Essential Fatty Acid Deficiency Prevention: Advanced Strategies for Researchers and Drug Development
This article provides a comprehensive analysis of contemporary strategies for preventing Essential Fatty Acid Deficiency (EFAD), with a focus on challenges and innovations relevant to researchers, scientists, and drug development...
Essential Fatty Acid Deficiency Prevention: Advanced Strategies for Researchers and Drug Development
Abstract
This article provides a comprehensive analysis of contemporary strategies for preventing Essential Fatty Acid Deficiency (EFAD), with a focus on challenges and innovations relevant to researchers, scientists, and drug development professionals. It explores the biochemical foundations and at-risk populations, details current and emerging methodological approaches for EFAD prevention, addresses diagnostic complexities and optimization hurdles with newer lipid injectable emulsions, and evaluates comparative evidence on novel formulations. The synthesis aims to inform clinical protocol refinement and guide the development of next-generation nutritional therapeutics.
The Biochemical Basis and Evolving Epidemiology of Essential Fatty Acid Deficiency
FAQs: Core Concepts for Researchers
Q1: What fundamentally defines LA and ALA as "essential" from a biochemical perspective? Humans lack the Δ-12 and Δ-15 desaturase enzymes required to insert double bonds at the n-6 or n-3 positions of a fatty acid carbon chain [1]. Because these specific unsaturated fatty acids cannot be synthesized de novo, LA (18:2n-6) and ALA (18:3n-3) must be obtained from the diet, fulfilling the criteria for essential nutrients [2] [1].
Q2: What is the clinical significance of the competition between LA and ALA metabolic pathways? LA and ALA compete for the same set of elongase and desaturase enzymes, notably Δ-6 and Δ-5 desaturase (FADS2 and FADS1), in the biosynthesis of longer-chain, more unsaturated fatty acids [2] [1]. This competition means that the dietary ratio of n-6 to n-3 PUFAs can influence the downstream production of bioactive lipids. High LA intake can potentially limit the conversion of ALA to eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) [1].
Q3: In a research setting, how is Essential Fatty Acid Deficiency (EFAD) definitively diagnosed? While clinical signs like scaly dermatitis and growth retardation are indicators, biochemical assessment is key [3]. The Holman index, or triene-to-tetraene (T:T) ratio, compares the levels of Mead acid (20:3n-9) to arachidonic acid (20:4n-6) [2]. A ratio exceeding 0.2 is commonly used to diagnose EFAD [2]. However, with modern lipid emulsions altering fatty acid profiles, reliance on this ratio alone is increasingly complex, and full fatty acid panels are recommended [2].
Q4: What are the critical considerations for designing parenteral nutrition regimens to prevent EFAD? Preventing EFAD in patients on parenteral nutrition requires providing adequate amounts of LA and ALA via lipid injectable emulsions (ILEs) [2]. The minimum requirement to prevent EFAD in adults is estimated at 3.2% of total energy from intravenous fat, equating to approximately 7.7 g/day of linoleic acid [2]. The shift from pure soybean oil-based ILEs to composite emulsions with lower essential fatty acid content necessitates careful attention to dosing to avoid deficiency [2].
Troubleshooting Common Experimental Challenges
Challenge 1: Inconsistent or Low Conversion Rates of ALA to DHA in Cell or Animal Models
- Potential Cause: The conversion of ALA to DHA is inherently low, especially in males, with tracer studies showing only 0%-4% conversion in men [4] [1].
- Solution:
- Account for Biological Sex: Utilize female models where conversion to DHA is significantly higher (up to 9% in women) due to the regulatory effect of estrogen [4] [1].
- Consider Genetic Background: Incorporate genotyping for common haplotypes in the FADS gene cluster (e.g., haplotype D is associated with higher FADS activity and greater conversion) [1].
- Bypass the Rate-Limiting Step: Supplement directly with stearidonic acid (SDA, 18:4n-3) or EPA to bypass the Δ-6 desaturase step, which is a major bottleneck in the pathway [2].
Challenge 2: Interpreting Inflammatory Biomarkers in the Context of High LA Diets
- Potential Cause: The hypothesis that high LA intake is uniformly pro-inflammatory due to its conversion to arachidonic acid (AA) is overly simplistic. Kinetic studies show fractional conversion of LA to AA is very low (0.3%-0.6%) and modifying LA intake has little effect on tissue AA levels in individuals consuming a typical Western diet [5].
- Solution:
- Measure Directly: Do not infer inflammatory status solely from LA intake. Directly measure specific oxylipins or eicosanoids (e.g., prostaglandins, leukotrienes) via LC-MS/MS.
- Assess the Balance: Evaluate the overall n-6 to n-3 PUFA ratio in plasma phospholipids or red blood cell membranes, as this balance is more indicative of the inflammatory milieu than LA alone [6].
- Reference Systematic Reviews: A review of 15 randomized controlled trials concluded that increasing dietary LA does not promote inflammation in healthy humans [5].
Challenge 3: Modeling Severe EFAD in Preclinical Studies
- Potential Cause: Standard laboratory chow is typically sufficient in EFAs, making it difficult to induce a deficient state.
- Solution:
- Use Specialized Diets: Employ precisely defined, fat-free or EFA-deficient diets. These diets must be administered over a sufficient period to deplete endogenous stores.
- Monitor Biochemical Markers: Confirm EFAD by regularly measuring the plasma T:T ratio, expecting a value >0.2, and observing a decline in LA and ALA levels [2].
- Validate with Positive Control: Include a group that receives a controlled EFA repletion (e.g., via topical application or dietary supplementation) to confirm reversal of deficiency symptoms [5] [3].
Table 1: Dietary Reference Intakes for Essential Fatty Acids
Adequate Intakes (AIs) for Linoleic Acid (LA) and Alpha-Linolenic Acid (ALA) as established by the National Academy of Medicine [5] [7] [1].
| Life Stage Group | LA (g/day) | ALA (g/day) |
|---|---|---|
| Infants (0-6 months) | 4.4 | 0.5 |
| Infants (7-12 months) | 4.6 | 0.5 |
| Children (1-3 years) | 7.0 | 0.7 |
| Males (19-50 years) | 17.0 | 1.6 |
| Females (19-50 years) | 12.0 | 1.1 |
| Pregnancy | 13.0 | 1.4 |
| Lactation | 13.0 | 1.3 |
Table 2: Key Biomarkers for Assessing Essential Fatty Acid Status
Commonly measured analytes for diagnosing deficiency and monitoring status in research and clinical settings [2] [3].
| Biomarker | Lipid Number | Significance & Interpretation |
|---|---|---|
| Linoleic Acid (LA) | 18:2n-6 | Primary EFA. Low levels indicate inadequate intake or absorption [2]. |
| Alpha-Linolenic Acid (ALA) | 18:3n-3 | Primary EFA. Low levels indicate inadequate intake or absorption [2]. |
| Arachidonic Acid (AA) | 20:4n-6 | Long-chain n-6 metabolite. Key structural component and eicosanoid precursor [5]. |
| Eicosapentaenoic Acid (EPA) | 20:5n-3 | Long-chain n-3 metabolite. Gives rise to anti-inflammatory eicosanoids [1]. |
| Docosahexaenoic Acid (DHA) | 22:6n-3 | Long-chain n-3 metabolite. Critical for brain and retinal function [1]. |
| Mead Acid | 20:3n-9 | Non-essential marker. Synthesized when EFA levels are low. Used in the Holman Index [2]. |
| Holman Index (T:T Ratio) | 20:3n-9 / 20:4n-6 | EFAD Diagnostic. A ratio > 0.2 is indicative of essential fatty acid deficiency [2]. |
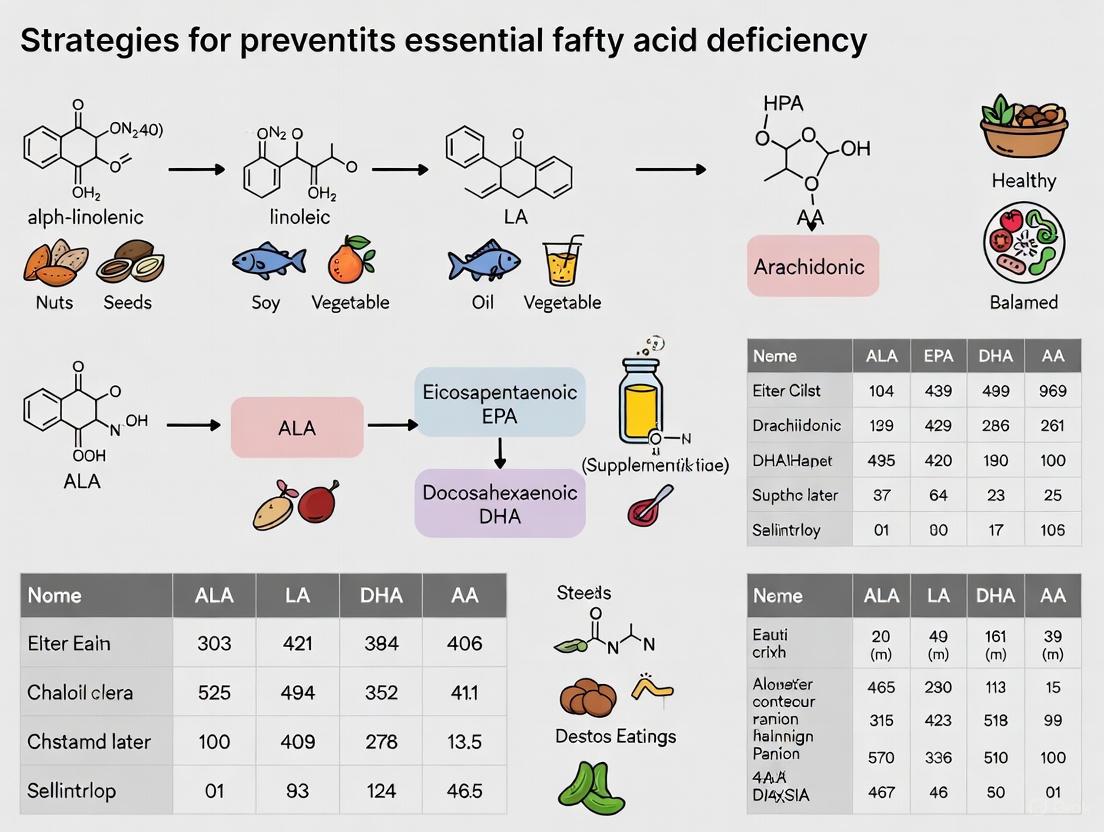
Essential Metabolic Pathways
Diagram 1: Metabolic Pathways of LA and ALA
Diagram 2: Experimental Workflow for EFAD Research
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for EFA Research
Key materials and their applications for studying essential fatty acid biochemistry and deficiency.
| Category | Item / Reagent | Function & Application in Research |
|---|---|---|
| Fatty Acid Standards | Pure LA and ALA isomers; Deuterated (d8-AA) or carbon-13 (¹³C-ALA) labeled internal standards. | Used for calibrating analytical equipment (GC-MS, LC-MS) and performing quantitative analysis and stable isotope tracer studies to track metabolic conversion [4]. |
| Defined Diets | Fat-free base diet; Custom EFA-deficient diet; Diets with controlled n-6/n-3 ratios. | For inducing EFAD in animal models or for controlled nutritional intervention studies to investigate the effects of specific fatty acids [2]. |
| Lipid Injectable Emulsions (ILEs) | Soybean oil-based ILE; Composite oil ILE (e.g., SMOFlipid); Fish oil-based ILE. | Critical for in vitro studies and for designing parenteral nutrition protocols in animal or clinical studies to prevent or treat EFAD [2]. |
| Analytical Kits & Assays | Fatty acid methyl ester (FAME) derivation kit; Eicosanoid/oxylipin profiling panel (ELISA or MS-based). | For preparing samples for gas chromatography (GC) and for quantifying downstream bioactive lipid mediators derived from EFAs [5] [6]. |
| Enzyme Inhibitors/Activators | Selective Δ-5 or Δ-6 desaturase inhibitors; PPARα/γ agonists. | To pharmacologically manipulate the metabolic pathways of LA and ALA in cell culture models to study enzyme function and regulation [8]. |
Frequently Asked Questions (FAQs) & Troubleshooting
FAQ 1: Why are linoleic acid (LA) and α-linolenic acid (ALA) classified as essential, and what are the practical implications for designing animal model studies?
- Answer: Humans and animals lack the enzymes (specifically, Δ12 and Δ15 desaturases) to introduce double bonds at the n-6 and n-3 positions of fatty acids [9]. Therefore, LA (18:2n-6) and ALA (18:3n-3) must be obtained from the diet. In research, this means control diets for animal studies must be carefully formulated to include these fatty acids. Using purified ingredients without verifying EFA content can inadvertently induce Essential Fatty Acid Deficiency (EFAD), confounding your results. The biochemical hallmark of EFAD is an elevated triene:tetraene (T:T) ratio (Mead acid: Arachidonic acid) above 0.4 [10].
FAQ 2: Our cell culture model shows unexpected inflammatory responses. Could the fatty acid composition of the serum supplement or growth media be a contributing factor?
- Answer: Absolutely. Traditional fetal bovine serum (FBS) has variable fatty acid profiles. High levels of ARA (20:4n-6) in media can predispose cells to a pro-inflammatory state due to its role as an eicosanoid precursor. To standardize experiments, consider using serum-free media or media supplemented with defined fatty acid-albumin complexes. This allows precise control over the n-6 to n-3 ratio, which can modulate inflammatory signaling pathways.
FAQ 3: When analyzing plasma fatty acid profiles to assess EFAD, is the triene:tetraene (T:T) ratio sufficient, or should we consider other parameters?
- Answer: Recent evidence suggests that the T:T ratio, while classic, should not be the sole criterion. A comprehensive assessment should include the complete fatty acid profile. Key indicators include low absolute levels of LA and ARA, along with elevated Mead acid (20:3n-9) [10]. Furthermore, genetic polymorphisms in fatty acid desaturase (FADS) genes can significantly influence an individual's capacity to generate ARA and EPA, meaning two subjects with the same dietary intake could have very different plasma profiles [10] [11].
FAQ 4: What are the key regulatory enzymes in the synthesis of long-chain PUFAs, and how can we modulate their activity in experimental models?
- Answer: The primary regulatory steps are the elongation and desaturation reactions. The key enzymes are the elongases (ELOVL) and desaturases (FADS). The Δ6-desaturase (FADS2) is the rate-limiting enzyme in the conversion of LA to ARA and ALA to EPA. Activity can be modulated pharmacologically, through genetic knockdown/overexpression, or by dietary means. For example, high dietary cholesterol and trans-fats can inhibit desaturase activity, while insulin and certain micronutrients can enhance it.
Experimental Protocols & Data Presentation
Protocol 1: Gas Chromatography (GC) Analysis of Serum Non-Esterified Fatty Acids (NEFAs)
This protocol is adapted from methods used in recent clinical research on EFAD [11].
- Sample Preparation: Add 75 µL of human serum to a glass tube containing 10 µg of an internal standard (e.g., tridecanoic acid, C13:0).
- Derivatization (Methylation): Add 5 mL of methanol-acetyl chloride (50:1 v/v) mixture. Incubate the sample for 45 minutes at 24–29°C in a heating block to convert fatty acids to fatty acid methyl esters (FAMEs).
- Reaction Quenching: Stop the methylation reaction by adding 3 mL of 6% sodium carbonate solution.
- Extraction: Extract the FAMEs by adding 150 µL of hexane and transfer the hexane layer to an injection vial.
- GC-FID Analysis:
- Instrument: Agilent 7890 GC system with Flame Ionization Detector (FID).
- Column: HP-88 capillary column (100 m × 0.25 mm, 0.2 μm film thickness).
- Carrier Gas: Helium at 2 mL/min.
- Temperature Program:
- Initial: 100°C held for 3 min.
- Ramp 1: 8°C/min to 175°C.
- Ramp 2: 3°C/min to 240°C, held for 10 min.
- Injection: 1 µL in split mode (5:1 ratio).
- Quantification: Quantify individual NEFAs by interpolating against calibration curves using the internal standard for normalization. Concentrations are expressed as µg/mL of serum [11].
Quantitative Data Tables
Table 1: Fatty Acid Composition of Select Intravenous Lipid Emulsions (ILEs)
| Fatty Acid(s) | 100% Soybean Oil (%) | 80% Olive Oil / 20% Soybean Oil (%) |
|---|---|---|
| Total Saturated | 15.6 | 16.6 |
| Palmitic acid (16:0) | 11.0 | 13.0 |
| Total Monounsaturated | 22.8 | 63.4 |
| Oleic acid (18:1n-9) | 20.9 | 59.7 |
| Total Polyunsaturated | 61.7 | 20.0 |
| Linoleic acid (18:2n-6) | 54.7 | 18.6 |
| α-Linolenic acid (18:3n-3) | 6.7 | 1.7 |
| Arachidonic acid (20:4n-6) | 0.2 | 0.2 |
| Docosahexaenoic acid (22:6n-3) | 0.1 | 0.1 |
Source: Adapted from Giuffrida et al. as cited in [10].
Table 2: Key Enzymes in the LC-PUFA Synthesis Pathway
| Enzyme | Systematic Name | Function in Pathway | Organelle Location |
|---|---|---|---|
| Δ6-desaturase | FADS2 | Rate-limiting step; desaturates LA to GLA (n-6) and ALA to SDA (n-3). | Endoplasmic Reticulum |
| Δ5-desaturase | FADS1 | Desaturates DGLA to ARA (n-6) and ETA to EPA (n-3). | Endoplasmic Reticulum |
| ELOVL2 | Elongase 2 | Critical for VLC-PUFA synthesis; elongates EPA to DPA (n-3) and ARA to Adrenic acid (n-6). | Endoplasmic Reticulum |
| ELOVL5 | Elongase 5 | Elongates GLA to DGLA (n-6) and SDA to ETA (n-3). | Endoplasmic Reticulum |
Pathway Visualization
LC-PUFA Synthesis Pathways
Experimental Workflow for EFAD Risk Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Fatty Acid Metabolism Research
| Item | Function / Application | Example Use Case |
|---|---|---|
| Fatty Acid Methyl Esters (FAME) | Calibration standards for Gas Chromatography (GC) analysis. | Quantifying specific fatty acids in biological samples (plasma, tissues, cells). |
| Tridecanoic Acid (C13:0) | Internal Standard for GC analysis. Added in a known quantity to correct for sample loss during preparation. | Protocol for serum NEFA analysis by GC-FID [11]. |
| HP-88 GC Column | A highly polar capillary column designed for the separation of fatty acid isomers, including cis/trans and positional isomers. | Resolving the complex mixture of fatty acids in biological samples [11]. |
| Fatty Acid-Albumin Complexes | Defined, serum-free delivery system for fatty acids in cell culture experiments. | Studying the specific effects of ARA, EPA, or DHA on inflammation without serum variability. |
| Specific ELISA Kits | Measurement of eicosanoids (e.g., prostaglandins, leukotrienes) derived from ARA and EPA. | Correlating changes in PUFA levels with functional inflammatory outputs. |
| FADS siRNA/shRNA | Genetic tools to knock down the expression of desaturase enzymes in cell models. | Investigating the functional role of specific desaturases in LC-PUFA synthesis. |
| Intravenous Lipid Emulsions | Clinically relevant lipid sources for in vivo studies or ex vivo models. | Comparing the biological effects of SO-based vs. OO/SO-based ILEs on EFAD markers [10]. |
Frequently Asked Questions (FAQs)
Q1: What historical progression in infant feeding led to modern parenteral nutrition support? The history of pediatric nutrition evolved from breastfeeding and wet nursing to modern enteral formulas and intravenous nutrition. Before the 20th century, the absence of reliable breast milk alternatives led to high infant mortality [12]. The first patented infant formula, developed by Justus von Liebig in 1864, used modified cow's milk as a base [12]. Research into intravenous lipid emulsions (ILEs) and their composition to prevent deficiencies like Essential Fatty Acid Deficiency (EFAD) represents a modern extension of this historical need to provide complete nutrition to vulnerable populations [13].
Q2: Which patient populations are at the highest risk for Essential Fatty Acid Deficiency (EFAD) in modern practice? Patients dependent on long-term parenteral nutrition are at the highest risk, particularly preterm infants [13]. This population has rapid growth demands and limited nutrient stores, making them vulnerable to fatty acid deficiencies if lipid emulsions are not carefully managed [13].
Q3: What are the key biochemical markers for diagnosing EFAD, and what are their target thresholds? The primary marker is the triene-to-tetraene (T:T) ratio, which measures the ratio of Mead acid (20:3n-9) to arachidonic acid (20:4n-6). A T:T ratio exceeding 0.2 is a classic indicator of EFAD [13]. Current research recommends also analyzing the complete plasma fatty acid profile, as the T:T ratio alone may not provide a full picture [13].
Q4: How does the composition of intravenous lipid emulsions (ILEs) influence the risk of EFAD? The fatty acid profile of the ILE directly impacts EFAD risk. A 2025 randomized controlled trial demonstrated that an 80% olive oil/20% soybean oil (OO/SO) ILE was effective and did not increase the risk of EFAD in pediatric patients compared to a 100% soybean oil (SO) ILE [13]. The OO/SO group showed a smaller increase in linoleic acid but stable arachidonic acid levels [13].
Q5: What role do genetic factors play in fatty acid metabolism for patients on parenteral nutrition? Genetic polymorphisms (common variations) in fatty acid desaturase (FADS) genes can significantly impact an individual's metabolism of essential fatty acids. These polymorphisms were frequently observed in patients with extreme arachidonic acid values, suggesting that genetic makeup should be considered in EFAD risk assessment and future research [13].
Experimental Data & Protocols
Table 1: Fatty Acid Profile Changes in a Pediatric RCT on Lipid Emulsions (2025)
This table summarizes key findings from a randomized controlled trial comparing two intravenous lipid emulsions in pediatric patients [13].
| Fatty Acid Metric | 80% Olive Oil / 20% Soybean Oil ILE | 100% Soybean Oil ILE | Clinical Significance |
|---|---|---|---|
| Linoleic Acid (18:2n-6) | Increased to a lesser extent | Increased | Confirms delivery of this essential fatty acid in both groups. |
| Arachidonic Acid (20:4n-6) | Remained stable | Remained stable | Suggests maintained metabolic conversion in both regimens. |
| Mead Acid (20:3n-9) | Demonstrated an increase | Demonstrated a decrease | Opposite trends highlight different metabolic pressures. |
| Triene:Tetraene (T:T) Ratio | Similar changes in both groups | Similar changes in both groups | No EFAD was observed in either group during the trial period. |
| Incidence of EFAD | None | None | OO/SO ILE is a safe alternative that does not increase short-term EFAD risk. |
Table 2: Essential Research Reagent Solutions for EFAD Prevention Studies
| Reagent / Material | Function in Research |
|---|---|
| Soybean Oil (SO) Intravenous Lipid Emulsion | Serves as a control or comparator in studies; a rich source of linoleic acid (omega-6) [13]. |
| Olive Oil/Soybean Oil (OO/SO) Blend ILE | An investigational emulsion used to study the effects of a reduced soybean oil and increased monounsaturated fat load [13]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | The analytical platform used for precise measurement and profiling of plasma fatty acid concentrations [13]. |
| Plasma/Serum Samples from Subjects | The biological matrix for quantifying fatty acid levels and calculating critical ratios like the T:T ratio [13]. |
| Genotyping Assays for FADS genes | Research tools to identify genetic polymorphisms in fatty acid desaturase genes that may influence metabolic outcomes [13]. |
Detailed Methodology: Plasma Fatty Acid Profiling and EFAD Assessment This protocol is central to monitoring EFAD in clinical trials [13].
- Sample Collection: Collect patient plasma or serum samples at baseline and at regular intervals during the study period.
- Lipid Extraction: Isolate total lipids from the plasma samples using a standardized method, such as liquid-liquid extraction with a chloroform-methanol mixture.
- Fatty Acid Derivatization: Convert the fatty acids in the lipid extract into fatty acid methyl esters (FAMEs) via transesterification, typically using boron trifluoride in methanol.
- Analysis by GC-MS:
- Inject the FAMEs into the Gas Chromatograph, which separates the individual fatty acid esters based on their chemical properties.
- The Mass Spectrometer then identifies and quantifies each specific fatty acid by its unique fragmentation pattern.
- Data Calculation & Interpretation:
- Quantify the concentrations of key fatty acids: Linoleic Acid (18:2n-6), Arachidonic Acid (20:4n-6), and Mead Acid (20:3n-9).
