Biosensors vs. Conventional Methods: A Performance Evaluation for Next-Generation Allergen Detection
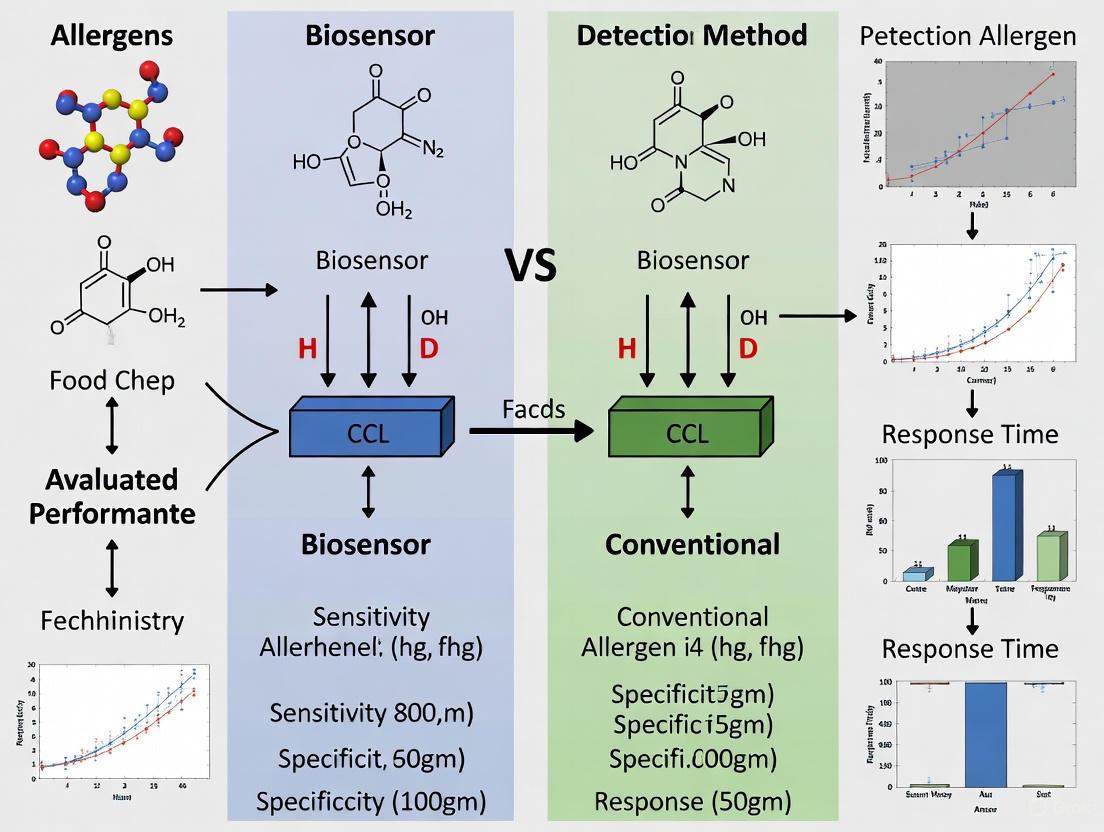
This article provides a comprehensive evaluation of emerging biosensing technologies against established conventional methods for allergen detection.
Biosensors vs. Conventional Methods: A Performance Evaluation for Next-Generation Allergen Detection
Abstract
This article provides a comprehensive evaluation of emerging biosensing technologies against established conventional methods for allergen detection. Aimed at researchers, scientists, and drug development professionals, it explores the foundational principles of colorimetric, fluorescent, electrochemical, SERS, and SPR biosensors, alongside portable platforms like lateral flow assays and microfluidic devices. The scope extends to methodological applications, critical troubleshooting of performance parameters such as sensitivity and dynamic range, and a direct comparative analysis of analytical capabilities. By synthesizing validation data and future prospects, this review serves as a strategic guide for selecting, optimizing, and advancing detection technologies to enhance food safety, clinical diagnostics, and biomanufacturing processes.
The Analytical Landscape: Foundational Principles of Allergen Detection Technologies
The Growing Public Health Imperative for Accurate Allergen Detection
Food allergy has emerged as a significant global public health concern, with increasing prevalence affecting individuals of all ages in both developed and developing countries [1]. According to recent studies, the incidence of food allergies in infants in China has risen from 7.7% in 2009 to 11.1% in 2019, reflecting a worrying worldwide trend [2]. In the United States alone, peanut allergies affect approximately 6.2 million individuals, posing a serious public health risk due to the potential for accidental exposure and life-threatening anaphylaxis [3]. Since the only effective prevention for affected individuals remains strict avoidance of allergenic foods, accurate detection and labeling become critical components of public health protection [2] [1].
This escalating health burden has prompted regulatory bodies worldwide to establish labeling requirements for major allergens. The European Union mandates declaration of 14 allergenic foods, while the United States focuses on the "big eight" allergens responsible for 90% of all food allergies [4]. Japan has implemented one of the most specific regulatory thresholds, requiring labeling at 10 μg allergen protein per gram of food and establishing official analytical methods for validation [2] [4]. Despite these regulatory frameworks, accidental exposure continues to occur, with more than half of food allergy reactions in restaurants happening even after staff are notified of a customer's allergy [3]. This reality underscores the critical need for reliable, sensitive, and accessible allergen detection methods that can protect susceptible populations while supporting food manufacturers in regulatory compliance.
Conventional Allergen Detection Methods: Foundations and Limitations
Traditional allergen detection methodologies have primarily relied on immunochemical and DNA-based techniques, each with distinct advantages and limitations for specific application scenarios.
Immunoassays and DNA-Based Methods
Enzyme-linked immunosorbent assay (ELISA) represents the gold standard in food allergen detection, offering high sensitivity, specificity, and relatively easy operation [2]. The Codex Alimentarius Commission has adopted ELISA as the official test for gluten allergens, specifying that gluten levels in food should not exceed 20 mg/kg [2]. Commercial ELISA kits are widely available for a broad selection of food allergens, with detection limits typically ranging from 1-25 ppm, making them suitable for most regulatory compliance testing [4]. However, ELISA presents several limitations: it is time-consuming (requiring up to 3.5 hours per analysis), relatively expensive for small sample batches, prone to cross-reactivity interference, and difficult to miniaturize for portable applications [4].
Polymerase chain reaction (PCR) methods provide an alternative approach that detects allergen-coding genes rather than the proteins themselves [2] [4]. These methods are particularly valuable for detecting highly processed allergenic foods where proteins may be denatured but DNA remains intact [2]. Germany has employed PCR as an official analytical tool for food allergen detection, and Japan recognizes both ELISA and PCR as official testing methods [2]. The primary advantage of PCR lies in the greater stability of DNA fragments compared to proteins, especially in processed foods. However, PCR is considered an indirect detection method and may be less suitable for food allergens containing high protein but low DNA content, such as eggs [4].
Mass Spectrometry and Emerging Conventional Techniques
Liquid chromatography with tandem mass spectrometry (LC-MS/MS) has gained traction for its ability to detect proteotypic peptides across complex food matrices, offering new levels of precision compared to immunochemical methods [5]. Mass spectrometry can simultaneously quantify specific proteins responsible for allergic responses, such as Ara h 3 and Ara h 6 in peanuts, Bos d 5 in milk, Gal d 1 and Gal d 2 in eggs, and tropomyosin in shellfish [5]. With detection limits as low as 0.01 ng/mL, mass spectrometry offers high sensitivity and specificity, with scalability across all key allergens featured in labeling regulations worldwide [5]. The technique is particularly valuable for multiplexed analysis and provides unambiguous identification of allergens, though it requires sophisticated instrumentation and specialized expertise [5].
Table 1: Comparison of Conventional Allergen Detection Methods
| Method | Detection Principle | Sensitivity | Analysis Time | Key Applications | Major Limitations |
|---|---|---|---|---|---|
| ELISA | Antigen-antibody binding | 1-25 ppm [4] | Up to 3.5 hours [4] | Regulatory compliance testing [2] | Cross-reactivity, difficult miniaturization [4] |
| PCR | DNA amplification | Varies by target | 2-4 hours | Processed foods, official testing [2] | Indirect detection, not suitable for low-DNA allergens [4] |
| Lateral Flow Immunoassay | Antigen-antibody binding | Moderate | 10-15 minutes | Rapid screening, qualitative testing [4] | Semi-quantitative, lower sensitivity [4] |
| Mass Spectrometry | Protein mass analysis | 0.01 ng/mL [5] | 1-2 hours | Multiplex detection, complex matrices [5] | Expensive equipment, requires expertise [5] |
Biosensing Technologies: Next-Generation Approaches
Biosensors represent a transformative approach to allergen detection, integrating biological recognition elements with transducers to convert molecular interactions into measurable signals [6]. These systems offer the potential for rapid, sensitive, and on-site detection, addressing critical limitations of conventional methods.
Electrochemical Biosensors
Electrochemical biosensors have shown significant promise for food allergen detection due to their high sensitivity, portability, and potential for miniaturization [4]. These sensors employ various recognition elements, including antibodies, nucleic acids, cells, and molecularly imprinted polymers, with nanomaterials playing a crucial role in enhancing signal transduction [4]. Recent innovations have demonstrated remarkable performance characteristics. For instance, an electrochemical immunosensor utilizing a nanocomposite of gold nanoparticles, molybdenum disulfide, and chitosan achieved a detection limit of 0.04 ng/mL for the BRCA-1 protein, though applied in cancer diagnostics, this showcases the sensitivity potential for allergen detection [7]. Similarly, enzyme-based solid-phase electrochemiluminescence sensors have been developed with wide linear ranges from 10 μM to 7.0 mM and limits of detection of 1 μM for targets like glucose, demonstrating principles applicable to allergen sensing [7].
The advantages of electrochemical biosensors include their compatibility with complex food matrices, minimal sample preparation requirements, and rapid analysis times. Additionally, their electrical readout system facilitates integration with digital technologies and point-of-care platforms, making them suitable for field-deployable applications in food manufacturing facilities, restaurants, and even home use [4].
CRISPR-Based Biosensing Platforms
CRISPR-based biosensors represent a revolutionary approach to nucleic acid detection, offering unprecedented specificity and sensitivity. The DETECTR system, which combines recombinase polymerase amplification with CRISPR-Cas12a, has been applied to peanut allergen detection targeting the Ara h1 DNA sequence [3]. This system operates under isothermal conditions, eliminating the need for thermal cycling equipment and enabling rapid, cost-effective detection suitable for point-of-use applications [3].
The CRISPR-Cas12a mechanism involves collateral cleavage of single-stranded DNA reporters upon recognition of a target sequence, producing a visible color change when linked to chromoproteins like amilCP [3]. Studies on DETECTR-based systems have reported sensitivity down to 10 aM (attomolar) and specificity above 95% for target DNA recognition [3]. When integrated into lateral flow biosensors, these systems create user-friendly, portable tests that can significantly reduce accidental exposures and improve food safety for individuals with peanut allergies [3].
Optical and Microfluidic Biosensors
Optical biosensors, including those based on surface plasmon resonance, fluorescence, and colorimetric detection, offer alternative transduction mechanisms for allergen detection. Recent advances include graphene-quantum dot hybrid biosensors that achieve femtomolar sensitivity through charge transfer-based quenching and recovery mechanisms [7]. These platforms have been validated for biotin-streptavidin and IgG-anti-IgG interactions, achieving limits of detection down to 0.1 fM, establishing a robust framework for next-generation biosensors [7].
Microfluidic biosensors integrate sample processing and detection within miniaturized channels, enabling precise fluid control with volumes as small as 10^(-6) to 10^(-15) mL [6]. These systems offer multiple advantages, including simultaneous detection of multiple parallel samples, high throughput, reduced reagent consumption, and shortened analysis times [6]. When combined with paper-based microfluidic analytical devices (μPADs), these systems eliminate the need for external power supplies through capillary action, further enhancing their field-deployability [6].
Table 2: Emerging Biosensing Platforms for Allergen Detection
| Technology | Detection Principle | Sensitivity | Analysis Time | Portability | Development Status |
|---|---|---|---|---|---|
| Electrochemical Biosensors | Electrochemical impedance, amperometry | 0.04 ng/mL [7] | Minutes | High [4] | Research with some commercial applications |
| CRISPR-DETECTR | CRISPR-Cas12a collateral cleavage | 10 aM [3] | <1 hour | High [3] | Proof-of-concept demonstrated |
| Microfluidic Biosensors | Lab-on-a-chip fluidics with various detectors | Varies by detection method | <30 minutes | High [6] | Active research and development |
| Optical Biosensors | Surface plasmon resonance, fluorescence | 0.1 fM [7] | Minutes to hours | Moderate | Research phase |
Experimental Protocols: Methodologies for Performance Validation
CRISPR-DETECTR for Peanut Allergen Detection
The CRISPR-DETECTR platform for peanut allergen detection employs a streamlined protocol that can be divided into three core stages: DNA extraction, amplification, and CRISPR-based detection [3].
Sample Preparation and DNA Extraction:
- Food Sample Homogenization: Grind food samples to a fine consistency using a manual grinder, motorized mini-blender, or rolling press to enhance protein/DNA extraction efficiency.
- DNA Extraction: Extract DNA using commercial food DNA extraction kits, following manufacturer protocols. Quantify DNA concentration using spectrophotometry.
- Target Selection: Focus on the Ara h1 gene, selecting conserved, stable regions that remain detectable after food processing and heating.
Recombinase Polymerase Amplification (RPA):
- Prepare RPA Master Mix: Combine the following components in a sterile microcentrifuge tube:
- 50-100 ng extracted DNA sample
- Forward and reverse primers specific to Ara h1 (0.4 μM each)
- Rehydration buffer (14.5 μL provided with RPA kit)
- Recombinase enzyme
- Single-stranded binding protein
- Strand-displacing DNA polymerase
- ATP and necessary cofactors
- Amplification Protocol: Incubate the reaction mixture at 37°C for 15-20 minutes for isothermal amplification.
CRISPR-Cas12a Detection:
- Prepare CRISPR Reaction Mix: To the amplified RPA product, add:
- Cas12a enzyme (50-100 nM)
- crRNA designed for Ara h1 target sequence (50-100 nM)
- Single-stranded DNA reporter labeled with fluorophore-quencher pair (100-200 nM)
- Incubation and Signal Detection: Incubate at 37°C for 10-15 minutes. Cas12a recognizes the target sequence, activates collateral cleavage activity, and separates fluorophore from quencher, generating a detectable signal.
- Lateral Flow Readout: Alternatively, use a chromoprotein-quencher system (e.g., amilCP) producing a strong blue color visible to the naked eye, and integrate with lateral flow strips for visual detection.
Validation and Quality Control:
- Include positive controls (known peanut-contaminated foods) and negative controls (peanut-free foods).
- Compare results against commercial peanut test kits to measure accuracy.
- Test different sample preparation methods to determine optimal protein extraction efficiency.
Electrochemical Immunosensor for Protein Allergens
Electrochemical biosensors for direct protein allergen detection follow a different approach, focusing on immunochemical recognition rather than DNA detection.
Electrode Modification and Sensor Fabrication:
- Electrode Preparation: Clean and polish working electrode (e.g., glassy carbon, gold, or screen-printed carbon electrodes) according to standard electrochemical protocols.
- Nanomaterial Modification: Deposit nanocomposite materials to enhance surface area and electron transfer. For example:
- Prepare graphene oxide solution and reduce on electrode surface
- Drop-cast gold nanoparticles (10-20 nm diameter) suspended in aqueous solution
- Apply molybdenum disulfide nanosheets functionalized with chitosan
- Antibody Immobilization: Immobilize capture antibodies specific to target allergen (e.g., anti-Ara h2 for peanut) through:
- Physical adsorption: Incubate with antibody solution (10-100 μg/mL) for 2 hours at 4°C
- Covalent attachment: Use EDC/NHS chemistry to form amide bonds with carboxyl-functionalized surfaces
- Affinity-based immobilization: Utilize protein A/G or streptavidin-biotin systems
Electrochemical Measurement Protocol:
- Blocking: Treat modified electrode with blocking buffer (e.g., 1% BSA, casein, or synthetic blockers) for 1 hour to minimize nonspecific binding.
- Sample Incubation: Incubate electrode with extracted food sample or standard solutions for 20-30 minutes with gentle agitation.
- Washing: Rinse electrode thoroughly with PBS or appropriate buffer to remove unbound materials.
- Detection Antibody Application: For sandwich assays, incubate with detection antibody labeled with electroactive tag (e.g., horseradish peroxidase, alkaline phosphatase) or directly with redox labels.
- Electrochemical Measurement: Perform measurement using suitable technique:
- Amperometry: Apply fixed potential and measure current over time
- Electrochemical Impedance Spectroscopy: Scan frequency range from 0.1 Hz to 100 kHz with 10 mV amplitude
- Square Wave Voltammetry: Scan from -0.5V to +0.5V with optimized pulse parameters
Data Analysis and Quantification:
- Calibration Curve: Measure standard solutions with known allergen concentrations to establish calibration curve.
- Signal Processing: Apply background subtraction and signal smoothing algorithms as needed.
- Quantitative Analysis: Calculate unknown concentrations from linear regression of calibration data.
- Validation: Compare results with reference methods (ELISA, MS) to verify accuracy.
Comparative Performance Analysis: Biosensors Versus Conventional Methods
The transition from conventional methods to biosensing platforms represents a paradigm shift in allergen detection capabilities, with each approach offering distinct advantages for specific application scenarios.
Sensitivity and Detection Limits
Modern biosensing platforms have achieved remarkable sensitivity levels that rival or exceed conventional methods. CRISPR-DETECTR systems demonstrate sensitivities down to 10 aM for target DNA sequences, while advanced electrochemical biosensors can detect protein targets at concentrations as low as 0.04 ng/mL [3] [7]. These sensitivity levels approach or surpass those of traditional ELISA (1-25 ppm) and mass spectrometry (0.01 ng/mL) [5] [4]. For context, the threshold for allergic reactions can be as low as 0.2 mg of peanut protein for highly sensitive individuals, necessitating detection capabilities in the parts-per-million range or lower [1]. Both biosensors and conventional methods can meet these sensitivity requirements, though biosensors often achieve them with simpler instrumentation and faster analysis times.
Analysis Time and Throughput
Analysis time represents one of the most significant advantages of biosensing platforms over conventional methods. While traditional ELISA requires up to 3.5 hours and PCR methods need 2-4 hours, biosensors can deliver results in minutes to under one hour [3] [4]. This accelerated timeline enables more rapid decision-making in food production environments and allows for more extensive testing regimes. Lateral flow biosensors, in particular, can provide results in 10-15 minutes, making them suitable for point-of-use applications where time is critical [4]. Microfluidic biosensors further enhance throughput capabilities through parallel processing of multiple samples, automating labor-intensive steps, and reducing hands-on time [6].
Portability and Point-of-Need Applications
Perhaps the most transformative advantage of biosensors is their compatibility with portable, point-of-need applications. Unlike conventional methods that require sophisticated laboratory infrastructure, biosensors can be engineered into compact, user-friendly devices suitable for field use [3] [4] [6]. The integration of biosensors with microfluidic platforms and lateral flow strips creates systems that require minimal technical expertise, enabling deployment in restaurants, homes, and food production facilities [3] [6]. This addresses a critical gap in food safety monitoring, as more than half of food allergy reactions occur in restaurant settings despite staff notification of allergies [3].
Table 3: Comprehensive Method Comparison for Allergen Detection
| Performance Characteristic | ELISA | PCR | Mass Spectrometry | Biosensors |
|---|---|---|---|---|
| Sensitivity | 1-25 ppm [4] | Varies by target | 0.01 ng/mL [5] | 0.04 ng/mL - 10 aM [3] [7] |
| Analysis Time | Up to 3.5 hours [4] | 2-4 hours | 1-2 hours | Minutes to 1 hour [3] |
| Quantitative Capability | Excellent | Good to excellent | Excellent | Good to excellent |
| Multiplexing Capacity | Limited | Moderate | High | Moderate to high |
| Equipment Cost | Moderate | Moderate | High | Low to moderate |
| Portability | Low | Low | Low | High [3] [6] |
| Ease of Use | Moderate training required | Specialized training required | Extensive training required | Simple to moderate [3] |
| Approval Status | Widely accepted and validated | Accepted in some jurisdictions [2] | Gaining acceptance | Emerging validation |
Technology Integration and Pathway Analysis
The evolution of allergen detection technologies follows a clear trajectory toward integration, miniaturization, and intelligence. The signaling pathways and technological relationships in advanced biosensing platforms can be visualized through the following workflow:
This integration pathway highlights the convergence of multiple technological approaches, from sample processing to detection output, enabling the development of comprehensive allergen detection systems that address the limitations of conventional methods.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of advanced allergen detection methods require specialized reagents and materials optimized for specific technological platforms.
Table 4: Essential Research Reagent Solutions for Allergen Detection Development
| Reagent/Material | Function | Application Examples | Technical Considerations |
|---|---|---|---|
| Recombinase Polymerase Amplification (RPA) Kits | Isothermal nucleic acid amplification | CRISPR-DETECTR platforms [3] | Maintain at recommended storage temperatures; optimize primer design for target sequences |
| CRISPR-Cas12a Enzymes | Target-specific recognition and collateral cleavage | Nucleic acid-based allergen detection [3] | Requires specific crRNA design; activity varies by buffer conditions |
| Chromoprotein-Quencher Systems (amilCP) | Visual signal generation | Lateral flow biosensors [3] | Provides color change visible to naked eye; consider colorblind accessibility |
| Gold Nanoparticles | Signal amplification, electrode modification | Electrochemical and optical biosensors [7] [4] | Control size distribution (10-20 nm optimal); functionalize surface for biomolecule conjugation |
| Graphene-Based Nanomaterials | Enhanced electron transfer, high surface area | Electrochemical sensor substrates [7] | Quality varies by synthesis method; optimize oxidation level for specific applications |
| Monoclonal/Polyclonal Antibodies | Specific allergen recognition | Immunoassays, immunosensors [2] [4] | Validate specificity for target epitopes; consider cross-reactivity with related proteins |
| Aptamers | Nucleic acid-based recognition elements | Alternative to antibodies in biosensors [4] | SELEX selection required; offers better stability than antibodies |
| Microfluidic Chip Substrates (PDMS, PMMA, Paper) | Miniaturized fluidic pathways | Microfluidic biosensors [6] | PDMS: optical transparency but protein adsorption; Paper: low cost but limited complexity |
The evolving landscape of allergen detection reflects a clear transition from conventional laboratory-based methods to advanced biosensing platforms that offer enhanced sensitivity, rapid analysis, and point-of-need capabilities. While traditional techniques like ELISA and PCR remain foundational for reference analysis and regulatory compliance, biosensors address critical gaps in the food safety ecosystem, particularly for rapid screening and field-deployable applications [2] [4].
Future developments in allergen detection will likely focus on several key areas. AI-enhanced testing and non-destructive diagnostics are reshaping allergen detection through methods such as hyperspectral imaging, Fourier Transform Infrared spectroscopy, and computer vision [5]. When combined with machine learning, these approaches allow non-destructive, real-time allergen detection without altering food integrity [5]. Multiplexed platforms capable of simultaneously detecting multiple allergens will address the growing need for comprehensive food safety assessment, particularly for products with complex ingredient profiles [5] [6]. Integration with cloud-based systems and Internet of Things technologies will enable real-time monitoring, data visualization, and predictive risk management across food production facilities [5].
The convergence of these technological advances with regulatory standards and public health priorities creates a compelling imperative for continued innovation in allergen detection. As these technologies mature, they will enable faster decision-making, enhance consumer safety, improve regulatory compliance, and ultimately reduce the public health burden of food allergies through more effective prevention and management strategies [5].
In the field of diagnostic science, certain conventional methods have established themselves as "gold standards" for the accurate detection and quantification of analytes due to their proven reliability, sensitivity, and specificity. Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) represent three pillars of analytical techniques widely used in clinical, research, and environmental settings [8] [9]. These methods provide the benchmark against which emerging technologies, such as novel biosensors, are evaluated [10]. This guide provides a comprehensive comparison of these established techniques, detailing their fundamental principles, experimental protocols, and analytical performance to serve as a reference for researchers and developers validating new diagnostic platforms.
Table 1: Core Principles and Applications of Gold Standard Methods
| Method | Fundamental Principle | Primary Target | Common Applications |
|---|---|---|---|
| ELISA | Antibody-antigen interaction with enzyme-mediated colorimetric detection [11] | Proteins, Antigens [10] | Clinical biomarkers (e.g., ferritin, cardiac markers), hormone detection, food allergens [8] [10] |
| PCR | Enzymatic amplification of specific DNA/RNA sequences | Nucleic Acids (DNA, RNA) [8] | Pathogen detection (e.g., SARS-CoV-2 [12]), food allergen detection from genetically modified organisms [8] |
| LC-MS/MS | Physical separation by liquid chromatography followed by mass-to-charge ratio analysis [9] | Small molecules, metabolites, proteins [13] [9] | Metabolomics, therapeutic drug monitoring, biomarker discovery and validation [13] [9] |
Principles and Experimental Protocols
Enzyme-Linked Immunosorbent Assay (ELISA)
The core principle of ELISA is the specific binding between an antibody and its target antigen, with detection achieved via an enzyme-linked conjugate that produces a measurable signal, typically a color change [11]. A common format is the sandwich ELISA, which is renowned for its high sensitivity [10].
Detailed Protocol for a Sandwich ELISA [10]:
- Coating: A capture antibody is immobilized onto the surface of a microplate well.
- Blocking: The well is treated with a blocking buffer (e.g., bovine serum albumin) to cover any remaining protein-binding sites, thereby minimizing non-specific binding.
- Sample Incubation: The sample containing the target antigen is added. If the antigen is present, it binds to the capture antibody.
- Detection Antibody Incubation: A second, enzyme-conjugated detection antibody is added, which binds to a different epitope on the captured antigen, forming a "sandwich."
- Washing: Between each step, the well is thoroughly washed to remove unbound components.
- Signal Development: A substrate solution is added. The enzyme conjugated to the detection antibody catalyzes a reaction that converts the substrate into a colored product.
