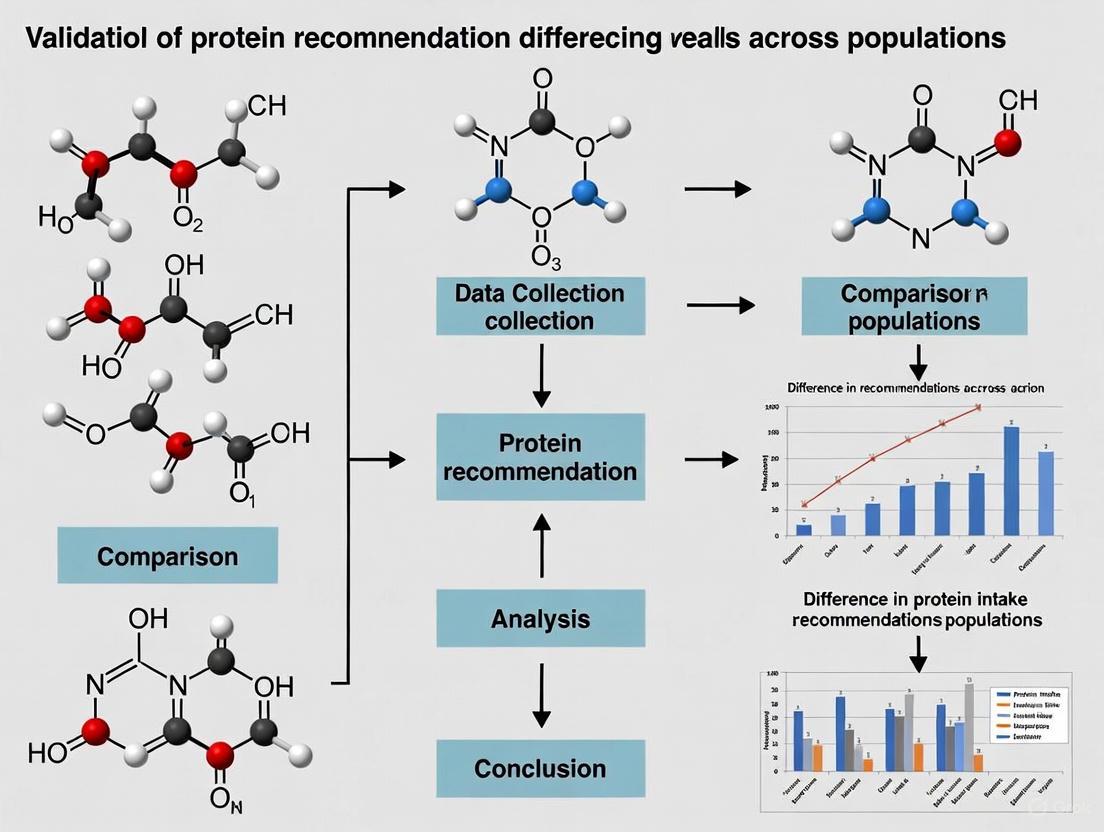
Beyond One-Size-Fits-All: Validating Protein Recommendations for Diverse Populations in Biomedical Research
Current dietary protein recommendations, largely based on outdated nitrogen balance studies, fail to account for the distinct physiological needs of different populations.
Beyond One-Size-Fits-All: Validating Protein Recommendations for Diverse Populations in Biomedical Research
Abstract
Current dietary protein recommendations, largely based on outdated nitrogen balance studies, fail to account for the distinct physiological needs of different populations. This article explores the critical need for validating and modernizing protein intake guidelines for specific demographic and clinical groups, including older adults, athletes, and individuals with metabolic conditions. We examine the limitations of existing recommendation frameworks, evaluate novel methodological approaches for protein requirement assessment, and discuss strategies for optimizing and validating protein intake protocols. By synthesizing evidence from recent meta-analyses, indicator amino acid oxidation studies, and clinical outcomes research, this review provides a roadmap for developing population-specific protein recommendations that support musculoskeletal health, metabolic function, and overall wellness in both research and clinical applications.
The Evolving Science of Protein Requirements: From Historical Benchmarks to Population-Specific Needs
The Recommended Dietary Allowance (RDA) for protein, established at 0.8 grams per kilogram of body weight per day (g/kg/d) for healthy adults, has remained fundamentally unchanged for decades despite significant advancements in nutritional science. This review critically examines the nitrogen balance methodology underpinning this recommendation and evaluates emerging evidence challenging its universal adequacy. We analyze limitations inherent in nitrogen balance studies, including population representativeness, methodological assumptions, and inadequate consideration of protein quality. Comparative data from alternative methodologies and functional outcome studies are synthesized, revealing that protein requirements may be substantially higher for specific populations, including older adults, vegans, and physically active individuals. This analysis concludes that a re-evaluation of current protein recommendations is warranted to reflect contemporary scientific evidence.
The current protein RDA of 0.8 g/kg/d primarily derives from nitrogen balance studies conducted in the mid-20th century, representing the intake sufficient to maintain nitrogen equilibrium in 97.5% of the population [1]. Nitrogen balance methodology calculates the difference between nitrogen ingested (primarily from dietary protein) and nitrogen excreted (in urine, feces, and other routes), with equilibrium achieved when intake matches losses [2]. While this approach has served as the historical gold standard for determining protein requirements, its limitations have become increasingly apparent as nutritional science has evolved.
Recent evidence challenges the universal applicability of the current RDA. Multiple lines of investigation—including re-analyses of original nitrogen balance data, studies employing the indicator amino acid oxidation (IAAO) technique, and research demonstrating functional benefits of higher protein intakes—suggest that the existing recommendations may be insufficient for optimizing health outcomes across diverse populations [3]. This review systematically evaluates the methodological constraints of nitrogen balance studies and synthesizes contemporary evidence supporting a re-evaluation of protein requirements to better reflect physiological needs for muscle maintenance, metabolic function, and overall health throughout the life course.
Foundations of Current Protein Recommendations
The Nitrogen Balance Methodology
Nitrogen balance determination relies on the principle that protein is the primary nitrogen-containing macronutrient, enabling protein status assessment through precise measurement of nitrogen intake and excretion. The fundamental equation is:
Nitrogen Balance (B) = Nitrogen Intake (I) - Nitrogen Losses (U + F + S)
Where U represents urinary nitrogen, F represents fecal nitrogen, and S represents integumental and other miscellaneous losses [2]. In healthy adults, nitrogen equilibrium (balance ≈ 0) indicates that protein intake matches requirements for maintaining body protein pools. The current RDA was derived from the estimated average requirement (EAR) of 0.66 g/kg/d, with the RDA calculated as EAR + 2 standard deviations to cover the needs of 97.5% of the population [4].
The 2002 meta-analysis by Rand et al. [4] of 235 individual subjects from 19 nitrogen balance studies established the foundation for current recommendations. This analysis reported a median EAR of 105 mg N·kg⁻¹·d⁻¹ (0.65 g protein·kg⁻¹·d⁻¹) and an RDA of 132 mg N·kg⁻¹·d⁻¹ (0.83 g protein·kg⁻¹·d⁻¹), rounded to 0.8 g/kg/d. Notably, this analysis concluded no significant differences in requirements based on age, sex, or dietary protein source, though plant-based diets were underrepresented [4].
Key Nitrogen Balance Studies Underpinning the RDA
Table 1: Foundational Nitrogen Balance Studies Informing Current Protein Recommendations
| Study/Reference | Population | Design | Key Findings | Limitations |
|---|---|---|---|---|
| Rand et al. (2002) meta-analysis [4] | 235 adults from 19 studies | Nitrogen balance analysis across multiple intakes | EAR: 0.65 g/kg/d; RDA: 0.83 g/kg/d | Limited representation of plant-based diets; narrow population |
| Original FAO/WHO/UNU (1985) | Mixed | Nitrogen balance | Established previous international standards | Methodological limitations in individual studies |
| "Vegetable diet" studies in Rand analysis [2] | Diets with >90% plant protein | Nitrogen balance | Average nitrogen balance: -2.21 mg N·kg⁻¹·d⁻¹ | Contained up to 10% animal protein; not strictly vegan |
Methodological Limitations of Nitrogen Balance Studies
Technical and Measurement Challenges
Nitrogen balance methodology contains systematic biases that tend to overestimate nitrogen retention and consequently underestimate true protein requirements. These technical limitations include:
- Overestimation of Nitrogen Intake: Analytical errors in determining the nitrogen content of diets lead to systematic overestimation of intake [3].
- Underestimation of Nitrogen Losses: Incomplete collection of urinary and fecal nitrogen, coupled with unmeasured integumental (skin, sweat, hair, nails) and other miscellaneous losses (estimated at 5-8 mg N·kg⁻¹·d⁻¹), results in underestimation of total nitrogen excretion [3] [5].
- Adaptation Periods: The relatively short adaptation periods (typically 5-14 days) used in nitrogen balance studies may be insufficient for the body to fully adjust to new protein intake levels, particularly at lower intakes where metabolic adaptation can create a false appearance of equilibrium [3].
These methodological shortcomings collectively bias nitrogen balance toward positivity, suggesting adequate protein intake at levels that may be insufficient for long-term maintenance of body protein pools.
Population Representativeness and Generalizability
The populations studied in foundational nitrogen balance research lack diversity in ways that critically limit the generalizability of the resulting RDA:
- Age Bias: Studies predominantly featured young adults (typically college-aged), despite evidence that protein metabolism and requirements change significantly with aging due to anabolic resistance [5].
- Sex Imbalance: Male participants were overrepresented, with limited investigation of potential sex-based differences in protein requirements [5].
- Health Status: Participants were generally healthy and lean, excluding those with conditions that might alter protein metabolism [5].