- Calculate the Triene-to-Tetraene (T:T) ratio: (20:3n-9 / 20:4n-6).
- Interpret results: A T:T ratio > 0.2 is indicative of EFAD. The complete profile provides a more comprehensive view of fatty acid status.
Research Visualization with Graphviz
Diagram 1: EFAD Research Workflow
Diagram 2: Fatty Acid Metabolism Pathway
Diagnostic Protocols and Biochemical Markers
How is Essential Fatty Acid Deficiency (EFAD) diagnosed in a research setting?
The diagnosis of EFAD in research relies on a combination of biochemical markers, with the Holman Index (triene:tetraene ratio) being a historical cornerstone. However, contemporary research practices emphasize a more comprehensive approach.
- Primary Diagnostic Marker: The Holman Index, or triene:tetraene ratio (T:T ratio), measures the ratio of Mead acid (a triene) to arachidonic acid (a tetraene). A ratio exceeding 0.05 in infants or 0.2 in adults is indicative of EFAD [2] [14]. This ratio increases when linoleic acid is deficient, as the body converts oleic acid to Mead acid instead of arachidonic acid [14].
- Comprehensive Fatty Acid Profiling: Relying solely on the T:T ratio is now considered insufficient. Current research diagnostics include full plasma fatty acid profiles to measure absolute levels of linoleic acid (LA), alpha-linolenic acid (ALA), arachidonic acid (ARA), and docosahexaenoic acid (DHA) [2] [13]. This is particularly crucial when studying patients on newer lipid emulsions, as their fatty acid composition can directly influence the T:T ratio [2].
- Genetic Analysis: Emerging research indicates that genetic polymorphisms in fatty acid desaturase (FADS) genes can significantly impact fatty acid levels, particularly arachidonic acid. Genotyping is recommended in research protocols for patients presenting with extreme fatty acid values to account for this variability [13].
Table 1: Key Analytical Markers for EFAD Research
| Analyte | Role in Diagnosis | Reference Range (Example) | Significance in EFAD |
|---|---|---|---|
| Holman Index (T:T Ratio) | Primary diagnostic index | <0.05 (Infants) [14] | Increases with deficiency [2] |
| Linoleic Acid (LA) | Essential ω-6 fatty acid | 1000-3300 nmol/mL [14] | Markedly decreased [14] |
| Alpha-Linolenic Acid (ALA) | Essential ω-3 fatty acid | 10-190 nmol/mL [14] | Markedly decreased [2] |
| Arachidonic Acid (ARA) | Downstream ω-6 metabolite | 110-1110 nmol/mL [14] | Decreased [2] |
| Mead Acid | ω-9 metabolite from oleic acid | 3-24 nmol/mL [14] | Significantly elevated [14] |
What are the clinical signs of EFAD that researchers should note in patient studies?
While biochemical markers are primary for research diagnosis, clinical signs provide crucial correlative data. The manifestation of symptoms often depends on the severity and duration of the deficiency.
- Dermatological Signs: The most common clinical sign is a generalized scaly dermatitis [3]. In infants, this can be severe and resemble congenital ichthyosis, and it is often accompanied by increased transepidermal water loss [3].
- Hematological and Hepatic Signs: EFAD can cause thrombocytopenia (low platelet count) and elevated liver transaminases, indicating hepatic involvement [14].
- Other Systemic Effects: Patients may experience growth failure, poor wound healing, and alopecia. In severe and chronic cases, intellectual disability can occur, especially in children [3].
Prevention Strategies & Lipid Emulsion Research
What are the minimum effective doses of different lipid emulsions to prevent EFAD in high-risk populations?
Preventing EFAD requires providing sufficient essential fatty acids intravenously. The minimum effective dose varies significantly based on the composition of the lipid injectable emulsion (ILE) used and the patient's underlying condition.
- Soybean Oil-based ILE (SO-ILE): For premature infants, a dose of 0.5 - 1 g/kg/day is typically sufficient to prevent EFAD [14].
- Fish Oil-based ILE (100%): To prevent EFAD, a dose of approximately 1 g/kg/day is required. It is important to note that while this ILE is effective at treating EFAD and reversing IFALD, it results in a distinct fatty acid profile with low linoleic and arachidonic acid levels [14].
- Mixed-Oil ILE (e.g., SMOFlipid): Preventing EFAD with a mixed-oil ILE containing 15% fish oil requires a significantly higher dose, estimated at 2.2 - 3 g/kg/day, which is dependent on gestational age and enteral intake [14].
- Olive/Soybean Oil-based ILE (OO/SO): Recent pediatric randomized controlled trials have shown that an 80% olive oil/20% soybean oil ILE is safe and does not increase the risk of EFAD when administered for an average of 10-11 days [13].
Table 2: Lipid Emulsion Dosing for EFAD Prevention in High-Risk Populations
| Lipid Emulsion Type | Key Fatty Acid Features | Minimum Preventive Dose (approx.) | Considerations for Researchers |
|---|---|---|---|
| 100% Soybean Oil | High in Linoleic Acid (LA) | 0.5 - 1 g/kg/day [14] | Pro-inflammatory; high phytosterols can contribute to liver disease [14] |
| 100% Fish Oil | High in EPA & DHA | 1 g/kg/day [14] | Effective for IFALD; results in low LA & ARA levels [14] |
| Mixed-Oil (SMOFlipid) | Balanced ω-6:ω-3 ratio | 2.2 - 3 g/kg/day [14] | Requires higher dosing for EFAD prevention; used off-label in infants [14] |
| Olive/Soybean Oil (OO/SO) | Lower in LA than pure SO | Effective in studied regimens [13] | Newer formulation; fatty acid profiles reflect ILE composition [2] [13] |
How do you balance the risk of EFAD with other complications like hypertriglyceridemia (HTG) in premature infants?
Managing lipid intake in premature infants is a central challenge in EFAD prevention research, as it involves weighing competing risks.
- Understanding HTG: Preterm infants have decreased triglyceride clearance, making them prone to HTG, especially during sepsis or stress. While severe complications from HTG are rare at levels below 500 mg/dL, a threshold of <250 mg/dL is generally well-tolerated [14].
- The EFAD Paradox: Restricting lipids to prevent HTG can inadvertently cause EFAD. Ironically, EFAD itself can exacerbate HTG by promoting de novo lipogenesis and fat mobilization from adipose stores [14].
- Research and Clinical Strategy: The goal is to provide the minimum effective dose of ILE to prevent EFAD while monitoring triglyceride levels. The choice of ILE is critical; for instance, fish oil-based ILE can enhance triglyceride clearance and is a therapeutic option for managing both HTG and EFAD [14].
Experimental Models & Research Gaps
What are the key reagents and materials for designing experiments on EFAD prevention?
Table 3: Research Reagent Solutions for EFAD Studies
| Reagent / Material | Function in Research | Example / Note |
|---|---|---|
| Lipid Injectable Emulsions (ILEs) | Investigative variable for prevention/treatment | Soybean, Fish Oil, Mixed-Oil, Olive/Soybean [2] [13] [14] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Gold standard for fatty acid profile analysis | Measures LA, ALA, ARA, Mead acid, etc. [2] |
| Genetic Sequencing Kits | Analysis of FADS gene polymorphisms | Explores genetic influence on fatty acid metabolism [13] |
| Commercial Fatty Acid Panels | Standardized plasma fatty acid analysis | Provides reference values for healthy and diseased states [2] |
What are the current knowledge gaps and future directions in EFAD prevention research?
Despite advances, several key questions remain unanswered, providing avenues for future research.
- Optimal Lipid Dose and Composition: Further research is needed to determine the precise ILE dose and oil composition that best supports growth, organogenesis, and neurodevelopment without promoting complications like IFALD or HTG [14].
- Long-Term Implications of Altered Profiles: The long-term consequences of the distinct fatty acid profiles produced by newer ILEs (e.g., low ARA with fish oil) on growth and neurodevelopment are not fully understood [14].
- Genetic Influences: The role of genetic polymorphisms in fatty acid desaturase enzymes and their impact on EFA requirements and metabolism in high-risk populations is a growing area of research [13].
- Refining Diagnostic Criteria: The shift from relying solely on the T:T ratio to using comprehensive fatty acid profiles needs further validation and standardization across different patient populations and ILE regimens [2].
Visualizing Essential Fatty Acid Metabolism and Deficiency
The following diagram illustrates the biochemical pathways of essential fatty acid metabolism and the metabolic shifts that occur during deficiency, which is fundamental to understanding its diagnosis and pathophysiology.
## Experimental Troubleshooting Guide
This guide addresses common experimental and clinical challenges in research on ARA and DHA deficiency, providing targeted solutions for scientists and drug development professionals.
FAQ 1: How can I definitively diagnose Essential Fatty Acid Deficiency (EFAD) in a preclinical pediatric model, as traditional biomarkers may be insufficient?
- Challenge: Relying solely on the Holman Index (Triene:Tetraene, T:T ratio) can be misleading. Experimental models may show biochemical EFAD without a conclusive T:T ratio.
- Solution: Implement a multi-parameter diagnostic workflow.
- Primary Analysis: Determine the plasma T:T ratio (Mead Acid: Arachidonic Acid). A value >0.4 is indicative of EFAD, while 0.2-0.4 is indeterminate [10].
- Confirmatory Profiling: Analyze the complete plasma fatty acid profile. Look for concomitant low linoleic acid (LA), low arachidonic acid (ARA), and high mead acid levels to confirm EFAD, even if the T:T ratio is borderline [10].
- Genetic Analysis: Incorporate genotyping for polymorphisms in the fatty acid desaturase (FADS) genes. Certain variants can significantly alter ARA levels and confound results, which is critical for patient stratification in clinical trials [10].
- Supporting Data: A 2025 randomized controlled trial (NCT04555044) in pediatric patients (n=101, 94 preterm infants) using an 80% olive oil/20% soybean oil ILE demonstrated that despite a lower LA intake and an increase in mead acid, no EFAD was observed. This underscores the necessity of a complete fatty acid profile over a single metric [10].
FAQ 2: Our intervention of enteral DHA/ARA supplementation in a very preterm infant model did not show neurodevelopmental improvement. What could explain this null finding?
- Challenge: Despite strong biological plausibility, nutritional interventions may not yield expected outcomes due to confounding factors.
- Solution: Re-evaluate your experimental design and statistical model for key covariates known to impact neurodevelopment.
- Adjust for Covariates: In your analysis, control for sex, in-hospital growth velocity, and socioeconomic factors (e.g., maternal education level). A 2025 follow-up study of the ImNuT trial (n=120 infants born <29 weeks GA) found that while ARA/DHA supplementation itself showed no significant effect, faster linear growth from day 28 to 36 weeks postmenstrual age was associated with higher cognitive scores at 2 years. Female sex and higher maternal education were also positive predictors [15].
- Dosage and Balance: Ensure your supplementation ratio is physiologically appropriate. An imbalance between DHA and ARA may lead to unexpected outcomes.
- Outcome Measures: Consider that neurodevelopmental effects may manifest later in childhood and may not be captured by assessments at 2 years of age.
- Protocol Insight: The ImNuT trial administered an enteral supplement of both ARA and DHA versus a medium-chain triglyceride control from the second day of life until 36 weeks postmenstrual age. Neurodevelopment was assessed at 2 years corrected age using Bayley-III and PDMS-2 [15].
FAQ 3: How do I model the impact of maternal liver disease on offspring outcomes, controlling for the confounding effect of obesity?
- Challenge: Maternal comorbidities like obesity are often entangled with conditions like metabolic dysfunction-associated steatotic liver disease (MASLD), making it difficult to isolate the effect of the liver disease itself.
- Solution: Employ a matched cohort study design.
- Study Group: Use a cohort of pregnant females with biopsy-proven MASLD.
- Control Groups:
- Primary Control: Match with females from the general population for baseline characteristics (e.g., age, parity).
- Secondary Control: Match with females who are overweight or obese but do not have known MASLD. This is critical to disentangle the effects of high BMI from the liver pathology.
- Experimental Findings: A nationwide cohort study using this design found that females with MASLD had a more than threefold increased risk of preterm birth compared to the general population. Crucially, this increased risk persisted even when compared to the overweight/obese control group, suggesting the liver disease itself has independent negative effects [16].
FAQ 4: Supplementing DHA in preterm infant models appears to increase the risk of Bronchopulmonary Dysplasia (BPD). How should this safety signal be investigated?
- Challenge: A recent meta-analysis has identified a potential adverse effect of DHA supplementation, which could halt a clinical development program.
- Solution: Investigate the role of ARA co-supplementation.
- Hypothesis: The increased risk of BPD may be linked to a depletion of ARA pools when high-dose DHA is administered without adequate ARA.
- Experimental Approach: Design an animal or clinical study comparing:
- Group A: DHA supplementation alone.
- Group B: DHA and ARA supplementation in a balanced ratio.
- Group C: Control (no supplementation or placebo).
- Outcome Measures: Primary outcome should be incidence of BPD-like pathology. Key biomarkers should include serial measurements of plasma and tissue levels of ARA, DHA, and inflammatory eicosanoid profiles.
- Evidence Base: A 2025 meta-analysis of 11 RCTs found that enteral DHA supplementation with or without ARA was associated with an 11% increased risk of BPD. The risk was more pronounced (15% increase) in the analysis of five trials that used DHA supplementation without ARA [17].
The following tables consolidate key quantitative findings from recent studies for easy reference.
Table 1: Pregnancy and Preterm Birth Risk Associated with MASLD
| Parameter | Finding | Source / Study Details |
|---|---|---|
| Preterm Birth Risk | >3x increased risk | Nationwide cohort: 240 MASLD vs. 1,140 matched control births [16]. |
| Risk vs. Obese Controls | Risk increase persisted | Comparison to overweight/obese women without MASLD [16]. |
| Caesarean Section Risk | 63% higher vs. general population; association explained by high BMI [16]. | |
| Congenital Malformations | No increased risk observed [16]. |
Table 2: Clinical Outcomes of Enteral ARA/DHA Supplementation in Preterm Infants
| Outcome Measure | Result | Study Details |
|---|---|---|
| Neurodevelopment (BSID-III) | No significant difference at 2 years CA | ImNuT trial: 120 infants <29 wks GA [15]. |
| Bronchopulmonary Dysplasia | 11% increased risk (RR 1.11, CI 1.00-1.22) | Meta-analysis of 9 RCTs (DHA ± ARA) [17]. |
| BPD (DHA without ARA) | 15% increased risk (RR 1.15, CI 1.03-1.28) | Meta-analysis of 5 RCTs [17]. |
| Mortality, NEC, Sepsis | No significant effects observed [17]. |
Table 3: Efficacy of Alternative Intravenous Lipid Emulsions (ILEs)
| ILE Type | Linoleic Acid (LA) Content | EFAD Risk in Pediatrics | Key Findings |
|---|---|---|---|
| 100% Soybean Oil (SO) | ~55% | Control | Traditional standard [10]. |
| 80% Olive Oil / 20% SO | ~18% | No increased risk | Well-tolerated, safe, and did not cause EFAD despite lower LA intake [10]. |
## Key Experimental Protocols
Protocol 1: Assessing Essential Fatty Acid Deficiency in Preclinical and Clinical Studies
This protocol is based on a rigorous methodology used in a recent pediatric RCT [10].
- Patient Population: Include subjects expected to require parenteral nutrition for at least 7 days. Exclusion criteria should include pre-existing liver disease, cholestasis, and severe hypertriglyceridemia.
- Intervention: Randomize subjects to receive different intravenous lipid emulsions (e.g., 100% SO ILE vs. a composite ILE like 80% OO/20% SO).
- Blood Sampling: Collect plasma samples at baseline and at the end of the intervention period.
- Biochemical Analysis:
- Fatty Acid Profile: Analyze plasma phospholipid fatty acids using gas chromatography. Key analytes include:
- Linoleic Acid (LA, 18:2n-6): Low levels indicate poor intake/status.
- Arachidonic Acid (ARA, 20:4n-6): Low levels suggest depletion.
- Mead Acid (20:3n-9): Elevated in EFAD.
- Holman Index Calculation: Calculate the Triene:Tetraene (T:T) ratio as Mead Acid / ARA.
- Fatty Acid Profile: Analyze plasma phospholipid fatty acids using gas chromatography. Key analytes include:
- Genetic Analysis: Extract DNA and genotype for common polymorphisms in the FADS1 and FADS2 gene clusters.
- Diagnosis:
- EFAD: T:T ratio > 0.4, confirmed by low LA and low ARA.
- Indeterminate: T:T ratio 0.2-0.4. Evaluate clinical signs (dermatitis, poor growth) and full fatty acid profile.
Protocol 2: Modeling the Impact of Maternal MASLD on Offspring
This protocol outlines a nested case-control study design derived from a nationwide registry study [16].
- Cohort Identification: Use national health registries to identify all singleton births within a defined period.
- Case Ascertainment (MASLD group): Identify mothers with a biopsy-proven diagnosis of MASLD.
- Control Selection:
- General Population Controls: Randomly select mothers from the registry, matching on factors like maternal age, year of birth, and parity.
- High-BMI Controls: Identify mothers who are overweight or obese (based on recorded BMI) but without a diagnosis of MASLD.
- Data Extraction: Extract data on primary outcomes (e.g., gestational age at delivery, preterm birth <37 weeks) and covariates (e.g., pre-pregnancy BMI, smoking, comorbidities).
- Statistical Analysis: Use Poisson regression to estimate adjusted risk ratios for preterm birth, comparing the MASLD group to each control group while adjusting for potential confounders.
## Visualized Workflows and Pathways
Fatty Acid Metabolism and Assessment
Preterm Infant Supplementation Workflow
## The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Models for EFA Deficiency Research
| Item / Model | Function / Purpose | Key Considerations |
|---|---|---|
| Biopsy-proven MASLD Murine Model | To study the independent effect of maternal liver disease on fetal development and preterm birth risk. | Ensure pairing with diet-induced obesity control groups to isolate the MASLD effect [16]. |
| 80% Olive Oil / 20% Soybean Oil ILE | A tool to study EFAD under conditions of low linoleic acid (LA) intake, mimicking specific clinical scenarios. | Use to validate that EFAD assessment relies on a full fatty acid profile, not just the T:T ratio [10]. |
| Enteral ARA & DHA Supplement | To investigate the effects of postnatal LC-PUFA supplementation on neurodevelopment and other morbidities in preterm models. | The ARA:DHA ratio is critical. Supplementing DHA without ARA may be associated with adverse outcomes like BPD [17]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | The gold-standard method for precise quantification of fatty acid profiles in plasma, tissues, and breast milk. | Essential for measuring LA, ARA, Mead Acid, DHA, and calculating the T:T ratio [10]. |
| FADS Genotyping Panel | To identify genetic polymorphisms in the fatty acid desaturase gene cluster that affect ARA and DHA synthesis. | Crucial for patient stratification and explaining inter-individual variability in fatty acid levels in clinical trials [10]. |
Prevention Protocols and Dosing Strategies in Clinical and Research Settings
Essential Fatty Acid Fundamentals
Biochemical Definitions and Pathways
What are the essential fatty acids and why are they designated as "essential"? Linoleic acid (LA; 18:2n-6) and α-linolenic acid (ALA; 18:3n-3) are considered essential fatty acids because humans lack the delta-12 and delta-15 desaturase enzymes necessary to insert a double bond at the n-6 or n-3 position of a fatty acid. Consequently, they must be obtained from the diet. [1] These fatty acids serve as precursors for the synthesis of long-chain polyunsaturated fatty acids (PUFA) that play critical roles in membrane structure, cellular signaling, and eicosanoid production. [1]
The metabolic pathways for LA and ALA involve a series of desaturation and elongation steps catalyzed by shared enzyme systems, creating competition between the n-6 and n-3 series for conversion to their respective long-chain derivatives. [1] The diagram below illustrates this metabolic pathway and the competitive inhibition between the n-6 and n-3 series.
Figure 1: Essential Fatty Acid Metabolic Pathway
Historical Context and Discovery
When were essential fatty acids first identified and how were their requirements established? The essential nature of fatty acids was first demonstrated by Burr and Burr in 1929-1930, who showed that rats fed fat-free diets developed deficiency symptoms that could be reversed by adding LA. [18] [2] This foundational work established that 0.6% of total dietary calories as LA prevented deficiency symptoms in rats. [18] Subsequent studies in human infants found that skin abnormalities resulting from low-fat diets resolved when LA was provided at ≥1% of total energy intake. [2] The historical understanding of requirements has been reevaluated, with some evidence suggesting original estimates may have been high due to concurrent omega-3 deficiency in control diets. [18]
Evidence-Based Intake Recommendations
General Population Requirements
What are the current dietary recommendations for LA and ALA intake in healthy adults? The Dietary Reference Intakes established by the National Academy of Medicine provide age and sex-specific recommendations for LA and ALA intake, presented in the table below. [19]
Table 1: Dietary Reference Intakes for Linoleic Acid (LA) and α-Linolenic Acid (ALA)
| Population Group | LA Adequate Intake (g/day) | LA AMDR (% energy) | ALA Adequate Intake (g/day) | ALA AMDR (% energy) |
|---|---|---|---|---|
| Men 19-50 years | 17 | 5-10 | 1.6 | 0.6-1.2 |
| Men 51-70+ years | 14 | 5-10 | 1.6 | 0.6-1.2 |
| Women 19-50 years | 12 | 5-10 | 1.1 | 0.6-1.2 |
| Women 51-70+ years | 11 | 5-10 | 1.1 | 0.6-1.2 |
AMDR = Acceptable Macronutrient Distribution Range
Most American adults meet or exceed LA intake recommendations, with NHANES data showing a trend of increasing LA consumption from 1999-2014. [19] However, the optimal n-6:n-3 ratio is approximately 4-5:1, while typical Western diets often exhibit ratios of 10:1 or higher. [20]
Special Population Considerations
How do essential fatty acid requirements differ across specific patient demographics? EFA requirements vary significantly based on age, clinical condition, and nutritional status. The following table summarizes evidence-based recommendations for special populations.
Table 2: Special Population Recommendations for Essential Fatty Acid Intake
| Population | LA Recommendation | ALA Recommendation | Key Evidence |
|---|---|---|---|
| Infants | ≥1% of total energy (minimum); 4% of total energy (optimal) [2] | Conditionally essential with DHA [2] | Prevents EFAD symptoms; improves growth efficiency [2] |
| Pregnancy/Lactation | Increased to support breast milk composition | DHA supplementation recommended [1] | Reduces early premature birth risk; supports neurological development [1] |
| Parenteral Nutrition Patients | 3.2% of total calories or 7.7 g/day linoleic acid [21] | Include with LA in lipid emulsions [2] | Prevents EFAD during continuous TPN [21] |
| Type 2 Diabetes | Maintain within AMDR | Maintain within AMDR | Higher intakes associated with reduced CVD and all-cause mortality [22] |
| Metabolic Syndrome | Balance with n-3 intake | Consider increased intake | May improve waist circumference, triglycerides, blood pressure [20] |
Experimental Protocols for EFAD Assessment
Biochemical Assessment of Fatty Acid Status
What are the standard methodologies for assessing essential fatty acid status in research settings? The gold standard for EFAD assessment is the Holman Index (triene:tetraene ratio), which measures the ratio of Mead acid (20:3n-9) to arachidonic acid (20:4n-6). A ratio exceeding 0.2 indicates EFAD, while a ratio of 0.4 indicates severe deficiency. [2] However, with newer lipid injectable emulsions, the T:T ratio alone may be insufficient for diagnosis, requiring comprehensive fatty acid profiling. [2]
Protocol: Serum Non-Esterified Fatty Acid Profiling by GC-FID
Application: Assessment of EFAD status in clinical research, particularly in studies of malnutrition and metabolic disorders. [11]
Materials Required:
- Internal Standard: Tridecanoic acid (C13:0)
- Derivatization Reagent: Methanol-acetyl chloride (50:1, v/v)
- Extraction Solvent: Hexane
- Equipment: Gas chromatograph with flame ionization detector (GC-FID), HP-88 column (100 m × 0.25 mm)
Procedure:
- Add 75 μL human serum to 10 μg internal standard (C13:0) in 5 mL methanol-acetyl chloride
- Incubate 45 minutes at 24-29°C in heating block
- Stop methylation reaction with 3 mL of 6% sodium carbonate
- Extract FAMEs with 150 μL hexane
- Inject 1 μL sample in split mode (ratio 1:5) into GC-FID
- Use temperature program: 100°C for 3 min, increase to 175°C at 8°C/min, then to 240°C at 3°C/min, hold 10 min
- Quantify using internal standard calibration and individual NEFA calibration curves [11]
Dietary Intake Assessment Methodology
What is the validated approach for assessing habitual fatty acid intake in population studies? The National Health and Nutrition Examination Survey (NHANES) employs 24-hour dietary recall methodology through the What We Eat in America (WWEIA) component to assess nutrient intake, including LA and ALA. [19] This validated approach uses the Automated Multiple-Pass Method to reduce bias in energy intake collection. [19]
Protocol: NHANES 24-Hour Dietary Recall Methodology
Application: Population-level assessment of fatty acid intake patterns and trends
Materials Required:
- Standardized dietary recall instrument
- USDA Food and Nutrient Database
- Multiple-pass data collection system
Procedure:
- Conduct in-person 24-hour dietary recalls by trained interviewers
- Utilize 5-step Automated Multiple-Pass Method:
- Quick list of foods consumed
- Forgotten foods probe
- Time and occasion probe
- Detail cycle for each food
- Final review probe
- Code foods using USDA Food Codes
- Calculate nutrient composition using USDA Survey Nutrient Databases
- Analyze data with appropriate statistical weights for population estimates [19]
Research Reagent Solutions
Table 3: Essential Research Reagents for Fatty Acid Analysis
| Reagent/Resource | Application | Technical Specifications |
|---|---|---|
| Gas Chromatograph with FID | Fatty acid separation and quantification | HP-88 column (100 m × 0.25 mm, 0.2 μm film); helium carrier gas (2 mL/min) [11] |
| Soybean Oil-Based ILE | Parenteral nutrition research | Provides 7.7 g linoleic acid per 1000 mL of 10% emulsion [21] |
| Tridecanoic Acid (C13:0) | Internal standard for GC analysis | Quantification standard for NEFA profiling [11] |
| Fatty Acid Methyl Esters (FAMEs) | Calibration standards | Individual NEFA standards for quantitative analysis [11] |
| NHANES Dietary Data | Population intake assessment | 24-hour recall data with USDA nutrient composition [19] |
Troubleshooting Guide: Common Experimental Challenges
EFAD Diagnosis Complications
Why might traditional EFAD diagnosis be insufficient in patients receiving newer lipid injectable emulsions? Newer composite ILEs with decreased soybean oil content alter circulating fatty acid profiles, making the Holman Index less reliable. [2] The fatty acid composition in these emulsions reflects in patient serum levels, potentially confounding deficiency diagnosis.