- Signal Measurement & Quantification: The reaction is stopped, and the intensity of the color is measured spectrophotometrically. The signal intensity is proportional to the amount of antigen present in the sample, and quantification is achieved by comparison to a standard curve.
Polymerase Chain Reaction (PCR)
PCR is a molecular technique that amplifies a specific region of DNA (or RNA, via reverse transcription) through repetitive thermal cycling, enabling the detection of trace amounts of nucleic acids [8]. Real-time PCR (qPCR) allows for the quantification of the amplified DNA by monitoring the fluorescence signal at each cycle.
Detailed Protocol for Real-Time PCR [12]:
- Nucleic Acid Extraction: The target DNA or RNA is purified from the sample matrix (e.g., nasopharyngeal swab, food sample).
- Reverse Transcription (if targeting RNA): For RNA viruses like SARS-CoV-2, the RNA is first transcribed into complementary DNA (cDNA) using a reverse transcriptase enzyme [12].
- Reaction Setup: The extracted DNA (or cDNA) is mixed with a master mix containing:
- Primers: Short, specific DNA sequences that flank the target region.
- Nucleotides: The building blocks (dNTPs) for new DNA strands.
- DNA Polymerase: A thermostable enzyme that synthesizes new DNA.
- Probe: A sequence-specific oligonucleotide with a fluorescent reporter and quencher (e.g., TaqMan probe).
- Amplification & Detection: The mixture is placed in a thermal cycler and subjected to repeated cycles of:
- Denaturation: High temperature (~95°C) separates the double-stranded DNA.
- Annealing: Lower temperature allows primers to bind to their specific target sequences.
- Extension: The DNA polymerase extends the primers, synthesizing new DNA strands. During this step, the probe is cleaved, separating the reporter from the quencher and generating a fluorescent signal.
- Quantification: The instrument measures the fluorescence in real-time. The cycle threshold (Ct), the point at which the fluorescence crosses a predetermined background level, is used for quantification. A lower Ct value indicates a higher initial concentration of the target [12].
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS)
LC-MS/MS combines the physical separation capabilities of liquid chromatography with the highly specific and sensitive detection of tandem mass spectrometry [9]. It is particularly valued for its ability to accurately quantify a wide range of analytes in complex biological matrices.
Detailed Protocol for a Quantitative LC-MS/MS Assay [14]:
- Sample Preparation: The sample (e.g., serum, tissue, sewage sludge) undergoes processing, which may include protein precipitation, solid-phase extraction (SPE), or other cleanup methods to remove interfering matrix components [14].
- Internal Standard Addition: A known amount of an isotopically labeled internal standard (e.g., erythromycin-13C2) is added to the sample. This standard corrects for analyte loss during preparation and matrix effects during ionization [9] [14].
- Liquid Chromatography (LC): The sample extract is injected into the LC system, where analytes are separated based on their chemical properties (e.g., hydrophobicity) as they pass through a chromatographic column.
- Ionization: The eluted analytes are ionized, typically using Electrospray Ionization (ESI), to form gas-phase ions.
- Mass Analysis (Tandem MS): The ions are first analyzed in the first mass analyzer (MS1) to select the precursor ion of the target analyte. The selected ions are then fragmented in a collision cell, and the resulting product ions are analyzed in the second mass analyzer (MS2).
- Detection & Quantification: The detector records a signal for a specific precursor-product ion transition for each analyte. The peak area of the analyte is compared to the peak area of the internal standard. Quantification is achieved by referencing a calibration curve prepared with known concentrations of the authentic standard [14].
Figure 1: LC-MS/MS Analytical Workflow. The process involves sample preparation, chromatographic separation, ionization, and two stages of mass spectrometric analysis for highly specific detection and quantification [9] [14].
Performance Comparison and Experimental Data
The choice among ELISA, PCR, and LC-MS/MS is dictated by the specific analytical requirements. The following table and experimental data highlight their comparative performance.
Table 2: Analytical Performance Comparison of ELISA, PCR, and LC-MS/MS
| Performance Metric | ELISA | PCR | LC-MS/MS |
|---|---|---|---|
| Sensitivity | High (immunoassay-based) [10] | Extremely High (can detect few copies) [12] | Very High (zeptomole range for HRP) [15] |
| Specificity | High (antibody-dependent) [11] | Very High (primer/probe sequence-dependent) | Very High (mass resolution-dependent) [9] |
| Multiplexing Capability | Low to Moderate [8] | Moderate to High (multiplex panels) | High (can analyze 1000s of features) [9] |
| Throughput | High (96-well plate format) | High | Moderate to High [9] |
| Analysis Time | Few hours [8] | Few hours [8] | Longer (includes separation time) |
| Quantification Accuracy | Good (can be affected by cross-reactivity) | Excellent (based on Ct value) [12] | Excellent (with isotope dilution) [9] [14] |
Experimental Data from Validation Studies
ELISA vs. Photonic Crystal Biosensor: A method comparison study for ferritin detection demonstrated that while a novel photonic crystal (PC) biosensor showed promise, its total calculated error (TEcalc) exceeded the total allowable error (TEa) when certified ELISAs were used as the reference method. This underscores the reliability of ELISA as a benchmark, while also indicating areas for optimization in newer platforms [10].
PCR vs. Rapid Antigen Test (RAT): The performance of the Standard Q COVID-19 RAT was evaluated against rRT-PCR. The study found that while the RAT had 100% specificity, its clinical sensitivity was highly dependent on the viral load. For samples with an RdRp Ct value ≤ 23.37 (high viral load), the RAT's sensitivity was 81.4%. However, for all specimens, the overall sensitivity dropped to 28.7%, highlighting the superior sensitivity of PCR for low-level detection [12].
LC-MS/MS Quantification Methods: A systematic study on antibiotic quantification in biosolids revealed that the choice of quantification method in LC-MS/MS significantly impacts results. Using external calibration alone led to substantial over- or under-estimation (e.g., 110–450% overestimation for erythromycin). The most accurate results were achieved using isotope dilution with an authentic target analog, which effectively compensates for matrix effects and analyte loss, showcasing a key advantage of LC-MS/MS for precise quantification in complex matrices [14].
The Scientist's Toolkit: Essential Research Reagents
The successful application of these gold standard methods relies on a set of critical reagents, each with a specific function.
Table 3: Key Research Reagent Solutions and Their Functions
| Reagent / Material | Function | Associated Method |
|---|---|---|
| Capture & Detection Antibodies | Biological recognition elements that provide specificity by binding to the target antigen. | ELISA [11] [10] |
| Primers and Probes | Short nucleic acid sequences that dictate the specificity of the amplification by binding to complementary target DNA/RNA. | PCR [12] |
| Isotopically Labeled Internal Standards | Chemically identical analogs of the analyte with heavy isotopes; used for precise normalization and compensation of matrix effects. | LC-MS/MS [9] [14] |
| Horseradish Peroxidase (HRP) | A common enzyme used in conjugates to catalyze a colorimetric, chemiluminescent, or fluorescent reaction for signal generation. | ELISA, Biosensors [11] [15] |
| Functionalized Iron-Oxide Nanoparticles (fAb-IONs) | Magnetic nanoparticles conjugated with antibodies; used for efficient extraction and purification of target antigens from complex samples like serum. | ELISA, PC Biosensor [10] |
ELISA, PCR, and LC-MS/MS each possess distinct strengths that solidify their status as gold standard methods. ELISA offers robust, high-throughput protein detection. PCR provides unparalleled sensitivity and specificity for nucleic acid amplification. LC-MS/MS delivers exceptional versatility, multiplexing capability, and quantification accuracy for a broad spectrum of molecules. The choice of method depends fundamentally on the analyte of interest and the required analytical performance. These established techniques provide the essential benchmark for validation and performance comparison of emerging analytical technologies, including modern biosensors.
The field of biosensing is revolutionizing diagnostic and monitoring capabilities across healthcare, food safety, and environmental protection. Biosensors are analytical devices that integrate a biological recognition element with a physicochemical transducer to produce a measurable signal proportional to the concentration of a target analyte [16]. This technological rise represents a paradigm shift from conventional laboratory-based detection methods, offering the potential for rapid, sensitive, and on-site analysis.
The core of any biosensor lies in two fundamental processes: bio-recognition, where a specific biological element selectively interacts with the target, and signal transduction, where this interaction is converted into a quantifiable output [16]. This guide provides a comparative evaluation of biosensor performance against traditional allergen detection methods, presenting structured experimental data and protocols to inform researchers and drug development professionals. We focus specifically on food allergen detection as a key application area where biosensors demonstrate significant advantages in sensitivity, speed, and portability [8].
Performance Comparison: Biosensors vs. Conventional Allergen Detection Methods
Traditional techniques for food allergen detection, such as enzyme-linked immunosorbent assay (ELISA), polymerase chain reaction (PCR), and liquid chromatography-tandem mass spectrometry (LC-MS/MS), have been the cornerstone of analytical testing. However, emerging biosensing technologies increasingly challenge their dominance, particularly for applications requiring rapid, on-site analysis [8].
Table 1: Performance Comparison of Allergen Detection Technologies
| Technology | Detection Principle | Typical LOD | Analysis Time | Multiplexing Capability | Portability | Key Applications |
|---|---|---|---|---|---|---|
| ELISA | Antibody-Antigen Binding | Moderate (ng-mcg/mL) | Hours | Low | Low | Laboratory confirmation |
| PCR | Nucleic Acid Amplification | High (pg-ng/mL) | 2-4 hours | Moderate | Low | Official analysis (Germany, Japan) |
| LC-MS/MS | Mass Spectrometry | High (pg-ng/mL) | Hours | High | Low | High-throughput lab testing |
| Electrochemical Biosensors | Electron Transfer | High (fM-nM) [17] | Minutes | Developing | High | Point-of-care, on-site screening |
| Optical Biosensors | Refractive Index/Luminescence | High (fM-nM) | Minutes | High | Moderate | Clinical diagnostics, food safety |
Table 2: Quantitative Performance Data for Emerging Biosensing Technologies in Food Allergen Detection
| Biosensing Technology | Target Allergen | Recognition Element | Linear Range | Limit of Detection (LOD) | Reference |
|---|---|---|---|---|---|
| Colorimetric LFA | Peanut | Antibody | 0.5–50 ng/mL | 0.5 ng/mL | [8] |
| Electrochemical Immunosensor | Tropomyosin | Antibody | 1–100 ng/mL | 0.3 ng/mL | [8] |
| Fluorescent Aptasensor | Major peanut allergen (Ara h 1) | Aptamer | 0.5–1000 ng/mL | 0.16 ng/mL | [8] |
| SERS Biosensing | Milk allergen (β-lactoglobulin) | Antibody | 0.01–100 ng/mL | 0.008 ng/mL | [8] |
The comparative data reveals that emerging biosensors consistently match or surpass the sensitivity of traditional methods like ELISA while offering significantly reduced analysis times. Furthermore, biosensors integrated into portable platforms such as lateral flow assays (LFAs) and microfluidic devices enable on-site detection capabilities that are simply not feasible with conventional techniques [8]. This addresses critical needs in food safety management, allowing for rapid screening throughout the production chain rather than relying solely on end-product laboratory testing.
Experimental Protocols for Biosensor Development and Validation
To ensure reliable and reproducible results, researchers follow standardized experimental protocols for biosensor development. The following sections detail key methodologies cited in recent literature.
Aptamer Characterization via Fluorescence Titration and Isothermal Titration Calorimetry (ITC)
Objective: To discover and characterize DNA aptamers for specific targets (e.g., bilirubin and biliverdin) by determining binding affinity and thermodynamic parameters.
Materials:
- Synthesized DNA aptamer candidates
- Target analytes (e.g., biliverdin, bilirubin)
- Thioflavin T (ThT) dye
- Binding buffer (appropriate pH and ionic strength)
- Fluorescence spectrophotometer
- Isothermal Titration Calorimeter
Procedure:
- Aptamer Preparation: Dilute the DNA aptamer in binding buffer and anneal by heating to 95°C for 5 minutes, followed by gradual cooling to room temperature.
- Fluorescence Titration:
- Prepare a solution containing the aptamer and ThT dye.
- Titrate with increasing concentrations of the target analyte.
- Measure fluorescence emission intensity at each addition.
- Plot fluorescence intensity versus analyte concentration to generate binding curves and calculate dissociation constant (Kd).
- Isothermal Titration Calorimetry:
- Load the aptamer solution into the sample cell and the target analyte into the syringe.
- Perform sequential injections of the analyte into the aptamer solution.
- Measure the heat absorbed or released with each injection.
- Integrate heat data and fit to an appropriate binding model to determine Kd, enthalpy change (ΔH), and entropy change (ΔS).
Validation: This protocol enabled the identification of a biliverdin aptamer with a Kd of 6 nM and LOD of 0.7 nM, and a bilirubin aptamer with a Kd of 203 nM and LOD of 47 nM, confirmed through orthogonal techniques [18].
Development of Electrochemical Immunosensors Using Nanomaterial-Modified Electrodes
Objective: To construct an ultrasensitive electrochemical immunosensor for biomarker detection (e.g., BRCA-1) using nanocomposite-modified electrodes.
Materials:
- Disposable pencil graphite electrodes
- Gold nanoparticles (AuNPs)
- Molybdenum disulfide (MoS₂)
- Chitosan (CS)
- Monoclonal anti-BRCA-1 antibodies
- BRCA-1 antigen standards
- Electrochemical workstation with potentiostat
Procedure:
- Electrode Modification:
- Prepare a nanocomposite suspension of AuNPs, MoS₂, and CS.
- Drop-cast the nanocomposite onto the surface of pre-polished pencil graphite electrodes and dry.
- Antibody Immobilization:
- Incubate the modified electrode with anti-BRCA-1 antibody solution.
- Wash to remove unbound antibodies.
- Electrochemical Measurement:
- Incubate the immunosensor with BRCA-1 antigen standards or samples.
- Perform electrochemical detection using differential pulse voltammetry (DPV) or electrochemical impedance spectroscopy (EIS).
- Measure current or impedance changes correlated with antigen concentration.
Validation: The constructed immunosensor demonstrated a linear detection range of 0.05–20 ng/mL for BRCA-1 with an LOD of 0.04 ng/mL, high reproducibility (RSD 3.59%), and maintained 98 ± 3% recovery in spiked serum samples [7].
Signaling Pathways and Experimental Workflows in Biosensing
The following diagrams illustrate core signaling pathways and experimental workflows fundamental to biosensor operation, based on transduction mechanisms described in the research literature.
Electrochemical Biosensor Signal Transduction Pathway
Workflow for Aptamer Characterization and Biosensor Development
The Scientist's Toolkit: Essential Research Reagent Solutions
The development and implementation of high-performance biosensors rely on specialized reagents and materials. The following table details key components essential for biosensor research and development.
Table 3: Essential Research Reagents for Biosensor Development
| Reagent/Material | Function | Example Applications |
|---|---|---|
| Nucleic Acid Aptamers | Synthetic recognition elements obtained via SELEX; offer high stability and specificity for targets | Bilirubin/biliverdin sensing [18], detection of small molecules, proteins |
| Monoclonal Antibodies | High-specificity biorecognition elements for antigen binding | Food allergen detection (e.g., tropomyosin) [8], cancer biomarkers (e.g., BRCA-1) [7] |
| Gold Nanoparticles (AuNPs) | Enhance electron transfer in electrochemical sensors; provide plasmonic effects in optical sensors | Electrode modification for immunosensors [7], SERS platforms [19] |
| Graphene & MoS₂ | 2D nanomaterials with high surface area and excellent electrical properties | Field-effect transistors (FETs), composite electrodes for improved sensitivity [7] |
| Thioflavin T (ThT) | Fluorescent dye that exhibits enhanced fluorescence upon binding to specific aptamer structures | Aptamer characterization via fluorescence titration [18] |
| Silver Nanoparticles (AgNPs) | Signal amplification in optical and electrochemical biosensors; drug delivery carriers | Plasmonic biosensors, monitoring drug release [20] |
| Molecularly Imprinted Polymers (MIPs) | Artificial receptors with tailor-made binding sites for specific molecules | Synthetic recognition elements as antibody alternatives [16] |
The comparative analysis presented in this guide demonstrates that biosensing technologies offer significant advantages over conventional detection methods, particularly in applications requiring rapid, sensitive, and on-site analysis such as food allergen monitoring. The core mechanisms of bio-recognition and signal transduction have evolved to provide detection capabilities that match or exceed traditional laboratory-based techniques while offering unprecedented portability and speed.
Future developments in biosensing will likely focus on integrating artificial intelligence for data interpretation, creating wearable biosensing systems, and developing IoT-connected platforms for real-time monitoring [17]. Furthermore, standardization of biosensor evaluation criteria, particularly concerning dynamic performance parameters such as response time and signal-to-noise ratio, will be critical for broader adoption in clinical and industrial settings [21]. As these technologies continue to mature, they hold the potential to transform diagnostic paradigms across healthcare, food safety, and environmental monitoring.
In the fields of food safety, clinical diagnostics, and pharmaceutical development, the reliability of analytical methods hinges on rigorously defined performance metrics. Sensitivity, specificity, and limit of detection (LOD) form the fundamental triad that determines whether a detection method can be trusted for critical decision-making. These parameters take on heightened importance when evaluating emerging biosensing technologies against established conventional methods, particularly in applications with significant public health implications such as allergen detection in foods [2] [22].
The global rise in food allergy prevalence has intensified the need for highly accurate detection methods, as avoidance remains the primary preventive strategy for susceptible individuals [2]. This comparative guide objectively examines how modern biosensors perform against traditional techniques like enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR), providing researchers with a structured framework for method selection and validation. By synthesizing current experimental data and standardized protocols, this analysis offers evidence-based insights into the evolving landscape of allergen detection technologies.
Defining the Core Performance Metrics
Limit of Detection (LOD)
The limit of detection represents the lowest concentration of an analyte that can be reliably distinguished from its absence. Formally defined as the minimum analyte concentration that produces a signal significantly different from the blank (typically with a signal-to-noise ratio of 3:1), LOD establishes the fundamental detection capability of an analytical method [22] [23]. While a lower LOD is often pursued as a marker of technological advancement, its practical importance varies significantly across applications. In food allergen detection, LOD values must be evaluated against clinically relevant thresholds established by regulatory bodies, which typically range from 0.1 to 20 mg/kg depending on the specific allergen and jurisdiction [2] [24].
Sensitivity
In analytical chemistry, sensitivity refers to the ability of a method to detect minute differences in analyte concentration, quantitatively expressed as the change in instrument response per unit change in analyte concentration [22]. Method sensitivity directly impacts the precision of quantitative measurements and determines whether a technique can monitor concentration changes within biologically or toxicologically relevant ranges. For biosensors, sensitivity is often enhanced through material engineering approaches that increase the available electrochemical interface, such as three-dimensional porous nanostructures that allow dense immobilization of bioreceptors [22].
Specificity
Specificity describes a method's capacity to detect only the target analyte without cross-reactivity to similar compounds or matrix interferences [25]. In immunochemical methods, specificity is determined by the molecular recognition properties of antibodies toward specific epitopes, while nucleic acid-based methods achieve specificity through complementary base pairing. High specificity is particularly challenging in complex food matrices where non-target components may resemble the analyte structurally or produce similar signals. Biosensors address this challenge through sophisticated surface chemistry and biorecognition elements that minimize nonspecific binding while maintaining affinity for the intended target [25] [26].
Comparative Performance Analysis: Biosensors vs. Conventional Methods
Table 1: Performance comparison of major allergen detection methodologies
| Method Type | Representative LOD | Key Strengths | Key Limitations | Detection Time | Multiplexing Capability |
|---|---|---|---|---|---|
| Immunoassays (ELISA) | 0.1-5 mg/kg [2] | High specificity, standardized protocols | Protein structure dependency, antibody cross-reactivity | 2-4 hours | Low to moderate |
| PCR Methods | 1-10 mg/kg [2] | Effective for processed foods, high specificity | Indirect detection, does not detect proteins directly | 1-3 hours | Moderate |
| Mass Spectrometry | 0.01-1 mg/kg [5] | High specificity and sensitivity, multiplexing | Expensive instrumentation, complex sample prep | 30 min - 2 hours | High |
| Biosensors | 0.01-0.1 mg/kg [5] [27] | Rapid response, portability, high sensitivity | Matrix effects, limited commercialization | 1 second - 30 minutes | Variable |
Table 2: Experimental performance data for specific detection platforms
| Technology Platform | Target Analyte | Reported LOD | Linear Range | Specificity Assessment | Reference |
|---|---|---|---|---|---|
| PCB Biosensor | HER2/CA15-3 biomarkers | 10⁻¹⁵ g/mL [27] | Not specified | Clinical validation with 29 saliva samples | [27] |
| Photonic Ring Resonator | IL-17A, CRP | Not specified | Clinically relevant ranges | Reference subtraction for nonspecific binding | [25] |
| Lateral Flow Immunoassay | Gluten | 20 mg/kg (CAC standard) [2] | Not specified | Visual detection, suitable for on-site use | [2] |
| Real-time PCR | Fish parvalbumin gene | Single copy detection [2] | 5 orders of magnitude | Species-specific detection | [2] |
| Electrochemical Biosensor | Tropomyosin | 0.01 ng/mL [5] | Not specified | Aptamer-based recognition | [2] |
Performance Trade-offs and Method Selection Considerations
The comparative data reveal significant trade-offs between conventional methods and emerging biosensor technologies. While ELISA offers well-established protocols and regulatory acceptance, its susceptibility to protein denaturation during food processing represents a substantial limitation [2]. PCR methods circumvent this issue by targeting more stable DNA markers but provide only indirect evidence of allergen presence since the problematic molecules are proteins, not nucleic acids [2].
Biosensors demonstrate remarkable improvements in detection speed and sensitivity, with some platforms achieving results within seconds and detecting attomolar concentrations [27]. However, these advanced systems face challenges related to matrix effects, nonspecific binding, and limited commercial availability [25] [23]. The optimal method selection depends heavily on the application context—while clinical settings may prioritize specificity and regulatory compliance, manufacturing environments often value speed and portability for rapid decision-making.
Experimental Protocols for Method Validation
Protocol 1: Validation of Biosensor Specificity Using Reference Probes
Background: Specificity validation is particularly challenging for label-free biosensors due to nonspecific binding (NSB) of matrix constituents in complex samples like serum or food extracts. A systematic framework inspired by FDA guidelines provides a standardized approach for control probe selection [25].
Materials:
- Photonic microring resonator (PhRR) sensors or comparable biosensor platform
- Target capture antibodies (e.g., anti-IL-17A, anti-CRP)
- Panel of negative control proteins (BSA, isotype-matched antibodies, cytochrome c, anti-FITC)
- Complex sample matrix (serum, food extract)
- Microfluidic packaging system with pressure-sensitive adhesive and PDMS gaskets
- Sterile PBS and assay diluents
Procedure:
- Functionalize sensor chips with capture antibodies and control probes in a multiplexed layout
- Package sensors in microfluidic devices using layer-by-layer assembly of PSA and PDMS
- Introduce sample matrices containing target analytes at clinically relevant concentrations
- Measure wavelength shifts for both specific capture and reference probes
- Calculate specific binding by subtracting reference signals from capture signals
- Evaluate control probe performance based on linearity, accuracy, and selectivity parameters
Validation Metrics: The optimal reference control varies by analyte. Experimental data indicate that while isotype-matching is conceptually appealing, the best-performing reference differs between targets—BSA scored highest (83%) for IL-17A detection, while a rat IgG1 isotype control performed best (95%) for CRP assays [25].
Protocol 2: LOD and Sensitivity Determination for Electrochemical Biosensors
Background: This protocol outlines the characterization of key analytical parameters for electrochemical biosensors, using allergen detection as an application example.
Materials:
- Glucose test strips (bare carbon electrode structure without enzymes)
- Ozone cleaner and ammonium hydroxide solution
- 3-Mercaptopropanyl-N-hydroxysuccinimide ester (NHS ester) in ethanol
- Target-specific antibodies (e.g., anti-tropomyosin, anti-Bos d 5)
- Ethanolamine blocking solution
- Electrochemical workstation with Bluetooth capability for data transmission
- Standard solutions of target allergen at varying concentrations
Procedure:
- Perform surface cleaning via ozone treatment (15 minutes) followed by ammonium hydroxide wash
- Functionalize electrode surface with NHS ester solution (2-hour immersion)
- Immobilize specific antibodies (20 μg/mL) by introducing to microfluidic channels
- Seal strips and refrigerate at 4°C for 18 hours
- Deactivate unreacted groups with ethanolamine
- Introduce standard solutions across clinically relevant concentration range
- Measure electrical signals (current-voltage characteristics, capacitance)
- Plot calibration curve of signal response versus analyte concentration
- Calculate LOD as mean blank signal plus three standard deviations
- Determine sensitivity as slope of the linear portion of the calibration curve
Validation Metrics: This approach has demonstrated exceptional sensitivity, with reported LOD values as low as 10⁻¹⁵ g/mL for protein biomarkers—4-5 orders of magnitude more sensitive than conventional ELISA [27].
Visualizing Biosensor Performance Evaluation
Diagram 1: A systematic framework for evaluating biosensor performance against conventional methods, emphasizing the interconnected relationship between core metrics and experimental validation.
Diagram 2: Experimental workflow for biosensor specificity validation using reference controls to account for nonspecific binding in complex sample matrices.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for biosensor development and validation
| Reagent/Material | Function | Application Examples | Considerations |
|---|---|---|---|
| NHS Ester Chemistry | Bioconjugation agent for immobilizing amine-containing biomolecules | Antibody attachment to sensor surfaces | Provides reactive sites for stable biorecognition element attachment [27] |
| Photonic Ring Resonators | Label-free detection via refractive index changes | Molecular binding kinetics studies | Enables reference subtraction for nonspecific binding [25] |
| Isotype-Matched Control Antibodies | Negative controls for specificity validation | Assessing nonspecific binding in immunoassays | Performance varies by target; requires empirical optimization [25] |
| Carbon Electrode Test Strips | Disposable sensing platforms | Electrochemical biosensors | Enable reusable PCB systems with disposable sensing elements [27] |
| Microfluidic Packaging Systems | Sample handling and delivery | Integrated biosensor systems | Incorporate PDMS gaskets and pressure-sensitive adhesives [25] |
| Phage Display Libraries | Source of novel binding elements | Aptamer and affinity reagent development | Alternative to traditional antibodies for recognition elements |
| Three-Dimensional Nanomaterials | Signal amplification | Enhancing sensor sensitivity | High surface-to-volume ratio improves signal magnitude [22] |
The comparative analysis of performance metrics reveals a nuanced landscape where no single detection technology universally outperforms all others across all parameters. Instead, method selection requires careful consideration of application-specific requirements, particularly the clinically or regulatory relevant concentration ranges for the target analyte [23].
