Food Allergen Thresholds and Detection Limits: A Scientific Framework for Risk Assessment and Method Selection
This article provides a comprehensive analysis of food allergen thresholds and the analytical methods used for their detection, tailored for researchers, scientists, and drug development professionals.
Food Allergen Thresholds and Detection Limits: A Scientific Framework for Risk Assessment and Method Selection
Abstract
This article provides a comprehensive analysis of food allergen thresholds and the analytical methods used for their detection, tailored for researchers, scientists, and drug development professionals. It explores the foundational concepts of individual and population thresholds, including the establishment of reference doses by international bodies. The review critically assesses current and emerging detection technologies—from ELISA and PCR to mass spectrometry and AI-enhanced diagnostics—highlighting their operational principles, capabilities, and limitations. A significant focus is placed on troubleshooting common analytical challenges, such as matrix effects and protein degradation in processed foods, and on the critical importance of method validation and comparative performance for ensuring accurate risk assessment and protecting public health.
Defining the Landscape: From Clinical Thresholds to Global Regulatory Standards
In both toxicology and food allergy research, the concept of a "threshold" is fundamental to understanding the relationship between dose and biological effect. A threshold dose is formally defined as the minimum dose of a substance that produces a minimal detectable biological effect in an organism [1]. At doses below this threshold, biological responses are typically absent, and increasing the dose above this level induces a corresponding increase in the percentage or severity of biological responses [1]. This principle forms the cornerstone of modern risk assessment for chemicals, pharmaceuticals, and food allergens, though its application differs significantly between individual susceptibility and population-level protection.
The establishment of these thresholds enables researchers and regulators to define safety standards, set acceptable exposure limits, and protect public health. In the specific context of food allergy research, which frames this technical guide, understanding these concepts is crucial for determining the levels of allergenic proteins that may trigger reactions in sensitive individuals and establishing protective labeling thresholds for the broader population [2] [3]. This whitepaper explores the core concepts of NOAEL, LOAEL, and ED, their methodological establishment, and their critical application in food safety and pharmaceutical development.
Core Threshold Concepts and Definitions
Fundamental Dose Descriptors
Toxicology and pharmacology rely on standardized dose descriptors to quantify the relationship between exposure and effect. The most critical of these are summarized in the table below.
Table 1: Fundamental Toxicological Dose Descriptors
| Acronym | Full Name | Definition | Common Units |
|---|---|---|---|
| NOAEL | No-Observed-Adverse-Effect Level | The highest exposure level at which there are no biologically significant increases in adverse effects [1] [4]. | mg/kg body-weight/day, ppm |
| LOAEL | Lowest-Observed-Adverse-Effect Level | The lowest exposure level that produces biologically significant increases in adverse effects [1] [4]. | mg/kg body-weight/day, ppm |
| NOEL | No-Observed-Effect Level | The maximum dose with no observable effect of any kind (adverse or non-adverse) [1]. | mg/kg body-weight/day, ppm |
| LD₅₀ | Median Lethal Dose | A statistically derived dose that kills 50% of test animals [1] [4]. | mg/kg body weight |
| EC₅₀ | Median Effective Concentration | The concentration that produces 50% of the maximal biological effect [1]. | mg/L, mol/L |
| EDI | Estimated Daily Intake | The measured or estimated amount of a substance consumed daily [5]. | mg/kg body-weight/day |
Population vs. Individual Thresholds
A critical distinction exists between thresholds applicable to populations and those relevant to individuals. Population thresholds like NOAEL and LOAEL are derived from group data and designed to protect the entire population, including sensitive subgroups. These are established through systematic testing in animal or human studies and incorporate safety factors to account for inter-species and inter-individual variability [1] [5].
In contrast, individual thresholds represent the dose at which a specific person exhibits a biological response. In food allergy, this is known as the eliciting dose (ED), which varies significantly between individuals based on their sensitivity [3]. For instance, the ED05 represents the dose of an allergen that elicits a reaction in 5% of the allergic population [3]. This individual variability means that while population thresholds establish generally safe exposure levels, they cannot guarantee protection for every single individual, particularly the most highly sensitive members of the population.
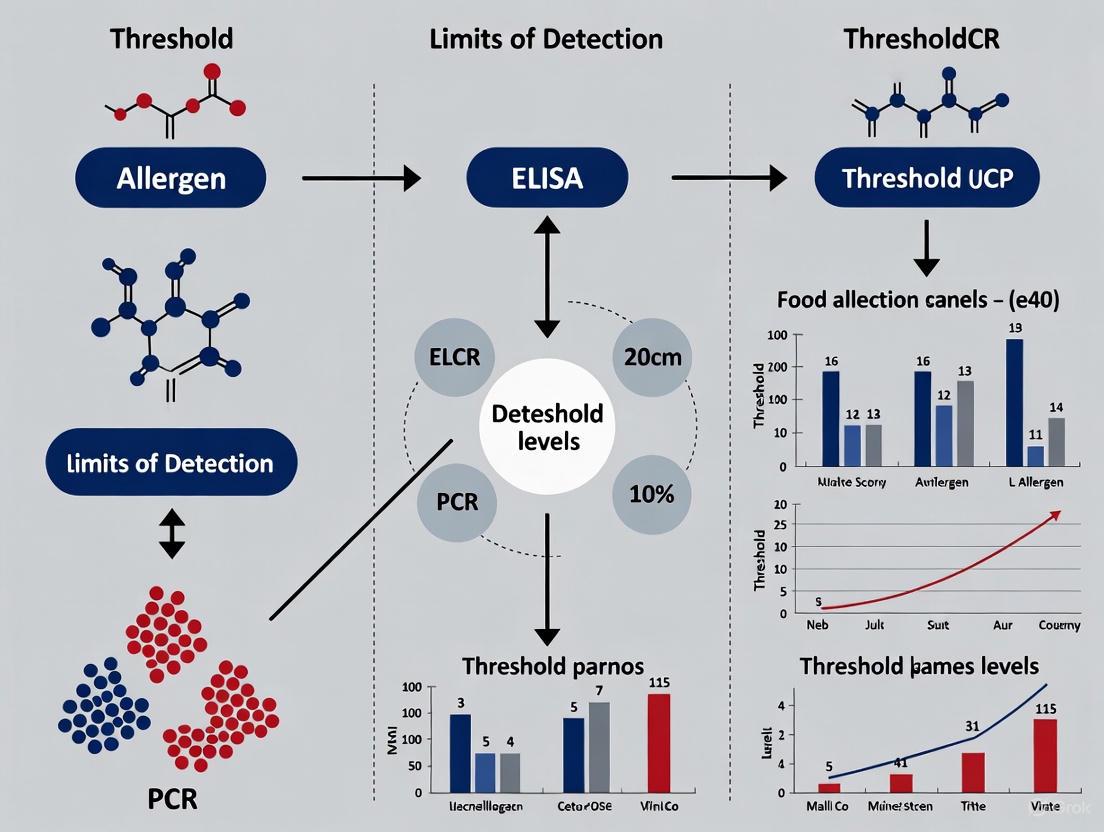
The relationship between these concepts and their progression from experimental data to public health protection is illustrated below.
Methodological Framework for Establishing Thresholds
Experimental Protocols for NOAEL/LOAEL Determination
The establishment of NOAEL and LOAEL values follows rigorous experimental protocols, primarily through repeated dose toxicity studies [1] [4]. The standard methodology involves:
1. Study Design:
- Population: Test species (typically rodents) divided into four groups: control (placebo), low dose, mid-dose, and high dose [1].
- Dosing Regimen: Each group receives the same daily dose for a specified period (28 days, 90 days, or chronic) via appropriate administration routes (oral, dermal, inhalation) [1].
- Parameters Monitored: Comprehensive biological parameters including clinical observations, body weight, food consumption, clinical pathology (hematology, clinical chemistry), organ weights, and histopathology [1].
2. Data Collection and Analysis:
- Necropsy and Tissue Sampling: Conducted at study completion to identify morphological changes [1].
- Statistical Analysis: Comparison of all measured parameters between treated and control groups using appropriate statistical tests to identify biologically significant differences [1].
- Dose-Response Assessment: Establishment of relationship between dose levels and observed effects [1].
3. Threshold Identification:
- NOAEL: The highest dose level without statistically or biologically significant adverse effects [1] [4].
- LOAEL: The lowest dose level with statistically or biologically significant adverse effects [1] [4].
Table 2: Example NOAEL and LOAEL Values from Experimental Studies
| Substance | Test System | NOAEL | LOAEL | Effect Type |
|---|---|---|---|---|
| Oxydemeton-methyl | Rat | 0.5 mg/kg/day | 2.3 mg/kg/day | Systemic toxicity [1] |
| Boron | Rat | 55 mg/kg/day | 76 mg/kg/day | Developmental effects [1] |
| Acetaminophen | Human | 25 mg/kg/day | 75 mg/kg/day | Hepatotoxicity [1] |
| Barium | Rat | 0.21 mg/kg/day | 0.51 mg/kg/day | Renal effects [1] |
Food Allergen Threshold Methodologies
For food allergens, threshold determination employs distinct clinical approaches centered on individual patient responses:
1. Controlled Oral Food Challenges (OFC):
- Design: Progressive administration of increasing amounts of the allergenic food under medical supervision [3].
- Dosing: Typically uses a logarithmic dosing scheme (e.g., 1mg, 3mg, 10mg, 30mg, 100mg, 300mg, 1000mg of protein) [3].
- Endpoint: Identification of the lowest dose that elicits objective allergic symptoms (the individual's eliciting dose) [3].
2. Population Threshold Estimation:
- Data Aggregation: Collection of individual eliciting doses from multiple patients [3].
- Statistical Modeling: Application of statistical models (such as log-normal or log-logistic) to individual data to estimate population thresholds like ED05 [3].
- Quality of Life Assessment: Studies show that knowledge of individual thresholds improves quality of life regardless of challenge outcome [3].
The following diagram illustrates the clinical workflow for establishing individual allergen thresholds and their application to population protection.
Statistical Considerations in Threshold Determination
Biomarker Evaluation and Cut Point Analysis
The evaluation of continuous biomarkers presents significant statistical challenges, particularly in the context of cut point selection for diagnostic or prognostic applications [6]. Key considerations include:
1. Information Loss through Discretization:
- Categorizing continuous biomarkers into discrete groups (e.g., "high" vs. "low") results in significant information loss [6].
- This practice assumes an abrupt change in risk at the cut point, which rarely reflects the true biological relationship [6].
- Arbitrary dichotomization using percentiles (e.g., median splits) can distort true dose-response relationships and reduce statistical power [6].
2. Minimal P-value Approach and Instability:
- A common but problematic method involves testing multiple potential cut points and selecting the one with the smallest P-value [6].
- This approach produces highly unstable cut points, inflates false discovery rates, and generates biased effect size estimates [6].
- The instability of such empirically-derived cut points hinders reproducibility across studies and clinical settings [6].
3. Proper Statistical Modeling:
- Continuous biomarkers should ideally be modeled as continuous variables using non-linear terms (splines, polynomials) when appropriate [6].
- When categorization is clinically necessary, pre-specified, biologically relevant cut points should be used whenever possible [6].
- Internal validation techniques (bootstrapping, cross-validation) and external validation in independent datasets are essential for verifying cut point stability [6].
Uncertainty Factors and Risk Assessment
The transition from experimentally observed thresholds to protective human exposure limits requires the application of uncertainty factors (UFs) to account for various sources of variability and uncertainty [1] [5]:
Reference Dose (RfD) = NOAEL ÷ (UFinter × UFintra) [1]
Where:
- UFinter (typically 10x): Accounts for interspecies differences between test animals and humans [1] [5].
- UFintra (typically 10x): Accounts for variability within the human population, including sensitive subgroups [1] [5].
When only LOAEL is available, additional uncertainty factors may be applied, resulting in more conservative (lower) reference doses [4].
Applications in Food Allergen Safety and Drug Development
Food Allergen Thresholds in Practice
The application of threshold concepts in food allergy management has evolved significantly, with several practical applications:
1. Precautionary Allergen Labeling (PAL):
- Informs consumers about potential unintended allergen presence [2].
- Threshold data help establish scientifically justified labeling levels rather than arbitrary thresholds [3].
2. Immunotherapy Guidance:
- Knowledge of individual thresholds helps tailor oral immunotherapy (OIT) starting doses and progression [3].
- Patients with higher baseline thresholds may respond more favorably to specific treatment protocols [3].
3. Risk Communication and Shared Decision-Making:
- Understanding individual thresholds empowers patients to make informed dietary choices [3].
- Clinicians act as risk management consultants, helping frame food allergy risks within the broader context of daily life risks [3].
4. Regulatory Frameworks:
- The FDA identifies nine major food allergens but has not established regulatory thresholds for any allergens [2].
- The Food Allergen Labeling and Consumer Protection Act (FALCPA) requires clear labeling of major food allergens [2].
The Scientist's Toolkit: Essential Research Materials
Table 3: Key Research Reagents and Materials for Threshold Studies
| Reagent/Material | Function in Threshold Research | Application Examples |
|---|---|---|
| ELISA Kits | Quantification of specific proteins or antibodies | Allergen detection in foods; specific IgE measurement [7] |
| Mass Spectrometry Systems | High-precision quantification of proteotypic peptides | Detection of specific allergen markers in complex food matrices [7] |
| Animal Models (Rodents) | In vivo toxicity and efficacy testing | NOAEL/LOAEL determination for chemicals and drugs [1] |
| Cell Culture Systems | In vitro assessment of biological effects | Mechanism of action studies; high-throughput screening [8] |
| Hyperspectral Imaging (HSI) | Non-destructive allergen detection | Food manufacturing quality control; real-time monitoring [7] |
| ATP Meters | Sanitation verification | Allergen control monitoring in production facilities [7] |
Emerging Innovations and Future Directions
The field of threshold determination continues to evolve with several promising technological and methodological advances:
1. Advanced Detection Technologies:
- AI-enhanced testing with hyperspectral imaging and Fourier Transform Infrared (FTIR) spectroscopy enables non-destructive, real-time allergen detection without altering food integrity [7].
- Mass spectrometry can simultaneously quantify specific allergenic proteins (e.g., Ara h 3 in peanut, Bos d 5 in milk) with detection limits as low as 0.01 ng/mL [7].
- Multiplexed immunoassays allow simultaneous detection of multiple allergens, improving efficiency and comprehensiveness [7].
2. Computational and Analytical Advances:
- Novel transcriptomic tools like THRESHOLD analyze gene expression consistency across patient populations, identifying co-regulation patterns critical for understanding disease mechanisms [9].
- Cloud-based platforms integrate multiple data streams (ATP readings, microbial counts, allergen detection) to provide visualized heat maps and trend analysis for predictive risk management [7].
3. Biomarker Development:
- Statistical frameworks for establishing "predictive biomarker" status require parameter stability across populations and limited within-person variability [10].
- Biomarkers that can be expressed as actual intake plus independent error can substitute for actual intake in disease association analyses [10].
- In immunotherapy development, biomarkers play key roles in demonstrating mechanism of action, dose optimization, and predicting adverse reactions [8].
These innovations are poised to transform threshold determination from primarily reactive to increasingly predictive, enabling more personalized approaches to safety assessment and clinical management.
The concepts of NOAEL, LOAEL, and ED provide a critical framework for understanding the relationship between exposure dose and biological effect across toxicology, immunology, and pharmaceutical development. The distinction between individual thresholds (such as eliciting doses for food allergens) and population thresholds (such as NOAEL-derived reference doses) is fundamental to developing effective public health protections while recognizing individual variability. As methodological innovations continue to emerge in detection technologies, computational analysis, and biomarker development, the precision and personalization of threshold-based safety determinations will continue to improve. This progression promises enhanced protection for sensitive individuals while potentially reducing unnecessary restrictions for the broader population, ultimately supporting the dual goals of safety and food freedom articulated in modern food allergy management [3].
The Joint FAO/WHO Expert Consultation on Risk Assessment of Food Allergens has pioneered a transformative approach to managing global food allergy risks through science-based thresholds. Food allergies affect approximately 220 million people worldwide, constituting a critical public health concern that demands international standardization [11] [12]. The FAO/WHO initiative, conducted through a series of expert meetings beginning in 2020, represents a comprehensive effort to establish quantitative risk assessment frameworks for priority food allergens [13] [11]. This systematic approach addresses the fundamental challenge in food allergen management: determining the level of exposure that protects sensitive individuals while facilitating practical food safety guidelines and evidence-based precautionary labeling.
The establishment of reference doses (RfDs) marks a paradigm shift from qualitative to quantitative food allergen management. These health-based guidance values specify the amount of protein from an allergenic source that the vast majority of allergic individuals can consume without experiencing an adverse reaction [14] [12]. This whitepaper examines the complete scientific framework underlying these international standards, detailing the methodological approaches, experimental foundations, and practical implementations of reference doses within global food safety systems. The FAO/WHO recommendations provide the scientific basis for updating the Codex Alimentarius, the collection of internationally recognized food standards and guidelines, thereby facilitating harmonized global trade while protecting public health [11] [12].
Global Priority Allergen List: Identification and Criteria
Hazard Prioritization Methodology
The FAO/WHO expert committee employed a structured, evidence-based framework to identify global priority allergens through systematic evaluation of three primary criteria: prevalence, potency, and severity [12]. This transparent, quantitative methodology enables consistent identification and prioritization of allergenic foods posing significant public health risks across diverse populations and geographic regions. The prevalence criterion evaluates the proportion of populations experiencing immune-mediated adverse reactions to specific foods, drawing from epidemiological studies across multiple geographic regions to establish global significance [12]. The potency criterion assesses the dose-response relationship, examining the minimal protein doses required to elicit allergic reactions in sensitive populations through controlled clinical studies [14] [12]. The severity criterion evaluates the potential of specific food allergens to cause severe reactions, including anaphylaxis, with a threshold of responsibility for at least 5% of all anaphylaxis cases reported to emergency services in three or more geographic regions [12].
This risk assessment framework was deliberately designed to be transparent and repeatable, allowing for re-evaluation as new epidemiological and clinical data emerges. The systematic application of these criteria ensures that prioritization decisions are based on scientific evidence rather than historical precedent or regional perceptions alone, creating a robust foundation for global food safety policy [12].
Globally Recognized Priority Allergens
Based on the comprehensive risk assessment, the FAO/WHO established a global priority allergen list comprising foods consistently associated with significant allergic reactions across multiple regions [12]. This list provides the foundation for international standardization and includes:
- Cereals containing gluten (wheat, rye, barley, and their hybridized strains)
- Crustacea (shrimp, crab, lobster)
- Eggs
- Fish
- Milk
- Peanut
- Sesame
- Tree nuts (almond, hazelnut, walnut, cashew, pistachio, pecan)
The inclusion of these allergens in the priority list reflects their demonstrated global public health significance based on the prevalence, potency, and severity criteria [12]. The list serves as the scientific basis for the Codex Alimentarius standards regarding mandatory allergen declaration on packaged foods, helping to ensure consistent protection for allergic consumers worldwide [11] [12].
Regionally Significant Allergens
The FAO/WHO framework acknowledges that some allergens, while not meeting the criteria for global priority status, may pose significant regional risks due to local consumption patterns or genetic predispositions in specific populations [12]. These regionally important allergens include:
- Soy
- Specific tree nuts (Brazil nuts, macadamia nuts, pine nuts)
- Celery
- Buckwheat
- Lupin
- Mustard
- Oats
The recognition of regionally important allergens allows individual countries or regions to implement targeted management strategies for foods that pose local risks while maintaining a consistent global framework. This flexible approach acknowledges the diverse dietary patterns and allergy profiles across different populations while working toward international harmonization [12].
FAO/WHO Recommended Reference Doses
Quantitative Reference Dose Values
The FAO/WHO expert committee established science-based reference doses (RfDs) for priority allergens, expressed in milligrams of total protein from the allergenic source [14]. These values represent the amount of allergenic protein that can be safely consumed by the vast majority of allergic individuals without triggering a reaction. The recommended reference doses are summarized in Table 1.
Table 1: FAO/WHO Recommended Reference Doses for Priority Allergens
| Allergen | RfD Recommendation (mg total protein) | Special Considerations |
|---|---|---|
| Walnut | 1.0 | Includes pecan |
| Pecan | 1.0 | Included with walnut |
| Cashew | 1.0 | Includes pistachio |
| Pistachio | 1.0 | Included with cashew |
| Almond | 1.0 | Provisional recommendation |
| Peanut | 2.0 | - |
| Egg | 2.0 | - |
| Milk | 2.0 | Finalized April 2022 |
| Sesame | 2.0 | Finalized April 2022 |
| Hazelnut | 3.0 | - |
| Wheat | 5.0 | - |
| Fish | 5.0 | - |
| Shrimp | 200.0 | - |
The establishment of these reference doses enables a transition from zero-tolerance policies to risk-based approaches that reflect the actual sensitivity of allergic populations [14]. The substantial variation in reference doses across different allergen categories (ranging from 1.0 mg for several tree nuts to 200.0 mg for shrimp) reflects the differential potency of these allergenic foods, with lower values indicating greater allergenic potency [14].
Scientific Basis for Dose Determination
Methodological Approaches
The FAO/WHO committee evaluated four distinct methodological approaches for establishing allergen thresholds before selecting the most appropriate frameworks [14]:
- Analytical-based approach: Relies on detection capabilities of analytical methods
- No Observed Adverse Effect Level (NOAEL) + Uncertainty Factor approach: Applies safety factors to established no-effect levels
- Benchmark Dose (BMD) with or without Margin of Exposure (MOE): Utilizes statistical modeling of dose-distribution relationships
- Probabilistic Hazard Assessment approach: Integrates population sensitivity and exposure data
The committee determined that the Benchmark Dose (BMD) approach and Probabilistic Hazard Assessment were most aligned with their charge and provided the most scientifically robust foundation for establishing reference doses [14]. The BMD approach specifically refers to a statistical modeling technique that identifies the dose that produces a predetermined response level (benchmark response) in a population, typically ranging from 1-10% for allergenic responses [14].
Clinical Data Integration
The reference dose values were derived through systematic evaluation of clinical data from controlled oral food challenges conducted with allergic individuals [14] [12]. These studies measure the minimal eliciting doses that provoke objective allergic symptoms in sensitized populations, establishing dose-response relationships for each priority allergen. The expert committee analyzed population-based threshold distributions to identify doses that would protect the vast majority (typically 90-99%) of allergic individuals [14].
The resulting reference doses incorporate comprehensive safety margins to account for uncertainties in the data and protect highly sensitive subpopulations. The values represent the total amount of allergenic protein that can be consumed in a single eating occasion while providing adequate protection for allergic consumers [14] [12].
Methodological Framework for Threshold Determination
Risk Assessment Protocol
The FAO/WHO established a systematic protocol for determining reference doses that integrates clinical evidence with population-based risk assessment approaches. The methodological framework consists of sequential phases that transform clinical data into actionable risk management tools, as visualized in Figure 1.
Figure 1: Risk Assessment Workflow for Allergen Threshold Determination
Clinical Challenge Study Methodology
Controlled oral food challenges represent the gold standard for generating data on minimal eliciting doses for food allergens. The experimental protocols for these studies require rigorous standardization to ensure reliability and comparability of results [14] [12].
Participant Selection Criteria
- Confirmed IgE-mediated allergy: Participants must have documented sensitization through positive skin prick tests (wheal diameter ≥3mm larger than negative control) and/or detectable allergen-specific IgE (≥0.35 kU/L) [15]
- Clinical history consistent with food allergy: Self-reported or physician-documented reactions to the challenge food
- Absence of exclusionary conditions: No history of severe anaphylaxis requiring ICU admission, unstable asthma, cardiovascular disease, or pregnancy
- Appropriate age representation: Inclusion of both pediatric and adult populations where applicable
- Medication washout periods: Antihistamines discontinued for 3-5 half-lives prior to challenge
Challenge Protocol Design
- Randomized, placebo-controlled, double-blind design: To eliminate bias and ensure scientific validity
- Graduated dosing regimen: Sequential administration of increasing doses (e.g., 0.1mg, 1mg, 10mg, 100mg, 1g, 3g, 10g of allergenic protein) at 15-30 minute intervals
- Dose preparation standardization: Use of defatted nut flours, spray-dried egg white, or purified protein isolates to ensure accurate protein quantification
- Objective symptom monitoring: Standardized assessment tools for evaluating cutaneous, respiratory, gastrointestinal, and cardiovascular symptoms
- Stopping criteria: Predefined symptom thresholds requiring termination of challenge (e.g., widespread urticaria, respiratory distress, 20% decrease in blood pressure)
- Emergency preparedness: Immediate access to epinephrine, antihistamines, corticosteroids, and resuscitation equipment
Statistical Analysis Framework
The dose-distribution modeling approach forms the statistical foundation for reference dose determination. This methodology applies statistical distributions to describe the variation in minimal eliciting doses across allergic populations [14].