- Limited Physical Activity: Studies often used sedentary individuals, failing to account for the increased protein needs of physically active populations [3].
- Underrepresentation of Vegetarian/Vegan Populations: The meta-analysis by Rand et al. included "vegetable diets" but these contained up to 10% animal protein, not reflecting strict vegetarian or vegan patterns [2].
Diagram 1: Methodological Limitations of Nitrogen Balance Studies
Conceptual and Interpretative Flaws
Beyond technical issues, nitrogen balance methodology suffers from fundamental conceptual limitations:
- Linearity Assumption: The relationship between nitrogen intake and balance is inherently curvilinear, with decreasing efficiency of protein utilization as zero balance is approached. Application of linear regression models to this relationship violates this physiological reality and may underestimate requirements [3].
- Adequacy Versus Optimization: Nitrogen balance establishes the minimum protein intake to prevent deficiency but provides no information about optimal intakes for physiological functions beyond equilibrium, such as muscle hypertrophy, immune function, or metabolic health [1] [5].
- Protein Quality Considerations: The RDA assumes consumption of high-quality, highly digestible protein with optimal amino acid composition (e.g., egg, milk). Plant proteins typically have lower digestibility and less optimal amino acid profiles, necessitating higher intakes to achieve equivalent nitrogen balance [2] [6].
Evidence Challenging the Current RDA
Studies in Specific Populations
Vegan and Plant-Based Populations
A 2023 controlled feeding study specifically investigated nitrogen balance in strict vegan men consuming exactly 0.8 g/kg/d of protein from mixed plant sources [2]. Both absolute nitrogen balance (-1.38 ± 1.22 g/d) and relative nitrogen balance (-18.60 ± 16.96 mg/kg/d) were significantly lower than zero (equilibrium), demonstrating that the current RDA is insufficient to maintain nitrogen balance in this population. This contrasts with the original Rand meta-analysis that included diets with up to 10% animal protein and highlights how protein quality affects requirements [2].
Older Adults
Multiple lines of evidence indicate increased protein requirements with aging. Short-term nitrogen balance studies suggest the protein RDA is inadequate for maintaining nitrogen equilibrium in older adults [6]. Retrospective analyses indicate nitrogen equilibrium is achieved at approximately 0.91 g/kg/d—15% higher than the current RDA [6]. Studies using the IAAO technique report increased protein requirements in older adults compared with younger counterparts [6]. This has led to calls from expert groups for protein intake recommendations of 1.2-1.7 g/kg/d for older adults to support muscle mass maintenance and prevent sarcopenia [6].
Physically Active Individuals
Meta-analyses of randomized controlled trials demonstrate that protein intakes greater than the RDA (typically 1.2-1.7 g/kg/d) differentially influence body composition under catabolic or anabolic conditions [7]. Specifically, protein intakes exceeding the RDA attenuate lean mass loss during energy restriction and increase lean mass during resistance training, whereas the RDA appears sufficient only under non-stressed conditions without exercise or calorie restriction [7].
Table 2: Protein Requirements Across Populations Based on Contemporary Evidence
| Population | Current RDA (g/kg/d) | Evidence-Based Suggested Intake (g/kg/d) | Key Evidence |
|---|---|---|---|
| Healthy Young Adults | 0.8 | 0.8-1.2 | RDA sufficient for basic equilibrium in non-stressed state [7] |
| Older Adults | 0.8 | 1.2-1.7 | IAAO studies, muscle preservation trials [6] |
| Strict Vegans | 0.8 | 1.0-1.3 | Negative nitrogen balance at RDA [2] |
| Resistance-Trained | 0.8 | 1.2-1.7 | Enhanced lean mass gains in meta-analyses [7] |
| Dieting/Energy Restricted | 0.8 | 1.6-2.2 | Preservation of lean mass during deficit [7] |
Indicator Amino Acid Oxidation (IAAO) Studies
The IAAO technique has emerged as a validated alternative to nitrogen balance for estimating protein and amino acid requirements. This method measures the oxidation of a labeled indispensable amino acid, with the breakpoint in oxidation indicating the requirement. IAAO studies generally suggest higher protein requirements than nitrogen balance, particularly in older adults and athletes [3]. The latest Dietary Reference Intakes acknowledged IAAO as the gold-standard method for estimating amino acid requirements but did not fully incorporate IAAO-derived values into protein recommendations [3].
Evidence from Functional Outcomes
Studies investigating functional outcomes beyond nitrogen balance provide compelling evidence for re-evaluating the RDA:
- Muscle Mass and Function: Higher protein intakes (≥1.2 g/kg/d) are associated with greater lean mass preservation, reduced risk of sarcopenia, and better physical function in older adults [8].
- Health Status: Observational data from NHANES indicate that older adults not meeting protein recommendations have significantly more functional limitations and lower grip strength [8].
- Metabolic Health: Adequate protein intake supports glucose homeostasis through maintenance of skeletal muscle mass, the primary site of glucose disposal [5].
Experimental Approaches and Methodologies
Nitrogen Balance Protocol
A standardized nitrogen balance study typically involves:
Participants: Recruited based on specific inclusion/exclusion criteria (e.g., healthy, weight-stable, specific age range) [2].
Dietary Control: Participants receive a eucaloric diet with precisely controlled protein content for an adaptation period (typically 5-14 days). Diets are individualized to meet energy needs based on equations like Harris-Benedict with an appropriate activity factor [2].
Nitrogen Intake Assessment: All foods are weighed and analyzed for nitrogen content, typically using the Dumas method, with careful accounting of uneaten portions [2].
Nitrogen Loss Measurement:
- Urinary Nitrogen: 24-hour urine collections with refrigeration and without preservatives. The first morning void is discarded, and all urine collected for 24 hours, including the first void the following morning [2].
- Fecal Nitrogen: Collection throughout the study period or during specific balance periods using fecal markers.
- Miscellaneous Losses: Estimated based on standard values (typically 5-8 mg N·kg⁻¹·d⁻¹) for skin, sweat, hair, and nail losses [3].
Calculation: Nitrogen balance = (Nitrogen intake) - (Urinary nitrogen + Fecal nitrogen + Miscellaneous losses) [2].
Indicator Amino Acid Oxidation (IAAO) Protocol
The IAAO technique represents a more contemporary approach:
Participants: Fed diets with varying levels of the test protein or amino acid.
Tracer Administration: Receives a labeled indispensable amino acid (typically [1-¹³C]phenylalanine).
Measurements: Breath samples collected to measure ¹³CO₂ enrichment, reflecting oxidation of the labeled amino acid.
Analysis: The breakpoint in the oxidation curve indicates the requirement, as oxidation increases once the requirement is exceeded [3].
Diagram 2: Comparison of Methodological Approaches for Determining Protein Requirements
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Methods for Protein Requirement Studies
| Reagent/Equipment | Specification/Standard | Research Application | Key Considerations |
|---|---|---|---|
| Controlled Diets | Precisely formulated protein content | Provides exact nitrogen intake | Protein quality, amino acid profile, digestibility |
| Urine Collection | 24-hour containers, refrigeration | Quantifies urinary nitrogen losses | Completeness of collection, storage conditions |
| Fecal Markers | Carmine red, blue dye | Marks fecal collection periods | Accurate separation of balance periods |
| Nitrogen Analyzer | Dumas combustion method | Measures nitrogen in food, urine, feces | Calibration, standardization |
| Amino Acid Tracers | [1-¹³C]phenylalanine, L-[1-¹³C]leucine | IAAO studies to determine requirements | Isotopic purity, administration route |
| Isotope Ratio Mass Spectrometer | High-precision ¹³CO₂ measurement | IAAO breath sample analysis | Sensitivity, calibration standards |
| Body Composition Tools | DXA, BIA, ADP | Measures lean mass changes | Validation for population, precision |
The critical analysis presented herein demonstrates significant limitations in the nitrogen balance methodology underpinning current protein RDAs. Methodological biases, narrow population sampling, and conceptual flaws related to the distinction between minimal versus optimal intake collectively challenge the universal applicability of the 0.8 g/kg/d recommendation. Contemporary evidence from controlled studies in specific populations, IAAO methodology, and functional outcome research consistently indicates higher protein requirements for numerous segments of the population, particularly older adults, vegans, and those engaged in regular physical activity.
These findings highlight the urgent need to re-evaluate current protein recommendations using contemporary methodologies and with consideration of diverse populations and functional outcomes. Future dietary guidelines should incorporate evidence beyond nitrogen balance to establish protein recommendations that optimize health outcomes across the lifespan, rather than merely preventing deficiency. The scientific consensus is increasingly converging on population-specific protein recommendations that better reflect modern understanding of protein needs for health preservation and chronic disease prevention.
Dietary protein is indispensable for numerous physiological functions, including the synthesis of muscle tissue, immune cell production, and wound healing. The establishment of a universal protein Recommended Dietary Allowance (RDA) of 0.8 grams per kilogram of body weight per day (g/kg/day) has historically provided a baseline for nutritional guidance [9]. However, a growing body of evidence underscores that this one-size-fits-all recommendation is insufficient for specific demographic groups with heightened anabolic demands or altered metabolic states [10] [11]. The validation of differential protein requirements across populations is a critical endeavor in nutritional science, moving beyond mere nitrogen balance to encompass functional outcomes such as muscle strength, physical capacity, and recovery from illness. This guide objectively compares protein recommendations for aging populations and athletes, synthesizing experimental data and detailing the methodologies that underpin these evidence-based conclusions.
Quantitative Comparison of Protein Recommendations Across Populations
The following table summarizes the evidence-based protein intake recommendations for different populations, highlighting the significant deviations from the standard RDA.