Traditional methods like ELISA and PCR maintain important advantages in standardization, regulatory acceptance, and established performance characteristics [2] [24]. However, emerging biosensor technologies offer compelling benefits in detection speed, sensitivity, and potential for portability that make them increasingly suitable for point-of-need applications [5] [27]. The experimental data indicate that biosensors can achieve remarkable detection limits, with some platforms demonstrating up to 10⁻¹⁵ g/mL sensitivity for protein biomarkers—significantly surpassing conventional ELISA [27].
Future developments in biosensor technology will likely focus on balancing the pursuit of ultra-low LODs with practical utility, addressing challenges related to matrix effects, reproducibility, and commercial scalability [22] [23]. For researchers and drug development professionals, this evolving landscape presents opportunities to implement detection strategies that align technical capabilities with real-world application requirements, ultimately enhancing food safety, diagnostic accuracy, and public health protection.
Biosensing in Action: Methodological Advances and Integrated Platforms
Biosensors are analytical devices that combine a biological recognition element with a physicochemical transducer to detect target analytes. The integration of biological specificity with sensitive signal transduction has established biosensors as powerful tools in clinical diagnostics, food safety, and environmental monitoring. The performance of any biosensing platform is fundamentally determined by its transduction mechanism, which directly influences sensitivity, selectivity, and practical applicability.
This guide provides a systematic comparison of three principal biosensing modalities: electrochemical, optical, and Surface-Enhanced Raman Spectroscopy (SERS)-based systems. Framed within the context of detecting food allergens—an area where conventional methods like Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) face limitations in cost, speed, and portability—this analysis evaluates emerging biosensor technologies against traditional benchmarks. For researchers and drug development professionals, understanding the operational principles, performance parameters, and experimental requirements of each modality is crucial for selecting the appropriate technology for specific applications.
Performance Comparison of Biosensing Modalities
The quantitative performance of electrochemical, optical, and SERS-based biosensors varies significantly across key metrics, influencing their suitability for different research or diagnostic applications. Table 1 summarizes the typical performance characteristics and comparative advantages of each modality.
Table 1: Performance Comparison of Biosensing Modalities
| Modality | Typical Limit of Detection (LOD) | Key Advantages | Common Bioreceptors | Representative Application |
|---|---|---|---|---|
| Electrochemical | Picomolar to femtomolar range [28] | High sensitivity, portability, low cost, miniaturization, works in turbid samples [29] | Enzymes, Antibodies, Aptamers, Cells [29] | Glucose monitoring, Food allergen detection (e.g., Ovalbumin) [30] [28] |
| Optical (General) | Varies by technique (e.g., SPR: ng/mL) [28] | Label-free detection, real-time monitoring, high specificity [31] | Antibodies, Nucleic acids [31] | Biomolecular interaction analysis, Body fat estimation [32] |
| SERS | Single-molecule level (in ideal conditions) [33] | Multiplexing capability, fingerprint identification, resistance to photobleaching [33] | Antibodies, Aptamers [19] [33] | Cancer biomarker detection (e.g., α-Fetoprotein) [19] |
Electrochemical biosensors transduce a biological recognition event into an electronic signal (current, potential, or impedance change). They are renowned for their exceptional sensitivity, often achieving detection limits in the picomolar to femtomolar range for food allergens [28]. A key advantage is their compatibility with miniaturized, portable, and low-cost point-of-care devices, as they are less affected by turbid samples or optically absorbing compounds compared to optical methods [29].
Optical biosensors, such as those based on Surface Plasmon Resonance (SPR), detect changes in the optical properties of a sensor surface. SPR measures the change in the refractive index upon analyte binding, enabling real-time, label-free monitoring of biomolecular interactions [31]. While some optical sensors for egg white allergens report limits of detection in the ng/mL range [28], advanced configurations can achieve higher sensitivity. For instance, a fiber-optic SPR sensor using CdSe-ZnCdS quantum dots demonstrated a sensitivity of 3540 nm/RIU for body fat estimation [32].
SERS-based biosensors leverage the enormous enhancement of Raman scattering signals from molecules adsorbed on or near nanostructured metallic surfaces, typically gold or silver [33]. This plasmonic enhancement can boost signals by factors of 10⁶ to 10⁸, enabling detection down to the single-molecule level under ideal conditions [33]. SERS provides a unique "fingerprint" identification of molecules and allows for multiplexed detection using a single wavelength excitation source [33]. Recent developments include the use of spiky Au-Ag nanostars to create powerful SERS platforms for detecting cancer biomarkers like α-fetoprotein [19].
Experimental Protocols and Methodologies
The reliability and performance of a biosensor are directly tied to the rigor of its experimental design and fabrication. Below are detailed protocols representative of each modality.
Electrochemical Immunosensor for Biomarker Detection
The development of a electrochemical immunosensor for the cancer biomarker BRCA-1 illustrates a common protocol involving nanomaterial-enhanced electrodes [7].
Workflow Overview:
- Electrode Modification: A pencil graphite electrode (PGE) is sequentially modified with chitosan (CS), molybdenum disulfide (MoS₂), and gold nanoparticles (AuNPs). Chitosan provides a biocompatible film, MoS₂ offers a high surface area and catalytic activity, and AuNPs facilitate electron transfer and antibody immobilization.
- Antibody Immobilization: Anti-BRCA-1 antibodies are immobilized onto the AuNP-modified surface, typically through covalent coupling or physical adsorption.
- Blocking: The remaining active sites on the electrode are blocked with a non-reactive protein (e.g., Bovine Serum Albumin) to prevent non-specific binding.
- Detection and Measurement: The immunosensor is incubated with the sample containing BRCA-1. The formation of the antigen-antibody complex hinders electron transfer at the electrode surface. The detection is performed using electrochemical techniques like differential pulse voltammetry (DPV) or electrochemical impedance spectroscopy (EIS) in a solution containing a redox probe like [Fe(CN)₆]³⁻/⁴⁻. The change in current or impedance is proportional to the analyte concentration.
This sensor achieved a linear detection range of 0.05–20 ng/mL and an LOD of 0.04 ng/mL, showcasing the high sensitivity attainable with electrochemical platforms [7].
SERS-Based Immunoassay for Protein Detection
A protocol for a SERS-based immunoassay for α-fetoprotein (AFP) utilizes the intense plasmonic properties of metallic nanostructures [19].
Workflow Overview:
- Substrate Fabrication: Spiky Au-Ag nanostars are synthesized as the SERS-active substrate. Their sharp tips act as "hotspots" generating intense electromagnetic fields for signal enhancement.
- Functionalization: The nanostars are functionalized with a capture antibody specific to the target protein (AFP).
- Immunocomplex Formation: The sample is introduced, and the target analyte binds to the capture antibody.
- Signal Generation with Raman Reporter: A secondary antibody, labeled with a Raman reporter molecule (e.g., malachite green), is added to form a sandwich immunocomplex. The reporter molecule provides a characteristic SERS signal upon laser excitation.
- Measurement and Analysis: The substrate is irradiated with a laser, and the SERS spectrum is collected. The intensity of the Raman reporter's characteristic peak is quantified and correlated with the analyte concentration.
This liquid-phase SERS platform addresses limitations in cancer biomarker detection by offering high sensitivity and specificity [19].
Fiber-Optic SPR Sensor with Quantum Dots
A protocol for a quantum dot-enhanced SPR sensor demonstrates the fusion of optical sensing with advanced nanomaterials for body fat estimation [32].
Workflow Overview:
- Fiber Preparation: A germanium dioxide (GeO₂) core optical fiber with sodium fluoride (NaF) cladding is used.
- Metal Deposition: An optimized thin layer of silver is deposited on the fiber core.
- Quantum Dot Coating: The silver layer is coated with CdSe-ZnCdS core-shell quantum dots (QDs). The QDs enhance the evanescent field and modify the refractive index properties, boosting sensitivity.
- Interrogation and Sensing: Light is launched through the fiber. The resonance condition (the specific wavelength at which surface plasmons are excited) is monitored via wavelength interrogation. Changes in the resonance wavelength are directly related to changes in the refractive index of the surrounding medium (e.g., due to the adhesion of fat tissue). The sensor achieved a maximum sensitivity of 3540 nm/RIU [32].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core enhancement mechanism of SERS and a generalized experimental workflow for electrochemical biosensing.
SERS Enhancement Mechanism
SERS enhancement arises from two primary mechanisms: the electromagnetic effect from plasmonic nanoparticles and the chemical effect from charge transfer [33].
Diagram 1: SERS enhancement mechanism involves electromagnetic and chemical effects.
Electrochemical Biosensor Workflow
The fabrication and operation of a typical nanomaterial-modified electrochemical immunosensor involves a sequence of critical steps [34] [7].
Diagram 2: Electrochemical biosensor development and detection workflow.
Research Reagent Solutions
The performance of modern biosensors is heavily dependent on the selection of nanomaterials and biological recognition elements. Table 2 details key reagents and their functions in biosensor development.
Table 2: Essential Research Reagents for Biosensor Development
| Reagent Category | Specific Examples | Function in Biosensor | Relevant Modality |
|---|---|---|---|
| Nanomaterials | Gold Nanoparticles (AuNPs) [33] [7], Graphene/Reduced Graphene Oxide (RGO) [34], Quantum Dots (CdSe-ZnCdS) [32], MXene Quantum Dots [31] | Enhance electron transfer, increase surface area, provide plasmonic enhancement, enable immobilization. | Electrochemical, Optical, SERS |
| Bioreceptors | Antibodies [19] [7], Aptamers [19] [28], Enzymes (Glucose Oxidase) [7] | Provide specific recognition and binding to the target analyte. | All |
| Electrode Materials | Gold [34], Indium Tin Oxide (ITO) [7], Pencil Graphite [7] | Serve as the transduction platform. Gold offers stability and easy functionalization. | Electrochemical |
| Signal Reporters | Raman Dyes (Malachite Green) [7], Enzymes (Horseradish Peroxidase), Redox Probes ([Fe(CN)₆]³⁻/⁴⁻) [34] | Generate a measurable signal (optical, electrochemical) upon analyte binding. | SERS, Electrochemical |
Electrochemical, optical, and SERS-based biosensing modalities each present a unique set of capabilities. Electrochemical sensors lead in miniaturization and cost-effectiveness for point-of-care testing, optical sensors like SPR excel in providing real-time, label-free interaction kinetics, and SERS offers unparalleled specificity and multiplexing potential.
The choice of biosensing modality depends on the specific application requirements, including the required sensitivity, need for portability, sample matrix, and available budget. The ongoing integration of novel nanomaterials like graphene, MXenes, and quantum dots is pushing the performance boundaries of all these platforms. For researchers in drug development and diagnostics, this comparative analysis provides a framework for selecting and optimizing the appropriate biosensing technology, ultimately contributing to advancements in healthcare, food safety, and personalized medicine. Future perspectives point toward the development of multi-modal sensors and the increased use of artificial intelligence for data analysis to further improve the accuracy and utility of biosensing systems.
The field of diagnostic testing is undergoing a revolutionary shift from centralized laboratory analyses toward decentralized, point-of-care (POC) testing. This transformation is largely driven by the development and refinement of lateral flow assays (LFAs) and paper-based microfluidic devices, which combine the principles of microfluidics with the practicality of paper substrates to create affordable, user-friendly, and rapid diagnostic platforms [35] [36]. These devices leverage capillary action to transport fluids through porous membranes without requiring external power sources, making them particularly valuable for resource-limited settings [36]. The COVID-19 pandemic dramatically accelerated the adoption and visibility of these technologies, with LFAs becoming household items for SARS-CoV-2 antigen detection [37] [38]. Beyond infectious disease diagnostics, these portable platforms have found significant applications in food safety monitoring, environmental surveillance, and clinical diagnostics, offering a compelling alternative to conventional methods such as enzyme-linked immunosorbent assays (ELISA), polymerase chain reaction (PCR), and liquid chromatography-tandem mass spectrometry (LC-MS/MS) [39] [8].
This review objectively compares the performance of LFA and paper-based microfluidic biosensors against conventional allergen detection methods, focusing on analytical performance parameters including sensitivity, specificity, assay time, and operational requirements. We provide structured experimental data and detailed methodologies to enable researchers to evaluate the current capabilities and limitations of these portable platforms within the broader context of biosensor performance evaluation.
Lateral Flow Immunoassays (LFIs)
LFAs are membrane-based diagnostic tests that operate on capillary action to transport samples across various zones containing recognition elements. A typical LFA strip consists of four overlapping membranes: a sample pad for application, a conjugate pad containing labeled bioreceptors, a detection membrane (usually nitrocellulose) with immobilized capture lines, and an absorbent pad to maintain flow [40]. These components are often mounted on a backing card for structural support. The fundamental principle involves the migration of the liquid sample, which resuspends the labeled conjugates, allowing the formation of complexes that are captured at specific test lines to generate a detectable signal, typically within 5-20 minutes [39] [40].
LFAs primarily operate in two formats: sandwich and competitive immunoassays. Sandwich assays are used for larger analytes with multiple epitopes (e.g., proteins), where the intensity of the test line increases proportionally with target concentration [40]. In contrast, competitive formats are employed for small molecules or single-epitope targets, where the test line intensity decreases as analyte concentration increases—an inverse relationship that can be less intuitive for users [40]. Competitive assays offer the advantage of requiring only one bioreceptor and being insensitive to the "hook effect," a phenomenon where extremely high analyte concentrations can cause false-negative results in sandwich assays [39] [40].
Paper-Based Microfluidic Devices
Paper-based microfluidics, or "lab on paper," represents a significant evolution beyond simple lateral flow strips. These devices create precisely defined hydrophilic-hydrophobic channels on paper substrates to guide liquid flow in controlled pathways for complex analytical procedures [36]. The technology was pioneered by the Whitesides Group at Harvard University, though earlier work by Müller in 1949 on paraffin-patterned paper channels represents its rudimentary beginning [36].
Multiple fabrication techniques have been developed for creating microfluidic channels on paper, including wax printing, inkjet printing, photolithography, and laser treatment [36]. The fundamental principle across these techniques is patterning hydrophilic-hydrophobic contrasts on paper to create micron-scale capillary channels. More advanced devices incorporate passive fluidic circuits with functional elements such as multi-bi-material cantilever (B-MaC) assemblies, delay channels, and buffer zones to enable sequential reagent delivery for complex assays like paper-based ELISA (p-ELISA) [41].
A particularly innovative application is the microfluidic paper-based analytical device (μPAD) for quantitative p-ELISA, which seamlessly executes conventional ELISA steps in a paper-based format. This device utilizes a passive fluidic circuit that autonomously sequences the loading of wash solutions, substrates, and stop solutions onto the detection zone, completing assays in under 30 minutes with minimal reagent requirements and equipment needs [41].
Table 1: Comparison of LFA and Paper-Based Microfluidic Platforms
| Feature | Lateral Flow Assays | Paper-Based Microfluidic Devices |
|---|---|---|
| Principle | Capillary flow through sequential zones | Controlled capillary flow through patterned channels |
| Complexity | Relatively simple | Can accommodate complex multi-step assays |
| Assay Types | Primarily immunoassays | Immunoassays, chemical assays, enzymatic assays |
| Multiplexing Capability | Limited | Enhanced through multi-channel designs |
| Fabrication | Membrane stacking and lamination | Patterning techniques (wax printing, photolithography, etc.) |
| Quantification | Semi-quantitative (visual) | Quantitative with reader systems |
| Fluid Control | Limited control | Advanced control (delay channels, valves, buffers) |
| Typical Assay Time | 1-20 minutes | 10-30 minutes |
Detection Mechanisms and Signal Enhancement
Multiple detection mechanisms are employed in these platforms, ranging from simple colorimetric tests read by the naked eye to more sophisticated systems requiring dedicated readers. Colorimetric detection using gold nanoparticles (AuNPs) remains the most common approach due to its simplicity and low cost [41]. However, recent advancements have incorporated fluorescent, electrochemical, and surface-enhanced Raman spectroscopy (SERS) detection methods to improve sensitivity [8]. For instance, gold-platinum nanoflowers (AuPt NFs) in LFIAs have demonstrated a 100-fold improvement in detection limits compared to conventional AuNP-based LFIAs [41].
The integration of smartphones as reader interfaces has significantly enhanced the quantitative capabilities of these platforms. Smartphone-based analysis incorporates digital image processing and quantification techniques, enabling accurate measurement of analyte concentrations directly from the device while providing a familiar user interface and wireless data transmission capabilities [39] [8].
Diagram 1: LFA Component Workflow. The diagram illustrates the sequential flow of liquid sample through the four key zones of a lateral flow assay strip, culminating in signal generation at the test and control lines.
Performance Comparison: Portable vs. Conventional Methods
Analytical Sensitivity and Detection Limits
Sensitivity, often expressed as the limit of detection (LOD), is a critical parameter when evaluating diagnostic platforms. The table below compares the LODs of various detection methods for specific analytes, highlighting the performance differences between portable and conventional platforms.
Table 2: Detection Limit Comparison Across Analytical Platforms
| Analytical Platform | Target Analyte | Limit of Detection (LOD) | Reference |
|---|---|---|---|
| p-ELISA μPAD | Rabbit IgG | 8.4 pM | [41] |
| AuPt NF-LFIA | Rabbit IgG | 5 pg/mL | [41] |
| Conventional ELISA | Rabbit IgG | 230 pg/mL | [41] |
| Passive Flow-Through | Total Hazelnut Protein (THP) | 0.1-1 ppm | [39] |
| Active Flow-Through | Total Hazelnut Protein (THP) | 0.05-0.5 ppm | [39] |
| Optimized LFIA | Total Hazelnut Protein (THP) | 0.1-0.5 ppm | [39] |
| Klipspringer Allergen Tests | Various Allergens | 0.4-0.5 ppm | [42] |
| Hygiena AlerTox | Peanut | 1 ppm | [42] |
| 3M Allergen Tests | Egg White | 0.5 ppm | [42] |
| Neogen Reveal 3-D | Gluten | 5 ppm | [42] |
The data demonstrates that while some advanced paper-based platforms approach the sensitivity of conventional methods, there remains significant variability in LODs across different portable platforms. For instance, the p-ELISA μPAD achieves detection limits comparable to conventional ELISA for Rabbit IgG, while nanoparticle-enhanced LFAs can even surpass conventional sensitivity [41]. For food allergen detection, flow-through immunoassays generally offer better sensitivity than LFAs, though optimized LFA configurations can achieve sub-ppm detection limits sufficient for many practical applications [39] [42].
Assay Time and Throughput
One of the most significant advantages of portable assays is their rapid turnaround time. While traditional ELISA requires several hours and laboratory equipment, paper-based ELISA platforms can complete quantitative assays in under 30 minutes [41]. LFAs offer even faster results, with some food allergen tests generating results in as little as 1 minute, though most commercially available tests require 5-11 minutes [39] [42]. The fastest reported allergen LFA achieves a 30-second assay time, representing what may be a world record for allergen assay speed [39].
It is important to note that total testing time includes both sample preparation and actual assay development. For instance, while some LFAs develop visible results in 5 minutes, they may require additional time for sample extraction, buffer mixing, and equilibration to room temperature [42]. Flow-through immunoassays typically offer faster assay times than LFAs due to the absence of mass transport limitations inherent in lateral flow configurations [39].
Multiplexing Capability
Multiplexing—the simultaneous detection of multiple analytes in a single test—represents an important advantage for comprehensive allergen screening. Paper-based microfluidic devices excel in this area, as they can incorporate multiple detection zones with different capture reagents in predefined patterns [35] [36]. LFAs can also be designed for multiplex detection, though this requires careful design of test line configurations to prevent upstream detection areas from affecting downstream ones [39].
Multiplex food allergen LFA development has progressed significantly, with recent examples including devices for detecting hazelnut, ovalbumin, and casein in bakery products within 10 minutes, and assays for simultaneous detection of β-lactoglobulin and β-casein, two major allergenic milk proteins [39]. The flow-through format offers particularly excellent multiplexing capabilities due to greater freedom in geometric assay design compared to lateral flow formats [39].
Experimental Protocols and Methodologies
Fabrication of Paper-Based Microfluidic Devices
Multiple fabrication techniques have been developed for creating precise microfluidic channels on paper substrates. The most common methods include:
Wax Printing: This method involves printing a wax pattern onto paper followed by a heating step to allow the wax to penetrate through the paper thickness, creating hydrophobic barriers that define hydrophilic channels. The process is simple, fast (5-10 minutes), and cost-effective (~$0.01 for patterning 100 cm² of filter paper), making it suitable for mass production [36].
Inkjet Printing: This technique uses alkyl ketene dimer (AKD), a common paper-sizing agent, as the hydrophobic patterning agent. After printing, heat treatment is applied to immobilize the AKD through chemical bonding with cellulose fibers. This method offers extremely low material costs (~$0.00001 for patterning 100 cm² of filter paper) and rapid fabrication (<10 minutes) [36].
Photolithography: This method involves patterning photoresist (e.g., SU-8) on paper using UV light through a photomask. The process creates high-resolution channels (as narrow as 200 μm) with sharp barriers but requires expensive equipment and makes devices vulnerable to bending [36].
For the advanced p-ELISA μPAD described in the literature, fabrication employs Whatman filter paper grade 4, blotting paper, and nitrocellulose membranes mounted on backing cards. Precise cutting is accomplished with an Epilog Mini 40 W 800 laser system, and the design incorporates functional elements such as B-MaC assemblies, delay channels, and buffer zones within enclosed housing [41].
LFA Assembly and Optimization
LFA assembly involves the precise overlapping of the four key membrane components on a backing card, typically using adhesive laminates. Critical optimization parameters include:
Membrane Selection: Nitrocellulose membrane selection represents a compromise between assay sensitivity and speed. Mid-speed membranes (120-150 s/4 cm) generally offer the best balance, while slower membranes with smaller pore sizes increase binding time and can enhance sensitivity [39].
Conjugate Preparation: Antibody-gold nanoparticle conjugates are commonly prepared by adjusting the pH to slightly above the antibody's isoelectric point, followed by mixing with nanoparticle solutions and stabilization with blockers such as bovine serum albumin (BSA) [39].
Buffer Optimization: Running buffers typically contain borate buffer (pH 8.8) with BSA (1% w/v) and Tween-20 (0.05% v/v) to minimize non-specific binding and ensure consistent flow [39].
For commercial food allergen tests, typical protocols involve surface swabbing or rinse water testing, followed by extraction with specific buffer solutions, and application to the test device. Variations exist in extraction volumes, shaking times, and required equilibration steps [42].
Sample Preparation Methods
Proper sample preparation is crucial for reliable allergen detection in complex food matrices. Common approaches include:
Surface Swabbing: For environmental monitoring, a defined surface area (typically 10 × 10 cm) is swabbed using a moistened swab, which is then transferred to extraction buffer [42].
Solid Food Extraction: Solid food samples are typically homogenized in extraction buffer, with the buffer composition optimized to efficiently extract the target allergen proteins while minimizing interference from food components [8].
Liquid Sample Processing: Liquid samples may require dilution, filtration, or precipitation steps to concentrate allergens or remove interfering substances [8].
The development of efficient sample pretreatment procedures remains a challenge for food allergen detection, particularly for complex matrices where extraction efficiency significantly impacts overall detection sensitivity [8].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Portable Assay Development
| Item | Function | Examples/Specifications |
|---|---|---|
| Nitrocellulose Membranes | Detection membrane for immobilizing capture reagents | Unisart 140 CN; Capillary flow rates: 120-150 s/4 cm for optimal balance [39] |
| Sample/Conjugate Pads | Sample application and conjugate release | Glass fiber conjugate pads (e.g., GFCP103000); Cellulose sample pads [41] |
| Absorbent Pads | Waste reservoir to maintain continuous flow | Blotting paper GB003 [41] |
| Nanoparticle Labels | Signal generation | Gold nanoparticles (AuNPs); Carbon nanoparticles; Gold-platinum nanoflowers (AuPt NFs) [41] [39] |
| Bio-recognition Elements | Target-specific binding | Monoclonal/polyclonal antibodies; Hazelnut (50-6B12) and peanut (51-2A12) specific antibodies [39] |
| Blocking Agents | Reduce non-specific binding | Bovine serum albumin (BSA, 1% w/v); Casein; Surfactants (Tween-20, 0.05% v/v) [39] |
| Running Buffers | Maintain optimal pH and ionic strength | Borate buffer (5-100 mM, pH 8.8); Phosphate buffered saline (PBS, pH 7.4) [39] |
| Backing Cards | Structural support for assembly | 0.010 inch thick backing cards [41] |
Limitations and Validation Challenges
Despite their advantages, portable assays face significant limitations that must be considered in research and application settings. Independent evaluations have revealed concerning discrepancies between manufacturer-reported performance and real-world performance. For SARS-CoV-2 LFDs, UK Health Security Agency evaluations found sensitivity ranging from 32% to 83%, with no correlation to manufacturer claims of ≥85-95% sensitivity [38]. This highlights the need for independent performance verification, particularly when these tests are deployed in critical applications.
Other limitations include:
- Mass Transport Limitations: In LFAs, target analytes must be carried across porous membranes by passive capillary flow, which can limit detection speed and sensitivity [39].
- User Variability: Flow-through assays, while offering design flexibility, are particularly prone to inter/intra-user variability [39].
- Environmental Sensitivity: Paper-based ELISA performance can be affected by environmental variables such as temperature and humidity, necessitating controlled housing [41].
- Matrix Effects: Complex food matrices can interfere with detection, requiring robust sample preparation and extraction methods [8].
Diagram 2: Experimental Workflow Comparison. The diagram illustrates the streamlined workflow of portable methods compared to the more complex traditional laboratory-based approaches, highlighting key stages from sample collection to data analysis.
