility.
The Analytical Target Profile (ATP) in Detail
Components of an Effective ATP
A well-constructed ATP documents all necessary requirements for the analytical procedure to ensure it generates reliable results for decision-making. The table below summarizes the core components of an ATP as illustrated in regulatory discussions.
Table 1: Key Components of an Analytical Target Profile (ATP)
| ATP Component | Description | Purpose |
|---|---|---|
| Intended Purpose | A clear description of what the procedure measures (e.g., quantitation of an active ingredient, impurity level, or biological activity) [64]. | Defines the fundamental goal of the analytical procedure. |
| Technology Selection | The selected technology (e.g., HPLC, cell-based assay, ELISA) and the rationale for its selection [64]. | Justifies the chosen analytical technique based on development studies, prior knowledge, or literature. |
| Link to CQAs | A summary of how the procedure provides reliable results for the Critical Quality Attribute(s) being assessed [64]. | Ensures the method is designed to control attributes impacting product quality, safety, and efficacy. |
| Performance Characteristics & Acceptance Criteria | Defines the required level for characteristics such as accuracy, precision, specificity, and range, along with justified acceptance criteria [64]. | Sets the quantitative standards the method must meet to be considered fit-for-purpose. |
| Reportable Range | The range over which the analytical procedure must meet the accuracy and precision criteria [64]. | Ensures reliable measurement across all relevant concentration levels. |
The ATP Development Workflow
The process of defining and utilizing an ATP follows a logical, sequential workflow that integrates with overall product development. The following diagram visualizes this lifecycle workflow and the key questions addressed at each stage.
Implementing the Enhanced Approach: From ATP to Control Strategy
Systematic Analytical Procedure Development
The enhanced approach in ICH Q14 advocates for a systematic development process grounded in scientific rigor and risk management. Key methodological tools include:
- Design of Experiments (DoE): A central tool for systematically assessing the effects of multiple method parameters and their interactions simultaneously [63]. DoE enables efficient identification of critical method parameters and builds a mathematical model to define the method's design space.
- Risk Assessment: Early risk management tools (e.g., Failure Mode and Effects Analysis) are used to identify potential parameters that could impact method performance [6]. This allows for a focused development effort on high-risk factors.
- Prior Knowledge: Leveraging existing knowledge from similar methods or molecules accelerates development and strengthens scientific justification [64].
Defining the Method Operable Design Region (MODR)
A key outcome of the enhanced development approach is the establishment of a Method Operable Design Region (MODR). The MODR is defined as the "combination of analytical procedure parameter ranges within which the analytical procedure performance criteria are fulfilled and the quality of the measured result is assured" [63]. Operating within the MODR provides flexibility, as changes within this pre-defined region are not considered regulatory post-approval changes and do not require re-approval [63]. The relationship between the ATP, development, and the MODR is illustrated below.
The Scientist's Toolkit: Essential Reagents and Solutions
The practical implementation of ICH Q14 principles relies on a suite of methodological and technological tools. The following table details key solutions and their functions in structured method development.
Table 2: Essential Research Reagent Solutions and Tools for ICH Q14-Compliant Method Development
| Tool / Solution | Function in Method Development |
|---|---|
| Design of Experiments (DoE) Software | Enables systematic planning of experiments to efficiently evaluate multiple parameters and their interactions, building a mathematical model of the method [63]. |
| Multivariate Statistical Analysis Tools | Supports the analysis of complex data sets from DoE studies to identify critical parameters and define the MODR [63]. |
| Reference Standards & Certified Materials | Provides the benchmark for accuracy, precision, and system suitability testing, ensuring the method is calibrated against a known quantity. |
| Chromatographic Columns & Reagents (HPLC/UPLC) | Critical components for chromatographic method development; selection is often studied in DoE to understand their impact on performance (e.g., resolution, peak shape). |
| Stressed & Degraded Samples | Used during development and validation to demonstrate the method's specificity and stability-indicating properties by separating analytes from degradation products. |
| Robustness Challenge Kits | Standardized sets of parameter variations (e.g., pH, temperature, flow rate) used to formally test the method's robustness within the proposed MODR. |
Experimental Protocols for Key Activities
Protocol for Defining the ATP
A structured protocol is essential for creating a scientifically sound ATP.
- Input Gathering: Collect all relevant information, including the QTPP, identified CQAs for the attribute to be measured, and desired reporting ranges [64].
- Define Intended Purpose: Draft a clear, concise statement of what the method must measure (e.g., "Quantify the active pharmaceutical ingredient in a drug product from 50% to 150% of the label claim with an accuracy of 98.0-102.0%") [64].
- Establish Performance Criteria: For each relevant performance characteristic (accuracy, precision, specificity, range), set justified acceptance criteria based on the product's needs, compendial requirements, and prior knowledge [64].
- Technology Selection and Rationale: Based on the ATP requirements, select an appropriate analytical technique (e.g., HPLC, ELISA) and document the scientific rationale for its selection [64].
- Documentation and Review: Document the finalized ATP and use it as the governing document for all subsequent development and validation activities.
Protocol for Conducting a DoE for MODR Definition
This protocol outlines the key steps for executing a DoE to establish a Method Operable Design Region.
- Define Objective: State the goal, e.g., "To define the MODR for the HPLC method parameters to ensure system suitability criteria are consistently met."
- Identify Factors and Responses:
- Factors: Select critical method parameters (e.g., pH of mobile phase, column temperature, gradient time) identified from risk assessment.