Benchmark Dose (BMD) Modeling
- Data fitting: Experimental dose-response data is fitted to appropriate statistical distributions (log-normal, log-logistic, Weibull)
- Benchmark response selection: Typically set at 1-10% of the responding population, representing a tolerable level of response
- BMD calculation: The dose associated with the selected benchmark response is calculated from the fitted distribution
- Uncertainty analysis: Confidence intervals around the BMD estimate are derived using parametric bootstrap or Bayesian methods
Probabilistic Risk Assessment
- Population threshold distribution: Characterizes the variation in individual threshold doses across the allergic population
- Exposure assessment: Integrates data on the distribution of allergen concentrations in food products
- Risk characterization: Combines threshold and exposure distributions to estimate the probability of allergic reactions across the population
- Sensitivity analysis: Evaluates the impact of uncertainty in model parameters on risk estimates
Implementation in Food Safety Systems
Precautionary Allergen Labelling (PAL) Framework
The FAO/WHO recommended implementation of a risk-based precautionary allergen labelling system utilizing the established reference doses [11] [14]. This system provides consistent, evidence-based guidance for indicating the potential presence of unintended allergens in food products. The logical decision process for applying PAL is illustrated in Figure 2.
Figure 2: Decision Framework for Precautionary Allergen Labelling
The PAL system enables quantitative risk management by comparing the estimated exposure to allergenic protein (calculated as concentration multiplied by serving size) with the established reference dose [14]. This represents a significant advancement over previous qualitative approaches that lacked scientific basis and often led to overuse of precautionary labels, diminishing their value for consumers [11] [14].
Global Harmonization Efforts
The FAO/WHO reference doses provide the scientific foundation for international standardization of food allergen management through the Codex Alimentarius Commission [11] [12]. The alignment of global food safety standards offers significant benefits:
- Consistent protection for allergic consumers regardless of geographic location
- Reduced trade barriers through harmonized regulatory requirements
- Improved risk communication with standardized labeling approaches
- Efficient allocation of food industry resources for allergen control measures
- Stimulated innovation in analytical detection methods and food processing technologies
The FAO/WHO recommendations have been presented to the Codex Committee on Food Labelling (CCFL) and the Codex Committee on Food Hygiene (CCFH) to support the development of internationally agreed food safety standards [11]. This represents a critical step toward global implementation of evidence-based allergen management practices.
Regional Implementation Considerations
While the FAO/WHO reference doses provide a scientific foundation for global standards, implementation may vary based on regional factors and regulatory frameworks [14]. In the United States, for example, the Food and Drug Administration (FDA) has historically maintained a zero-tolerance approach for certain allergens, particularly peanuts, though the agency established a threshold of 20 ppm for gluten-free labeling in 2013 [14]. This suggests that regulatory adoption of the FAO/WHO reference doses may proceed gradually, with initial resistance to moving away from established zero-tolerance positions [14].
Regional differences in priority allergens also necessitate flexible implementation approaches. For example, while the FAO/WHO recognizes sesame as a global priority allergen (with a reference dose of 2.0 mg protein), the United States only added sesame as a major food allergen with the 2021 passage of the FASTER Act [14]. Similarly, regionally important allergens such as lupin, buckwheat, or specific tree nuts may require tailored management strategies in areas where they represent significant allergic risks [12].
Research Reagents and Methodological Tools
Essential Research Materials
The experimental protocols underlying food allergen threshold research require specialized reagents and analytical tools. Table 2 summarizes the key research solutions essential for generating the scientific evidence supporting reference dose establishment.
Table 2: Essential Research Reagents and Methodological Tools
| Research Reagent/Solution | Function/Application | Technical Specifications |
|---|---|---|
| Defatted Allergen Extracts | Oral challenge material preparation | Protein content standardized to 1-100 mg/g |
| Allergen-specific IgE Assays | Participant screening and characterization | ImmunoCAP Phadia systems; threshold ≥0.35 kU/L [16] [15] |
| Skin Prick Test (SPT) Solutions | IgE-mediated sensitivity confirmation | Glycerinated extracts (1:10-1:20 w/v); histamine control (10 mg/mL) [15] |
| Protein Reference Standards | Analytical method calibration | Certified reference materials (NIST, IRMM) |
| Mass Spectrometry Reagents | Allergen detection and quantification | Trypsin for protein digestion, iTRAQ/TMT tags for multiplexing |
| ELISA Kits | Food matrix protein quantification | Sandwich format with monoclonal/polyclonal antibody pairs |
| Molecular Allergen Components | Component-resolved diagnostics | Recombinant or natural purified allergens (rBet v 1, rAra h 2, etc.) [15] |
Analytical Method Requirements
The accurate quantification of allergenic proteins in food matrices represents a critical methodological challenge in implementing reference dose-based management systems. Analytical techniques must demonstrate sufficient sensitivity, specificity, and reproducibility to support risk-based decision making [14].
Method Performance Criteria
- Detection sensitivity: Lower limit of detection sufficient to quantify proteins at levels corresponding to reference doses (typically 0.1-10 ppm protein)
- Quantification accuracy: Recovery rates of 50-150% across relevant food matrices
- Matrix tolerance: Reliable performance in complex processed food systems
- Specificity: No cross-reactivity with non-target proteins or food components
- Precision: Inter- and intra-assay coefficient of variation <15-20%
Method Validation Protocols
- Collaborative trials: Ring tests across multiple laboratories to establish reproducibility
- Reference material characterization: Certification of calibrants for method standardization
- Matrix-specific validation: Performance verification in representative food categories
- Proficiency testing: Ongoing assessment of laboratory performance through blinded samples
Future Directions and Research Needs
The establishment of FAO/WHO reference doses represents a foundational achievement in food allergen risk assessment, but several areas require continued research and methodology development. Future efforts should focus on advancing the scientific basis for allergen management through targeted investigations.
Evidence Gaps and Research Priorities
- Population-level threshold variation: Expanded clinical challenge studies across diverse geographic and demographic groups
- Impact of food processing: Systematic evaluation of how thermal processing, fermentation, and other technologies alter allergen potency
- Co-factor effects: Controlled studies examining how exercise, alcohol, medications, and physiological states affect individual thresholds
- Pediatric-specific sensitivity: Age-stratified threshold data to address the unique needs of children with food allergies
- Longitudinal threshold stability: Prospective studies examining how individual thresholds change over time
Methodological Innovations
- Advanced protein quantification: Mass spectrometry-based methods for specific allergen target peptides
- Biomarker development: Correlates of reaction severity to supplement threshold data
- In vitro correlational models: Cell-based assays that predict clinical reactivity
- Data integration platforms: Harmonized databases combining threshold, prevalence, and severity information
The FAO/WHO initiative has established a robust scientific framework for global management of food allergens through evidence-based reference doses. Ongoing research and international collaboration will further refine these standards, enhancing protection for allergic consumers while supporting innovation in the global food industry.
The Role of Thresholds in Risk Assessment and Shared Clinical Decision-Making
In the field of food allergy, a threshold of reactivity is defined as the amount of allergen that an allergic individual can consume without experiencing an adverse reaction. Quantifying these thresholds has become fundamental to modern risk assessment and clinical management, shifting practice from universal avoidance to more personalized approaches. Food allergy affects approximately 1 in 10 adults and 1 in 13 children, creating a significant public health burden that extends beyond physical health to encompass nutrition, psychology, and quality of life [3]. The establishment of evidence-based thresholds enables clinicians, regulators, and patients to move beyond precautionary principles toward scientifically-grounded risk management strategies.
Historically, food allergy management universally treated all patients as being at risk for anaphylaxis and mandated strict avoidance of allergenic foods in all forms and amounts [17]. However, research over the past two decades has demonstrated that many patients tolerate small amounts of allergen without reaction [17]. This discovery laid the foundation for threshold-based approaches that now inform everything from regulatory policy to individual treatment decisions. The evolving science of thresholds represents a paradigm shift in food allergy management, allowing for more nuanced clinical decision-making through shared decision-making processes that actively engage patients in their care [3].
Quantitative Threshold Data for Major Allergens
International research consortia have systematically collected and analyzed threshold data from controlled oral food challenges to establish population-based reference doses for major allergens. These eliciting doses (ED) describe the amount of allergen protein that will produce a reaction in a given percentage of the allergic population. The ED05 and ED10 values represent the doses at which 5% and 10% of allergic individuals would react, respectively [17].
Table 1: Eliciting Doses for Major Food Allergens
| Food | Discrete ED05 (mg) | Cumulative ED05 (mg) | Discrete ED10 (mg) | Cumulative ED10 (mg) |
|---|---|---|---|---|
| Peanut | 2.1 | 3.9 | 7.1 | 9.0 |
| Egg | 2.3 | 2.4 | 6.3 | 7.4 |
| Milk | 2.4 | 3.1 | 7.1 | 9.6 |
| Cashew | 0.8 | 1.6 | 3.4 | 6.2 |
| Shrimp | 280 | 429 | 723 | 1265 |
| Sesame | 2.7 | 4.2 | 10.3 | 16.1 |
Source: Adapted from Hourihane et al. [17]
The Food and Agriculture Organization (FAO) and World Health Organization (WHO) have established reference doses based on the ED05 for global priority allergens to guide regulatory decisions and precautionary allergen labeling [18]. These values represent the level of exposure without appreciable health risks for most allergic consumers.
Table 2: FAO/WHO Recommended Reference Doses for Global Priority Allergens
| Global Priority Allergens | Recommended Reference Doses (mg Total Protein from Allergen Source) |
|---|---|
| Tree nuts (walnut, pecan, cashew, pistachio, almond) | 1.0 |
| Milk | 2.0 |
| Peanut | 2.0 |
| Egg | 2.0 |
| Sesame | 2.0 |
| Hazelnut | 3.0 |
| Wheat | 5.0 |
| Fish | 5.0 |
| Shrimp | 200 |
Source: FAO/WHO Expert Consultation [18]
Methodological Approaches to Threshold Determination
Experimental Protocols for Threshold Assessment
The gold standard for determining individual thresholds is the double-blind, placebo-controlled food challenge (DBPCFC), conducted using internationally standardized protocols. An expert consensus established in 2004 and refined in 2014 provides detailed methodology for challenge-based threshold determination [17]. The experimental workflow follows a rigorous, stepwise approach to ensure patient safety and data reliability.
Figure 1: Experimental workflow for determining allergen thresholds through controlled food challenges. LOAEL: Lowest Observed Adverse Effect Level; NOAEL: No Observed Adverse Effect Level.
Key Methodological Considerations
The DBPCFC protocol incorporates several critical safety and scientific elements. Challenges begin with minimal doses (typically 0.1-1mg of allergen protein) that are unlikely to provoke severe reactions, with dose escalation following predetermined intervals (15-30 minutes) based on the allergen and patient history [17]. The dosing matrix must effectively mask the allergen while maintaining protein integrity and accurate concentration. Active and placebo challenges are conducted on separate days in randomized order to maintain blinding.
Throughout the challenge, patients undergo continuous symptom monitoring using standardized scoring systems such as the PRACTALL criteria or similar validated tools. The challenge endpoint is determined by either the development of objective clinical symptoms or administration of the complete predetermined dose sequence. The lowest dose that produces objective symptoms is recorded as the Lowest Observed Adverse Effect Level (LOAEL), while the preceding dose is designated the No Observed Adverse Effect Level (NOAEL) [17].
Statistical analysis of population threshold data utilizes interval-censoring survival analysis to account for the range between NOAEL and LOAEL values for each individual. This approach enables modeling of the dose-response relationship across the population and calculation of eliciting doses (EDx) for specific percentiles of the allergic population [17].
Threshold Applications in Risk Assessment and Clinical Management
Regulatory and Public Health Applications
Threshold data provides the scientific foundation for evidence-based precautionary allergen labeling (PAL) policies. The VITAL (Voluntary Incidental Trace Allergen Labelling) program utilizes reference doses to establish action levels for food products, determining when precautionary "may contain" labeling is appropriate [18]. This scientifically-grounded approach addresses the problematic variability in current PAL practices, which often leads to consumer confusion and disregard for warnings [18].
Internationally, the Codex Alimentarius Commission has adopted a Code of Practice on Food Allergen Management (CXC 80-2020) based on threshold concepts, promoting global harmonization of allergen management and labeling requirements [18]. Regulatory bodies including the U.S. FDA and European Food Safety Authority (EFSA) utilize threshold data in evaluating the public health importance of food allergens and establishing labeling frameworks [2] [19].
Clinical Implementation and Shared Decision-Making
In clinical practice, knowledge of individual thresholds facilitates personalized management strategies through shared decision-making processes [3]. Threshold information guides multiple aspects of clinical care:
Oral Immunotherapy (OIT) Dosing: Baseline thresholds inform OIT initiation protocols, with higher threshold patients potentially beginning at more advanced dosing stages or utilizing accelerated protocols [17] [3]. A 2017 study by Garvey et al. demonstrated successful home-based OIT induction in children with high peanut thresholds (mild reactions at >1 peanut), with 50% achieving sustained unresponsiveness [3].
Precautionary Label Interpretation: Patients with thresholds above population reference doses may be advised they can safely consume products with precautionary labeling for their allergen, significantly expanding food choices [3]. Clinical surveys indicate 57% of allergists allow ingestion to specified amounts when thresholds are known [3].
Quality of Life Enhancement: Single-dose low-dose challenges (e.g., 1.5mg peanut protein) have demonstrated significant improvements in food allergy-related quality of life regardless of challenge outcome, providing empowerment through knowledge [17] [3]. This approach has proven highly cost-effective (>$19 million per life-year saved) [3].
Analytical Methods Supporting Threshold Implementation
Accurate allergen detection and quantification are essential for implementing threshold-based approaches. Method selection depends on the specific application, with each technology offering distinct advantages and limitations.
Table 3: Analytical Methods for Allergen Detection and Quantification
| Method Category | Specific Technologies | Detection Capabilities | Applications | Considerations |
|---|---|---|---|---|
| Immunoassays | ELISA, Lateral Flow, Multiplex Microarray Immunoassay | Intact proteins or large fragments (>15 amino acids); typically 1-10 ppm | Routine testing, regulatory compliance | Gold standard; may detect non-reactive proteins; commercial availability |
| Molecular Biology | PCR, Real-time PCR | Allergen DNA; species-specific sequences | Difficult-to-measure allergens, processed foods | High sensitivity; correlates with protein; detects potential, not actual, allergenicity |
| Mass Spectrometry | LC-MS/MS, MRM | Proteotypic peptides; 0.01 ng/mL sensitivity | Complex matrices, hydrolyzed proteins, method validation | High specificity; absolute quantification; requires specialized expertise |
| Emerging Technologies | Hyperspectral Imaging, Fourier Transform Infrared Spectroscopy, Biosensors | Non-destructive, real-time detection | Processing facilities, rapid screening | Non-destructive; requires validation; limited commercial availability |
Source: Adapted from food allergen analysis literature [7] [18] [20]
A reference measurement system using the mass fraction of total protein from the allergenic ingredient as the primary reference quantity has been proposed to improve comparability across methods and laboratories [20]. This metrology-based approach establishes metrological traceability through primary reference measurement methods, certified reference materials, and reference laboratories, as demonstrated for milk protein in cookies [20].
Variability and Stability of Thresholds
Thresholds demonstrate both inter-individual variability (differences between people) and intra-individual variability (changes within the same person over time). Short-term threshold variation can reach up to 3 logs, though 71.2% of individuals show limited variation within half-log [3]. Multiple factors contribute to this variability:
Cofactors: Exercise and sleep deprivation independently reduce peanut reactivity thresholds by approximately 45%, with sleep deprivation also increasing reaction severity by 48% [3]. Other cofactors include illness, temperature extremes, medications (NSAIDs, beta-blockers), alcohol consumption, and menstruation [3].
Immunologic Status: Underlying mast cell disorders, high-affinity specific IgE concentrations, intestinal permeability, and active immunomodulatory treatments (OIT, omalizumab) influence individual thresholds [3].
Phenotype Considerations: Food allergies demonstrate varying persistence patterns—egg and milk allergies often resolve while peanut, tree nut, and seafood allergies typically persist [3]. These phenotypic differences inform long-term threshold expectations and management strategies.
Despite these variations, thresholds tend toward stability in the short-term, providing a reasonable basis for clinical decision-making when considered alongside individual patient factors [3].
Research Reagents and Materials
The following essential research reagents and materials form the foundation of threshold research and clinical application:
Table 4: Essential Research Reagents for Threshold Studies
| Reagent/Material | Specifications | Research Application | Critical Functions |
|---|---|---|---|
| Food Allergen Reference Materials | Certified reference materials (CRMs) with specified protein content; e.g., NIST peanut butter SRM 2387 | Method calibration, quality control | Provides metrological traceability, ensures analytical accuracy and comparability |
| Allergen-Specific Immunoassays | Validated ELISA kits for major allergens; e.g., RIDASCREEN, Veratox | Food testing, environmental monitoring | Quantifies allergen concentrations in food and environmental samples |
| Mass Spectrometry Standards | Stable isotope-labeled peptide standards for major allergen targets (Ara h 1-6, Bos d 5, Gal d 1-2) | Reference method development, method validation | Enables absolute quantification of specific allergenic proteins via LC-MS/MS |
| Food Challenge Materials | Pharmaceutical-grade allergen powders (e.g., peanut flour) or characterized food sources | Controlled oral food challenges | Provides precise, reproducible dosing for threshold determination |
| Biological Reference Materials | Human serum pools with characterized IgE specificity and concentration | Immunoassay calibration, basophil activation tests | Standardizes IgE detection across platforms and laboratories |
| DNA Extraction and PCR Kits | Validated for complex processed food matrices | Species identification in allergenic foods | Detects allergen sources in difficult matrices where protein detection may fail |
Source: Compiled from analytical methodology literature [18] [20]
Threshold-based approaches have fundamentally transformed food allergy risk assessment and clinical management, replacing universal precaution with evidence-based, personalized strategies. The continued refinement of threshold data, analytical methods, and clinical implementation frameworks supports increasingly precise risk assessment and shared clinical decision-making. Future directions include expanding threshold data for less common allergens, refining understanding of threshold modifiers, developing rapid point-of-care threshold assessment tools, and further harmonizing international regulatory approaches based on population reference doses. As threshold science continues to evolve, it promises to further enhance food safety and quality of life for allergic consumers through increasingly sophisticated risk management frameworks.
The Food Allergen Labeling and Consumer Protection Act of 2004 (FALCPA) represents a cornerstone of U.S. food safety policy, enacted to address the serious public health challenge posed by food allergies [21]. By establishing a standardized framework for declaring major allergens, FALCPA aimed to protect the millions of Americans affected by food allergies by ensuring clear, consistent labeling that enables avoidance of trigger foods. The regulatory landscape continues to evolve, as demonstrated by the recent Food Allergy Safety, Treatment, Education, and Research (FASTER) Act of 2021, which expanded mandatory labeling to include sesame as the ninth major food allergen effective January 1, 2023 [2] [22]. These regulatory developments occur alongside significant advances in the scientific understanding of food allergen thresholds and detection methodologies, creating dynamic interplay between policy, analytical science, and public health protection.
This whitepaper examines the core provisions of FALCPA and the FASTER Act, analyzes recent updates to interpretive guidance, and explores the critical relationship between regulatory frameworks and the scientific research on allergen thresholds and detection limits. For researchers and drug development professionals, understanding these evolving requirements is essential for designing studies, developing analytical methods, and contributing to evidence-based policy refinements that protect allergic consumers while supporting innovation.
Core Legislative Frameworks: FALCPA to FASTER Act
FALCPA: The Foundational Mandate
FALCPA was enacted in response to findings that approximately 2% of adults and 5% of infants and young children in the United States suffered from food allergies, with eight foods or food groups accounting for 90% of all food allergies [21]. The law identified eight "major food allergens": milk, eggs, fish, Crustacean shellfish, tree nuts, peanuts, wheat, and soybeans [2]. FALCPA mandated two primary labeling approaches for declaring these allergens:
- Parenthetical declaration within the ingredient list (e.g., "lecithin (soy)")
- Separate "Contains" statement immediately following the ingredient list (e.g., "Contains wheat, milk, and soy") [2]
The law specifically required that the type of tree nut (e.g., almonds, pecans, walnuts), the species of fish, and the species of Crustacean shellfish be declared, recognizing the variable allergenic potential within these categories [2]. FALCPA's requirements extended to ingredients derived from major food allergens, with limited exceptions such as highly refined oils [21].
The FASTER Act: Expanding Protection to Sesame
The FASTER Act of 2021 marked the first expansion of U.S. food allergen labeling requirements since FALCPA's implementation. Driven by advocacy efforts and evidence that over 1.5 million people in the U.S. are allergic to sesame, with reactions that can be severe or fatal, the law added sesame as the ninth major food allergen [22]. Effective January 1, 2023, sesame must be labeled in the same manner as the original eight major allergens [2] [23].
The FASTER Act also mandated that the Secretary of Health and Human Services report to Congress on food allergy prevalence, severity, and management, establishing a process for considering future modifications to the major allergen list based on emerging science [22]. This provision creates a pathway for potentially adding other emerging allergens as scientific evidence of their public health significance accumulates.
Table 1: Major Food Allergens Under U.S. Law
| Allergen Category | Specific Examples Required | Effective Date |
|---|---|---|
| Milk | Cow, goat, sheep (as of 2025 guidance) | January 1, 2006 |
| Egg | Chicken, duck, quail (as of 2025 guidance) | January 1, 2006 |
| Fish | Bass, flounder, cod (species required) | January 1, 2006 |
| Crustacean Shellfish | Crab, lobster, shrimp (species required) | January 1, 2006 |
| Tree Nuts | Almond, walnut, etc. (12 types as of 2025) | January 1, 2006 |
| Peanuts | January 1, 2006 | |
| Wheat | January 1, 2006 | |
| Soybeans | January 1, 2006 | |
| Sesame | January 1, 2023 |
Recent Regulatory Updates and Refinements
FDA's 2025 Guidance: Revised Tree Nut List and Expanded Definitions
In January 2025, the FDA published the fifth edition of its guidance "Questions and Answers Regarding Food Allergens," implementing significant changes based on stakeholder input and scientific review [24] [25]. These updates reflect the evolving understanding of allergen prevalence and potency:
- Reduced Tree Nut List: The list of tree nuts requiring mandatory allergen labeling was reduced from 23 to 12 types based on a "robust body of scientific evidence" [24] [25]. Coconut, previously a source of confusion for consumers and industry, is no longer considered a major food allergen under the revised guidance [24].
- Expanded "Milk" Definition: The definition now includes milk from domesticated ruminant animals beyond cows, including goats and sheep [24] [25].
- Expanded "Egg" Definition: The definition now includes eggs from various domesticated birds beyond chickens, including ducks, geese, and quail [24] [25].
Table 2: FDA's 2025 Revised Tree Nut List
| Tree Nuts Requiring Labeling | Tree Nuts No Longer Requiring Labeling |
|---|---|
| Almond | Beech nut |
| Black walnut | Butternut |
| Brazil nut | Chestnut |
| California walnut | Chinquapin |
| Cashew | Coconut |
| Filbert (hazelnut) | Ginkgo nut |
| Heartnut (Japanese walnut) | Hickory nut |
| Macadamia nut | Palm nut |
| Pecan | Pili nut |
| Pine nut | Shea nut |
| Pistachio | Cola (kola) nut |
| English and Persian walnut |
Alcohol Beverage Labeling Proposal
In January 2025, the Alcohol and Tobacco Tax and Trade Bureau (TTB) proposed requiring mandatory allergen labeling for wines, distilled spirits, and malt beverages [26]. This proposal would close a long-standing regulatory gap, as these products were previously exempt from FALCPA's mandatory allergen labeling requirements. The proposed compliance date is five years from publication of a final rule [26].
Food Allergen Thresholds and Analytical Detection Methods
The Science of Thresholds and Reactivity
Food allergy thresholds represent the minimum dose of an allergenic protein required to elicit an objective clinical reaction in sensitive individuals. Understanding these thresholds is critical for risk assessment and management. Key research findings include:
- Thresholds and reaction severity are distinct constructs, with only approximately 4.5% of patients reacting to 5 mg of peanut protein experiencing anaphylaxis [3].
- Thresholds demonstrate short-term stability within a half-log variation in 71.2% of individuals, but can be influenced by co-factors such as exercise, sleep deprivation, illness, and medications [3].
- The eliciting dose for 5% of the peanut-allergic population (ED05) has been established at 1.5 mg of peanut protein (approximately 6 mg of whole peanut), providing a scientifically-derived reference point for risk management decisions [3].
Figure 1: Factors Influencing Food Allergen Thresholds and Outcomes
Analytical Methods for Allergen Detection
Validated analytical methods are essential for verifying compliance with allergen labeling requirements and conducting threshold research. The field is evolving from traditional immunoassays toward increasingly sophisticated multiplexed platforms:
- Traditional Methods: Enzyme-linked immunosorbent assays (ELISA) and polymerase chain reaction (PCR) have been widely used but have limitations in scope, specificity, and the ability to detect multiple allergens simultaneously [7].
- Mass Spectrometry: Emerging as a powerful tool for simultaneously quantifying specific proteins (e.g., Ara h 3 and Ara h 6 for peanut; Bos d 5 for milk) with high sensitivity and specificity, even in complex food matrices [7].
- AI-Enhanced Platforms: Hyperspectral imaging (HSI), Fourier Transform Infrared (FTIR) spectroscopy, and computer vision combined with machine learning enable non-destructive, real-time allergen detection without altering food integrity [7].
- Integrated Control Systems: Cloud-based platforms that incorporate adenosine triphosphate (ATP) readings with allergen data provide sanitation verification and predictive risk management through centralized dashboards [7].