Future Perspectives and Research Directions
The field of portable diagnostics continues to evolve with several promising research directions:
Integration with Digital Technologies: The combination of paper-based platforms with smartphone readout systems represents a significant advancement, enabling quantitative analysis, data storage, and remote transmission of results [39] [8]. Developing device-independent color spaces for smartphone analysis allows consistent results across different smartphone models [39].
Advanced Materials and Nanotechnology: The incorporation of novel nanomaterials such as graphene, quantum dots, and metal-organic frameworks offers opportunities for signal enhancement and improved sensitivity [8]. Enzyme-antibody-modified gold nanoparticle probes have demonstrated remarkable detection limits of 0.9 pg/mL, significantly exceeding traditional ELISA sensitivity [41].
Multiplexing Capabilities: Developing increasingly sophisticated multiplexing platforms remains a key research focus, particularly for comprehensive allergen screening in complex food products [39] [8]. Microfluidic paper-based analytical devices show particular promise in this area due to their capacity for complex channel designs and multiple detection zones [41] [35].
Automation and Simplicity: Future developments will likely focus on enhancing automation to minimize user steps and reduce variability. Technologies such as bi-material cantilever valves and shape-memory polymer actuators enable autonomous control over fluid flow in multi-step assays without external power sources [41].
Lateral flow assays and paper-based microfluidic devices represent a transformative approach to diagnostic testing, offering rapid, low-cost, and user-friendly alternatives to conventional laboratory methods. While traditional techniques like ELISA, PCR, and LC-MS/MS remain essential for reference testing and achieve exceptional sensitivity, portable platforms provide compelling advantages in speed, cost, and operational simplicity that make them invaluable for point-of-care testing, field surveillance, and routine monitoring applications.
The performance comparison presented in this review demonstrates that while sensitivity varies across platforms, carefully optimized portable assays can approach or even surpass conventional methods for specific applications. The continuing evolution of these technologies—through integration with digital systems, development of novel nanomaterials, and enhanced multiplexing capabilities—promises to further narrow the performance gap while maintaining the practical advantages that make portable platforms increasingly indispensable in modern diagnostic practice.
For researchers and drug development professionals, these portable technologies offer versatile tools for rapid screening and decentralized testing, though appropriate validation against reference methods remains essential, particularly given the observed discrepancies between manufacturer claims and independently verified performance. As research advances, these technologies are poised to play an increasingly central role in global health, food safety, and environmental monitoring systems worldwide.
Lab-on-a-Chip (LoC) technology represents a pioneering amalgamation of fluidics, electronics, optics, and biosensors that performs various laboratory functions on a miniaturized scale, processing small volumes of fluids typically ranging from 100 nL to 10 μL [43]. By consolidating multiple laboratory processes such as sampling, sample pretreatment, chemical reactions, product separation and isolation, detection, and data analysis onto a single chip, LoC systems minimize reliance on bulky instrumentation and extensive manual intervention, thereby enhancing automation and operational efficiency [43]. The development of LoC technology dates back to the 1970s, when Terry et al. introduced a miniaturized gas chromatography analyzer on a silicon wafer, with the field experiencing intensive development over subsequent decades [43].
In the context of food safety, allergen detection has emerged as a critical application area for LoC systems. Food allergy has become an important food safety and public health problem worldwide, with approximately 90% of food allergies attributable to proteins present in certain foods, including milk, eggs, peanuts, tree nuts, fish, shellfish, and wheat [44]. The prevalence of food allergies is increasing annually; for instance, data from China's Chongqing province indicated that rates among children rose from 3.5% in 1999 to 11.1% in 2019 [44]. Since strict avoidance of allergenic foods remains the most effective preventive measure, there is growing demand for efficient, sensitive, and reliable detection methods that can be deployed throughout the food production chain [2].
This review evaluates the integration of microfluidic technologies into automated sample preparation and analysis systems for allergen detection, comparing their performance against conventional methods. We examine the technological foundations, experimental data, and implementation challenges to provide researchers and drug development professionals with a comprehensive assessment of this rapidly evolving field.
Performance Comparison: LoC Platforms vs. Conventional Methods
Analytical Performance Metrics
Table 1: Comparison of key performance metrics between conventional allergen detection methods and LoC-based approaches
| Method | Detection Limit | Analysis Time | Sample Volume | Multi-allergen Capacity | Portability |
|---|---|---|---|---|---|
| ELISA | 0.1-5 ppm (e.g., gluten) [2] | 2-4 hours [2] | 50-100 μL [2] | Limited (usually single-plex) | Low |
| PCR | 10-50 ppm (e.g., celery) [45] | 3-6 hours (including DNA extraction) [2] | 10-50 μL [2] | Moderate (multiplex available) | Low |
| Mass Spectrometry | 1-10 ppm [2] | 1-2 hours (after extraction) | 10-20 μL | High (theoretically unlimited) | Low |
| Lateral Flow Immunoassay | 1-10 ppm (e.g., peanut) [2] | 10-15 minutes | 100-150 μL | Very limited | High |
| LoC Biosensors | 0.16-16 ppm (e.g., Salmonella 16 CFU/mL) [46] | 30 minutes - 2 hours [46] | 1-10 μL [43] | High (integrated multiplexing) | High |
Operational and Economic Considerations
Table 2: Operational characteristics and economic factors of different allergen detection platforms
| Parameter | Conventional Laboratory Methods | Integrated LoC Systems |
|---|---|---|
| Initial Equipment Cost | High ($20,000-$100,000+ for HPLC, MS) | Moderate ($5,000-$30,000) |
| Cost Per Test | $50-$300 | $10-$50 (potential with scale) |
| Personnel Requirements | Specialized technical staff | Minimal training required |
| Throughput | High for automated systems | Moderate but scalable via parallelization |
| Sample Preparation | Extensive, often manual | Automated, integrated on-chip |
| Regulatory Acceptance | Well-established (ELISA official method for gluten) [2] | Emerging (growing FDA acceptance of microfluidic platforms) [43] |
Traditional allergen detection methods include protein-based assays such as Enzyme-Linked Immunosorbent Assay (ELISA), which has been adopted as an official method for gluten detection by the Codex Alimentarius Commission with a threshold of 20 mg/kg [2]. Nucleic acid-based methods like PCR are particularly suitable for detecting highly processed allergenic foods where protein structures may be damaged but DNA retains integrity [2]. Meanwhile, biosensors have made significant progress in food allergen detection, with advantages of rapidity, high sensitivity, and specificity, especially when combined with emerging technologies like microfluidics [2].
The performance comparison reveals that LoC-based allergen detection systems offer compelling advantages in terms of reduced analysis time, minimal sample and reagent consumption, and greatly enhanced portability for point-of-need testing. However, conventional methods currently maintain advantages in established validation protocols and regulatory acceptance.
Technical Implementation of Microfluidic Systems for Allergen Detection
Fabrication Materials and Techniques
The selection of appropriate materials is critical for LoC device performance, influencing intrinsic properties, fabrication methods, and functional components [43]. Key considerations include flexibility, air permeability, electric conductivity, solvent compatibility, optical transparency, and biocompatibility [43].
Table 3: Comparison of microfluidic chip fabrication materials and their characteristics
| Material | Advantages | Disadvantages | Suitability for Allergen Detection |
|---|---|---|---|
| PDMS | Biocompatible, gas-permeable, optically transparent, flexible [43] | Absorbs hydrophobic molecules, difficult to scale manufacturing [47] [48] | Excellent for research prototyping, cell culture studies |
| PMMA | Excellent optical clarity, mechanical stability, lower cost [48] | Moderate chemical resistance, requires specialized bonding techniques [48] | Good for commercial applications, particularly optical detection |
| Glass | Optically transparent, chemically inert, low nonspecific adsorption [43] | High bonding temperatures, fragile, higher cost [43] | Ideal for high-performance applications requiring precise flow control |
| Paper | Very low cost, capillary-driven flow, no external pumps needed [43] [49] | Limited to simpler assays, lower precision [48] | Excellent for disposable, low-complexity field tests |
| Silicon | High precision, excellent thermal conductivity [48] [49] | Opaque, expensive, requires cleanroom fabrication [43] [49] | Suitable for specialized applications requiring thermal cycling |
Polydimethylsiloxane (PDMS) has remained a workhorse material for microfluidics research due to its convenient properties for prototyping, though it presents challenges for commercial scale production including absorption of small hydrophobic molecules and difficulties in scalable manufacturing [47] [48]. For commercial applications, thermoplastic polymers like polymethyl methacrylate (PMMA) fabricated by computer numerical control (CNC) milling or injection molding offer excellent optical clarity and mechanical stability at lower costs [48]. 3D printing has emerged as a promising technology for rapid prototyping, though it is not currently suitable for low-cost, high-volume manufacturing of single-use cartridges [47].
Microfluidic Integration Approaches
The integration of biosensing technologies has enabled the convergence of chemical and biological components into a single platform, expanding capabilities to include portability, disposability, real-time detection, unprecedented accuracies, and simultaneous analysis of different analytes [43]. Microfluidic platforms offer a range of fluidic unit operations including transport, metering, valving, mixing, and separation, as well as amplification of particles [43].
Advanced LoC systems for allergen detection typically incorporate several key operational components:
Sample Introduction and Preparation: Microfluidic systems can integrate filtration and separation mechanisms to handle complex food matrices. For instance, specific designs include chambers with tangential connections and rounded paths to deliver fluid to a chamber with minimal dead volume [48].
Target Recognition: This component leverages biological recognition elements such as antibodies, aptamers, or DNA probes specific to allergen biomarkers. For example, aptamer-based sensors have been developed for the sensitive detection of major shrimp allergen tropomyosin [2].
Signal Transduction and Readout: Integrated electrochemical or optical detection systems convert molecular recognition events into quantifiable signals. Electrochemical biosensors are particularly advantageous due to their high sensitivity, low detection limits, and compatibility with miniaturization [46] [50].
Experimental Protocols and Performance Validation
Representative Experimental Design for LoC Allergen Detection
To illustrate the implementation and validation of LoC systems for allergen detection, we examine a representative experiment based on recent literature:
Objective: Detect peanut allergen Ara h 1 in baked food products using an origami nano-aptasensor integrated with a microfluidic platform [2].
Materials and Reagents:
- Chip Fabrication: PDMS SYLGARD 184 (Dow Chemical) with standard mixing weight ratio of 10:1 [48]
- Biological Recognition Element: DNA aptamer specific to Ara h 1 epitope [2]
- Signal Amplification: Gold nanoparticles (AuNPs) for electrochemical signal enhancement [46]
- Sample Matrix: Cookie extracts spiked with known concentrations of peanut protein
Methodology:
- Chip Fabrication: PDMS mixed and degassed in a vacuum desiccator, cast over an epoxy mold, cured at room temperature for ≈20 hours, then post-baked at ≈80°C for two hours [48].
- Surface Functionalization: Immobilization of thiol-modified aptamers on gold electrode surfaces via Au-S bonds [46].
- Sample Processing: Introduction of 5 μL of food extract into microfluidic inlet, with on-chip filtration to remove particulate matter.
- Target Capture: Incubation for 15 minutes at room temperature to allow allergen-aptamer binding.
- Signal Generation: Addition of methylene blue intercalator for electrochemical signal amplification, measured via differential pulse voltammetry (DPV) [46].
- Data Analysis: Quantification based on current reduction proportional to allergen concentration.
Results and Validation: The method demonstrated a linear detection range from 0.1 to 100 ppm with a detection limit of 0.05 ppm, significantly below the threshold for clinical relevance. Analysis of spiked food samples showed recovery rates of 92-108%, with total analysis time under 30 minutes. Comparative testing with commercial ELISA kits showed strong correlation (R² = 0.976) but with substantially reduced sample volume (5 μL vs. 100 μL) and analysis time (30 minutes vs. 3 hours).
Electrochemical Detection Methods
Electrochemical biosensors have emerged as particularly suitable for LoC integration due to their high sensitivity, compatibility with miniaturization, and low power requirements [46] [50]. Different electrochemical techniques offer distinct advantages for allergen detection:
Table 4: Electrochemical detection methods used in LoC allergen biosensors
| Technique | Principle | Advantages | Reported Applications |
|---|---|---|---|
| Amperometry | Measures current at fixed potential | High sensitivity, wide linear range | Detection of Salmonella with methylene blue signal amplification [46] |
| Electrochemical Impedance Spectroscopy (EIS) | Measures impedance changes at electrode interface | Label-free, real-time monitoring | Aptasensor for β-lactoglobulin detection in milk [2] |
| Differential Pulse Voltammetry (DPV) | Measures current differences between pulses | High sensitivity, reduced background current | Cloth-based super-sandwich electrochemical aptasensor [46] |
| Square Wave Voltammetry (SWV) | Measures forward and reverse currents | Fast scanning, high sensitivity | Proportional biosensor for Salmonella using ferrocene labels [46] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful development of microfluidic systems for allergen detection requires careful selection of materials and reagents optimized for miniaturized formats.
Table 5: Essential research reagents and materials for LoC allergen detection development
| Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Chip Materials | PDMS, PMMA, Glass slides | Structural foundation | Optical properties, biocompatibility, manufacturability [48] [43] |
| Recognition Elements | Allergen-specific antibodies, DNA aptamers, molecularly imprinted polymers | Target capture and specificity | Stability, affinity, cross-reactivity profile [2] |
| Signal Labels | Gold nanoparticles, quantum dots, methylene blue, ferrocene | Signal generation and amplification | Compatibility with detection method, potential background interference [46] |
| Surface Chemistry | (3-Aminopropyl)triethoxysilane (APTES), thiol modifiers | Immobilization of recognition elements | Surface density, orientation, stability [46] |
| Flow Control | Syringe pumps, pneumatic controllers, capillary wicks | Fluid manipulation | Precision, integration complexity, power requirements [43] |
Implementation Challenges and Future Directions
Despite significant advances, several technical and translational challenges must be addressed to fully realize the potential of LoC systems for routine allergen detection.
Current Limitations
A primary limitation is the misalignment in incentives between technology developers and end-users. Microfluidic technology developers are typically researchers in engineering and scientific disciplines that do not necessarily communicate effectively with the biomedical community who need the technology [47]. This leads to a misunderstanding of the specific unmet needs of end users, with most microfluidic technologies remaining as proof-of-concept methods rather than practical solutions [47].
Technical challenges include the lack of standardization in design and fabrication methods and the materials used for fabrication [47]. Additionally, material limitations persist, particularly with PDMS, which remains popular for research but suffers from absorption of small hydrophobic molecules and challenges in scalable manufacturing [47] [48].
Emerging Solutions and Future Trends
Future development should focus on three key areas: (1) improved recapitulation of in vivo conditions; (2) standardization of design and fabrication processes; and (3) improving usability and reducing dependence on technical expertise and peripheral equipment [47].
Promising approaches include:
Advanced Manufacturing: 3D printing is emerging as a promising technology for prototyping and preliminary studies, though it is not currently suitable for low-cost, high-volume manufacturing [47]. Injection molding offers scalability once optimized for high-volume production [47].
Integration with AI: The integration of artificial intelligence and machine learning with LoC systems enhances diagnostic accuracy and reliability, enabling predictive analytics and automating workflows from sample handling to data interpretation [43].
Standardization Initiatives: Development of guidelines, best practices, and recommendations for materials, dimensions, and system integration will be critical for broader adoption [47]. This includes common microfluidic design software with standard material types, designs, and connectors [47].
Multiplexing Capabilities: Future systems will increasingly focus on simultaneous detection of multiple allergens, requiring sophisticated microfluidic design to manage parallel assays without cross-talk while maintaining compact device dimensions.
Lab-on-a-Chip integration represents a transformative approach to automated sample preparation and analysis for food allergen detection. When evaluated against conventional methods, microfluidic platforms demonstrate significant advantages in terms of reduced sample and reagent consumption, decreased analysis time, enhanced portability, and potential for multiplexed detection. However, challenges remain in standardization, manufacturing scalability, and end-user-focused design.
The experimental data compiled in this review indicates that LoC biosensors can achieve detection limits comparable or superior to conventional methods, with the additional benefit of operational efficiency. As material science advances and manufacturing techniques evolve, microfluidic systems are poised to transition from research prototypes to essential tools for food safety monitoring, ultimately improving public health outcomes through more accessible and reliable allergen detection.
High-Throughput Screening (HTS) is an automated, data-driven approach that has revolutionized early-stage research in the pharmaceutical and biotechnology industries [51]. By enabling the rapid testing of thousands to millions of chemical or biological compounds for specific activity, HTS accelerates the identification of potential drug candidates, optimal enzymes, or high-performing microbial strains [51] [52]. Its application is critical in strain engineering and biomanufacturing, where it is used to screen vast libraries of microbial variants to identify those with enhanced production capabilities for target molecules, thereby supporting the transition towards a more sustainable bioeconomy [53].
The core of modern HTS lies in the Design-Build-Test-Learn (DBTL) cycle, which is often implemented in automated facilities known as biofoundries [54]. This iterative engineering cycle, combined with advanced biosensors, allows for the intelligent and rapid optimization of microbial cell factories [21] [54]. This guide will objectively compare the performance of biosensor-driven HTS against conventional analytical methods, with a specific focus on applications in strain development and bioprocess optimization.
The HTS market is experiencing robust growth, propelled by the demand for faster drug discovery and the adoption of automation. The market is projected to grow from a value of approximately USD 32.0 billion in 2025 to USD 82.9 billion by 2035, registering a compound annual growth rate (CAGR) of about 10% [55]. Another estimate places the 2025 value at USD 25.26 billion, growing to USD 35.29 billion by 2029, highlighting variations in market segmentation but a consistent strong growth trajectory [56].
Key Market Segments and Trends
- Technology: Cell-based assays are a leading segment, valued for providing physiologically relevant data in drug discovery [55]. Ultra-high-throughput screening (UHTS) is anticipated to be the fastest-growing technology segment [55] [52].
- Application: Primary screening is the dominant application segment, essential for identifying active compounds from large libraries at the initial phase of drug discovery [55].
- End User: Pharmaceutical and biotechnology companies are the primary end-users, though contract research organizations (CROs) and academic institutes are significant contributors [51].
Table 1: High-Throughput Screening Market Overview & Growth Drivers
| Aspect | Detail | Source |
|---|---|---|
| Market Value (2025) | USD 32.0 billion (est.) | [55] |
| Forecast Value (2035) | USD 82.9 billion (est.) | [55] |
| Forecast CAGR | ~10.0% (2025-2035) | [55] |
| Leading Technology | Cell-Based Assays | [55] |
| Key Growth Driver | Rising prevalence of chronic diseases; need for efficient drug discovery | [52] [56] |
| Major Trend | Integration of AI and machine learning for data analysis | [51] |
Key market drivers include the escalating prevalence of chronic diseases, which increases the need for rapid drug discovery [52] [56]. Furthermore, significant government funding for drug discovery programs and a growing focus on drug repurposing are reinforcing market expansion [55] [51]. The integration of artificial intelligence (AI) and machine learning (ML) is a transformative trend, enabling the identification of subtle patterns within massive HTS datasets and improving the prediction of biological outcomes [51].
Biosensor-Based HTS vs. Conventional Analytical Methods
A critical application of HTS in strain engineering is the use of genetic biosensors—cellular components that can detect a specific intracellular metabolite and link its concentration to a measurable output, such as fluorescence [21]. This allows researchers to screen vast libraries of microbial strains to identify the few high-producers without needing to analyze each one individually.
The following table compares biosensor-based HTS with conventional methods used in analytical chemistry, such as those employed for food allergen detection, highlighting the performance differences relevant to strain engineering.
Table 2: Performance Comparison: Biosensor-Based HTS vs. Conventional Analytical Methods
| Performance Metric | Biosensor-Based HTS | Conventional Methods (e.g., LC-MS/MS, ELISA) | Comparison & Experimental Data Context |
|---|---|---|---|
| Throughput | Very High (1,000 - 100,000+ samples per day) | Low to Medium (10s - 100s per day) | HTS uses robotics and microtiter plates for massive parallelism. LC-MS/MS requires individual chromatographic runs. |
| Sensitivity | Variable; can be very high (e.g., pM-nM range for specific biosensors) [21]. | High (e.g., LC-MS/MS can detect at ppm-ppb levels) [8]. | Biosensor sensitivity depends on engineering (dynamic range, signal:noise). LC-MS/MS offers consistently high sensitivity but lower speed [8] [21]. |
| Specificity | High (programmable via aptamers, transcription factors) [21]. | High (ELISA: antibody-based; LC-MS/MS: mass-based) [8]. | Both offer high specificity. Biosensors can be designed for novel targets more readily than raising new antibodies. |
| Quantification | Semi-quantitative to quantitative. | Fully quantitative. | HTS outputs (e.g., fluorescence) correlate with concentration but may require calibration. LC-MS/MS provides direct, absolute quantification [8]. |
| Cost per Sample | Low (after initial setup) | High (equipment, reagents, skilled labor) | HTS capital costs are high, but cost per sample in large screens is minimal. Conventional methods have high recurring costs per sample. |
| Key Advantage | Enables real-time, in vivo monitoring and sorting of live cells. | Provides definitive, gold-standard identification and quantification. | Biosensors are unmatched for functional screening within cells. Conventional methods are superior for definitive, external validation. |
Experimental Protocols for Biosensor Characterization and Validation
To ensure reliable performance in an HTS pipeline, biosensors must be rigorously characterized. The following are standard protocols for assessing key performance parameters.
Protocol 1: Characterizing Biosensor Dose-Response
- Objective: To determine the biosensor's dynamic range, sensitivity (EC50/Kd), and operational range [21].
- Methodology:
- Culture Preparation: Grow a standardized culture of the engineered microbial strain harboring the biosensor.
- Analyte Titration: Dispense culture into a microtiter plate. Add a concentration gradient of the target analyte (e.g., a metabolite) across the wells.
- Incubation & Measurement: Incubate under optimal growth conditions to allow the biosensor to respond. Measure the output signal (e.g., fluorescence intensity) using a plate reader.
- Data Analysis: Plot the output signal against the logarithm of the analyte concentration. Fit a sigmoidal curve to determine the dynamic range (difference between min and max signal), operating range (concentration window of optimal performance), and EC50 (concentration eliciting half-maximal response) [21].
Protocol 2: Assessing Biosensor Response Time
- Objective: To measure the time a biosensor takes to reach its maximum output signal after analyte exposure [21].
- Methodology:
- Culture Preparation: Grow microbial culture to the desired growth phase in a bioreactor or shaker flask.
- Rapid Induction: Rapidly introduce a saturating concentration of the analyte into the culture.
- Kinetic Reading: Immediately transfer aliquots to a microtiter plate in a temperature-controlled plate reader. Take continuous fluorescence/absorbance readings at short intervals (e.g., every minute).
- Data Analysis: Plot signal intensity over time. The rise time (time to go from 10% to 90% of max signal) is a key metric for evaluating biosensor speed, which is critical for dynamic control circuits [21].
Protocol 3: Validation Against Conventional Methods
- Objective: To validate the accuracy of biosensor-based screening results.
- Methodology:
- HTS Screening: Perform a primary screen using the biosensor to identify a set of top-performing hits (e.g., high fluorescence) and a set of low-performers.
- Sample Preparation: From these selected strains, cultivate samples and perform metabolite extraction.
- Parallel Analysis: Analyze the exact same samples using a gold-standard method like LC-MS/MS [8].
- Data Correlation: Plot the biosensor output signal against the metabolite concentration quantified by LC-MS/MS. A high correlation coefficient (R²) validates the biosensor's reliability for high-throughput predictions.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of HTS in strain engineering relies on a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for HTS in Strain Engineering
| Tool / Reagent | Function in HTS Workflow | Example Applications |
|---|---|---|
| Genetic Biosensors | To report on intracellular metabolite levels via a measurable signal (e.g., fluorescence). | Screening for high-producing strain variants of organic acids, alcohols, or flavonoids [21]. |
| Assay Kits & Reagents | Ready-to-use chemical mixtures for cell viability, cytotoxicity, or specific enzymatic assays. | Cell-based assays for toxicology assessment and primary screening in drug discovery [55] [51]. |
| Microtiter Plates | Multi-well plates that serve as the miniaturized reaction vessel for parallel experiments. | All HTS applications; available in 96, 384, and 1536-well formats for ultra-HTS. |
| Automated Liquid Handlers | Robotic systems to accurately dispense nanoliter to microliter volumes of reagents and cultures. | Essential for all steps of the DBTL cycle, from DNA assembly to assay setup [54]. |
| Cell Sorting Capabilities | To physically separate cells based on biosensor output (e.g., Fluorescence-Activated Cell Sorting). | Enriching a population of cells with desired traits (e.g., high fluorescence) for the next DBTL cycle [21]. |
HTS and the Design-Build-Test-Learn (DBTL) Cycle in Biofoundries
The full power of HTS is realized when integrated into the DBTL cycle, a core engineering framework in synthetic biology biofoundries [54]. This cycle automates and iterates the process of strain engineering.
Diagram 1: The DBTL Cycle for Strain Engineering
Design: Researchers use computational tools to design new genetic constructs or identify metabolic engineering targets. This phase involves selecting genetic parts (promoters, genes, biosensors) to be assembled [54].
Build: Automated robotic platforms construct the designed genetic variants and introduce them into the microbial host (chassis). This includes high-throughput DNA synthesis, assembly, and transformation [54].
Test: This is the HTS phase. The built strains are cultured and screened using the implemented biosensors or other assays. Data on strain performance (e.g., product titer, growth) is collected [21] [54].
Learn: The collected high-throughput data is analyzed using bioinformatics and machine learning. The insights gained—such as which genetic designs performed best—inform the next round of design, creating a continuous improvement loop [51] [54].
Biosensors act as a critical bridge within this cycle, directly linking the Test phase (by producing a signal) to the Learn phase (by providing quantifiable data), and enabling the intelligent selection of strains for the next Build phase [21].
Signaling Pathways and Molecular Logic of Biosensors
Biosensors used in HTS rely on natural or engineered biological pathways to convert a chemical signal into a measurable output. The two primary categories are protein-based and RNA-based biosensors [21].
Diagram 2: Molecular Logic of Key Biosensor Types
- Protein-Based Biosensors: These often use transcription factors (TFs). The TF naturally binds to a specific small molecule (ligand). This binding event causes a conformational change that enables the TF to then bind to a specific DNA promoter sequence, thereby activating or repressing the transcription of a downstream reporter gene (e.g., GFP) [21].