- Responses: Define critical method performance outputs (e.g., resolution, tailing factor, retention time).
- Select Experimental Design: Choose an appropriate design (e.g., Full Factorial, Central Composite) that allows for modeling the relationship between factors and responses.
- Execute Experiments: Run the experiments in a randomized order to minimize bias.
- Analyze Data and Build Model: Use statistical software to analyze the data, build a mathematical model, and create contour plots to visualize the relationship between parameters and performance.
- Verify the MODR: Conduct verification experiments at set points within the proposed MODR to confirm that the model accurately predicts method performance.
The Lifecycle Approach: Integration with ICH Q12 and Continuous Improvement
ICH Q14 embeds analytical procedures within a full lifecycle management framework, as outlined in ICH Q12 [64]. The ATP is a living document that facilitates this approach. After a method is approved and implemented, its performance is continuously monitored during routine use [6]. Data from quality control charts and ongoing testing are reviewed. If performance drifts or new technologies emerge, the ATP provides the basis for evaluating the impact of any proposed changes [64]. Changes that stay within the predefined MODR can be managed through the company's Pharmaceutical Quality System without prior regulatory approval, enabling agile and continuous improvement while maintaining product quality [63]. This lifecycle view transforms the analytical procedure from a static document into a dynamic, knowledge-driven system.
Applying a Risk-Based and Science-Driven Strategy for Compliance
In the highly regulated pharmaceutical industry, the approach to compliance and analytical method validation is undergoing a profound transformation. Organizations are shifting from reactive, checklist-based compliance to a proactive, strategic framework that integrates risk-based principles and scientific rigor. This evolution is particularly evident in the recent updates to the International Council for Harmonisation (ICH) guidelines, which now emphasize a lifecycle approach to analytical procedures [61]. The modern regulatory landscape demands more than mere box-ticking—it requires demonstrated understanding and control based on sound science and risk assessment [11].
A risk-based approach (RBA) fundamentally changes how organizations prioritize their compliance efforts. Instead of treating all requirements equally, RBA focuses resources on the areas of highest potential impact, ensuring that the most significant threats to product quality and patient safety receive appropriate attention [65] [66]. This strategy aligns compliance activities with business objectives while enhancing operational efficiency and regulatory defensibility [67]. When combined with science-driven development principles, it creates a robust framework for maintaining compliance throughout the entire analytical procedure lifecycle.
The Foundation: Understanding Risk-Based Compliance
Core Principles of a Risk-Based Approach
A risk-based approach to compliance management involves identifying, assessing, and prioritizing risks based on their potential impact and likelihood [65] [66]. This methodology enables organizations to allocate resources more efficiently by focusing on high-risk areas while applying less intensive measures to lower-risk concerns [68]. The fundamental principle is that not all risks deserve equal attention—resources should be directed where they can provide the greatest protective value [67].
The key elements of an effective risk-based approach include systematic risk identification, thorough assessment using standardized methodologies, strategic prioritization based on criticality, tailored control and mitigation planning, continuous monitoring and reporting, and alignment with overarching business objectives [68]. These elements work together to create a dynamic system that responds to changing conditions rather than maintaining a static compliance posture.
Benefits Over Traditional Compliance Methods
Traditional compliance strategies often employ a checklist mentality, ensuring every requirement is addressed regardless of its risk level [65]. This approach can be resource-intensive and may overlook significant risks that fall outside the predefined checklist [67]. In contrast, a risk-based approach offers several distinct advantages that enhance both compliance outcomes and organizational performance.
Enhanced Resource Allocation: Organizations can concentrate resources on addressing the most critical risks, avoiding unnecessary expenditures on low-risk activities [66]. This optimization is particularly valuable for organizations with limited compliance personnel or budgets.
Improved Regulatory Defensibility: Regulators increasingly expect risk-based compliance programs [67]. Demonstrating a systematic approach to identifying and mitigating risks provides stronger evidence of compliance commitment than checklist-based documentation.
Greater Operational Resilience: By focusing on the most significant threats, organizations can build stronger defenses against potentially disruptive events, reducing the likelihood and impact of compliance failures [67].
Proactive Compliance Posture: A risk-based approach enables organizations to anticipate regulatory changes and emerging risks rather than merely reacting to issues as they arise [66]. This forward-looking orientation helps future-proof compliance efforts.
The Regulatory Evolution: ICH Q2(R1) to Q2(R2) and Q14
Limitations of the Traditional Approach
The original ICH Q2(R1) guideline, established in 1994, provided a foundational framework for analytical method validation but showed increasing limitations as pharmaceutical science advanced [6]. Primarily designed for traditional small molecule drugs and conventional analytical techniques, it offered minimal guidance for the unique challenges posed by complex biologics and modern analytical technologies [6] [61]. The guideline's prescriptive nature sometimes led to ritualistic interpretation, where laboratories would validate parameters simply because they were mentioned in the guidance, regardless of their relevance to the specific method [15].
This traditional approach treated method validation as a one-time event rather than an ongoing process, creating potential gaps in maintaining method performance throughout its operational life [6]. The focus was primarily on the validation phase, with little emphasis on systematic method development or continuous monitoring, creating a disjointed lifecycle for analytical procedures [15].