Solution: Implement comprehensive fatty acid panels rather than relying solely on the T:T ratio. Use population-specific reference values that account for modern ILE formulations. [2]
Conversion Efficiency Variability
How should researchers account for the variability in ALA to EPA and DHA conversion? Conversion efficiency of ALA to long-chain n-3 PUFAs shows significant interindividual variation: approximately 8% to EPA and 0-4% to DHA in men, versus 21% to EPA and 9% to DHA in women. [1] This variability is influenced by estrogen levels and genetic polymorphisms in FADS enzymes. [1]
Solution: Stratify analyses by gender and genotype for FADS polymorphisms. Consider direct measurement of long-chain PUFA status rather than relying solely on precursor intake.
Oxidative Stability Issues
How can researchers prevent oxidative degradation of PUFAs in experimental systems? ALA is highly susceptible to oxidation due to three double bonds, with oxidation rates higher than other common fatty acids. [20] This can compromise experimental results and lead to formation of potentially harmful oxidation metabolites.
Solution: Implement micro- and nano-encapsulation technologies to improve oxidative stability. [20] Add natural or synthetic antioxidants (e.g., tocopherols) to experimental preparations. Control for light, heat, and air exposure during sample processing and storage.
Frequently Asked Questions
Q1: What is the minimum LA intake required to prevent deficiency in adult humans? A: The minimum LA requirement for adults is approximately 1% of total energy intake, though recommendations are typically set higher at 5-10% of energy to account for individual variability and ensure sufficiency. [18] [19] In parenteral nutrition, 3.2% of total calories as intravenous fat prevents EFAD. [21]
Q2: Are there situations where DHA and ARA should be considered conditionally essential? A: Yes, DHA and ARA are considered conditionally essential in preterm infants and those with severe liver disease, as the enzymes needed for their formation from precursors have decreased activity. [2]
Q3: How does the modern Western diet disrupt optimal n-6:n-3 ratios? A: The standard American diet contains 14-25 times more omega-6 than omega-3 fatty acids, with LA consumption increasing from approximately 2 g/day in 1865 to 29 g/day in 2008 - a 25-fold increase. [18] This dramatically shifts the n-6:n-3 ratio from evolutionary norms of approximately 1-4:1 to ratios of 10:1 or higher. [18] [20]
Q4: What are the clinical signs of essential fatty acid deficiency? A: Classical EFAD manifestations include growth retardation (in infants), skin desquamation and dryness, leathery thickening, exudation, perianal irritation, and tail necrosis (in animal models). [18] [2] Biochemical signs precede clinical symptoms.
Q5: How long does it take to develop EFAD during fat-free parenteral nutrition? A: The development of EFAD depends on baseline fatty acid stores. Infants with low stores may develop deficiency within days to weeks, while well-nourished adults may take longer. The half-life of LA is approximately two years, meaning the impact of reducing excessive LA intake occurs slowly. [18]
Standardized Dosing and Initiation Schedules
Lipid injectable emulsions (ILEs) are a critical source of calories and essential fatty acids (EFAs) in parenteral nutrition (PN). Dosing is weight-based and varies by patient age group. The following table summarizes the standard dosing and initiation schedules for ILEs in pediatric and adult populations [23].
Table 1: Standard ILE Dosing and Initiation Schedules
| Age Group | Recommended Initial Dosage | Recommended Maximum Dosage | Initial Infusion Rate | Maximum Infusion Rate |
|---|---|---|---|---|
| Preterm/Neonates (<2 years) | 0.5 to 1 g/kg/day | 3 g/kg/day | 0.1 to 0.2 mL/kg/hour for first 15-30 min | 0.75 mL/kg/hour |
| Pediatric (2 to <12 years) | 1 to 2 g/kg/day | 3 g/kg/day | 0.2 to 0.4 mL/kg/hour for first 15-30 min | 0.75 mL/kg/hour |
| Pediatric (12 to 17 years) | 1 g/kg/day | 3 g/kg/day | 0.2 to 0.4 mL/kg/hour for first 15-30 min | 0.75 mL/kg/hour |
| Adults | 1 to 1.5 g/kg/day | 2.5 g/kg/day | 0.2 mL/kg/hour for first 15-30 min | 0.5 mL/kg/hour |
Frequently Asked Questions (FAQs) on ILE Dosing and EFAD Prevention
Q1: What is the minimum dose of ILE required to prevent Essential Fatty Acid Deficiency (EFAD)? A minimum intake of 0.25 g/kg/day of linoleic acid is recommended to prevent EFAD in preterm infants, and 0.1 g/kg/day for term infants and children [10]. Since different ILEs have varying linoleic acid content, the total lipid dose should be adjusted to meet these EFA requirements [10].
Q2: How do different lipid emulsions compare in their fatty acid composition? The choice of ILE impacts the supply of EFAs. Soybean oil (SO)-based ILEs are rich in linoleic acid, while olive oil (OO)/SO-based ILEs contain less. The table below provides a comparative overview [10].
Table 2: Fatty Acid Composition of Different Lipid Emulsions
| Fatty Acid | 100% Soybean Oil ILE (%) | 80% Olive Oil / 20% Soybean Oil ILE (%) |
|---|---|---|
| Linoleic Acid (LA, 18:2n-6) | 54.7 | 18.6 |
| α-Linolenic Acid (ALA, 18:3n-3) | 6.7 | 1.7 |
| Total Polyunsaturated Fatty Acids (PUFAs) | 61.7 | 20.0 |
| Oleic Acid (18:1n-9) | 20.9 | 59.7 |
| Total Monounsaturated Fatty Acids (MUFAs) | 22.8 | 63.4 |
Q3: What are the critical steps for safely initiating and advancing an ILE infusion? Safety during ILE infusion is paramount [23]. The process should begin at the recommended initial dosage (e.g., 1 g/kg/day for adults). The infusion should start at a slow initial rate (e.g., 0.2 mL/kg/hr for adults) for the first 15-30 minutes while monitoring for acute reactions. If tolerated, the rate can be gradually increased to the goal rate. The infusion should never exceed the maximum infusion rate (e.g., 0.5 mL/kg/hr for adults) to avoid clinical decompensation, which can include acute respiratory distress and metabolic acidosis [23].
Q4: How is EFAD biochemically defined and monitored in research settings? EFAD is traditionally defined by a plasma triene-to-tetraene (T:T) ratio (Holman Index) above 0.4 [10]. However, recent research suggests that assessment should not rely solely on the T:T ratio. It should include a full analysis of the plasma fatty acid profile, confirming low linoleic acid, low arachidonic acid, and high mead acid in the context of an elevated T:T ratio [10]. Genetic polymorphisms in fatty acid desaturase genes should also be considered as they can influence arachidonic acid levels [10].
Troubleshooting Common ILE Dosing and Administration Issues
Problem: Rapid onset of hypertriglyceridemia after ILE initiation.
- Potential Cause: The infusion rate may exceed the patient's lipid clearance capacity, or the maximum daily dose may be too high.
- Solution: Ensure the infusion rate does not exceed the recommended maximum infusion rate for the age group [23]. Monitor serum triglycerides; if elevated, reduce the lipid dose or slow the infusion rate. For severe hypertriglyceridemia (>1,000 mg/dL), ILE is contraindicated [23].
Problem: Suspected EFAD despite ILE administration.
- Potential Cause: The specific ILE in use may not provide sufficient linoleic acid at the current dose to meet the patient's EFA requirements.
- Solution: Calculate the daily linoleic acid delivery based on the ILE's composition and the prescribed dose. Compare this to the recommended minimums (0.25 g/kg/day for preterm infants; 0.1 g/kg/day for term infants/children) [10]. Consider switching to or supplementing with an ILE that has a higher linoleic acid content (e.g., SO-based ILE) to meet EFA needs [10].
Problem: Medication error involving ILE dose.
- Potential Cause: PN is a high-alert medication, and errors can occur during prescribing, transcription, or preparation. A known case involved a 10-fold sodium overdose due to a transcription error that multiple checks failed to catch [24].
- Solution: Implement a standardized PN-use process with interdisciplinary oversight [24]. Use independent double-checks at each step (prescribing, order review, preparation, and administration). For research protocols, utilize gravimetric and product control during compounding to detect and prevent errors [25].
Experimental Protocol: Assessing EFAD Risk with a Novel ILE
This protocol is modeled on a recent pediatric clinical trial evaluating an 80% olive oil/20% soybean oil ILE versus a 100% soybean oil ILE [10].
- Objective: To evaluate the risk of developing EFAD in a pediatric population receiving a novel ILE compared to a standard ILE.
- Study Design: Randomized, double-blind, controlled, multicenter trial.
- Population: Pediatric inpatients (e.g., preterm infants) expected to require PN for at least 7 days.
- Intervention:
- Group A: Novel ILE (e.g., 80% OO/20% SO).
- Group B: Standard ILE (e.g., 100% SO).
- Dosing: Start at 1 g/kg/day and increase by 1 g/kg/day to a target of 2.5-3 g/kg/day for infants.
- Primary Outcome: Incidence of EFAD, defined as a plasma triene:tetraene (T:T) ratio >0.4, confirmed with low linoleic acid, low arachidonic acid, and high mead acid.
- Key Methodological Assessments:
- Plasma Fatty Acid Profiling: Perform at baseline and at the end of the study period. Analyze for linoleic acid, arachidonic acid, mead acid, and calculate the T:T ratio.
- Genetic Analysis: Conduct genetic polymorphism analysis of fatty acid desaturase (FADS) genes in patients presenting with extreme arachidonic acid values.
- Clinical Monitoring: Monitor for clinical signs of EFAD (dermatitis, diarrhea, poor wound healing) and adverse events.
Experimental Workflow for ILE EFAD Risk Assessment
The Scientist's Toolkit: Key Reagents for ILE and EFAD Research
Table 3: Essential Research Reagents and Materials
| Item | Function in Research |
|---|---|
| Soybean Oil (SO) ILE | Serves as the historical control and reference standard for EFA content in comparative studies [10]. |
| Composite ILEs (e.g., OO/SO) | The investigational emulsions used to test hypotheses about reduced PUFA load, immunomodulation, and EFAD risk [10] [23]. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | The analytical tool for performing detailed plasma fatty acid profiling to quantify specific FAs (LA, ARA, Mead acid) and calculate the T:T ratio [10]. |
| Genotyping Assays (e.g., PCR) | Used to identify genetic polymorphisms in fatty acid desaturase (FADS) genes that can confound the interpretation of arachidonic acid levels and EFAD status [10]. |
| Triglyceride & Liver Enzyme Assays | Standard clinical chemistry tests for monitoring metabolic tolerance and safety of ILE dosing regimens [23]. |
Troubleshooting Guides
Gastrointestinal Intolerance in Enteral Feeding Models
Q: What are the common causes and solutions for gastrointestinal intolerance (e.g., abdominal distension, diarrhea, vomiting) in animal or human subject models during enteral nutrition studies?
A: Gastrointestinal complications can significantly impede nutrient absorption and compromise study data on fatty acid intake. The table below outlines common causes and research-focused solutions. [26]
| Concern | Possible Causes in Research Models | Possible Prevention and Solutions |
|---|---|---|
| Abdominal distension, pain, cramping, nausea, vomiting, diarrhea | - Initial feed intolerance.- Feed administered too rapidly.- Formula contamination or improper handling.- Gut dysmotility influenced by anesthetics or experimental medications.- Formula temperature too cold. | - Check tube placement in the model.- Administer feeds and flushes more slowly; consider smaller, more frequent feeding protocols.- Adhere strictly to formula preparation and storage guidelines; use aseptic techniques.- Warm the formula to room temperature before administration.- Review and document all concomitant medications. |
| Constipation | - Low fluid intake.- Low fiber intake in formula.- Reduced activity level of the model.- Medication side effects. | - Increase fluid volume in the protocol.- Increase fiber content of the formula, if research parameters allow.- Increase activity level, if possible.- Conduct a medication review. |
| Anthropometric Concerns (e.g., unintentional weight loss, excessive weight gain) | - Improper preparation of formula leading to inaccurate calorie/nutrient delivery.- Excessive or inadequate feed volumes.- Change in metabolic demand due to the underlying studied condition. | - Standardize and audit feed preparation, mixing, and recipe across all subjects.- Re-calculate energy and volume requirements based on the model's current status.- Assess formula type and concentration for appropriateness to the research goals. |
Mechanical and Tube-Related Complications
Q: How should researchers address frequent feeding tube blockages during continuous infusion protocols for lipid-rich formulas?
A: Tube blockages can interrupt nutrition delivery, potentially leading to variable fatty acid intake and confounding results. The following troubleshooting guide is recommended. [26]
| Concern | Possible Causes | Possible Prevention and Solutions |
|---|---|---|
| Tube blockages | - Inadequate water flushes.- Inadequate flushing with medication administration.- Inappropriate tube size for viscous formulas. | - Establish a strict flushing protocol: flush tube before, in between, and after giving medications or formula.- Ensure the tube is not clamped or kinked.- For blockages: use a syringe with warm water and gently push and pull on the plunger. Gently massage the tube. If unresolved, replace the tube. |
Frequently Asked Questions (FAQs)
Q: Why is the prevention of Essential Fatty Acid Deficiency (EFAD) a critical endpoint in modern enteral nutrition research?
A EFAD arises from insufficient intake of linoleic acid (LA) and alpha-linolenic acid (ALA). Because of their high metabolic demands, research models can develop EFAD rapidly if lipid intake is omitted or insufficient, making its prevention a key indicator of nutritional protocol efficacy. Biochemical EFAD is traditionally characterized by an elevated triene-to-tetraene (T:T) ratio (Holman Index) >0.4. Beyond this, research now emphasizes analyzing the complete fatty acid profile, including arachidonic acid (ARA) and mead acid, and considering genetic polymorphisms in fatty acid desaturase genes for a comprehensive assessment. [10]
Q: How does the choice of lipid emulsion impact EFAD risk and research outcomes in studies requiring parenteral supplementation?
A While soybean oil (SO)-based Intravenous Lipid Emulsions (ILEs) have been the historical standard, they are high in pro-inflammatory ω-6 fatty acids. Newer composite ILEs are designed to improve safety and efficacy profiles. [27]
- Soybean Oil (SO) ILE: Contains ~55% LA, providing a high dose of EFAs but also a high load of ω-6 PUFAs.
- Olive Oil/Soybean Oil (OO/SO) ILE (80/20): Contains ~18% LA. Recent studies confirm that an OO/SO ILE is well-tolerated, safe, and does not increase the risk of EFAD in pediatric patients compared to 100% SO ILE, despite the lower LA content. This supports its use in protocols where modulating inflammatory response is a factor. [10]
Q: What are the critical methodological considerations for administering lipid emulsions in a research setting?
A Several practical issues must be addressed in the experimental protocol. [27]
- Administration Rate: While a rate below 0.1 g/kg/hr is often recommended, faster administration may be possible depending on the model and research objectives.
- Drug Interactions: Administration of ILEs via a piggyback line to basic infusion formulations is generally acceptable. Direct admixture with other drugs is contraindicated.
- Use in Critically Ill Models: Second- and third-generation fat emulsions are considered safe for critically ill subjects, though pure SO should be used with caution.
- Postoperative Administration: Lipid emulsion administration is feasible immediately after surgery, but due to endogenous energy mobilization, it is preferable to initiate administration from the third to fourth postoperative day.
Experimental Protocols & Data Presentation
Protocol: Assessing EFAD Risk in Preclinical Models
Objective: To evaluate the risk of Essential Fatty Acid Deficiency (EFAD) in subjects receiving different enteral nutrition formulas or supplemental oil strategies.
Methodology (Adapted from a pediatric clinical trial design): [10]
- Subject Allocation: Randomize subjects into experimental groups (e.g., Group A: Standard SO-based formula; Group B: Formula with OO/SO-based lipid blend).
- Intervention: Administer the assigned enteral nutrition regimen, ensuring it provides a minimum LA intake of 0.25 g/kg/day for preterm models or 0.1 g/kg/day for term/older models to prevent EFAD.
- Duration: Continue the nutritional intervention for a predefined period, e.g., 7-14 days.
- Sample Collection: Collect plasma samples at baseline and endpoint for fatty acid profile analysis.
- Primary Outcome Measure - EFAD Incidence: Determine EFAD incidence using a plasma triene:tetraene (T:T) ratio >0.4. Confirm biochemically in the context of low LA, low ARA, and high mead acid.
- Secondary Outcome Measures:
- Clinical EFAD: Monitor for clinical features (dermatitis, diarrhea, poor wound healing, growth failure).
- Full Fatty Acid Profile: Analyze changes in linoleic acid, arachidonic acid, and mead acid.
- Genetic Analysis (Optional): Analyze genetic polymorphisms in fatty acid desaturase genes (
FADScluster) in subjects presenting extreme ARA values.
Quantitative Data: Fatty Acid Composition of Select Lipid Emulsions
The table below summarizes the fatty acid composition of two key intravenous lipid emulsions, relevant for designing parenteral supplementation arms in studies. [10]
Table: Fatty Acid Profile of Select Lipid Emulsions (Percentage of Total Fatty Acids)
| Fatty Acid | 100% Soybean Oil ILE | 80% Olive Oil / 20% Soybean Oil ILE |
|---|---|---|
| Total Saturated Fatty Acids | 15.6% | 16.6% |
| Total Monounsaturated Fatty Acids | 22.8% | 63.4% |
| Oleic acid (18:1n-9) | 20.9% | 59.7% |
| Total Polyunsaturated Fatty Acids (PUFAs) | 61.7% | 20.0% |
| Linoleic acid (18:2n-6) | 54.7% | 18.6% |
| α-Linolenic acid (18:3n-3) | 6.7% | 1.7% |
| Arachidonic acid (20:4n-6) | 0.2% | 0.2% |
| Docosahexaenoic acid (22:6n-3) | 0.1% | 0.1% |
Experimental Workflow for EFAD Prevention Research
The following diagram outlines the logical workflow for a research study investigating enteral nutrition strategies.
Research Workflow for EFAD Prevention
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Enteral Nutrition and EFAD Research
| Item | Function / Application in Research |
|---|---|
| Soybean Oil (SO) Intravenous Lipid Emulsion | First-generation ILE; used as a control arm due to its high linoleic acid content (~55%). Serves as a benchmark for EFA delivery. |
| Olive Oil/Soybean Oil (OO/SO) ILE (80/20) | Second-generation ILE; investigated for its potential to provide sufficient EFA (18% LA) while delivering a higher, potentially immunomodulatory, monounsaturated fatty acid (oleic acid) load. |
| Gas Chromatography-Mass Spectrometry (GC-MS) | The analytical gold standard for detailed plasma fatty acid profile analysis, crucial for measuring LA, ARA, mead acid, and calculating the T:T ratio. |
| PCR Assays for FADS Genotyping | Used to identify genetic polymorphisms in the fatty acid desaturase (FADS1/2) genes, which can significantly influence fatty acid metabolism and requirements in a study population. |
| Standardized Enteral Formulas (Varying Lipid Sources) | Commercially available or custom-formulated enteral diets with defined lipid sources (e.g., soy, olive, MCT, fish oil) to test specific hypotheses about lipid composition and EFAD prevention. |
| Feeding Tubes (e.g., Gastrostomy Tubes) | Medical devices for the reliable and sustained administration of liquid enteral formulas directly to the stomach or intestines in animal or human models, ensuring consistent nutrient delivery. |
What is the biochemical basis for essential fatty acid deficiency (EFAD) monitoring?
Answer: Humans lack the Δ12 and Δ15 desaturase enzymes necessary to synthesize linoleic acid (LA, 18:2n-6) and α-linolenic acid (ALA, 18:3n-3), making these polyunsaturated fatty acids (PUFAs) essential dietary components [1]. EFAD occurs when intake, absorption, or metabolism of these fats is severely compromised [28]. Biochemically, LA and ALA deficiency leads to a reduction in their downstream metabolites, including arachidonic acid (ARA) and docosahexaenoic acid (DHA) [29]. Consequently, the non-essential ω-9 fatty acid, oleic acid, undergoes increased elongation and desaturation to form Mead acid (20:3n-9) [29] [2]. The increase in this triene relative to the tetraene ARA forms the basis of the primary diagnostic biomarker, the Holman Index or triene:tetraene (T:T) ratio [29] [2].
What are the core analytes in an essential fatty acid panel?
Answer: A comprehensive essential fatty acid panel should quantify the concentrations of key fatty acids from the ω-6, ω-3, and ω-9 pathways to assess status and identify deficiency. The critical analytes are summarized in the table below.
Table 1: Core Analytes in an Essential Fatty Acid Panel
| Fatty Acid Type | Key Analytes | Biological Significance |
|---|---|---|
| ω-6 PUFAs | Linoleic Acid (LA), Arachidonic Acid (ARA) | LA is the essential parent; ARA is a crucial downstream metabolite for inflammatory mediators and cell membranes [29] [1]. |
| ω-3 PUFAs | α-Linolenic Acid (ALA), Eicosapentaenoic Acid (EPA), Docosahexaenoic Acid (DHA) | ALA is the essential parent; EPA and DHA are vital for neurological development and anti-inflammatory responses [29] [1]. |
| ω-9 PUFA | Mead Acid | A marker of EFAD; increases when LA and ALA are limited [29] [2]. |
| Saturation Index | Holman Index (T:T Ratio) | The primary diagnostic biomarker, calculated as [Mead Acid]/[ARA] [29] [2]. |
The Holman Index (T:T Ratio): A Critical Diagnostic Tool
What is the Holman Index and how is it interpreted?
Answer: The Holman Index, or triene:tetraene (T:T) ratio, is the gold-standard biochemical measure for diagnosing EFAD. It is calculated as the concentration of the trienoic Mead acid (20:3n-9) divided by the concentration of the tetraenoic arachidonic acid (20:4n-6) [29] [2].
Table 2: Clinical Interpretation of the Holman Index (T:T Ratio)
| T:T Ratio | Interpretation |
|---|---|
| < 0.2 | Normal; indicates sufficient essential fatty acid status [2]. |
| > 0.2 | Biochemical EFAD; indicates a deficiency state, often preceding clinical symptoms [29] [2]. |
| > 0.4 | Clinical EFAD; associated with the manifestation of overt signs and symptoms of deficiency [2]. |
What are the limitations of the Holman Index in modern research?