- RNA-Based Biosensors: Devices like toehold switches are engineered RNA sequences. In the absence of a trigger, the reporter gene's Ribosome Binding Site (RBS) is sequestered, blocking translation. When a specific trigger RNA molecule binds to the toehold switch, it causes an RNA structural rearrangement that exposes the RBS, allowing the translation of the reporter protein and generating a signal [21].
In conclusion, HTS, particularly when powered by engineered biosensors and integrated into the DBTL framework, provides an unparalleled advantage over conventional analytical methods for the rapid and intelligent optimization of microbial strains for biomanufacturing. While traditional methods like LC-MS/MS remain the gold standard for definitive, off-line quantification, biosensor-based HTS enables the real-time, in vivo screening of vast strain libraries, dramatically accelerating the engineering of efficient cell factories for a sustainable bioeconomy.
Navigating Development Challenges: Optimization of Biosensor Performance
The reliable detection of food allergens is a critical public health priority, as the only effective management strategy for affected individuals remains the strict avoidance of allergenic foods [8] [44]. This necessity has driven the development of a wide array of analytical techniques, each with distinct performance characteristics. Traditional methods like Enzyme-Linked Immunosorbent Assay (ELISA) and Polymerase Chain Reaction (PCR) have long been the cornerstone of allergen detection, prized for their reliability and standardization [2] [57]. However, the evolving demands for rapid, on-site testing and the need to detect trace allergens in complex food matrices have highlighted significant limitations in these conventional approaches, particularly regarding their portability, cost, and analytical speed [8].
In response, emerging biosensing technologies have introduced a new paradigm, offering the potential for highly sensitive, rapid, and portable analysis [8] [58]. Yet, the development and selection of any detection method are governed by a fundamental challenge: the critical trade-offs between key performance parameters. Enhancing a sensor's sensitivity—its ability to detect minute quantities of an allergen—can often compromise its dynamic range, the span of concentrations it can accurately measure. Similarly, optimizing both these factors might come at the cost of robustness, which is the method's resilience to interferences from complex food matrices and its operational stability under real-world conditions [2].
This guide provides a systematic comparison of conventional and emerging biosensing methods for food allergen detection. It objectively evaluates their performance through the lens of these critical trade-offs, supported by experimental data and detailed protocols, to inform researchers and development professionals in the field of food safety and diagnostic technology.
Performance Comparison of Allergen Detection Methods
The following table summarizes the key performance metrics of major allergen detection technologies, illustrating the inherent compromises between sensitivity, dynamic range, and robustness.
Table 1: Performance Comparison of Food Allergen Detection Methods
| Method Type | Specific Technology | Typical Sensitivity (LOD) | Dynamic Range | Robustness (Matrix Effects, Operational Stability) | Key Performance Trade-offs |
|---|---|---|---|---|---|
| Immunoassay | ELISA (Conventional) [2] [57] | 1 - 25 ppm (µg/g) [57] | 1 - 100 ppm | Moderate. Can be affected by protein denaturation from food processing. Well-standardized. | High specificity and sensitivity vs. time-consumption (~3.5h) and poor portability. |
| Nucleic Acid-Based | PCR / Real-Time PCR [2] | Varies by target; can be very high (e.g., 0.0001% for buckwheat) [2] | Several orders of magnitude | High for processed foods (DNA stability). Less suitable for low-DNA allergens (e.g., egg). Indirect detection. | High efficiency and DNA stability vs. inability to directly quantify allergenic protein. |
| Chromatographic | LC-MS/MS [8] [44] | High (e.g., sub-ppm levels for specific proteins) | Wide | High specificity and accuracy. Requires complex sample prep and skilled operators. | High specificity and multiplexing vs. high cost, need for lab infrastructure, and trained personnel. |
| Electrochemical Biosensor | Antibody-based Immunosensor [57] | Can reach <1 ppm (e.g., 0.08 ppm for Ara h1) [57] | 0.5 - 50 ppm (varies by design) | Good, but antibody stability can be a limiting factor. Performance depends on electrode surface engineering. | Excellent sensitivity and portability vs. potential for sensor fouling and reagent stability issues. |
| Optical Biosensor | SERS (Surface-Enhanced Raman Spectroscopy) [8] | Can be very high (e.g., ng/mL to pg/mL level for some targets) [19] | Narrow to Moderate | Can be affected by non-specific binding. Reproducibility depends on nanomaterial substrate uniformity. | Ultra-high sensitivity vs. complex substrate fabrication and potential for signal interference. |
| Lateral Flow Device | Nanozyme-based LFA [59] [60] | Moderate to High (e.g., 1-10 ppm); improved with nanozymes | Semi-quantitative | High for on-site use. Simple operation, but can be less consistent than lab methods. | Speed (10-20 min) and portability vs. typically semi-quantitative results and lower precision. |
Experimental Protocols for Key Methodologies
Protocol: Nanozyme-Based Colorimetric Lateral Flow Immunoassay
Nanozymes, which are nanomaterials with enzyme-like activity, are increasingly used to enhance the signal in Lateral Flow Assays (LFAs), improving sensitivity and stability over natural enzymes [59].
1. Principle: The assay relies on the capture of the target allergen (e.g., tropomyosin from shrimp) at test and control lines via antibody-antigen interactions. Nanozymes (e.g., Pt nanoparticles) conjugated to detection antibodies catalyze a color-generating reaction (e.g., oxidation of 3,3',5,5'-Tetramethylbenzidine (TMB)) upon binding, providing a quantifiable signal [59] [60].
2. Key Reagents and Materials:
- Recognition Elements: Monoclonal anti-tropomyosin antibodies (for test line and detector conjugation).
- Signal Probe: Platinum nanoparticles (PtNPs) acting as a peroxidase mimic.
- Chromogenic Substrate: TMB-H₂O₂ solution.
- Platform: Nitrocellulose membrane, sample pad, conjugate pad, and absorbent pad assembled on a backing card.
- Sample: Extracted food sample, diluted in appropriate buffer (e.g., PBS).
3. Step-by-Step Workflow: 1. Conjugate Pad Preparation: Disperse and dry the PtNP-antibody conjugates on the conjugate pad. 2. Membrane Preparation: Dispense capture antibody (test line) and a secondary antibody (control line) onto the nitrocellulose membrane. 3. Assay Execution: Apply the liquid food sample to the sample pad. The sample migrates via capillary action. 4. Complex Formation: The target allergen in the sample binds to the PtNP-antibody conjugate on the pad, forming a complex. 5. Capture and Signal Generation: The complex is captured at the test line by the immobilized antibody. The control line captures excess conjugates, validating the assay. 6. Signal Development: The strip is dipped into or incubated with the TMB substrate solution. The PtNPs at the test line catalyze the oxidation of TMB, producing a blue color. 7. Detection & Analysis: The color intensity is measured visually or quantitatively using a smartphone camera or a portable strip reader. The intensity is proportional to the allergen concentration.
Diagram: Workflow of a Nanozyme-Based Lateral Flow Immunoassay
Protocol: Electrochemical Immunosensor for Peanut Allergin Ara h 1
Electrochemical biosensors translate a biological recognition event (e.g., antibody-allergen binding) into a quantifiable electrical signal, offering high sensitivity and potential for miniaturization [57].
1. Principle: A specific antibody for the target allergen (e.g., Ara h 1) is immobilized on a working electrode surface. The binding of the allergen to the antibody alters the electrochemical properties at the electrode-solution interface (e.g., increasing electron transfer resistance), which is measured using techniques like Electrochemical Impedance Spectroscopy (EIS) [57].
2. Key Reagents and Materials:
- Working Electrode: Gold screen-printed electrode (SPE) or carbon electrode.
- Nanomaterial Modifiers: Gold nanoparticles (AuNPs) or graphene to enhance electrode surface area and conductivity.
- Recognition Element: Anti-Ara h 1 monoclonal antibody.
- Electrochemical Probe: A redox couple such as [Fe(CN)₆]³⁻/⁴⁻.
- Buffer Systems: Phosphate Buffered Saline (PBS) for dilution and washing.
3. Step-by-Step Workflow: 1. Electrode Modification: Drop-cast a suspension of AuNPs onto the working electrode surface and dry to form a nano-structured film. 2. Antibody Immobilization: Incubate the modified electrode with the anti-Ara h 1 antibody solution. The antibodies chemisorb onto the AuNP surface. 3. Blocking: Treat the electrode with a blocking agent (e.g., Bovine Serum Albumin, BSA) to cover any non-specific binding sites. 4. Baseline Measurement: Measure the EIS signal of the [Fe(CN)₆]³⁻/⁴⁻ probe in buffer as a baseline (Rₑₜ₁). 5. Allergen Incubation: Expose the functionalized electrode to the sample extract containing Ara h 1. 6. Signal Measurement: Wash the electrode and measure the EIS signal again (Rₑₜ₂). The formation of the antibody-allergen complex hinders electron transfer, causing an increase in charge transfer resistance (ΔRₑₜ = Rₑₜ₂ - Rₑₜ₁). 7. Quantification: The ΔRₑₜ is proportional to the logarithm of the Ara h 1 concentration, allowing for quantification via a pre-established calibration curve.
Diagram: Electrochemical Immunosensor Mechanism Using EIS
The Scientist's Toolkit: Key Research Reagent Solutions
The performance of biosensors is critically dependent on the quality and properties of the reagents used. The table below details essential materials and their functions in the development of advanced allergen biosensors.
Table 2: Essential Research Reagents for Allergen Biosensor Development
| Reagent Category | Specific Example | Key Function in Biosensor Development |
|---|---|---|
| Bio-recognition Elements | Monoclonal/Polyclonal Antibodies [8] [57] | Provide high specificity by binding to a unique epitope on the target allergen protein. |
| DNA Aptamers [2] [58] | Single-stranded DNA/RNA oligonucleotides that bind targets with high affinity; offer better stability and easier modification than antibodies. | |
| Signal Transduction Materials | Gold Nanoparticles (AuNPs) [58] [57] | Used for signal amplification in colorimetric, electrochemical, and SERS biosensors due to their unique plasmonic and conductive properties. |
| Nanozymes (e.g., Pt, Fe₃O₄ NPs) [59] | Nanomaterials that mimic enzyme activity (e.g., peroxidase) to catalyze signal generation, offering superior stability over natural enzymes. | |
| Quantum Dots (QDs) [58] | Semiconductor nanoparticles used as fluorescent labels for highly sensitive optical detection. | |
| Platform & Immobilization Materials | Screen-Printed Electrodes (SPEs) [57] | Disposable, miniaturized electrodes that form the basis of portable, low-cost electrochemical sensors. |
| Nitrocellulose Membranes [8] | The porous matrix in lateral flow devices that enables capillary flow and immobilization of capture reagents at test and control lines. | |
| Molecularly Imprinted Polymers (MIPs) [8] | Synthetic polymers with tailor-made cavities that mimic natural antibody sites, offering a stable and cost-effective alternative for allergen recognition. |
Analysis of Performance Trade-offs and Future Directions
The data and protocols presented reveal a clear landscape of performance compromises. Traditional methods like ELISA and LC-MS/MS offer high robustness and reliability, making them irreplaceable for standardized laboratory confirmation. However, they trade off portability, speed, and cost-effectiveness [8] [2]. Conversely, emerging biosensors excel in sensitivity and potential for on-site use but often face challenges in robustness, particularly concerning the stability of biological recognition elements (e.g., antibodies) and signal interference from complex food matrices like chocolate or cooked meats [8] [57].
A key strategy to mitigate these trade-offs is the integration of nanomaterials and dual-mode sensing. Nanozymes, for instance, enhance sensitivity and stability in LFAs, addressing the traditional trade-off between robustness and signal strength [59] [60]. Furthermore, the combination of multiple detection principles (e.g., capacitive and localized surface plasmon resonance) in a single device can cross-validate results, improving reliability and expanding the dynamic range without sacrificing sensitivity [60]. Future research is poised to further overcome these trade-offs through the development of novel biorecognition elements like engineered aptamers, the creation of more robust synthetic receptors (MIPs), and the integration of artificial intelligence for data analysis to correct for matrix effects and improve prediction accuracy [8] [5].
The accurate detection of specific analytes, such as food allergens or clinical biomarkers, in complex samples is a cornerstone of food safety and medical diagnostics. However, the presence of matrix effects—where non-target components in a sample interfere with the detection process—poses a significant challenge to the reliability of analytical results. Matrix effects can arise from various components, including organic matter, proteins, lipids, and salts, which can cause nonspecific adsorption, mask target epitopes, or quench signal responses, ultimately compromising the sensitivity, specificity, and accuracy of the detection method [61] [62]. For biosensors, which are designed to be rapid, sensitive, and potentially deployable at the point-of-care, matrix effects represent a major barrier to their translation from controlled laboratory settings to real-world applications [61]. Consequently, robust and tailored sample preparation protocols are not merely a preliminary step but a critical determinant for the successful performance of any analytical technique, especially when evaluating novel biosensors against conventional methods.
This guide provides a systematic comparison of sample preparation strategies designed to mitigate matrix effects in complex food and biological matrices. It details specific experimental protocols and presents quantitative data on their performance, offering researchers a practical toolkit for method development and validation.
Sample Preparation Fundamentals: A Systematic Workflow
The overarching goal of sample preparation is to isolate, purify, and concentrate the target analyte while removing interfering substances. The following diagram illustrates a generalized decision-making workflow for selecting and optimizing a sample preparation strategy, adaptable for both food and biological samples.
Figure 1: A generalized workflow for sample preparation to overcome matrix effects.
Sample Preparation for Food Allergen Detection
The detection of allergenic proteins in food is notoriously challenged by matrix complexity and the structural diversity of the proteins themselves. Food processing (e.g., heating) can denature proteins, masking antibody-binding epitopes and further complicating detection [63] [2]. The following sections outline common and advanced preparation methods.
Conventional Food Sample Preparation
Core Protocol: Aqueous Buffer Extraction for Allergen Detection
- Principle: Solubilization of target proteins using a buffered solution, often combined with mechanical agitation.
- Reagents: Phosphate-Buffered Saline (PBS), Tris-Buffered Saline (TBS), or commercially available proprietary extraction buffers. Additives like surfactants (e.g., Tween-20) or reducing agents (e.g., Dithiothreitol) are frequently included to enhance protein solubility and accessibility [8] [2].
- Procedure:
- Homogenization: Grind solid food samples into a fine powder using a blender or mortar and pestle under chilled conditions.
- Weighing: Accurately weigh 1.0 ± 0.05 g of the homogenized sample into a 50 mL centrifuge tube.
- Dilution: Add 10 mL of the selected extraction buffer (e.g., PBS with 0.05% Tween-20) to achieve a 1:10 (w/v) dilution.
- Agitation: Vortex vigorously for 30 seconds, then place on a rotary shaker or orbital mixer for 15-20 minutes at room temperature.
- Clarification: Centrifuge at 10,000 × g for 10 minutes at 4°C.
- Collection: Carefully collect the supernatant for immediate analysis or further clean-up. The pellet contains insoluble debris and lipids [64] [2].
Advanced Processing for Complex Matrices
For highly processed foods or matrices with high fat or pigment content, basic extraction is insufficient. Advanced techniques are required to reduce interference and improve detection limits.
Advanced Protocol: Combined Enzymatic and Physical Processing
- Principle: Uses specific enzymes to break down complex matrix components (e.g., lipids, starches) that can entrap or shield allergens, followed by physical treatment to fully release targets.
- Reagents: Specific enzymes (e.g., lipases for fat degradation, proteases for non-target protein digestion), organic solvents (e.g., hexane for defatting), and extraction buffers.
- Procedure (e.g., for a high-fat matrix like chocolate):
- Defatting: Perform an initial defatting step using hexane or petroleum ether. Add solvent, vortex, centrifuge, and discard the organic (top) layer. Air-dry the pellet to remove residual solvent [64].
- Enzymatic Treatment: Resuspend the defatted pellet in a suitable buffer and add the selected enzyme. Incubate at the enzyme's optimal temperature (e.g., 37°C for 1 hour).
- Physical Treatment: Apply a physical method such as microwave irradiation or ultrasound to disrupt structures and enhance extraction efficiency [63].
- Final Extraction: Proceed with the standard aqueous buffer extraction protocol as described in Section 3.1 [63] [57].
Table 1: Comparison of Food Sample Preparation Methods and Their Impact on Allergen Detection
| Method | Key Procedural Steps | Target Matrix | Impact on Matrix Effects & Performance | Key Limitations |
|---|---|---|---|---|
| Aqueous Buffer Extraction | Homogenization, dilution, agitation, centrifugation [2]. | Broadly applicable (baked goods, dairy). | Reduces particulate interference; simple but may be insufficient for processed/complex foods [8]. | Limited effectiveness for denatured proteins or high-fat matrices. |
| Organic Solvent Defatting | Sample is mixed with solvent (e.g., hexane), vortexed, centrifuged, solvent layer discarded [64]. | High-fat foods (chocolate, nuts, fried foods). | Significantly reduces lipid-related interference, improving assay accuracy and signal-to-noise ratio [64]. | Not suitable for all analytes; potential for co-precipitation of target proteins. |
| Combined Methods (e.g., Enzymatic + Microwave) | Sequential defatting, enzymatic digestion, and microwave-assisted extraction [63] [57]. | Highly processed or complex matrices (infant formula, cooked meats). | Most effective for minimizing matrix effects; can recover allergens from denatured/embedded states [63]. | Time-consuming; requires optimization of multiple steps; higher cost. |
Sample Preparation for Biological Fluids
Biological matrices like blood serum, plasma, and urine present distinct challenges, including high abundance of non-target proteins (e.g., albumin, immunoglobulins), salts, and cellular components that can foul sensor surfaces [61].
Core Protocol: Dilution and Buffer Exchange
Core Protocol: Dilution and Buffer Exchange for Serum/Plasma
- Principle: Reduces the concentration of interfering substances by dilution and replaces the native matrix with a compatible assay buffer.
- Reagents: Assay-specific buffer (e.g., HEPES, PBS), spin desalting columns (e.g., Zeba columns).
- Procedure:
- Dilution: Dilute the serum/plasma sample 1:10 to 1:100 in the chosen assay buffer. Vortex to mix.
- Buffer Exchange (if needed): For more stringent requirements, use a spin desalting column according to the manufacturer's instructions. This effectively removes salts and small molecules while transferring the analyte into the desired buffer.
- Clarification: Centrifuge the diluted/exchanged sample at high speed (e.g., 14,000 × g for 5-10 minutes) to remove any precipitates or microparticles before analysis [61] [65].
Advanced Protocol: Solid Phase Extraction (SPE) and Immunoaffinity Clean-up
Advanced Protocol: Solid Phase Extraction (SPE) for Pre-concentration and Purification
- Principle: Uses a cartridge containing a sorbent to selectively bind the target analyte or impurities. It is highly effective for pre-concentrating trace analytes and removing a wide range of interferents.
- Reagents: SPE cartridges (C18, ion-exchange, mixed-mode), conditioning solvents (methanol, acetonitrile), elution solvents.
- Procedure (as applied to biological or environmental extracts):
- Conditioning: Pass 5-10 mL of methanol through the sorbent bed, followed by 5-10 mL of water or a weak buffer. Do not let the bed dry out.
- Loading: Load the prepared sample (e.g., diluted serum or a sediment extract) onto the cartridge at a controlled, slow flow rate (1-2 mL/min).
- Washing: Wash with 5-10 mL of a weak buffer or water/organic solvent mixture to remove weakly bound interferents.
- Elution: Elute the target analyte(s) with 2-5 mL of a strong solvent (e.g., high percentage of methanol or acetonitrile, possibly with acid/base modifiers).
- Reconstitution: Evaporate the eluent to dryness under a gentle stream of nitrogen and reconstitute the residue in the assay buffer compatible with the downstream detection method [62] [64].
Table 2: Comparison of Biological Sample Preparation Methods for Biosensor Applications
| Method | Key Procedural Steps | Target Matrix | Impact on Matrix Effects & Performance | Key Limitations |
|---|---|---|---|---|
| Dilution | Simple mixing of sample with buffer [61]. | Serum, plasma, urine. | Fastest method; reduces overall matrix concentration; minimal sample loss. | Can dilute the target analyte below the limit of detection; does not remove specific interferents. |
| Ultrafiltration | Centrifugation through a molecular weight cut-off (MWCO) membrane [63]. | Serum, plasma, processed food extracts. | Removes high-MW proteins and particulates; can desalt and pre-concentrate analytes. | Membrane fouling; potential for non-specific binding of analyte to the membrane. |
| Solid Phase Extraction (SPE) | Conditioning, loading, washing, elution, reconstitution [62]. | Complex biological and food extracts. | Highly effective clean-up and pre-concentration; can significantly improve LOD and specificity [62]. | More complex; requires optimization; potential for incomplete recovery of the target. |
Experimental Data: Quantifying the Impact of Sample Preparation
The effectiveness of a sample preparation strategy is quantitatively assessed by key figures of merit. The following data, compiled from recent studies, demonstrates the clear impact of sample preparation on analytical performance.
Table 3: Quantitative Performance Metrics of Different Preparation Methods
| Sample Type | Target Analyte | Preparation Method | Key Performance Metrics | Citation |
|---|---|---|---|---|
| Lake Sediments | 44 Trace Organic Contaminants | Pressurized Liquid Extraction (PLE) with Diatomaceous Earth + SPE | Recoveries: >60% for 34 compounds.Matrix Effects: Corrected to between -13.3% and +17.8% using internal standards. | [62] |
| Cow's Milk | β-Lactoglobulin (Allergen) | Enzymatic Digestion & Ultrafiltration | Result: Significant reduction of allergenic activity by removing or hydrolyzing the target protein. | [63] |
| Cow's Milk | β-Lactoglobulin (Allergen) | Microwave & Enzymatic Treatment | Result: Inhibition of allergenic properties through combined physical and biochemical processing. | [63] |
| Peanut Kernels | Ara h 1 & Ara h 2 (Allergens) | Enzymatic Treatment | Result: Demonstrated reduction in allergenicity, confirming the efficacy of the preparation step. | [63] |
| General Food Matrices | Allergens (e.g., Tropomyosin) | Immunoaffinity Capture on Magnetic Beads | Result: Selective isolation and pre-concentration from complex food matrices, improving biosensor sensitivity. | [8] |
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of the protocols above requires a suite of core reagents and materials. The following table details this essential toolkit.
Table 4: Research Reagent Solutions for Sample Preparation
| Item / Reagent | Function / Purpose | Key Considerations |
|---|---|---|
| Extraction Buffers (PBS, TBS) | Provides a stable pH and ionic strength environment for protein solubilization and stability. | The inclusion of surfactants (Tween-20) is often critical for efficient extraction from solid food matrices. |
| Organic Solvents (Hexane, Acetonitrile, Methanol) | Used for defatting, protein precipitation, and as eluents in SPE. | Purity grade is critical; compatibility with plasticware and downstream assays must be considered. |
| Enzymes (Lipases, Proteases) | Breaks down specific matrix components (fats, proteins) to liberate entrapped analytes and reduce interference. | Specificity, temperature, and pH optima must be matched to the application to avoid degrading the target analyte. |
| Solid Phase Extraction (SPE) Cartridges | Selective retention of target analytes or impurities for clean-up and pre-concentration. | Sorbent chemistry (C18, ion-exchange, immunoaffinity) must be selected based on the analyte's physicochemical properties. |
| Internal Standards (Stable Isotope-Labeled Analogs) | Added to the sample at the beginning of preparation to correct for analyte loss during preparation and to quantify matrix effects. | Considered the most efficient technique for correcting matrix effects in mass spectrometry without affecting sensitivity [62]. |
| Magnetic Beads (functionalized with antibodies/aptamers) | Enable selective capture and separation of targets from complex liquids using a magnetic field, simplifying wash steps. | Useful for automating sample preparation and integrating it with biosensor platforms [8]. |
Matrix effects are an inescapable challenge in the analysis of complex food and biological samples. As demonstrated through the protocols and data presented, the choice of sample preparation strategy is not ancillary but fundamental to the success of the analytical method, whether a conventional ELISA or an emerging biosensor platform. While simple dilution can suffice for some applications, complex matrices demand sophisticated, multi-step approaches like SPE, enzymatic treatment, or immunoaffinity capture to achieve the sensitivity and specificity required for reliable detection. The ongoing development of biosensors is intrinsically linked to advances in sample preparation, with trends pointing toward the integration of miniaturized, automated clean-up steps directly into microfluidic and lateral flow devices. For researchers, a rigorous, systematic approach to sample preparation—validated with appropriate metrics and internal standards—is indispensable for generating accurate, reproducible, and meaningful data.
The accurate detection of food allergens is a critical public health issue, with effective management relying on the vigilant avoidance of trigger foods by allergic consumers. The performance of detection methods is paramount, as trace amounts of an allergen can provoke severe, life-threatening reactions [66] [67]. The stability of a biosensor—encompassing its robustness against signal noise and its reproducibility across tests—is therefore not merely a technical specification but a fundamental determinant of its real-world safety efficacy. Signal noise can arise from multiple sources, including complex food matrices, environmental interferences, and electronic fluctuations, all of which can obscure detection and lead to false negatives or positives [68]. Similarly, reproducibility ensures that a test performs consistently in different hands and in varied settings, such as a quality control laboratory in a food processing plant or a point-of-use scenario in a restaurant kitchen. This guide objectively compares the performance of emerging biosensing platforms against conventional allergen detection methods, with a focused evaluation on their engineered strategies to mitigate instability and enhance reliability. The following sections provide a detailed comparison of method capabilities, delve into the experimental protocols that generate performance data, and visualize the core strategies that underpin stable biosensor design.
Comparative Analysis of Detection Methods
The landscape of food allergen detection is diverse, ranging from traditional immunological assays to novel biosensors and non-specific hygiene tests. The choice of method often involves a trade-off between sensitivity, specificity, speed, and suitability for on-site application. The table below summarizes the key performance characteristics of several prominent methods.