Table 3: Analytical Methods for Allergen Detection and Characterization
| Method Category | Specific Technologies | Key Applications in Threshold Research |
|---|---|---|
| Immunoassays | ELISA, Lateral Flow Devices | Quantification of specific allergenic proteins; rapid screening |
| Molecular Biology | PCR, Real-time PCR | Detection of allergen-encoding DNA sequences; species identification |
| Mass Spectrometry | LC-MS/MS, Multiple Reaction Monitoring | Multiplexed protein quantification; detection of proteotypic peptides |
| Spectroscopy | HSI, FTIR, Computer Vision | Non-destructive screening; real-time monitoring in processing facilities |
| Integrated Systems | Cloud-based ATP + Allergen Monitoring | Sanitation verification; predictive risk management |
Research Gaps and Future Directions
The evolving regulatory landscape highlights several critical research needs that represent opportunities for scientific advancement:
- Threshold Standardization: Developing standardized approaches for establishing population thresholds for all major allergens, moving beyond peanut to include tree nuts, sesame, and other emerging allergens [3].
- Matrix Effects: Understanding how food matrices alter allergen bioavailability and reactivity, and incorporating these findings into risk assessment models [3].
- Clinical- Analytical Correlation: Strengthening the relationship between clinically relevant thresholds and analytical detection capabilities to ensure public health protection [7].
- Cofactor Impact: Quantifying the effects of exercise, sleep deprivation, and other cofactors on individual thresholds to improve personalized risk assessment [3].
Figure 2: Research-to-Policy Pipeline for Food Allergen Management
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Materials for Food Allergen Threshold Research
| Research Tool Category | Specific Examples | Research Application |
|---|---|---|
| Reference Materials | Purified native proteins (Ara h 2, Cor a 9, Ses i 1), Certified reference materials | Method calibration, quality control, challenge meal preparation |
| Immunoassay Reagents | Monoclonal/polyclonal antibodies, ELISA kits, Lateral flow devices | Protein quantification, rapid screening, method comparison |
| Mass Spec Standards | Stable isotope-labeled peptides, Tryptic digest standards | Targeted protein quantification, method validation |
| Molecular Biology | Primer/probe sets, DNA extraction kits, Positive control DNA | Allergen source identification, GMO detection |
| Cell-Based Assays | Basophil activation test reagents, Histamine release assay components | Assessment of biological activity, cross-reactivity studies |
The regulatory frameworks established by FALCPA and the FASTER Act have created a dynamic ecosystem where policy evolves in response to scientific advances and public health needs. The 2025 FDA guidance revisions demonstrate this iterative process, refining definitions based on emerging evidence. For researchers and drug development professionals, understanding these frameworks is essential for designing clinically relevant studies and developing detection methods that align with regulatory priorities.
The future of food allergen management lies in strengthening the connection between clinical threshold research, advanced analytical detection capabilities, and evidence-based policy. By addressing critical research gaps in threshold standardization, matrix effects, and cofactor impacts, the scientific community can contribute to more precise, personalized approaches to allergen management that enhance both consumer protection and quality of life for allergic individuals.
Analytical Toolkit: Principles, Workflows, and Applications of Detection Methodologies
The Enzyme-Linked Immunosorbent Assay (ELISA) represents a cornerstone immunological technique for the specific detection and quantification of proteins, playing an indispensable role in food safety and allergen detection research. This plate-based assay leverages the specificity of antigen-antibody interactions, coupled with an enzymatic reaction to generate a measurable signal [27] [28]. Within the context of food allergen research, ELISA provides the foundational analytical sensitivity required to establish thresholds and limits of detection (LOD), which are critical for protecting sensitive individuals while enabling informed risk management [2] [3]. The technique's ability to accurately quantify trace amounts of specific allergenic proteins (e.g., from peanut, milk, or walnut) in complex food matrices makes it a gold standard for compliance with labeling regulations and for the development of evidence-based food safety policies [2] [29].
This guide provides an in-depth examination of ELISA methodologies, from core principles to advanced applications, with a specific focus on their role in quantifying food allergens and determining human eliciting doses. We detail standard and next-generation protocols, data analysis methods for robust quantification, and the direct application of these techniques in setting public health standards for allergen management.
Core Principles and Common ELISA Protocols
Fundamental Mechanism
At its core, ELISA detects the presence of a target molecule (antigen or antibody) by immobilizing it on a solid phase (typically a polystyrene microplate) and then using an enzyme-linked antibody that produces a colorimetric, fluorescent, or chemiluminescent signal upon reaction with a substrate [27] [28]. The key components of any ELISA system include:
- Solid Phase: 96- or 384-well microplates that passively bind proteins [27] [28].
- Capture Molecule: An antibody or antigen coated onto the plate to specifically bind the target.
- Detection Molecule: An enzyme-conjugated antibody that provides the signal.
- Signal Generation System: An enzyme (e.g., Horseradish Peroxidase (HRP) or Alkaline Phosphatase (AP)) and its corresponding substrate (e.g., TMB for HRP) [27].
The relationship between the signal generated (Optical Density, OD) and the target concentration can be positive (in sandwich and indirect ELISA) or negative (in competitive ELISA), depending on the assay format [30].
Common ELISA Formats and Experimental Protocols
The choice of ELISA format depends on the nature of the target analyte and the research objective. The most prevalent formats are detailed below.
Sandwich ELISA
Sandwich ELISA is the most sensitive and specific format for quantifying proteins and is widely used for detecting food allergens [30] [28]. Its protocol is as follows:
Workflow Diagram for Sandwich ELISA
Step-by-Step Protocol:
- Coating: Dilute the specific capture antibody in a carbonate-bicarbonate buffer (pH 9.4) or phosphate-buffered saline (PBS, pH 7.4) to a concentration typically between 2–10 μg/mL. Add 100 μL per well to a 96-well microplate and incubate for several hours to overnight at 4–37°C [28].
- Washing and Blocking: Remove the coating solution and wash the plate 2-3 times with a wash buffer (e.g., PBS with 0.05% Tween 20, PBST). Add 200-300 μL of a blocking buffer (e.g., 1-5% BSA or non-fat dry milk in PBST) to each well to cover all unsaturated binding sites. Incubate for 1-2 hours at room temperature [28].
- Sample and Standard Incubation: Wash the plate. Add 100 μL of the test samples (e.g., food extract) and a serial dilution of the standard antigen (e.g., purified peanut protein) to designated wells. Incubate for 1-2 hours at room temperature to allow the target antigen to be captured [30] [27].
- Detection Antibody Incubation: Wash the plate to remove unbound antigen. Add 100 μL of the enzyme-conjugated detection antibody (specific to a different epitope on the antigen) to each well. Incubate for 1-2 hours at room temperature [30].
- Signal Development: Wash the plate thoroughly to remove unbound detection antibody. Add 100 μL of the enzyme substrate (e.g., TMB for HRP). Incubate in the dark for 15-30 minutes to allow color development [27].
- Signal Measurement: Stop the reaction by adding 50 μL of a stop solution (e.g., 1M H₂SO₄ for TMB). Read the optical density (OD) immediately using a microplate reader at the appropriate wavelength (e.g., 450 nm for TMB) [30] [27].
Competitive ELISA
This format is often used for detecting small molecules, such as certain hormones or chemical contaminants, which may have only a single antibody binding site [30] [28].
Workflow Diagram for Competitive ELISA
Step-by-Step Protocol: The initial coating and blocking steps are similar. The key difference is in step 3: the sample (containing the unknown amount of antigen) is mixed with a fixed, limited concentration of the enzyme-linked antibody before adding it to the antigen-coated plate. The target antigen in the sample and the immobilized antigen on the plate compete for binding to the antibody. After incubation and washing, the subsequent substrate addition and signal detection steps are the same. A higher concentration of antigen in the sample results in less antibody binding to the plate and, therefore, a lower final signal [30] [28].
Indirect ELISA
Indirect ELISA is primarily used for detecting antibodies in a sample, for instance, in serological studies to determine immune response [27].
Protocol: The plate is coated with a specific antigen. After blocking, the test sample (e.g., serum) is added. If present, specific antibodies will bind to the antigen. A secondary, enzyme-conjugated antibody (e.g., anti-human IgG) is then added to detect the bound primary antibody. The signal is developed and measured as described previously [27].
Quantitative Analysis and Data Interpretation
Accurate quantification is a primary strength of ELISA, making it essential for determining allergen thresholds.
Standard Curve and Curve Fitting
Quantification relies on a standard curve generated from known concentrations of a reference standard [30].
- Serial Dilution: Prepare a series of 2-fold to 5-fold dilutions from a high-concentration stock of the purified standard (e.g., peanut protein) in the same matrix as the sample to minimize matrix effects [30].
- Replicates: Run each standard and sample in duplicate or triplicate to ensure consistency and identify pipetting errors [30].
- Background Subtraction: Subtract the average OD value of the blank (zero standard) wells from all other standard and sample readings [30].
- Curve Fitting: Plot the mean adjusted OD (y-axis) against the standard concentration (x-axis, typically log-transformed). The 4-parameter logistic (4PL) model is the most widely used and accurate for fitting the sigmoidal standard curve of an ELISA [30].
The 4-parameter logistic (4PL) equation is: Y = D + (A - D) / (1 + (X / C)^B) Where:
- A = minimum asymptote (background signal)
- D = maximum asymptote (saturation signal)
- C = inflection point (EC50)
- B = slope factor [30]
Calculating Sample Concentrations and Quality Control
- Interpolation: Use the fitted standard curve equation to interpolate the concentration of unknown samples from their adjusted OD values. Ensure sample ODs fall within the range of the standard curve; if not, the sample must be diluted and re-run [30].
- Dilution Factor Correction: Multiply the interpolated concentration by the sample's dilution factor to obtain the original concentration [30].
- Quality Control:
Quantitative Data in Food Allergy Thresholds
ELISA-derived quantitative data on allergen levels in food directly supports clinical research into allergen thresholds. The following table summarizes key quantitative concepts and their relevance.
Table 1: Key Quantitative Concepts in ELISA and Allergen Threshold Research
| Concept | Description | Role in Allergen Threshold Research |
|---|---|---|
| Limit of Detection (LOD) | The lowest concentration of an analyte that can be reliably distinguished from zero [30]. | Determines the lowest level of allergen contamination a method can identify, crucial for detecting trace amounts. |
| Dynamic Range | The concentration interval over which the assay provides accurate quantitative results [30]. | Defines the span of allergen concentrations that can be measured without sample dilution. |
| Eliciting Dose (ED) | The dose of allergenic protein that provokes an allergic reaction in a defined percentage of the population (e.g., ED01, ED05) [29]. | Informs the establishment of reference doses and action levels for precautionary allergen labeling. |
| Coefficient of Variation (CV%) | A measure of assay precision and reproducibility [30]. | Ensures that data on allergen levels in foods are reliable and reproducible across different labs and tests. |
The clinical relevance is clear: studies using oral food challenges have established that, for example, the estimated eliciting doses for walnut protein are 0.8 mg (ED01) and 3.8 mg (ED05) [29]. ELISA is the key laboratory tool that allows regulators and food producers to monitor and ensure that allergen levels in products are below these public health-based thresholds.
The Scientist's Toolkit: Essential Research Reagents and Materials
Setting up a robust ELISA laboratory requires specific materials and reagents. The following table details the essential components.
Table 2: Key Research Reagent Solutions for ELISA
| Item | Function | Key Considerations |
|---|---|---|
| Microplates | Solid phase for immobilizing antigens/antibodies [27] [28]. | Use high-protein-binding polystyrene plates (not tissue culture treated). Clear for colorimetry, black/white for fluorescence/chemiluminescence [28]. |
| Capture & Detection Antibodies | Provide specificity for the target analyte. | For sandwich ELISA, a matched antibody pair against different, non-overlapping epitopes is critical [28]. |
| Enzyme Conjugates | Signal generation. Horseradish Peroxidase (HRP) and Alkaline Phosphatase (AP) are most common [27] [28]. | Conjugated to the detection antibody (direct) or a secondary antibody (indirect). |
| Chromogenic/ECL Substrates | React with the enzyme to produce a measurable signal (color or light) [27]. | TMB is a common chromogen for HRP. Chemiluminescent substrates offer higher sensitivity [28]. |
| Blocking Buffer | Covers unsaturated binding sites on the plate to prevent non-specific adsorption of proteins [28]. | Typically 1-5% BSA or non-fat dry milk in a buffer like PBS. |
| Wash Buffer | Removes unbound reagents between steps to reduce background noise [27]. | Typically PBS or Tris buffer with a detergent like Tween-20 (e.g., PBST). |
| Standard Antigen | Pure form of the target analyte used to generate the standard curve [30]. | Must be highly purified and accurately quantified. Critical for absolute quantification of unknowns. |
| Microplate Reader | Instrument to measure the signal (absorbance, fluorescence, or luminescence) from the plate [27]. | Must be compatible with the plate format and detection method (e.g., 450 nm filter for TMB). |
Advancements and Future Directions in ELISA Technology
While traditional ELISA remains a workhorse, several advanced platforms have emerged to address its limitations, such as moderate sensitivity and single-plexing capability.
- Next-Generation ELISA (ELISA 2.0): These platforms incorporate technologies like digital detection, single-molecule sensing, and nanomaterials to achieve ultra-high sensitivity and multiplexing [31]. The market for these advanced assays is growing at a CAGR of 9.6%, reflecting rapid adoption [31].
- Digital ELISA: This method uses femtoliter-sized chambers to isolate individual enzyme-labeled immunocomplexes on beads, allowing for single-molecule counting. It can improve sensitivity by up to 10,000-fold compared to conventional ELISA, achieving detection limits in the attomolar (aM) range [32].
- Multiplexed Assays (e.g., MSD): Platforms like Meso Scale Discovery (MSD) use electrochemiluminescence to simultaneously detect multiple analytes from a single sample. This provides superior sensitivity and a broader dynamic range than traditional colorimetric ELISA, while also saving time, sample volume, and cost [33].
- Novel Detection Probes: Research continues into innovative probes, such as temperature-responsive liposomes containing fluorescent dyes. These can act as powerful signal amplifiers, with one study demonstrating a limit of detection for PSA as low as 0.97 aM [32].
These advancements are particularly relevant for food allergen research, as they promise even more sensitive detection of trace allergens and the ability to profile multiple allergenic proteins simultaneously in a single, efficient assay.
ELISA stands as a powerful, versatile, and robust technique that is central to the field of food allergen research. Its well-established workflows, combined with rigorous quantitative analysis, generate the reliable data necessary to define allergen thresholds and guide evidence-based food safety regulations. As the field moves forward, the integration of next-generation immunoassay technologies will further enhance our ability to detect and quantify food allergens with unparalleled sensitivity and efficiency, ultimately contributing to improved public health outcomes and a better quality of life for food-allergic individuals.
Quantitative PCR (qPCR) and related DNA amplification techniques represent a cornerstone of modern analytical methods for detecting specific biological targets. Within food safety research, particularly in the context of food allergen thresholds and limits of detection, these techniques provide the sensitivity and specificity required to trace minute amounts of allergen-derived genetic material [34]. Food allergies impact a significant portion of the population, with reactions ranging from mild symptoms to life-threatening anaphylaxis [2]. While the immune response is triggered by proteins, DNA-based detection methods offer a powerful indirect approach for identifying the presence of allergenic foods, as they can detect the genetic signature of an allergenic ingredient even when the protein itself is present in trace amounts [3]. This technical guide explores the core PCR workflows, assesses their applicability for quantifying allergenic proteins indirectly, and details their inherent limitations, providing a framework for their use in advanced food allergen research.
Core Principles of PCR and Quantitative Workflows
Fundamental PCR Technologies
The polymerase chain reaction (PCR) is a laboratory technique for amplifying specific DNA fragments from a small initial sample through repeated cycles of denaturation, annealing, and extension [35]. Quantitative PCR (qPCR), also known as real-time PCR, builds upon this foundation by enabling the monitoring of DNA amplification as it occurs, which allows for the quantification of the initial amount of target DNA [34]. When the target analytes are proteins, such as food allergens, an initial conversion step is required. Reverse Transcription Quantitative PCR (RT-qPCR) is used for RNA targets and involves generating complementary DNA (cDNA) from RNA via reverse transcriptase before proceeding with qPCR amplification [34]. This is particularly useful for studying gene expression, which can be correlated with protein production.
The quantification in qPCR is based on the Cq (Quantification Cycle) value, which is the PCR cycle number at which the sample's fluorescence crosses a predefined threshold [34] [35]. A lower Cq value indicates a higher starting concentration of the target nucleic acid. This relationship is foundational for creating standard curves and performing absolute or relative quantification.
Key PCR Workflow Diagrams
The following diagrams illustrate the logical and procedural relationships in DNA-based detection workflows for allergen analysis.
PCR Workflow for Allergen Detection
LoD Determination Workflow
Experimental Protocols for Detection and Quantification
Establishing Limits of Detection and Quantification
For any diagnostic assay, defining its sensitivity is critical. In the context of food allergen detection, two key performance parameters are the Limit of Detection (LoD) and the Limit of Quantification (LoQ) [36]. The LoD is the lowest amount of analyte that can be detected with a stated probability (typically 95%), while the LoQ is the lowest amount that can be quantified with acceptable accuracy and precision [36]. The following protocol outlines the procedure for determining the LoD for a qPCR assay, a process crucial for validating the sensitivity of an allergen detection method.
Step-by-Step Protocol for Determining LoD in qPCR [37]:
- Create Primary Serial Dilutions: Prepare a dilution series of the target DNA (e.g., a cloned amplicon specific to the allergenic food). Use a 1:10 dilution factor, starting from a concentration known to be detectable (e.g., 1000 copies/reaction) down to a concentration likely below the detection limit (e.g., 1 copy/reaction).
- Initial qPCR Run: Test each dilution in triplicate using the established qPCR protocol. Include a no-template control (NTC) with water to check for contamination.
- Tabulate Initial Results: Record the detection rate (number of positive replicates / total replicates) at each concentration. This identifies the approximate range of the LoD (e.g., between 10 and 100 copies/reaction).
- Create Secondary Dilutions: Perform a finer serial dilution (e.g., 1:2) within the identified range (e.g., from 100 copies/reaction down to ~1.5 copies/reaction).
- High-Replicate qPCR Run: Analyze each of these secondary concentrations in a larger number of replicates (10-20) to build a robust statistical model.
- Calculate the LoD: The LoD is defined as the lowest concentration at which the target is detected in ≥95% of the replicates [37]. For more precise statistical modeling, a logistic regression approach can be applied to the data from the high-replicate experiment to determine the concentration with a 95% detection probability [36].
One-Step vs. Two-Step RT-qPCR
When detecting an allergen by targeting messenger RNA (mRNA), the reverse transcription and amplification steps can be combined or separated. The choice between these protocols depends on the experimental needs.
Table 1: Comparison of One-Step and Two-Step RT-qPCR Protocols
| Feature | One-Step RT-qPCR | Two-Step RT-qPCR |
|---|---|---|
| Procedure | Reverse transcription and PCR amplification occur in a single tube with a unified buffer [34]. | Reverse transcription and PCR amplification are performed in two separate, sequential reactions [34]. |
| Priming | Target-specific; uses one of the PCR primers to prime the reverse transcription [34]. | Uses general primers: oligo(dT) (binds to poly-A tail) or random hexamers (bind across RNA transcript) [34]. |
| Advantages | - Faster, with fewer hands-on steps.- Reduced risk of cross-contamination [34]. | - Flexible; cDNA can be stored and used for multiple different PCR assays.- More efficient for analyzing multiple transcripts from a single RNA sample [34]. |
| Best For | High-throughput studies of a single gene across many samples [34]. | Studies where the same cDNA sample will be used to probe multiple different genetic targets [34]. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of PCR-based allergen detection requires a suite of specialized reagents and instruments. The selection of these components directly impacts the assay's specificity, sensitivity, and reproducibility.
Table 2: Key Research Reagent Solutions for PCR-Based Detection
| Reagent / Material | Function and Importance in Allergen Detection |
|---|---|
| Taq Polymerase | A thermostable DNA polymerase that synthesizes new DNA strands during PCR. Its stability at high temperatures is fundamental to the automated thermal cycling process [35]. |
| Detection Chemistry | SYBR Green: A fluorescent dye that intercalates into double-stranded DNA. It is cost-effective but less specific, as it binds to any dsDNA (including primer-dimers) [34].TaqMan Probes: Sequence-specific fluorogenic probes that provide higher specificity by only emitting a signal when cleaved during amplification of the correct target [34]. |
| Reverse Transcriptase | An enzyme used in RT-qPCR to convert RNA into complementary DNA (cDNA), enabling the detection of RNA targets or the study of gene expression related to allergen production [34]. |
| Sequence-Specific Primers | Short, single-stranded DNA fragments that are designed to be complementary to and flank the target DNA sequence. Their design is critical for the specificity and efficiency of the amplification [34]. |
| Standard Reference Material | Calibrated samples (e.g., genomic DNA with known copy number) used to generate a standard curve for absolute quantification. This is essential for determining the actual amount of allergen-specific DNA in an unknown sample [36]. |
Applicability and Critical Limitations in Protein Quantification
Indirect Measurement and Correlation Challenges
The primary limitation of DNA-based detection for food allergen analysis is that it measures a surrogate marker (DNA/RNA) rather than the actual allergenic protein itself [3]. This indirect approach creates several challenges:
- Variable Gene Expression: The relationship between the number of gene copies (DNA) or mRNA transcripts and the amount of protein produced is not always constant. Factors such as the food source, its growing conditions, and processing can disrupt the correlation between DNA amount and protein abundance [3].
- Differential Impact of Processing: Food processing (e.g., heating, fermentation, high-pressure treatment) affects DNA and proteins differently. Proteins may be denatured, losing their allergenic potential, while DNA, being more stable, may still be detected. This can lead to overestimation of allergen risk. Conversely, some processes may degrade DNA more efficiently than proteins, leading to potential false negatives [3].
Defining and Determining Analytical Thresholds
The concepts of Limit of Blank (LoB) and Limit of Detection (LoD) are fundamental to validating any analytical method, including those for allergen detection.
Table 3: Key Performance Parameters for Detection Assays
| Parameter | Definition | Interpretation in Food Allergen Context |
|---|---|---|
| Limit of Blank (LoB) | The highest apparent analyte concentration expected to be found in replicates of a blank sample (containing no analyte) [36] [38]. | Represents the "noise" level of the assay. A result above the LoB suggests a detection, but confirmation is needed. |
| Limit of Detection (LoD) | The lowest true concentration of the analyte at which the detection is probable (typically ≥95% of the time) [36] [37] [38]. | The lowest amount of allergen-specific DNA that the assay can reliably detect. It is always greater than the LoB. |
| Limit of Quantification (LoQ) | The lowest concentration at which the analyte can not only be detected but also measured with acceptable precision and accuracy [36]. | The lowest amount of allergen-specific DNA that can be reliably quantified. This is crucial for threshold-based risk assessments. |
Determining these limits for qPCR is complicated by its logarithmic output (Cq values). Standard methods for calculating LoB and LoD, which assume a linear, normally distributed response, are not directly applicable. Instead, methods involving multiple replicates at low concentrations and probabilistic models (like logistic regression) must be employed [36].
Technical and Practical Constraints
- Extreme Sensitivity to Contamination: The power of PCR to amplify trace amounts of DNA makes it highly susceptible to false positives from laboratory contamination, requiring stringent laboratory practices and segregated workspaces [35].
- Inhibition and Interference: Substances commonly found in complex food matrices (e.g., polyphenols, polysaccharides, fats, and certain salts) can inhibit the PCR reaction, leading to reduced efficiency or false-negative results [35]. Extensive sample cleanup and the use of internal controls are necessary to overcome this.
- Complex Result Interpretation: While qPCR provides a quantitative Cq value, translating this into a meaningful and accurate concentration of allergenic protein remains a significant hurdle. It requires a well-validated standard curve and an understanding of the relationship between the DNA target and the protein of interest in the specific food matrix being tested [35].
DNA-based detection methods, particularly qPCR and RT-qPCR, offer unparalleled sensitivity and specificity for identifying the genetic material of allergenic foods, making them indispensable tools in the food safety researcher's arsenal. Their ability to detect trace amounts of allergen-specific DNA is critical for compliance with labeling regulations and for protecting sensitive individuals. However, their application in the context of protein quantification is inherently indirect and is fraught with challenges related to variable biological correlations and matrix effects. A thorough understanding of PCR workflows, coupled with rigorous validation of performance parameters like LoD and LoQ, is essential for generating reliable data. Future advancements will likely focus on better correlating DNA markers with protein allergenicity and integrating these methods with direct protein detection platforms to provide a more comprehensive risk assessment strategy.
Food allergies represent a significant and growing global public health concern, impacting an estimated 1 in 10 adults and 1 in 13 children [3]. For affected individuals, exposure to specific allergenic proteins can trigger reactions ranging from mild symptoms to severe, life-threatening anaphylaxis. As there is currently no cure, the cornerstone of management remains strict avoidance of allergenic foods, making accurate food labeling a critical necessity [2] [39]. This public health imperative drives the need for highly sensitive and specific analytical methods to detect and quantify trace amounts of allergens in complex food matrices.
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) has emerged as a powerful confirmatory technique for food allergen analysis, overcoming several limitations associated with traditional methods like Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR). While ELISA can suffer from antibody cross-reactivity and PCR provides only indirect detection via DNA, LC-MS/MS enables the direct, multiplexed analysis of allergenic proteins through their characteristic peptide signatures [40] [39]. This technical guide explores the application of targeted LC-MS/MS, specifically using Multiple Reaction Monitoring (MRM), for the precise quantification of allergen-derived peptides within challenging food samples, framing this methodology within essential research on food allergen thresholds and limits of detection.