Answer: While foundational, the Holman Index has several critical limitations that researchers must consider:
- Influence of Modern Lipid Emulsions: The T:T ratio was established using soybean oil-based emulsions rich in LA. Newer composite lipid emulsions (e.g., SMOFlipid, Omegaven) have different fatty acid profiles. Providing pre-formed ARA and DHA can maintain a normal T:T ratio even when dietary LA and ALA are below traditional minimum requirements, potentially making the index an unreliable sole marker of deficiency in these contexts [29] [2].
- Lack of ω-3 Status: The index does not account for the status of ω-3 fatty acids (ALA, EPA, DHA). A patient could have a normal T:T ratio but be deficient in ω-3 PUFAs, which are critical for neurological and visual function [29] [1].
- Assay Variability: Different assays and laboratories may have varying reference ranges. The specific assay used and its associated reference values must be considered when interpreting results [28].
Troubleshooting Guide: Common Experimental Challenges
How should we interpret a normal T:T ratio in a patient receiving a fish oil-based lipid emulsion?
Issue: A patient receiving fish oil monotherapy (e.g., Omegaven) has a normal T:T ratio despite minimal intake of LA and ALA.
Solution: This is an expected finding that challenges the traditional definition of essentiality. Fish oil emulsions provide pre-formed DHA and, to a lesser extent, ARA. Evidence from animal studies shows that providing ARA and DHA directly can prevent EFAD and support normal growth and reproduction over multiple generations, even in the near-absence of LA and ALA [29]. In this scenario, the normal T:T ratio is accurate and indicates sufficiency of the "true" essential fatty acids (ARA and DHA). Researchers should:
- Trust the biochemical data. A normal T:T ratio indicates the patient is not deficient.
- Expand the analysis. Include a full fatty acid panel to confirm adequate levels of ARA and DHA.
- Re-evaluate requirements. Understand that EFA requirements may be met by downstream metabolites, not solely the parent compounds LA and ALA [29].
What if the fatty acid profile data conflicts with the clinical picture?
Issue: A patient has biochemical evidence of EFAD (e.g., elevated T:T ratio) but no classic clinical symptoms (e.g., dermatitis), or vice versa.
Solution:
- Confirm the assay. Ensure the fatty acid profile was performed using a reliable method, such as gas chromatography-mass spectrometry (GC-MS) or gas chromatography-flame ionization detection (GC-FID) [11] [28].
- Consider the timeline. Biochemical changes (elevated T:T ratio) can appear within 7-10 days of fat-free nutrition in a continuous feeding scenario, while clinical signs like scaly dermatitis, growth faltering, and impaired wound healing may take weeks to manifest [29] [30].
- Investigate confounding factors. The patient's underlying condition (e.g., malabsorption, environmental enteric dysfunction) can exacerbate deficiency and alter typical presentations. Research in undernourished children with EED has shown EFAD is associated with growth faltering even without overt skin manifestations [11].
- Use a comprehensive panel. Relying on the T:T ratio alone can be misleading. A full fatty acid profile provides a more complete picture, including ω-3 status [2] [28].
Experimental Protocols & Methodologies
Detailed Methodology: Serum Non-Esterified Fatty Acid (NEFA) Profiling by GC-FID
This protocol is adapted from metabolomics studies investigating EFAD in association with growth faltering [11].
Principle: Non-esterified fatty acids (NEFAs) are extracted from serum and derivatized to fatty acid methyl esters (FAMEs) for separation and quantification by gas chromatography.
Workflow:
Step-by-Step Procedure:
- Sample Preparation: Pipette 75 µL of human serum into a glass tube.
- Internal Standard Addition: Add 10 µg of tridecanoic acid (C13:0) dissolved in 5 mL of methanol-acetyl chloride (50:1, v/v) as an internal standard for quantification.
- Derivatization: Incubate the mixture for 45 minutes in a heating block maintained at 24-29°C to convert NEFAs to FAMEs.
- Reaction Termination: Add 3 mL of 6% (w/v) sodium carbonate solution to stop the methylation reaction.
- FAME Extraction: Add 150 µL of hexane, vortex mix, and collect the hexane layer containing the FAMEs into an injection vial.
- GC-FID Analysis:
- Instrument: Agilent 7890 GC system with FID.
- Column: HP-88 capillary column (100 m × 0.25 mm, 0.2 μm film).
- Injection: 1 µL, split mode (ratio 1:5), inlet temperature 250°C.
- Oven Program:
- Initial: 100°C for 3 min.
- Ramp 1: 8°C/min to 175°C.
- Ramp 2: 3°C/min to 240°C.
- Hold: 240°C for 10 min.
- Carrier Gas: Helium at 2 mL/min.
- Quantification: Quantify individual NEFAs by interpolating against the internal standard (C13:0) calibration curve. Report concentrations as µg/mL of serum [11].
Protocol for Establishing EFAD in a Preclinical Model
This protocol is based on studies that challenged the traditional view of essential fatty acids [29].
Objective: To determine if ARA and DHA alone can prevent EFAD in the absence of LA and ALA.
Experimental Design:
- Animals: Weanling mice.
- Dietary Groups:
- Control Diet: Contains adequate LA and ALA.
- EFA-Deficient Diet: Devoid of LA and ALA.
- Test Diet: Devoid of LA and ALA but supplemented with pre-formed ARA and DHA as the sole PUFAs.
- Duration: Long-term, multi-generational (e.g., 5 generations).
Key Assessments:
- Biochemical: Monitor the Holman Index (T:T ratio) in plasma weekly until stable, then periodically.
- Clinical: Track growth (weight), reproductive success (litter size and viability), and inspect for clinical signs of EFAD (dermatitis, alopecia).
- Tissue Analysis: Upon sacrifice, analyze fatty acid composition in tissues (e.g., liver, brain) to confirm incorporation of ARA and DHA and absence of Mead acid accumulation.
Expected Outcomes: Mice fed the test diet (ARA + DHA only) should not develop an elevated T:T ratio or clinical signs of EFAD and should demonstrate normal growth and reproduction through multiple generations, supporting the hypothesis that these downstream metabolites can fulfill essential fatty acid requirements [29].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagents for EFAD Studies
| Reagent / Material | Function / Application in Research |
|---|---|
| Gas Chromatograph (GC) with Flame Ionization Detector (FID) or Mass Spectrometer (MS) | The core instrument for separating and quantifying individual fatty acids in biological samples (serum, plasma, tissues) [11]. |
| Stable Isotope-Labeled Fatty Acids (e.g., 13C-LA, 13C-ALA) | Tracers used in kinetic studies to elucidate metabolic pathways, conversion efficiencies, and turnover rates in vivo. |
| Specialized Lipid Emulsions (e.g., Soybean, Fish Oil, Olive/Olive-Soy, SMOFlipid) | Used in preclinical and clinical research to compare the effects of different fatty acid compositions on EFAD prevention and other outcomes [29] [28]. |
| Fatty Acid Methyl Ester (FAME) Standards | Certified reference materials used for peak identification and calibration curves in GC analysis [11]. |
| Δ-6 and Δ-5 Desaturase Enzyme Assays | Used to measure the activity of key enzymes in the PUFA elongation/desaturation pathway, which can be influenced by diet, genetics, and health status [1]. |
Core Concepts: FADS Genetics and Fatty Acid Metabolism
What are the FADS genes and why are they critical in fatty acid research?
The Fatty Acid Desaturase (FADS) gene cluster on chromosome 11 (11q12–q13.1) includes three genes—FADS1, FADS2, and FADS3—that encode enzymes vital for polyunsaturated fatty acid (PUFA) metabolism [31] [32]. FADS1 and FADS2 encode the rate-limiting delta-5 desaturase (D5D) and delta-6 desaturase (D6D) enzymes, respectively, which catalyze the formation of double bonds in long-chain PUFAs (LC-PUFAs) [32] [33]. These enzymes determine the efficiency of converting dietary essential fatty acids (linoleic acid [LA] and alpha-linolenic acid [ALA]) into biologically active LC-PUFAs such as arachidonic acid (ARA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA) [32] [34]. The FADS3 gene's function is less clearly defined [31] [35].
How do genetic variations in the FADS cluster influence fatty acid status?
Common single nucleotide polymorphisms (SNPs) in the FADS cluster are major genetic determinants of LC-PUFA levels in blood, cells, and tissues [32]. These SNPs significantly impact the activity of desaturase enzymes, thereby altering the composition of LC-PUFA-containing complex lipids like phospholipids, lyso-phospholipids, and endocannabinoids [35]. The minor alleles of several FADS SNPs (e.g., rs174537, rs174556, rs174570) are consistently associated with reduced desaturase activity, leading to an accumulation of metabolic precursors (e.g., dihomo-γ-linolenic acid [DGLA]) and decreased levels of products (e.g., ARA) [31] [36] [35]. This genetic variation is a key source of inter-individual and inter-population differences in PUFA status.
Diagram Title: FADS-Mediated LC-PUFA Biosynthesis Pathways
Essential Methodologies and Analytical Approaches
What are the standard protocols for assessing FADS activity and genetic influence?
Desaturase activities are conventionally estimated using product-to-precursor ratios in blood or tissue samples, as direct enzyme measurement is complex [37]. These indices serve as reliable proxies for in vivo enzyme activity.
D5D (FADS1) Activity:
- Calculation: ARA (20:4n-6) / DGLA (20:3n-6) [37]
- Protocol: Fatty acid composition is typically determined by gas chromatography (GC). Lipids are extracted from plasma or erythrocyte membranes using methods like Bligh and Dyer. After extraction, fatty acids are derivatized to fatty acid methyl esters (FAMEs) using boron trifluoride-methanol and quantified by GC with a flame ionization detector (FID). Peaks are identified by comparing retention times to external FAME standards, and fatty acid concentrations are expressed as a percentage of total fatty acids [38] [37].
D6D (FADS2) Activity:
- Calculation: GLA (18:3n-6) / LA (18:2n-6) [37]
- Protocol: The sample preparation and GC analysis follow the same rigorous steps as for D5D measurement, ensuring consistency across assays [37].
What methods are used for genotyping FADS polymorphisms?
- DNA Extraction: Genomic DNA is isolated from peripheral blood leukocytes or other tissues using commercial kits (e.g., QIAamp DNA Mini Kit) [36].
- Genotyping Platforms: Multiple high-throughput methods are employed:
- TaqMan Assays: Used for genotyping specific SNPs (e.g., rs738409 in PNPLA3) with high specificity [31].
- BeadChip Arrays: Platforms like the Infinium Exome BeadChip or the Axiom Precision Medicine Research Array enable genome-wide genotyping or focused analysis of many SNPs simultaneously [38] [36].
- High-Resolution Melting (HRM) Analysis: A post-PCR method used to identify genetic variants based on DNA melting curve profiles, as applied in recent intervention studies [34].
- Quality Control (QC): Essential steps include assessing sample call rates, testing for Hardy-Weinberg equilibrium (HWE), and verifying minor allele frequency (MAF) against reference databases [38] [36].
Troubleshooting Common Experimental Challenges
We observe inconsistent associations between FADS genotypes and DHA levels across studies. How should we interpret this?
Inconsistent associations, particularly for DHA, are a known challenge and often stem from population-specific allele frequencies and dietary intake differences [34]. For example, the minor allele (T) of FADS1 rs174537 is associated with lower plasma DHA in some European cohorts but with higher DHA in some East Asian cohorts with coronary artery disease or type 2 diabetes [34]. This discrepancy may be partly explained by the difference in allele frequencies (T allele ~35% in Europeans vs. ~57% in East Asians) [34]. Always consider the ancestral background of your cohort and, if possible, adjust for genetic principal components in your analysis [38]. Furthermore, the availability of dietary precursor fatty acids can modulate the phenotypic expression of these genotypes.
Our lipidomic analysis shows unexpected variability in FADS-associated lipid species. What could be the cause?
The FADS locus regulates a wide array of complex lipids, not just free fatty acids [35]. A key finding is that genetic variation at this locus most strongly influences lipids containing fatty acids that are downstream of the FADS1 (Δ5 desaturase) step. When you encounter variability:
- Verify the Lipid Class: Focus on phospholipids (e.g., phosphatidylinositol, phosphatidylethanolamine, phosphatidylcholine), as these are highly associated with FADS genotypes [31] [35]. For instance, the levels of C36:4 phosphatidylinositol (PI) and C38:3 phosphatidylethanolamine (PE) in human liver are strongly linked to FADS SNPs [31].
- Check the Fatty Acid Position: The sn-2 position of phospholipids is highly enriched with LC-PUFAs through remodeling pathways, and this composition is influenced by FADS activity [35].
- Confirm Analytical Technique: Use targeted lipidomics with ESI-tandem mass spectrometry for precise quantification of individual lipid molecular species, as this method can distinguish between different phospholipid classes containing the same fatty acid [31] [35].
How can we determine if a FADS SNP is functional or merely a marker in linkage disequilibrium?
To establish a functional link, an integrated multi-omics approach is required:
- Expression QTL (eQTL) Analysis: Test if the SNP is associated with the expression levels of FADS1 or FADS2 mRNA in relevant tissues (e.g., liver, adipose). For example, the minor allele of rs174556 is associated with decreased hepatic expression of FADS1 [31], and the minor allele of rs174570 is associated with decreased expression of both FADS1 and FADS2 in adipose tissue [36].
- Methylation QTL (mQTL) Analysis: Investigate if the SNP is associated with DNA methylation changes at CpG sites in the FADS promoter region. The SNP rs174537, for instance, is located in a putative promoter region and is a strong genetic proxy for DNA methylation, which can directly influence gene expression [34] [36].
- Mediation Analysis: Statistically test whether the effect of the SNP on fatty acid levels is mediated (explained) by its effect on DNA methylation or gene expression [36].
Quantitative Data and Research Reagents
Summary of Key FADS Polymorphisms and Their Metabolic Impact
Table 1: Key FADS Gene Polymorphisms and Associated Metabolic Phenotypes
| Gene | SNP | Major/Minor Allele | Primary Functional Association | Impact on Fatty Acids & Lipids | Key References |
|---|---|---|---|---|---|
| FADS1 | rs174537 | G/T | Proxy for DNA methylation; regulates FADS1 expression | Minor (T) allele: ↑ DGLA, ↓ ARA; associated with ↑ hepatic fat content | [31] [34] |
| FADS1 | rs174556 | C/T | Associated with hepatic FADS1 mRNA expression | Minor (T) allele: ↓ FADS1 expression; alters liver phospholipid composition | [31] |
| FADS1 | rs174547 | T/C | In strong LD with other FADS1 SNPs; tag SNP | Minor (C) allele: ↓ D5D activity, ↓ HDL-C in T2D | [37] |
| FADS2 | rs174570 | C/T | eQTL for FADS1 & FADS2; mQTL for CpG sites | Minor (T) allele: ↓ FADS1/FADS2 expression; alters multiple LC-PUFA lipids | [38] [36] |
| FADS2 | rs174576 | C/T | Often used as a tag SNP for the locus | Minor (T) allele: strongly associated with ↑ C36:4 PI and C38:3 PE in liver | [31] |
| FADS1/FADS2 | rs174564 | A/G | Peak association for many complex lipids | Minor (G) allele: ↓ FADS1, ↑ FADS2 expression; strongly ↓ ARA-containing phospholipids | [35] |
Table 2: Response to Fish Oil Supplementation by Genotype (Example from an Intervention Study)
| Genotype Group | Baseline EPA/DHA | Post-Supplementation EPA/DHA Change | Omega-3 Index Response | Study |
|---|---|---|---|---|
| ELOVL2 rs953413 (GG) | No significant difference | Significant increase | Significant improvement | [34] |
| ELOVL2 rs953413 (GA+AA) | No significant difference | Greater significant increase | More favorable metabolic response | [34] |
| FADS1 rs174537 (GG) | Varies by population | Significant increase | Significant improvement | [34] |
| FADS1 rs174537 (TT) | Varies by population | Significant increase (magnitude may differ) | Significant improvement | [34] |
The Scientist's Toolkit: Essential Research Reagents and Resources
Table 3: Key Research Reagents and Resources for FADS Studies
| Reagent / Resource | Function / Application | Example Specifications / Notes |
|---|---|---|
| Gas Chromatograph with FID | Quantifying fatty acid composition in blood/tissues. | Equipped with a capillary column (e.g., Agilent J&W DB-225); uses internal standard (e.g., C17:0). Critical for calculating desaturase indices. [38] [37] |
| ESI-Tandem Mass Spectrometer | Targeted lipidomic analysis of complex lipids (e.g., phospholipids). | Enables precise measurement of individual lipid molecular species (e.g., specific phosphatidylinositols) affected by FADS genotype. [31] [35] |
| Genotyping Platform | Determining FADS SNP alleles in study participants. | Includes TaqMan assays for specific SNPs, or BeadChip arrays (e.g., Illumina Infinium, Affymetrix Axiom) for high-throughput analysis. [31] [34] [38] |
| Commercial Fatty Acid Standards | Identifying and quantifying fatty acid peaks in GC. | Standard mixtures (e.g., FAME 37 from Sigma-Aldrich) are essential for accurate peak assignment and quantification. [38] |
| DNA/RNA Extraction Kits | Isolating high-quality nucleic acids from biological samples. | Kits such as QIAamp DNA Mini Kit and RNeasy Plus Universal Kit ensure pure DNA/RNA for genotyping and expression studies. [36] |
FAQs for Research Design and Application
How should we account for population stratification in FADS genetic studies?
Population stratification is a critical concern because allele frequencies in the FADS cluster vary dramatically among ethnicities [32] [39]. For example, approximately 80% of African Americans carry two copies of alleles associated with higher ARA levels, compared to only about 45% of European Americans [32]. This can confound associations if not properly addressed. To mitigate this:
- Genomic Control: Use genome-wide data to calculate principal components (PCs) and include these PCs as covariates in your association models to control for ancestry [38] [36].
- Stratified Analysis: If sample size permits, analyze different ancestral groups separately.
- Report Ancestry: Always clearly describe the ancestral background of your study population, as findings in one group may not be directly generalizable to another [34] [39].
What is the evidence for gene-diet interactions involving FADS polymorphisms?
Strong evidence shows that FADS genotypes interact with dietary PUFA intake to influence lipid profiles and metabolic health [32] [38]. For instance:
- Carriers of the FADS1 rs174546 TT genotype (associated with reduced desaturase activity) who consumed higher amounts of DHA or had a higher dietary LA/ALA ratio showed lower serum concentrations of total cholesterol, VLDL, and non-HDL cholesterol [38].
- The modern Western diet, high in LA (6-8% of calories) and with a high LA to ALA ratio (>10:1), may disproportionately increase the production of pro-inflammatory ARA-derived eicosanoids in individuals with genetic variants associated with high desaturase efficiency [32].
- These interactions underscore that universal dietary recommendations for PUFAs may be suboptimal, and genetic background should be considered for personalized nutrition strategies [32] [34] [38].
How are FADS polymorphisms linked to disease risk in the context of fatty acid deficiency prevention?
FADS variants modulate the risk of diseases where LC-PUFA status is implicated, highlighting their importance in prevention research.
- Hepatic Fat Accumulation: The minor alleles of FADS1 SNPs are associated with increased total hepatic fat content, suggesting a role in NAFLD pathogenesis [31].
- Cardiometabolic Risk: FADS polymorphisms are linked to altered blood lipid levels (e.g., HDL-C, VLDL) and are associated with coronary artery disease, metabolic syndrome, and type 2 diabetes [32] [33] [37].
- Inflammation and Resolution: By regulating the balance between ARA (n-6) and EPA/DHA (n-3), FADS genotypes influence the substrate availability for producing both pro-inflammatory eicosanoids and specialized pro-resolving mediators (e.g., resolvins, protectins), thereby affecting inflammatory processes [32] [34].
Navigating Diagnostic Challenges and Optimizing Protocols with Modern Lipid Emulsions
For decades, the Holman Index, also known as the triene-to-tetraene (T:T) ratio, has served as the primary biochemical marker for diagnosing essential fatty acid (EFA) deficiency. This ratio quantifies the relationship between mead acid (20:3ω-9), an non-essential fatty acid that accumulates during deficiency states, and arachidonic acid (20:4ω-6), an essential omega-6 fatty acid. A T:T ratio > 0.2 has traditionally indicated biochemical EFA deficiency, with clinical signs typically appearing at ratios > 0.4 [29]. However, evolving clinical evidence and advancements in nutritional science have revealed significant limitations of this standalone measurement. This technical support guide examines why the T:T ratio alone is insufficient for modern research and clinical practice, providing troubleshooting guidance and methodological recommendations for scientists investigating EFA deficiency prevention strategies.
FAQ: Understanding the Holman Index and Its Limitations
What is the fundamental biochemical principle behind the Holman Index? The Holman Index is based on the competitive inhibition between fatty acid families for desaturase enzymes. During EFA deficiency, the absence of linoleic acid (LA) and alpha-linolenic acid (ALA) allows oleic acid to be metabolized to mead acid. The ratio of this triene (mead acid) to tetraene (arachidonic acid) provides an index of deficiency severity, with elevation indicating a shift toward non-essential fatty acid metabolism [29].
Why might a patient with normal T:T ratio still exhibit EFA deficiency symptoms? The T:T ratio specifically reflects arachidonic acid status relative to mead acid but fails to account for omega-3 fatty acid status. Patients can develop omega-3 deficiency symptoms, including neurological and visual impairments, while maintaining a normal T:T ratio [29] [40]. This limitation is particularly relevant with modern lipid emulsions that alter typical fatty acid profiles.
How do novel lipid emulsions challenge traditional T:T ratio interpretation? Modern composite lipid emulsions (e.g., SMOFlipid) and fish oil-based emulsions significantly alter erythrocyte membrane fatty acid composition, increasing EPA and DHA while potentially decreasing arachidonic acid. Research shows these changes can occur without elevating the T:T ratio, demonstrating that the ratio may not detect deficiency states in patients receiving these therapies [41] [42].
What genetic factors influence T:T ratio reliability? Recent evidence indicates that genetic polymorphisms in fatty acid desaturase genes can significantly impact arachidonic acid levels independently of EFA status. Patients with these polymorphisms may present with extreme arachidonic acid values that distort T:T ratio interpretation without true deficiency [13].
How does linoleic acid concentration compare to T:T ratio for clinical correlation? In pediatric cystic fibrosis patients, serum phospholipid linoleic acid concentration ≥21 mol% demonstrated stronger correlations with growth parameters and pulmonary function than the T:T ratio. Patients with adequate LA showed significantly better weight, height, BMI, and FEV1 outcomes, suggesting LA concentration may be a more clinically relevant biomarker [43].
Troubleshooting Guide: Experimental Challenges in EFA Deficiency Research
Problem 1: Inconsistent Results Between Biochemical and Clinical EFA Deficiency
Potential Cause: The T:T ratio measures a specific metabolic imbalance but doesn't reflect overall EFA status or functional deficits.
Solution: Implement a comprehensive fatty acid profiling approach:
- Methodology: Use gas chromatography-mass spectrometry to analyze plasma and erythrocyte membrane fatty acids
- Parameters: Quantify individual fatty acids (LA, ALA, AA, EPA, DHA, Mead acid) rather than relying solely on ratios
- Frequency: Monitor profiles serially in longitudinal studies as fatty acid status can fluctuate
Supporting Evidence: Studies of home parenteral nutrition patients receiving omega-3 enriched emulsions showed substantial alterations in EPA and DHA without T:T ratio changes, indicating the ratio's insensitivity to important fatty acid modifications [41].
Problem 2: Failure to Detect Early or Subtle Deficiency States
Potential Cause: The T:T ratio elevation occurs only after substantial depletion of EFA stores.
Solution: Incorporate multiple sensitive biomarkers:
- Linoleic Acid Threshold: Monitor absolute LA concentrations with <21 mol% in serum phospholipids indicating deficiency risk [43]
- Omega-3 Index: Measure erythrocyte EPA+DHA as a percentage of total fatty acids (target >8%) [42]
- Functional Assays: Include inflammatory markers and visual function tests that reflect EFA functional status
Problem 3: Genetic Variability Affecting Interpretation
Potential Cause: Polymorphisms in FADS genes alter desaturase activity and fatty acid conversion.