Table 1: Comparison of Allergen and Food Residue Detection Methods
| Method Name | Detection Principle | Reported Sensitivity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| iEAT2 Biosensor [66] | Electrochemical Immunoassay | Detects gliadin, Ara h1, ovalbumin below allergic reaction thresholds [66]. | Rapid (15 min), portable, simultaneous multi-allergen detection [66]. | Requires sample pre-processing; limited to allergens with available antibodies. |
| Lateral Flow Immunoassay (LFI) [69] | Immuno-chromatography | Best sensitivity for 10 out of 14 tested foods [69]. | Rapid, user-friendly, widely available for specific allergens [69]. | Not commercially available for all allergens; primarily qualitative/semi-quantitative [69]. |
| A3 Test (ATP+ADP+AMP) [69] | Bioluminescence (Total Adenylate) | Lower detection limits than ATP test for 40 allergenic foods; better than protein swab tests for most foods except gelatin [69]. | Broad-spectrum, detects food debris from many sources; rapid and quantitative [69]. | Non-specific; detects general food residue, not specific allergens [69]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) [67] | Immunoassay | Varies by allergen and kit; considered a gold standard. | High specificity and sensitivity; quantitative; well-established [67]. | Susceptible to processing-induced protein changes; lab-based, longer time-to-result [67]. |
| Mass Spectrometry (MS) [67] | Mass-to-Charge Ratio Analysis | High sensitivity, particularly for peptide markers. | High specificity and precision; can detect hydrolyzed allergens [67]. | Requires sophisticated equipment and expertise; complex sample preparation [67]. |
Experimental Protocols for Key Methods
Understanding the published experimental protocols is essential for interpreting performance data and assessing the robustness of a detection method. The following details are synthesized from validation studies and provide a framework for how key metrics are established.
Protocol for Electrochemical Biosensor (iEAT2)
The iEAT2 system exemplifies a modern approach to rapid, on-site allergen detection, and its protocol is designed for simplicity and speed [66].
- Sample Preparation: A small food sample is first ground using a dedicated torsion device for homogenization. The allergenic proteins are then extracted into a suitable buffer solution.
- Allergen Capture and Signal Generation: The food extract is mixed with magnetic beads coated with antibodies specific to the target allergen (e.g., anti-gliadin for gluten). The beads capture the allergen and are then separated from the matrix using a magnet. After washing, the beads are incubated with a second, enzyme-linked (e.g., Horseradish Peroxidase or HRP) detection antibody, forming a "sandwich" complex.
- Electrochemical Detection: The bead complex is introduced into the biosensor's electrochemical cell. An enzyme substrate is added, and the ensuing enzymatic reaction produces an electroactive product. The sensor applies a voltage and measures the resulting electrical current, which is directly proportional to the concentration of the target allergen.
- Validation & Stability Metrics: The entire process is completed within 15 minutes. The system's stability is demonstrated by its ability to perform 16 simultaneous, independent electrochemical measurements, confirming minimal cross-talk and high reproducibility. Sensitivity is validated by confirming detection limits below established clinical threshold doses for allergic reactions [66].
Protocol for Total Adenylate (A3) Testing
The A3 test is a non-specific but rapid method for verifying surface hygiene and the potential presence of allergenic food residues [69].
- Sample Collection: A swab is used to collect a sample from a defined surface area (e.g., 10 cm x 10 cm) on food processing equipment. The swab is typically moistened with a buffer to enhance recovery.
- Extraction and Reaction: The swab is placed in an extraction tube to release the collected material. An aliquot of the extract is then combined with a reagent containing luciferase, the enzyme responsible for bioluminescence in fireflies.
- Signal Measurement: The reaction mixture is placed in a luminometer. The instrument measures the light produced (in Relative Light Units or RLUs) when luciferase reacts with the total adenylates (ATP, ADP, and AMP) present in the sample.
- Validation & Stability Metrics: The method's effectiveness is validated by its Limit of Detection (LOD) for various foods, which is superior to traditional ATP tests. Its stability for allergen control is demonstrated in field studies where A3 values correlate with the removal of allergenic proteins (measured by ELISA) during cleaning procedures in food processing plants [69].
Engineering Strategies for Enhanced Stability
The reproducibility and noise resilience of a biosensor are not accidental but are the result of deliberate engineering choices at the interface and system levels.
Interface Engineering with Advanced Materials
A stable biosensor interface is crucial for maintaining the biological activity of recognition elements and ensuring consistent signal transduction.
- Nanomaterial-Enhanced Interfaces: The use of gold nanoparticles (AuNPs) provides a large surface area, excellent biocompatibility, and high conductivity, which improves the adsorption of biomolecules and accelerates electron transfer, leading to a more stable and sensitive signal response [70]. For instance, one study showed an AuNP-modified electrode retained 96% of its initial current response after one month, significantly outperforming other modifications [70].
- Polymer and Composite Matrices: Materials like chitosan and conducting polymers (e.g., polyaniline) form robust, biocompatible films that effectively entrap biomolecules. Composites such as graphene-chitosan combine the high conductivity and surface area of graphene with the superior film-forming and stabilizing properties of chitosan, creating a synergistic interface that enhances overall sensor stability [70].
System-Level Noise Mitigation
Beyond the molecular interface, system-level design is critical for handling environmental and electronic noise.
- Multi-Electrode Architecture for Parallel Analysis: The iEAT2 system employs a scalable array of electrochemical cells that function as independent current sources. This design allows for simultaneous multi-analyte detection and internal consistency checks, which simplifies electronics and reduces measurement variability compared to sequential testing [66].
- Experimental Noise Cancellation: In electrochemical systems, noise from power-line interference (PLI) and other ambient sources can be mitigated. One advanced method involves using a reference channel with electric field sensors to capture ambient noise in real-time. This "noise replica" is then used to program an ideal Wiener filter, which is applied to the primary signal channel to subtract the noise, thereby preserving the true signal morphology with high fidelity [68].
Diagram: Core Strategies for Engineering Stability in Biosensors
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and deployment of advanced allergen biosensors rely on a suite of specialized reagents and materials. The following table outlines key components and their functions in a typical assay.
Table 2: Key Research Reagent Solutions for Allergen Biosensing
| Reagent / Material | Function in Assay | Specific Example |
|---|---|---|
| Immunomagnetic Beads | Capture and separate target allergens from complex food matrices using antibody-antigen binding, thus purifying the sample and reducing interference [66]. | Dynabeads M-270 Epoxy [66]. |
| Enzyme-Labeled Antibodies | Serve as detection probes; the enzyme (e.g., HRP) catalyzes a reaction to generate a measurable (electro- or chemiluminescent) signal proportional to the allergen concentration [66]. | Horseradish Peroxidase (HRP)-conjugated detection antibodies [66]. |
| Electrochemical Substrate | The molecule that is converted by the enzyme label into an electroactive product, generating a current that is measured by the sensor [66]. | 3,3',5,5'-Tetramethylbenzidine (TMB) [66]. |
| Nanomaterial Composites | Form the core sensing interface; enhance stability, increase surface area for bioreceptor immobilization, and improve electrical conductivity for signal transduction [70]. | Gold Nanoparticles (AuNPs), Graphene-Oxide Chitosan (GO-CS) composites [70]. |
| Allergen Extraction Buffer | A solution designed to efficiently and reproducibly extract allergenic proteins from various food types, which is a critical and often challenging step in sample preparation [66] [67]. | Commercial extraction buffers from allergen ELISA kits [66]. |
Diagram: iEAT2 Biosensor Workflow for Reproducible Allergen Detection
The strategic engineering of biosensors is fundamentally enhancing the stability and reliability of food allergen detection. As demonstrated by platforms like the iEAT2, the integration of advanced materials for robust interfaces, coupled with system-level designs for noise cancellation and parallelized measurement, directly addresses the critical challenges of signal noise and reproducibility. While conventional methods like ELISA and LFI remain fit-for-purpose for many applications, the latest biosensors offer a compelling combination of speed, portability, and multi-analyte capability without compromising on sensitivity. The continued development and validation of these engineered solutions, supported by transparent experimental protocols and standardized reagents, are paving the way for more trustworthy tools that can empower both industrial quality control and, ultimately, consumer safety.
In the field of diagnostic and monitoring technologies, biosensors have emerged as indispensable tools for healthcare, food safety, and environmental monitoring. The performance of these biosensors is critically dependent on two key parameters: dynamic range, which defines the concentration interval over which a biosensor provides a quantifiable response, and response time, which determines how quickly this response is generated. Within the specific context of food allergen detection—a growing public health concern where accurate labeling is the primary preventive measure—the limitations of conventional methods become particularly evident. Techniques such as enzyme-linked immunosorbent assay (ELISA) and polymerase chain reaction (PCR), while established, often present constraints in sensitivity, speed, and operational complexity, creating a compelling case for biosensor advancement [57] [2].
This review objectively compares the performance of next-generation biosensors against conventional allergen detection methods, with a specific focus on how genetic engineering and surface immobilization strategies are being leveraged to tune dynamic range and response time. We synthesize recent experimental data to provide a clear comparison of capabilities and outline the detailed methodologies that enable these performance enhancements, providing researchers and developers with a practical guide for biosensor optimization.
Performance Comparison: Biosensors vs. Conventional Allergen Detection Methods
The evaluation of analytical techniques is paramount for selecting the appropriate method for a given application. Table 1 provides a direct comparison of the key performance metrics for conventional allergen detection methods against emerging biosensor technologies, highlighting the trade-offs in sensitivity, speed, cost, and potential for multiplexing and portability.
Table 1: Performance Comparison of Allergen Detection Methods
| Method Type | Specific Technique | Limit of Detection (LOD) | Assay Time | Multi-analyte Capability | Portability | Key Advantages | Main Limitations |
|---|---|---|---|---|---|---|---|
| Conventional (Protein-based) | ELISA (Enzyme-Linked Immunosorbent Assay) | 1–25 ppm [57] | Up to 3.5 hours [57] | Moderate [2] | Low [57] | High sensitivity & specificity; standardized [2] | Time-consuming; expensive for small batches; cross-reactivity [57] |
| Conventional (DNA-based) | PCR (Polymerase Chain Reaction) | Varies by target (e.g., highly sensitive for nuts) [2] | 2–4 hours (including sample prep) [2] | High (Real-time PCR) [2] | Low | High efficiency for processed foods; stable DNA target [2] | Indirect detection; not suitable for low-DNA allergens (e.g., egg) [57] |
| Biosensors (Electrochemical) | Antibody-based Immunosensor | ~0.3 ppm (Tropomyosin) [57] | Minutes [57] | Emerging [57] | High | Rapid; high sensitivity; cost-effective [57] [2] | Stability of biological recognition element |
| Biosensors (Optical) | RNA Integrity Biosensor | N/A (Reports integrity, not concentration) | Rapid (Colorimetric output) [71] | Low | High | Simple colorimetric output; suitable for resource-limited settings [71] | Application-specific (e.g., RNA quality control) |
| Biosensors (Genetically Encoded) | cdGreen2 (for c-di-GMP) | Kd = 214 nM [72] | Real-time (High temporal resolution) [72] | Moderate (Ratiometric) [72] | Moderate (Requires imaging) | Real-time, single-cell monitoring in vivo [72] | Primarily for research and compound screening |
The data reveals that electrochemical biosensors excel in providing rapid, on-site detection with sensitivities that meet or exceed those of conventional ELISA, while genetically encoded sensors offer unparalleled capabilities for real-time, dynamic monitoring, albeit in more specialized research contexts.
Strategy 1: Genetic and Protein Engineering for Enhanced Dynamic Range
Genetic engineering provides a powerful toolkit for fundamentally redesigning the core sensing architecture of biosensors to achieve a wider dynamic range and faster response. This approach involves the deliberate re-engineering of proteins and nucleic acids to optimize their ligand-binding properties and signal transduction mechanisms.
Experimental Protocol: Directed Evolution of a Genetically Encoded Biosensor
A prime example of this strategy is the development of cdGreen2, a genetically encoded ratiometric biosensor for the bacterial second messenger c-di-GMP [72]. The following protocol outlines the key steps:
- Library Construction: Generate a diverse library of biosensor variants by sandwiching a circularly permuted enhanced green fluorescent protein (cpEGFP) between two c-di-GMP-binding C-terminal domains (CTDs) of the transcription factor BldD (BldDCTD). Introduce variation by modulating the length, rigidity, and amino acid composition (e.g., alternating Pro/Ser or Ala/Gly residues) of the peptide linkers connecting the domains [72].
- Host Strain Transformation: Clone the biosensor library into an expression vector and transform it into a bacterial host strain (e.g., E. coli AKS494) where the intracellular c-di-GMP concentration can be systematically controlled, ranging from <50 nM to >5 µM [72].
- Fluorescence-Activated Cell Sorting (FACS): Subject the transformed library to iterative rounds of FACS. Cells are sorted under alternating regimes of high and low c-di-GMP concentration to enrich for variants that display the largest difference in fluorescence intensity between the two states [72].
- Ratiometric Refinement (Optional): To correct for variations in biosensor expression levels, convert the intensiometric sensor into a ratiometric one. Using a "Matryoshka" approach, insert a reference fluorescent protein (e.g., mScarlet-I) into the loop connecting the original EGFP N- and C-termini. This allows the c-di-GMP signal (from cpEGFP) to be normalized against the reference signal, providing an internal control [72].
- In Vitro Characterization: Purify the selected biosensor variant (e.g., via hexa-His tag) and perform in vitro titration with c-di-GMP. Generate a dose-response curve by measuring fluorescence excitation at 497 nm and 405 nm upon ligand binding, which exhibit inverse responses. Fit the data to a sigmoidal model to calculate the dissociation constant (Kd) and dynamic range [72].
This directed evolution process yielded cdGreen2, which demonstrates a 12-fold increase in fluorescence intensity and a Kd of 214 nM, enabling it to faithfully track c-di-GMP dynamics in single cells with high temporal resolution [72].
Experimental Protocol: Toehold-Mediated Strand Displacement for Tunable Response
An alternative genetic strategy utilizes synthetic nucleic acids. An enzyme-responsive electrochemical DNA biosensor was designed with a single immobilization probe featuring a two-loop hairpin structure [73]. The key steps for tuning its dynamic range are as follows:
- Probe Design: Design a hairpin-like DNA probe with independent domains: one for target recognition and another containing a specific site (e.g., an EcoRI restriction endonuclease recognition site).
- Assay Configuration:
- Standard Mode: The target DNA binds directly to the probe via toehold-mediated strand displacement, leading to a measurable electrochemical signal.
- Enhanced Mode: Prior to target introduction, the immobilized probe is treated with EcoRI. The enzyme cleaves the probe, liberating the toehold region and making it more accessible. This pre-cleavage step significantly enhances the target-binding affinity [73].
- Performance Measurement: Electrochemically measure the signal response (e.g., via amperometry or voltammetry) for a series of target concentrations, with and without the enzyme pre-cleavage step. The dynamic range and limit of detection are then calculated and compared for the two operational modes [73].
This clever use of an enzyme to "uncage" the binding site resulted in a biosensor with a significantly extended dynamic range and a lower detection limit, even in complex media like serum [73].
The logical workflow for engineering a biosensor's core sensing element, from design to validation, is summarized in the diagram below.
Strategy 2: Surface Immobilization and Interfacial Engineering to Control Response Dynamics
The performance of a biosensor is not solely determined by its recognition element; the method by which this element is anchored to the transducer surface—the immobilization strategy—profoundly affects its stability, orientation, and accessibility, thereby directly influencing response time and operational stability.
Experimental Protocol: Engineering the Bio-Interface
The goal of interfacial engineering is to create a stable, ordered, and efficient connection between the biological recognition layer and the physical transducer. Key methodologies include:
- Surface Functionalization:
- Covalent Immobilization: Activate the transducer surface (e.g., gold, graphene, or metal oxides) with functional groups. A common approach involves forming Self-Assembled Monolayers (SAMs) of alkanethiols on gold, followed by coupling bioreceptors (antibodies, aptamers) via carboxyl, amine, or thiol chemistry [74].
- Non-covalent Immobilization: Utilize affinity interactions (e.g., biotin-streptavidin), electrostatic adsorption, or encapsulation within biocompatible polymers like chitosan or polydopamine [74].
- Nanomaterial Enhancement: Integrate nanomaterials such as graphene, carbon nanotubes (CNTs), or gold nanoparticles (AuNPs) onto the transducer surface. Their high surface-to-volume ratio allows for a higher density of immobilized bioreceptors, while their excellent electrical conductivity can enhance signal transduction in electrochemical sensors [74] [75].
- Post-Immobilization Processing:
- Annealing: Subject the functionalized sensor to a controlled thermal annealing process. This post-treatment can drive the reorganization of molecular chains on the surface, enhancing structural order, reducing grain boundaries, and improving charge transport, which collectively boosts signal stability and response time [76].
- Solvent Engineering: Pre-determine the microscopic morphology of the immobilization layer by modulating solvent properties and processing techniques during coating. This controls molecular stacking order and orientation, which directly impacts carrier mobility and interface quality in electronic biosensors [76].
The Role of Artificial Intelligence (AI) in Optimization
A paradigm shift in interfacial engineering is the use of Artificial Intelligence (AI) and Machine Learning (ML). AI models can predict optimal material compositions, surface topographies, and bioreceptor configurations by analyzing vast datasets, thereby accelerating the optimization cycle [74]. For instance, ML algorithms have been used to optimize the structural parameters of a graphene-based biosensor, achieving a peak sensitivity of 1785 nm/RIU for breast cancer detection [75]. Similarly, AI-guided molecular dynamics simulations provide atomic-level insights into bioreceptor-substrate interactions, aiding the design of surfaces that maximize binding affinity and minimize non-specific fouling [74].
The following diagram illustrates the multi-level approach to optimizing a biosensor's interface, from molecular design to functional deployment.
The Scientist's Toolkit: Essential Reagents and Materials
The experimental protocols outlined above rely on a set of core reagents and materials. Table 2 catalogues these key research solutions and their functions, serving as a starting point for experimental design.
Table 2: Research Reagent Solutions for Biosensor Engineering
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Circularly Permuted FPs | Core scaffold for intensiometric biosensors; sensitive to microenvironment changes. | cpEGFP (circularly permuted Enhanced Green Fluorescent Protein) [72] |
| Ligand-Binding Domains | Provides specificity for the target analyte. | BldDCTD (binds c-di-GMP) [72] |
| Reference FPs | Enables ratiometric sensing and normalizes for expression variance. | mScarlet-I [72] |
| Restriction Endonucleases | Used to enzymatically "tune" probe accessibility and dynamic range. | EcoRI [73] |
| Self-Assembled Monolayers (SAMs) | Forms a well-ordered, functionalized interface on transducer surfaces for controlled immobilization. | Alkanethiols on gold [74] [76] |
| Functionalization Agents | Introduces chemical groups (-COOH, -NH₂) for covalent bioreceptor attachment. | (3-Aminopropyl)triethoxysilane (APTES) [74] |
| Nanomaterials | Enhances signal transduction and increases bioreceptor loading capacity. | Graphene, Carbon Nanotubes (CNTs), Gold Nanoparticles (AuNPs) [74] [75] |
| Polymer Coatings | Provides a biocompatible matrix for immobilization and reduces non-specific fouling. | Polyethylene glycol (PEG), polydopamine (PDA), chitosan [74] |
The strategic engineering of biosensors through genetic design and advanced immobilization represents a significant leap beyond the capabilities of conventional analytical methods. As demonstrated, directed evolution and rational probe design can systematically tailor dynamic range and specificity, while sophisticated interfacial chemistry can drastically improve response time and stability. The integration of AI and machine learning further accelerates this optimization process, moving beyond traditional trial-and-error approaches.
For the field of food allergen detection, these advancements translate directly into practical benefits: the potential for rapid, on-site tests with sensitivity rivaling laboratory-based ELISA, and the development of robust, continuous monitoring systems. The future of biosensing lies in the continued convergence of synthetic biology, materials science, and data analytics, paving the way for a new generation of intelligent, adaptive, and highly precise diagnostic tools that will enhance food safety, therapeutic drug monitoring, and personalized medicine.
Head-to-Head Validation: A Comparative Analysis of Biosensor Efficacy
The accurate and sensitive detection of target molecules is a cornerstone of progress in biomedical research, clinical diagnostics, and food safety. For decades, conventional techniques including Enzyme-Linked Immunosorbent Assay (ELISA), Polymerase Chain Reaction (PCR), and Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) have served as fundamental analytical tools. However, the emergence of biosensor technologies presents a powerful alternative, promising rapid, sensitive, and portable detection. This guide provides an objective, data-driven comparison of the performance of modern biosensors against these established methods, focusing on key metrics such as sensitivity, specificity, and operational practicality to inform researchers and development professionals in their methodological selections.
The following tables summarize the core performance characteristics and operational parameters of each technology based on recent comparative studies.
Table 1: Analytical Performance Comparison
| Detection Method | Typical Limit of Detection (LOD) | Dynamic Range | Assay Time | Key Advantages |
|---|---|---|---|---|
| Biosensors (Electrochemical) | 20 zeptomoles (for HRP) [15]; 0.03 µg/mL (in plasma) [77] | Wide [15] | Minutes to <30 min [77] | Portability, rapid analysis, cost-effective, suitable for point-of-care testing [77] [78] |
| Biosensors (Chemiluminescent) | 45 zeptomoles (for HRP); 12 fM (for IgG) [15] | Wide [15] | Longer than electrochemical [15] | Ultra-high sensitivity, simple instrumentation [15] |
| ELISA | 1–10 pg/mL (for proteins) [79] | Moderate | Up to 3.5 hours [4] | Well-established, standardized, high-throughput capability [4] |
| PCR/dPCR | Varies by target; dPCR enables single-molecule detection [80] | Wide (for dPCR) [80] | 1 to several hours [80] | High sensitivity for nucleic acids, absolute quantification with dPCR [80] |
| LC-MS/MS | 0.05–0.5 pg (for small molecules); 1 mg/kg (for food allergens) [79] [81] | Wide | High (sample preparation and run time) [81] | High specificity, multiplexing capability, does not require specific antibodies [81] |
Table 2: Operational and Practical Considerations
| Detection Method | Multiplexing Potential | Key Limitations | Typical Cost |
|---|---|---|---|
| Biosensors | Moderate (developing) | May have lower reproducibility; requires optimization [15] | Low (potentially <$10 per test) [78] |
| ELISA | Low | Susceptible to cross-reactivity; requires high-quality antibodies; lower sensitivity than newer methods [4] [81] | Moderate |
| PCR/dPCR | Moderate (for qPCR) | Detects DNA, not the protein itself; can be affected by food processing [4] [81] | High (especially for dPCR) [80] |
| LC-MS/MS | High | High cost of equipment and operation; requires skilled personnel [81] | Very High |
Detailed Experimental Protocols from Cited Studies
Comparative Protocol: Electrochemical vs. Chemiluminescent Biosensors
A direct challenge between electron- (electrochemical) and photon- (chemiluminescence) based biosensors was conducted using identical reagents and analytical formats to ensure a fair comparison [15].
- Analytes: Horseradish peroxidase (HRP) activity, hydrogen peroxide, glucose, and mouse IgG (using a sandwich immunoassay format) [15].
- Biospecific Reagents: The same batch of biospecific reagents, including antibodies and enzymes, was used for both detection platforms [15].
- Platforms: Amperometric detection was used for electrochemical biosensors, while chemiluminescence (CL) detection was used for optical biosensors. Both bench-top and portable miniaturised formats were evaluated [15].
- Key Findings: The study demonstrated that both types of biosensors offered similar detectability, with each showing slight advantages in specific scenarios. CL biosensors generally provided slightly higher detectability for some targets (e.g., 4 pmol for H₂O₂ vs. 210 pmol for amperometry), while amperometric biosensors were faster, making them more suitable for real-time monitoring and wearable devices [15].
Comparative Protocol: LC-MS/MS vs. Electrochemical Immunosensor
A 2025 study directly compared an LC-MS/MS method and a novel electrochemical immunosensor for detecting the antibiotic clarithromycin in human plasma [77].
- LC-MS/MS Method:
- Sample Preparation: Protein precipitation followed by liquid-liquid extraction using tert-butyl methyl ether.
- Instrumentation: Ultra-performance liquid chromatography coupled with tandem mass spectrometry.
- Validation: The method demonstrated excellent linearity and precision within a validated range of 0.1 to 4.0 µg/mL, with an LOD of 0.03 µg/mL [77].
- Electrochemical Immunosensor:
- Platform: Utilized functionalized magnetic beads and screen-printed carbon electrodes.
- Assay Format: Immunosensing approach.
- Performance: Achieved the same LOD (0.03 µg/mL) as the LC-MS/MS method, with a rapid analysis time of under 30 minutes and high selectivity in the complex plasma matrix [77].
- Conclusion: The two platforms showed complementary strengths: LC-MS/MS offered robustness and regulatory alignment for centralized labs, while the electrochemical immunosensor provided portability, speed, and operational simplicity for point-of-care applications [77].
Performance of Immuno-PCR vs. ELISA
Immuno-PCR (iPCR) is a powerful hybrid technique that combines immunological specificity with the exponential signal amplification of PCR.
- Principle: An antibody is conjugated to a DNA reporter molecule. After the antibody binds to its target antigen, the DNA reporter is amplified by PCR, allowing for ultra-sensitive quantification [79].
- Sensitivity: iPCR possesses a sensitivity that is 100 to 10,000 times higher than that of traditional ELISA. The LOD of iPCR can reach femtogram levels (10⁻¹⁵ g), compared to picogram levels (10⁻¹² g) for ELISA, with a wide linear range from 1 fg/mL to 10 pg/mL [79].
- Application Example: A study found that the quantitative sensitivity of iPCR in detecting the food allergen tropomyosin was 20 times higher than that of a comparable ELISA method [79].
Visualizing Biosensor Technologies and Workflows
The following diagrams illustrate the core principles and experimental workflows of the key biosensor technologies discussed.
Fundamental Biosensor Transduction Principles
Electrochemical Immunosensor Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
The development and operation of high-performance biosensors rely on specialized reagents and materials.