Core Principles: LC-MS/MS and Multiple Reaction Monitoring (MRM)
In the context of food allergen analysis, LC-MS/MS functions by detecting and quantifying specific peptide sequences that are unique surrogates for the parent allergenic protein. The analytical process involves several key stages: (1) extraction of proteins from the food matrix, (2) enzymatic digestion of proteins into peptides, (3) chromatographic separation of peptides, (4) ionization of peptides, and (5) mass spectrometric detection and quantification [40] [41].
The MRM technique on a triple quadrupole mass spectrometer is the cornerstone of robust quantification. In the first quadrupole (Q1), a specific precursor ion (the peptide ion) is selected. This ion is then fragmented in the second quadrupole (Q2, the collision cell), and a specific, characteristic product ion is selected in the third quadrupole (Q3) for detection. Monitoring a unique peptide ion and its fragment ion provides two stages of mass selectivity, resulting in high specificity and significantly reduced chemical noise [42] [41]. To further maximize confidence, it is standard practice to monitor two or three MRM transitions per peptide [41]. The ratio of these transitions should be consistent between the authentic standard and the sample, providing a confirmatory parameter. The high specificity of MRM allows for accurate quantification even in the presence of co-eluting interferences from complex food matrices such as chocolate, spices, or cooked meats [43].
Critical Methodological Components
Signature Peptide Selection
The selection of appropriate signature peptides is the most critical step in developing a robust LC-MS/MS method. These peptides must be unique to the target allergenic protein and not present in any other proteins within the sample matrix. Key selection criteria include:
- Unique Amino Acid Sequence: The peptide must be a unique identifier for the allergenic source. For instance, a method for livestock meat allergens selected peptides from myoglobin and myosin light chain as quantitative markers for beef, lamb, pork, chicken, and duck [42].
- Stability and Detectability: Peptides should be resistant to modifications during food processing (e.g., Maillard reaction) and should ionize efficiently under ESI conditions [41].
- Absence of Post-Translational Modifications: Peptides with labile modification sites (e.g., deamidation) are generally avoided to ensure consistent quantification.
- Length: Peptides between 8 and 20 amino acids are typically ideal, as they are long enough to be unique and fragment predictably.
Bioinformatics tools and protein databases are used for initial in silico selection, which is then verified empirically by analyzing digests of the pure allergen [41].
Comprehensive Sample Preparation Protocol
Proper sample preparation is vital for achieving high sensitivity and accuracy. A typical, rugged protocol for a complex, baked food matrix is detailed below [41]:
- Homogenization: The food sample (1 g) is finely ground to ensure a representative aliquot.
- Defatting (if needed): For fatty matrices like nuts or chocolate, the homogenate is extracted twice with hexane and dried by evaporation to remove interfering lipids.
- Protein Extraction: The defatted pellet is mixed with an extraction buffer (e.g., 4 mL) designed to solubilize proteins. Buffers often contain denaturants like urea and reducing agents like dithiothreitol (DTT) to break disulfide bonds.
- Reduction and Alkylation: The protein extract is reduced with DTT (e.g., 50 µL at 60°C for 1 hour) to break disulfide bonds and then alkylated with a reagent like iodoacetamide (e.g., 25 µL at room temperature in the dark) to prevent reformation. This step is critical for consistent enzymatic digestion.
- Enzymatic Digestion: Trypsin (e.g., 20 µg) is added to the modified proteins and incubated for several hours (e.g., 3-12 hours) at 37°C to cleave proteins into peptides at the C-terminal side of lysine and arginine residues.
- Digestion Quenching: The reaction is neutralized with acid (e.g., 30 µL of formic acid).
- Clean-up: The digested sample is centrifugally filtered using a molecular weight cut-off filter (e.g., 10 kDa) to remove large particulates and undigested proteins. Solid-phase extraction (SPE) may also be employed to further purify and concentrate the peptide mixture, which is crucial for achieving low limits of detection [40].
LC-MS/MS Instrumental Analysis
- Liquid Chromatography: Tryptic peptides (e.g., 30 µL injection volume) are separated using a reversed-phase C18 column (e.g., Phenomenex Kinetex C18, 2.6 µm, 100 x 3 mm) with a fast, linear gradient (e.g., over 12 minutes) of water and acetonitrile, both modified with 0.1% formic acid to enhance ionization [41].
- Mass Spectrometry Detection: A triple quadrupole mass spectrometer is used in positive electrospray ionization (ESI+) mode. The Scheduled MRM algorithm is highly recommended for methods monitoring many transitions. It monitors each MRM transition only around its expected retention time, allowing a sufficient number of data points across each peak while maintaining a high number of concurrent MRM measurements. Key instrument parameters include an ion source temperature of 500°C and optimized compound-dependent parameters like collision energy [41].
Performance Data and Allergen Threshold Context
Method validation is essential to demonstrate sensitivity, accuracy, and precision. The following table summarizes typical validation parameters and performance data from recent LC-MS/MS methods for allergen detection.
Table 1: Analytical Performance of LC-MS/MS Methods for Food Allergen Detection
| Allergen Category / Source | Target Proteins / Peptides | Limit of Detection (LOD) | Limit of Quantification (LOQ) | Recovery (%) | Precision (RSD%) |
|---|---|---|---|---|---|
| Livestock & Poultry Meat [42] | Myoglobin, Myosin Light Chain (5 peptides) | 2.0–5.0 mg/kg | 5.0–10.0 mg/kg | 80.2–101.5% | < 13.8% |
| Pistachio [43] | Pis v 1, Pis v 2, Pis v 3, Pis v 4, Pis v 5 | SDL* = 1 mg/kg | N/R | N/R | Good reproducibility |
| Multi-Allergen Screening (12 allergens) [41] | Various (44 signature peptides) | ~10 ppm (10 mg/kg) | N/R | N/R | High linearity (R² > 0.95) |
SDL: Screening Detection Limit; N/R: Not explicitly reported in the sourced context.
The sensitivity of modern LC-MS/MS methods aligns closely with the emerging understanding of clinical threshold doses, which are the amounts of an allergenic protein required to elicit a reaction in sensitive individuals. These thresholds are critical for risk assessment and informing regulatory action levels. The following table lists reference doses for common allergens, providing context for the clinical relevance of the LODs achieved by analytical methods.
Table 2: Clinical Threshold Doses for Common Food Allergens [44]
| Food Allergen | ED01 (mg of protein) | ED05 (mg of protein) |
|---|---|---|
| Walnut | 0.03 | 0.08 |
| Cashew | 0.05 | 0.80 |
| Peanut | 0.20 | 2.10 |
| Egg | 0.20 | 2.30 |
| Milk | 0.20 | 2.40 |
| Hazelnut | 0.10 | 3.50 |
ED01: Eliciting Dose for 1% of the allergic population; ED05: Eliciting Dose for 5% of the allergic population.
It is important to note that thresholds and reaction severity are distinct constructs and can be influenced by co-factors such as exercise, sleep deprivation, and illness [3]. Furthermore, as of January 2025, the U.S. Food and Drug Administration (FDA) has not established a regulatory threshold for any food allergens, though the agency is actively exploring the application of risk-based thresholds through stakeholder meetings and scientific review [2] [45].
Experimental Workflow and Signaling Pathways
The entire process from sample to result can be visualized as a sequential workflow. The following diagram illustrates the key stages of the LC-MS/MS method for targeted peptide analysis in food allergens.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of an LC-MS/MS allergen method requires carefully selected reagents and materials. The following table details key components and their functions.
Table 3: Essential Research Reagent Solutions for LC-MS/MS Allergen Analysis
| Reagent / Material | Function / Purpose | Example from Literature |
|---|---|---|
| Extraction Buffer | Solubilizes and denatures proteins from the complex food matrix. | Ammonium bicarbonate buffer with urea and dithiothreitol (DTT) [42] [40]. |
| Reducing Agent | Breaks disulfide bonds in proteins to unfold the structure for digestion. | Dithiothreitol (DTT) [42] [41]. |
| Alkylating Agent | Modifies cysteine residues to prevent reformation of disulfide bonds. | Iodoacetamide (IAA) [42] [41]. |
| Protease (Enzyme) | Cleaves proteins into predictable peptides for mass spectrometry analysis. | Sequencing-grade trypsin [42] [41]. |
| Stable Isotope-Labeled Peptides | Internal standards for precise quantification, correcting for matrix effects and recovery losses. | Added before or after digestion, depending on the standard design [42] [43]. |
| Solid-Phase Extraction (SPE) Cartridges | Purifies and concentrates the peptide digest, removing salts and other interferents. | Strata-X or similar reversed-phase cartridges [40]. |
| LC Column | Chromatographically separates peptides prior to mass spec introduction. | Phenomenex Kinetex C18 column [41]. |
LC-MS/MS has firmly established itself as a confirmatory, multiplexed, and highly specific platform for the detection and quantification of food allergens. By targeting signature peptides, this technology overcomes the cross-reactivity limitations of ELISA and the indirect nature of PCR, providing direct evidence of the presence of an allergenic protein. As research continues to refine clinical thresholds for the major allergens, the sensitivity and robustness of LC-MS/MS methods will play an indispensable role in validating these safety levels. This will empower regulatory bodies to make science-based decisions and ultimately enhance consumer protection for the millions of individuals managing food allergies worldwide. Future developments will likely focus on expanding multiplexing capabilities, standardizing methods across laboratories, and further improving throughput and accessibility for routine food safety monitoring.
The accurate detection and quantification of food allergens is a critical public health priority, driven by the increasing global prevalence of food allergies [46]. For sensitized individuals, strict avoidance is the primary management strategy, making reliable food labeling and effective sanitation protocols essential components of food safety programs [46] [2]. The foundation of these efforts lies in understanding food allergen thresholds—the lowest dose of an allergen that can elicit an adverse reaction in a sensitized individual—and the limits of detection (LOD) of the analytical methods used to detect them [3]. This guide details three emerging and rapid methodologies—Lateral Flow Devices (LFDs), Adenosine Triphosphate (ATP) and A3 monitoring, and AI-Enhanced Diagnostics—that are transforming how researchers and the food industry approach allergen detection and risk assessment.
Lateral Flow Devices (LFDs) for Allergen Detection
Principles and Technology
Lateral Flow Devices (LFDs), also known as immunochromatographic strip tests, are rapid, on-site screening tools based on sandwich immunoassay principles [47] [48]. They are designed for the specific detection of allergenic proteins. The core mechanism involves the capillary migration of a liquid sample along a nitrocellulose membrane, where it encounters antibodies conjugated to colored particles (typically colloidal gold or latex) [47]. If the target allergen is present in the sample, it forms a complex with these conjugated antibodies. This complex continues to flow along the strip until it is captured by a second, fixed antibody at the Test Line, producing a visible signal [47]. A Control Line confirms that the test has functioned correctly [48].
Key performance features of modern LFDs include:
- Speed: Results are typically available within 5-15 minutes [47] [48].
- Portability: Compact and user-friendly design enables testing in processing environments without sophisticated lab infrastructure [49] [48].
- Hook Effect Mitigation: Some advanced LFDs incorporate a "hook line" to prevent false-negative results that can occur at extremely high allergen concentrations due to the prozone effect [47].
Experimental Protocol for Surface Sampling and Testing
Objective: To verify the removal of allergenic residue from food contact surfaces after cleaning. Materials: LFD test kit (including test strips, extraction buffer, and swabs), timer, and a portable reader (for semi-quantitative analysis) [49] [47].
Procedure:
- Sample Collection: Use a sterile swab provided in the kit. Moisten the swab with the appropriate extraction buffer and thoroughly swab a defined surface area (e.g., 10 cm x 10 cm) [49].
- Sample Elution: Place the swab back into the tube containing extraction buffer. Agitate vigorously to elute any residual protein from the swab into the buffer [47].
- Test Execution: Remove the LFD test strip from its protective pouch. Dip the sample pad end of the strip into the extracted solution. Alternatively, apply a specified number of drops to the sample window using the provided dropper [47] [48].
- Incubation and Development: Allow the test to develop at room temperature for the time specified by the manufacturer (usually 5-15 minutes). Do not read results after the designated time [48].
- Result Interpretation:
- (Optional) Semi-Quantitative Analysis: Use a portable reader to scan the test strip. This provides a quantitative measurement of signal intensity, offering a more objective result than visual inspection [47].
Performance Data and Limitations
Table 1: Comparison of Detection Limits for Selected Allergenic Foods via LFD and Other Methods
| Allergenic Food | LFD | A3 Test | Protein Swab | Conventional ATP Test |
|---|---|---|---|---|
| Peanut | Very High Sensitivity [50] | Variable | Lower than A3 [50] | Lower than A3 [50] |
| Crustacean Shellfish | Good Sensitivity | Comparable or better than LFD for some [50] | Lower than A3 [50] | Lower than A3 [50] |
| Processed Grains | Good Sensitivity | Comparable to LFD for some [50] | Lower than A3 [50] | Lower than A3 [50] |
| Wheat Flour | Good Sensitivity | Lower than LFD [50] | Lower than A3 [50] | Lower than A3 [50] |
Limitations of LFDs include their primarily qualitative (positive/negative) output, though readers are adding quantification. Test performance can be matrix-dependent, and the method may not detect allergens that have been extensively hydrolyzed or denatured by processing, as the antibody may no longer recognize the altered protein structure [49] [51].
ATP (A3) Monitoring for Hygiene Verification
Principles and Technology
Adenosine Triphosphate (ATP) monitoring is a well-established hygiene verification technique that provides a rapid, indirect assessment of surface cleanliness. ATP is a universal energy molecule found in all living cells, including bacteria, yeast, mold, and food residues [52]. The A3 test is an advanced form that detects not only ATP but also its breakdown products, Adenosine Diphosphate (ADP) and Adenosine Monophosphate (AMP). This is crucial because many food materials contain significant amounts of ADP and AMP, especially after ATP degrades during processing or storage, making the A3 test more sensitive for detecting food debris than conventional ATP tests [50].
The detection is based on a bioluminescence reaction. The enzyme luciferase, in the presence of ATP (and converted ADP/AMP), catalyzes the oxidation of luciferin, producing light [52]. The amount of light produced, measured in Relative Light Units (RLU) by a device called a luminometer, is proportional to the amount of these nucleotides present, and thus to the level of organic contamination on a surface [50] [52].
Experimental Protocol for Cleaning Validation
Objective: To validate the effectiveness of a cleaning procedure in removing allergenic food residue from processing equipment. Materials: A3 or ATP monitoring system (including luminometer and specialized swabs), sanitizer, and cleaning tools [52].
Procedure:
- Pre-Cleaning Baseline (Optional): Perform a test on the equipment surface before cleaning to establish a baseline contamination level.
- Cleaning and Sanitation: Execute the standard cleaning and sanitation procedure for the equipment.
- Sampling:
- Activate the swab according to the manufacturer's instructions, typically by inserting it into a pre-filled reagent tube [52].
- Firmly swab a defined area of the food contact surface (e.g., 10 cm x 10 cm or a specific equipment part), using a criss-cross pattern while rotating the swab to cover the entire area [52].
- Measurement:
- Re-insert the swab into the reagent tube and activate it to release the reagent.
- Place the swab tube into the luminometer and initiate the reading.
- Record the RLU value displayed on the luminometer [52].
- Interpretation and Action:
- Compare the RLU value to pre-established pass/fail thresholds for that specific surface and product. These thresholds are set during initial validation studies [52].
- Pass: RLU value is below the threshold. Production can commence.
- Fail: RLU value exceeds the threshold. The surface must be recleaned and retested before production begins [52].
Performance Data and Role in Allergen Control
Table 2: Detection Capabilities of Hygiene Monitoring Methods
| Method | Target | Key Strength | Key Limitation in Allergen Context |
|---|---|---|---|
| A3 Test | ATP, ADP, AMP (General organic residue) | Rapid, broad-spectrum, cost-effective; detects foods low in ATP [50] | Not allergen-specific; result does not confirm presence/absence of a specific allergen [49] [50] |
| Conventional ATP Test | ATP only | Rapid, indicates viable cell presence [52] | Misses many allergenic foods low in ATP [50] |
| Protein Swab | General protein | Low cost, rapid colorimetric result [49] | Not allergen-specific; color interpretation can be subjective [49] |
| LFD | Specific allergenic protein | High specificity and sensitivity for target allergen [50] | Specific to a single allergen; may be affected by food processing [49] |
While not allergen-specific, the A3 test is highly effective as an initial screening tool. It can detect the risk of allergen cross-contact resulting from inadequate cleaning, as the presence of general food residue indicates a potential for allergen presence [50]. A field study demonstrated that A3 levels correlated with specific allergen protein (e.g., milk) concentrations measured by ELISA throughout the cleaning process [50].
AI-Enhanced Diagnostics and Predictive Analytics
Principles and Technology
Artificial Intelligence (AI), particularly machine learning and predictive modeling, is emerging as a transformative tool in food allergy diagnostics and management. These systems analyze complex, multi-dimensional datasets to predict individual patient outcomes and personalize treatment strategies [53]. The underlying principle involves training algorithms on vast datasets that include immunological markers (e.g., specific IgE levels), clinical history, component-resolved diagnostics, protein structure data, and outcomes from previous patients [53]. These models identify hidden patterns and correlations that are difficult for humans to discern, enabling them to forecast an individual's risk of reacting to a specific allergen dose and to predict their likely reaction severity [3] [53].
Application in Clinical Protocols: Predicting Thresholds and Personalizing Immunotherapy
Objective: To utilize AI models for safer, more personalized food allergy management without relying solely on high-risk oral food challenges (OFCs).
Protocol Workflow:
- Data Ingestion: Collect comprehensive patient data, including:
- Model Analysis: The AI algorithm processes this data against its trained model of protein structures and historical patient outcomes to generate predictive insights [53].
- Output and Clinical Decision Support:
- Threshold Prediction: The model estimates a patient's individual eliciting dose (ED) for an allergen, effectively predicting their threshold [53]. This can stratify patients into risk categories (e.g., those with high vs. low thresholds) [3].
- Treatment Personalization: For patients undergoing Oral Immunotherapy (OIT), the AI model can recommend a personalized starting dose and dose escalation schedule, minimizing the risk of severe reactions during treatment [53]. Studies have shown the feasibility of using threshold data to guide home-based OIT induction [3].
- Risk Stratification: Models can identify patients at higher risk of severe reactions based on a combination of factors, allowing for tailored management plans [53].
This data-driven approach shifts the paradigm from reactive, one-size-fits-all protocols using OFCs to proactive, precision medicine that enhances patient safety [53].
Performance and Future Directions
AI models demonstrate significant potential. For instance, predictive models are being used to eliminate the need for traditional food challenges in some patients, thereby avoiding unnecessary risk [53]. Furthermore, understanding that thresholds are dynamic and can be lowered by co-factors like exercise or sleep deprivation is a complex variable that AI models are well-suited to incorporate [3]. The future of AI in this field involves continuous model refinement with real-world data, expansion to include more allergens, and integration with other 'omics' data for even greater predictive accuracy [53].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Allergen Detection and Diagnostics
| Reagent / Material | Function | Application Context |
|---|---|---|
| Monoclonal Antibodies | Highly specific antibodies that bind to a single epitope on a target allergenic protein. | Used in ELISA and LFD development to minimize cross-reactivity and ensure precise detection of specific allergen markers (e.g., casein in milk) [47] [51]. |
| Polyclonal Antibodies | A mixture of antibodies that recognize multiple epitopes on a target protein. | Used in ELISA kits for processed foods, where proteins may be denatured, increasing the likelihood of detecting fragmented allergens [51]. |
| Luciferin-Luciferase Enzyme Complex | Key reagents in the bioluminescence reaction that detects ATP/ADP/AMP. | The core component of ATP and A3 monitoring swabs; produces light signal proportional to nucleotide concentration [52]. |
| Protein Extraction Buffers | Chemical solutions designed to solubilize and release proteins from complex food matrices. | Critical first step in ELISA, LFD, and MS protocols; efficiency directly impacts detection sensitivity, especially for challenging matrices like chocolate or meat [49] [47]. |
| Unique Peptide Markers | Synthesized peptide sequences that are unique to a specific allergenic protein. | Serve as reference standards and targets for Mass Spectrometry (MS) methods, enabling highly specific and multiplexed allergen detection [51]. |
| Immunological Assay Kits (ELISA) | Complete kits containing pre-coated plates, antibodies, buffers, and substrates. | Gold standard for quantitative allergen detection in the laboratory; used for validating other methods and for final product verification [49] [47]. |
The fields of food allergen detection and diagnostics are advancing rapidly, moving beyond traditional laboratory-based methods. Lateral Flow Devices offer rapid, on-site screening capabilities crucial for routine monitoring and cleaning verification. ATP (A3) monitoring provides a nonspecific but highly effective and immediate assessment of general hygiene, which is a prerequisite for effective allergen control. Finally, AI-enhanced diagnostics represent a paradigm shift towards precision medicine, using predictive analytics to understand individual thresholds and personalize management strategies, thereby reducing patient risk and improving quality of life. Together, these emerging and rapid methods provide a powerful, multi-layered toolkit for researchers and clinicians dedicated to advancing food safety and patient care in the context of food allergies.
Navigating Analytical Challenges: Matrix Effects, Processing, and Cross-Reactivity
Food processing induces complex structural modifications in proteins that significantly impact allergen detection and immunoreactivity. Techniques such as thermal treatment, enzymatic hydrolysis, and high-pressure processing can denature proteins, degrade epitopes, or mask allergenic components, complicating analytical detection. This whitepaper examines the interplay between processing methodologies and the efficacy of major allergen detection platforms, including immunoassays, mass spectrometry, and molecular techniques. Within the broader context of food allergen threshold and limit of detection research, we synthesize experimental data on detection limits, provide detailed protocols for key methodologies, and outline critical reagent solutions. The convergence of processing-induced changes and detection capabilities presents a substantial challenge for accurate risk assessment, underscoring need for integrated approaches in regulatory and safety frameworks.
The accurate detection and quantification of food allergens is a cornerstone of public health policy and clinical management. This process is profoundly complicated by the fact that most foods are processed prior to consumption. Processing methodologies—ranging from thermal applications to enzymatic hydrolysis—induce structural and conformational changes in allergenic proteins [54] [55]. These alterations can destroy, create, or mask the epitopes recognized by antibodies in immunoassays or the target peptides analyzed in mass spectrometry, thereby directly impacting the reported allergen levels [44]. Consequently, a deep understanding of how processing affects both allergenicity and detectability is paramount for establishing meaningful allergen thresholds and limits of detection (LOD). This technical guide explores these intricate interactions, providing researchers and drug development professionals with a detailed analysis of the challenges and state-of-the-art solutions in this critical field.
Food Processing Technologies and Allergenic Protein Modification
Food processing technologies are broadly categorized into thermal, non-thermal, and biological methods. Each mechanism exerts distinct effects on protein structure, influencing both allergenic potential and analytical detectability.
Thermal Processing
Thermal processing is among the most common methods, with effects ranging from mild denaturation to extensive aggregation.
- Mechanisms of Epitope Modification: Heat treatment leads to the sequential loss of tertiary (55–70°C) and secondary (70–80°C) protein structure, rupture of disulfide bonds (80–90°C), and formation of aggregates (90–100°C) [55]. These changes primarily disrupt conformational epitopes, which are dependent on the native protein fold. In contrast, linear epitopes, comprised of continuous amino acid sequences, often remain intact unless the protein is extensively hydrolyzed [56]. However, heating can also expose previously hidden linear epitopes, potentially increasing immunoreactivity in certain cases [55].
- Variable Effects by Food Matrix: The impact of heat is highly variable. For instance, ovomucoid in egg white is highly heat-stable, whereas ovalbumin is more labile [55]. In peanuts, dry roasting (baking) can increase the allergenic potential of Ara h 1 and Ara h 2 by up to 90% due to protein aggregation, while boiling or frying may slightly reduce it [55]. Casein in milk, lacking a defined tertiary structure, is largely unaffected by heat, while β-lactoglobulin sees its IgG-binding capacity altered [55].
Non-Thermal Physical Processing
Emerging non-thermal technologies offer alternatives that minimize thermal degradation while effectively modifying allergens.
- High Hydrostatic Pressure (HHP): HHP, especially when combined with moderate heat, can induce protein denaturation and unfolding, potentially disrupting conformational epitopes [56].
- Cold Plasma (CP): CP technology generates reactive oxygen and nitrogen species that oxidize amino acid side chains, leading to protein cross-linking and aggregation, which can reduce IgE binding [56].
- Pulsed Electric Fields (PEF) and Ultrasound (UT): These methods can cause protein denaturation and the exposure of hydrophobic groups, altering their immunoreactive profile [56] [44].
Biological and Chemical Processing
- Enzymatic Hydrolysis: This is one of the most effective industrial methods for reducing allergenicity. Proteases cleave peptide bonds, destroying conformational and linear epitopes. However, incomplete hydrolysis can generate peptides that retain allergenic activity or form new allergenic aggregates [54] [55]. The efficacy depends on the enzyme specificity and the accessibility of cleavage sites within the protein structure.
- Fermentation: Microbial metabolism during fermentation can degrade allergenic proteins or alter the food matrix, reducing immunoreactivity. It is considered, alongside hydrolysis, as having the highest potential to effectively reduce allergenicity [54].