Solution: Implement genetic screening in study protocols:
- Method: Genotype for common FADS variants (rs174537, rs174575, rs174455)
- Analysis: Stratify results based on genotype or include as covariate in statistical models
- Application: Particularly crucial in studies with diverse populations or when extreme AA values are observed [13]
Problem 4: Impact of Modern Lipid Emulsions on Traditional Metrics
Potential Cause: Newer lipid emulsions with olive oil, MCT, and fish oil create atypical fatty acid patterns that don't follow traditional deficiency paradigms.
Solution: Establish emulsion-specific reference ranges:
- Baseline Assessment: Obtain comprehensive fatty acid profile before initiating therapy
- Emulsion-Specific Targets: Develop expected ranges based on emulsion composition
- Longitudinal Monitoring: Track individual patient trends rather than relying on population norms
Supporting Evidence: Pediatric studies with olive oil-based emulsions (80% olive/20% soybean) showed stable AA values and no EFAD despite different fatty acid patterns compared to pure soybean emulsions [13].
Experimental Protocols for Comprehensive EFA Assessment
Protocol 1: Comprehensive Fatty Acid Profiling in Plasma and Erythrocytes
Principle: Simultaneous quantification of multiple fatty acid classes provides a complete picture of EFA status beyond the T:T ratio.
Materials:
- Venous blood collection tubes (EDTA)
- Centrifuge capable of 3000×g
- Solid-phase extraction system
- Gas chromatograph with mass spectrometer
- Fatty acid methyl ester standards
Procedure:
- Collect fasting blood samples and separate plasma and erythrocytes by centrifugation
- Extract total lipids using Folch method (chloroform:methanol 2:1 v/v)
- Separate phospholipid fraction using aminopropyl solid-phase extraction cartridges
- Prepare fatty acid methyl esters with boron trifluoride-methanol
- Analyze by GC-MS using a 100-m capillary column with programmed temperature ramp
- Quantify using internal standard method with heneicosanoic acid (21:0) as internal standard
Interpretation: Calculate molar percentages of individual fatty acids and key ratios. Compare to method-specific reference ranges.
Protocol 2: Genetic Analysis of FADS Polymorphisms
Principle: Identify genetic variants that affect fatty acid desaturation and metabolism.
Materials:
- DNA extraction kit
- PCR reagents and thermal cycler
- TaqMan genotyping assays or sequencing platform
- FADS1 and FADS2 SNP panels
Procedure:
- Extract DNA from whole blood or saliva
- Amplify FADS gene regions of interest using PCR
- Genotype key SNPs (rs174537, rs174575, rs174455) using validated assays
- Verify genotype quality with duplicate samples and controls
- Associate genotypes with fatty acid profiles and metabolic outcomes
Interpretation: Classify patients by FADS genotype and adjust expected fatty acid patterns accordingly.
Quantitative Data Comparison: Traditional vs. Comprehensive Assessment
Table 1: Comparative Performance of EFA Deficiency Assessment Methods
| Assessment Method | Analytical Target | Deficiency Threshold | Clinical Correlation Strength | Limitations |
|---|---|---|---|---|
| Holman Index (T:T ratio) | Mead acid:AA ratio | >0.2 (biochemical) >0.4 (clinical) | Moderate for classical deficiency | Insensitive to ω-3 status; affected by genetic variation |
| Linoleic Acid Concentration | Serum phospholipid LA | <21 mol% (at-risk) <15 mol% (deficient) | Strong for growth and pulmonary outcomes | Does not reflect ω-3 status; requires specific methodology |
| Omega-3 Index | Erythrocyte EPA+DHA | <4% (deficient) >8% (target) | Strong for cardiovascular and neurological outcomes | Does not assess ω-6 status; requires specialized analysis |
| Comprehensive Profiling | Multiple fatty acid classes | Method-specific reference ranges | Excellent for complete assessment | Technically demanding; higher cost; complex interpretation |
Table 2: Impact of Different Lipid Emulsions on Fatty Acid Parameters
| Lipid Emulsion Type | LA Content (%) | ALA Content (%) | EPA+DHA Content (%) | Effect on T:T Ratio | Effect on ω-3 Index |
|---|---|---|---|---|---|
| Soybean Oil (Intralipid) | 50 | 9 | 0 | Reference | Decrease or no change |
| Fish Oil (Omegaven) | 4.4 | 1.8 | 31.3 | No significant increase | Significant increase |
| Composite (SMOFlipid) | 21.4 | 2.5 | 5 | No significant increase | Moderate increase |
| Olive/Soybean (Clinoleic) | 18.5 | 2 | 0 | No significant increase | No significant change |
Research Reagent Solutions for EFA Deficiency Studies
Table 3: Essential Research Materials for EFA Deficiency Investigations
| Reagent/Material | Function/Application | Key Considerations |
|---|---|---|
| Lipid Emulsions (SO, FO, MCT, OO, SMOF) | Investigate effects of different fatty acid compositions on EFA status | Varying EFA content allows modeling of different deficiency states; monitor liver function parameters |
| Fatty Acid Methyl Ester Standards | GC-MS quantification of fatty acid profiles | Must include Mead acid, AA, LA, ALA, EPA, DHA for comprehensive assessment |
| Aminopropyl SPE Cartridges | Separation of phospholipid fraction for profiling | Provides specific membrane composition data versus total plasma fatty acids |
| FADS Genotyping Assays | Analysis of genetic polymorphisms affecting fatty acid metabolism | Essential for interpreting atypical fatty acid patterns and personalizing reference ranges |
| Erythrocyte Isolation Kits | Preparation of samples for omega-3 index determination | Provides long-term status indicator versus plasma's short-term fluctuations |
Metabolic Pathways and Experimental Workflows
Essential Fatty Acid Metabolic Pathway and Holman Index Limitations
Comparative Workflow: Traditional vs. Comprehensive EFA Assessment
The Holman Index represents an important historical tool for identifying severe, classical EFA deficiency but possesses significant limitations for contemporary research and clinical practice. The T:T ratio alone fails to detect omega-3 specific deficiency, demonstrates poor correlation with clinical outcomes in certain populations, and proves unreliable with modern lipid emulsions and in individuals with FADS genetic variations. Researchers should implement comprehensive assessment protocols that include complete fatty acid profiling, genetic analysis, and multiple biomarker interpretation to accurately characterize EFA status and advance deficiency prevention strategies.
The composition of intravenous lipid emulsions (ILEs) used in parenteral nutrition (PN) is shifting from traditional pure soybean oil (SO) formulations toward soybean-oil-sparing alternatives. These modern ILEs partially replace SO with oils such as olive oil (OO), medium-chain triglycerides (MCT), and fish oil (FO) to reduce the high omega-6 polyunsaturated fatty acid (PUFA) content, which is linked to pro-inflammatory and immunosuppressive effects [44] [45]. A primary concern with this shift is whether reducing the SO content, a major source of the essential fatty acid (EFA) linoleic acid (LA), increases the risk of Essential Fatty Acid Deficiency (EFAD) [10]. EFAD can develop rapidly, particularly in infants, if ILE is omitted from PN, and its biochemical hallmark is an elevated triene-to-tetraene (T:T) ratio [10] [46]. This resource center provides evidence-based guidance for researchers assessing EFAD risk in the context of modern ILEs.
Frequently Asked Questions (FAQs)
FAQ 1: What is the primary biochemical marker for EFAD, and is it sufficient for assessment? The traditional primary marker is the plasma triene:tetraene (T:T) ratio, specifically the ratio of mead acid (a non-essential fatty acid) to arachidonic acid (ARA) [10] [46]. A ratio above 0.2-0.4 is generally considered diagnostic for EFAD [10] [46]. However, recent evidence suggests this single marker is not sufficient. A comprehensive assessment should also include the analysis of the complete fatty acid profile—specifically low levels of linoleic acid (LA) and arachidonic acid (ARA), alongside high mead acid—and an evaluation of genetic polymorphisms in fatty acid desaturase (FADS) genes [10].
FAQ 2: Do soybean-oil-sparing ILEs increase the risk of EFAD in pediatric populations? Current evidence indicates that soybean-oil-sparing ILEs do not increase the risk of EFAD in pediatric patients. A 2025 randomized, double-blind, controlled study in pediatric patients (including 94 preterm infants) comparing an 80% olive oil/20% soybean oil (OO/SO) ILE to a 100% SO ILE found that no EFAD was observed in either group over a treatment duration of approximately 10-11 days [10]. While LA levels increased to a lesser extent in the OO/SO group, ARA levels remained stable in both [10].
FAQ 3: What are the generations of ILEs and their compositions? ILEs are categorized into generations based on their oil source composition [44]:
- First Generation: 100% Soybean Oil
- Second Generation: Soybean oil mixed with MCTs or safflower oil
- Third Generation: 80% Olive Oil / 20% Soybean Oil
- Fourth Generation: Any formulation containing fish oil (e.g., mixtures of SO, MCT, OO, and FO)
FAQ 4: Beyond EFAD prevention, what are the clinical benefits of newer ILEs? Newer-generation ILEs, particularly those containing fish oil, are associated with significant clinical benefits linked to their anti-inflammatory and pro-resolving properties [44] [45] [47]. Meta-analyses of randomized controlled trials (RCTs) have shown that fish-oil-containing ILEs can lead to:
- A 40% reduction in infections [44] [47].
- A 56% reduction in sepsis [44] [47].
- Significantly shorter ICU and hospital length of stay [44] [47].
- A trend toward reduced mortality [44].
Troubleshooting Guide: Common Experimental Challenges
Challenge 1: Interpreting Conflicting Biomarker Results
- Problem: A study subject has a triene:tetraene (T:T) ratio in the "indeterminate" range (0.2-0.4), making EFAD diagnosis unclear [10].
- Solution: Do not rely solely on the T:T ratio. Implement a comprehensive fatty acid profiling via gas chromatography [10] [48]. Confirm EFAD by looking for a pattern of low LA, low ARA, and high mead acid simultaneously [10]. Furthermore, consider genetic analysis for polymorphisms in the fatty acid desaturase (FADS) genes, as these can significantly influence fatty acid levels and explain outliers [10].
Challenge 2: Selecting an Appropriate Preclinical Model for Neonatal ILE Studies
- Problem: The unique lipid requirements of preterm infants, including the need for preformed arachidonic acid (ARA) and docosahexaenoic acid (DHA), are not adequately met by ILEs designed for adults [48].
- Solution: The neonatal piglet model is a well-established and translatable model for studying infant lipid metabolism [48]. Key methodological considerations include:
- Dosing Translation: Account for the faster growth rate; a dose of 10 g/kg/day in piglets translates to approximately 2 g/kg/day in human infants [48].
- Tissue Analysis: After a standard study period (e.g., 14 days), collect key tissues (serum, liver, brain, lung, retina, jejunum) and analyze fatty acid composition in total phospholipids to assess deposition [48].
- Novel Formulation Testing: Use the model to test novel ILEs specifically designed for neonates, which provide optimized levels of ARA and DHA while sparing eicosapentaenoic acid (EPA), as high EPA can inhibit ARA tissue deposition [48].
Challenge 3: Accounting for Clinical Outcomes Beyond Biochemical EFAD
- Problem: A study confirms an ILE does not cause EFAD, but fails to capture its potential to induce pro-inflammatory effects.
- Solution: Expand the outcome measures. For ILEs with high SO content, assess inflammatory markers (e.g., cytokines) and monitor for hepatobiliary complications like PNALD [44] [45]. For ILEs containing FO, measure biomarkers of inflammation resolution, such as specialized pro-resolving mediators (SPMs) like resolvins and protectins, which are derived from EPA and DHA [47].
Structured Data for Experimental Design
Table 1: Fatty Acid Composition of Key Intravenous Lipid Emulsions (ILEs)
This table provides a comparison of common ILEs, highlighting the reduction in linoleic acid (LA) in soybean-oil-sparing formulations. [10] [44]
| Product Name (Example) | Lipid Sources | Linoleic Acid (LA) % | α-Linolenic Acid (ALA) % | ARA % | EPA % | DHA % | n-6:n-3 Ratio |
|---|---|---|---|---|---|---|---|
| SO-ILE (Intralipid) | 100% Soybean Oil | ~54.7 | ~6.7 | 0.2 | 0 | 0.1 | ~7:1 |
| OO/SO-ILE (Clinoleic) | 80% Olive Oil, 20% Soybean Oil | ~18.6 | ~1.7 | 0.2 | 0 | 0.1 | ~9:1 |
| SO/MCT/FO-ILE (Lipidem) | 40% SO, 50% MCT, 10% FO | ~24.5 | ~3.5 | 0 | ~3.5 | ~2.5 | ~2.7:1 |
| SO/MCT/OO/FO-ILE (SMOFlipid) | 30% SO, 30% MCT, 25% OO, 15% FO | ~21.4 | ~2.5 | 0.15-0.6 | ~3 | ~2 | ~2.5:1 |
| FO-ILE (Omegaven) | 100% Fish Oil | ~4.4 | ~1.8 | 1-4 | ~19.2 | ~12.1 | ~1:8 |
Table 2: Core Protocol for a Randomized Controlled Trial (RCT) Assessing EFAD Risk
This table outlines a methodology based on a recent pediatric RCT, adaptable for research in other populations. [10]
| Protocol Element | Description & Rationale |
|---|---|
| Study Design | Randomized, double-blind, controlled, multicenter trial. |
| Population | Patients expected to require PN for ≥7 days. Key exclusion: pre-existing liver disease, severe hypertriglyceridemia. |
| Intervention & Comparator | Intervention: 80% OO / 20% SO ILE (e.g., Clinoleic).Comparator: 100% SO ILE (e.g., Intralipid). |
| Dosing | Start at 1 g/kg/day and increase incrementally to goal (e.g., 2.5-3 g/kg/day for infants). |
| Primary Outcome | Incidence of EFAD, defined by a plasma T:T ratio >0.4, confirmed by low LA, low ARA, and high mead acid. |
| Key Biomarkers | Plasma Fatty Acid Profile: LA, ARA, Mead Acid, EPA, DHA.T:T Ratio Calculation: Mead Acid / ARA. |
| Additional Analyses | Genetic polymorphism analysis in fatty acid desaturase (FADS) genes in patients with extreme ARA values. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Significance in EFAD Research |
|---|---|
| Gas Liquid Chromatography | The gold-standard method for precise separation and quantification of individual fatty acids in plasma or tissue samples [48]. |
| Commercial ILEs (Intralipid, Clinoleic, SMOFlipid) | Standardized reagents for use as comparators or test articles in preclinical and clinical studies [10] [44]. |
| Neonatal Piglet Model | A translatable animal model for studying ILE metabolism, fatty acid deposition in tissues, and related outcomes like immune function and neurodevelopment [48]. |
| ELISA/Luminex Kits | For quantifying downstream protein biomarkers, such as inflammatory cytokines (e.g., IL-6, TNF-α) in serum or tissue homogenates [48]. |
| Genetic Sequencing Kits | For identifying polymorphisms in the FADS gene cluster, which can confound fatty acid profile results and are a key variable in personalized nutrition research [10]. |
| Specialized Pro-Resolving Mediator (SPM) Assays | To measure bioactive metabolites of omega-3 PUFAs (e.g., Resolvins, Protectins) that mediate the active resolution of inflammation [47]. |
Visualizing Metabolic Pathways and Experimental Logic
Fatty Acid Metabolism & EFAD Biomarkers
Experimental Workflow for EFAD Risk Assessment
Essential fatty acid deficiency (EFAD) represents a significant clinical challenge in both research and therapeutic contexts. This technical support guide provides researchers and drug development professionals with comprehensive methodologies for integrating full fatty acid profiles with clinical signs to enhance EFAD prevention strategies. The systematic approach outlined below facilitates accurate detection, monitoring, and intervention in experimental and clinical settings.
Core Diagnostic Parameters and Clinical Correlations
Key Fatty Acid Markers and Interpretation
Table 1: Essential Fatty Acid Biomarkers and Diagnostic Significance
| Biomarker | Normal Function | Deficiency Indicator | Clinical Correlation |
|---|---|---|---|
| Linoleic Acid (LA) | Precursor for omega-6 series; maintains skin integrity | Decreased plasma levels | Scaling dermatitis, impaired wound healing [13] |
| Arachidonic Acid (AA) | Eicosanoid production; inflammatory mediation | Decreased plasma levels | Compromised immune function, growth retardation [13] |
| Triene:Tetraene Ratio (T:T) | Balance of fatty acid metabolism | Ratio >0.2 indicates EFAD | Correlates with severity of deficiency symptoms [13] |
| Mead Acid (20:3ω-9) | Alternative pathway product | Elevated in deficiency | Marker of prolonged EFAD status [13] |
| Omega-3 Fatty Acids | Neurological development, anti-inflammatory | Decreased levels | Cognitive impairment, visual dysfunction [49] |
Analytical Methodologies for Fatty Acid Profiling
Nuclear Magnetic Resonance (NMR) Spectroscopy
- Protocol: Plasma/serum samples collected in EDTA tubes, centrifuged at 2500g for 10 minutes at 4°C, with supernatant stored at -80°C until analysis [49]
- Measurement Parameters: Absolute concentrations and percentages of specific components to total fatty acids assessed using Nightingale Health's NMR metabolomics platform [49]
- Applications: High-throughput analysis suitable for large cohort studies (demonstrated in n=148,308 UK Biobank participants) [49]
Gas Chromatography-Mass Spectrometry (GC-MS)
- Sample Preparation: Lipid extraction using Folch method, methylation, and separation on capillary columns
- Quantification: Absolute quantification using internal standards (e.g., heptadecanoic acid)
- Advantages: High sensitivity for detecting subtle changes in fatty acid profiles; ideal for pediatric populations with limited sample volumes [13]
Troubleshooting Guides for Experimental Challenges
Pre-Analytical Variables
FAQ: How should samples be handled to prevent fatty acid degradation?
- Collect blood in EDTA tubes and process within 2 hours of collection
- Centrifuge at 2500g for 10 minutes at 4°C
- Aliquot plasma/serum and store at -80°C in cryovials
- Avoid repeated freeze-thaw cycles (maximum 2 cycles recommended)
FAQ: What dietary confounding factors should be controlled in study design?
- Standardize fasting duration (8-12 hours) before sampling
- Document recent dietary intake of omega-3 and omega-6 rich foods
- Consider genetic polymorphisms in fatty acid desaturase (FADS) genes that affect metabolism [13]
Analytical Challenges
FAQ: How to address inconsistent triene:tetraene ratios?
- Validate with complete fatty acid profile rather than single ratio
- Consider genetic polymorphisms in patients with extreme arachidonic acid values [13]
- Correlate with clinical signs (dermatitis, growth metrics) for confirmation
FAQ: What quality controls ensure analytical precision?
- Include internal standards in each batch
- Participate in external proficiency testing programs
- Maintain coefficient of variation <10% for major fatty acids
Advanced Integration Approaches
Multi-Omics Correlation Strategies
Multi-Omics Integration Workflow for EFAD Research
Biomarker Integration Framework
Table 2: Correlation Between Fatty Acid Profiles and Clinical Endpoints
| Fatty Acid Parameter | Associated Clinical Signs | Research Context | Intervention Threshold |
|---|---|---|---|
| Linoleic acid <28% total FA | Dermatitis, hair loss | Pediatric parenteral nutrition [13] | Initiate lipid emulsion <1.0g/kg/day |
| ω-6:ω-3 ratio >10:1 | Inflammatory markers ↑ | Alzheimer's disease risk assessment [49] | Dietary modification |
| L-FABP elevation | Liver steatosis, fibrosis | Metabolic dysfunction-associated steatotic liver disease [50] | Hepatoprotective agents |
| SCFA reduction (butyrate) | Cachexia, weight loss | Gastric cancer complications [51] | Prebiotic supplementation |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Fatty Acid Deficiency Research
| Reagent/Material | Function | Application Example |
|---|---|---|
| Olive oil-based intravenous lipid emulsion | EFAD prevention | 80% olive oil/20% soybean oil blend in pediatric trials [13] |
| Liver-type fatty acid binding protein (L-FABP) ELISA kits | Hepatic steatosis biomarker | Quantifying MASLD progression in pediatric patients [50] |
| MedDRA coding terminology | Adverse event classification | Standardizing EFAD clinical signs in FAERS database [52] [53] |
| FADS genotyping panels | Genetic polymorphism detection | Identifying patients with extreme arachidonic acid metabolism [13] |
| Short-chain fatty acid standards | GC-MS quantification | Profiling acetate, butyrate, heptanoate in cachexia studies [51] |
Methodological Validation and Quality Assurance
Protocol Implementation Framework
Fatty Acid Analysis Quality Assurance Pathway
Statistical Considerations for EFAD Research
- Sample Size Calculation: Utilize GPower software with effect size OR=1.5, α=0.05, power ≥85% (validated with n=199 in pediatric study) [50]
- Confounding Adjustment: Multivariate regression for age, gender, APOE ε4 status (in neurological contexts) [49]
- Longitudinal Analysis: Mixed-effects models for repeated fatty acid measurements
Integrating comprehensive fatty acid profiling with clinical signs provides a powerful framework for EFAD prevention research. The methodologies and troubleshooting guides presented here enable researchers to implement robust diagnostic approaches that account for genetic, metabolic, and clinical variables. This systematic integration advances personalized prevention strategies and enhances translational applications in both clinical and research settings.
Troubleshooting Guide: ILE Complications and Research Solutions
Table 1: Common ILE-Related Complications and Diagnostic Approaches
| Complication | Key Risk Factors | Primary Diagnostic Methods | Preventive Research Strategies |
|---|---|---|---|
| Essential Fatty Acid Deficiency (EFAD) | Fat-free PN, specific ILE formulations with low LA content [10]. | Plasma T:T ratio > 0.4; low linoleic acid (LA) and arachidonic acid (ARA); clinical features (dermatitis) [10]. | Ensure minimum LA intake (0.1-0.25 g/kg/day); use ILEs with sufficient LA; monitor full fatty acid profile [10]. |
| Hepatotoxicity/Liver Disease | Long-term PN, specific underlying diseases (e.g., hypertriglyceridemia) [54] [55]. | Serum liver enzymes (ALT, AST), MRI for steatosis (>5% liver fat) [55]. | Omega-3 supplementation; use of alternative ILE formulations (e.g., olive oil-based) [55] [56] [10]. |
| Inflammation | Use of soybean oil-based ILEs in certain contexts [57]. | Measurement of inflammatory cytokines (TNF-α, IL-6) [57]. | Use of SCFAs (e.g., sodium butyrate) or omega-3 fatty acids to modulate inflammatory pathways [57] [56]. |
Frequently Asked Questions
Q1: How can I minimize the risk of EFAD when using modern, soybean oil-reduced ILEs in my preclinical models?
The concern that reducing soybean oil content increases EFAD risk is valid, but can be managed with precise monitoring. A recent pediatric RCT demonstrated that an 80% olive oil/20% soybean oil ILE did not increase the incidence of EFAD compared to a 100% soybean oil ILE, despite delivering less linoleic acid (LA) [10].
Critical recommendations for researchers:
- Go Beyond the T:T Ratio: Rely on a complete plasma fatty acid profile, not just the triene:tetraene (T:T) ratio. Monitor LA, arachidonic acid (ARA), and mead acid levels [10].
- Consider Genetic Factors: Be aware that genetic polymorphisms in fatty acid desaturase (FADS) genes can significantly impact ARA levels and EFAD biomarkers, potentially confounding results [10].
- Ensure Minimum LA Intake: In study designs, ensure provision of at least the recommended minimum LA intake (0.25 g/kg/day for preterm infants, 0.1 g/kg/day for term infants and children) [10].
Q2: What are the latest findings on Omega-3 fatty acids concerning hepatotoxicity and liver protection?
Omega-3 fatty acids have a well-established safety profile regarding liver injury and are increasingly shown to be hepatoprotective.
- Safety Profile: Large-scale randomized controlled trials and clinical use have found omega-3 fatty acids (including prescription forms like Lovaza and Vascepa) are "unlikely" causes of clinically apparent liver injury. In high doses for hypertriglyceridemia, ALT elevations were minor, transient, and comparable to placebo [54].
- Protective Effects: A 2023 UK Biobank cohort study found omega-3 supplementation reduced the risk of incident liver disease by 28.4%. Protective associations were particularly strong for alcoholic liver disease (44% risk reduction), liver failure (45% risk reduction), and non-alcoholic fatty liver disease (22% risk reduction) [55].
- Mechanistic Insights: Preclinical models suggest omega-3 fatty acids protect against hepatic steatosis. In a murine model of parenteral nutrition-induced liver injury, enteral omega-3 supplementation completely prevented hepatic pathology and normalized liver function tests [56].