Table 1: Evidence-Based Daily Protein Intake Recommendations by Population
| Population Group | Recommended Intake (g/kg/day) | Key Rationale and Evidence Base |
|---|---|---|
| General Healthy Adults (RDA) | 0.8 [9] | Based on classic nitrogen balance studies to prevent deficiency. |
| Healthy Older Adults | 1.0 - 1.2 [12] [11] | Counters anabolic resistance and age-related muscle loss (sarcopenia) [10]. |
| Older Adults with Acute/Chronic Illness | 1.2 - 1.5 [12] [11] | Supports increased demands for immune function and tissue repair. |
| Recreational Endurance Athletes | ~1.0 [13] | May not differ significantly from sedentary adults if exercise intensity is low. |
| Elite Endurance Athletes | 1.46 - 1.8 [13] | Offsets protein oxidation during prolonged exercise and aids recovery. |
| Strength/Power Athletes | 1.4 - 2.0 [9] [13] | Supports muscle protein synthesis (MPS) and adaptation to resistance training. |
For optimal anabolic stimulation, especially in older adults, research also emphasizes the importance of protein distribution, recommending 25-30 g of high-quality protein per meal to maximize Muscle Protein Synthesis (MPS) rates [12]. Furthermore, the amino acid leucine is identified as a critical trigger for MPS, with some studies suggesting that older adults may benefit from consuming 2.8–3 g of leucine per meal to overcome anabolic resistance [12].
Experimental Protocols for Determining Protein Requirements
The validation of protein recommendations relies on sophisticated metabolic techniques. The following section details the core methodologies cited in the literature.
Nitrogen Balance Technique
This method involves precisely measuring all nitrogen (N) ingested and all nitrogen excreted over a controlled period [9]. Participants consume a diet with varying, known levels of protein (nitrogen intake) for periods of 10-14 days. During the final 3-5 days, total nitrogen losses are measured from urine, feces, skin, and other miscellaneous sources [10]. Nitrogen balance is calculated as: Nitrogen Balance = Nitrogen Intake - Nitrogen Losses.
B. Data Analysis and Requirement Determination
Linear regression is performed on the different nitrogen intake levels and their corresponding balance measures. The Estimated Average Requirement (EAR) is determined by interpolating the intake level that results in zero nitrogen balance (intake = losses). The RDA is set at two standard deviations above the EAR to cover the needs of ~97.5% of the population [10].
C. Limitations
The nitrogen balance technique has recognized shortcomings. It may underestimate protein needs for optimal function, as it does not directly measure outcomes like muscle mass or physical performance [9]. The methodology itself can be prone to errors in the complete collection of nitrogen losses [10].
Indicator Amino Acid Oxidation (IAAO)
The IAAO method is considered a more dynamic and precise alternative [10]. Study participants are fed diets with varying levels of protein intake. One indispensable (essential) amino acid, typically L-[1-¹³C]phenylalanine, is labeled as the "indicator" and administered. When dietary protein is deficient, the body cannot fully utilize the indicator amino acid for protein synthesis, leading to its oxidation.
B. Data Analysis and Requirement Determination
The oxidation rate of the labeled indicator amino acid is measured by analyzing ¹³CO₂ in the breath. As protein intake approaches the individual's requirement, the body utilizes more of the indicator amino acid for synthesis, and its oxidation decreases. The breakpoint in the oxidation curve, where further protein intake no longer reduces oxidation, is identified through biphasic linear regression and represents the average protein requirement [10].
C. Key Findings
Studies using IAAO have reported higher requirements than the RDA, suggesting values of 0.94 g/kg/day for older men and 0.96 g/kg/day for older women, with safe intake levels (analogous to an RDA) of 1.24 g/kg/day and 1.29 g/kg/day, respectively [10].
Molecular Pathways and Experimental Workflows
The cellular mechanism by which protein intake stimulates muscle growth, and the experimental workflow for identifying proteins in complex mixtures, are foundational to this field.
Leucine-Mediated Muscle Protein Synthesis Signaling Pathway
The following diagram illustrates the key molecular pathway through which dietary protein, and specifically the amino acid leucine, stimulates muscle protein synthesis, a process crucial for adapting to exercise and countering age-related anabolic resistance.
Diagram Title: Leucine Activates Muscle Protein Synthesis
Shotgun Proteomics Workflow for Protein Identification
In basic research, proteomics techniques are used to understand protein expression and interactions. The shotgun proteomics workflow is a key method for identifying a wide array of proteins from biological samples.
Diagram Title: Shotgun Proteomics Identification Process
Research Reagent Solutions for Protein Metabolism Studies
The following table details key reagents and materials essential for conducting research in protein metabolism and requirements.
Table 2: Essential Research Reagents and Materials
| Research Reagent / Material | Function and Application in Research |
|---|---|
| L-[1-¹³C]Phenylalanine | A stable isotope-labeled amino acid used as the "indicator" in the IAAO technique to measure whole-body protein metabolism and determine requirements [10]. |
| Stable Isotope-Labeled Amino Acids (e.g., ¹³C-Leucine) | Used in tracer infusion studies to directly measure rates of Muscle Protein Synthesis (MPS) and breakdown in response to dietary or exercise interventions [10]. |
| Reference Protein Sources (e.g., Casein, Whey, Egg) | Highly-characterized proteins used in controlled feeding studies to compare the anabolic properties, digestibility, and amino acid bioavailability of different protein types [14]. |
| Protein Sequence Databases (e.g., UniProt) | Curated databases of protein sequences that are essential for the peptide spectrum matching step in shotgun proteomics workflows [15]. |
| Mass Spectrometer | The core instrument used in proteomics and metabolic studies for precise measurement of peptide masses (m/z) and fragmentation patterns (MS/MS) for identification [15]. |
The evidence compellingly demonstrates that protein requirements are not static but are instead dictated by demographic and physiological imperatives. The validation of increased needs for aging populations and athletes moves beyond the simplistic prevention of deficiency towards the promotion of functional health, performance, and recovery. While the RDA of 0.8 g/kg/day remains a benchmark for sedentary adults, research validates daily intakes of 1.0-1.2 g/kg for healthy older adults, 1.2-1.5 g/kg for those who are ill, and 1.4-2.0 g/kg for athletes [10] [9] [12]. Future research must continue to refine these recommendations using robust methodologies like IAAO and direct measures of MPS, with a focus on long-term functional outcomes as the primary validation metric.
Dietary protein is a critical macronutrient for human health, supporting functions from cellular structure and immune function to muscle maintenance. However, the balance between its consumption and actual physiological requirements varies dramatically across the globe, creating significant public health challenges. This guide provides a comparative analysis of global protein consumption patterns against established recommended intakes, synthesizing current data on disparities, their health implications, and the methodologies underpinning protein research. For researchers and drug development professionals, understanding these patterns is essential for designing targeted nutritional interventions and public health strategies that address both undernutrition and overconsumption. The analysis is framed within the broader context of validating differences in protein recommendations across diverse populations, highlighting that a one-size-fits-all approach is inadequate for global nutritional guidance [6].
Global Protein Consumption Patterns
Global protein consumption is characterized by profound geographical and socioeconomic disparities. In high-income countries, protein intake, particularly from animal sources, significantly exceeds average requirements. Conversely, in many low-income regions, protein intake is insufficient to meet basic physiological needs, contributing to malnutrition and its associated burdens [6] [16].
Table 1: Global and Regional Per Capita Protein Consumption Patterns
| Region/Country | Total Protein Consumption (g/person/day) | Animal Protein Contribution | Plant Protein Contribution | Key Consumption Notes |
|---|---|---|---|---|
| Global Average | ~142% of requirement [16] | ~40% of total [6] | ~60% of total [6] | Supply is sufficient if equitably distributed. |
| United States | >50% from animal products [6] | High | Lower | Men consume ~2x RDA; women ~1.5x RDA [17]. |
| United Kingdom | Animal-based dominant [6] | High | Lower | Habitual intake declines with age [6]. |
| Wealthy Regions | >50% above requirement [17] | High | Variable | 42% of global population lives in such countries [16]. |
| Sub-Saharan Africa | Among lowest globally [17] | Lower | Higher | High prevalence of protein-energy malnutrition [6] [16]. |
| Parts of Asia | Variable | Variable | Higher | West/Southern India: high reliance on rice/millet [6]. |
Consumption patterns are also influenced by gender and socioeconomic status. A 2025 cross-sectional study of Italian adults found that men had significantly higher consumption of meat and processed meat, while women consumed more plant-based proteins like soy. These gender differences persisted across socioeconomic levels, with low-income men consuming the most meat and processed meat. These dietary choices were further associated with body composition; high meat consumption correlated with a higher BMI, while soy consumption was associated with a lower BMI [18]. This illustrates that protein consumption is not merely a biological necessity but a complex behavior shaped by cultural norms, economic access, and gender identities [18].
Established Protein Recommendations and Intake Guidelines
Protein recommendations are not universal; they vary by age, physiological status, and activity level. Most national guidelines for healthy adults are based on preventing deficiency rather than optimizing long-term health.