Key Advancements in Modern Guidelines
The simultaneous introduction of ICH Q2(R2) and ICH Q14 represents a significant modernization of analytical procedure guidelines [11]. These updated guidelines shift from a prescriptive, "check-the-box" approach to a more scientific, lifecycle-based model that emphasizes understanding and control [11] [61]. This evolution addresses the increasing complexity of biopharmaceutical products and embraces advances in analytical technology that were not adequately covered in the original guidance [6].
Table: Key Changes from ICH Q2(R1) to the New Framework
| Aspect | Traditional Approach (ICH Q2(R1)) | Modern Approach (ICH Q2(R2) & Q14) |
|---|---|---|
| Overall Philosophy | One-time validation event | Continuous lifecycle management [6] |
| Method Development | Minimal guidance provided | Structured framework with ATP and QbD principles [11] |
| Regulatory Flexibility | Rigid, prescriptive requirements | Science- and risk-based justification [61] |
| Technology Scope | Primarily traditional chromatography | Includes modern techniques like multivariate methods [11] |
| Post-Approval Changes | Often requires regulatory submissions | More flexible management through risk-based control strategy [11] |
| Documentation Emphasis | Validation parameters and results | Comprehensive understanding and control [6] |
A cornerstone of the modern approach is the Analytical Target Profile (ATP), introduced in ICH Q14 [11]. The ATP represents a prospective summary of an analytical procedure's required performance characteristics, serving as the foundation for method development and validation planning [11]. By defining the ATP at the beginning of development, laboratories can design fit-for-purpose methods with clearly defined objectives, facilitating a more systematic and efficient validation process [11].
The enhanced approach also incorporates Quality by Design (QbD) principles into analytical development, emphasizing prior knowledge and risk assessment to build quality into methods from the outset [61]. This proactive stance contrasts with the traditional approach, which often relied on retrospective troubleshooting of method failures [6].
Implementing the Strategy: A Practical Framework
The Analytical Procedure Lifecycle
The modern guidelines introduce a comprehensive lifecycle approach to analytical procedures, encompassing three interconnected stages: procedure design and development, procedure performance qualification (validation), and ongoing procedure performance verification [15]. This continuous lifecycle model replaces the traditional linear progression with a more dynamic system that incorporates feedback loops for continuous improvement [6].
The lifecycle begins with defining an Analytical Target Profile (ATP), which specifies the procedure's intended purpose and performance requirements [11] [15]. This foundational document guides the subsequent development and validation activities, ensuring alignment with the method's intended use [11]. The ATP serves as the quality target for method development, similar to how a Quality Target Product Profile guides drug product development [61].
Risk Assessment Methodology
Risk assessment forms the backbone of a science-based compliance strategy. ICH Q9 quality risk management principles provide a systematic framework for identifying and evaluating potential risks to analytical procedure performance [11]. This proactive assessment enables developers to focus on controlling critical parameters that could affect method reliability [6].
Table: Essential Risk Assessment Tools for Analytical Development
| Tool | Primary Function | Application in Analytical Procedures |
|---|---|---|
| Risk Register | Comprehensive listing of identified risks, their impact, probability, and mitigation strategies [66] | Central repository for monitoring and managing risks throughout the analytical procedure lifecycle |
| Failure Mode and Effects Analysis (FMEA) | Systematic approach for identifying potential failures in a process or design [66] [6] | Prioritizing potential method failures based on severity, occurrence, and detection |
| Root Cause Analysis | Identifying underlying causes of risks or failures [66] | Addressing fundamental sources of method variability rather than symptoms |
| Probability and Impact Matrix | Prioritizing risks by assessing likelihood and potential consequences [66] | Focusing development and validation efforts on the most significant risks to method performance |
During method development, risk assessment helps identify which factors (e.g., sample preparation, chromatographic conditions, instrument parameters) potentially affect method performance [6]. This understanding guides experimentation to establish appropriate controls and method ranges [61]. The enhanced approach described in ICH Q14 encourages more extensive characterization studies to establish method robustness, linking this knowledge to a risk-based control strategy [11].
Experimental Protocols for Risk-Based Method Validation
Implementing a risk-based approach requires specific experimental protocols that align with the principles of ICH Q2(R2) and Q14. The validation process should be tailored to the method's specific use cases and risk profile, moving beyond the traditional one-size-fits-all approach [11].
Protocol 1: Analytical Target Profile Development
- Objective: Define the performance requirements for the analytical procedure based on its intended use [11]
- Methodology: Conduct a systematic review of the analytical needs, including the analyte characteristics, matrix effects, required sensitivity, and precision [15]
- Output: A documented ATP specifying the procedure's performance criteria, which will guide development and validation activities [11]
Protocol 2: Risk-Based Parameter Selection for Validation
- Objective: Identify which validation parameters require evaluation based on the method's intended use and risk assessment [11]
- Methodology: Apply a decision tree based on the type of analytical procedure (identification, testing for impurities, assay, etc.) and prior knowledge [11]
- Output: A tailored validation protocol that focuses resources on the most relevant parameters [11]
Protocol 3: Design of Experiments for Robustness Testing
- Objective: Establish method robustness through structured experimentation rather than one-factor-at-a-time studies [6]
- Methodology: Use statistical experimental design to evaluate the effect of multiple method parameters and their interactions on performance [61]
- Output: A proven acceptable range for critical method parameters that supports the control strategy [11]
The experimental workflow below illustrates how these protocols integrate into a comprehensive validation approach:
Successful implementation of a risk-based compliance strategy requires both technical tools and organizational frameworks. The following resources provide the necessary foundation for executing the approaches described in this guide.