Q3: Which signaling pathways should I target to mitigate ILE-induced inflammation in vitro?
Short-chain fatty acids (SCFAs) and omega-3 fatty acids offer promising mechanisms to counteract inflammation.
Key Pathway - SCFAs (e.g., Sodium Butyrate):
- Mechanism: In IFN-γ-stimulated RAW 264.7 murine macrophage cells, SCFAs (sodium butyrate, sodium phenylbutyrate, sodium phenylacetate) exhibit potent anti-inflammatory effects [57].
- Targets: They inhibit the pro-inflammatory NF-κB pathway by repressing its DNA binding and transcriptional activity. They also repress IFN-γ-induced phosphorylation of ERK1/2 in the MAPK signaling pathway [57].
- Outcome: This dual inhibition leads to reduced expression of iNOS, TNF-α, and IL-6, while enhancing the anti-inflammatory cytokine IL-10 [57].
The diagram below illustrates this anti-inflammatory signaling pathway.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Reagents and Models for ILE Research
| Research Reagent / Model | Function in Research | Key Considerations |
|---|---|---|
| 80% Olive Oil / 20% Soybean Oil ILE | Models modern, mixed-oil ILEs with reduced inflammatory potential and ω-6 FA load [10]. | Confirm LA content is sufficient to prevent EFAD in long-term studies (~18% of total fatty acids) [10]. |
| Omega-3 Fatty Acid Emulsions (EPA/DHA) | Used to investigate hepatoprotective and anti-inflammatory effects in PN settings [56]. | Purity and ratio of EPA:DHA can influence outcomes. Suitable for both enteral and IV administration in models [56]. |
| Short-Chain Fatty Acids (e.g., Sodium Butyrate) | In vitro tool to inhibit NF-κB and ERK signaling pathways in immune cells, reducing inflammation [57]. | Potency can vary (NaB > NaPB > NaPA). Effective in IFN-γ-stimulated macrophages like RAW 264.7 cells [57]. |
| IFN-γ-stimulated RAW 264.7 Murine Macrophages | Standardized in vitro model for studying the anti-inflammatory mechanisms of compounds like SCFAs [57]. | Ensure proper stimulation and controls. Measure outputs like iNOS, TNF-α, IL-6, and IL-10 for a complete picture [57]. |
| Plasma Fatty Acid Profiling (NMR/GC) | Gold-standard method for comprehensive EFAD assessment, beyond the T:T ratio [10]. | Allows simultaneous quantification of LA, ARA, mead acid, and other FAs. Essential for validating self-reported supplement intake in studies [55]. |
Experimental Protocol: Assessing Anti-Inflammatory Effects of Compounds in Macrophages
This protocol is adapted from foundational research on SCFAs [57].
Objective: To evaluate the potential of test compounds (e.g., SCFAs, omega-3 derivatives) to mitigate inflammation in an IFN-γ-stimulated macrophage model.
Materials:
- Cell Line: RAW 264.7 murine macrophage cells
- Inducer: Recombinant murine IFN-γ
- Test Compounds: e.g., Sodium butyrate (NaB), sodium phenylbutyrate (NaPB), sodium phenylacetate (NaPA)
- Key Reagents: Antibodies for phospho-ERK1/2, total ERK, NF-κB p65; ELISA kits for TNF-α, IL-6, IL-10; iNOS detection reagents
Methodology:
- Cell Culture & Stimulation:
- Culture RAW 264.7 cells in standard medium.
- Pre-treat cells with varying concentrations of the test compound for a predetermined time (e.g., 1-2 hours).
- Stimulate cells with IFN-γ (e.g., 10 ng/mL) for 4-24 hours to induce inflammation.
Analysis of Inflammatory Markers (24 hours post-stimulation):
- Protein Level: Collect cell culture supernatant. Quantify secretion of TNF-α, IL-6, and IL-10 using ELISA.
- Gene Expression Level (Optional): Extract total RNA. Analyze mRNA expression of iNOS, TNF-α, IL-6, and IL-10 using RT-qPCR.
Analysis of Signaling Pathways (15-30 minutes post-stimulation for phosphorylation):
- Western Blotting: Harvest cell lysates. Probe for phospho-ERK1/2 and total ERK to assess MAPK pathway inhibition.
- NF-κB Activation: Perform EMSA (Electrophoretic Mobility Shift Assay) or a nuclear fractionation Western blot to measure NF-κB DNA-binding activity and nuclear translocation.
Expected Outcomes: Potent anti-inflammatory compounds like NaB will show a dose-dependent repression of phospho-ERK, NF-κB activation, and pro-inflammatory cytokines (TNF-α, IL-6, iNOS), while potentially enhancing IL-10 expression [57].
Core Concepts & Frequently Asked Questions (FAQs)
FAQ 1: What defines Essential Fatty Acid Deficiency (EFAD) in a research context? Biochemical EFAD is traditionally defined by a plasma triene-to-tetraene (T:T) ratio > 0.2 [2]. This ratio measures mead acid (a marker of deficiency) against arachidonic acid. However, contemporary research emphasizes that diagnosis should not rely on the T:T ratio alone. It should be confirmed through a complete plasma fatty acid profile showing low linoleic acid (LA), low arachidonic acid (ARA), and high mead acid [10] [2]. Clinical signs, such as dermatitis, diarrhea, and poor wound healing, can also manifest [10].
FAQ 2: Does using an olive oil-based ILE increase the risk of EFAD compared to a pure soybean oil ILE? Recent high-quality evidence indicates that it does not. A 2025 randomized, double-blind, controlled trial in pediatric patients found that an 80% olive oil/20% soybean oil ILE did not increase the risk of EFAD compared to a 100% soybean oil ILE, with no cases of EFAD observed in either group over a mean treatment duration of approximately 10-11 days [10] [13] [58]. This demonstrates that reducing soybean oil content does not automatically lead to deficiency.
FAQ 3: What are the key fatty acid compositional differences between common ILE types? The risk of EFAD is influenced by the essential fatty acid content of the ILE. The table below summarizes key differences.
| ILE Type | Linoleic Acid (LA) Content | Alpha-Linolenic Acid (ALA) Content | Oleic Acid Content |
|---|---|---|---|
| 100% Soybean Oil [10] | ~55% | ~6.7% | ~21% |
| 80% Olive Oil / 20% Soybean Oil [10] | ~18% | ~1.7% | ~60% |
| Safflower Oil (Historical) [2] | High in LA | Very Low/None | Not Specified |
FAQ 4: What minimum intake of linoleic acid is recommended to prevent EFAD? To prevent EFAD, the minimum recommended intake of linoleic acid is 0.25 g/kg/day for preterm infants and 0.1 g/kg/day for term infants and children [10]. In a study of pediatric intestinal failure patients on mixed-oil ILEs without lipid restriction, a median fat intake of 1.7 g/kg/day was sufficient to prevent EFAD [59].
FAQ 5: Beyond the T:T ratio, what other factors are critical for a modern EFAD assessment? A comprehensive assessment must include:
- Complete Fatty Acid Profile: Analyzing individual levels of LA, ARA, and mead acid provides a more accurate picture than the T:T ratio alone [10] [13].
- Genetic Polymorphisms: Variations in fatty acid desaturase (FADS) genes can significantly impact fatty acid levels, particularly ARA, and should be considered when evaluating extreme values [10] [13] [58].
Troubleshooting Guide: Common Experimental & Clinical Scenarios
Issue 1: A patient's T:T ratio is elevated (e.g., >0.2), but clinical signs of EFAD are absent.
- Investigation Path:
- Analyze the Full Profile: Check the individual concentrations of LA, ARA, and mead acid. An elevated T:T ratio may be driven by a slight increase in mead acid while LA and ARA levels remain within acceptable limits, which is a different clinical picture than full EFAD [10].
- Review the ILE Composition: The fatty acid profile often reflects the ILE being administered. Newer composite ILEs with lower LA content will naturally result in lower plasma LA levels without necessarily indicating a pathological deficiency [2].
- Consider Genetic Analysis: Screen for polymorphisms in the FADS genes, as these can lead to naturally lower ARA levels, affecting the T:T ratio without true deficiency [10].
Issue 2: Uncertainty in designing a study to evaluate EFAD risk for a novel composite ILE.
- Recommended Protocol:
- Study Design: Implement a randomized, double-blind, controlled trial, which is considered the gold standard for this type of investigation [10] [13].
- Primary Outcome: Define the incidence of EFAD based on both biochemical (T:T ratio > 0.2 plus full fatty acid profile) and clinical criteria [10].
- Key Methodologies:
- Comparison Group: Compare the novel ILE against a well-established ILE, such as a 100% soybean oil-based product [10].
The following diagram illustrates the core diagnostic workflow for investigating a potential EFAD case in a clinical or research setting.
Detailed Experimental Protocols
Protocol 1: Plasma Fatty Acid Profiling via GC-FID
This method is used to quantify non-esterified fatty acids (NEFAs) in serum or plasma samples [11].
Workflow:
- Sample Preparation: Add 75 µL of human serum to a glass tube containing an internal standard (e.g., 10 µg of tridecanoic acid, C13:0).
- Derivatization: Add a methanol-acetyl chloride mixture (50:1 v/v) to convert fatty acids to fatty acid methyl esters (FAMEs). Incubate for 45 minutes at 24–29°C.
- Reaction Termination & Extraction: Stop the reaction with 6% sodium carbonate. Extract the FAMEs with hexane and transfer to a GC vial.
- GC-FID Analysis:
- Column: Use a highly polar capillary column (e.g., HP-88, 100 m × 0.25 mm, 0.2 µm film).
- Injection: 1 µL in split mode.
- Oven Program: Start at 100°C for 3 min, ramp to 175°C at 8°C/min, then to 240°C at 3°C/min, and hold for 10 min.
- Carrier Gas: Helium at 2 mL/min.
- Quantification: Quantify individual fatty acids by interpolating against calibration curves using the internal standard for normalization. Express concentrations as µg/mL of serum [11].
Protocol 2: Assessing EFAD in a Clinical Trial of a Novel ILE
This protocol is based on a recent pediatric RCT evaluating an olive oil-based ILE [10] [13].
Workflow:
- Patient Recruitment: Enroll patients expected to require PN for a sufficient duration (e.g., ≥7 days). Preterm infants are a key population due to their high susceptibility.
- Randomization & Blinding: Randomly assign patients to receive either the novel ILE or a comparator ILE (e.g., 100% soybean oil) in a double-blind manner.
- ILE Administration: Follow a standardized dosing schedule (e.g., start at 1 g/kg/day and increase to 2.5–3 g/kg/day in infants).
- Blood Sampling: Collect plasma samples at baseline and at the end of the study period.
- Primary Outcome Measurement:
- EFAD Incidence: Determine EFAD based on a plasma T:T ratio > 0.4 (or > 0.2, as defined a priori) in the context of a full fatty acid profile (low LA, low ARA, high mead acid) and/or clinical signs of deficiency [10].
- Genetic Analysis (Secondary): For patients presenting with extreme ARA values, perform genetic analysis to identify polymorphisms in the fatty acid desaturase (FADS) genes [10].
The Scientist's Toolkit: Research Reagent Solutions
The table below lists essential materials and their functions for research in this field.
| Research Reagent / Material | Function / Explanation |
|---|---|
| Gas Chromatograph with Flame Ionization Detector (GC-FID) | The core instrument for separating and quantifying individual fatty acids in plasma samples to create a detailed fatty acid profile [11]. |
| Polar Capillary GC Column (e.g., HP-88) | A long (100m), highly polar column essential for resolving the complex mixture of fatty acid methyl esters (FAMEs) based on their chain length and degree of unsaturation [11]. |
| Stable Isotope-Labeled Internal Standards (e.g., ¹³C-LA) | Used in mass spectrometry-based assays for highly precise and accurate quantification of specific fatty acids, correcting for losses during sample preparation. |
| Commercial Plasma Fatty Acid Panels | Pre-configured kits that provide standardized protocols and reagents for analyzing a defined set of fatty acids, useful for high-throughput screening. |
| Genotyping Assays for FADS SNPs | Kits or designed assays to identify common single nucleotide polymorphisms (SNPs) in the FADS1 and FADS2 genes, which are crucial for interpreting inter-individual variation in fatty acid levels [10]. |
| Olive Oil/Soybean Oil (OO/SO) & Soybean Oil (SO) ILEs | The critical intervention materials for comparative studies. The 80/20 OO/SO ILE is a key modern composite emulsion, while the 100% SO ILE serves as a historical control [10] [13]. |
The biochemical pathways of essential fatty acids are fundamental to understanding EFAD. The diagram below maps the metabolism of omega-6 and omega-3 fatty acids and the origin of mead acid, which is the key marker of deficiency.
Comparative Efficacy and Safety of Novel Lipid Emulsions in Preventing EFAD
Frequently Asked Questions (FAQs) on Clinical Outcomes
Q1: In critically ill adult patients, do olive oil-based ILEs lead to better clinical outcomes than traditional soybean oil-based ILEs?
A: In a key double-blind, randomized controlled trial involving 100 medical-surgical ICU patients, no significant differences were found in major clinical outcomes between soybean oil-based and olive oil-based ILEs. The study reported similar rates of nosocomial infections, length of hospital stay, mortality, and non-infectious complications such as acute renal failure [60] [61]. The table below summarizes the key findings.
Table 1: Comparison of Clinical Outcomes from a Major RCT (Umpierrez et al.)
| Clinical Outcome | Soybean Oil-Based ILE (n=49) | Olive Oil-Based ILE (n=51) | P-value |
|---|---|---|---|
| Nosocomial Infections | 43% | 57% | 0.16 |
| Hospital Length of Stay (days) | 47 ± 47 | 41 ± 36 | 0.49 |
| Hospital Mortality | 16.3% | 9.8% | 0.38 |
| Acute Renal Failure | 26% | 18% | 0.34 |
Q2: What about blends that include fish oil? How do they compare to olive oil-based ILEs?
A: A 2024 secondary analysis of an RCT in critically ill post-surgical adults compared an olive oil-based ILE (OO-ILE) with a mixed-lipid ILE containing soybean oil, MCT, olive oil, and fish oil (SMOF-ILE). The study found no significant differences between the two groups in clinical outcomes such as ICU length of stay, days on mechanical ventilation, or mortality. Furthermore, both emulsions were equally effective in reducing certain inflammatory cytokines (IL-1β and IL-6) over a seven-day period [62].
Q3: If clinical outcomes are often similar, what is the proposed mechanistic rationale for using alternative ILEs?
A: The primary rationale involves the modulation of inflammatory pathways. Traditional soybean oil ILEs are high in the omega-6 PUFA linoleic acid, which is a precursor to arachidonic acid (AA). AA is metabolized into potent pro-inflammatory eicosanoids (e.g., prostaglandins, leukotrienes). It is hypothesized that reducing the linoleic acid content by using olive oil-based (high in less inflammatory monounsaturated fats) or fish oil-based (rich in anti-inflammatory omega-3 PUFAs EPA and DHA) emulsions may attenuate an excessive inflammatory response, though this does not always translate to differences in gross clinical outcomes in short-term studies [61] [62] [63].
Troubleshooting Guides for Experimental Research
Problem 1: Inconsistent Results in Animal Models of EFAD
- Potential Cause: The use of an inappropriate control diet or an insufficient duration for inducing deficiency.
- Solution: Ensure the fat-free, high-carbohydrate diet is properly formulated and administered. In a murine model, severe hepatic steatosis was induced after 19 days on a defined, fat-free liquid diet [64]. Always include a positive control group fed a standard diet containing EFAs (e.g., AIN-93M with soybean oil) to confirm the model's validity.
Problem 2: Unable to Detect Meaningful Differences in Inflammatory Markers
- Potential Cause: The timing of biomarker measurement may not align with the peak of the inflammatory or resolution response.
- Solution: Implement a rigorous, serial sampling protocol. In the clinical trial by Umpierrez et al., markers were measured at baseline and then serially during PN administration. The 2024 study by Sanchez et al. measured markers at baseline and on day 7, allowing for the observation of within-group changes [60] [62].
Problem 3: Confounding Results in Lipid Mediator Profiles
- Potential Cause: The competitive dynamics between omega-3 and omega-6 PUFA pathways are not being accounted for in the analysis.
- Solution: Quantify the precursor fatty acid pools. Remember that enzymes like desaturases and elongases do not strongly discriminate between n-3 and n-6 structures; their substrate availability drives the production of downstream mediators [63]. Accurate measurement of tissue or plasma levels of linoleic acid (LA), alpha-linolenic acid (ALA), arachidonic acid (AA), EPA, and DHA is crucial for interpreting mediator profiles.
Experimental Protocols for Key Studies
Protocol 1: Randomized Controlled Trial in Critically Ill Adults
This protocol is based on the study by Umpierrez et al. [60] [61].
- Objective: To compare the effect of soybean oil-based vs. olive oil-based ILEs on nosocomial infections and metabolic parameters in ICU patients requiring PN.
- Study Design: Prospective, double-blind, randomized, controlled trial.
- Population: 100 adult medical-surgical ICU patients expected to require PN for >5 days.
- Exclusion Criteria: Septic shock, active malignancy, cirrhosis (bilirubin ≥10 mg/dL), chronic renal failure requiring dialysis, baseline triglycerides >400 mg/dL.
- Intervention:
- Group 1 (n=49): Received PN with soybean oil-based ILE (Intralipid 100% soybean oil).
- Group 2 (n=51): Received PN with olive oil-based ILE (ClinOleic ~80% olive oil, ~20% soybean oil).
- PN was administered for up to 28 days, providing total daily calories at 1.3x basal energy expenditure and 1.5 g/kg/day of protein.
- Primary Outcome: Rate of new nosocomial infections (culture-proven, using CDC criteria).
- Secondary Outcomes: Hospital and ICU length of stay, mortality, glycemic control, inflammatory/oxidative stress markers, granulocyte and monocyte functions.
- Key Methodology:
- Randomization & Blinding: A research pharmacist used a computer-generated table for treatment assignment. The emulsions were visually similar to maintain blinding.
- Glycemic Control: Bedside glucose monitoring was performed, and insulin protocols were used to maintain blood glucose targets.
- Infection Surveillance: The study team actively monitored culture data, antimicrobial use, and clinical signs daily using standardized CDC criteria.
Protocol 2: Murine Model of Essential Fatty Acid Deficiency
This protocol is adapted from the research presented in [64].
- Objective: To determine if DHA and AA alone can prevent EFAD and hepatic steatosis.
- Animal Model: 4-6 week old C57Bl/6 mice (n=5 per group).
- Diets:
- EFAD Model Groups: Fed a fat-free, high-carbohydrate liquid diet (HCD) ad libitum for 19 days.
- Control Group: Fed a standard AIN-93M diet containing soybean oil.
- Intervention via Gavage: Mice on the HCD received a daily lipid mixture providing 5% of daily calories. The composition varied by group:
- HCD-0: 100% hydrogenated coconut oil (EFA-deficient control).
- HCD-2.1: Lipid mix providing 2.1% of calories from a 20:1 ratio of DHA:AA.
- HCD-4.2: Lipid mix providing 4.2% of calories from a 20:1 ratio of DHA:AA.
- Primary Endpoints:
- Liver Histology: H&E staining of liver sections, graded for steatosis by a blinded pathologist.
- Biochemical EFAD: Assessment of serum and liver fatty acid profiles via gas chromatography to measure the triene:tetraene ratio.
- Liver Function: Serum alanine aminotransferase (ALT) levels.
Signaling Pathways & Experimental Workflows
Pathway: ILE Modulation of Inflammation
Workflow: RCT on ILEs in ICU
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Key Materials and Reagents for ILE and EFAD Research
| Item | Function / Application | Example from Literature |
|---|---|---|
| Soybean Oil-Based ILE | Control intervention; a pure soybean oil emulsion for benchmarking against newer formulations. | Intralipid [60] [61] |
| Olive Oil-Based ILE | Experimental intervention; a blend typically 80% olive oil/20% soybean oil to test the "low linoleic acid" hypothesis. | ClinOleic [60] [61] |
| Mixed-Oil ILE (SMOF) | Experimental intervention; a composite emulsion (Soybean, MCT, Olive, Fish Oil) to test synergistic effects of multiple lipid sources. | Used in Sanchez et al. [62] |
| Fat-Free High-Carbohydrate Diet | To induce Essential Fatty Acid Deficiency (EFAD) and hepatic steatosis in animal models. | Defined liquid diet [64] |
| Hydrogenated Coconut Oil (HCO) | A source of saturated fat with negligible PUFAs, used to balance calories in gavage studies without providing EFAs. | Used in mouse model gavage [64] |
| Purified DHA & AA | For targeted supplementation studies to determine if these downstream fatty acids alone can prevent or reverse EFAD. | >87% DHA (Martek), 98% AA (Cayman Chemical) [64] |
Essential Fatty Acid Metabolism and ILE Composition
Biochemical Pathways and the Holman Index
The metabolism of essential fatty acids involves two competing pathways for the omega-6 and omega-3 families. Linoleic acid (LA, 18:2n-6) and alpha-linolenic acid (ALA, 18:3n-3) are considered essential because they cannot be synthesized by humans and must be obtained from the diet. [1] These fatty acids compete for the same elongase and desaturase enzymes to produce longer-chain, more unsaturated fatty acids. [29] [1]
- LA Metabolism: LA is converted to arachidonic acid (ARA, 20:4n-6), a key component of cell membranes and a precursor for pro-inflammatory eicosanoids. [29]
- ALA Metabolism: ALA is converted to eicosapentaenoic acid (EPA, 20:5n-3) and docosahexaenoic acid (DHA, 22:6n-3), which are important for anti-inflammatory processes and neural system function. [29] [65]
- EFAD Indicator: When LA and ALA are deficient, the body uses oleic acid to produce the non-essential omega-9 fatty acid, 5,8,11-eicosatrienoic acid (Mead acid). [29] [66] The ratio of this triene (Mead acid) to tetraene (ARA) in plasma, known as the Holman index or triene:tetraene (T:T) ratio, is a key biochemical diagnostic for Essential Fatty Acid Deficiency (EFAD). A ratio >0.2 indicates biochemical EFAD, while clinical symptoms often appear at ratios >0.4. [29] [66]
Injectable Lipid Emulsion (ILE) Profiles
The fatty acid composition of an ILE is determined by its oil sources. Different ILEs provide varying amounts of LA, ALA, and their downstream metabolites, which directly influences plasma biomarker levels. [29]
Table 1: Fatty Acid Composition of Different Injectable Lipid Emulsions (%, weight/weight approximate) [29]
| Component | Intralipid (SOLE) | Omegaven (FOLE) | ClinOleic | SMOFlipid |
|---|---|---|---|---|
| Soybean Oil | 100% | 20% | 30% | |
| MCT | 50% | |||
| Olive Oil | 80% | |||
| Fish Oil | 100% | 15% | ||
| LA | 50% | 4.4% | 18.5% | 21.4% |
| ALA | 9% | 1.8% | 2% | 2.5% |
| ARA | 0% | 1-4% | 0% | 0.15-0.6% |
| EPA | 0% | 19.2% | 0% | 3% |
| DHA | 0% | 12.1% | 0% | 2% |
Abbreviations: SOLE: Soybean Oil-based Lipid Emulsion; FOLE: Fish Oil-based Lipid Emulsion; MCT: Medium-Chain Triglycerides.
Frequently Asked Questions (FAQs) for Researchers
FAQ 1: Why might a patient on a fish oil-based ILE (FOLE) not develop EFAD, despite low LA and ALA content?
Emerging evidence challenges the traditional view that only LA and ALA can reverse EFAD. Studies suggest that providing the downstream metabolites of these acids, specifically ARA and DHA, can also prevent and reverse EFAD. [29] Animal studies have shown that mice fed a diet with ARA and DHA as the sole polyunsaturated fats not only avoided EFAD but also survived and reproduced successfully for five generations. [29] Therefore, FOLEs, which are rich in pre-formed DHA and ARA, can meet essential fatty acid requirements despite their low precursor content.
FAQ 2: How reliable are plasma fatty acid levels as biomarkers of dietary intake from ILEs?
The correlation between dietary intake and plasma levels varies by fatty acid. Research shows that dietary intakes of LA, ARA, EPA, and DHA are weakly but significantly correlated with their respective percentages in plasma total fatty acids. [67] However, no significant correlation is typically observed between dietary ALA intake and its plasma levels. [67] Furthermore, plasma levels of long-chain PUFA like ARA and DHA are not strongly influenced by the intake of their 18-carbon precursors (LA and ALA, respectively), highlighting the inefficiency of this conversion in humans. [67] This supports the use of plasma LA, ARA, EPA, and DHA, but not ALA, as biomarkers for monitoring ILE intake.