The following diagram illustrates how different processing methods target protein structures and influence epitope availability.
Diagram 1: Impact of Food Processing on Protein Epitopes. Processing methods denature, fragment, or aggregate proteins, thereby destroying, exposing, or masking allergenic epitopes and directly impacting detection.
Analytical Detection Platforms and Processing Interference
The choice of detection platform is critical, as its susceptibility to processing-induced changes varies significantly. No single method is universally reliable for all processed foods.
Immunoassays (e.g., ELISA)
Immunoassays are widely used but are highly susceptible to structural changes in proteins.
- Principle and Vulnerability: These assays rely on antibodies binding to specific epitopes (either conformational or linear) on the target protein [44] [57]. Processing that denatures the protein can destroy the antibody's target epitope, leading to false negatives [44]. Conversely, unfolding can expose previously hidden epitopes, potentially causing overestimation.
- Matrix Effects and Cross-Reactivity: Components in complex, processed food matrices can interfere with antibody binding, and antibodies may cross-react with structurally similar, non-target proteins, compromising specificity [57].
DNA-Based Methods (e.g., Real-Time PCR)
DNA-based methods target allergen source genes rather than proteins themselves.
- Principle and Advantages: Techniques like TaqMan real-time PCR amplify species-specific DNA sequences, allowing detection of allergens from nuts, sesame, and other sources with high sensitivity (LODs as low as 0.1 mg/kg) [58]. DNA is generally more stable to thermal processing than protein conformation.
- Key Limitation: There is no direct correlation between the amount of detected DNA and the concentration of the allergenic protein. A negative PCR result does not guarantee the absence of the allergenic protein, especially in highly refined products like oils where DNA may be removed [58].
Mass Spectrometry (MS)
MS is emerging as a highly precise and reliable technique for allergen detection.
- Principle: MS detects and quantifies specific "proteotypic" peptides that are unique to the allergenic protein [7] [44]. Since it targets a peptide's mass-to-charge ratio, it is less affected by protein conformation.
- Advantages: MS can achieve multiplexing (simultaneous quantification of multiple allergens like Ara h 3, Ara h 6, Gal d 1, etc.), high specificity, and sensitivity (detection limits as low as 0.01 ng/mL have been reported) [7]. It is considered the "gold standard" for accurate quantification in complex matrices.
Emerging and Rapid Techniques
- Aptamer-Based Biosensors: Aptamers are synthetic oligonucleotides selected for high affinity to specific targets. They offer advantages over antibodies, including superior stability and lower production costs. They can be integrated into electrochemical and optical sensors for rapid, on-site detection [57].
- ATP+Adenylate (A3) Tests: Traditionally used for hygiene monitoring, A3 tests detect adenosine triphosphate and its degradation products. They are a non-specific but rapid and effective screening tool for detecting food residue that may contain allergens, with performance often surpassing conventional protein swab tests [50].
Table 1: Comparison of Major Allergen Detection Platforms
| Detection Platform | Target | Key Advantage | Key Disadvantage | Impact of Processing |
|---|---|---|---|---|
| Immunoassay (ELISA) | Protein Epitopes | High specificity for native protein; Widely available | Antibody binding dependent on protein structure | High - Denaturation can cause false negatives/positives |
| Real-Time PCR | Species-specific DNA | Highly sensitive and specific; DNA is thermally stable | No direct correlation with protein concentration | Low to Moderate - DNA degradation in harsh processes |
| Mass Spectrometry | Proteotypic Peptides | Unaffected by protein conformation; Multiplexing capability | High equipment cost; Requires expertise | Low - Targets stable peptide sequences |
| Aptamer-Based Sensors | Protein Structure | High stability; Cost-effective; Rapid | Relatively new technology; Limited commercial kits | Moderate - Dependent on aptamer target site |
| Adenylate (A3) Test | ATP/ADP/AMP | Rapid, non-specific hygiene screening | Does not identify specific allergen | Indirect - Correlates with residual food debris |
Table 2: Experimentally Determined Detection Limits for Various Allergens and Methods
| Allergen/Food | Detection Method | Reported Detection Limit | Context / Notes | Source |
|---|---|---|---|---|
| Various Nuts | TaqMan Real-Time PCR | 0.1 mg/kg | Peanut, hazelnut, pistachio, almond, etc. | [58] |
| Multiple Allergens | Mass Spectrometry | 0.01 ng/mL | Can target specific proteins (e.g., Ara h 3, Bos d 5) | [7] |
| Food Residues | A3 (ATP+ADP+AMP) Test | Varies by food | More sensitive than conventional ATP test for many foods | [50] |
Experimental Protocols for Key Detection Methodologies
This protocol is designed for the specific detection of nut DNA in complex food products.
Sample Preparation and DNA Extraction:
- Homogenize 200 mg of the food sample.
- Extract genomic DNA using a commercial kit suitable for processed foods (e.g., with silica-membrane technology). Include steps for removing potential PCR inhibitors like polysaccharides and polyphenols.
- Quantify the extracted DNA using UV spectrophotometry and adjust to a working concentration (e.g., 10 ng/μL).
Primer and Probe Design:
- Design species-specific primer pairs and TaqMan probes to target the plant Internal Transcribed Spacer (ITS) region.
- Dual-label the TaqMan probe with a reporter fluorophore (e.g., 6-carboxyfluorescein, FAM) at the 5' end and a quencher fluorophore (e.g., Blackberry, BBQ) at the 3' end.
Real-Time PCR Amplification:
- Prepare a 25 μL reaction mixture containing: 1X TaqMan Master Mix, 300 nM of each primer, 200 nM of the TaqMan probe, and 5 μL of template DNA.
- Perform amplification in a real-time PCR cycler with the following thermal profile:
- Hold: 95°C for 10 min (polymerase activation).
- 45 Cycles: 95°C for 15 sec (denaturation), 60°C for 1 min (annealing/extension).
- Record the fluorescence signal at the end of each annealing/extension step.
Data Analysis:
- Determine the Cycle Threshold (Ct) value for each sample.
- Construct a standard curve using serial dilutions of DNA from a known concentration of the target nut.
- Interpolate the Ct values of unknown samples against the standard curve for quantitative analysis.
This protocol verifies the removal of allergenic food residues from processing equipment surfaces.
Surface Sampling:
- Use a sterile, moisturized swab specifically designed for adenylate testing.
- Swab a defined surface area (e.g., 10 x 10 cm) of the equipment after the cleaning procedure. Use a consistent, firm pressure and a systematic pattern to cover the entire area.
- For complex geometries, use a larger number of swabs to ensure representative sampling.
Sample Elution and Measurement:
- Immediately after sampling, insert the swab into the assay buffer provided with the A3 test kit and vortex thoroughly to elute the collected residue.
- Transfer the buffer into a cuvette or a reaction tube compatible with the luminometer.
- Add the necessary enzymes (luciferase and converting enzymes) to convert ADP and AMP to ATP, followed by the measurement of total bioluminescence.
Interpretation and Result:
- The luminometer provides a reading in Relative Light Units (RLU).
- Establish a threshold RLU value for a "clean" surface through validation studies correlating A3 results with specific allergen presence (e.g., via ELISA or LFI).
- A reading below the established threshold indicates effective cleaning and a low risk of allergen cross-contact.
The following workflow summarizes the parallel paths for detecting allergens in finished products and on processing equipment.
Diagram 2: Allergen Detection and Control Workflow. Two primary pathways exist for allergen risk management: analysis of finished food products (Path A) and hygiene monitoring of processing equipment (Path B).
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for Food Allergen Research
| Reagent / Material | Function and Role in Research | Example Applications |
|---|---|---|
| Species-Specific Primers & TaqMan Probes | Enable highly specific amplification and detection of target DNA sequences from allergenic foods. | Detection and quantification of nut, sesame, or other allergen sources in complex food matrices via real-time PCR [58]. |
| Monoclonal/Polyclonal Antibodies | Core recognition elements in immunoassays; bind to specific epitopes on allergenic proteins. | Development and deployment of ELISA kits and Lateral Flow Immunoassays (LFI) for specific allergens like gluten, peanut, or milk [50] [59]. |
| Synthetic Aptamers | oligonucleotide-based recognition elements offering high stability and affinity for target proteins. | Integration into novel biosensors for rapid, on-site allergen detection; potential use as immunomodulators to suppress allergic responses [57]. |
| Stable Isotope-Labeled Peptides | Internal standards for mass spectrometry that co-elute and fragment identically to target peptides, enabling precise quantification. | Absolute quantification of specific allergenic proteins (e.g., Ara h 3, Bos d 5) using LC-MS/MS, correcting for matrix effects and ion suppression [7] [44]. |
| A3 (ATP+ADP+AMP) Assay Kits | Provide all necessary reagents and enzymes (luciferase, converting enzymes) to measure total adenylates as a marker for hygiene. | Rapid, non-specific verification of cleaning efficacy on food processing equipment surfaces to prevent allergen cross-contact [50]. |
The interaction between food processing and allergen detection presents a formidable analytical challenge with direct implications for public health. As this guide has detailed, processing can denature, hydrolyze, or mask allergenic proteins, thereby compromising the accuracy of commonly used detection methods like ELISA, which rely on native protein structures. This necessitates a paradigm shift towards more robust detection strategies, such as mass spectrometry, which targets stable peptide sequences, and the complementary use of DNA-based and rapid hygiene tests.
Future research must focus on several key areas to advance the field of allergen threshold and limit of detection research. First, there is a critical need to develop standardized reference materials made from processed foods to validate detection methods against realistic matrix effects. Second, the integration of multi-omics approaches—correlating proteomic (MS) data with genomic (PCR) and immunologic (IgE-binding) data—will provide a more holistic understanding of how processing affects both detectability and allergenicity [54] [44]. Finally, emerging technologies like AI-powered hyperspectral imaging and biosensors promise faster, non-destructive screening, but require extensive validation [7]. By adopting these integrated approaches, the scientific community can overcome the current limitations and establish more reliable, processing-resistant frameworks for allergen risk assessment and management, ultimately ensuring greater safety for allergic consumers.
The accurate determination of food allergen thresholds and limits of detection is fundamentally challenged by matrix interferences in complex food systems. Fats, tannins, and other food components interact with allergenic proteins and analytical reagents, leading to skewed results that impact both risk assessment and regulatory compliance. This technical guide examines the molecular mechanisms of these interferences and provides validated strategies to overcome them, forming a critical foundation for advancing food allergen research and ensuring public health safety.
The pursuit of precise food allergen thresholds is central to protecting sensitive individuals while enabling informed food choices. The limit of detection (LOD) and eliciting dose (ED) for allergens like peanut protein can be as low as 0.1 mg and 1.5 mg, respectively, necessitating extremely sensitive and specific detection methods [3]. However, the complex nature of food matrices introduces significant analytical challenges that can mask, bind, or chemically modify allergenic proteins, leading to both false positives and, more dangerously, false negatives.
Matrix effects arise from the diverse molecular components that constitute food, including proteins, lipids, carbohydrates, and polyphenols. These components can compete for binding sites in immunoassays, precipitate target analytes, or modify epitope structures through covalent and non-covalent interactions. The implications extend beyond analytical chemistry into public health, as inaccurate threshold determinations directly impact the safety of food-allergic consumers, estimated to include 1 in 10 adults and 1 in 13 children [3]. Understanding and mitigating these interferences is therefore essential for developing reliable detection methodologies that support evidence-based regulatory frameworks and effective allergen management.
Fundamental Interference Mechanisms
Molecular Interactions with Food Matrices
Table 1: Primary Interference Mechanisms in Food Matrices
| Matrix Component | Interaction Type | Key Interfering Foods | Impact on Allergen Detection |
|---|---|---|---|
| Lipids (Fats/Oils) | Hydrophobic binding, emulsification, protein coating | Dairy, oils, nuts, fried foods | Reduces antibody binding, increases matrix background, modifies protein solubility |
| Tannins & Polyphenols | Hydrogen bonding, protein precipitation, covalent modification | Tea, wine, chocolate, berries, nuts | Precipitates target proteins, masks epitopes, quenches signal generation |
| Proteins | Protein-protein interactions, competitive binding | Meat, dairy, eggs, soy | Cross-reacts with detection antibodies, creates background interference |
| Carbohydrates | Hydrogen bonding, viscosity effects, encapsulation | Starchy foods, grains, thickeners | Traps allergens physically, increases solution viscosity, hinders extraction |
Food matrices interfere with allergen detection through several well-characterized mechanisms. Hydrophobic interactions dominate in lipid-rich systems, where allergenic proteins partition into fat phases or become encapsulated by lipid micelles, effectively reducing their availability for detection in aqueous extracts [60]. This is particularly problematic for methods like ELISA that rely on liquid-phase antigen-antibody interactions.
Polyphenolic compounds, particularly tannins, present a dual challenge through their ability to form both reversible and irreversible complexes with proteins. Tannins are characterized by their specific ability to precipitate alkaloids, gelatin, and other proteins [61]. The molecular basis for this interaction involves multiple hydrogen bonds and hydrophobic effects between the phenolic hydroxyl groups of tannins and peptide bonds in proteins. This precipitation effect directly removes the target analyte from solution, while sub-precipitation concentrations can still mask critical epitopes through molecular complexation, preventing antibody recognition [61] [60].
The structural diversity of tannins directly influences their interference potential. Condensed tannins (proanthocyanidins) consist of flavan-3-ol units (e.g., catechin, epicatechin) linked through carbon-carbon bonds, with molecular weights ranging from monomers to oligomers of up to forty units [61]. Higher molecular weight proanthocyanidins with greater mean degree of polymerization (mDP) demonstrate increased protein-binding capacity and astringency, correlating with their interference potential in analytical systems [61]. Hydrolyzable tannins (gallotannins and ellagitannins), derived from gallic acid esters with glucose, represent another significant class of interferents commonly found in fruits, nuts, and wine [61].
Impact on Analytical Parameters
Matrix effects systematically impact critical analytical parameters including extraction efficiency, detection sensitivity, and method precision. The partition coefficient of analytes between the food matrix and extraction buffer determines the efficiency of allergen recovery, with hydrophobic allergens in high-fat matrices demonstrating recovery rates as low as 30-40% without appropriate mitigation strategies [60]. Furthermore, matrix components can directly inhibit enzymatic reactions in ELISA systems or quench fluorescent signals in modern biosensors, leading to an underestimation of allergen content that poses significant risks to sensitive individuals.
Experimental Strategies for Interference Mitigation
Sample Preparation and Extraction Protocols
Table 2: Optimized Extraction Protocols for Challenging Matrices
| Matrix Type | Recommended Extraction Buffer | Key Additives | Processing Conditions | Expected Recovery Improvement |
|---|---|---|---|---|
| High-Fat Foods | PBS with 0.5-1% Tween-20 | Lipase (0.1 U/mL), SDS (0.1%) | 45°C with agitation, defatting with hexane | 70% → 90-95% |
| Tannin-Rich Foods | PBS with 1-2% PVPP | BSA (0.5%), β-mercaptoethanol (1%) | Centrifugation at 10,000 × g, pH 7.4 | 45% → 85-90% |
| Complex Multi-Component | Commercial allergen extraction buffers | Polymer adsorbents, reducing agents | Sequential extraction, ultrasonic assistance | 50% → 80-85% |
Effective sample preparation is the primary defense against matrix interferences. For lipid-rich matrices, a sequential defatting approach using hexane or petroleum ether followed by protein extraction with surfactants significantly improves recovery. The incorporation of lipase enzymes (0.1 U/mL) during extraction hydrolyzes triglycerides, releasing encapsulated proteins and improving accessibility to detection antibodies [60].
For tannin-rich systems, the addition of polyvinylpolypyrrolidone (PVPP) at 1-2% w/v effectively adsorbs phenolic compounds through hydrogen bonding, preventing their interaction with target proteins [61]. Competitive binding agents such as bovine serum albumin (BSA) at 0.5% can be added to sacrifice non-specific binding sites, preserving the target allergens for detection. The use of high-ionic-strength buffers (0.5-1 M NaCl) disrupts weak electrostatic interactions between tannins and proteins, while maintaining neutral pH conditions prevents the oxidation of phenolic compounds to more reactive quinones [61] [60].
Complex foods containing multiple interferents benefit from specialized commercial extraction buffers specifically formulated for allergen detection. These typically contain a combination of surfactants, polymers, and competitive binding agents designed to address multiple interference mechanisms simultaneously. Physical processing methods including ultrasonication and high-speed homogenization improve extraction efficiency by disrupting physical barriers and increasing the surface area available for extraction.
Analytical Method Selection and Validation
The choice of analytical platform significantly influences susceptibility to matrix effects. Immunoassays (ELISA) remain widely used but are particularly vulnerable to epitope masking and non-specific binding. Mass spectrometry-based methods (LC-MS/MS) offer superior specificity through mass identification but still face challenges with ionization suppression from co-eluting matrix components.
Method validation must include robust matrix-matched calibration using blank matrix samples spiked with known allergen concentrations. The standard addition method provides the most accurate quantification in complex matrices by accounting for recovery losses and signal suppression. For regulatory compliance, the implementation of orthogonal methods (e.g., ELISA followed by MS confirmation) provides the highest level of confidence in results obtained from challenging matrices.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Matrix Interference Management
| Reagent Category | Specific Examples | Mechanism of Action | Application Notes |
|---|---|---|---|
| Surfactants | Tween-20, SDS, CHAPS | Solubilize hydrophobic proteins, disrupt lipid interactions | SDS may denature proteins; use at 0.1-0.5% for ELISA |
| Polymer Adsorbents | PVPP, activated charcoal | Bind phenolic compounds via H-bonding | PVPP at 1-2% w/v effectively removes tannins |
| Competitive Binding Agents | BSA, casein, skim milk | Block non-specific binding sites | Use non-cross-reactive species (e.g., fish gelatin) |
| Enzymatic Treatments | Lipase, protease inhibitors | Digest interfering components | Lipase pre-treatment for high-fat matrices |
| Reducing Agents | β-mercaptoethanol, DTT | Break disulfide bonds, improve extraction | May disrupt native protein structure |
| Commercial Kits | Specific allergen extraction kits | Optimized multi-component formulations | Follow manufacturer's protocols precisely |
The selection of appropriate reagents is critical for successful allergen detection in challenging matrices. Surfactants maintain protein solubility and prevent aggregation, with non-ionic varieties (Tween-20) preferred for immunoassays to preserve protein conformation and antibody binding. Polymer adsorbents like PVPP are particularly effective for tannin-rich matrices, with an optimal contact time of 15-30 minutes during extraction to maximize polyphenol binding without significant allergen loss [61].
Competitive binding agents including BSA (0.5-1%) and non-fat dry milk (1-3%) block non-specific binding sites on plastic surfaces and matrix components, reducing background signal in immunoassays. For applications requiring minimal interference with target detection, species-specific proteins (e.g., fish gelatin for mammalian allergen detection) prevent cross-reactivity while maintaining blocking efficacy.
Enzymatic pre-treatments offer matrix-specific solutions, with lipase (0.1 U/mL, 37°C, 30 minutes) effectively degrading fat barriers in dairy and oil-rich products, while cellulase and pectinase can improve extraction from plant-based matrices with high fiber content. The inclusion of protease inhibitor cocktails is essential when using enzymatic pre-treatments to prevent unintended degradation of target allergens.
Advanced Methodologies and Workflows
Integrated Multi-Technique Approaches
Advanced workflow integration provides comprehensive solutions for challenging matrices. The combination of immunoaffinity capture with LC-MS/MS detection leverages the sample clean-up capabilities of antibody-based enrichment with the specificity of mass-based detection. This approach effectively separates target allergens from matrix interferents before analysis, significantly reducing background noise and improving sensitivity in complex foods [60].
Biosensor platforms utilizing surface plasmon resonance (SPR) or quartz crystal microbalance (QCM) offer real-time monitoring of binding events, enabling the discrimination between specific allergen detection and non-specific matrix binding through kinetic analysis. These label-free methods are particularly valuable for characterizing matrix effects and developing interference-resistant detection strategies.
The emerging field of molecularly imprinted polymers (MIPs) provides synthetic recognition elements that demonstrate superior stability in harsh matrix conditions compared to biological antibodies. MIPs maintain functionality in organic solvents, extreme pH, and high ionic strength environments where traditional immunoassays would fail, offering promising alternatives for challenging applications.
Quantification and Data Analysis
Accurate quantification in the presence of matrix effects requires specialized analytical approaches. The method of standard addition involves spiking duplicate aliquots of the sample extract with known concentrations of the target allergen, effectively creating an internal calibration curve that accounts for matrix-induced suppression or enhancement. This approach provides the most accurate results but increases analytical time and cost.
For high-throughput applications, matrix-matched calibration curves prepared in blank matrix extracts provide a practical compromise, though they require verification of the blank matrix's true allergen-free status. The use of stable isotope-labeled internal standards in mass spectrometry methods corrects for variable extraction efficiency and ionization suppression, representing the gold standard for quantification in complex matrices.
Quality control measures must include recovery assessments using spiked samples at multiple relevant concentrations, with acceptable recovery ranges established based on the intended application (typically 70-120% for quantitative methods). The consistent monitoring of quality control data enables the detection of changing matrix effects between product batches or seasonal variations in raw materials.
Matrix interferences present significant but surmountable challenges in food allergen detection and threshold determination. The strategic integration of appropriate sample preparation techniques, reagent selections, and analytical methodologies enables reliable allergen quantification across diverse food systems. As food allergen management continues to evolve toward more precise threshold-based approaches, the effective mitigation of matrix effects becomes increasingly critical for both risk assessment and regulatory compliance.
Future advancements will likely focus on multiplexed detection platforms capable of simultaneously quantifying multiple allergens while internally correcting for matrix effects, rapid screening methods with integrated clean-up steps for point-of-use applications, and reference materials with well-characterized matrix compositions to support method validation. The continued collaboration between food chemists, analytical scientists, and clinical researchers will drive innovation in this critical field, ultimately enhancing the safety and quality of life for food-allergic consumers worldwide.
Within the broader research on food allergen thresholds and limits of detection, a significant challenge persists: the accurate differentiation of true allergens from biologically similar species due to immunoglobulin E (IgE) cross-reactivity [62]. Cross-reactivity occurs when the immune system recognizes similar protein structures in different allergen sources, leading to IgE antibodies binding to epitopes from distinct allergens [62]. This phenomenon complicates diagnostic accuracy, impacts risk assessment, and presents substantial challenges for both clinical management and regulatory policies regarding food safety.
The clinical implications are profound. Cross-reactivity can lead to overdiagnosis of food allergies, as positive test results may not correlate with clinical symptoms [63]. For instance, more than 50% of peanut-allergic individuals show positive tests to other legumes, yet approximately 95% can tolerate them without symptoms [63]. Understanding these pitfalls is thus essential for developing precise diagnostic tools and establishing clinically relevant threshold levels that protect sensitive individuals without imposing unnecessary dietary restrictions.
Molecular Mechanisms of Allergen Cross-Reactivity
Fundamental Immunological Principles
At its core, cross-reactivity is an immunological phenomenon driven by structural biology. It is defined as the recognition of two or more distinct allergen molecules by antibodies or T cells of the same specificity, initially primed against a primary sensitizer [62]. The mechanistic basis lies in the structural similarity of epitopes - the specific regions of antigens recognized by immune receptors [62].
Table 1: Key Definitions in Molecular Allergology
| Term | Definition |
|---|---|
| Cross-reactivity | Recognition of epitopes from distinct allergens by the same IgE molecule, usually occurring with a primary sensitizer inducing IgE antibodies that bind shared epitopes [62] |
| Genuine sensitization | Sensitization that can be attributed to a given allergenic source, as opposed to cross-reactive sensitization [62] |
| Panallergen | Protein belonging to a family that shares regions of highly conserved sequence and 3-dimensional structure, resulting in IgE cross-reactivity [62] |
| Component-resolved diagnosis | Allergy diagnosis comprising investigation at the molecular allergen level, enabling discrimination between genuine sensitization and cross-reactivity [62] |
The molecular basis for cross-reactivity stems from shared structural features between proteins from different biological sources. When the immune system produces IgE antibodies against an allergen from one source, these antibodies may bind to similar epitopes on proteins from unrelated sources if they share sufficient amino acid sequence identity or structural homology [62] [64]. This cross-recognition can occur at the level of linear epitopes (sequential stretches of 6-10 amino acids) or conformational epitopes (three-dimensional structures composed of non-sequential amino acids) [62].
Protein Families and Structural Classification
Research has demonstrated that allergenic proteins are not randomly distributed across protein space but cluster within a limited number of protein structural families. Bioinformatics analyses reveal that all known allergens can be grouped into approximately 130-143 of the 9,318 distinct families in the Pfam database [64]. This clustering explains many observed cross-reactivity patterns.