Table: Essential Resources for Risk-Based Analytical Compliance
| Resource Category | Specific Tools & Techniques | Function & Application |
|---|---|---|
| Risk Assessment Tools | Risk Register [66], FMEA [66] [6], Root Cause Analysis [66], Bowtie Model [66] | Systematic identification, analysis, and control of risks to analytical data quality |
| Statistical Methods | Probability and Impact Matrix [66], Experimental Design (DoE) [61], Multivariate Analysis [11] | Designing efficient studies, establishing method ranges, and evaluating method robustness |
| Documentation Frameworks | Analytical Target Profile [11], Enhanced Method Development Reports [6], Knowledge Management Systems | Capturing and retaining method understanding and supporting regulatory submissions |
| Quality Systems | Change Management [11], Deviation Management, Continuous Monitoring [66] | Maintaining the validated state and facilitating continuous improvement |
| Technical Guidelines | ICH Q2(R2) [11], ICH Q14 [11], ICH Q9 [61], USP <1220> [15] | Reference standards for current regulatory expectations and best practices |
The transition from a checklist-based compliance approach to a risk-based, science-driven strategy represents a significant evolution in pharmaceutical quality systems. By embracing the principles outlined in modern ICH guidelines, organizations can build more robust and reliable analytical procedures while enhancing regulatory defensibility [11]. This integrated approach transforms compliance from a bureaucratic exercise into a strategic capability that supports both quality and business objectives [67].
The simultaneous implementation of ICH Q2(R2) and ICH Q14 creates a powerful synergy that supports a more holistic understanding of analytical procedures [61]. Through the application of Quality by Design principles, risk management, and lifecycle thinking, organizations can develop methods that are not only validated but truly robust and maintainable [6]. This scientific approach facilitates more efficient post-approval changes and continuous improvement, benefiting both industry and regulators [11].
For researchers, scientists, and drug development professionals, adopting this strategy requires a shift in mindset from "what does the guideline require" to "what does good science demand" [15]. By focusing on building quality into methods from the beginning and maintaining vigilance throughout the procedure lifecycle, organizations can achieve sustainable compliance that adapts to evolving scientific and regulatory landscapes [61].
In the modern pharmaceutical landscape, the integration of robust analytical methodologies and strategic lifecycle management (LCM) has become a critical imperative for drug development professionals. The International Council for Harmonisation (ICH) Q2(R1) guideline, "Validation of Analytical Procedures: Text and Methodology," provides the foundational framework for ensuring the quality, safety, and efficacy of pharmaceutical products through validated analytical methods [5] [3]. This guidance harmonizes the requirements for validating analytical procedures, detailing the essential validation parameters and methodologies that underpin reliable pharmaceutical analysis [7].
Simultaneously, pharmaceutical LCM has evolved from a tactical afterthought to a core strategic function essential for maximizing a drug's therapeutic and commercial potential from early development through post-patent expiration [69]. Effective LCM encompasses developmental, commercial, and regulatory/legal strategies that work synergistically to optimize a product's value proposition over time [69]. For researchers and scientists, understanding the intersection of these domains—where rigorous analytical control meets strategic lifecycle planning—creates powerful opportunities to enhance product viability, extend therapeutic utility, and ensure regulatory compliance throughout a drug's commercial lifetime.
Foundational Principles: ICH Q2(R1) and Analytical Method Validation
The Role and Importance of Analytical Method Validation
Analytical method validation provides documented evidence that offers a high degree of assurance that an analytical procedure will consistently deliver results that meet its predefined specifications and quality attributes [7]. According to ICH Q2(R1), validation is a mandatory requirement for pharmaceutical registration, ensuring the utmost precision of outcomes, cost-effectiveness, and global recognition of drugs by international regulatory bodies [7]. A validated procedure ensures reliability and consistency in planned outcomes while focusing on the compliance of the product and analysis of the final product, which is significant throughout the pharmaceutical product lifecycle [7].
Validation is particularly crucial for analyzing Active Pharmaceutical Ingredients (APIs), pharmaceutical excipients, and finished dosage forms. It provides a highly accurate, exact, and intended outcome, making it a necessary prerequisite for pharmaceutical testing [7]. The process fundamentally supports Good Laboratory Practices (GLP) and Current Good Manufacturing Practices (cGMP) compliance, ensuring that every pharmaceutical sector tests excipients, in-process quality control materials, packaging materials, and raw materials efficiently for their efficacy study [7].