FAQ 3: What are the critical pre-analytical factors that can skew plasma fatty acid biomarker data?
Sample integrity is paramount for reliable data. Key issues include:
- Temperature Regulation: Fatty acids are sensitive to degradation. Inconsistent freezing or thawing of plasma samples can alter biomarker profiles. [68]
- Sample Preparation Consistency: Variability in processing (e.g., centrifugation speed, time) can introduce bias. Standardized protocols for sample handling are essential. [69] [68]
- Contamination: Introduction of environmental lipids or cross-contamination between samples can lead to false signals. Using dedicated, clean equipment and reagents is critical. [68]
Troubleshooting Common Experimental Challenges
Challenge 1: High variability in plasma fatty acid measurements within treatment groups.
- Potential Cause: Inconsistent sample collection or storage conditions.
- Solution: Implement a strict, standardized SOP for all pre-analytical steps. This includes uniform blood draw tubes, consistent centrifugation protocols, immediate freezing of plasma at -80°C, and avoiding repeated freeze-thaw cycles. [68]
Challenge 2: Unexpectedly high plasma Mead acid levels in a group receiving an ILE with adequate LA.
- Potential Cause: Impaired metabolic conversion of LA to ARA due to genetic polymorphisms or physiological state.
- Solution: Genotype subjects for common variants in the
FADS1andFADS2gene cluster. These polymorphisms can significantly impact the efficiency of converting LA to ARA and explain up to 30% of the variability in long-chain PUFA levels among individuals. [1] Account for this in your experimental design and data analysis.
Challenge 3: Inability to detect a significant correlation between ILE ALA provision and plasma EPA/DHA.
- Expected Biological Response: This is a common finding. The conversion of ALA to EPA and DHA is inefficient in humans (typically 0-9% for DHA in men and ~9% in women). [1] The pathways are also competitively inhibited by high LA intake. [29] [1]
- Solution: This result aligns with established biology. Focus the analysis on the correlation between provided long-chain PUFAs (like DHA from FOLE) and their plasma levels, rather than on precursor-product relationships.
The Scientist's Toolkit: Key Reagents and Methods
Table 2: Essential Materials and Methods for Plasma Fatty Acid Biomarker Analysis
| Item / Reagent | Function / Application | Key Considerations |
|---|---|---|
| Gas Chromatography with Flame Ionization Detection (GC-FID) or Mass Spectrometry (GC-MS) | The gold standard for separating, identifying, and quantifying individual fatty acids in plasma samples. [70] | Provides high resolution and sensitivity for complex fatty acid profiles. |
| Boron Trifluoride (BF₃) in Methanol | A common reagent for transesterification, converting fatty acids in plasma lipids into fatty acid methyl esters (FAMEs) for GC analysis. | Requires careful handling; reagent purity is critical for accurate results. |
| Stable Isotope-Labeled Fatty Acids | Internal standards added to the sample to correct for losses during extraction and derivatization, improving quantitative accuracy. | Essential for high-precision work. |
| Solid Phase Extraction (SPE) Columns | Used to isolate specific lipid classes from plasma before analysis (e.g., separating phospholipids from triglycerides). | Allows for more specific biomarker analysis within different lipid pools. |
| Certified Reference Standards | Commercially available mixtures of known FAMEs used to calibrate the GC system and identify peaks in experimental samples. | Necessary for proper peak identification and quantification. |
Standard Operating Procedure: Plasma Fatty Acid Profiling
Objective: To extract, derive, and quantify the fatty acid composition from total plasma lipids.
- Lipid Extraction: Add a 200 µL plasma aliquot to a glass tube. Add a known amount of internal standard. Perform a Folch or Bligh & Dyer extraction using a 2:1 (v/v) chloroform:methanol mixture to isolate total lipids. [70]
- Transesterification: Evaporate the organic solvent under nitrogen. Re-dissolve the lipid extract in toluene. Add BF₃ in methanol (e.g., 14% w/w). Heat the mixture at 100°C for 45-60 minutes to form FAMEs. [71]
- FAME Extraction and Concentration: After cooling, add water and hexane to the mixture. Vortex and centrifuge to separate phases. Collect the hexane (upper) layer containing the FAMEs. Wash the hexane layer and evaporate it under a gentle stream of nitrogen. Reconstitute the FAMEs in a small volume of hexane for GC injection.
- GC Analysis: Inject the FAME sample onto a polar capillary GC column. Use a temperature gradient program to separate the FAMEs. Identify fatty acids by comparing retention times to certified reference standards. Quantify using the internal standard method. [70] [67]
- Data Analysis: Calculate the relative percentage of each fatty acid. Compute the Holman index (Mead Acid / ARA ratio) and other relevant ratios.
Experimental Workflow for ILE Impact Studies
The following diagram outlines a logical workflow for a study designed to assess the impact of different ILEs on plasma fatty acid biomarkers.
Troubleshooting Guide: Common Experimental Challenges in Fatty Acid Research
Q1: Our preclinical data suggests a potential signal of liver function alteration with a novel lipid formulation. How should we systematically assess liver safety in a clinical trial?
A: To comprehensively assess liver safety, integrate the following markers and methodologies into your trial protocol, moving beyond standard liver enzymes (ALT, AST) to capture the spectrum of steatotic liver disease [72] [73]:
- Liver Enzymes and Function Tests: Continue to monitor ALT, AST, GGT, ALB, and T.Bilirubin as foundational measures [72].
- Novel Biomarkers for MASLD: Investigate emerging biomarkers like Liver-type Fatty Acid Binding Protein (L-FABP). Serum L-FABP has shown high diagnostic accuracy (AUC of 0.885) for Metabolic dysfunction-associated steatotic liver disease (MASLD) in pediatric populations, with a cutoff value of 5.7 ng/mL providing 72.73% sensitivity and 93.62% specificity [72] [50]. It is also prognostic, with each 1-unit increase in L-FABP associated with significantly higher odds of fibrosis progression [72].
- Arachidonic Acid Metabolism (AAM) Pathway Genes: In models of NAFLD, biomarkers involved in AAM, such as PTGS1 (COX-1), show significant upregulation and are linked to disease progression. Including qRT-PCR or western blot analysis for these genes can provide mechanistic insights [74].
- Non-Invasive Fibrosis Assessment: Utilize scores like the FIB-4 index or MASLD fibrosis score, especially in adult populations, to gauge fibrosis severity without invasive biopsy [73].
Q2: Clinical trials in critical care settings have yielded conflicting results on using omega-3 levels as a prognostic marker. What could explain this, and how can we design a trial to avoid these pitfalls?
A: Conflicting results often stem from patient heterogeneity, timing of measurement, and narrow biomarker selection. A 2025 case-control study of 86 ICU patients found no significant correlation between erythrocyte membrane levels of EPA, DHA, or the combined Omega-3 index and mortality or clinical severity scores (APACHE II, SOFA) [75].
- Designing a Robust Trial:
- Broaden Biomarker Scope: Do not rely solely on the Omega-3 index. Incorporate a complete fatty acid profile, including linoleic acid, arachidonic acid, and mead acid, to calculate the triene:tetraene (T:T) ratio, a classic marker for Essential Fatty Acid Deficiency (EFAD) [13] [10].
- Account for Genetic Variability: Analyze genetic polymorphisms in fatty acid desaturase (FADS) genes, as these can significantly influence fatty acid levels and metabolic outcomes independent of intake [13] [10].
- Standardize Timing: Collect baseline blood samples immediately upon ICU admission to reflect pre-morbid nutritional status rather than disease-induced changes [75].
Q3: In a trial of a low-linoleic acid lipid emulsion, how do we definitively rule out Essential Fatty Acid Deficiency (EFAD)?
A: Recent RCTs demonstrate that EFAD risk can be managed even with reduced soybean oil content. A 2025 pediatric RCT (n=101) found that an 80% olive oil/20% soybean oil (OO/SO) ILE did not cause EFAD over a mean treatment duration of 10 days [13] [10].
- Definitive Assessment Protocol:
- Primary Marker: Measure the plasma triene:tetraene (T:T) ratio (mead acid:arachidonic acid). A value > 0.4 is indicative of EFAD [10].
- Confirm with Full Profile: Confirmatory diagnosis requires a full plasma fatty acid profile showing low linoleic acid (LA), low arachidonic acid (ARA), and high mead acid [10].
- Clinical Correlation: Monitor for clinical signs such as dermatitis, diarrhea, poor wound healing, and growth failure (in pediatrics) [10].
Table 1: Clinical Outcomes and Safety Profiles of Fatty Acid Formulations
| Intervention / Context | Infection & Immunity Findings | Liver Function & Safety Findings | Key Clinical Outcomes |
|---|---|---|---|
| Prescription Omega-3 (Cardiovascular) [76] | Not a primary focus of trials discussed. | Indicated for severe hypertriglyceridemia (TG >500 mg/dL). Purified EPA (Icosapent ethyl) is used for CV risk reduction in patients with high triglycerides on statins [76]. | REDUCE-IT (EPA): Significant CV event reduction.STRENGTH/OMEMI (EPA+DHA): No CV benefit shown [76]. |
| Olive/Soybean Oil ILE (Parenteral Nutrition) [13] [10] | Well-tolerated, supports innate immunity, associated with fewer infections. | No increased hepatobiliary disturbances vs. soybean oil ILE. No EFAD observed [10]. | Safe for use in pediatric patients, including preterm infants. Provides effective nutritional support [13] [10]. |
| Omega-3 Status (Critical Illness) [75] | No direct link found between omega-3 index and infection rates or immune scores. | Not a primary endpoint; study focused on omega-3 as a prognostic marker, not a direct hepatotoxin [75]. | No association found between erythrocyte Omega-3 index and 28-/60-day mortality or clinical severity scores (APACHE II, SOFA) [75]. |
| SARS-CoV-2 Infection [77] | Lower micronutrient status (Zn, Se, Vit D) correlated with greater disease severity (hospitalization). | Not a primary endpoint. The study focused on virus-induced alterations in host lipid metabolism [77]. | Patients showed significantly increased omega-3 (DHA, EPA) and omega-6 (AA) PUFAs vs. healthy controls [77]. |
Table 2: Diagnostic Performance of Liver Biomarkers in Metabolic Dysfunction-associated Steatotic Liver Disease (MASLD)
| Biomarker | Associated Condition | Diagnostic/Monitoring Utility | Performance Metrics |
|---|---|---|---|
| L-FABP [72] [50] | Pediatric MASLD | Diagnoses MASLD and predicts fibrosis progression. | AUC: 0.885; Sensitivity: 72.73%; Specificity: 93.62% (Cutoff: 5.7 ng/mL) [72]. |
| PTGS1 (COX-1) [74] | NAFLD (Mouse Model) | A key biomarker from the arachidonic acid metabolism pathway; expression is upregulated in NAFLD. | Identified via bioinformatics; validated by qRT-PCR and western blot in vivo [74]. |
| TyG Index [73] | Early-stage NAFLD | A accessible, non-invasive metabolic marker for early screening. | Commonly associated with early-stage NAFLD in systematic reviews [73]. |
| CK-18 [73] | NASH | A non-invasive marker for detecting steatohepatitis (NASH). | Linked to NASH detection in clinical studies [73]. |
Essential Experimental Protocols
Protocol 1: GC-MS Analysis of Erythrocyte Membrane Fatty Acids
Application: Determining Omega-3 status and essential fatty acid profiles in clinical studies [75].
Detailed Methodology:
- Blood Collection & Processing: Collect venous blood in heparinized tubes. Centrifuge at 1500–2000 × g for 10-15 minutes to separate plasma and buffy coat. Wash red blood cells (RBCs) twice with Tris-buffered saline (e.g., 20 mM Tris-HCl, 145 mM NaCl, pH 7.5) [75].
- Membrane Isolation: Lyse washed RBCs and centrifuge at high speed (e.g., 20,000 × g) to isolate the erythrocyte membrane pellet [75].
- Lipid Extraction (Folch Method): Add 3 mL of chloroform:methanol (2:1 v/v) to 300 µL of membrane suspension. Spike with an internal standard (e.g., 30 µL of heptadecanoic acid, 1 mg/mL). Vortex, add 0.6 mL of 0.9% NaCl, centrifuge, and collect the lower organic phase. Dry over anhydrous sodium sulfate [75].
- Fatty Acid Methyl Ester (FAME) Derivatization: Add 1 mL of 14% BF₃ in methanol to the dried lipid extract. Heat at 80°C for 1 hour. Cool, add 1 mL hexane and 0.5 mL HPLC-grade water, vortex, centrifuge, and collect the upper hexane layer containing FAMEs. Dry under a stream of nitrogen and reconstitute in 200 µL hexane for injection [75].
- GC-MS Analysis:
- Column: SP-2560 fused silica capillary column.
- Carrier Gas: Helium at 1 mL/min.
- Injector Temp: 280°C.
- Oven Program: Initial 130°C, ramp at 4°C/min to 245°C, hold for 3 min.
- Detection: Mass spectrometry in total ion monitoring mode [75].
Protocol 2: Evaluating L-FABP as a Serum Biomarker for MASLD
Application: Non-invasive diagnosis and staging of Metabolic Dysfunction-associated Steatotic Liver Disease [72] [50].
Detailed Methodology:
- Patient Stratification: Recruit patients and controls, confirmed via abdominal ultrasound. Exclude other liver diseases (e.g., HCV, HBV, cirrhosis) [72] [50].
- Blood Sample Processing: Collect fasting blood samples in yellow gel (clot activator) tubes. Centrifuge at 1500 RPM for 10 minutes at 20°C to separate serum [72].
- L-FABP ELISA: Analyze serum L-FABP levels using a commercial ELISA kit (e.g., Cat. No E2159Hu) per manufacturer's instructions [72].
- Data Analysis:
- Perform logistic regression to assess the association between L-FABP levels and MASLD odds.
- Construct a Receiver Operating Characteristic (ROC) curve to determine diagnostic accuracy (AUC, optimal cutoff, sensitivity, specificity) [72].
- Analyze the relationship between L-FABP levels and fibrosis stage (e.g., F2 to F3 progression) to evaluate prognostic utility [72].
Visualizing Mechanisms and Workflows
Fatty Acid Immunomodulation Pathways
Essential Fatty Acid Deficiency Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for Fatty Acid Deficiency and Liver Safety Research
| Research Reagent / Material | Primary Function in Research | Example Application Context |
|---|---|---|
| Commercial L-FABP ELISA Kit | Quantifies serum L-FABP concentration for non-invasive diagnosis and prognosis of MASLD. | Diagnosing and staging MASLD in pediatric or adult cohorts [72] [50]. |
| SP-2560 GC Capillary Column | High-resolution separation of fatty acid methyl esters (FAMEs) for precise quantification. | Profiling erythrocyte membrane fatty acids to determine Omega-3 index or EFAD status [75]. |
| BF₃-Methanol Reagent | Catalyzes the derivatization of fatty acids to their volatile methyl esters (FAMEs) for GC analysis. | Sample preparation for GC-MS-based fatty acid profiling [75]. |
| Specific ILE Formulations (e.g., 80% OO/20% SO) | Investigational product for assessing safety and efficacy of reduced-soybean oil lipid emulsions. | Clinical trials evaluating PN strategies and EFAD risk in pediatric/preterm populations [13] [10]. |
| Polyclonal/Monoclonal Antibodies for PTGS1, GPX2 | Detects expression of key AAM pathway proteins via western blot or IHC. | Validating the role of arachidonic acid metabolism in NAFLD/NASH models [74]. |
FAQs on Novel Lipid Emulsions and EFAD Prevention
Q1: What are the main types of novel lipid emulsions being developed to prevent Essential Fatty Acid Deficiency (EFAD)?
The field has moved beyond first-generation, pure soybean-oil emulsions. The main novel types include [78] [79]:
- Fish oil-based emulsions (FOLE): Rich in omega-3 fatty acids (EPA and DHA), known for anti-inflammatory properties and potential to treat PN-associated liver disease (PNALD).
- Mixed-oil emulsions (e.g., SMOFlipid): Composite formulations that combine various oil sources, such as soybean oil, medium-chain triglycerides (MCT), olive oil, and fish oil, to balance the fatty acid profile.
- Olive oil-based emulsions: High in monounsaturated fats, which support immune function and are less prone to oxidation.
- Medium-chain triglyceride (MCT) emulsions: Often used in blends, MCTs are rapidly metabolized for energy and can help manage malabsorption syndromes.
Q2: Can fish oil alone prevent EFAD, given its low linoleic acid content?
Yes, emerging evidence suggests it can. While fish oil is low in linoleic acid (an omega-6 EFA), it contains pre-formed longer-chain fatty acids like arachidonic acid (AA). A preclinical study established that fish oil as the sole lipid source can prevent EFAD, with a total omega-6 fatty acid requirement of only 0.30–0.56% of dietary energy—approximately half of the conventionally recommended 1% from linoleic acid [80]. This is attributed to the presence of AA, which is more efficient at meeting omega-6 requirements [80].
Q3: What are the key clinical advantages of mixed-oil lipid emulsions over traditional formulations?
Mixed-oil emulsions, such as SMOFlipid, are designed to offer a balanced fatty acid profile. Their advantages include [78] [81] [79]:
- Reduced Inflammation: A lower omega-6 to omega-3 ratio helps modulate inflammatory responses.
- Improved Liver Outcomes: Associated with a lower risk of PN-associated liver disease (PNALD) compared to pure soybean-oil emulsions.
- Potential Infection Rate Reduction: Some clinical data links mixed-oil emulsions to reduced rates of catheter-related bloodstream infections, potentially due to the inhibition of microbial biofilm formation.
Q4: What role do phytosterols play in lipid emulsion safety?
Phytosterols, plant-derived sterols abundant in soybean and other vegetable oil-based emulsions, are increasingly implicated in the development of Intestinal Failure-Associated Liver Disease (IFALD). Their accumulation is associated with cholestasis and liver injury. Strategies to mitigate this include using fish-oil emulsions (which are naturally low in phytosterols) or developing novel emulsions where phytosterols have been depleted [82].
Q5: How is artificial intelligence (AI) impacting the development of future TPN formulations?
AI and machine learning are poised to revolutionize TPN personalization. These technologies can analyze real-time patient data to [78]:
- Optimize Nutrient Formulations: Create individualized TPN recipes that match expert-level prescriptions.
- Predict Stability Issues: Forecast potential incompatibilities or instability in complex admixtures.
- Streamline Adjustments: Enable dynamic, data-driven adjustments to TPN based on a patient's evolving metabolic status.
Troubleshooting Common Experimental Challenges
Problem: Interpreting conflicting results on fungal infection outcomes with different lipid emulsions.
Solution: Consider the emulsion's impact on microbial biofilm formation. In vitro studies show that mixed-oil emulsions can inhibit Candida albicans biofilm formation by approximately 50%, while soybean-oil and fish-oil emulsions may stimulate it [81]. When designing animal models or interpreting in vivo data, factor in this direct microbiological effect, which can confound purely immune-mediated outcomes. Ensure your experimental model controls for catheter-related infection variables.
Problem: Determining the minimum effective dose of a novel fish-oil emulsion to prevent EFAD in a murine model.
Solution: Refer to established dietary energy requirements. The mouse study by [80] provides a benchmark. Diets with 1% fish oil by weight resulted in clear EFAD, 5% was marginal, and 10% effectively prevented EFAD. This corresponded to a total omega-6 fatty acid requirement of between 0.30% and 0.56% of dietary energy. Use these values as a starting point for dose-finding studies with your specific formulation.
Problem: Differentiating the hepatotoxic effects of phytosterols from those of pro-inflammatory omega-6 fatty acids.
Solution: Implement a factorial study design that isolates these variables. A recent investigation using a phytosterol-depleted soybean oil (L-SOLE) in a mouse model of IFALD demonstrated that reducing phytosterols alone led to lesser biochemical and histological liver injury, independent of the oil's fatty acid profile [82]. To confirm the primary culprit in your experiments, compare:
- Standard soybean-oil emulsion (high phytosterols, high omega-6).
- Phytosterol-depleted soybean-oil emulsion (low phytosterols, high omega-6).
- Fish-oil emulsion (low phytosterols, low omega-6).
Quantitative Data on Lipid Emulsions
Table 1: Comparison of Key Lipid Emulsion Types and Their Properties
| Emulsion Type | Composition | Key Fatty Acid Features | Clinical Implications & Evidence |
|---|---|---|---|
| Soybean Oil (SOLE) | 100% Soybean Oil | High in pro-inflammatory omega-6 PUFAs (Linoleic Acid). High phytosterols. | Traditional standard. Associated with increased risk of PNALD and inflammation [79] [82]. |
| Fish Oil (FOLE) | 100% Fish Oil | Rich in anti-inflammatory omega-3 PUFAs (EPA, DHA). Very low phytosterols. | Prevents/treats PNALD. Prevents EFAD despite low Linoleic acid, likely due to Arachidonic acid content [80] [82]. |
| Mixed-Oil (SMOF) | Blend of Soy, MCT, Olive, and Fish Oils | Balanced omega-6/omega-3 ratio. Moderate phytosterol content. | Reduces inflammation; associated with lower catheter infection rates; considered a modern standard of care [78] [81]. |
| Olive Oil-based | High in Olive Oil | Rich in monounsaturated fats (Oleic acid). Lower in PUFA than SOLE. | Supports immune function, generates less oxidative stress [79]. |
Table 2: Experimental Data on EFAD Prevention with Fish Oil
| Parameter | 1% Fish Oil Diet | 5% Fish Oil Diet | 10% Fish Oil Diet | Control (Soybean Diet) |
|---|---|---|---|---|
| EFAD Status | Clear Deficiency | Marginal | Prevented | Prevented |
| Weight Gain | Impaired (in pair-fed group) | Highest caloric efficiency | Normal | Normal |
| Total Omega-6 Requirement (as % of dietary energy) | Below requirement | ~0.30% - 0.56% | Above requirement | Met via Linoleic Acid |
| Conclusion | Induces EFAD | Near the minimum requirement | Effective at preventing EFAD | Effective at preventing EFAD |
Data adapted from [80].
Detailed Experimental Protocol: Establishing Minimum Fat Requirements
This protocol is adapted from the classic study by Barr et al. (1981) and modernized with insights from recent research [21] [80].
Objective: To determine the minimum dose and type of intravenous lipid emulsion required to prevent Essential Fatty Acid Deficiency (EFAD) in a preclinical TPN model.
Materials:
- Animal Model: Rodents (e.g., mice or rats) or larger animals (e.g., piglets for greater translational relevance).
- Lipid Emulsions: Test emulsions (e.g., novel fish-oil, mixed-oil) and control emulsions (soybean-oil, phytosterol-depleted).
- TPN Solutions: Fat-free base TPN solutions.
- Analytical Equipment: GC-FID or GC-MS for fatty acid profiling [11].
Methodology:
- Study Groups: Randomize animals into several groups:
- Group 1: Fat-free TPN (negative control).
- Group 2: TPN + Soybean-oil emulsion at a standard dose (e.g., providing >3.2% of total calories as fat - positive control) [21].
- Group 3-N: TPN + Novel lipid emulsion at varying doses (e.g., low, medium, high).
- Administration: Administer TPN continuously via central venous catheter for a minimum of 14 days [21].
- Monitoring: Track weight, caloric intake, and clinical signs.
- Sample Collection: Collect plasma/serum at baseline, weekly, and at endpoint.
- Endpoint Analysis:
- Biochemical EFAD: Analyze plasma phospholipids or non-esterified fatty acids (NEFA) via GC-FID. Calculate the triene-tetraene ratio (Mead acid/AA). A ratio >0.2 is considered abnormal, and >0.4 is diagnostic for EFAD [80] [11].
- Clinical Outcomes: Assess growth, skin integrity, and liver function.
- Liver Histology: Examine for steatosis, inflammation, and cholestasis.
Workflow Diagram: This diagram outlines the key decision points in the experimental protocol for evaluating a novel lipid emulsion.