Table 2: Summary of Protein Recommendations for Adults
| Population Group | Recommended Dietary Allowance (RDA) | Elevated/Upper Intake Level | Key Rationale and Notes |
|---|---|---|---|
| Healthy Adults (Avg.) | 0.8 g/kg/day [19] [17] | 1.0-1.6 g/kg/day for active individuals [19] | Minimum to prevent nitrogen loss; safe upper limit ~2 g/kg/day [19]. |
| Older Adults (>40-50) | 0.75-0.8 g/kg/day (UK/US RDA) [6] | 1.0-1.7 g/kg/day [6] [20] | To counteract sarcopenia (age-related muscle loss) [6] [20]. |
| Regular Exercisers | RDA: 0.8 g/kg/day | 1.1-1.5 g/kg/day [20] | Supports repair and adaptation. |
| Weightlifters/Athletes | RDA: 0.8 g/kg/day | 1.2-1.7 g/kg/day [20] | For muscle building and recovery; >2 g/kg/day is excessive [20]. |
The evidence base for these recommendations is evolving. Recent research using novel stable isotope pulse methods suggests that traditional techniques may have underestimated net protein breakdown, potentially indicating higher requirements. This new concept posits a relationship between habitual protein intake and an individual's requirements, which may be lower in older adults and those with comorbidities [21]. Furthermore, the source and quality of protein are critical. Animal proteins are generally "complete" with all essential amino acids, while most plant proteins are "incomplete." The Digestible Indispensable Amino Acid Score (DIAAS) is the preferred method for evaluating protein quality, accounting for ileal digestibility. Achieving adequate intake with plant-based diets requires consuming a variety of sources to ensure a complementary amino acid profile [6] [17].
Disparities Between Consumption and Recommendations
The gap between actual consumption and recommended intakes presents a dual public health burden of excess and deficiency.
Overnutrition in High-Income Countries: In wealthy nations, average protein consumption far exceeds the RDA. For instance, American men consume about twice the RDA, and women about 1.5 times it [17]. This overconsumption is largely driven by abundant access to animal products. However, despite high total intake, dietary patterns often lack diversity and do not align with recommendations for specific protein subgroups, such as seafood and legumes [17]. This suggests that the focus in these regions should shift from quantity to quality and source of protein.
Undernutrition in Vulnerable Populations: At the other extreme, an estimated 570 million people live in countries where the total digestible protein supply is insufficient to meet the population's average requirements [16]. This is starkly evident in regions like West Africa and Southern India, where diets rely heavily on low-protein staples and childhood protein malnutrition is prevalent [6]. Furthermore, within otherwise well-nourished populations, specific groups are at risk. Older adults, for example, frequently consume less protein than recommended, a concern exacerbated by the fact that they often consume lower-quality proteins, further compromising musculoskeletal health [6].
The Quality and Timing Gap: Disparities extend beyond gross quantity. The consumption of low-quality proteins, which lack essential amino acids or have poor digestibility, can render an apparently adequate intake functionally insufficient [6] [17]. Additionally, the timing of protein consumption is often suboptimal. In many Western populations, protein intake is skewed heavily toward the evening meal, whereas distributing 15-30 grams of high-quality protein evenly across meals is more effective for stimulating muscle protein synthesis throughout the day [20].
Public Health Implications
The disparities in protein consumption have significant consequences for population health and healthcare systems.
Health Risks of Overnutrition: Chronic consumption of protein significantly above requirements, especially from animal sources high in saturated fat, can pose health risks. While a recent 2025 umbrella review found no major association between total, animal, or plant protein intake and the risk of coronary heart disease or stroke, the certainty of evidence was "probable" for CHD and "possible" for stroke [22]. However, high-protein diets can lead to elevated blood lipids if the protein sources are also high in saturated fat, and they may pose a risk to individuals predisposed to kidney disease [20]. Furthermore, any excess calories from protein, like other macronutrients, are stored as body fat [20].
Health Risks of Undernutrition: Protein inadequacy remains a debilitating issue, leading to stunted growth in children, anemia, physical weakness, edema, vascular dysfunction, and impaired immunity [19]. In older adults, insufficient protein intake accelerates sarcopenia, leading to loss of muscle mass, strength, and functional independence, which is a major predictor of mortality [6] [20].
Beyond Protein: The Micronutrient Gap: A critical public health insight is that producing more protein alone will not solve global hunger. An estimated 2.8 billion people suffer from "hidden hunger," or micronutrient deficiencies, and many of these individuals may actually have adequate or even surplus protein and energy intake [16]. Therefore, interventions aimed at closing protein gaps must also consider the delivery of essential micronutrients. For example, supplementing with cereals provides zinc and fiber, dairy provides calcium and riboflavin, and meat provides bioavailable iron and vitamin B12 [16].
Experimental Protocols for Protein Research
Validating protein requirements and understanding metabolic fate relies on sophisticated experimental protocols.
Stable Isotope Tracer Methods
This is the gold standard for measuring whole-body protein metabolism. The protocol involves administering amino acids labeled with non-radioactive stable isotopes (e.g., ^13C-Leucine or ^13C-Phenylalanine) and tracing their appearance in plasma, breath, or other compartments.
- Primed Constant Infusion: A classic method where a loading dose (prime) of a labeled amino acid is followed by a continuous, prolonged intravenous infusion. Plasma samples are taken to measure the dilution of the tracer, which allows calculation of the Rate of Appearance (Ra) of the amino acid in the plasma, representing whole-body protein breakdown [21].
- Pulse Tracer Administration: A newer approach involving a single bolus or short-term infusion. Compartmental modeling of the tracer and product (e.g., labeled tyrosine from phenylalanine) kinetics is used to estimate intracellular amino acid production. This method suggests intracellular protein breakdown is significantly higher than estimates from plasma-based methods, potentially leading to revised, higher protein requirement estimates [21].
Protein Quality Assessment: The DIAAS Method
The Digestible Indispensable Amino Acid Score (DIAAS) is the FAO-recommended method for evaluating protein quality, replacing the older Protein Digestibility-Corrected Amino Acid Score (PDCAAS).
- Analysis: Determine the content of each indispensable (essential) amino acid (IAA) in a gram of the test protein.
- Reference Comparison: Compare this to the content of the same IAA in a gram of a reference protein pattern (based on human requirements).
- Ileal Digestibility: The key differentiator from PDCAAS. Digestibility is calculated based on the amount of each IAA absorbed at the end of the small intestine (ileum), typically measured in animal models (e.g., pigs) or increasingly via in vitro digestion systems. This provides a more accurate measure than fecal digestibility, which is confounded by microbial metabolism in the colon [6].
- Calculation: DIAAS = [(mg of digestible dietary IAA in 1 g of test protein) / (mg of the same IAA in 1 g of reference protein)] × 100. A score ≥100 indicates a high-quality protein that is fully utilized [6].
Research Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents and Materials for Protein Metabolism Studies
| Reagent/Material | Function in Research | Example Application |
|---|---|---|
| L-[ring-^13C₆]Phenylalanine | Stable isotope tracer for amino acid kinetics. | Quantifying whole-body protein breakdown and synthesis rates via primed constant or pulse infusion [21]. |
| L-[1-^13C]Leucine | Stable isotope tracer; its oxidation can be measured. | Assessing protein metabolism and amino acid oxidation via breath ^13CO₂ analysis [21]. |
| Bioelectrical Impedance Analyser (BIA) | Measures body composition (fat mass, fat-free mass). | Evaluating the impact of protein interventions on muscle mass in clinical trials [18]. |
| In Vitro Digestion Model | Simulates human gastrointestinal digestion. | Screening protein digestibility and bioaccessibility without invasive in vivo studies [6]. |
| Tanita BC-420 MA BIA | A specific, validated BIA device. | Used in cross-sectional studies to link protein intake to body composition parameters [18]. |
| Alpha-ketoisocaproic acid (KIC) | A metabolite of leucine. | Plasma KIC enrichment is used as a proxy for intracellular leucine enrichment to improve accuracy of leucine tracer studies [21]. |
Visualization of Research Workflows
Protein Assessment Workflow
Health Outcome Pathway
For decades, the assessment of dietary protein quality relied primarily on the Protein Digestibility Corrected Amino Acid Score (PDCAAS). However, in 2013, a Food and Agriculture Organization (FAO) Expert Consultation recommended the Digestible Indispensable Amino Acid Score (DIAAS) as a more accurate method for evaluating protein quality, citing several limitations in the PDCAAS approach [23] [24]. This paradigm shift represents a significant advancement in nutritional science, particularly for researchers and drug development professionals who require precise understanding of protein utilization in human physiology. The fundamental difference between these methods lies in their approach to digestibility: PDCAAS uses fecal digestibility estimates, which can be influenced by microbial activity in the large intestine, while DIAAS is based on ileal digestibility measured at the end of the small intestine, providing a more accurate representation of amino acid absorption [25] [24]. This technical improvement allows for better prediction of how efficiently amino acids from various food sources become bioavailable for metabolic processes, tissue repair, and protein synthesis—critical considerations for nutritional interventions and therapeutic formulations.
The DIAAS method addresses several specific limitations of PDCAAS. First, it considers the individual digestibility of each indispensable amino acid rather than applying a single crude protein digestibility value [24]. Second, DIAAS does not truncate values at 100%, allowing for differentiation between high-quality protein sources that exceed requirements [23] [25]. Third, it specifically accounts for lysine bioavailability in processed foods where Maillard reactions may have occurred, using true ileal digestible reactive lysine rather than total lysine [23]. For researchers investigating protein metabolism across different populations, these methodological refinements provide enhanced tools for evaluating protein sources and their potential to meet specific physiological needs.
DIAAS: Methodology and Calculation
Fundamental Principles and Calculation
The Digestible Indispensable Amino Acid Score is calculated based on a food's content of digestible indispensable amino acids relative to a reference amino acid pattern for a specific age group [25]. The calculation involves:
DIAAS (%) = 100 × (mg of digestible dietary indispensable amino acid in 1 g of the dietary protein / mg of the same dietary indispensable amino acid in 1 g of the reference protein) [23]
The score is determined by the first-limiting digestible indispensable amino acid—the amino acid with the lowest ratio when compared to the reference pattern [26]. This calculation requires two key pieces of information for each indispensable amino acid: the concentration in the food protein and its true ileal digestibility coefficient. The FAO has established reference amino acid patterns for three distinct age groups: 0-6 months, 6 months to 3 years, and over 3 years (including adults) [25], acknowledging that amino acid requirements differ across developmental stages—a crucial consideration for research targeting specific populations.