Panallergens represent particularly problematic categories for cross-reactivity. These proteins belong to highly conserved families with widespread distribution across plant and animal kingdoms. Notable examples include:
- Profilins: Actin-binding proteins present in all eukaryotic cells
- Pathogenesis-related (PR-10) proteins: Including the Bet v 1 family from birch pollen
- Lipid transfer proteins (LTPs): Stable proteins resistant to heat and digestion
- Tropomyosins: Major allergens in crustacean shellfish and insects
- Parvalbumins: Calcium-binding proteins in fish and amphibians
The following diagram illustrates the relationship between protein structural similarity and clinical cross-reactivity:
Figure 1: Molecular pathway from protein structural similarity to clinical cross-reactivity
Clinical Patterns and Prevalence Data
Cross-reactivity manifests in predictable patterns across food groups, with significant variations in clinical risk. The following table summarizes quantitative data on cross-reactivity risks between biologically related species:
Table 2: Quantitative Cross-Reactivity Risks Between Biologically Similar Species
| Allergen Group | Specific Sources | Cross-Reactivity Risk | Clinical Notes |
|---|---|---|---|
| Mammalian Milks | Cow's milk vs. goat/sheep milk | ~90% [65] [63] | High cross-reactivity due to protein homology |
| Cow's milk vs. mare/donkey milk | ~5% [63] | Lower cross-reactivity | |
| Tree Nuts | Cashew vs. pistachio | High degree [65] | Botanical relationship (Anacardiaceae family) |
| Walnut vs. pecan | High degree [65] [63] | Botanical relationship | |
| Different tree nut genera | Variable [63] | Most patients not allergic to all tree nuts | |
| Fish | Different fish species | ~50% [63] | Fresh and saltwater fish |
| Shellfish | Crustacean shellfish (shrimp, lobster, crab) | ~75% [63] | High cross-reactivity within crustaceans |
| Crustacean vs. mollusks | Lower risk [63] | Limited cross-reactivity between classes | |
| Legumes | Peanut vs. other legumes (soy, beans) | >50% sensitization, but ~95% tolerance [63] | High rate of asymptomatic sensitization |
Pollen-Food Allergy Syndrome (PFAS)
A particularly common form of cross-reactivity is Pollen-Food Allergy Syndrome (PFAS), also known as oral allergy syndrome [65] [63]. This condition occurs when individuals sensitized to pollen allergens experience symptoms from raw fruits, vegetables, or nuts containing structurally similar proteins.
Table 3: Common Pollen-Food Cross-Reactivity Patterns
| Pollen Source | Cross-Reactive Foods | Responsible Panallergen |
|---|---|---|
| Birch pollen | Apple, peach, cherry, pear, carrot, hazelnut, peanut [65] [63] | Bet v 1 (PR-10 protein) |
| Ragweed | Melons (watermelon, cantaloupe), banana, zucchini | Profilin |
| Grass pollen | Tomato, potato, peach, melon | Multiple panallergens |
| Mugwort | Celery, carrot, spices, mango | Lipid Transfer Protein |
PFAS symptoms are typically limited to the oropharynx and include itching, tingling, or mild swelling of the lips, tongue, palate, and throat [65] [63]. These symptoms result from the lability of the responsible proteins, which are often denatured by heat processing or gastric digestion [63]. Consequently, individuals with PFAS can typically tolerate cooked forms of foods that cause reactions when raw.
Detection and Diagnostic Challenges
Limitations of Conventional Diagnostic Methods
Traditional allergy diagnostics rely on skin prick testing (SPT) and serum-specific IgE measurements using whole allergen extracts [62] [66]. These methods have inherent limitations in addressing cross-reactivity:
- Limited Specificity: SPT and extract-based IgE tests have approximately 30-60% specificity, leading to frequent false positives [66]
- Inability to Discriminate: Whole extracts contain multiple proteins, preventing differentiation between genuine sensitization and cross-reactivity [62]
- Component Mixing: Cross-reactive epitopes may dominate the immune response, masking unique markers for genuine sensitization
Advanced Diagnostic Approaches
Component-resolved diagnosis (CRD) represents a paradigm shift in addressing cross-reactivity pitfalls [62]. By testing IgE reactivity to specific purified or recombinant allergen molecules, CRD enables:
- Discrimination between genuine sensitization and cross-reactivity through marker allergens [62]
- Assessment of clinical risk severity based on reactivity profiles to specific protein components
- Personalized management strategies tailored to individual sensitization patterns
The following workflow illustrates the component-resolved diagnostic approach for differentiating true allergens from cross-reactive species:
Figure 2: Component-resolved diagnosis workflow for differentiating sensitization types
Analytical Detection Methods for Food Matrices
Detecting allergenic foods in complex matrices presents significant technical challenges, particularly with cross-reactive antibodies used in immunoassays. The following table compares major analytical approaches:
Table 4: Methodologies for Allergen Detection in Foods
| Method Type | Principle | Advantages | Limitations for Cross-Reactivity |
|---|---|---|---|
| Immunoassays (ELISA, LFIA) | Antibody-antigen binding using antibodies against specific allergenic proteins [39] | High sensitivity, specificity, throughput | Antibody cross-reactivity with similar proteins from unrelated sources |
| Mass Spectrometry | Detection of signature peptides from allergenic proteins [7] [39] | High specificity, multiplexing capability, not affected by antibody cross-reactivity | Complex sample preparation, matrix effects, equipment cost |
| DNA-based Methods (PCR) | Amplification of species-specific DNA sequences [39] | High specificity for biological species, works in processed foods | Indirect detection (does not measure proteins), cannot differentiate allergenic from non-allergenic proteins |
| Biosensors | Bio-recognition elements coupled to transducers [39] | Rapid, portable, potential for multiplexing | Limited commercial availability, validation requirements |
Research Reagents and Experimental Solutions
Advancing research on cross-reactivity requires specialized reagents and methodologies. The following toolkit outlines essential resources for investigating allergen cross-reactivity:
Table 5: Research Reagent Solutions for Cross-Reactivity Studies
| Research Tool | Function and Application | Key Features |
|---|---|---|
| Recombinant Allergens | Component-resolved diagnosis, inhibition assays, structural studies [62] | Pure molecular species, defined epitope structure, reproducible production |
| Monoclonal Antibodies | Epitope mapping, cross-reactivity studies, immunoassay development [64] | Specific to single epitopes, unlimited supply, consistent properties |
| Peptide Microarrays | Linear epitope mapping, identification of cross-reactive epitopes [64] | High-throughput screening, comprehensive epitope analysis |
| Allergen Databases | Bioinformatics analysis, sequence comparisons, structural modeling [64] | IUIS, SDAP, Allergome, FARRP provide curated allergen information |
| Biosimilar Allergen Extracts | Skin testing, in vitro diagnostics, challenge materials [62] | Standardized compositions, biological activity preservation |
Future Directions and Research Implications
Emerging Technologies
Innovative approaches are transforming allergen detection and cross-reactivity assessment:
- AI-enhanced testing and non-destructive diagnostics using hyperspectral imaging and FTIR spectroscopy [7]
- Multiplexed immunoassays and mass spectrometry with detection limits as low as 0.01 ng/mL [7]
- Biosensor platforms incorporating microfluidics and novel transducers for rapid, on-site detection [39]
- Bioinformatics tools for predicting cross-reactivity based on structural modeling and epitope comparison [64]
Implications for Thresholds and Risk Assessment
Understanding cross-reactivity is essential for establishing scientifically sound allergen thresholds and evidence-based regulatory policies. Key considerations include:
- Dose-response relationships may differ between genuine allergens and cross-reactive proteins [3]
- Individual thresholds vary significantly and can be affected by co-factors such as exercise, sleep deprivation, and medications [3]
- Matrix effects influence allergen bioavailability and clinical reactivity [39]
- Sensitization patterns identified through component-resolved diagnosis can inform personalized threshold assessments [62]
Future research should prioritize standardization of component-based approaches, validation of threshold methodologies across diverse populations, and integration of clinical and molecular data to refine risk assessment models. By addressing these cross-reactivity pitfalls, we can advance toward more precise diagnostic and management strategies that improve both safety and quality of life for allergic individuals.
This guide details the critical laboratory practices of spike-and-recovery experiments and incurred sample analysis, framing them within essential methodologies for validating analytical techniques used in food allergen detection and threshold research. The accuracy of data generated by methods like the Enzyme-Linked Immunosorbent Assay (ELISA) is foundational for establishing reliable food allergen thresholds and limits of detection (LOD) [2] [39]. Without rigorous validation, the reliability of data informing public health policies and food labeling requirements remains questionable. These practices are vital for generating the high-quality data necessary to protect consumers with food allergies, a growing public health concern worldwide [39].
Core Validation Concepts and Their Importance
Spike-and-Recovery Assessment
Spike-and-recovery experiments evaluate the accuracy of an analytical method by determining whether the sample matrix (e.g., a complex food product) interferes with the detection of the analyte (e.g., an allergenic protein) [67] [68]. This is achieved by adding ("spiking") a known amount of purified analyte into the natural sample matrix and then measuring the percentage of the analyte that is successfully recovered ("recovery") when compared to the same spike in a standard diluent [67].
The core purpose is to identify matrix effects. Components in a food sample, such as high fat content, polyphenols, or other proteins, can bind to the allergen or the assay antibodies, leading to either under-recovery (inhibition) or over-recovery (enhancement) of the signal [68]. For instance, a study on medicinal herbs demonstrated that spiked analytes could show perfect recovery (~100%) while native analytes trapped within the plant material were only extracted at 73-94%, highlighting that spike recovery alone can be misleading if extraction efficiency is not properly investigated [69].
The Role of Positive Controls and Linearity of Dilution
Positive controls, which are samples with a known, predetermined concentration of the analyte, are used throughout method validation and routine analysis to monitor assay performance and ensure consistency [70]. In the context of spike-and-recovery, the spiked samples themselves act as a form of positive control for assessing accuracy within a specific matrix.
Linearity of dilution is a related experiment that assesses whether a sample's dose response is linear over the assay's working range [67]. It provides information on the precision of results for samples tested at different dilution levels in a chosen diluent. Good linearity allows for the accurate analysis of samples with high analyte levels by diluting them to fall within the standard curve, ensuring methodological flexibility [67]. Poor linearity often indicates that the sample matrix, sample diluent, or standard diluent differentially affects analyte detection upon dilution, which are the same underlying causes of poor spike-and-recovery [67].
Incurred Sample Analysis (ISA) and Incurred Sample Reanalysis (ISR)
While spike-and-recovery tests a purified standard added to a matrix, Incurred Sample Analysis (ISA) and Incurred Sample Reanalysis (ISR) evaluate the method's performance with real, study-derived samples. "Incurred" samples are biological samples (e.g., serum, plasma) collected from subjects (humans or animals) after exposure to a drug or, by extension, a food allergen. These samples contain the analyte that has been subjected to in vivo metabolic processes, which may alter its form (e.g., through protein degradation or complexation) compared to the purified standard used for spiking [71].
ISR is the practice of reanalyzing a subset of these incurred samples in a separate analytical run to confirm the reproducibility and reliability of the original results [71] [72]. It became a standard expectation in regulated bioanalysis after regulatory agencies observed discrepancies between original and repeat analysis results in numerous submissions [71]. ISR verifies that the method can accurately quantify the analyte as it natively exists in the sample, accounting for all in vivo effects.
Table 1: Comparison of Key Validation Practices
| Practice | Primary Purpose | Sample Type | Evaluates |
|---|---|---|---|
| Spike-and-Recovery | Assess accuracy and matrix interference | Sample matrix spiked with purified analyte | Recovery of a known standard; impact of matrix components |
| Linearity of Dilution | Assess precision across dilutions | Natural or spiked sample at multiple dilutions | Effect of dilution on analyte detectability |
| Incurred Sample Reanalysis (ISR) | Confirm reproducibility and reliability | Study-derived samples containing in vivo metabolites | Assay performance with the true, processed analyte |
Detailed Experimental Protocols
Protocol for Spike-and-Recovery and Linearity-of-Dilution
The following workflow outlines the key steps for conducting a combined spike-and-recovery and linearity-of-dilution experiment [67] [68].
Workflow for Combined Validation Experiment
Step-by-Step Procedure:
- Prepare Sample Matrix: Obtain the natural test sample matrix (e.g., a food extract) that will be used in the actual study [67].
- Determine Minimum Required Dilution (MRD): Conduct a preliminary dilution linearity study to establish the minimum dilution factor needed to overcome matrix interference and ensure the sample is within the assay's analytical range [68].
- Prepare Spike Solutions: Prepare a concentrated stock solution of the purified analyte (e.g., recombinant allergenic protein) in the standard diluent. The concentration should be calculated such that when added to the sample, it results in 3-4 final concentrations covering the analytical range of the assay (e.g., low, medium, high) [68]. The lowest spike concentration should be at least 2 times the assay's Limit of Quantitation (LOQ) [68].
- Spike the Matrix:
- For each sample type and spike level, add a known volume of the spike solution to the neat (undiluted) sample matrix [67] [68].
- In parallel, prepare a "zero standard" control by adding an equal volume of standard diluent (without analyte) to the neat sample. This measures the endogenous level of the analyte [68].
- Prepare the reference standard in the standard diluent alone.
- Perform Serial Dilutions (for Linearity): Take the spiked sample and the unspiked natural sample and prepare a series of dilutions (e.g., neat, 1:2, 1:4, 1:8) in the chosen sample diluent [67].
- Analyze Samples: Run all spiked samples, zero standard controls, diluted samples, and reference standards in the assay (e.g., ELISA) according to the established protocol. All samples should be analyzed in replicate (e.g., duplicate or triplicate) [67].
- Calculate Recovery and Assess Linearity:
- Spike Recovery (%) is calculated as:
(Measured concentration in spiked sample - Measured concentration in unspiked sample) / Theoretical spike concentration × 100%[68]. - Linearity is assessed by plotting the observed concentration (multiplied by the dilution factor) against the expected concentration (based on the neat value) for each dilution. The recovery percentage for each dilution is calculated as:
(Observed concentration × Dilution Factor) / Expected neat concentration × 100%[67].
- Spike Recovery (%) is calculated as:
Interpretation of Results:
- Spike Recovery: According to ICH, FDA, and EMA guidelines, recovery values within 75% to 125% are generally considered acceptable [68]. Values outside this range indicate significant matrix interference.
- Linearity of Dilution: The dilution-adjusted recoveries should also fall within an acceptable range (e.g., 80-120%). A consistent recovery across dilutions indicates good linearity [67].
Table 2: Example ELISA Spike and Recovery Data for Human IL-1 beta in Urine [67]
| Sample | No Spike (0 pg/mL) | Low Spike (15 pg/mL) | Medium Spike (40 pg/mL) | High Spike (80 pg/mL) |
|---|---|---|---|---|
| Diluent Control | 0.0 | 17.0 | 44.1 | 81.6 |
| Donor 1 | 0.7 | 14.6 | 39.6 | 69.6 |
| Donor 2 | 0.0 | 17.8 | 41.6 | 74.8 |
| Donor 9 | 0.7 | 12.4 | 37.6 | 68.2 |
| Mean Recovery (% ± S.D.) | NA | 86.3% ± 9.9% | 85.8% ± 6.7% | 84.6% ± 3.5% |
Table 3: Example ELISA Linearity-of-Dilution Results [67]
| Sample | Dilution Factor (DF) | Observed (pg/mL) × DF | Expected (pg/mL) | Recovery % |
|---|---|---|---|---|
| ConA-stimulated Cell Culture Supernatant | Neat | 131.5 | 131.5 | 100 |
| 1:2 | 149.9 | 114 | ||
| 1:4 | 162.2 | 123 | ||
| 1:8 | 165.4 | 126 |
Protocol for Incurred Sample Reanalysis (ISR)
The following workflow outlines the standard process for conducting ISR [71].
Incurred Sample Reanalysis Workflow
Step-by-Step Procedure:
- Original Analysis: The full set of incurred samples is analyzed, and the initial concentration values are recorded.
- Select ISR Subset: A predefined percentage of incurred samples (often 5-10%) is selected for reanalysis. Selection should be based on scientific rationale, including samples across various concentration levels (especially near the peak concentration - Cmax - and the elimination phase), from different subjects, and representing different time points [71].
- Reanalyze Samples: The selected samples are reanalyzed in a separate analytical run by a different analyst if possible. The reanalysis should be performed with the same number of replicates as the original analysis (e.g., singlicate for LC/MS, duplicate for LBA) [71].
- Calculate Difference: For each pair of original and repeat results, the percent difference is calculated.
- Percent Difference (%) =
(Repeat Concentration - Original Concentration) / Mean of Original and Repeat Concentrations × 100%
- Percent Difference (%) =
- Assess ISR Acceptance: The ISR passes if a minimum of 67% (or two-thirds) of the reanalyzed samples have a percent difference within ±20% of the mean value [71].
Troubleshooting and Best Practices
Addressing Poor Spike-and-Recovery Results
When recovery falls outside the acceptable range (75-125%), the following adjustments can be made [67] [68]:
- Alter the Standard/Sample Diluent: Modify the standard diluent to more closely match the sample matrix. For example, if analyzing culture supernatants, use culture medium as the diluent. Alternatively, change the sample diluent. Diluting the sample in a standard diluent (e.g., PBS with 1% BSA) can often correct recovery problems by reducing the concentration of interfering components [67].
- Modify the Sample Matrix: Adjust the pH of the sample matrix to match the optimized standard diluent, or add a carrier protein like BSA to stabilize the analyte [67].
- Further Process the Sample: If interference persists, further process the sample using alternative methods, such as additional dilution, filtration, or precipitation, to remove interfering substances [68].
Key Considerations for ISR
- Documentation: Procedures for ISR, including sample selection criteria, acceptance criteria, and documentation requirements, must be described a priori in a standard operating procedure (SOP) or study plan [71].
- Distinction from Repeats: ISR should not be confused with repeat analysis for "assignable cause" (e.g., instrument failure) or for "pharmacokinetic reasons" (e.g., incongruous data), which are governed by different rules and justifications [71].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Validation Experiments
| Item | Function | Example & Notes |
|---|---|---|
| Purified Allergen / Analyte Standard | Serves as the reference material for preparing calibration standards and spike solutions. | Recombinant allergenic proteins (e.g., Ara h 1 for peanut); should be highly characterized and pure [39]. |
| Specific Antibody Pairs | The core biorecognition elements for sandwich ELISA-based detection. | Monoclonal or polyclonal antibodies specific to the target allergen; critical for assay sensitivity and specificity [70] [39]. |
| Commercial ELISA Kit | Provides a standardized, optimized set of reagents and protocols for specific allergen detection. | Kits from various suppliers for allergens like peanut, milk, egg; often include pre-coated plates, standards, and antibodies [67]. |
| Matrix-Matched Diluent | A diluent that closely mimics the natural sample matrix to minimize interference. | For a serum sample, the diluent could be a buffer with a similar protein background (e.g., PBS with 1% BSA) [67]. |
| Sample Preparation Tools | For homogenizing and extracting the allergen from complex food matrices. | Stomachers, centrifuges, and specific extraction buffers designed to efficiently release the target protein without degrading it [70]. |
Spike recovery and incurred sample analysis are complementary pillars of a robust bioanalytical method validation framework. Spike recovery identifies and helps correct for matrix interference using a purified standard, while incurred sample reanalysis confirms the method's reliability for measuring the true, metabolized analyte in real-world samples. Adherence to these practices, guided by international standards and scientific judgment, is non-negotiable for producing data that can confidently inform critical decisions in food safety, public health, and regulatory policy, particularly in the evolving field of food allergen threshold research.
Benchmarking Performance: Method Validation, Comparative Data, and Standardization Gaps
Food allergies represent a significant and growing global public health concern, with accurate detection methods being paramount for consumer safety, regulatory compliance, and effective risk management [39] [2]. The incidence of food allergies is increasing annually, affecting approximately 8% of children and 4% of adults worldwide [42]. In the United States alone, undeclared allergens are one of the leading causes of food recalls, accounting for 34.1% of all food recalls [73]. Within this context, the selection of appropriate analytical methods for allergen detection becomes critical for food manufacturers, regulatory agencies, and research institutions.
This technical guide provides a comprehensive comparison of the three principal analytical platforms used in food allergen detection: Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and Mass Spectrometry (MS). Each method operates on distinct analytical principles, offering unique advantages and limitations in sensitivity, specificity, multiplexing capability, and applicability across different food matrices [39]. ELISA, which detects allergenic proteins using antibody-antigen interactions, remains the gold standard for routine allergen screening due to its cost-effectiveness and regulatory acceptance [73]. PCR, targeting allergen-specific DNA sequences, provides exceptional specificity and is particularly valuable for processed foods where proteins may be denatured [73] [74]. Mass spectrometry, which directly detects and quantifies allergenic proteins and peptides, offers high specificity and multiplexing capabilities, emerging as a powerful tool for complex analytical challenges [43] [42].
Understanding the comparative performance characteristics of these methods is essential for developing effective allergen control plans, validating cleaning procedures, and ensuring accurate product labeling. This review synthesizes current research to guide method selection based on analytical requirements, food matrix properties, and regulatory considerations.
Performance Comparison of Detection Methods
Quantitative Performance Metrics Across Allergens
Table 1: Comparative sensitivity of ELISA, PCR, and MS methods for major food allergens
| Allergen | ELISA Sensitivity | PCR Sensitivity | MS Sensitivity | Key Protein/DNA Targets |
|---|---|---|---|---|
| Peanut | Low ppm levels [73] | Not specified | 0.01 ng/mL [7] | Ara h 3, Ara h 6 [7] |
| Milk | Low ppm levels [73] | Not specified | 0.01 ng/mL [7] | Bos d 5 [7] |
| Egg | Low ppm levels [73] | Not specified | 0.01 ng/mL [7] | Gal d 1, Gal d 2 [7] |
| Shellfish | Not specified | Not specified | 0.01 ng/mL [7] | Tropomyosin [7] |
| Pistachio | Cross-reactivity issues with cashew [43] | Cross-reactivity issues with cashew [43] | SDL: 1 mg/kg [43] | Pis v 1, Pis v 2, Pis v 3, Pis v 4, Pis v 5 [43] |
| Meat Allergens | Limited for processed meats [42] | Limited for processed meats [42] | LOD: 2.0-5.0 mg/kg [42] | Myoglobin, myosin light chain [42] |
| Wheat Gluten | CAC official method (20 mg/kg) [39] | Official method in Germany [39] | Not specified | HMW-GS, LMW-GS [74] |
Method Characteristics and Applicability
Table 2: General characteristics and performance parameters of ELISA, PCR, and MS methods
| Parameter | ELISA | PCR | Mass Spectrometry |
|---|---|---|---|
| Analytical Target | Proteins (antigen-antibody) [39] | DNA (allergen-specific sequences) [39] | Proteins/Peptides (mass-to-charge ratio) [43] [39] |
| Detection Principle | Antibody binding and enzymatic colorimetric reaction [39] | DNA amplification through thermal cycling [74] | Ion separation based on mass-to-charge ratio [43] |
| Multiplexing Capacity | Limited (single-analyte) [43] | Moderate (multiple primer sets) [74] | High (multiple allergens simultaneously) [7] [43] |
| Specificity Challenges | Antibody cross-reactivity [43] [39] | Cross-reactivity between similar species (e.g., pistachio/cashew) [43] | Minimal cross-reactivity [43] |
| Throughput | High [73] | Moderate to High [74] | Moderate [43] |
| Cost Profile | Cost-effective [73] | Moderate [73] | High (equipment and expertise) [43] |
| Regulatory Status | FDA, USDA approved; CAC official method for gluten [73] [39] | Official method in Germany, Japan [39] | Emerging for official controls [43] |
| Ideal Application | Routine screening of unprocessed or lightly processed foods [73] | Highly processed foods where proteins are denatured [73] | Complex matrices; requires unambiguous identification [43] [42] |
Experimental Protocols and Methodologies
ELISA-Based Allergen Detection
The ELISA method leverages the specific binding between antibodies and target allergenic proteins. The protocol begins with protein extraction from the food matrix using appropriate buffers, often requiring optimization for different matrix types [73] [39]. For processed foods, extraction may involve steps to renature proteins or expose hidden epitopes. The extracted samples are then added to microplate wells pre-coated with capture antibodies specific to the target allergen. After incubation and washing, a detection antibody conjugated to an enzyme (typically horseradish peroxidase or alkaline phosphatase) is added, forming an antibody-antigen-antibody sandwich complex [39].
Following additional washing steps to remove unbound antibodies, a substrate solution is added, which the enzyme converts to a colored product. The intensity of this color, measured spectrophotometrically, is proportional to the amount of allergen present in the sample [39]. Quantification is achieved by comparing sample absorbance to a standard curve generated with known concentrations of the purified allergen. The FDA and other regulatory bodies have established specific ELISA-based protocols for allergens like gluten, with a defined action level of 20 mg/kg [39] [2].
PCR-Based Allergen Detection
PCR methods target specific DNA sequences unique to allergenic foods, providing an indirect approach to allergen detection [74] [39]. The protocol initiates with DNA extraction from the food matrix using CTAB-based methods or commercial kits, designed to obtain high-quality DNA free from PCR inhibitors [74]. For processed foods, this step is critical as DNA fragmentation can occur during thermal processing, requiring optimization of extraction protocols.
Primer design is a crucial aspect, targeting species-specific genes or allergen-encoding sequences. For wheat detection, primers may target high-molecular-weight glutenin subunit (HMW-GS) or low-molecular-weight glutenin subunit (LMW-GS) genes, while for maize, targets include Zea m 14, Zea m 8, and zein genes [74]. To address DNA degradation in processed foods, amplicon size should be limited to 200-300 bp for reliable detection [74] [39]. The reaction mixture typically includes template DNA, specific primers, dNTPs, reaction buffer, and DNA polymerase. Thermal cycling involves denaturation (95°C), annealing (primer-specific temperature, typically 50-65°C), and extension (72°C) for 30-40 cycles. Amplification products are detected through gel electrophoresis, fluorescence, or other detection systems. Real-time PCR (qPCR) allows for quantification by monitoring fluorescence accumulation during each cycle [39].