Core Validation Parameters and Acceptance Criteria
The ICH Q2(R1) guideline establishes several critical validation characteristics that must be evaluated to demonstrate method suitability. The table below summarizes these key parameters and their essential requirements:
Table 1: Core Analytical Method Validation Parameters per ICH Q2(R1)
| Parameter | Definition | Typical Requirements & Methodology |
|---|---|---|
| Specificity | Ability to assess unequivocally the analyte in the presence of components that may be expected to be present | Demonstration of discrimination between analyte, impurities, degradation products, etc. Verified using chromatographic separation or spectral discrimination. |
| Accuracy | Closeness of agreement between the value which is accepted as a true value or an accepted reference value and the value found | Established across specified range, typically with % Recovery studies (often 80-120% of target concentration). |
| Precision | Degree of agreement among individual test results when the procedure is applied repeatedly to multiple samplings | Includes:• Repeatability: Same operating conditions over short interval (<2% RSD often expected for assay)• Intermediate Precision: Within-laboratory variations (different days, analysts, equipment) |
| Linearity | Ability of the method to obtain test results directly proportional to analyte concentration within a given range | Minimum of 5 concentrations evaluated. Correlation coefficient (r) >0.999 often expected for chromatographic assays. |
| Range | Interval between the upper and lower concentrations of analyte for which suitable precision, accuracy, and linearity have been demonstrated | Established from linearity studies, must encompass intended use concentrations (e.g., 80-120% of test concentration for assay). |
| Detection Limit (LOD) | Lowest amount of analyte that can be detected, but not necessarily quantified, under stated experimental conditions | Determined by signal-to-noise ratio (typically 3:1) or based on standard deviation of response and slope. |
| Quantitation Limit (LOQ) | Lowest amount of analyte that can be quantitatively determined with suitable precision and accuracy under stated experimental conditions | Determined by signal-to-noise ratio (typically 10:1) or based on standard deviation of response and slope. |
| Robustness | Capacity of the method to remain unaffected by small, deliberate variations in method parameters | Evaluation of impact of variations in parameters such as pH, mobile phase composition, temperature, flow rate. |
These parameters form the scientific foundation for demonstrating that an analytical method is fit for its intended purpose throughout the product lifecycle. The validation process requires careful planning, execution, and documentation to provide regulatory authorities with confidence in the reliability of the data generated [7] [12].
The Analytical Method Lifecycle Workflow
The following diagram illustrates the comprehensive workflow for analytical method development, validation, and lifecycle management, integrating both traditional Q2(R1) principles and modern enhanced approaches:
Diagram: Analytical Method Lifecycle Workflow
This workflow emphasizes that method validation is not a one-time event but part of a continuous quality process. Under ICH Q2(R1), revalidation is required when modifications occur in the manufacturing process, composition of the finished product, or the analytical method itself [7]. This lifecycle approach aligns with the pharmaceutical industry's increasing focus on ongoing method verification and performance monitoring to ensure methods remain fit-for-purpose throughout their operational use [6].
The Evolving Landscape: From ICH Q2(R1) to Modern Lifecycle Approaches
The Transition to ICH Q2(R2) and ICH Q14
The regulatory landscape for analytical procedures is evolving with the introduction of ICH Q2(R2) and ICH Q14, which represent a significant shift in the standards governing analytical procedure development and validation [6]. These updated guidelines address the increasing complexity of biologic development and the need for more flexible, science-based approaches to method validation [6].
ICH Q2(R2) enhances the original Q2(R1) guidance by providing more detailed consideration of validation parameters for a broader range of analytical techniques, including those used for biological compounds [12]. Concurrently, ICH Q14 introduces a structured approach to analytical procedure development, emphasizing Quality by Design (QbD) principles, risk management, and the definition of an Analytical Target Profile (ATP) early in the development process [6]. Together, these guidelines facilitate a more holistic, science- and risk-based approach to analytical procedures throughout their lifecycle.
Key Enhancements in Modern Analytical Quality Systems
The transition from ICH Q2(R1) to the enhanced approach incorporates several critical advancements:
Table 2: Evolution from ICH Q2(R1) to Modern Lifecycle Approaches
| Aspect | Traditional Approach (Q2(R1)) | Enhanced Approach (Q2(R2) & Q14) |
|---|---|---|
| Philosophy | Validation as one-time event | Lifecycle management with continuous validation |
| Development | Empirical; trial-and-error | Structured; based on ATP and QbD principles |
| Risk Management | Implicit | Explicit, systematic risk assessments |
| Documentation | Focus on validation report | Comprehensive knowledge management |
| Regulatory Flexibility | Fixed conditions | Established Conditions with post-approval change management |
| Technology Adoption | Limited scope | Accommodates advanced analytics (MVDA, PAT) |
The implementation of a lifecycle approach advocates for continuous validation and assessment throughout the method's operational use, rather than treating validation as a one-time event [6]. This shift requires organizations to implement systems for ongoing method evaluation and improvement, integrating quality control and method optimization as continuous activities [6]. This change helps ensure that methods remain effective and compliant over time, adapting to new technologies and regulatory updates while ensuring better consistency and reliability of analytical results [6].
Strategic Integration: Connecting Analytical Quality to Product Lifecycle Management
The Three Pillars of Pharmaceutical Lifecycle Management
For drug development professionals, understanding how analytical quality supports broader product strategy is essential. Modern pharmaceutical LCM rests upon three fundamental pillars that work synergistically to maximize a drug's value proposition over time [69]:
Developmental Strategies: Focus on enhancing a product's clinical profile and expanding its approved indications through additional clinical trials, new formulation development, and novel delivery systems [69].
Commercial Strategies: Aim to optimize product positioning, pricing, and promotional activities to maximize market uptake and value through sophisticated marketing, patient support programs, and strategic pricing models [69].
Regulatory and Legal Strategies: Focus on maximizing market exclusivity periods through patent protections, regulatory exclusivity provisions, and other legal mechanisms to extend a product's period of market protection [69].
Analytical method validation plays a critical enabling role across all three pillars by providing the robust data needed to support new indication approvals, formulation improvements, and regulatory submissions that form the foundation of LCM strategies.
Analytical Methods as Enablers of Lifecycle Extension
Validated analytical methods directly support key LCM initiatives:
Indication Expansion: Robust bioanalytical methods are essential for clinical trials supporting new indications, requiring demonstrated specificity, accuracy, and precision across relevant matrices [69] [7].