Reference Amino Acid Patterns
The reference patterns used in DIAAS calculations were derived from updated understanding of human amino acid requirements [25]:
Table 1: FAO Reference Amino Acid Patterns for DIAAS Calculation (mg/g protein)
| Amino Acid | 0-6 months | 6 mo-3 years | Over 3 years |
|---|---|---|---|
| Histidine | 21 | 20 | 16 |
| Isoleucine | 55 | 32 | 30 |
| Leucine | 96 | 66 | 61 |
| Lysine | 69 | 57 | 48 |
| Methionine + Cysteine | 33 | 27 | 23 |
| Phenylalanine + Tyrosine | 94 | 52 | 41 |
| Threonine | 44 | 31 | 25 |
| Tryptophan | 17 | 8.5 | 6.6 |
| Valine | 55 | 43 | 40 |
These reference patterns reflect the understanding that infants and young children have higher relative requirements for most indispensable amino acids to support rapid growth and development [25]. For researchers studying specific populations, selection of the appropriate reference pattern is essential for accurate protein quality assessment.
DIAAS vs. PDCAAS: Key Methodological Differences
The transition from PDCAAS to DIAAS represents a significant advancement in protein quality assessment methodology. The key differences between these approaches have important implications for research and product development:
Table 2: Comparison of PDCAAS and DIAAS Methodologies
| Aspect | PDCAAS | DIAAS |
|---|---|---|
| Digestibility Site | Fecal | Ileal (end of small intestine) |
| Digestibility Basis | Single crude protein value | Individual amino acids |
| Score Truncation | Truncated at 100% | Not truncated |
| Experimental Model | Rats | Growing pigs (preferred) |
| Lysine Assessment | Total lysine | Reactive lysine in processed foods |
| Reference Pattern | 2-5 year-old children only | Three age-specific patterns |
The use of ileal digestibility in DIAAS is physiologically superior because it measures amino acid absorption before microbial metabolism in the colon, which can alter the composition and amount of amino acids that actually reach systemic circulation [25] [24]. The avoidance of score truncation enables researchers to distinguish between protein sources that exceed requirements, which is particularly valuable for formulating products targeted at populations with elevated protein needs, such as athletes or older adults [23]. Additionally, the age-specific reference patterns align with our understanding that amino acid requirements differ across life stages, allowing for more precise nutritional planning and product development for specific demographic groups.
Animal vs. Plant-Based Proteins
Substantial research has documented significant variation in DIAAS values across different protein sources, with general patterns showing higher scores for animal-based proteins compared to plant-based sources [26]. However, considerable variation exists within these broad categories, and processing methods can significantly impact protein quality.
Table 3: DIAAS Values for Selected Protein Sources (based on 0.5-3 year reference pattern)
| Protein Source | DIAAS (%) | Limiting Amino Acid(s) | Quality Classification |
|---|---|---|---|
| Animal-Based Sources | |||
| Pork meat | >100 | - | Excellent |
| Whey Protein Isolate | 109 | Valine | Excellent |
| Whole milk | 114 | Sulfur amino acids | Excellent |
| Egg | 113 | Histidine | Excellent |
| Beef | 112 | - | Excellent |
| Casein | >100 | - | Excellent |
| Gelatin | <75 | Tryptophan | No quality claim |
| Plant-Based Sources | |||
| Potato protein | >100 | - | Excellent |
| Soy Protein Isolate | 90 | Sulfur amino acids | High |
| Tofu | 97 | Sulfur amino acids | High |
| Chickpeas | 83 | Sulfur amino acids | High |
| Pea Protein Concentrate | 82 | Sulfur amino acids | High |
| Cooked kidney beans | 59 | - | No quality claim |
| Wheat flour | 40 | Lysine | No quality claim |
| Rice Protein Concentrate | 37 | Lysine | No quality claim |
| Corn-based cereal | 1 | Lysine | No quality claim |
According to FAO recommendations, proteins are classified as: excellent quality (DIAAS ≥100), high quality (DIAAS 75-99), or no quality claim (DIAAS <75) [26]. The data reveal that while many plant-based proteins fall into the "high quality" category, their DIAAS values are typically lower than animal proteins due to limitations in specific indispensable amino acids and/or reduced digestibility [27]. The most common limiting amino acids in plant proteins are lysine in cereals and sulfur-containing amino acids (methionine and cysteine) in legumes [6] [26].
Impact of Food Processing and Matrix Effects
Recent research has highlighted that protein quality is not solely determined by the raw protein source but is significantly influenced by processing methods and food matrix effects. A 2025 study evaluating commercial protein bars found that despite high protein content claims, all tested bars had relatively low DIAAS values (highest was 61), primarily due to the inclusion of lower-quality proteins like collagen and interactions with other ingredients such as carbohydrates and fibers that reduced amino acid bioaccessibility [28]. This demonstrates how food formulation can substantially alter the nutritional quality of protein, an important consideration for product development.
Processing can also improve protein quality in some cases. Heat processing may inactivate anti-nutritional factors present in plant proteins such as trypsin inhibitors and lectins, thereby improving protein digestibility [27]. However, excessive heat treatment can promote Maillard reactions that reduce lysine bioavailability [23]. These competing effects underscore the need for optimized processing conditions to maximize protein nutritional quality.
Methodologies for Determining DIAAS
In Vivo Assessment Methods
The gold standard for DIAAS determination involves measuring true ileal amino acid digestibility in humans or animal models. The growing pig has been validated as the preferred animal model due to similarities in gastrointestinal physiology and digestive processes to humans [23] [26]. For human studies, a dual stable isotope tracer approach has been developed as a non-invasive method to determine true ileal amino acid digestibility across different physiological states [23] [29].
A recent study protocol illustrates the application of this method: older men received primed constant infusions of [1,2-13C2] leucine while consuming protein blends containing universally labeled 13C-spirulina and 2H-cell free amino acid mix [29]. The ratio of 13C:2H enrichment in plasma compared to the test drink was used to determine digestibility, with the free amino acid mixture representing 100% bioavailability [29]. This innovative approach enables researchers to study protein digestibility in vulnerable populations without invasive procedures like naso-ileal intubation.
In Vitro Digestion Models
While in vivo methods provide the most accurate assessment, they are resource-intensive and not always practical for screening multiple protein sources. Consequently, validated in vitro digestion simulation systems have been developed that correlate with in vivo findings [6] [28]. The INFOGEST method, an internationally standardized static in vitro simulation of gastrointestinal digestion, has been specifically validated for determining DIAAS of both animal and plant-based proteins [28].
The INFOGEST protocol involves sequential incubation of food samples with simulated salivary, gastric, and intestinal fluids under controlled pH, time, and electrolyte composition conditions [28]. The digestibility of individual amino acids is then determined by analyzing the bioaccessible fraction after intestinal digestion. This method enables rapid, cost-effective screening of protein digestibility, though it may not fully capture all aspects of the complex human digestive system, particularly microbial interactions and the role of the gut-brain axis in digestion regulation.
Protein Requirements Across Populations: Implications of Protein Quality
Age-Related Variations in Protein Needs
Understanding protein requirements across different populations is essential for contextualizing the importance of protein quality. Current evidence suggests that protein needs may be higher than traditional recommendations, particularly for older adults. A 2025 meta-analysis comparing protein requirements determined by nitrogen balance (NB) and indicator amino acid oxidation (IAAO) methods found that IAAO-derived requirements were approximately 30% higher than NB-based estimates [30]. For non-athletes, the IAAO method yielded a mean requirement of 0.88 g/kg/d compared to 0.64 g/kg/d with the NB method [30].
The anabolic resistance associated with aging, coupled with typically lower food intake, places older adults at particular risk of protein inadequacy [6]. Research indicates that approximately 40% of older adults in North America consume less than the recommended dietary allowance for protein [6]. This insufficiency is compounded by the fact that protein intake tends to decline with age, with adults over 75 years consuming 11-19% less protein than those under 64 years [6]. Furthermore, the relative contribution of animal proteins to overall protein intake is often lower in older individuals with inadequate gross protein intake, potentially exacerbating quality-related deficiencies [6].
Protein Quality in Dietary Patterns
For populations with limited protein intake, either due to low total food consumption or selective consumption patterns (e.g., vegetarian/vegan diets), protein quality becomes a critical factor in maintaining nitrogen balance and muscle protein synthesis. The DIAAS framework helps quantify the potential compensatory intake needed when relying on lower-quality protein sources.
Research demonstrates that complementary protein mixtures can achieve higher DIAAS values than individual components through strategic combination of proteins with different limiting amino acids [26]. For example, blending legumes (limiting in sulfur amino acids but rich in lysine) with cereals (limiting in lysine but adequate in sulfur amino acids) can produce a more balanced amino acid profile [26]. Mathematical modeling of protein mixtures has identified optimal ratios that maximize DIAAS, highlighting the potential of targeted food formulation to enhance protein nutritional quality, particularly in plant-based products [26].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Materials for Protein Quality Assessment
| Reagent/Material | Function in Research | Application Examples |
|---|---|---|
| Stable Isotope Tracers | Enable tracking of amino acid absorption and metabolism without radioactivity | [1,2-13C2] leucine for IAAO studies [29] [30] |
| Universally Labeled Proteins | Intrinsically labeled proteins for digestibility studies | U-13C spirulina as reporter protein [29] |
| Simulated Digestive Fluids | Standardized in vitro digestion following INFOGEST protocol | Gastric/intestinal fluid simulations [28] |
| Amino Acid Standards | Reference for HPLC/UPLC-MS quantification of individual amino acids | Establishing calibration curves [26] |
| Reference Proteins | Controls with known DIAAS for method validation | Casein, whey protein isolates [26] [24] |
| Cell-Free Amino Acid Mix | Reference for 100% bioavailability in dual-tracer studies | U-2H labeled AA mix [29] |
The adoption of DIAAS represents a significant advancement in protein quality assessment, providing researchers and product developers with a more accurate tool for evaluating the nutritional value of protein sources. The method's emphasis on ileal digestibility of individual amino acids offers physiological relevance that surpasses previous scoring systems. Evidence to date confirms that protein quality varies substantially across sources, with animal-derived proteins typically demonstrating higher DIAAS values, though strategic formulation of plant protein mixtures can achieve complementary effects that enhance overall protein quality.