Mass Spectrometry-Based Allergen Detection
LC-MS/MS methods for allergen detection directly target proteotypic peptides derived from allergenic proteins, offering high specificity and multiplexing capability [43] [42]. The protocol begins with protein extraction from the food matrix using optimized buffers, often containing chaotropic agents like urea or surfactants to improve solubility [42]. Extracted proteins are then reduced (typically with dithiothreitol, DTT) and alkylated (with iodoacetamide, IAA) to break disulfide bonds and prevent reformation.
Proteolytic digestion, most commonly with trypsin, follows to cleave proteins into peptides at specific amino acid residues (arginine and lysine) [43] [42]. The resulting peptide mixture undergoes purification, often via solid-phase extraction, to remove contaminants that may interfere with subsequent analysis. For quantification, stable isotope-labeled internal standard peptides are added, which co-elute with their native counterparts but are distinguished by mass [42].
Liquid chromatography separates the peptides based on hydrophobicity before introduction to the mass spectrometer. In the MS, peptides are ionized (typically via electrospray ionization) and separated in the first mass analyzer (Q1) based on their mass-to-charge ratio (m/z). Selected precursor ions are then fragmented via collision-induced dissociation, and the resulting product ions are analyzed in the second mass analyzer (Q3) [43] [42]. Detection utilizes multiple reaction monitoring (MRM), where specific precursor-product ion transitions are monitored for each target peptide, providing high specificity and sensitivity. Quantification is achieved by comparing the peak areas of native peptides to their corresponding internal standards [42].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for allergen detection methodologies
| Reagent/Material | Function | Application Across Methods |
|---|---|---|
| Specific Antibodies | Recognition and binding to target allergenic proteins | ELISA (capture and detection) [39] |
| Allergen-Specific Primers | Amplification of target DNA sequences | PCR (target identification) [74] |
| Stable Isotope-Labeled Peptides | Internal standards for quantification | MS (quantitative accuracy) [42] |
| Trypsin (Proteomics Grade) | Proteolytic digestion of proteins into peptides | MS (sample preparation) [43] [42] |
| DNA Polymerase (Taq) | DNA amplification through PCR | PCR (nucleic acid amplification) [74] |
| Magnetic Beads (Antibody-Coated) | Immunoaffinity capture of target proteins | ELISA, MS (sample enrichment) [39] |
| Chromatography Columns (C18) | Reversed-phase separation of peptides | MS (LC separation) [43] [42] |
| Reference Allergen Materials | Method calibration and quality control | All methods (standardization) [39] |
The comparative analysis of ELISA, PCR, and mass spectrometry reveals a complementary relationship between these analytical platforms in food allergen detection. ELISA remains the workhorse for routine testing due to its established protocols, regulatory acceptance, and cost-effectiveness, achieving detection sensitivities at low parts per million (ppm) levels for major allergens like peanut, milk, and egg [73]. PCR provides exceptional specificity and reliability for detecting allergens in processed foods where protein integrity is compromised, with optimized protocols targeting 200-300 bp amplicons to address DNA fragmentation during thermal processing [74] [39]. Mass spectrometry emerges as the most specific and versatile platform, capable of multiplexed detection of multiple allergens simultaneously with sensitivity reaching 0.01 ng/mL for key allergens, while directly targeting the allergenic proteins themselves rather than surrogate markers [7] [43].
The selection of an appropriate detection method must consider the specific analytical requirements, including the target allergen, food matrix complexity, processing history, and required sensitivity. As regulatory frameworks evolve and detection technologies advance, method harmonization and standardization will be crucial for improving the reliability and comparability of allergen detection data across laboratories and jurisdictions. Future developments in biosensors, hyperspectral imaging, and AI-enhanced detection platforms promise to further transform the landscape of food allergen testing, offering opportunities for real-time monitoring and predictive risk management [7].
Proficiency Testing (PT) is a cornerstone of quality assurance in analytical laboratories, providing an objective assessment of a laboratory's testing performance against established standards or peer laboratories. Within the critical field of food allergen detection and thresholds research, PT is indispensable for ensuring the reliability, accuracy, and comparability of data upon which public health decisions and regulatory frameworks are based. The fundamental purpose of PT is to use inter-laboratory comparisons to determine the performance of individual laboratories for specific tests or measurements and to monitor laboratories' continuing performance [citation4]. As global food supply chains become more complex and regulatory landscapes evolve, the demand for robust, validated analytical methods has intensified. The global laboratory proficiency testing market, valued at USD 1.58 billion in 2025 and projected to reach USD 1.98 billion by 2030, reflects this critical need for quality differentiation and compliance assurance [citation4].
In the specific context of food allergen research, establishing thresholds—the minimum dose of an allergenic protein that can elicit an adverse reaction in sensitive individuals—requires analytical methods of exceptional precision and reproducibility. The U.S. Food and Drug Administration (FDA) currently does not establish a threshold level for any allergens, underscoring the foundational role of analytical research in this domain [citation2]. The recent passage of the Food Allergy Safety, Treatment, Education, and Research (FASTER) Act, which declared sesame as the 9th major food allergen, further highlights the dynamic nature of this field and the continuous need for reliable data [citation2]. This technical guide will analyze the sources and magnitude of inter-laboratory variability revealed through PT data, with a specific focus on methodologies and implications for food allergen detection and threshold research.
Methodological Frameworks for Proficiency Testing
Core Design Principles for Effective PT Schemes
A well-designed proficiency testing scheme is structured to simulate routine testing conditions as closely as possible while maintaining the integrity necessary for objective inter-laboratory comparison. Effective PT design incorporates several key principles: the use of homogeneous and stable test samples, a statistically sufficient number of participant laboratories, predefined performance criteria, and robust data analysis protocols. The design must account for the specific analytical challenges of the target analytes—for food allergens, this includes considerations of matrix effects, protein extraction efficiency, and the potential for cross-contact. The primary objective is to identify variability arising from the analytical process itself, separate from sample preparation or data interpretation differences that might occur in real-world testing scenarios [citation1].
PT programs can be categorized by provider type, with independent/third-party providers holding 54.45% of the market share in 2024, a preference that underscores the importance of perceived objectivity in these assessments [citation4]. The structure of a PT typically involves a central coordinating body that prepares and distributes identical samples to all participating laboratories, which then analyze the samples using their standard operating procedures and report back their results within a specified timeframe. The coordinating body then analyzes the collective results, often using statistical methods detailed in Section 4, and provides individual feedback to participants along with a summary of overall performance.
Experimental Protocols for PT in Food Allergen Detection
Implementing a PT scheme for food allergen detection requires meticulous protocol development. The following detailed methodology is adapted from successful inter-laboratory studies in analogous fields, such as environmental surveillance, and tailored for allergen testing applications [citation1]:
Sample Generation and Homogenization: Prepare a stock of uniform test samples representing the food matrices commonly tested for allergen residues (e.g., baked goods, sauces, chocolate). For solid matrices, use cryogenic grinding to achieve a homogeneous particle size. The test materials should be spiked with known, varying concentrations of the target allergenic protein (e.g., peanut, milk, egg) covering the relevant range from detection limit to higher concentrations. The use of incurred samples (where the allergen is incorporated during processing) is preferable to spiked samples for better real-world relevance. Each sample is then split into identical aliquots for distribution.
Blinded Distribution: Distribute the blinded samples to participating laboratories with instructions mirroring routine sample handling procedures. Include necessary information on any potential hazards and storage conditions. A minimum of 5-8 laboratories is recommended for statistically meaningful results, though larger cohorts provide more robust data.
Defined Analytical Phase: While laboratories typically use their in-house validated methods, a PT may specify core pre-analytical and analytical processes to isolate specific sources of variability. For example, a study might mandate:
- Pre-analytical Process: A specific sample extraction protocol, such as using a standardized buffer solution and extraction time/temperature, to minimize variability from sample preparation [citation1].
- Analytical Process: The use of a specified reference material for creating standard curves in quantitative methods like ELISA or LC-MS/MS, as differences in standard curves have been identified as a primary source of quantitative variability [citation1].
Data Collection and Reporting: Establish a standardized reporting template requiring participants to provide raw data, calculated concentrations (with units), details of the method used (including kit lot numbers for commercial assays), and any relevant quality control measures observed during the analysis.
Inclusion of Controls: Incorporate negative control samples (free of the target allergen) and positive controls with a known, undisclosed concentration to assess false positive/negative rates and quantitative accuracy, respectively. A process control (e.g., a non-target protein to monitor recovery) can also be added to evaluate extraction efficiency [citation1].
The following workflow diagram illustrates the logical sequence of a standardized PT scheme, from development to final analysis.
Proficiency testing data consistently reveals multiple potential sources of variability in analytical measurements. Understanding and quantifying these sources is the first step toward method harmonization and improved data quality.
Analytical Phase Variability
The analytical phase—the process of quantifying the target analyte—often constitutes the most significant source of inter-laboratory discrepancy. A 2025 study evaluating interlaboratory variability in wastewater-based epidemiology, which shares methodological similarities with food allergen detection (e.g., trace analysis in complex matrices), used a two-way ANOVA framework within Generalized Linear Models. This analysis revealed that the primary source of variability was associated with the analytical phase itself [citation1]. This variability frequently stems from:
- Differences in Standard Curves: The use of different reference materials, standard concentrations, or curve-fitting algorithms by laboratories can lead to substantial quantitative differences, even when using the same instrumental platform [citation1].
- Methodological Differences: Variations in the core detection technology (e.g., different commercial ELISA kits, in-house versus commercial methods, or LC-MS/MS instrument configurations) contribute significantly to variability. Paracchini et al. (cited in [citation1]) confirm this variability on a large scale, noting differences across academia, industry, and public health laboratories.
- Instrument Calibration and Performance: Drift in instrument calibration over time or differences in performance characteristics between instruments of the same model can introduce error.
Pre-analytical and Sample-Related Variability
Variability introduced before the analytical measurement begins can be just as critical. Key factors include:
- Sample Concentration and Extraction Efficiency: Inefficient or inconsistent recovery of the target analyte from the complex food matrix is a major hurdle. Pecson et al. calculated that the theoretical Limit of Detection (LOD) of different Standard Operating Procedures (SOPs) could span seven orders of magnitude, highlighting the profound impact of pre-analytical methods on sensitivity and overall performance [citation1].
- Matrix Effects: The composition of the food matrix (e.g., fat, protein, carbohydrate content) can interfere with the detection method, leading to signal suppression or enhancement. Different extraction protocols may mitigate these effects to varying degrees.
- Operator Technique: Manual sample preparation steps are susceptible to differences in operator technique, despite detailed SOPs.
Data Analysis and Interpretation Variability
Finally, how data is processed and interpreted can vary between laboratories:
- Calculation Algorithms: Different approaches to calculating final concentrations from raw data (e.g., different methods of handling values below the LOD) can affect results.
- Criteria for Positivity: The threshold for determining a positive result (e.g., a signal-to-noise ratio) may not be uniformly applied.
The following diagram synthesizes these key sources of variability and their relationships into a single cause-and-effect structure.
Statistical Tools for Analyzing PT Data
Robust statistical analysis is required to transform raw PT data into meaningful insights about laboratory performance and methodological performance. The following methods are most commonly applied.
Analysis of Variance (ANOVA) Frameworks
ANOVA models are powerful for partitioning the total observed variance into its constituent components. A two-way ANOVA framework within Generalized Linear Models can be applied to determine whether variability is primarily associated with differences between samples, differences between laboratories, or an interaction effect. This approach was used effectively to identify the analytical phase as the main source of variability in a multi-laboratory study [citation1]. In practice, this involves setting the laboratory and the sample as fixed factors and testing for their main effects and interaction. A significant effect for the laboratory factor indicates systematic differences between laboratories (i.e., inter-laboratory bias).
Performance Evaluation Against Acceptance Criteria
Laboratory performance is often judged by comparing their results to predefined acceptance limits. These limits can be based on regulatory standards, such as the Clinical Laboratory Improvement Amendments (CLIA) criteria, which were updated with stricter limits effective in 2025 [75]. While CLIA specifically governs clinical laboratories, its framework for setting evidence-based, analyte-specific performance goals is a model for other fields. For food allergen testing, where formal federal thresholds do not yet exist, acceptance criteria might be derived from expert consensus or risk-based reference doses (RfDs), such as those recommended by the FAO/WHO expert committee (e.g., 2.0 mg total protein for peanut, 2.0 mg for milk) [14].
A laboratory's result for a PT sample is typically judged as acceptable if it falls within ± a specified percentage or absolute amount of the assigned value (the reference or consensus mean). The following table summarizes selected 2025 CLIA proficiency testing acceptance limits, illustrating the application of such criteria. The tightening of these standards over time reflects a global trend toward stricter quality requirements [75].
Table: Selected 2025 CLIA Proficiency Testing Acceptance Limits (Adapted from [75])
| Analyte or Test | 2025 CLIA Acceptance Criterion |
|---|---|
| Chemistry | |
| Albumin | Target Value (TV) ± 8% |
| Cholesterol, total | TV ± 10% |
| Creatinine | TV ± 0.2 mg/dL or ± 10% (greater) |
| Glucose | TV ± 6 mg/dL or ± 8% (greater) |
| Potassium | TV ± 0.3 mmol/L |
| Toxicology | |
| Blood lead | TV ± 10% or 2 mcg/dL (greater) |
| Digoxin | TV ± 15% or ± 0.2 ng/mL (greater) |
| Hematology | |
| Erythrocyte count | TV ± 4% |
| Hemoglobin | TV ± 4% |
| Leukocyte count | TV ± 10% |
Descriptive Statistics and Graphical Methods
Basic descriptive statistics provide the foundation for PT data analysis:
- Assigned Value: The value attributed to a particular property of a PT item, often determined as the consensus mean or median of participant results.
- Standard Deviation for Proficiency Assessment (sₚ): A measure of the spread of results used for proficiency assessment, often based on a robust standard deviation or a predefined standard.
- Z-Scores: A standardized performance statistic calculated as ( Z = (x{lab} - X)/sₚ ), where ( x{lab} ) is the laboratory's result, ( X ) is the assigned value, and ( sₚ ) is the standard deviation for proficiency assessment. A |Z| ≤ 2.0 is generally considered satisfactory, 2.0 < |Z| < 3.0 is questionable, and |Z| ≥ 3.0 is unsatisfactory.
Graphical methods such as Youden plots, which plot results for one sample against results for another to identify consistent laboratory bias, and histograms of all participant results, are invaluable for visualizing overall performance and identifying outliers.
The Scientist's Toolkit: Essential Reagents and Materials
The reliability of proficiency testing and food allergen research hinges on the quality and appropriateness of the research reagents and materials used. The following table details key solutions and their critical functions in the experimental workflow.
Table: Key Research Reagent Solutions for Food Allergen Proficiency Testing
| Item Category | Specific Examples / Protocols | Primary Function in PT/Research |
|---|---|---|
| Reference Materials & Controls | Certified Allergen Reference Materials (e.g., Peanut, Milk protein); Process Control Virus (e.g., Murine Norovirus) [citation1] | Provides a traceable benchmark for quantifying allergenic protein; monitors recovery efficiency during sample extraction and concentration steps. |
| Sample Concentration Reagents | Polyethylene Glycol (PEG) 8000; Sodium Chloride [citation1] | Concentrates trace levels of allergenic protein from large volume liquid samples or complex food matrix extracts, improving method sensitivity. |
| Nucleic Acid/Protein Extraction Kits | Commercial RNA extraction kits; Protein extraction buffers | Isolates and purifies the target analyte (allergenic protein or, for some methods, allergen-encoding DNA) from the complex food matrix, reducing interferents. |
| Molecular Detection Assays | qPCR assays targeting specific genes; ELISA kits; LC-MS/MS reference methods | Provides the specific mechanism for detecting and quantifying the presence and amount of the target allergen with high sensitivity and specificity. |
| Standard Curve Components | Synthetic DNA standards; Purified protein calibrators | Enables quantitative conversion of instrument signal (e.g., fluorescence, absorbance) into a specific concentration of the target analyte. |
Case Study: PT in Wastewater Surveillance and Lessons for Allergen Research
A 2025 inter-calibration study monitoring SARS-CoV-2 in wastewater provides a highly relevant case study on evaluating inter-laboratory variability. This study involved four laboratories analyzing three wastewater samples in parallel using identical pre-analytical (PEG-8000-based centrifugation) and analytical processes (qPCR) [citation1]. Despite this standardized protocol, robust statistical analysis using a two-way ANOVA framework and Bonferroni post hoc tests revealed that the primary source of variability was still associated with the analytical phase. The study authors concluded that this was "likely influenced by differences in the standard curves used by the laboratories to quantify SARS-CoV-2 concentrations" [citation1].
This finding offers critical lessons for food allergen threshold research:
- Protocol Standardization is Necessary but Not Sufficient: Even with a unified SOP, subtle differences in implementation (like standard curve construction) can drive significant variability.
- Statistical Methods are Key to Diagnosing Variability: The use of advanced statistical models like two-way ANOVA is crucial for moving beyond simple pass/fail metrics and identifying the root cause of discrepancies.
- Implications for Allergen Thresholds: Establishing definitive thresholds for food allergens (e.g., the eliciting dose for 5% of the population, or ED05) requires analytical methods that produce consistent results across different laboratories. The variability observed in even controlled PT studies underscores the challenge in defining a single, universal threshold that is independent of the detection methodology. This reinforces the importance of ongoing PT and method harmonization efforts, such as those discussed by the FAO/WHO committee, to build a reliable evidence base for potential future regulatory thresholds [citation9].
The analysis of proficiency testing data provides an unambiguous, quantitative measure of real-world inter-laboratory variability, serving as a critical diagnostic tool for improving analytical quality in food allergen research. The consistent identification of the analytical phase—particularly differences in standard curves and methodological platforms—as a primary source of discrepancy highlights a key area for standardization efforts. As research continues to refine understanding of food allergen thresholds, the reliability of the underlying analytical data is paramount. Future efforts must focus on the development of certified reference materials for major allergens, the validation of harmonized standard operating procedures, and the wider adoption of routine proficiency testing. By systematically identifying and mitigating the sources of variability revealed through PT, the scientific community can generate the robust, reproducible data necessary to support evidence-based food safety policies, allergen labeling regulations, and ultimately, improved public health protection for allergic individuals.
In the field of food safety, the precise detection and quantification of allergenic proteins is a critical public health imperative. For the millions of individuals living with food allergies, accurate food labeling represents their primary defense against potentially life-threatening reactions [2]. The analytical sciences supporting allergen detection operate at the intersection of immunology, food chemistry, and regulatory policy, where the operational definitions of Limits of Detection (LOD) and Quantification (LOQ) carry significant implications for both consumer protection and industry practice [18]. Unlike chemical contaminants with established toxicological thresholds, allergenic proteins present unique analytical challenges due to the complex interplay between protein structure, matrix effects, and individual immune response variability [39]. This technical guide examines the fundamental principles, methodological frameworks, and persistent challenges in defining and reporting LOD and LOQ for food allergens, providing researchers with a comprehensive resource for advancing this rapidly evolving field.
Operational Definitions and Fundamental Concepts
Distinguishing Detection from Quantification
In allergen analysis, the Limit of Detection (LOD) and Limit of Quantification (LOQ) represent distinct performance characteristics that must be clearly defined in any analytical method.
- Limit of Detection (LOD): The lowest concentration of an allergenic protein that can be reliably distinguished from a blank sample, typically with a signal-to-noise ratio of 3:1. The LOD answers the fundamental question of presence or absence but does not provide accurate concentration data [39].
- Limit of Quantification (LOQ): The lowest concentration at which the allergenic protein can be quantitatively determined with acceptable precision and accuracy (typically ±20% and signal-to-noise ratio of 10:1). The LOQ establishes the threshold for reliable measurement that informs risk assessment decisions [76].
These parameters are particularly challenging to establish for food allergens due to the protein complexity and matrix effects that influence analytical performance. The absence of universally accepted reference materials further complicates inter-laboratory comparisons and method validation [18].
Conceptual Relationship to Biological Response
A critical consideration in allergen detection is the relationship between analytical sensitivity (LOD/LOQ) and biological relevance (minimum eliciting dose). Reference doses established by international bodies provide guidance on threshold levels that protect most allergic consumers, creating a target for analytical method development [18].
Table 1: FAO/WHO Recommended Reference Doses for Priority Allergens
| Global Priority Allergen | Recommended Reference Dose (mg total protein) |
|---|---|
| Tree nuts (walnut, pecan, cashew, pistachio, almond) | 1.0 |
| Milk | 2.0 |
| Peanut | 2.0 |
| Egg | 2.0 |
| Sesame | 2.0 |
| Hazelnut | 3.0 |
| Wheat | 5.0 |
| Fish | 5.0 |
| Shrimp | 200 |
The ideal analytical method would have LOQ values sufficient to detect allergens below these reference doses in typical food servings, though this remains challenging for highly potent allergens like tree nuts at their reference dose of 1.0 mg total protein [18].
Current Methodological Approaches
Protein-Based Detection Methods
Immunoassays, particularly Enzyme-Linked Immunosorbent Assay (ELISA), remain the gold standard for allergen detection due to their specificity, sensitivity, and commercial availability. ELISA methods directly target allergenic proteins or epitopes using antibody-antigen interactions, providing a functional measurement that often correlates with allergenic potential [39]. However, these methods face limitations with processed foods where protein denaturation alters antibody recognition sites [18].
Mass spectrometry (MS) has emerged as a powerful complementary technique, particularly liquid chromatography-tandem mass spectrometry (LC-MS/MS). MS methods target signature peptides unique to specific allergens, offering multiplexing capabilities and greater specificity through sequence verification [18]. The ThRAll project has developed MS-based prototype reference methods for six major allergens (cow's milk, hen's egg, soybean, peanut, hazelnut, and almond) using incurred matrices that mimic highly processed foods [76].
Table 2: Comparison of Major Allergen Detection Methodologies
| Method Type | LOD Range | Advantages | Limitations |
|---|---|---|---|
| ELISA | 0.1-5 ppm (varies by allergen) | High throughput, commercial availability, cost-effective | Susceptible to protein denaturation, antibody cross-reactivity |
| Lateral Flow | 1-10 ppm | Rapid, on-site testing, minimal training | Semi-quantitative, lower sensitivity |
| PCR | 5-50 ppm | Resilient to processing, specific to species | Indirect (measures DNA, not protein), correlation to protein uncertain |
| Mass Spectrometry | 0.5-10 ppm | High specificity, multiplexing, absolute quantification | Complex sample preparation, expensive instrumentation, requires expertise |
Emerging Biosensor Technologies
Biosensors represent the next generation of allergen detection tools, combining biological recognition elements with transducer systems to create rapid, sensitive platforms. Recent developments include electrochemical immunosensors for simultaneous detection of multiple peanut allergens and aptamer-based sensors targeting tropomyosin in shrimp [39]. These platforms show particular promise for on-site testing in production environments where rapid results can inform manufacturing decisions. The integration of microfluidic technologies with biosensors further enhances their potential for portable, user-friendly applications [39].
Experimental Protocols for Method Validation
Establishing LOD and LOQ for ELISA Methods
The following protocol outlines the standardized approach for determining LOD and LOQ in immunoassays, based on established guidelines for allergen detection methods [39]:
Preparation of Calibration Standards: Create a dilution series of the purified allergen protein in appropriate buffer and analyte-free food matrix. Include at least six concentration points spanning the expected detection range.
Analysis of Blank Samples: Process and analyze at least 20 replicates of the blank (allergen-free) matrix to establish baseline signal distribution.
Calculation of LOD: Determine the mean signal of blanks plus three times the standard deviation of blank replicates. Convert this signal value to concentration using the standard curve.
Determination of LOQ: Identify the lowest standard concentration that can be measured with intra- and inter-assay precision of ±20% CV and accuracy of 80-120%.
Matrix Effects Assessment: Validate LOD/LOQ in various food matrices (chocolate, baked goods, broth powders) to account for extraction efficiency differences [76].
MS-Based Allergen Quantification Workflow
Mass spectrometry methods require specialized approaches for LOD/LOQ determination [76]:
Signature Peptide Selection: Identify proteotypic peptides unique to the target allergen that are stable during processing and detectable by MS.
Internal Standard Incorporation: Use stable isotope-labeled peptide analogs as internal standards to correct for ionization efficiency variations.
Sample Preparation Optimization: Employ extraction buffers that maximize protein solubility while minimizing interference, such as the optimized buffer developed for oyster allergen extraction [18].
LC-MS/MS Analysis: Implement multiple reaction monitoring (MRM) transitions for each target peptide, with at least three transitions per analyte for confirmation.
Data Processing: Use peak area ratios of native to isotope-labeled peptides for quantification, with LOD/LOQ determined from the signal-to-noise ratio in the matrix.
The following workflow diagram illustrates the complete process for establishing LOD and LOQ using MS-based approaches:
Critical Challenges in Reporting and Standardization
Methodological Limitations and Variability
The determination and reporting of LOD and LOQ values face several persistent challenges that impact their utility in risk assessment:
Matrix Effects: The same allergen may exhibit different extraction efficiencies and detection capabilities across food matrices. For example, chocolate and broth powders present particularly challenging matrices due to tannin interference and high salt content, respectively [76]. This necessitates matrix-specific LOD/LOQ reporting rather than universal values.