Table 3: Essential Reagents and Materials for Biosensor Development
| Item | Function/Application | Example from Literature |
|---|---|---|
| Screen-Printed Carbon Electrodes (SPCEs) | Low-cost, disposable, mass-producible platform for electrochemical biosensors [77]. | Used as the base transducer in a clarithromycin immunosensor [77]. |
| Functionalized Magnetic Beads | Solid support for immobilizing recognition elements (e.g., antibodies); enable easy separation and concentration of the target analyte [77]. | Used for antibody immobilization in an electrochemical immunosensor for plasma analysis [77]. |
| Nanomaterials (e.g., Graphene, NPs) | Enhance signal amplification, improve electrode conductivity, and increase surface area for biomolecule immobilization [59] [4]. | Graphene Field-Effect Transistor (GFET) chips used for ultralow LOD detection of GFAP [82]. |
| Specific Antibodies | High-affinity biological recognition elements that provide the core specificity of immunosensors [15] [77]. | Monoclonal antibodies against the S1 spike protein were electro-inserted into cell membranes for a SARS-CoV-2 biosensor [78]. |
| Enzyme Labels (e.g., HRP) | Catalyze reactions that generate measurable electrochemical or optical signals in affinity biosensors [15]. | HRP was used as a label in both electrochemical and CL biosensors for the detection of mouse IgG [15]. |
| Cell-based Recognition Elements | Whole cells used as biorecognition elements that respond to the presence of a target with a measurable change in electrical properties [78]. | Vero cells with electro-inserted antibodies formed the basis of a Bioelectric Recognition Assay (BERA) for SARS-CoV-2 [78]. |
The comparative data clearly illustrates that no single detection technology universally outperforms all others in every metric. Instead, each has its own strategic niche. Biosensors, particularly electrochemical and CL variants, excel in applications demanding rapid results, portability, and potential for low-cost point-of-care testing, with sensitivities that can meet or exceed those of traditional methods like ELISA [15] [77]. ELISA remains a widely used, standardized tool for high-throughput laboratory analysis, though it is generally less sensitive than newer techniques [79]. PCR and dPCR are indispensable for nucleic acid detection, with dPCR providing supreme sensitivity and absolute quantification for genetic targets [80]. Finally, LC-MS/MS represents the gold standard for specificity and multiplexing in complex matrices, particularly when antibodies are unavailable or cross-reactivity is a concern, though it requires sophisticated infrastructure [81].
The choice among these technologies should be guided by the specific requirements of the application, including the required sensitivity, the nature of the sample matrix, the need for portability, and considerations of cost and operational complexity. The ongoing development of biosensors, especially those leveraging nanomaterials and innovative transduction principles, continues to narrow the performance gap with conventional methods, offering powerful new tools for researchers and clinicians.
Food allergy is a significant global public health concern, with prevalence rates of approximately 8% in children and 5% in adults in developed Western countries [83]. For allergic individuals, strict avoidance of allergenic foods remains the only effective prevention strategy, as no definitive treatments currently exist [8]. This reality places tremendous importance on accurate, sensitive, and specific detection methods for food allergens to ensure proper labeling and prevent accidental exposure.
Traditional allergen detection methodologies include immunoassays such as enzyme-linked immunosorbent assay (ELISA), nucleic acid-based methods like polymerase chain reaction (PCR), and chromatographic techniques including liquid chromatography-tandem mass spectrometry (LC-MS/MS) [8] [2]. While these methods provide reliable detection, they face limitations including lengthy analysis times, requirements for sophisticated laboratory equipment and trained personnel, and relatively poor portability for on-site applications [8] [4]. These constraints have driven research toward developing novel biosensing technologies that offer rapid, sensitive, and portable alternatives for allergen detection.
This case study provides a comprehensive evaluation of emerging biosensor configurations for specific allergen targets, comparing their performance against conventional methods and with each other. By examining experimental data and technical specifications across multiple detection platforms, we aim to provide researchers and drug development professionals with critical insights for selecting appropriate biosensor technologies for specific application requirements.
Conventional Methods: Establishing the Baseline
Before evaluating biosensor technologies, it is essential to understand the performance metrics of conventional allergen detection methods that currently serve as reference standards.
Table 1: Performance Metrics of Conventional Allergen Detection Methods
| Method Type | Specific Example | Typical Detection Limit | Analysis Time | Key Advantages | Principal Limitations |
|---|---|---|---|---|---|
| Immunoassay | ELISA | 1-25 ppm [4] | Up to 3.5 hours [4] | High sensitivity and specificity; standardized protocols | Limited multiplexing capability; cross-reactivity issues |
| Nucleic Acid-Based | PCR | Varies by allergen | 2-4 hours | High specificity; suitable for processed foods | Does not detect allergens directly; affected by processing |
| Chromatographic | LC-MS/MS | Low ppm range [8] | Several hours | High selectivity and accuracy | Costly equipment; requires technical expertise |
These conventional methods have established the foundational performance expectations for allergen detection. Immunoassays, particularly ELISA, remain the most widely used method for quantitative allergen detection due to well-established protocols and commercial availability [2]. DNA-based methods like PCR provide an effective alternative, especially for highly processed foods where proteins may be denatured but DNA retains sufficient integrity for detection [2]. LC-MS/MS offers highly selective and accurate detection but requires sophisticated instrumentation and operational expertise, limiting its application to well-equipped laboratory settings [8].
Biosensors are defined as analytical devices that integrate a biological recognition element with a physicochemical transducer to produce a measurable signal proportional to the concentration of the target analyte [58]. The fundamental components include a biorecognition element (antibodies, aptamers, enzymes, etc.), a transducer (electrochemical, optical, piezoelectric, etc.), and a signal processing system that converts the biological interaction into a quantifiable output [8] [58].
Biosensor Classification by Transduction Mechanism
Biosensors for allergen detection are primarily categorized based on their transduction mechanism:
Electrochemical Biosensors measure changes in electrical properties (current, potential, impedance) resulting from antigen-antibody or aptamer-allergen binding events [4] [28]. These sensors are further classified as amperometric, potentiometric, impedimetric, or conductometric based on the specific electrical parameter measured.
Optical Biosensors detect changes in light properties resulting from allergen binding, including variations in absorbance, fluorescence, luminescence, or refractive index [8] [28]. Surface plasmon resonance (SPR) and fluorescence-based sensors represent prominent examples in this category.
Colorimetric Biosensors produce visual color changes detectable by the naked eye or simple readers, making them particularly suitable for point-of-care applications [8].
Mass-Sensitive Biosensors detect changes in mass resulting from binding events using piezoelectric crystals or surface acoustic wave devices [58].
Nanomaterial Integration in Biosensors
The integration of nanomaterials has significantly enhanced biosensor performance by improving sensitivity, stability, and response time [83] [58]. Key nanomaterials employed in allergen biosensors include:
Gold nanoparticles (AuNPs): Utilized for their exceptional conductivity, biocompatibility, and surface functionalization properties [83] [58].
Quantum dots (QDs): Semiconductor nanocrystals with size-tunable fluorescence properties ideal for optical detection [83].
Carbon nanomaterials: Including graphene, carbon nanotubes, and carbon dots valued for their high surface area and electrical conductivity [58].
Magnetic nanoparticles: Enable efficient separation and concentration of target allergens from complex food matrices [8].
Comparative Performance Analysis of Biosensor Platforms
To objectively evaluate different biosensor configurations, we have compiled experimental data from recent research publications, focusing on their performance with specific allergen targets.
Table 2: Performance Comparison of Biosensor Platforms for Specific Allergen Detection
| Allergen Target | Biosensor Platform | Nanomaterial Enhancement | Detection Limit | Detection Time | Linear Range | Reference |
|---|---|---|---|---|---|---|
| Peanut (Ara h 1) | Electrochemical immunosensor | Gold nanoparticles | 0.3 ng/mL [4] | < 30 min | 1-100 ng/mL [4] | Alves et al. |
| Egg white (Ovalbumin) | Fluorescent biosensor | Carbon dots | 0.22 ng/mL [2] | ~60 min | 0.5-100 ng/mL [2] | Fu et al. |
| Shrimp (Tropomyosin) | Aptasensor | Gold nanoparticles | 0.52 ng/mL [2] | ~45 min | 1-1000 ng/mL [2] | Chinnappan et al. |
| Milk (β-lactoglobulin) | Electrochemical aptasensor | Graphene | 0.13 ng/mL [4] | < 25 min | 1-1000 ng/mL [4] | Eissa et al. |
| Cashew nut | Colorimetric saltatory rolling circle amplification | - | 3.4 pg/mL [2] | ~90 min | 0.01-100 ng/mL [2] | Chen et al. |
| Multiple allergens | Lateral flow immunoassay | Gold nanoparticles | Visual: 1 ppm [8] | 10-15 min | Qualitative | Hnasko et al. |
The data reveals that electrochemical biosensors frequently achieve superior sensitivity, often detecting allergens at picogram per milliliter concentrations [4] [28]. This exceptional performance stems from the direct transduction of biological binding events into electrical signals, which can be precisely measured and amplified. The integration of nanomaterials such as gold nanoparticles and graphene further enhances sensitivity by increasing the effective surface area for biorecognition element immobilization and facilitating electron transfer processes [83] [4].
Optical biosensors, particularly those utilizing fluorescence detection, also demonstrate impressive sensitivity while offering additional advantages for multiplexed detection [28]. However, they often require more complex instrumentation than their electrochemical counterparts. Colorimetric biosensors and lateral flow assays, while generally less sensitive, provide unparalleled advantages for point-of-care applications due to their simplicity, rapid response, and minimal equipment requirements [8] [84].
Experimental Protocols: Methodologies for Key Biosensor Platforms
Electrochemical Immunosensor for Peanut Allergen (Ara h 1)
Principle: This protocol details the development of an electrochemical immunosensor for detecting the major peanut allergen Ara h 1, utilizing gold nanoparticle-modified electrodes for signal enhancement [4].
Materials and Reagents:
- Gold nanoparticle-coated screen-printed carbon electrodes
- Anti-Ara h 1 monoclonal antibodies
- Ara h 1 allergen standard
- Bovine serum albumin (BSA) for blocking non-specific binding sites
- Phosphate buffer saline (PBS) for washing and dilution
- Electrochemical redox probe ([Fe(CN)₆]³⁻/⁴⁻)
Procedure:
- Electrode Modification: Clean and polish screen-printed carbon electrodes, then electrodeposit gold nanoparticles onto the electrode surface.
- Antibody Immobilization: Incubate anti-Ara h 1 antibodies on the gold nanoparticle-modified electrode surface for 12 hours at 4°C.
- Blocking: Treat the electrode with BSA solution (1% w/v) for 1 hour to block non-specific binding sites.
- Allergen Detection: Incubate the modified electrode with samples containing Ara h 1 allergen for 30 minutes at room temperature.
- Electrochemical Measurement: Perform electrochemical impedance spectroscopy (EIS) in the presence of [Fe(CN)₆]³⁻/⁴⁻ redox probe.
- Signal Analysis: Measure the charge transfer resistance (Rct) increase, which correlates with Ara h 1 concentration.
Signal Measurement: The binding of Ara h 1 to the immobilized antibodies increases the electron transfer resistance at the electrode surface, which is quantified through EIS measurements [4].
Fluorescent Biosensor for Egg White Allergen (Ovalbumin)
Principle: This protocol describes a fluorescence resonance energy transfer (FRET)-based biosensor utilizing carbon dots for sensitive detection of ovalbumin, a major egg white allergen [2] [28].
Materials and Reagents:
- N, O, P-co-doped carbon dots (NOP-CDs)
- Ovalbumin-specific aptamer labeled with quencher
- Ovalbumin allergen standard
- Buffer solution (10 mM Tris-HCl, pH 7.4)
- Spectrofluorometer for fluorescence measurement
Procedure:
- CDs-Aptamer Conjugate Preparation: Incubate NOP-CDs with ovalbumin-specific aptamers for 2 hours at 37°C to form CDs-aptamer conjugates.
- Baseline Measurement: Measure the fluorescence intensity of the CDs-aptamer conjugate (excitation: 360 nm).
- Allergen Detection: Add samples containing ovalbumin to the CDs-aptamer conjugate and incubate for 45 minutes at 37°C.
- Fluorescence Measurement: Record the fluorescence recovery after allergen binding.
- Quantification: Calculate ovalbumin concentration based on the fluorescence intensity increase.
Signal Measurement: In the absence of ovalbumin, the aptamer-quencher conjugate binds to CDs, quenching their fluorescence. When ovalbumin is present, it binds specifically to the aptamer, releasing the quencher and restoring CD fluorescence proportional to ovalbumin concentration [2].
Signaling Pathways and Detection Mechanisms
The detection mechanisms in biosensors rely on specific biochemical interactions and their transduction into measurable signals. The following diagram illustrates the fundamental signaling pathways across different biosensor platforms.
Figure 1: Signaling Pathways in Allergen Biosensors
The signaling pathway begins with the specific biorecognition event between the target allergen and the biological recognition element (antibody, aptamer, or enzyme). This binding event triggers a physicochemical change that is converted into a measurable signal by the transducer. The specific transduction mechanism depends on the biosensor platform: electrochemical sensors detect changes in electrical properties, optical sensors monitor alterations in light characteristics, and colorimetric sensors produce visible color changes. Finally, the signal processing system converts this transducer output into a quantifiable readout correlating with allergen concentration.
Research Reagent Solutions: Essential Materials for Biosensor Development
The development and implementation of allergen biosensors require specific reagents and materials optimized for each detection platform.
Table 3: Essential Research Reagents for Allergen Biosensor Development
| Reagent Category | Specific Examples | Function in Biosensor | Application Notes |
|---|---|---|---|
| Biological Recognition Elements | Anti-Ara h 1 antibodies, Ovalbumin aptamers, β-lactoglobulin imprinted polymers | Target-specific binding | Antibodies offer high specificity; aptamers provide better stability; MIPs have longer shelf life |
| Nanomaterials | Gold nanoparticles, Graphene quantum dots, Carbon nanotubes, Magnetic nanoparticles | Signal amplification and enhancement | AuNPs excel in electrochemical sensors; QDs optimal for fluorescence-based detection |
| Signal Transduction Elements | Electrochemical redox probes ([Fe(CN)₆]³⁻/⁴⁻), Fluorescent dyes (FITC, RITC), Enzymatic labels (HRP, ALP) | Generate measurable signal | Choice depends on detection mechanism; enzymatic labels provide signal amplification |
| Surface Chemistry Reagents | N-hydroxysuccinimide (NHS), Ethyl(dimethylaminopropyl) carbodiimide (EDC), Glutaraldehyde, Thiol compounds | Immobilize recognition elements | Critical for sensor stability and reproducibility; varies by substrate material |
| Blocking Agents | Bovine serum albumin (BSA), Casein, Skim milk powder | Prevent non-specific binding | Essential for reducing background signal in complex matrices |
| Reference Allergens | Purified natural allergens, Recombinant allergens, Allergen extracts | Calibration and validation | Required for sensor calibration and performance verification |
The selection of appropriate research reagents significantly influences biosensor performance. Biological recognition elements determine the specificity of the detection system, with antibodies providing exceptional specificity but limited stability, while aptamers offer superior stability and modification flexibility [2] [4]. Nanomaterials enhance sensitivity through various mechanisms including increased surface area, catalytic properties, and signal amplification capabilities [83] [58]. Surface chemistry reagents are crucial for stable immobilization of recognition elements, directly impacting sensor reproducibility and lifespan [85].
This comprehensive evaluation of biosensor configurations for specific allergen targets demonstrates that emerging biosensing technologies offer significant advantages over conventional methods in terms of sensitivity, detection time, and portability. Electrochemical biosensors consistently achieve superior sensitivity, often detecting allergens at picogram per milliliter concentrations, making them ideal for applications requiring ultralow detection limits [4] [28]. Optical biosensors provide excellent performance with additional capabilities for multiplexed detection, while colorimetric platforms offer unparalleled advantages for point-of-care applications despite their generally lower sensitivity [8] [84].
The integration of nanomaterials has substantially enhanced biosensor performance across all platforms by improving sensitivity, stability, and response time [83] [58]. Gold nanoparticles have emerged as particularly versatile nanomaterials, finding applications in both electrochemical and optical biosensors. Similarly, carbon-based nanomaterials including graphene and carbon dots have demonstrated exceptional performance in enhancing electron transfer and fluorescence properties, respectively.
Future development in allergen biosensing should address several remaining challenges, including the need for improved sample preparation methods compatible with complex food matrices, enhanced multiplexing capabilities for simultaneous detection of multiple allergens, and greater standardization to enable comparison across different platforms and laboratories [8]. Additionally, the transition from proof-of-concept studies to validated commercial applications requires more extensive testing with real food samples across a wider range of allergen concentrations [28].
The continuing advancement of biosensor technologies, particularly through the integration of novel nanomaterials and innovative transduction mechanisms, holds tremendous promise for developing increasingly sophisticated allergen detection platforms that meet the critical needs of both food manufacturers and allergic consumers.
The paradigm for diagnosing infectious diseases, food allergens, and other health conditions is progressively shifting from centralized laboratories to decentralized, point-of-care (POC) settings. This transition is largely driven by the development of advanced biosensors, which promise rapid, portable, and cost-effective diagnostics. However, their real-world applicability hinges on a critical evaluation of their performance against conventional laboratory methods. Framed within a broader thesis on evaluating biosensor performance, this guide provides an objective comparison based on empirical data. It examines key POC suitability parameters—specifically cost, operational speed, and portability—for a range of emerging biosensor platforms against established conventional techniques, providing researchers and drug development professionals with a evidence-based framework for technology selection.
Performance Comparison: Biosensors vs. Conventional Methods
The following tables summarize the quantitative performance data for various diagnostic technologies, highlighting the comparative advantages of modern biosensors.
Table 1: Performance Comparison of Infectious Disease Diagnostics
| Technology | Application | Sensitivity | Specificity | Limit of Detection (LOD) | Assay Time | Key Advantage |
|---|---|---|---|---|---|---|
| CRISPR-Cas12 (DETECTR) [86] | SARS-CoV-2 Detection | ~95% | ~98% | 10 copies/µL | ~30 minutes | Rapid, equipment-free POC use [86] |
| CRISPR-Cas13 (SHERLOCK) [86] | Zika Virus Detection | Attomolar | Near 100% | Attomolar | N/S | Exceptional single-base specificity [86] |
| Antigen Rapid Test (Ag-RDT) [87] | SARS-CoV-2 Detection | N/S | N/S | N/S | Minutes | Cost-effective in LMICs [87] |
| RT-PCR (Conventional) [86] | SARS-CoV-2 Detection | High | High | Low | Several hours | Gold standard sensitivity [86] |
Note: N/S = Not Specified in the sourced research.
Table 2: Performance Comparison of Allergen Detection Platforms
| Technology | Application | Detection Mechanism | Limit of Detection (LOD) | Assay Time | Portability |
|---|---|---|---|---|---|
| Smartphone iSPR [88] | Hazelnut Allergen in Milk | Imaging Surface Plasmon Resonance | 0.04 - 0.53 µg/mL | N/S | Portable, 3D-printed microfluidic chip [88] |
| Portable Fluorescence Reader [89] | Allergen-specific IgE | Fluorescence Immunoassay | 500 dye molecules/µm² | ~1 second (readout) | Portable, low-cost [89] |
| Allergy Amulet [90] | Food Allergens | N/S | Lower than known reaction triggers | ~1 minute | "World's smallest" consumer sensor [90] |
| Conventional SPR [88] | Hazelnut Allergen in Milk | Surface Plasmon Resonance | Comparable to smartphone iSPR | N/S | Benchtop, laboratory-bound [88] |
| ELISA (Conventional) [91] | Allergen-specific Antibodies | Colorimetric Immunoassay | Lower than SPR | Several hours | Laboratory-bound [91] |
Detailed Experimental Protocols and Principles
To understand the data in the comparison tables, it is essential to examine the experimental methodologies that generated them. This section details the protocols and working principles of the key technologies.
CRISPR-Based Diagnostic Assays (e.g., DETECTR/SHERLOCK)
Principle: CRISPR-based diagnostics utilize Cas proteins (e.g., Cas12, Cas13) programmed with guide RNA (gRNA) to locate specific nucleic acid sequences. Upon target binding, these enzymes exhibit non-specific "collateral cleavage" activity, degrading reporter molecules (e.g., fluorescently-quenched nucleic acid probes) to generate a detectable signal [86].
Protocol for SARS-CoV-2 Detection with DETECTR [86]:
- Sample Preparation: Viral RNA is extracted from patient nasopharyngeal swabs.
- Isothermal Amplification: The target region (e.g., SARS-CoV-2 N and E genes) is amplified using Recombinase Polymerase Amplification (RPA) or LAMP at a constant temperature (37-42°C), eliminating the need for a thermal cycler.
- CRISPR-Cas12 Detection: The amplified product is mixed with:
- Cas12 Enzyme
- Target-specific gRNA
- Fluorescent Reporter Probes
- Incubation & Reaction: The mixture is incubated at 37°C for ~30 minutes. If the target viral sequence is present, Cas12/gRNA complex binds and cleaves it, activating collateral cleavage of the reporter and emitting fluorescence.
- Result Readout: Fluorescence can be measured with a portable fluorometer or visualized on a lateral flow dipstick, providing a visual yes/no result.
Portable Smartphone-Based Biosensors
Principle: Surface Plasmon Resonance (SPR) detects biomolecular interactions in real-time by monitoring changes in the refractive index on a thin gold sensor surface. Miniaturized, smartphone-based SPR (iSPR) systems leverage the phone's camera and processing power to function as a portable lab [88].
Protocol for Hazelnut Allergen Detection with Smartphone iSPR [88]:
- Sensor Functionalization: A disposable microfluidic SPR chip is coated with antibodies specific to the hazelnut allergen protein (e.g., Cor a 1).
- Sample Preparation: Plant-based milk samples are diluted 10x in an appropriate buffer.
- Baseline Establishment: The buffer is flowed through the microfluidic channel while the smartphone iSPR records a baseline signal.
- Sample Injection & Binding: The prepared sample is injected. If the allergen is present, it binds to the immobilized antibodies, causing a measurable shift in the SPR angle.
- Real-Time Monitoring: The smartphone app records the sensorgram (response vs. time) in real-time.
- Regeneration: The surface is regenerated with a mild acid or buffer to remove bound analyte for chip re-use.
- Data Analysis: The smartphone software calculates the allergen concentration based on the signal intensity, achieving limits of detection as low as 0.04 µg/mL in various plant-based milks [88].
Peptide Epitope-Based Multiplexed Allergy Diagnostic
Principle: This novel approach uses short, synthesized peptide sequences (epitopes) instead of full allergen proteins, immobilized on an SPR chip. It detects and differentiates individual patients' allergen-specific antibody (IgE/IgG) profiles, enabling highly personalized diagnostics [91].
Protocol for Multiplexed Allergy Assessment [91]:
- Chip Functionalization: An SPR sensor chip is coated with a low-fouling background. Multiple flow channels are individually immobilized with distinct peptide epitopes for allergens like peanut and hazelnut using click chemistry.
- Sample Introduction: A small volume of patient serum is injected into the microfluidic system and flows over the peptide-coated channels.
- Antibody Binding: Allergen-specific IgE and IgG antibodies from the serum bind to their corresponding peptide epitopes.
- Signal Acquisition: The portable SPR instrument (e.g., MarkerSense) monitors antibody binding in real-time across all channels simultaneously.
- Multidimensional Analysis: An innovative analysis of the entire sensing area generates a unique antibody binding signature for the patient. This pattern distinguishes between mere sensitization and clinical allergy and can discern different sera related to the same allergen [91].
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful development and deployment of POC biosensors rely on a suite of specialized reagents and materials.
Table 3: Key Research Reagent Solutions for Biosensor Development
| Reagent/Material | Function in Experiment | Specific Example |
|---|---|---|
| Cas Effector Proteins [86] | Target-specific nucleic acid recognition and collateral cleavage for signal generation. | Cas12a, Cas13a used in DETECTR and SHERLOCK systems. |
| Guide RNA (gRNA) [86] | Programs the Cas protein to bind to a specific DNA or RNA target sequence. | ~20-30 nt RNA sequence complementary to SARS-CoV-2 gene. |
| Peptide Epitopes [91] | Serve as minimal, specific recognition elements for patient antibodies, enabling personalized diagnostics. | Synthesized peptides like EO14 (SDQNKVLQPH) for hazelnut allergy. |
| Low-Fouling Surface Coatings [91] | Minimize non-specific adsorption of proteins or other biomolecules to the sensor surface, improving signal-to-noise ratio. | OptoDex for photo-immobilization; carboxymethylated dextran. |
| Nanoparticles [63] | Enhance signal transduction, improve electrochemical response, or increase surface area for bioreceptor immobilization. | Gold nanoparticles (AuNPs), graphene, quantum dots. |
| Fluorescent Reporters [89] | Provide a detectable signal upon a positive binding or cleavage event. | AlexaFluor 647, quenched nucleic acid probes (FQ-reporters). |
Critical Analysis and Research Implications
The experimental data demonstrates a clear trend: while conventional methods like RT-PCR and ELISA remain gold standards for sensitivity, advanced biosensors are rapidly closing this gap while offering unparalleled advantages in speed, cost, and portability.
- Speed and Portability: CRISPR assays can deliver results in 30-60 minutes outside a lab setting [86], while a portable fluorescence reader can achieve readout in about one second [89]. The miniaturization of complex technologies like SPR into smartphone-based platforms marks a significant leap toward true POC deployment [88].
- Cost-Effectiveness: Economic evaluations confirm that RDTs can be cost-effective or even cost-saving in low-resource settings, particularly when considering broader healthcare costs [87] [92]. The significantly lower manufacturing cost of portable readers (up to 40x less than commercial systems) further underscores this advantage [89].
- The Future is Multiplexed and Personalized: The shift from detecting a single analyte to multiplexed panels, as seen in the 88-plex allergen screening [89] and peptide-epitope mapping [91], represents the future of diagnostics. This allows for comprehensive patient profiling and more informed clinical decisions.
In conclusion, the evidence strongly supports the real-world applicability of biosensors for POC use. The ongoing integration of these platforms with machine learning for data analysis and the continued development of low-cost materials will further solidify their role in revolutionizing diagnostic medicine [86].