Important research gaps remain, including the need for more comprehensive DIAAS data on commonly consumed foods, better understanding of the effects of food processing and matrix interactions on amino acid bioavailability, and development of rapid, cost-effective in vitro methods that strongly correlate with in vivo findings [23]. Additionally, the first overarching recommendation from the 2011 FAO Consultation—to treat each indispensable amino acid as an individual nutrient—has received limited attention, suggesting a need for more research focusing on specific amino acid metabolism rather than protein as a aggregate nutrient [23].
For researchers and drug development professionals, the DIAAS framework provides enhanced capability to design nutritional interventions and therapeutic products targeted to specific population needs, from supporting healthy aging to addressing metabolic disorders. As global protein supply challenges intensify and alternative protein sources emerge, accurate assessment of protein quality becomes increasingly crucial for developing sustainable, nutritionally adequate food systems.
Dietary protein is a critical macronutrient for human health, supporting vital functions from cellular structure to immune response. The establishment of universal protein recommendations, such as the Recommended Dietary Allowance (RDA) of 0.8 g per kg of body weight per day for adults, represents a foundational scientific consensus. However, emerging research reveals that these one-size-fits-all guidelines may be insufficient for specific population subgroups, creating significant evidence gaps that hinder personalized nutritional guidance. This review systematically identifies and evaluates these gaps, focusing on the methodological limitations in establishing protein requirements and the pressing need for population-specific dietary recommendations.
The current protein RDA of 0.8 g/kg/day is primarily derived from nitrogen balance studies focused on preventing deficiency rather than optimizing health across diverse physiological states. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health. Learn more: PMC Disclaimer | PMC Copyright Notice [31]. This approach has been challenged by more recent research indicating that protein needs vary substantially based on age, health status, and physiological demands. Furthermore, the assumption of high-quality protein consumption underlying these recommendations fails to account for the varying protein quality in different dietary patterns, particularly those relying heavily on plant-based sources. This analysis compares the evidence supporting current protein recommendations against emerging research needs, providing a framework for future investigation to refine population-specific protein requirements.
Comparative Analysis of Protein Recommendations Across Populations
Table 1: Current Protein Recommendations and Identified Gaps for Different Populations
| Population Group | Current Recommendation | Proposed New Targets | Key Evidence Gaps |
|---|---|---|---|
| Healthy Adults (18+ years) | 0.8 g/kg/day [32] | 0.65-0.83 g/kg/day (based on meta-analysis) [4] | Long-term efficacy studies; optimal intake for chronic disease prevention |
| Adults >65 Years | 0.8 g/kg/day | 1.0-1.2 g/kg/day (healthy); 1.2-1.5 g/kg/day (ill/ malnourished) [31] | Effective strategies to increase intake; impact on functional outcomes |
| Older Adults (40-65 Years) | 0.8 g/kg/day | Limited evidence for increased intake | Optimal intake for preventing sarcopenia onset; per-meal distribution |
| Athletes | 0.8 g/kg/day | 1.4-2.0 g/kg/day [33] | Sport-specific requirements; timing strategies for different training modalities |
| Plant-Based Consumers | 0.8 g/kg/day | Higher intakes suggested to compensate for quality [6] | Accurate protein quality assessment; complementary protein strategies |
Table 2: Protein Intake Patterns and Deficiencies in Older Adults
| Parameter | Adults 51-60 Years | Adults 61-70 Years | Adults >70 Years |
|---|---|---|---|
| Not meeting 0.8 g/kg/day | Up to 46% [8] | Similar deficit patterns | Up to 46% [8] |
| Associated diet quality | Significantly poorer [8] | Significantly poorer [8] | Significantly poorer [8] |
| Functional limitations | Significantly more in low protein consumers [8] | Significantly more in low protein consumers [8] | Significantly more in low protein consumers [8] |
| Grip strength | Not significantly different | Not significantly different | Significantly lower in low protein consumers [8] |
The disparity between current recommendations and physiological needs is particularly pronounced in aging populations. Muscle mass declines gradually from the third decade of life, with a 30-50% decrease reported between ages 40 and 80 [31]. Despite this physiological reality, protein recommendations remain unchanged until age 65, creating a significant evidence gap for adults in the 40-65 age range. Observational data reveals that protein intake actually declines with advancing age while requirements may be increasing, creating a concerning nutritional paradox. In Dutch older adults, approximately 50% consume less than 1.0 g/kg/day [34], and similar patterns are observed across Western countries [6].
Methodological Limitations in Protein Requirement Research
Nitrogen Balance Technique Constraints
The nitrogen balance method, which underpins current protein recommendations, has significant methodological limitations that contribute to ongoing evidence gaps. This approach may be inaccurate due to unaccounted routes of nitrogen input and output [31], potentially underestimating true protein requirements. Furthermore, nitrogen balance studies are typically conducted in controlled clinical environments, limiting assessment to short-term outcomes rather than long-term physiological adaptations [31]. The technique fundamentally establishes minimum requirements to prevent deficiency rather than optimal intakes for health promotion or disease prevention.
Recent meta-analyses of nitrogen balance studies suggest the RDA should be approximately 0.65 g/kg/day for the estimated average requirement and 0.83 g/kg/day for the RDA [4]. These values challenge the current 0.8 g/kg/day RDA and highlight the ongoing debate surrounding methodological approaches to determining protein requirements. The continued reliance on nitrogen balance studies without complementary methodologies represents a significant constraint in advancing the field of protein requirements research.
Emerging Techniques and Their Potential
The indicator amino acid oxidation (IAAO) technique has emerged as a promising alternative methodology, with studies using this approach reporting increased protein requirements in older adults compared with younger counterparts [6]. This method offers several advantages, including reduced subject burden and shorter study durations, potentially facilitating research in more diverse populations and settings.
Other innovative approaches include in vitro digestion modeling systems to screen protein quality from novel sources [6] and improved assessment tools such as the Protein Screener (Pro-MS) that can identify individuals with habitually low protein intake [35]. One study validated a protein intake screening tool for UK adults with an area under the curve of 0.731, indicating reasonable accuracy in identifying individuals consuming ≤1.0 g/kg/day [35]. While these methodologies show promise, they have not yet been widely adopted or validated across diverse populations, representing both an evidence gap and opportunity for future research.
Key Evidence Gaps in Population-Specific Protein Requirements
Aging Population Research Needs
The aging population presents particularly complex evidence gaps regarding protein requirements. While consensus groups recommend 1.0-1.2 g/kg/day for healthy adults over 65 [31], the appropriate intake for adults aged 40-65 years remains poorly defined despite the onset of sarcopenia in this demographic. The loss of muscle mass begins as early as age 40, with an accelerated decline after age 50 [31], yet targeted protein recommendations for this critical prevention window are lacking.
Beyond total daily intake, the distribution pattern of protein consumption throughout the day represents another significant evidence gap. Current evidence suggests that consuming 25-30 g of high-quality protein per meal optimally stimulates muscle protein synthesis [31], but the application of this research to older adults with anabolic resistance requires further investigation. The estimated per-meal threshold for plant proteins is particularly understudied [31], creating practical challenges for clinicians advising patients following plant-based diets.
The assessment of protein quality represents a fundamental evidence gap with implications for dietary recommendations and environmental sustainability. The Digestible Indispensable Amino Acid Score (DIAAS) has replaced the Protein Digestibility Corrected Amino Acid Score (PDCAAS) as the preferred method for evaluating protein quality [6], but application remains limited. Plant proteins generally have lower DIAAS values due to incomplete amino acid profiles and reduced digestibility [6], but the implications for population recommendations when consuming mixed diets requires clarification.
Table 3: Protein Quality Assessment and Research Needs
| Protein Source | Amino Acid Limitations | Digestibility Concerns | Research Priorities |
|---|---|---|---|
| Animal Proteins | Generally complete amino acid profile | High digestibility | Environmental impact; health effects in different life stages |
| Soy Protein | Complete amino acid profile | Moderate to high digestibility | Hormonal effects in specific populations; processing optimization |
| Legume Proteins | Often limited in methionine | Reduced by anti-nutrients (phytates, protease inhibitors) | Effective processing methods; complementary protein strategies |
| Cereal Proteins | Often limited in lysine | Reduced by fiber interactions; compact protein structures | Biofortification approaches; fermentation techniques |
| Novel Proteins | Varies by source (insects, fungi, algae) | Unknown without specific testing | Safety assessment; allergenicity; cultural acceptance |
The environmental implications of protein production necessitate research on sustainable alternatives. Animal protein production requires large areas of dedicated land, water, and energy while generating significant greenhouse gas emissions [31]. Transitioning to more plant-based proteins requires understanding how to maintain protein quality while shifting consumption patterns—a critical evidence gap given that plant-based nutrition may affect appetite and energy intake in older adults at risk of malnutrition [31].
Experimental Approaches and Methodological Frameworks
Nitrogen Balance Protocol
The nitrogen balance technique remains a foundational methodology for determining protein requirements, despite its limitations. The following protocol outlines a standardized approach:
Objective: To determine protein requirements by measuring nitrogen intake and output to establish equilibrium.