Processing Impact: Thermal processing, fermentation, and hydrolysis can alter protein structure and epitope recognition, significantly affecting method performance. Studies demonstrate that ELISA may fail to detect allergens in thermally processed samples, while PCR maintains sensitivity but loses correlation with protein content [18].
Reference Material Absence: The lack of standardized reference materials for most allergens creates substantial inter-laboratory variability. Without harmonized calibrants, LOD/LOQ values reported in different studies cannot be directly compared [18].
Inconsistent Terminology and Reporting Standards
The field suffers from inconsistent terminology that obscures method performance and limitations:
Variable Definitions: Some methods report "detection limits" based on buffer-spiked samples rather than incurred matrices, creating artificially optimistic performance claims [39].
Epitope Recognition: Immunoassays may detect different epitopes (linear vs. conformational) without clear reporting of how this affects the clinical relevance of detected proteins [18].
Units Inconsistency: Reported values may use varying units (ppm, μg/g, mg total protein) without clear conversion factors, complicating comparison across studies [18].
The Researcher's Toolkit: Essential Reagents and Materials
Successful implementation of allergen detection methods requires carefully selected reagents and reference materials. The following table details essential components for establishing reliable LOD and LOQ values:
Table 3: Essential Research Reagents for Allergen Detection and Quantification
| Reagent/Material | Function | Technical Considerations |
|---|---|---|
| Monoclonal/Polyclonal Antibodies | Molecular recognition of allergen epitopes in immunoassays | Specificity, affinity, recognition of linear vs. conformational epitopes |
| Stable Isotope-Labeled Peptides | Internal standards for MS-based quantification | Sequence match to native peptides, purity, position of labeled amino acids |
| Certified Reference Materials | Method calibration and quality control | Protein purity, characterization, stability, commutability with food matrices |
| Allergen-Specific Primers/Probes | DNA targets for PCR detection | Specificity, amplicon size, resistance to degradation during processing |
| Extraction Buffers | Protein solubilization and recovery | Compatibility with detection method, inhibition removal, stability |
| Incurred Reference Materials | Method validation in realistic conditions | Homogeneity, stability, characterization of allergen content |
Future Perspectives and Concluding Remarks
The field of allergen detection continues to evolve with several promising developments aimed at addressing current LOD/LOQ challenges. Multiplexed detection platforms capable of simultaneously quantifying multiple allergens in a single analysis are gaining traction, with microarray immunoassays and multiplex MS panels showing particular promise [18]. International harmonization efforts, such as the ThRAll project and FAO/WHO expert consultations, are working to establish standardized protocols and data reporting requirements that will enhance comparability across studies [76].
The growing application of biosensors and rapid screening methods addresses the need for on-site detection tools, though these technologies must still demonstrate reliability comparable to laboratory methods [39]. As mass spectrometry becomes more accessible and sensitive, its role as a reference method is likely to expand, particularly for complex matrices and processed foods where immunoassays struggle with accuracy [18].
Ultimately, progress in defining and applying LOD and LOQ values for allergen detection requires closer collaboration between analytical chemists, clinical researchers, and regulatory scientists. Only through this interdisciplinary approach can we develop detection methods whose operational limits align with the biological thresholds that protect allergic consumers while supporting feasible manufacturing practices. The establishment of clinically relevant reference doses by international bodies represents a significant step forward, but translating these health-based guidance values into analytical performance criteria remains an ongoing challenge for the field.
The management of food allergens represents a significant global public health challenge, affecting millions of individuals and requiring rigorous scientific approaches to ensure safety. Within this field, a substantial standardization gap impedes progress in establishing reliable, reproducible, and actionable safety frameworks. This gap manifests primarily in the lack of harmonized reference materials and standardized analytical methods for detecting and quantifying allergenic proteins in food products. The absence of these fundamental tools creates inconsistencies in data generation, complicates risk assessment, and ultimately jeopardizes the safety of food-allergic consumers. Research indicates that food allergies affect approximately 8% of children and 11% of adults in the United States, highlighting the scale of the population reliant on accurate food allergen management [77]. Despite this significant health burden, the current analytical landscape is characterized by variability that undermines the development of evidence-based thresholds and effective regulatory policies. This whitepaper examines the critical need for harmonization in food allergen research, detailing the current limitations, ongoing initiatives, and essential tools required to bridge this standardization gap and advance public health protection.
Current Challenges and Limitations in Allergen Analysis
The Variability in Analytical Methods and Targets
The fundamental challenge in food allergen analysis stems from the diversity of analytical platforms and the lack of agreement on molecular targets. Current detection and quantification methods primarily include immunoassays (ELISA), polymerase chain reaction (PCR), and mass spectrometry (MS), each with distinct limitations and variabilities. As noted by researchers, "all current analytical approaches exhibit severe deficiencies" that can only be addressed through proper use of appropriate reference materials [78]. This variability is particularly pronounced in immunoassays, where different kits may target diverse fractions of the same allergenic molecule, leading to inconsistent results. For instance, with gluten analysis, the lack of a clearly defined analyte and agreed-upon common marker or conversion factor results in significant variability between different test kits [79]. Even when using a common calibrant, inherent differences in antibody selectivity persist, generating data that are not directly comparable across studies or jurisdictions. This inconsistency presents a major obstacle for food business operators implementing risk assessment plans and for regulators establishing enforcement protocols.
The Impact of Processing on Allergen Detection
A further complication arises from the impact of food processing on allergen detection. Food processing techniques can alter the structure of allergenic proteins, affecting their detectability by analytical methods without necessarily reducing their allergenicity. Antibodies used in ELISA methods may not recognize denatured or aggregated proteins, while MS methods might target peptides that become inaccessible or modified during processing. This creates a disconnect between what is measured analytically and what may actually trigger an allergic reaction in sensitized individuals. The problem is particularly acute for methods that rely on DNA detection (PCR), as the presence of DNA does not directly correlate with the presence of allergenic protein. The need for reference materials that represent "real-world" processed foods, rather than simple raw ingredients, is therefore critical for method development and validation. As highlighted by research initiatives, developing incurred matrices that mimic highly processed foods is essential for improving the relevance and reliability of allergen detection methods [76].
Essential Research Reagent Solutions: A Scientist's Toolkit
The development of reliable allergen detection methods depends critically on access to well-characterized reagents and materials. The following table summarizes the key research reagent solutions required for advancing food allergen analysis:
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Certified Reference Materials (CRMs) | Skim milk powder (BCR-685), Whole milk powder (NIST SRM 1549a), Peanut butter (NIST SRM 2387) [79] | Provide traceable calibrants for quantitative analysis; enable method harmonization across laboratories. |
| Incurred Processed Matrices | Milk powder cookies (MoniQA), Chocolate dessert with peanut (LGCQC101-KT), Incurred chocolate bars & broth powder (ThRAll project) [79] [76] | Mimic real-world processed foods; validate method performance for different food matrices and processing conditions. |
| Characterized Allergen Ingredients | Light roasted peanut flour (LGCQC1020), Spray-dried whole egg (NIST SRM 8445), Peanut kit with varying roast levels (IRMM-481) [79] | Provide raw materials of known composition and protein content for method development and quality control. |
| Protein Extracts & Antigens | Allergen-specific extracts for immunoassays (e.g., caseins, whey proteins, Ara h peptides) [80] | Serve as critical reagents for antibody production, assay calibration, and epitope characterization. |
| Quality Control Materials | Biscuits containing hazelnut/peanut (T27171QC), Cake mix with gluten/egg/milk (FCAL7-PRO10RM) [79] | Enable routine monitoring of analytical performance and inter-laboratory proficiency testing. |
The availability and proper utilization of these reagents form the foundation for reliable allergen analysis. Particularly important is the development of incurred processed food matrices, where allergenic ingredients are incorporated into a food matrix and subjected to processing conditions that mimic commercial manufacturing. These materials help address the critical challenge of detecting allergens in complex, processed food systems, which is essential for generating data that accurately reflects real-world scenarios [79].
Standardized Experimental Protocols for Allergen Detection and Quantification
The ThRAll Project's MS-Based Reference Method Framework
The "Detection and Quantification of Allergens in Foods and Minimum Eliciting Doses in Food-Allergic Individuals" (ThRAll) project, funded by the European Food Safety Authority (EFSA), has developed a systematic approach for creating harmonized reference methods. The project focuses on establishing a quantitative mass spectrometry-based prototype reference method for six key allergenic foods: cow's milk, hen's egg, soybean, peanut, hazelnut, and almond [76]. The experimental workflow involves multiple critical stages, beginning with the use of well-characterized reference and quality control materials from established sources (iFAAM, MANOE, Allersens, MoniQA, and LGC Standards). The protocol then utilizes specifically designed incurred matrices that mimic highly processed foods, ensuring that methods are validated against relevant and challenging sample types. Key steps in the methodology include: (1) protein extraction from the food matrix under standardized conditions, (2) enzymatic digestion using specific proteases (typically trypsin) to generate signature peptides, (3) liquid chromatography separation coupled to tandem mass spectrometry (LC-MS/MS) for peptide detection and quantification, and (4) data analysis using stable isotope-labeled peptide standards for precise quantification [76]. This targeted MS approach provides a potential reference method against which other rapid screening methods can be validated.
Validation Guidelines for Immunoassays
For immunoassay-based methods, the AOAC International has published updated validation guidelines for food allergen immunoassays (Appendix M), which provide a standardized framework for assessing method performance [81]. These guidelines specify detailed protocols for validation studies, including requirements for sensitivity, specificity, accuracy, precision, and robustness. The experimental parameters defined include: (1) detection limits (LOD) and quantification limits (LOQ) determined in appropriate food matrices, (2) cross-reactivity assessments against a panel of related and unrelated food commodities, (3) reproducibility studies across multiple laboratories, operators, and days, and (4) stability studies evaluating reagent and sample storage conditions. The guidelines also address the critical issue of calibrator characterization, requiring that calibrants be traceable to well-defined reference materials whenever possible. By following these standardized validation protocols, researchers can generate comparable data across different platforms and locations, thereby enhancing the reliability of allergen detection results used for regulatory decisions and risk assessments.
Visualization of Method Harmonization and Reference Material Development
The Path to Harmonized Allergen Analysis
The following diagram illustrates the interconnected components required to achieve harmonized allergen analysis and how they address the current standardization gap:
Reference Material Development Workflow
The development of certified reference materials follows a rigorous process to ensure reliability and traceability, as illustrated below:
Global Initiatives and Future Directions
Ongoing International Collaborations
Significant international efforts are underway to address the standardization gap in food allergen analysis. Key initiatives include:
The ThRAll Project: This EFSA-funded collaboration between research institutions across Europe aims to develop harmonized reference methods for allergen detection and generate quality data on minimum eliciting doses [76]. The project focuses on creating a toolbox for quality data generation from low-dose oral food challenges and establishing standardized protocols for data collection and curation.
iFAAM Consortium: This large-scale international project has worked to develop integrated approaches to food allergen risk assessment and management. It has contributed to the development of reference materials and ring-trial testing protocols for method validation [78].
AOAC International: The Gluten and Food Allergens (GFA) program, launched in 2021, has developed validation guidelines for both food allergen and gluten methods through dedicated working groups [81]. The recently published Appendix M provides specific guidance on validation protocols for immunoassays.
VITAL Program 4.0: The Allergen Bureau's Voluntary Incidental Trace Allergen Labelling program represents a risk-based approach for precautionary allergen labelling. The latest version incorporates updated reference doses and supports quantitative risk assessments for the food industry [82].
The Critical Role of Common Data Elements
Beyond reference materials and methods, there is a growing recognition of the need for standardized data collection and reporting in food allergy research. The development of Common Data Elements (CDEs) for food allergy clinical trials represents a crucial step toward data harmonization [77]. CDEs are standardized, precisely defined questions paired with specific allowable responses, used systematically across different studies to ensure consistent data collection. The National Institutes of Health (NIH) has supported the development of FA-specific CDEs to facilitate data interoperability and alignment with the FAIR (Findable, Accessible, Interoperable, and Reusable) principles. Initiatives such as the Core Outcome Measures for Food Allergy (COMFA) and the Food Allergy Data Dictionary (FADD) are working to establish these standardized data elements, which will enable more effective pooling and comparison of data from multiple studies [77]. This harmonization of clinical data is essential for establishing reliable dose-response relationships and evidence-based allergen thresholds.
The standardization of reference materials and analytical methods represents a fundamental prerequisite for advancing food allergen research and protecting public health. Significant progress has been made through international collaborations, development of incurred reference materials, and establishment of validation guidelines. However, critical gaps remain in achieving full harmonization across methods, platforms, and jurisdictions. The path forward requires sustained commitment to several key priorities: (1) expanding the range of available certified reference materials to cover priority allergens and processed matrices, (2) establishing internationally recognized sets of analytical targets and standardized protocols, (3) implementing common data elements for consistent reporting of clinical and analytical data, and (4) promoting global alignment on risk assessment approaches and regulatory frameworks. By addressing these priorities, the scientific community can bridge the current standardization gap and establish a robust foundation for evidence-based food allergen management that reliably protects sensitive consumers while supporting innovation in the food industry.
Conclusion
The precise determination of food allergen thresholds and the selection of fit-for-purpose detection methodologies are foundational to accurate risk assessment and the protection of allergic consumers. This synthesis underscores that while established methods like ELISA remain workhorses, their limitations in processed foods necessitate a complementary approach incorporating advanced techniques like MS and emerging AI tools. A critical takeaway is that methodological choice must be guided by a deep understanding of the allergen's form, the food matrix, and the required clinical relevance. Future progress hinges on closing key evidence gaps: the development of harmonized, incurred reference materials; the establishment of scientifically robust regulatory thresholds for all major allergens; and the continued innovation of rapid, multi-allergen, and point-of-use platforms. For biomedical research, these advances will directly enable more refined clinical studies on threshold stability, empower the development of novel therapeutics and diagnostics, and ultimately contribute to a more predictive and personalized approach to food allergy management.
References
- 1. dose - Wikipedia Threshold [https://en.wikipedia.org/wiki/Threshold_dose]
- 2. Food Allergies [https://www.fda.gov/food/nutrition-food-labeling-and-critical-foods/food-allergies]
- 3. Food allergy thresholds, context, and balance in 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322902/]
- 4. of Definition Dose Descriptors (LD50, LC50, EC50...) Toxicological [https://www.chemsafetypro.com/Topics/CRA/Toxicology_Dose_Descriptors.html]
- 5. Use of acceptable daily intake (ADI) as a health-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8138992/]
- 6. Statistical Considerations in the Evaluation of Continuous ... [https://jnm.snmjournals.org/content/62/5/605]
- 7. Innovations shaping the future of food allergen testing [https://allergenbureau.net/innovations-shaping-the-future-of-food-allergen-testing/]
- 8. An overview of statistical methods for biomarkers relevant to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11371698/]
- 9. THRESHOLD: a comprehensive transcriptomic analysis tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574675/]
- 10. Criteria for Acceptable Dietary Intake Biomarkers - PubMed [https://pubmed.ncbi.nlm.nih.gov/35642392/]
- 11. Food allergens | Food safety and quality [https://www.fao.org/food-safety/scientific-advice/food-allergens/en/]
- 12. Understanding Global Food Allergens: FAO/WHO Risk ... [https://www.anaphylaxis.org.uk/my-account/media-centre/membership-news/understanding-global-food-allergens-fao-who-risk-assessment/]
- 13. Ad hoc Joint FAO/WHO Expert Consultation on Risk ... [https://www.who.int/news-room/events/detail/2025/11/03/default-calendar/ad-hoc-joint-fao-who-expert-consultation-on-risk-assessment-of-food-allergens-reference-doses-for-cereals-containing-gluten-or-gluten]
- 14. FAO/WHO Set Allergen Thresholds. Will the U.S.? - [https://achesonfoodsafetyconsulting.com/fao-who-set-allergen-thresholds-will-the-u-s/]
- 15. Guidelines for the use and interpretation of diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4593201/]
- 16. A new way forward? Examining the potential of quantitative ... [https://aacijournal.biomedcentral.com/articles/10.1186/s13223-022-00717-8]
- 17. Identifying thresholds of reaction for different foods - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11382767/]
- 18. Analytical Methods for Allergen Control in Food Processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093617/]
- 19. Food allergens - EFSA - European Union [https://www.efsa.europa.eu/en/safe2eat/food-allergens]
- 20. Food allergen analysis: Considerations for establishing a ... [https://www.sciencedirect.com/science/article/pii/S0308814623010099]
- 21. Food Allergen Labeling and Consumer Protection Act of 2004 ( FALCPA ) [https://www.fda.gov/food/food-allergensgluten-free-guidance-documents-regulatory-information/food-allergen-labeling-and-consumer-protection-act-2004-falcpa]
- 22. How FARE Advocates Helped Pass the FASTER Act [https://www.foodallergy.org/resources/how-fare-advocates-helped-pass-faster-act]
- 23. The FASTER Act: What Food Companies Need to Know ... [https://www.reedsmith.com/en/perspectives/2022/12/the-faster-act]
- 24. Update to FDA Guidance for Food Allergen Labeling - FoodAllergy.org [https://www.foodallergy.org/fare-blog/update-fda-guidance-food-allergen-labeling]
- 25. Food Allergen Labeling Guidance for Industry [https://www.fda.gov/food/food-allergensgluten-free-guidance-documents-regulatory-information/frequently-asked-questions-food-allergen-labeling-guidance-industry]
- 26. Federal Register :: Major Food Allergen Labeling for Wines, Distilled... [https://www.federalregister.gov/documents/2025/01/17/2025-00955/major-food-allergen-labeling-for-wines-distilled-spirits-and-malt-beverages]
- 27. An overview of ELISA: a review and update on best laboratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11808753/]
- 28. ELISA Assay Technique | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa.html]
- 29. New study cracks walnut allergy thresholds [https://allergenbureau.net/new-study-cracks-walnut-allergy-thresholds/]
- 30. How to Analyze ELISA Data and Calculate Results [https://www.bosterbio.com/blog/post/how-to-analyze-elisa-data-and-calculate-results-step-by-step-guide-with-troubleshooting-tips?srsltid=AfmBOor-2X6HALwd4wuii-ad3yavLD9k6PKaH5TGYj_N274ONmC3wmgN]
- 31. Next-Generation ELISA (ELISA 2.0) Market Research ... [https://www.insightaceanalytic.com/report/next-generation-elisa-market/3241]
- 32. A rapid and highly sensitive biomarker detection platform ... [https://www.nature.com/articles/s41598-020-75011-x]
- 33. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 34. Introduction to Quantitative PCR (qPCR) Gene Expression ... [https://www.thermofisher.com/us/en/home/life-science/pcr/real-time-pcr/real-time-pcr-learning-center/gene-expression-analysis-real-time-pcr-information/introduction-gene-expression.html]
- 35. Polymerase Chain Reaction (PCR) - StatPearls - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK589663/]
- 36. Methods to determine limit of detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5496743/]
- 37. The How and Why of Limit of Detection [https://bitesizebio.com/44092/how-to-calculate-the-limit-of-detection-for-an-assay-and-why-youd-want-to/]
- 38. How to characterize the Limit of Blank and ... [https://www.stillatechnologies.com/digital-pcr/naica-system-analysis/how-to-characterize-the-limit-of-blank-and-the-limit-of-detection-in-crystal-digital-pcr/]
- 39. Research progress on detection methods for food allergens [https://www.sciencedirect.com/science/article/abs/pii/S0889157524009402]
- 40. Advanced Analysis of Allergens in Foods: LC–MS ... [https://www.spectroscopyonline.com/view/advanced-analysis-allergens-foods-lc-ms-ms-methodologies-and-future-insights]
- 41. Simultaneous analysis of 12 food allergens in baked and ... [https://sciex.com/tech-notes/food-beverage/food-and-beverage/simultaneous-analysis-of-12-food-allergens-in-baked-and-raw-food]
- 42. Development and validation of an LC-MS/MS method for a ... [https://www.sciencedirect.com/science/article/abs/pii/S0308814625032169]
- 43. Allergens in Food: Analytical LC-MS/MS Method for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428185/]
- 44. Advances in Food Processing Techniques for Allergenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12651889/]
- 45. Virtual Public Meeting and Listening Session on Food ... [https://www.fda.gov/food/workshops-meetings-webinars-food-and-dietary-supplements/virtual-public-meeting-and-listening-session-food-allergen-thresholds-and-their-potential]
- 46. Food Allergenicity Evaluation Methods: Classification, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191692/]
- 47. The Science of Allergen Detection: Lateral Flow and ELISA ... [https://www.prognosis-biotech.com/news-events/the-science-of-allergen-detection-lateral-flow-and-elisa-explained/]
- 48. Lateral Flow Technology [https://www.hygiena.com/learning-center/technology-guide/lateral-flow-technology-for-fast-and-easy-hygiene-and-food-safety-testing]
- 49. Food Allergen Analysis [https://allergenbureau.net/food-allergens/food-allergen-analysis/]
- 50. Comparison of Detection Limits for Allergenic Foods ... [https://www.sciencedirect.com/science/article/pii/S0362028X22103376]
- 51. UK FSA's review of main allergen detection methods [https://allergenbureau.net/uk-fsas-review-of-main-allergen-detection-methods/]
- 52. Your Guide to Adenosine Triphosphate (ATP) Testing [https://www.neogen.com/en/usac/neocenter/blog/your-guide-to-atp-testing/]
- 53. How AI Is Transforming Food Allergy Care [https://foodallergyinstitute.com/for-providers/how-ai-is-transforming-food-allergy-care]
- 54. Review: Food processing and allergenicity [https://www.sciencedirect.com/science/article/pii/S0278691515000848]
- 55. The Effect of Food Processing on Food Allergens. Important ... [https://nutriterra.org/ro/effect-food-processing-food-allergens-important-aspects-covid-19/]
- 56. Traditional and Emerging Physical Processing Technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12168111/]
- 57. Unraveling the mysteries of food allergens: aptamer-driven ... [https://www.sciencedirect.com/science/article/abs/pii/S0963996925013596]
- 58. Detection of Food Allergens by Taqman Real-Time PCR ... [https://pubmed.ncbi.nlm.nih.gov/28315214/]
- 59. United States Food Allergen Testing Market Trends ... [https://vocal.media/feast/united-states-food-allergen-testing-market-trends-and-summary-2025-2033]
- 60. Interactions between food matrices and odorants: A review [https://www.sciencedirect.com/science/article/abs/pii/S0308814624037361]
- 61. Tannins in Food: Insights into the Molecular Perception of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7321337/]
- 62. A systematic review of allergen cross-reactivity: Translating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10959674/]
- 63. Food Allergies and Cross-Reactivity [https://kidswithfoodallergies.org/living-with-food-allergies/what-is-a-food-allergy/food-allergies-and-cross-reactivity/]
- 64. An Allergen Portrait Gallery: Representative Structures and an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2964044/]
- 65. Cross Reactivity & Food Allergies [https://www.thermofisher.com/diagnostic-education/patient/ca/en/understanding-allergies/cross-reactivity.html]
- 66. Food Allergies: Detection and Management [https://www.aafp.org/pubs/afp/issues/2008/0615/p1678.html]
- 67. Spike and Recovery and Linearity of Dilution Assessment [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/overview-elisa/spike-recovery-linearity-assessment.html]
- 68. Spike and Recovery: How to Generate Reliable Data [https://www.cygnustechnologies.com/generating-spike-recovery-analysis-data?srsltid=AfmBOoqbRT1n-Pajii3DJ30VZZEzUdGViw8cGPNqgAvG1Rs7uR5GM5LM]
- 69. A critical view on spike recovery for accuracy evaluation ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708511007412]
- 70. Validation Procedures for Quantification of Food Allergens ... [https://pubmed.ncbi.nlm.nih.gov/37737992/]
- 71. Repeat Analysis and Incurred Sample Reanalysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389737/]
- 72. Essential Guide to ISR in Bioanalysis [https://www.celegence.com/incurred-sample-reanalysis-bioanalysis-guide/]
- 73. The Growing Importance of Allergen Testing: How Certified ... [https://fsns.com/the-growing-importance-of-allergen-testing-how-certified-group-ensures-food-safety-with-elisa/]
- 74. Development of PCR Methods for Detecting Wheat and Maize ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551070/]
- 75. 2025 CLIA Acceptance Limits for Proficiency Testing [https://www.westgard.com/clia-a-quality/quality-requirements/2024-clia-requirements.html]
- 76. Detection and Quantification of Allergens in Foods ... [https://www.food.gov.uk/research/background-and-objectives-detection-and-quantification-of-allergens-in-foods-and-minimum-eliciting-doses-in-food-allergic]
- 77. Common data elements for food allergy clinical trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12043398/]
- 78. FSA FS101206 Development of Quality for Control ... Materials Food [https://research.manchester.ac.uk/en/projects/fsa-fs101206-development-of-quality-control-materials-for-food-al/]
- 79. Development of reference : materials , Reference ... materials quality [https://www.food.gov.uk/research/development-of-reference-materials-reference-materials-quality-control-and-harmonisation-of-analysis]
- 80. source Allergen and materials of quality extracts control allergenic [https://pubmed.ncbi.nlm.nih.gov/9281463/]
- 81. New Food Allergen Method Validation Guidelines Published [https://www.aoac.org/news/new-food-allergen-method-validation-guidelines-published-oma-appendix-m-revised/]
- 82. International Developments on Allergen Labelling [https://foodallergycanada.ca/international-developments-on-allergen-labelling-spring-2025-issue/]