Formulation Improvements: When developing new formulations (e.g., extended-release versions, alternative delivery systems), validated stability-indicating methods must demonstrate specificity toward degradation products and the ability to discriminate between formulation components [69] [7].
Patent Protection Strategies: Secondary patents often cover specific polymorphic forms, enantiomers, or formulation aspects whose characterization depends on validated analytical methods [69].
Technology Integration: The incorporation of artificial intelligence and machine learning in LCM enables more data-driven decision-making, revealing previously unidentified opportunities for lifecycle extension [69].
Implementation Framework: Best Practices for Integrated Method Validation and Lifecycle Management
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of integrated validation and lifecycle strategies requires specific materials and reagents. The following table details key research reagent solutions and their functions in analytical method development and validation:
Table 3: Essential Research Reagent Solutions for Analytical Method Development & Validation
| Reagent/Material | Function in Method Development & Validation | Key Quality Attributes |
|---|---|---|
| Reference Standards | • Method calibration• Accuracy determination• System suitability | • High purity (>95%)• Fully characterized• Documented stability |
| Chromatographic Columns | • Separation of analytes from impurities• Specificity demonstration | • Appropriate selectivity• Reproducible lot-to-lot performance• Documented stability |
| Mobile Phase Reagents | • Creating optimal separation conditions• Robustness evaluation | • HPLC grade or higher• Low UV absorbance• Controlled pH and composition |
| Sample Preparation Solvents | • Extraction of analytes from matrix• Specificity and accuracy studies | • Appropriate solubility properties• Compatibility with analytical system• Minimal interference |
| System Suitability Standards | • Verification of chromatographic system performance• Precision monitoring | • Well-characterized resolution mixture• Documented stability• Representative of analytes |
Strategic Recommendations for Successful Implementation
To effectively integrate modern analytical quality systems with comprehensive lifecycle management, organizations should adopt these strategic approaches:
Early LCM Planning with Analytical Quality by Design
- Begin lifecycle management planning during the R&D phase, with analytical method development commencing early in product development [69]
- Implement Quality by Design principles for analytical procedures, focusing on defining the Analytical Target Profile and identifying critical method attributes early in the process [6]
- Adopt a proactive risk management strategy during method development, using tools such as Failure Mode and Effects Analysis (FMEA) to systematically evaluate potential risks [6]
Cross-Functional Collaboration and Training
- Invest in training programs to familiarize staff with evolving guidelines and their practical applications, ensuring a smooth transition to updated standards [6]
- Foster collaboration between analytical development, regulatory affairs, and commercial teams to ensure alignment with overall product strategy [69] [6]
- Implement a portfolio perspective for LCM, considering how individual products complement and potentially compete with others in a company's portfolio [69]
Technology Integration and Data Management
- Leverage artificial intelligence and machine learning to transform pharmaceutical LCM, enabling more data-driven decision-making and revealing previously unidentified opportunities [69]
- Implement robust documentation systems and data integrity measures, ensuring comprehensive record-keeping and reporting that facilitates regulatory inspections and audits [6]
- Adopt a lifecycle management approach for electronic Common Technical Document (eCTD) applications, keeping only the most current information in the current view to streamline regulatory reviews [70]
Continuous Improvement and Knowledge Management
- Reassess existing analytical methods and validation processes considering new guidelines, identifying areas for improvement and integrating lifecycle management principles [6]
- Establish systems for ongoing method performance monitoring, including regularly scheduled reviews to ensure methods remain effective under changing analytical conditions [6]
- Maintain a comprehensive submission tracker that outlines all content contained in submissions, serving as a guide and checklist to ensure all necessary steps are completed [70]
The strategic integration of robust analytical method validation and comprehensive lifecycle management represents a transformative opportunity for pharmaceutical researchers, scientists, and drug development professionals. By embracing the foundational principles of ICH Q2(R1) while adopting the enhanced approaches outlined in ICH Q2(R2) and Q14, organizations can create a seamless continuum from method development to product optimization and lifecycle extension.
This integrated approach enables continuous value creation throughout a drug's commercial lifetime, from maximizing returns on R&D investment through robust analytical control strategies to extending product viability through formulation improvements and indication expansions supported by validated methods. For today's pharmaceutical professionals, mastering this intersection of analytical science and strategic management is not merely advantageous—it is essential for delivering sustainable patient value in an increasingly complex and competitive global marketplace.
The future of pharmaceutical development belongs to those who can effectively bridge scientific rigor with strategic vision, creating products that deliver both therapeutic value and commercial sustainability throughout their entire lifecycle.
Conclusion
ICH Q2(R1) remains a foundational pillar for ensuring the reliability of analytical data in the pharmaceutical industry. Its structured approach to validating specificity, accuracy, precision, and other key parameters is essential for demonstrating that methods are fit-for-purpose. However, the regulatory landscape is evolving with the introduction of ICH Q2(R2) and Q14, which emphasize a more holistic, science- and risk-based lifecycle management of analytical procedures. For biomedical and clinical research, this evolution promises more robust, adaptable, and efficient methods, ultimately enhancing drug quality and accelerating the development of safer, more effective therapies for patients. Embracing the core principles of Q2(R1) while adapting to the enhanced approaches of the new guidelines is the path forward for analytical excellence.