Subjects: Healthy adults representing the target population (e.g., older adults, athletes) with controlled physical activity levels.
Dietary Control:
- Provision of controlled diets with varying protein levels (0.1-1.5 g/kg/day)
- Precise measurement of all food intake and composition
- Adaptation period of 5-7 days at each test protein level
Sample Collection:
- Total urine collection for 24-hour periods throughout the study
- Stool collection for nitrogen content analysis
- Assessment of other nitrogen losses (skin, sweat, hair)
Analysis:
- Nitrogen content of diet, urine, and feces using Kjeldahl or Dumas method
- Calculation: Nitrogen Balance = Nitrogen Intake - (Urinary Nitrogen + Fecal Nitrogen + Miscellaneous Losses)
Data Interpretation: Requirement determined as the intake level at which nitrogen equilibrium is maintained.
This protocol was used in the meta-analysis that established requirements of 0.65 g/kg/day for the EAR and 0.83 g/kg/day for the RDA [4]. Recent applications suggest these values may better reflect true requirements than the current RDA of 0.8 g/kg/day.
Indicator Amino Acid Oxidation (IAAO)
The IAAO method represents a more modern approach to determining protein requirements:
Principle: Based on the concept that when one indispensable amino acid is deficient for protein synthesis, all other amino acids including the indicator amino acid will be oxidized.
Subjects: Typically studied in a metabolic research setting with controlled dietary intake.
Dietary Protocol:
- Adaptation to test protein levels for shorter periods than nitrogen balance (1-2 days)
- Provision of diets with varying protein levels but constant energy
- Use of amino acid mixtures to create specific protein quality profiles
Tracer Administration:
- Administration of stable isotope-labeled amino acid (typically [1-13C]phenylalanine)
- Continuous infusion or bolus protocols depending on study design
Sample Collection:
- Breath samples for 13CO2 enrichment measurement
- Blood samples for amino acid concentrations and enrichment
Analysis:
- Measurement of 13CO2 enrichment in breath samples
- Calculation of indicator amino acid oxidation rate
- Identification of breakpoint where oxidation rapidly increases indicating requirement
Advantages: Shorter study duration, less subject burden, applicable to vulnerable populations [6].
This method has demonstrated higher protein requirements in older adults compared to younger individuals, suggesting potential limitations in the current RDA [6].
Diagram 1: Methodological Framework for Protein Requirement Research. This flowchart illustrates the decision process for selecting appropriate methodologies based on research questions and population characteristics.
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 4: Essential Research Tools for Protein Requirement Studies
| Tool/Reagent | Application | Specific Examples | Research Considerations |
|---|---|---|---|
| Stable Isotope Tracers | IAAO studies to determine requirements | [1-13C]phenylalanine, [2H3]leucine | Purity verification; appropriate dosing strategies |
| Amino Acid Mixtures | Protein quality studies; controlled diets | Crystalline amino acids patterned after target proteins | Palatability challenges; matching physiological ratios |
| Indirect Calorimetry | Measure energy expenditure and substrate oxidation | Metabolic carts with breath collection | Calibration with standard gases; steady-state conditions |
| Body Composition Tools | Assess muscle mass changes | DEXA, BIA, MRI, CT | Method-specific precision errors; validation in population |
| Dietary Assessment Platforms | Measure habitual intake and compliance | 24-hour recalls, food frequency questionnaires, food diaries | Systematic biases; memory effects; cultural appropriateness |
| Protein Quality Assays | In vitro digestibility assessment | INFOGEST static digestion model | Correlation with in vivo results; anti-nutrient analysis |
| Muscle Biopsy Tools | Acute MPS measurement | Bergström needle with suction | Standardization of processing; analytical variability |
The selection of appropriate research tools depends heavily on the specific research question and population being studied. For example, while nitrogen balance studies require precise collection of all nitrogen outputs, IAAO studies depend on highly specific tracer methodologies and mass spectrometry analysis. Body composition assessment presents particular challenges in older adults, where fluid shifts may affect methods like bioelectrical impedance analysis.
Beyond laboratory methodologies, validated assessment tools for dietary intake and protein-specific screening instruments are essential for population-based research. The development of a protein intake screener for UK adults demonstrates the potential for efficient identification of individuals with low protein intake [35], though such tools require population-specific validation before widespread implementation.
Future Research Directions and Priority Populations
Several key populations merit prioritized investigation for protein requirements research. Older adults (particularly those aged 40-65 years) represent a critical target given the onset of sarcopenia during this life stage and the current absence of evidence-based recommendations. Research should focus not only on total protein intake but also on distribution patterns throughout the day, anabolic resistance mechanisms, and practical interventions to improve protein intake in those with declining appetite or functional limitations.
Individuals following plant-based diets constitute another priority population, as current recommendations assume high-quality protein consumption. Research must establish conversion factors for different protein sources and determine whether protein requirements increase when relying primarily on plant proteins. The complementary effects of different plant proteins and the impact of food processing on protein quality represent additional research priorities.
Athletes and physically active individuals require further sport-specific protein recommendation research, particularly regarding timing, distribution, and optimal protein sources for different training modalities. The efficacy of protein interventions in clinical populations, including those with renal impairment, metabolic conditions, or acute critical illness, represents another significant evidence gap with direct clinical implications.
Diagram 2: Research Priority Framework for Population-Specific Protein Requirements. This diagram illustrates the interconnected relationships between priority populations and research needs, highlighting the multidimensional approach required to address current evidence gaps.
From a methodological perspective, future research should prioritize long-term studies that evaluate functional outcomes rather than relying solely on short-term nitrogen balance or MPS measurements. The development and validation of improved assessment tools, including biomarkers of protein intake and status, would significantly advance the field. Finally, research integrating environmental sustainability with protein requirements would provide valuable guidance for developing recommendations that optimize both human and planetary health.
Significant evidence gaps persist in our understanding of protein requirements across diverse populations, limiting the development of evidence-based, personalized protein recommendations. Current guidelines, based primarily on short-term nitrogen balance studies assuming high-quality protein intake, fail to address the nuanced needs of aging adults, plant-based consumers, and individuals with varying physiological demands. Methodological limitations, including the focus on preventing deficiency rather than promoting optimal health, further constrain our understanding.
Addressing these evidence gaps requires a multidisciplinary approach incorporating validated assessment tools, long-term functional outcomes, and consideration of environmental sustainability. Priority should be given to research in vulnerable populations, including adults aged 40-65 years experiencing early sarcopenia and those following plant-based diets who may be consuming proteins with reduced quality and digestibility. Through targeted investigation of these evidence gaps, the scientific community can develop refined, population-specific protein recommendations that optimize health across the lifespan while promoting sustainable food systems.
Advanced Methodologies for Protein Requirement Assessment and Clinical Application
For decades, the determination of protein requirements has relied predominantly on the nitrogen balance (NB) method, which has formed the basis for dietary reference intakes worldwide. However, significant methodological limitations have prompted the scientific community to seek more robust and accurate alternatives. The indicator amino acid oxidation (IAAO) technique has emerged as a superior methodological approach, offering enhanced precision and reliability for determining protein and amino acid requirements across diverse populations. This paradigm shift is supported by a growing body of evidence demonstrating consistent discrepancies between these two methods, with IAAO-derived requirements consistently exceeding NB-based estimates by approximately 30% across multiple population subgroups.
The fundamental distinction between these methodologies lies in their conceptual foundations: while NB measures a static equilibrium between nitrogen intake and excretion, IAAO dynamically assesses the metabolic utilization of amino acids for protein synthesis at the cellular level. This technical advancement allows researchers to move beyond mere maintenance of body mass to optimization of metabolic function. As global interest in precision nutrition intensifies, particularly for specialized populations including athletes, older adults, and clinical groups, the validation of IAAO as the new gold standard represents a critical evolution in nutritional science with far-reaching implications for research, clinical practice, and public health policy.
Quantitative Comparison: IAAO vs. Nitrogen Balance
Recent meta-analyses have provided compelling quantitative evidence establishing significant differences between protein requirements determined via IAAO versus traditional NB methodology. A comprehensive umbrella review and meta-analysis published in 2025, encompassing 43 NB articles (777 participants) and 17 IAAO articles (186 participants), revealed consistent and statistically significant disparities across population subgroups [30] [36].
Table 1: Protein Requirement Comparison Between NB and IAAO Methods
| Population | NB Method (g/kg/d) | IAAO Method (g/kg/d) | Percentage Difference |
|---|---|---|---|
| Non-athletes | 0.64 (95% CI: 0.61, 0.68) | 0.88 (95% CI: 0.85, 0.90) | 36% higher with IAAO |
| Athletes | 1.27 (95% CI: 1.06, 1.47) | 1.61 (95% CI: 1.44, 1.78) | 27% higher with IAAO |
| Older Adults | 0.64-0.70 (linear regression) | 0.85-0.96 (breakpoint) | 30-37% higher with IAAO |
| Children | 0.76 (EAR) | 1.25-1.30 (breakpoint) | 58-71% higher with IAAO |
The data demonstrate that IAAO-derived protein requirements are substantially higher than NB estimates, with an average difference of approximately 30% across populations [30] [36]. This discrepancy is particularly pronounced in athletic populations, where IAAO suggests protein requirements up to 1.61-2.10 g/kg/d for endurance and resistance-trained athletes, significantly exceeding the NB-based estimates of 1.27 g/kg/d [30] [37]. Similarly, for older adults with sarcopenia, recent IAAO studies indicate requirements of 1.21 g/kg/d for the estimated average requirement (EAR) and 1.54 g/kg/d for recommended nutrient intake (RNI), substantially higher than current recommendations based on NB methodology [38].