Metabolic Pathways in EFAD and Emulsion Action
This diagram illustrates the biochemical pathways of essential fatty acids and how deficiency alters metabolism, providing a framework for understanding how novel emulsions intervene.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for Lipid Emulsion and EFAD Research
| Reagent / Material | Function / Application in Research | Example / Notes |
|---|---|---|
| Soybean Oil Emulsion (SOLE) | Traditional control; induces a pro-inflammatory and high-phytosterol baseline for comparison. | Intralipid [81] [82]. |
| Fish Oil Emulsion (FOLE) | Investigate omega-3 monotherapy for liver disease and test EFAD prevention via non-linoleic acid pathways. | Omegaven [78] [82]. |
| Mixed-Oil Emulsion | Benchmark against modern clinical standards; study balanced fatty acid profiles. | SMOFlipid [78] [81]. |
| Gas Chromatography with Flame Ionization Detection (GC-FID) | The gold standard for precise quantification of fatty acid methyl esters (FAMEs) in plasma, serum, or tissues [80] [11]. | Critical for calculating triene-tetraene ratios. |
| Internal Standard (for GC) | Ensures accurate quantification of fatty acids during sample preparation and analysis. | Tridecanoic acid (C13:0) [11]. |
| Phytosterol-Depleted Emulsions | Isolate the hepatotoxic effects of phytosterols from those of fatty acids in IFALD models [82]. | Experimental reagent (e.g., L-SOLE). |
| Animal TPN Model | Preclinical in vivo system to study the safety, efficacy, and metabolic effects of novel formulations over time. | Mouse, rat, or neonatal piglet models [80] [82]. |
Frequently Asked Questions (FAQs): Core Conceptual Gaps
FAQ 1.1: What is the primary challenge in diagnosing Essential Fatty Acid Deficiency (EFAD) in patients receiving modern lipid injectable emulsions (ILEs)? The primary challenge is the reliance on the traditional Holman index (triene:tetraene or T:T ratio) as a sole diagnostic marker. With the use of newer ILEs that have variable oil and fatty acid content, alterations in patient fatty acid profiles reflect the ILE composition itself, making identification of a true deficiency more complex. The T:T ratio alone is now considered insufficient for an accurate diagnosis, necessitating a more comprehensive analysis of fatty acid panels. [2]
FAQ 1.2: For a child with Intestinal Failure-Associated Liver Disease (IFALD) on long-term parenteral nutrition, what is the evidence gap regarding the use of 100% fish-oil ILE? While 100% fish-oil ILE (at 1 g/kg/day) is effective for reversing cholestasis, a key evidence gap exists concerning its long-term adequacy in supplying sufficient essential fatty acids (linoleic acid [LA] and alpha-linolenic acid [ALA]) for neurodevelopment. Although one study found a low risk of biochemical EFAD, it also noted marked decreases in ARA, LA, and ALA levels, requiring long-term neurodevelopmental outcome studies to confirm sufficiency. [83]
FAQ 1.3: How does environmental enteric dysfunction (EED) complicate EFAD research in low- and middle-income countries (LMICs)? In EED, EFAD is not solely due to inadequate dietary intake. The condition is characterized by intestinal inflammation and malabsorption, which disrupts the uptake of lipids and other nutrients. This means that even with dietary interventions, absorption may be compromised. Research must therefore focus on both correcting EFAD and improving gut health to facilitate childhood growth in these high-risk settings. [11]
FAQ 1.4: What is a critical methodological consideration for personalizing omega-3 supplementation in clinical research? Blood concentrations of EPA and DHA (e.g., the Omega-3 Index) are superior predictors of health outcomes compared to dietary intake data alone. Interindividual variability in bioavailability, metabolism, and genetic factors (like FADS gene polymorphisms) can cause up to a 13-fold difference in omega-3 uptake. Future research must incorporate blood-level monitoring to develop truly personalized dosing strategies. [84]
FAQ 1.5: Why is the ratio of omega-6 to omega-3 PUFAs a target for intervention in conditions like anorexia nervosa (AN)? A dysregulated n-6:n-3 ratio leads to an imbalance in the synthesis of eicosanoids, which are potent bioactive lipid mediators. A high ratio favoring n-6 PUFAs can promote a pro-inflammatory state. In AN, a differential postprandial shift in n-6 derived eicosanoids has been observed, which may underlie profound food aversion. Personalized PUFA formulations that correct this ratio are a novel potential therapeutic target. [85]
Troubleshooting Common Experimental Challenges
Challenge: Inconsistent Neurodevelopmental Outcomes in Postnatal Supplementation Trials
Problem: Studies investigating the impact of postnatal lipid supplementation on neurodevelopment in children, particularly in LMICs, show mixed and complex results. [86]
Solution Strategy:
- Root Cause: Variability is often attributed to differences in the choice of fatty acids, dosage, treatment windows, and the type and age of neurodevelopmental assessments.
- Actionable Steps:
- Standardize Assessments: Utilize a core, validated set of neuropsychological tools that capture specific domains such as auditory-phonological, visual-perceptual, and visual-attentional processing, which have been shown to mediate the effects of PUFAs on literacy. [87]
- Define Intervention Window: Differentiate studies based on clear developmental windows (e.g., first 2 years of life vs. school-age) and ensure the supplementation period is aligned with the targeted neurodevelopmental process.
- Control for Baseline Status: Measure and account for children's baseline essential fatty acid status, as deficiencies may influence the magnitude of response to supplementation. [86] [11]
Challenge: Interpreting Biochemical Markers of EFAD with Modern ILEs
Problem: The traditional triene:tetraene (T:T) ratio may not accurately reflect essential fatty acid status in patients receiving modern composite lipid emulsions, leading to potential misdiagnosis. [2]
Solution Strategy:
- Root Cause: The fatty acid composition of newer ILEs (e.g., those containing fish oil, olive oil) directly influences the patient's plasma fatty acid profile, which can confound the T:T ratio.
- Actionable Steps:
- Comprehensive Profiling: Move beyond the T:T ratio and implement full fatty acid panels that measure absolute and relative levels of LA, ALA, ARA, EPA, DHA, and Mead acid.
- Establish New Baselines: Develop product-specific reference ranges for fatty acid parameters in target populations (e.g., preterm infants, adults with intestinal failure) receiving these modern ILEs.
- Correlate with Clinical Signs: Always correlate biochemical data with clinical examination for signs of EFAD, such as dry, scaly dermatitis or impaired growth. [2]
Detailed Experimental Protocols
Protocol: Assessing Fatty Acid Status and EFAD Risk in a Pediatric PN Cohort
Aim: To longitudinally evaluate the risk of biochemical and clinical EFAD in children requiring long-term parenteral nutrition with a modern ILE.
Background: This protocol is adapted from a longitudinal study of children with IFALD treated with 100% fish-oil ILE, which monitored fatty acid levels for up to four years. [83]
Materials:
- Research Reagent Solutions:
- Serum/Plasma Collection Tubes: For fatty acid profiling.
- Internal Standard: Tridecanoic acid (C13:0) for gas chromatography.
- Derivatization Reagents: Methanol-acetyl chloride mixture for fatty acid methylation.
- GC-FID System: Equipped with a highly polar capillary column (e.g., HP-88, 100 m × 0.25 mm). [11]
- Anthropometric Tools: Standardized equipment for measuring weight, height/length, and head circumference.
Methodology:
- Patient Enrollment: Enroll patients receiving a defined regimen of the ILE under investigation (e.g., 1 g/kg/day).
- Baseline Sampling: Collect baseline blood samples and anthropometric measurements.
- Longitudinal Monitoring: Schedule follow-up blood draws at regular intervals (e.g., weeks 4, 8, 16, and every 3-6 months thereafter).
- Sample Processing: a. Extract serum/plasma from blood samples. b. Add internal standard (C13:0) to a defined volume of serum. c. Derivatize fatty acids to methyl esters (FAMEs) using methanol-acetyl chloride. d. Extract FAMEs with hexane for analysis. [11]
- GC-FID Analysis: Separate and quantify individual FAMES using a temperature-gradient method. Identify fatty acids by comparing retention times to certified standards.
- Data Analysis: a. Calculate the T:T ratio (Mead acid:ARA). b. Track absolute and relative concentrations of LA, ALA, ARA, EPA, and DHA. c. Correlate biochemical data with growth Z-scores (WAZ, HAZ, WHZ) and clinical status.
Protocol: Evaluating the Impact of PUFA Supplementation on Neurocognitive Mediators
Aim: To determine which neurocognitive systems (e.g., auditory-phonological, visual-attentional) mediate the effect of omega-3 LCPUFA levels on literacy skills in children.
Background: This protocol is based on a study that used mediation analysis to link fatty acid levels with neuropsychological factors in children with dyslexia. [87]
Materials:
- Research Reagent Solutions:
- Blood Collection Kits: For plasma and red blood cell (RBC) fatty acid analysis.
- Standardized Neuropsychological Test Batteries: Assessing:
- Literacy: Reading (speed, accuracy) and writing skills.
- Auditory Processing: Phonological awareness tasks.
- Visual Processing: Visual perceptual and magnocellular function tests.
- Attention: Continuous performance tests and executive function tasks.
- GC-MS or GC-FID Systems: For high-sensitivity fatty acid profiling.
Methodology:
- Cohort Recruitment: Recruit a target population of children with a range of abilities (e.g., typical development and diagnosed with developmental dyslexia).
- Blood Sampling and Analysis: Collect blood samples to determine RBC membrane levels of EPA, DHA, ARA, and other relevant PUFAs.
- Neuropsychological Assessment: Administer a comprehensive battery of tests in a controlled environment to extract key cognitive factors.
- Statistical Mediation Analysis: a. Perform factor analysis (e.g., Principal Component Analysis) on neuropsychological test scores to derive core latent factors (e.g., Auditory Phonological, Visual-Attentional). b. Use Generalized Linear Model mediation analyses to test whether the neurocognitive factors significantly mediate the relationship between PUFA levels (independent variable) and literacy performance (dependent variable). [87]
Data Presentation
Table 1: Evidence Gaps in Long-Term Outcomes of Specific Lipid Emulsions
| Population | Intervention | Key Evidence Gap | Recommended Future Research |
|---|---|---|---|
| Children with IFALD [83] | Long-term 100% fish-oil ILE (1 g/kg/day) | Long-term neurodevelopmental adequacy due to decreased ARA, LA, and ALA levels. | Prospective cohort studies tracking neurodevelopmental scores (e.g., Bayley Scales) alongside fatty acid profiles for 3+ years. |
| Adult HPN Patients [42] | Omega-3 PUFA-enriched MCT/LCT ILE vs. standard MCT/LCT ILE | Long-term liver safety and efficacy beyond 8-12 weeks. | Multicenter RCTs with treatment durations of 6-12 months, focusing on IFALD incidence and PN dependency. |
| Undernourished Children with EED [11] | Nutritional Supplementation | Efficacy of interventions correcting EFAD in the context of malabsorption. | RCTs of lipid-based nutrient supplements coupled with biomarkers of gut integrity and inflammation. |
Table 2: Targets for Personalized Dosing Strategies
| Factor Influencing Personalization | Current Challenge | Research Target |
|---|---|---|
| Genetic Variation (FADS1/FADS2) [84] | Differential capacity to synthesize LC-PUFAs from precursors (ALA, LA). | Genotype-based dosing trials to determine if FADS minor allele carriers require pre-formed EPA/DHA and ARA. |
| Disease-Related Malabsorption (EED, IF) [11] | Standard oral/enteral dosing may be ineffective due to mucosal damage. | Develop and test absorbable lipid formulations (e.g., structured lipids, phospholipid-bound DHA) in target populations. |
| Baseline Omega-3 Status [84] | Wide interindividual variability in blood response to supplementation (up to 13-fold). | Use the Omega-3 Index as a baseline biomarker to titrate dose in intervention studies, aiming for a target level (e.g., >8%). |
| Underlying Psychiatric Pathology (AN) [85] | Altered postprandial PUFA metabolism may contribute to food aversion. | Test if personalized n-6:n-3 PUFA formulations can normalize eicosanoid shifts and improve food tolerance. |
Visual Workflows
EFAD Research Pathway
PUFA Neurodevelopment Mediation
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research |
|---|---|
| HP-88 GC Column | A 100-meter, highly polar capillary column for optimal separation of complex fatty acid methyl ester (FAME) mixtures, crucial for accurate identification and quantification. [11] |
| Tridecanoic Acid (C13:0) | An internal standard used in gas chromatography. It is added in a known quantity to serum samples before processing to correct for losses during extraction and derivatization, ensuring quantitative accuracy. [11] |
| Standardized Neuropsychological Batteries | Validated sets of cognitive tests (e.g., for literacy, attention, executive function) used to generate reliable and comparable outcome measures across different studies and populations. [87] |
| Omega-3 Index | A standardized blood test that measures the percentage of EPA and DHA in red blood cell membranes. It serves as a reliable, long-term biomarker of omega-3 status for baseline stratification and outcome measurement. [84] |
| Structured Lipid Emulsions | Investigational ILEs containing specifically designed triglycerides (e.g., medium-chain and long-chain fatty acids on the same glycerol backbone) to enhance absorption in patients with fat malabsorption. [2] |
Conclusion
The prevention of Essential Fatty Acid Deficiency is entering a new paradigm, moving beyond simple linoleic acid supplementation and the traditional Holman Index. Successful strategies now require a nuanced understanding of how modern, composite lipid emulsions influence fatty acid biochemistry and diagnostic parameters. Future efforts must focus on developing refined, personalized prevention protocols that integrate comprehensive fatty acid profiling and genetic data. For researchers and drug developers, significant opportunities lie in creating next-generation ILEs that optimize essential fatty acid delivery while minimizing pro-inflammatory and hepatotoxic effects, ultimately improving outcomes for the most vulnerable patients.
References
- 1. Essential Fatty Acids | Linus Pauling Institute [https://lpi.oregonstate.edu/mic/other-nutrients/essential-fatty-acids]
- 2. Essential fatty acid deficiency in parenteral nutrition [https://pmc.ncbi.nlm.nih.gov/articles/PMC11879921/]
- 3. Essential Fatty Acid Deficiency - Nutritional Disorders [https://www.merckmanuals.com/professional/nutritional-disorders/undernutrition/essential-fatty-acid-deficiency]
- 4. Metabolism of alpha-linolenic acid in humans [https://pubmed.ncbi.nlm.nih.gov/16828546/]
- 5. Linoleic Acid - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3650500/]
- 6. The Role of Linoleic Acid in Health and Inflammation [https://mitohealth.com/biomarkers/linoleic-acid]
- 7. Alpha-Linolenic Acid (Ala) - Uses, Side Effects, and More [https://www.webmd.com/vitamins/ai/ingredientmono-1035/alpha-linolenic-acid]
- 8. Linoleic Acid - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/linoleic-acid]
- 9. 6.12: Fatty Acid Synthesis [https://bio.libretexts.org/Bookshelves/Biochemistry/Book%3A_Biochemistry_Free_and_Easy_(Ahern_and_Rajagopal)/06%3A_Metabolism_I_-_Oxidative_Reductive_Processes/6.12%3A_Fatty_Acid_Synthesis]
- 10. Essential fatty acid deficiency, olive oil‐based intravenous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314573/]
- 11. Essential Fatty Acid Deficiency Associates with Growth ... [https://www.mdpi.com/2218-1989/13/4/489]
- 12. Enteral Infant Formulas: A Narrative Review of Historical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094131/]
- 13. Essential fatty acid deficiency, olive oil-based intravenous ... [https://pubmed.ncbi.nlm.nih.gov/40415417/]
- 14. Essential Fatty Acid Deficiency in an Extremely Premature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10191592/]
- 15. High dose arachidonic and docosahexaenoic acid in very ... [https://www.sciencedirect.com/science/article/pii/S0261561425001475]
- 16. Fatty liver in pregnancy may increase risk of preterm birth [https://news.ki.se/fatty-liver-in-pregnancy-may-increase-risk-of-preterm-birth]
- 17. Effect of enteral supplementation of DHA with or without ... [https://pubmed.ncbi.nlm.nih.gov/40233974/]
- 18. Linoleic Acid: A Narrative Review of the Effects ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10386285/]
- 19. Trends in linoleic acid intake in the United States adult ... [https://www.sciencedirect.com/science/article/abs/pii/S0952327818301108]
- 20. Current Insights into the Effects of Dietary α-Linolenic Acid ... [https://www.mdpi.com/1422-0067/25/9/4909]
- 21. Essential fatty acid deficiency during total parenteral nutrition [https://pubmed.ncbi.nlm.nih.gov/6782957/]
- 22. Associations of dietary linoleic acid and alpha linolenic ... [https://www.frontiersin.org/journals/clinical-diabetes-and-healthcare/articles/10.3389/fcdhc.2024.1318578/full]
- 23. Clinolipid (Lipid Injectable Emulsion) for Intravenous Use [https://ushospitalproducts.baxter.com/clinolipid-20-lipid-injectable-emulsion-usp-0]
- 24. Total Parenteral Nutrition, Multifarious Errors | PSNet - AHRQ [https://psnet.ahrq.gov/web-mm/total-parenteral-nutrition-multifarious-errors]
- 25. Detection and reduction of errors in parenteral nutrition ... [https://www.sciencedirect.com/science/article/pii/S1130634323009339]
- 26. Troubleshooting for Enteral Nutrition [https://peas.albertahealthservices.ca/GuidelineViewer/Index/10316]
- 27. Improving the usability of lipid emulsions and optimizing ... [https://www.e-acnm.org/journal/view.php?doi=10.15747/ACNM.25.0015]
- 28. Essential Fatty Acid Requirements and Intravenous Lipid Emulsions - PubMed [https://pubmed.ncbi.nlm.nih.gov/30908685/]
- 29. Redefining essential fatty acids in the era of novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5840041/]
- 30. Essential fatty acid deficiency in adults receiving total ... [https://www.sciencedirect.com/science/article/pii/S0002916523341066]
- 31. Fatty Acid Desaturase 1 (FADS1) Gene Polymorphisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4280302/]
- 32. Genetic Variants in the FADS Gene: Implications for Dietary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4070521/]
- 33. Fatty acid desaturase genetic variations in heart failure and ... [https://www.sciencedirect.com/science/article/pii/S2666602225000321]
- 34. The influence of FADS1 and ELOVL2 genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11924656/]
- 35. FADS genetic and metabolomic analyses identify the ∆5 ... [https://www.nature.com/articles/s41598-020-71948-1]
- 36. FADS1-FADS2 genetic polymorphisms are associated with ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-018-0545-5]
- 37. FADS Gene Polymorphisms, Fatty Acid Desaturase ... [https://www.mdpi.com/1660-4601/14/6/572]
- 38. FADS1 and FADS2 Gene Polymorphisms Affect Omega-3 ... [https://www.mdpi.com/2218-1989/15/12/758]
- 39. The association of fatty acid desaturase gene ... [https://www.sciencedirect.com/science/article/pii/S0002916522030118]
- 40. The Slow Discovery of the Importance of ω3 Essential Fatty ... [https://www.sciencedirect.com/science/article/pii/S0022316623017467]
- 41. Erythrocyte fatty acid membrane composition in children on ... [https://www.sciencedirect.com/science/article/pii/S0002916522001514]
- 42. Safe and well-tolerated long-term parenteral nutrition ... [https://www.sciencedirect.com/science/article/abs/pii/S0261561424004047]
- 43. Serum linoleic acid status as a clinical indicator of essential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4482449/]
- 44. Lipid Emulsions In Parenteral Nutrition: Does it Matter? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150783/]
- 45. Parenteral nutritional support in surgical patients: expert ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1546089/full]
- 46. Essential Fatty Acid Deficiency [https://practicalgastro.com/2017/06/01/essential-fatty-acid-deficiency/]
- 47. The role of lipid emulsions containing omega-3 fatty acids for ... [https://ccforum.biomedcentral.com/articles/10.1186/s13054-024-05053-4]
- 48. Fatty acid profiles in blood and tissues of parenteral nutrition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581466/]
- 49. The blood lipidome fatty acid profile predicts the disease ... [https://www.nature.com/articles/s41398-025-03526-w]
- 50. Evaluating liver type fatty acid binding protein as a diagnostic ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0333581]
- 51. Multi-omics integration reveals gut Microbiome and Short- ... [https://pubmed.ncbi.nlm.nih.gov/41085833/]
- 52. FDA Adverse Event Reporting System (FAERS) Essentials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12393772/]
- 53. FDA's Adverse Event Reporting System (FAERS) [https://www.fda.gov/drugs/surveillance/fdas-adverse-event-reporting-system-faers]
- 54. Omega-3 Fatty Acids - LiverTox - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK548910/]
- 55. Omega-3 intake is associated with liver disease protection [https://pmc.ncbi.nlm.nih.gov/articles/PMC10394692/]
- 56. Omega-3 Fatty Acid Supplementation Prevents Hepatic ... [https://www.nature.com/articles/pr200572]
- 57. Anti- inflammatory effects of short chain fatty in... acids [https://pubmed.ncbi.nlm.nih.gov/17161819/]
- 58. Essential fatty acid deficiency, olive oil-based intravenous ... [https://scholars.uthscsa.edu/en/publications/essential-fatty-acid-deficiency-olive-oil-based-intravenous-lipid]
- 59. Composite lipid emulsion use and essential fatty acid ... [https://pubmed.ncbi.nlm.nih.gov/37392380/]
- 60. A double-blind, randomized clinical trial comparing soybean ... [https://pubmed.ncbi.nlm.nih.gov/22488002/]
- 61. A double-blind, randomized clinical trial comparing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3738173/]
- 62. Comparison of n-3 PUFA-Enriched vs. Olive-Oil-Based ... [https://www.mdpi.com/1422-0067/25/21/11739]
- 63. Consequences of Essential Fatty Acids [https://www.mdpi.com/2072-6643/4/9/1338]
- 64. DOCOSAHEXAENOIC ACID AND ARACHIDONIC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3380148/]
- 65. Fatty Acids: Essential Nutrients and Important Biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496588/]
- 66. 5,8,11 Icosatrienoic Acid - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/5-8-11-icosatrienoic-acid]
- 67. n-6 and n-3 polyunsaturated Plasma as fatty of... acids biomarkers [https://www.nature.com/articles/1602836?error=cookies_not_supported]
- 68. Common Lab Issues That Impact Biomarker Data [https://blog.omni-inc.com/blog/common-lab-issues-that-impact-biomarker-data]
- 69. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 70. Biomarkers of Fat and Fatty Acid Intake [https://www.sciencedirect.com/science/article/pii/S002231662215707X]
- 71. (PDF) Plasma : fatty of dietary intake? acids Biomarkers [https://www.academia.edu/117600997/Plasma_fatty_acids_Biomarkers_of_dietary_intake]
- 72. Evaluating liver type fatty acid binding protein as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483236/]
- 73. alcoholic fatty liver disease: evidence integration of ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1652996/full]
- 74. Identification and verification of biomarkers associated with ... [https://www.nature.com/articles/s41598-025-92972-z]
- 75. A case-control study on the diagnostic role of Omega-3 ... [https://www.nature.com/articles/s41598-025-09391-3]
- 76. NLA 2025: Exploring the Evidence Behind Omega-3 Fatty ... [https://www.pharmacytimes.com/view/nla-2025-exploring-the-evidence-behind-omega-3-fatty-acids-for-cardiovascular-risk]
- 77. Micronutrient status and fatty acid profile of adults with ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1608300/full]
- 78. The Future of TPN: Advances in Parenteral Nutrition Therapy [https://www.pharmko.com/blog/the-future-of-tpn-advances-in-parenteral-nutrition-therapy]
- 79. How to Optimize Fat Emulsions in TPN for Better Patient ... [https://www.pharmko.com/blog/how-to-optimize-fat-emulsions-in-tpn-for-better-patient-outcomes]
- 80. FISH OIL PREVENTS ESSENTIAL FATTY ACID ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3364597/]
- 81. Assessment of the association between mixed-oil lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303084/]
- 82. Depletion of phytosterols from intravenous lipid emulsions [https://www.nature.com/articles/s41390-025-03877-6]
- 83. Essential fatty acid deficiency in children treated with long ... [https://pubmed.ncbi.nlm.nih.gov/40538156/]
- 84. Omega-3 fatty acids and fetal brain development [https://www.explorationpub.com/Journals/ent/Article/1004107]
- 85. Personalized polyunsaturated fatty acids as a potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5792652/]
- 86. The importance of lipids for neurodevelopment in low and ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1488647/full]
- 87. SFI Health™ Reports Promising Results From a ... [https://www.businesswire.com/news/home/20251126097656/en/SFI-Health-Reports-Promising-Results-From-a-Preliminary-Study-Evaluating-the-Impact-of-Long-Chain-Polyunsaturated-Fatty-Acids-on-Reading-and-Writing-Skills-in-Children]