References
- 1. Quo Vadis Analytical Procedure Development and ... [https://www.spectroscopyonline.com/view/quo-vadis-analytical-procedure-development-and-validation]
- 2. ICH Q2 Analytical Method Validation | PPTX [https://www.slideshare.net/slideshow/ich-q2-analytical-method-validation/68242229]
- 3. ICH Q2(R1) Validation of Analytical Procedures [https://www.gmp-compliance.org/guidelines/gmp-guideline/ich-q2r1-validation-of-analytical-procedures-text-and-methodology]
- 4. ICH Guidance; Validation of Analytical Procedures: Text ... [https://jordilabs.com/lab-testing/regulatory/ich-q2-r1/]
- 5. Q2(R1) Validation of Analytical Procedures: Text and ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r1-validation-analytical-procedures-text-and-methodology-guidance-industry]
- 6. Navigating the Biopharmaceutical Method Validation [https://synergbiopharma.com/navigating-the-evolution-from-ich-q2r1-to-ich-q2r2-and-implementation-of-ich-q14-in-biopharmaceutical-method-validation/]
- 7. A holistic perspective on analytical method validation ... [https://ajbps.org/a-holistic-perspective-on-analytical-method-validation-under-international-council-for-harmonisation-q2r1]
- 8. Evolution of ICH Q2 guideline (Validation of Analytical ... [https://biopharmaspec.com/blog/evolution-of-ich-q2-guideline-validation-of-analytical-procedures/]
- 9. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 10. Best Practices For Successful Method Validation [https://lgmpharma.com/blog/best-practices-for-successful-method-validation/]
- 11. ICH and FDA Guidelines for Analytical Method Validation [https://www.labmanager.com/ich-and-fda-guidelines-for-analytical-method-validation-34252]
- 12. ICH Guidelines for Analytical Method Validation Explained [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 13. Analytical Method Validation in Pharmaceuticals | Step-by- ... [https://www.pharmaguideline.com/2010/12/analytical-method-validation.html]
- 14. Method categories according to the ICH Q2(R1) - Lösungsfabrik [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/method-categories]
- 15. Understanding the Lifecycle Approach for Analytical ... [https://www.chromatographyonline.com/view/understanding-lifecycle-approach-analytical-procedures]
- 16. Analytical Methodology: Validation, Verification, or ... [https://vicihealthsciences.com/analytical-methodology-validation-verification-qualification/]
- 17. Analytical Method Validation: Back to Basics, Part I [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-i]
- 18. Key ICH Method Validation Parameters to Know [https://altabrisagroup.com/ich-method-validation-parameters/]
- 19. Comparing Method Validation Guidelines: What You Need ... [https://www.linkedin.com/pulse/comparing-method-validation-guidelines-what-you-need-know-pharcell-z5zrf]
- 20. Statistical Process Control (SPC): Methodology, Tools, and ... [https://investigationsquality.com/2025/04/08/statistical-process-control-spc-methodology-tools-and-strategic-application/]
- 21. Validation of Testing Methods for Tobacco Products [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/validation-and-verification-analytical-testing-methods-used-tobacco-products]
- 22. What is Statistical Process Control? SPC Quality Tools [https://asq.org/quality-resources/statistical-process-control?srsltid=AfmBOooCXK-xwpH8syJCfXu-MdOv8EuEfGnm7R-xMvKmWyEQ9mHTKtPD]
- 23. ICH Q2(R2) Validation of analytical procedures - Scientific guideline | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/ich-q2r2-validation-analytical-procedures-scientific-guideline]
- 24. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 25. The 6 Key Aspects of Analytical Method Validation [https://www.elementlabsolutions.com/uk/chromatography-blog/post/6-key-aspects-of-analytical-method-validation]
- 26. Accuracy, Precision, and Reliability of Chemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3026088/]
- 27. ICH Topic Q 2 (R1) - Validation of analytical procedures [https://www.tga.gov.au/resources/resources/international-scientific-guidelines-adopted-australia/ich-topic-q-2-r1-validation-analytical-procedures-text-and-methodology]
- 28. Key Validation Characteristics in ICH Q2 [https://altabrisagroup.com/validation-characteristics-ich-q2/]
- 29. Understanding the ich ( Q ) guideline 2 R 1 [https://www.linkedin.com/pulse/understanding-ich-q2r1-guideline-priyadarshana-asolkar-cipgc]
- 30. guidelines | PPTX Q 2 r 1 [https://www.slideshare.net/slideshow/q2-r1-guidelines/78687506]
- 31. Analytical Method Development and Validation in ... [https://resolvemass.ca/analytical-method-development-and-validation-in-pharmaceuticals/]
- 32. The Linearity or Reportable Range Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson26.html]
- 33. Ensuring Linearity in Method Validation - A Step-by- ... [https://altabrisagroup.com/linearity-in-method-validation/]
- 34. Linearity of Calibration Curves for Analytical Methods [https://www.intechopen.com/chapters/58596]
- 35. What is meant by the limit of detection and quantification (LOD ... [https://mpl.loesungsfabrik.de/en/english-blog/method-validation/limit-of-detection-quantifcation]
- 36. Limit of Quantitation - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/limit-of-quantitation]
- 37. Detection limit [https://en.wikipedia.org/wiki/Detection_limit]