Food allergy has become a critical global public health issue, with increasing prevalence affecting individuals of all ages and imposing a heavy burden on healthcare systems and patient quality of life [8] [1]. Since complete avoidance of allergenic foods remains the only effective prevention method for susceptible individuals, accurate detection and labeling of food allergens is paramount for consumer protection [8] [2]. The global regulatory landscape reflects this concern, with various jurisdictions mandating allergen labeling for major allergenic foods, though the specific requirements and thresholds vary significantly [57] [2]. The European Union requires declaration of 14 major allergens, the United States focuses on the "big eight," while Japan employs a tiered system of mandatory and recommended labeling with a defined threshold of 10 μg allergen protein per gram of food [57]. This patchwork of regulatory approaches underscores the challenges in establishing universal standards for allergen detection and management.
Within this complex landscape, conventional detection methods like enzyme-linked immunosorbent assay (ELISA), polymerase chain reaction (PCR), and liquid chromatography-tandem mass spectrometry (LC-MS/MS) have formed the backbone of allergen testing regimes [8] [2]. These established techniques offer recognized reliability but present limitations in speed, cost, portability, and applicability to on-site testing scenarios [8] [57]. Emerging biosensing technologies promise to address these limitations, offering potential for rapid, sensitive, and portable allergen detection [8] [59]. However, the transition from laboratory innovation to widespread clinical and industrial adoption faces significant hurdles related to validation, standardization, cost-effectiveness, and regulatory acceptance [93]. This article examines the performance characteristics of emerging biosensor technologies in comparison to conventional methods, with particular focus on the regulatory and standardization gaps that impede their broader adoption.
Performance Comparison: Biosensors Versus Conventional Methods
Analytical Performance Metrics
Table 1: Comparative analysis of major allergen detection technologies
| Method Type | Detection Principle | Limit of Detection | Analysis Time | Multiplexing Capability | Portability |
|---|---|---|---|---|---|
| Immunoassays (ELISA) | Antibody-antigen binding | 1–25 ppm [57] | Up to 3.5 hours [57] | Limited [8] | Low [57] |
| PCR Methods | DNA amplification | Varies by allergen | Several hours [8] | Moderate (real-time PCR) [57] | Low [8] |
| LC-MS/MS | Mass spectrometric detection | ~0.01 ng/mL for specific proteins [5] | Extensive sample preparation [8] | High [5] | Low [8] |
| Electrochemical Biosensors | Electron transfer measurement | ~0.08 ng/mL for tropomyosin [2] | Minutes to <1 hour [57] | Developing [57] | High [57] |
| Optical Biosensors | Colorimetric/fluorescence changes | 32.1 ng/mL for gliadin [94] | Minutes [8] [94] | Moderate [8] | High [8] |
| Nanozyme-based Sensors | Enzyme-mimetic catalysis | Sub-ppm levels [59] | Rapid assays [59] | Developing [59] | High [59] |
The performance comparison reveals distinct advantages and limitations for each technology category. Conventional methods like ELISA and PCR offer well-established reliability and sensitivity but require laboratory settings, trained personnel, and significant time investments [8] [57]. LC-MS/MS provides exceptional specificity and multiplexing capability for detecting specific allergenic proteins like Ara h 3 (peanut), Bos d 5 (milk), and tropomyosin (shellfish), with detection limits as low as 0.01 ng/mL, but requires costly equipment and extensive sample preparation [8] [5]. Biosensors demonstrate superior performance in rapidity and portability, with electrochemical biosensors achieving impressive detection limits rivaling traditional methods, and optical biosensors offering simple visual detection suitable for field applications [8] [57] [94]. Nanozyme-based sensors represent a particularly promising advancement, offering enhanced stability compared to natural enzymes while maintaining high catalytic efficiency for signal amplification [59].
Practical Implementation Considerations
Table 2: Practical implementation characteristics of detection methods
| Method Type | Cost Per Analysis | Ease of Use | Sample Throughput | Matrix Effects Resistance | Regulatory Acceptance |
|---|---|---|---|---|---|
| Immunoassays (ELISA) | Moderate (commercial kits) [57] | Moderate training required [57] | High with automation [57] | Susceptible to processing effects [57] | High (established standards) [2] |
| PCR Methods | Moderate to high [57] | Specialized training needed [8] | Moderate to high [57] | DNA stability advantage [2] | Established in some regions [2] |
| LC-MS/MS | High (equipment and operation) [8] | Extensive expertise required [8] | High [5] | High with proper sample prep [5] | Growing acceptance [5] |
| Portable Biosensors | Low to moderate [8] | Minimal training [8] [94] | Low to moderate [93] | Varies; requires validation [93] | Limited (emerging technology) [93] |
| Lab-on-a-Chip Biosensors | Moderate (device cost) [8] | Moderate simplicity [8] | Moderate [8] | Integration helps mitigation [8] | Early development stage [8] |
Beyond analytical performance, practical implementation factors significantly influence method selection and adoption. Conventional methods benefit from established infrastructure, standardized protocols, and regulatory acceptance, but incur substantial costs for equipment, reagents, and trained personnel [8] [57]. Biosensors offer compelling advantages in operational simplicity, reduced analysis time, and potential for cost-effective deployment in non-laboratory settings [8]. However, issues with sample throughput, matrix effects in complex food systems, and limited regulatory acceptance currently restrict their widespread implementation [93]. The integration of biosensors with portable platforms like lateral flow assays (LFAs), microfluidic chips, and paper-based devices represents a promising direction for overcoming these limitations, enabling rapid, on-site screening with minimal sample preparation [8].
Experimental Protocols: From Conventional to Emerging Methods
Standard ELISA Protocol for Allergen Detection
The enzyme-linked immunosorbent assay (ELISA) remains the gold standard for quantitative allergen detection due to its sensitivity, specificity, and standardization capability [57] [2]. A typical sandwich ELISA protocol for food allergen detection proceeds as follows: First, a 96-well plate is coated with capture antibody specific to the target allergen (e.g., anti-Ara h 1 for peanut detection) in carbonate/bicarbonate coating buffer (pH 9.6) and incubated overnight at 4°C. The plate is then washed with phosphate-buffered saline containing Tween 20 (PBST) to remove unbound antibodies. Blocking is performed using 1-5% bovine serum albumin (BSA) or non-fat dry milk in PBS to prevent non-specific binding, with incubation for 1-2 hours at 37°C. Food samples are prepared through extraction in PBS or specialized extraction buffers, with potential additional steps for defatting or clarification for complex matrices [57].
After another washing step, samples and standards are added to the plate and incubated for 1-2 hours at 37°C to allow allergen binding to the capture antibody. The plate is washed again, followed by addition of enzyme-conjugated detection antibody (typically horseradish peroxidase or alkaline phosphatase conjugates) and incubation for 1-2 hours at 37°C. Unbound detection antibody is removed by washing, and substrate solution (e.g., TMB for HRP or pNPP for AP) is added. Color development is stopped after 15-30 minutes using stop solution (e.g., sulfuric acid for TMB), and absorbance is measured using a plate reader [57] [2]. The entire process requires 3-4 hours with additional time for sample preparation, and results are quantified against a standard curve generated from known allergen concentrations.
Aptamer-Based Colorimetric Biosensor for Gliadin Detection
A representative emerging biosensor protocol for gluten detection illustrates the methodological differences and advantages of novel approaches [94]. This label-free aptamer-based colorimetric biosensor utilizes gold nanoparticles (AuNPs) functionalized with gliadin-specific aptamers. The experimental workflow begins with synthesis of citrate-capped AuNPs (~13 nm diameter) using the Turkevich method, followed by characterization through UV-Vis spectroscopy and transmission electron microscopy. Gliadin-binding aptamers are synthesized and purified through HPLC, then functionalized with thiol groups for AuNP conjugation. Aptamer immobilization on AuNPs is performed in Tris-EDTA buffer with gradual salt aging to optimize surface density and maintain nanoparticle stability [94].
For gliadin detection, food samples (bread, cookies, pasta) are extracted using 60% ethanol solution with vigorous mixing and centrifugation. The extracted supernatant is mixed with aptamer-functionalized AuNPs and incubated for 10-15 minutes at room temperature. Sodium chloride solution is then added to a final concentration of 50 mM, and the mixture is incubated for an additional 5 minutes. In the absence of gliadin, the aptamers maintain AuNP dispersion against salt-induced aggregation, resulting in a red color. When gliadin is present, it binds to the aptamers, reducing their protective effect and allowing salt-induced aggregation that produces a color shift to blue [94]. The color change is quantified through UV-Vis spectroscopy by measuring the ratio of absorbance at 520 nm and 620 nm, or in some implementations, visually assessed for rapid screening. This method achieves detection limits of 32.1 ng/mL within 20 minutes total analysis time, demonstrating significant advantages in speed and simplicity compared to traditional ELISA [94].
Figure 1: Experimental workflow for aptamer-based colorimetric biosensor
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key research reagents and materials for allergen detection development
| Reagent/Material | Function and Importance | Representative Examples |
|---|---|---|
| Bio-recognition Elements | Molecular components that specifically bind target allergens; determine assay specificity | Antibodies (monoclonal/polyclonal) [8], aptamers [94], DNA probes [57], molecularly imprinted polymers [8] |
| Signal Transduction Elements | Convert molecular recognition into measurable signals; determine detection sensitivity | Enzymes (HRP, ALP) [57], fluorophores [8], electroactive probes [57], nanozymes [59], gold nanoparticles [94] |
| Nanomaterials | Enhance signal amplification, improve immobilization, increase stability | Gold nanoparticles [94], graphene oxide [2], carbon nanotubes [57], quantum dots [2], metal-organic frameworks [2] |
| Platform Substrates | Physical support for assay construction; determine format and application setting | Lateral flow strips [8], microfluidic chips [8], paper-based devices [8], screen-printed electrodes [57] |
| Reference Materials | Enable method calibration, validation, and standardization; essential for quantitative accuracy | Certified allergen reference materials [57], purified allergen proteins [2], stable isotope-labeled peptides [2] |
The development and implementation of effective allergen detection methods relies on a sophisticated toolkit of reagents and materials. Bio-recognition elements form the foundation of assay specificity, with antibodies offering high affinity but potential batch-to-batch variability, while aptamers provide superior stability and reproducibility but may require extensive selection processes [8] [94]. Signal transduction elements determine detection sensitivity, with traditional enzymes offering high catalytic efficiency but limited stability, and emerging nanozymes providing enhanced stability while maintaining catalytic activity [59] [57]. Nanomaterials play increasingly important roles in signal amplification and stability enhancement, with gold nanoparticles enabling simple colorimetric detection, while graphene and carbon nanomaterials enhance electrochemical sensing performance [57] [94]. Platform substrates define the operational format, with lateral flow devices offering ultimate simplicity for field use, while microfluidic chips enable sophisticated fluid handling and multiplexing capabilities [8]. Reference materials remain critically important for method validation and standardization, yet their limited availability and high cost represent significant barriers to method harmonization and regulatory acceptance [57].
Regulatory and Standardization Challenges
The adoption of biosensor technologies in clinical and industrial settings faces substantial regulatory and standardization hurdles that extend beyond technical performance characteristics. A primary challenge lies in the validation of biosensor performance for real-world samples, where matrix effects from complex food compositions can significantly impact detection accuracy and reliability [93]. While laboratory demonstrations often utilize purified allergen preparations or simple matrices, transition to commercial applications requires extensive validation across diverse food products with varying protein, fat, carbohydrate, and preservative content [93] [57]. This validation process demands substantial resources and represents a significant barrier for technology developers, particularly small enterprises and academic spin-offs.
The regulatory landscape itself presents challenges through fragmentation and inconsistency across jurisdictions. Differing allergen labeling requirements, varying lists of mandatory allergens, and disparate threshold definitions create a complex environment for method validation and standardization [57] [2]. While Japan has established a specific threshold of 10 μg allergen protein per gram of food with defined official methods, most regions lack standardized thresholds and validation protocols [57]. This regulatory patchwork complicates the development of universal biosensor platforms and increases the cost of market entry across different geographical regions.
Additionally, the clinical and food safety communities demonstrate justifiable conservatism regarding new technologies, particularly where public health implications are significant [93]. This conservatism, coupled with substantial existing investment in conventional laboratory infrastructure, creates resistance to technological disruption. As noted in assessments of biosensor implementation challenges, "the clinical community is regarded to be particularly conservative as it pertains to the introduction of new technologies" [93]. Overcoming this resistance requires not only demonstrated technical superiority but also compelling economic arguments regarding cost-per-test, operational efficiency, and potential for reduced recall incidents.
The integration of biosensors with existing quality systems and regulatory frameworks presents further challenges. Traditional methods like ELISA benefit from extensive performance data, standardized protocols, and established proficiency testing programs [57] [2]. Biosensors must demonstrate comparable reliability while addressing unique considerations such as shelf-life stability of biological recognition elements, reader calibration and maintenance, operator training requirements, and data integrity management [93]. These factors collectively contribute to the significant gap between laboratory demonstration of biosensor capability and widespread clinical or industrial adoption.
Biosensor technologies demonstrate compelling advantages for allergen detection, including rapid analysis times, portability for on-site testing, minimal sample preparation requirements, and potential for cost-effective deployment [8]. Performance metrics for emerging biosensors increasingly rival those of conventional methods, with detection sensitivities approaching or exceeding established techniques and significant improvements in analysis speed [8] [94]. However, the transition from promising technology to widespread adoption requires addressing significant challenges in validation standardization, regulatory alignment, and integration with existing quality systems.
Bridging this adoption gap will require coordinated efforts across multiple stakeholders. Technology developers must prioritize real-world validation in complex matrices and address practical implementation considerations such as shelf-life, batch-to-batch reproducibility, and user-friendly design [93]. Regulatory agencies should work toward harmonized requirements and standardized validation protocols to reduce market entry barriers [57] [2]. The research community can contribute through development of certified reference materials, inter-laboratory validation studies, and objective performance comparisons [57]. End-users in clinical and industrial settings play a crucial role by providing practical requirements guidance and participating in field validation studies.
The future trajectory of allergen detection likely involves hybrid approaches, where biosensors provide rapid screening capabilities while conventional methods confirm positive results and provide quantitative validation [8] [5]. Advances in complementary technologies, including artificial intelligence for data interpretation, smartphone integration for result reporting, and cloud connectivity for data management, will further enhance the value proposition of biosensor platforms [5]. As these technologies mature and validation databases expand, biosensors are positioned to play increasingly important roles in allergen detection ecosystems, ultimately enhancing consumer protection through more accessible, rapid, and cost-effective monitoring capabilities.
Conclusion
Biosensing technologies demonstrate a compelling value proposition for allergen detection, offering significant advantages in speed, portability, and potential for point-of-care use compared to conventional methods. While challenges in standardization, robustness in complex matrices, and seamless integration with sample preparation remain, the trajectory of innovation is clear. Future progress hinges on developing multiplexed detection systems, creating universal sample preparation protocols, and establishing rigorous validation standards. The convergence of biosensors with advanced materials, microfluidics, and data science is poised to unlock unprecedented capabilities in predictive risk management, personalized allergy management, and intelligent, distributed monitoring systems, ultimately transforming public health and safety protocols.
References
- 1. Advances in Food Processing Techniques for Allergenicity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12651889/]
- 2. Research progress on detection methods for food allergens [https://www.sciencedirect.com/science/article/abs/pii/S0889157524009402]
- 3. CRISPR-based peanut allergen detection: Targeting Ara h1 ... [https://biotreks.org/e202539/]
- 4. Recent Advances in Electrochemical Sensing Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313194/]
- 5. Innovations shaping the future of food allergen testing [https://allergenbureau.net/innovations-shaping-the-future-of-food-allergen-testing/]
- 6. a promising analytical tool for on-site detection of mycotoxins [https://www.nature.com/articles/s41538-025-00444-5]
- 7. Biosensors, Volume 15, Issue 5 (May 2025) – 69 articles [https://www.mdpi.com/2079-6374/15/5]
- 8. Recent progresses on emerging biosensing technologies ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224424001614]
- 9. Mass Spectrometry Advancements and Applications for ... [https://www.mdpi.com/1422-0067/25/18/9880]
- 10. Comparison of Methods Study between a Photonic Crystal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5677296/]
- 11. Critical overview on the application of sensors and biosensors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7112812/]
- 12. Clinical Performance of the Standard Q COVID-19 Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8203442/]
- 13. Non-targeted LC-MS and CE-MS for biomarker discovery ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969721040845]
- 14. Impact of LC-MS/MS quantification methods on analytical ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969723030462]
- 15. A challenge in biosensors: Is it better to measure a photon ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566320300907]
- 16. Point-of-care biosensors for infectious disease diagnosis [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03897a?page=search]
- 17. Aptamer-based electrochemical biosensors: Signal ... [https://www.sciencedirect.com/science/article/pii/S2666053925000840]
- 18. Experimental data supporting DNA aptamer recognition of ... [https://www.frdr-dfdr.ca/repo/dataset/3a97cb68-60a8-41f1-b51a-09111f678d47]
- 19. Biosensors, Volume 15, Issue 9 (September 2025) [https://www.mdpi.com/2079-6374/15/9]
- 20. Silver Nanoparticles for Biosensing and Drug Delivery [https://pubmed.ncbi.nlm.nih.gov/40422070/]
- 21. Challenges and Opportunities in Smart Biosensing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455640/]
- 22. The measures of biosensor performance and how to ... [https://blog.igii.uk/the-measures-of-biosensor-performance-and-how-to-improve-accuracy]
- 23. When lower isn't always better in biosensor research and ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566324006766]
- 24. Review of Methods for the Detection of Allergens in Novel ... [https://science.food.gov.uk/article/125903-review-of-methods-for-the-detection-of-allergens-in-novel-food-alternative-proteins]
- 25. Everything's under Control: Maximizing Biosensor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11840803/]
- 26. Performance metrics and enabling technologies for ... [https://www.nature.com/articles/s41467-018-06419-3]
- 27. A Rapid, Non-Invasive Approach to Breast Cancer Screening [https://www.mdpi.com/2079-6374/15/6/386]
- 28. Detecting egg white allergens using bio/nano-sensors; a ... [https://www.sciencedirect.com/science/article/abs/pii/S0001868625001794]
- 29. Electrochemical Biosensors - Sensor Principles and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3663003/]
- 30. Emerging electrochemical biosensing approaches for ... [https://www.sciencedirect.com/science/article/abs/pii/S0924224422000474]
- 31. Biomedical Applications of an Ultra-Sensitive Surface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496527/]
- 32. CdSe-ZnCdS quantum dot-assisted fiber-optic SPR sensor ... [https://www.sciencedirect.com/science/article/pii/S2949822825009189]
- 33. Biosensing Using SERS Active Gold Nanostructures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8539114/]
- 34. Controlling parameters and characteristics of ... [https://www.nature.com/articles/s41598-019-43680-y]
- 35. Paper-based microfluidics: Simplified fabrication and assay ... [https://www.sciencedirect.com/science/article/pii/S0925400521002495]
- 36. A perspective on paper-based microfluidics: Current status ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3365319/]
- 37. Evaluating the performance characteristics of five lateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9130972/]
- 38. Evaluation of SARS-CoV-2 lateral flow device sensitivity [https://www.sciencedirect.com/science/article/pii/S2589537025003864]
- 39. A Critical Comparison between Flow-through and Lateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6956089/]
- 40. A comprehensive review of competitive lateral flow assays ... [https://pubs.rsc.org/en/content/articlehtml/2025/lc/d4lc01075b]
- 41. A Microfluidic Paper-Based Lateral Flow Device for ... [https://www.mdpi.com/2673-8023/4/2/22]
- 42. Allergen Tests: An Honest Comparison of Four Lateral ... [https://www.klipspringer.com/blogs/allergen-tests-lateral-flow-tests/]
- 43. Lab on chip for medical and clinical applications [https://pubs.rsc.org/en/content/articlehtml/2025/sd/d5sd00096c]
- 44. Food Allergenicity Evaluation Methods: Classification, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191692/]
- 45. Review of allergen analytical testing methodologies [https://www.food.gov.uk/research/review-of-allergen-analytical-testing-methodologies-allergen-detection-methods-unbiased-literature-search]
- 46. Review of Electrochemical Biosensors for Food Safety Detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC9688552/]
- 47. fulfilling the promise of lab-on-a-chip technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10964744/]
- 48. Microfluidics chips fabrication techniques comparison [https://www.nature.com/articles/s41598-024-80332-2]
- 49. Introduction to lab-on-a-chip 2024: review, history and future [https://elveflow.com/microfluidic-reviews/introduction-to-lab-on-a-chip-review-history-and-future/]
- 50. Electrochemical Biosensors in Food Safety: Challenges ... [https://www.mdpi.com/1420-3049/26/10/2940]
- 51. High Throughput Screening Market Size & Trends | 2033 [https://straitsresearch.com/report/high-throughput-screening-market]
- 52. 2025 High Throughput Screening (HTS) Industry Trends ... [https://www.openpr.com/news/4125058/2025-high-throughput-screening-hts-industry-trends-report]
- 53. The Future of Biomanufacturing: IDTechEx Explores White ... [https://www.idtechex.com/en/research-article/the-future-of-biomanufacturing-idtechex-explores-white-biotechnology/33114]
- 54. Frontiers in biofoundry: opportunities and challenges [https://www.frontiersin.org/journals/synthetic-biology/articles/10.3389/fsybi.2025.1630026/full]
- 55. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 56. High Throughput Screening Market Size, Share Report [https://www.thebusinessresearchcompany.com/report/high-throughput-screening-hts-global-market-report]
- 57. Recent Advances in Electrochemical Sensing Strategies ... [https://www.mdpi.com/2079-6374/12/7/503]
- 58. A Systematic Review of Food Allergy: Nanobiosensor and ... [https://www.mdpi.com/2079-6374/10/12/194]
- 59. Enzyme- and nanozyme-based food allergen detections [https://www.sciencedirect.com/science/article/pii/S0924224425001529]
- 60. Biosensors and Bioelectronics | Vol 277, 1 June 2025 [https://www.sciencedirect.com/journal/biosensors-and-bioelectronics/vol/277/suppl/C]
- 61. Transformative biomedical devices to overcome biomatrix ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325002477]
- 62. Method development and comprehensive study of matrix ... [https://www.sciencedirect.com/science/article/pii/S0021967324008781]
- 63. A Systematic Review of Food Allergy: Nanobiosensor and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7760337/]
- 64. Sample Preparation and Analytical Techniques in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9956155/]
- 65. Reliable Strategy for Analysis of Complex Biosensor Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC6150654/]
- 66. Scalable electrochemical system for rapid on-site detection ... [https://www.sciencedirect.com/science/article/abs/pii/S0956566325000168]
- 67. Analytical Methods for Allergen Control in Food Processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10093617/]
- 68. An Experimental Method for Bio-Signal Denoising Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10098882/]
- 69. Comparison of Detection Limits for Allergenic Foods ... [https://www.sciencedirect.com/science/article/pii/S0362028X22103376]
- 70. Materials and Methods of Biosensor Interfaces With Stability [https://www.frontiersin.org/journals/materials/articles/10.3389/fmats.2020.583739/full]
- 71. Enhancing the performance of an in vitro RNA biosensor ... [https://pubmed.ncbi.nlm.nih.gov/40071731/]
- 72. A genetically encoded biosensor to monitor dynamic changes of... [https://www.nature.com/articles/s41467-024-48295-0?error=cookies_not_supported&code=405e09b9-a551-40c6-8e89-f310d907e7de]
- 73. An enzyme- responsive electrochemical DNA biosensor achieving... [https://pubmed.ncbi.nlm.nih.gov/36925289/]
- 74. AI-Enhanced Surface Functionalization in Biosensors [https://www.sciencedirect.com/science/article/abs/pii/S0165993625003887]
- 75. Enhancement and optimization of a graphene-based ... [https://www.nature.com/articles/s41598-025-20570-0]
- 76. Performance Optimization Strategies for Polymer Organic ... [https://www.mdpi.com/1424-8220/25/22/6891]
- 77. Comparative analysis of LC-MS/MS and electrochemical ... [https://pubmed.ncbi.nlm.nih.gov/41145825/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0QI_Cs_JBYsspJi5jWgmeQ3I0TQ0yjRNjyJdwscp1ao&fc=None&ff=20251106112552&v=2.18.0.post22+67771e2]
- 78. Development and performance characteristics evaluation of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8051012/]
- 79. Immuno-PCR: A high-sensitivity approach for biomarker ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898125001688]
- 80. Quantitative or digital PCR? A comparative analysis for ... [https://www.sciencedirect.com/science/article/abs/pii/S0165993624001584]
- 81. Allergens in Food: Analytical LC-MS/MS Method for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428185/]
- 82. Graphene biosensors outcompete ELISA and Simoa for ... [https://www.graphenea.com/blogs/graphene-news/graphene-biosensors-outcompete-elisa-and-simoa-for-point-of-care-diagnostics?srsltid=AfmBOoqUr-SIzpPt_xx2zrpVu9ifrxDvBghHue60mRbEpEXwxtuKPzrA]
- 83. Biosensing Based on Nanoparticles for Food Allergens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5948517/]
- 84. A comparison of optical, electrochemical, magnetic, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6736529/]
- 85. Allergen Microarrays and New Physical Approaches to ... [https://www.mdpi.com/2079-6374/14/7/353]
- 86. Recent developments and future directions in point-of-care ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717804/]
- 87. Cost & Cost-Effectiveness of Implementing SD Biosensor ... [https://www.medrxiv.org/content/10.1101/2023.01.05.23284225v1]
- 88. A portable smartphone-based imaging surface plasmon ... [https://www.sciencedirect.com/science/article/pii/S0039914023001170]
- 89. Portable Fluorescence Biosensing System for Low-Cost ... [https://www.mdpi.com/2504-3900/97/1/173]
- 90. Allergy Amulet [https://www.allergyamulet.com/]
- 91. Point-of-care personalized rapid diagnosis of allergies ... [https://www.sciencedirect.com/science/article/abs/pii/S092540052401089X]
- 92. Cost-effectiveness of COVID rapid diagnostic tests for patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11293649/]
- 93. Challenges in the application of biosensor technology ... [https://www.frontiersin.org/journals/sensors/articles/10.3389/fsens.2025.1641221/full]
- 94. Can Biosensors Replace ELISA For Measuring Gluten In ... [https://allergenbureau.net/can-biosensors-replace-elisa-for-measuring-gluten-in-foods/]