- 38. Limit of Blank, Limit of Detection and Limit of Quantitation [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556583/]
- 39. Performance Characteristics In Analytical Method Validation [https://gmpinsiders.com/performance-characteristics-method-validation/]
- 40. 3 Key Regulatory Guidelines for Method Validation [https://altabrisagroup.com/regulatory-guidelines-for-method-validation/]
- 41. The Hidden Risks in Analytical Method Validation - [https://pharmuni.com/2025/05/16/the-hidden-risks-in-analytical-method-validation/]
- 42. Common Mistakes in Method Validation and How to Avoid ... [https://www.linkedin.com/pulse/common-mistakes-method-validation-how-avoid-them-part-oona-mcpolin]
- 43. Common Mistakes in Method Validation and How to Avoid ... [https://www.linkedin.com/pulse/common-mistakes-method-validation-how-avoid-them-part-oona-mcpolin-2]
- 44. Challenges in Analytical Method Development and ... [https://www.biopharminternational.com/view/challenges-analytical-method-development-and-validation]
- 45. Some good validation practices for analytical procedures [https://www.a3p.org/en/bonnes-pratiques-validation/]
- 46. How To Perform Accuracy In Analytical Method Validation [https://pharmaguru.co/accuracy-in-analytical-method-validation/]
- 47. Characterization of Precision and Accuracy and Total ... [https://bebpa.org/characterization-of-precision-and-accuracy-and-total-analytical-error-for-bioassays/]
- 48. Analytical Method Validation, Verification or Qualification [https://www.lachmanconsultants.com/2022/12/analytical-method-validation-verification-or-qualification-what-to-use-and-when/]
- 49. Validation, Verification, and Transfer of Analytical ... [https://www.usp.org/events-training/course/validation-verification-and-transfer-analytical-procedures-demand]
- 50. Proposed Revision of USP <1225> Published in the ... [https://www.gmp-compliance.org/gmp-news/proposed-revision-of-usp-1225-published-in-the-pharmacopeial-forum]
- 51. USP <1225> Revised: Aligning Compendial Validation with ... [https://investigationsquality.com/2025/11/13/usp-1225-revised-aligning-compendial-validation-with-ich-q2r2-and-q14s-lifecycle-vision/]
- 52. Amit Andhale's Post - Analytical Method Validation [https://www.linkedin.com/posts/amitandhale_validation-amv2025-ich-activity-7395567873747808256-4ZKY]
- 53. Analytical Procedures and Validation_Specificity ... [https://nitrosamines.usp.org/t/analytical-procedures-and-validation-specificity-parameter-requirment/13578]
- 54. Highlights from FDA's Analytical Test Method Validation ... [https://www.propharmagroup.com/thought-leadership/fda-analytical-test-method-validation-guidance]
- 55. Method Validation: Ensuring Data Integrity in Analytical Labs [https://www.labmanager.com/method-validation-ensuring-data-integrity-in-analytical-labs-34436]
- 56. A lifecycle approach to the qualification of analytical ... [https://cleanroomtechnology.com/a-lifecycle-approach-to-the-qualification-of-analytical-procedures-148049]
- 57. Quo Vadis Analytical Procedure Development and ... [https://www.chromatographyonline.com/view/quo-vadis-analytical-procedure-development-and-validation-]
- 58. Recent Advances in Analytical Method Validation as per ... [https://www.ijpsjournal.com/article/Recent+Advances+in+Analytical+Method+Validation+as+per+ICH+Q2R2+A+Comparative+Review+with+ICH+Q2R1]
- 59. Revised ICH Guideline Q2(R1) On Validation Of Analytical ... [https://www.starodub.nl/updates/revised-ich-guideline-q2r1-on-validation-of-analytical-procedures/]
- 60. ICH Q2(R2) Validation of Analytical Procedures [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 61. New ICH Q2 (R2) and ICH Q14: a Step Forward Towards the ... [https://blog.pqegroup.com/ra-phv/new-ich-q2-r2-and-ich-q14]
- 62. Advancements and knowledge gaps in ICH Q2(R2) [https://www.europeanpharmaceuticalreview.com/article/228989/advancements-and-knowledge-gaps-in-ich-q2r2/]
- 63. ICH Q14 and the Paradigm Shift in Pharmaceutical Analytics [https://www.gmp-journal.com/current-articles/details/ich-q14-and-the-paradigm-shift-in-pharmaceutical-analytics.html]
- 64. Applying ICH Q14 in Pharmaceuticals Part 1 [https://premier-research.com/perspectives/applying-ich-q14-in-pharmaceuticals-part-1-the-application-of-analytical-target-profile-in-analytical-method-development/]
- 65. Risk-Based Approach to Compliance Management [https://www.standardfusion.com/blog/risk-based-approach-to-compliance-management]
- 66. Necessity of Risk-based Compliance Practices [https://www.scrut.io/post/the-necessity-of-a-risk-based-approach-in-modern-compliance]
- 67. Building a Risk-Based Compliance Program: Step-by- ... [https://www.centraleyes.com/building-a-risk-based-compliance-program-guide/]
- 68. What is Risk-Based Approach and Its Key Benefits [https://www.metricstream.com/learn/risk-based-approach.html]
- 69. How Pharmaceutical Life Cycle Management Strategies ... [https://www.drugpatentwatch.com/blog/how-pharmaceutical-life-cycle-management-strategies-are-evolving/?srsltid=AfmBOor8HOa7c-eJ3ZszcBhgtz25aLC0SesH-76FXNIG7H0TFK1VSpyx]
- 70. Understanding regulatory lifecycle management: The basics [https://www.cardinalhealth.com/en/services/manufacturer/biopharmaceutical/drug-development-and-regulatory/resources-for-regulatory-consulting/regulatory-affairs/understanding-regulatory-lifecycle-management.html]