Table 2: IAAO-Determined Protein Requirements Across Populations
| Population | EAR (Breakpoint) g/kg/d | RDA/RNI (Upper 95% CI) g/kg/d | Key Studies |
|---|---|---|---|
| General Young Adults | 0.87-0.93 | 1.17-1.29 | Matsumoto et al., 2023 [37] |
| Resistance-Trained Athletes | 1.49-2.00 | - | Bandegan et al., 2017; Mazzulla et al., 2020 [30] |
| Endurance Athletes | 1.65-2.10 | - | Matsumoto et al., 2023 [37] |
| Older Adults | 0.85-0.96 | 1.13-1.95 | Wu et al., 2025; Rafii et al., 2015 [37] [38] |
| Children | 1.25-1.30 | 1.50-1.55 | Matsumoto et al., 2023 [37] |
| Pregnant Women | 1.22-1.52 | - | Matsumoto et al., 2023 [37] |
Methodological Foundations: Experimental Protocols
Nitrogen Balance Technique
The traditional NB method estimates protein requirements by quantifying the difference between nitrogen intake and excretion, with the requirement defined as the intake at which net balance equals zero [30] [3]. The protocol involves:
- Dietary Control: Participants consume test diets with varying protein levels, typically for adaptation periods of 5-14 days at each intake level [3].
- Collection Periods: Complete collection of all urinary, fecal, and integumentary losses during the final 3-5 days of each adaptation period.
- Nitrogen Analysis: Precise measurement of nitrogen content in diets, urine, feces, and estimated miscellaneous losses using the Kjeldahl method or Dumas combustion.
- Balance Calculation: Nitrogen balance = (Nitrogen intake) - (Urinary nitrogen + Fecal nitrogen + Miscellaneous losses).
The method suffers from systematic errors, including potential overestimation of nitrogen intake and underestimation of nitrogen losses, particularly through skin, sweat, and other routes difficult to quantify accurately [30] [3]. Additionally, the linear regression model applied to NB data fails to account for the curvilinear relationship between nitrogen intake and balance, particularly as zero balance is approached [3].
Indicator Amino Acid Oxidation Technique
The IAAO method is based on the fundamental principle that when one indispensable amino acid is deficient for protein synthesis, all other amino acids, including the "indicator" amino acid, will be oxidized [39] [40]. The experimental protocol involves:
Figure 1: IAAO Experimental Workflow. The diagram illustrates the sequential steps in the IAAO technique, from controlled diet administration to breakpoint analysis for protein requirement determination.
Dietary Protocol: Participants consume diets with graded levels of the test protein or amino acid for short adaptation periods (typically 1-2 days), with the indicator amino acid (usually L-[1-13C]phenylalanine) maintained at constant intake across all test levels [39] [38].
Tracer Administration: On the study day, a stable isotope tracer (e.g., L-[1-13C]phenylalanine) is administered orally or intravenously, often using a "sip-feeding" approach with hourly small meals [41].
Breath Sample Collection: Breath samples are collected at baseline and regular intervals (typically every 30-60 minutes) over 4-8 hours to measure 13CO2 enrichment [39] [38].
Analysis and Breakpoint Determination: The fractional oxidation of the indicator amino acid (F13CO2) is plotted against protein intake, with the breakpoint identified using nonlinear mixed-effects (NLME) models or biphasic linear regression analysis [41] [38].
The IAAO method's advantages include shorter study duration, minimal adaptation periods, reduced participant burden, and the ability to study vulnerable populations. However, considerations include the extrapolation from hourly oxidation rates to daily requirements and the translation from amino acid mixtures to whole-food proteins [41].
Advanced Applications and Research Implications
Metabolic Availability and Protein Quality Assessment
Beyond determining protein requirements, the IAAO method has been innovatively applied to assess the metabolic availability (MA) of amino acids from dietary proteins, providing a sophisticated measure of protein quality that surpasses traditional digestibility measures [42]. This application is particularly valuable for evaluating plant-based protein sources, which are increasingly important in global sustainable nutrition strategies.
Research using IAAO to assess legumes has revealed that while lysine metabolic availability is generally high (>80%), methionine shows relatively lower availability (<80%), identifying potential limiting amino acids in plant-based diets [42]. This precise quantification of amino acid utilization from complex foods represents a significant advancement over crude protein content measures or fecal digestibility coefficients, enabling more accurate formulation of complementary proteins and dietary recommendations for vegetarian and vegan populations.
Special Population Requirements
The minimally invasive nature of the IAAO technique has enabled requirement determination in populations previously difficult to study using NB methodology [37] [38]:
- Sarcopenic Older Adults: Recent IAAO studies demonstrate protein requirements of 1.21 g/kg/d (EAR) and 1.54 g/kg/d (RNI) for older adults with sarcopenia, substantially higher than current recommendations [38].
- Athletes: IAAO reveals distinct requirements for different athletic populations: 1.49-2.00 g/kg/d for resistance-trained athletes and 1.65-2.10 g/kg/d for endurance athletes [37].
- Pregnant Women: IAAO studies indicate requirements vary by gestational stage, with higher needs in late pregnancy, challenging the one-value-fits-all approach in current guidelines [37] [43].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for IAAO Studies
| Reagent/Equipment | Specification | Research Function |
|---|---|---|
| Stable Isotope Tracers | L-[1-13C]phenylalanine (≥99% atom enrichment) | Indicator amino acid for oxidation measurement |
| Isocaloric Protein Diets | Crystalline amino acid mixtures or purified proteins | Test diets with graded protein levels |
| Breath Collection Apparatus | Falcon tubes with straws or specialized breath bags | Non-invasive collection of 13CO2 samples |
| Isotope Ratio Mass Spectrometer | High-precision IRMS with automated inlet systems | Analysis of 13C enrichment in breath CO2 |
| Protein-Free Products | Protein-free cookies, starches, and flavorings | Base diet components with minimal amino acid content |
| Indirect Calorimetry System | Metabolic carts with canopy hoods or mouthpieces | Measurement of CO2 production rates |
| Statistical Analysis Software | R, SAS, or specialized nonlinear mixed-effects models | Breakpoint analysis of oxidation curves |
The cumulative evidence from comparative meta-analyses, methodological evaluations, and population-specific studies firmly establishes the IAAO technique as the new gold standard for determining protein and amino acid requirements. The consistent demonstration of approximately 30% higher protein requirements using IAAO compared to NB methodology has profound implications for dietary recommendations worldwide, potentially necessitating revisions to current dietary reference intakes across multiple population groups.
The superior precision, reduced methodological artifacts, and applicability to diverse populations position IAAO as the preferred method for advancing nutritional science. Future research directions should include expanded application across life stages, increased inclusion of female participants, validation of whole-food protein utilization, and translation of short-term metabolic studies to long-term functional health outcomes. As precision nutrition evolves, the IAAO methodology provides the robust scientific foundation necessary for developing individualized protein recommendations that optimize health, function, and disease resistance across the human lifespan.
Development and Validation of Protein Intake Screening Tools for Research and Clinical Use
Accurate assessment of dietary protein intake is fundamental for research and clinical practice, particularly in populations where adequate protein is critical for preserving muscle mass and physical function. Traditional dietary assessment methods, including food frequency questionnaires (FFQs), dietary records, and 24-hour recalls, present significant limitations including high participant burden, requirement for specialized analysis, and time-intensive administration [44] [45]. For older adults, these challenges are compounded by physical limitations and recall bias [46]. Consequently, a pressing need exists for validated, rapid screening tools that can efficiently identify individuals with habitually low protein intake who may benefit from targeted nutritional interventions [44] [45]. This review compares the development, validation, and performance of emerging protein screening tools, focusing on their applicability across different populations and settings.
The clinical urgency driving this field stems from substantial evidence that a high prevalence of older adults consume protein below recommended levels. International expert groups, including the PROT-AGE study group and the European Society for Clinical Nutrition and Metabolism (ESPEN), recommend protein intakes of 1.0–1.2 g/kg body weight/day for healthy older adults, significantly higher than the UK Reference Nutrient Intake (0.75 g/kg/d) and the U.S. Recommended Dietary Allowance (0.8 g/kg/d) [44] [31] [3]. Despite these recommendations, epidemiological studies indicate that approximately 30-50% of community-dwelling older adults have protein intakes ≤1.0 g/kg adjusted body weight/day [45] [46], placing them at increased risk for sarcopenia, mobility limitations, and negative health outcomes.
The development of short food questionnaires represents a methodological advancement aimed at balancing the competing demands of accuracy, practicality, and participant burden. The table below summarizes the key characteristics of developed and validated protein screening tools.
Table 1: Developed and Validated Protein Intake Screening Tools
| Tool Name | Target Population | Number of Items | Target Threshold | Reference Standard | Development/Validation Sample |
|---|---|---|---|---|---|
| Pro55+ (Original) | Community-dwelling older adults (≥55 years) | 10 food questions + demographics | ≤1.0 g/kg adjusted BW/d | 238-item FFQ | LASA study (Development): n=1,348; HELIUS study (Validation): n=563 [45] |
| ProScreenerUK (Adapted) | UK adult population (18-91 years) | 10 food questions + demographics | ≤1.0 g/kg adjusted BW/d | 130-item EPIC FFQ | UK validation sample: n=184 [44] |
| German Pro55+ (Translated) | German older adults (≥70 years, mean 81.6) | 10 food questions + demographics | ≤1.0 g/kg adjusted BW/d & <0.8 g/kg adjusted BW/d | 3-day dietary record | German validation sample: n=144 [46] |
The Protein Screener 55+ (Pro55+) was the pioneering tool developed in the Netherlands, comprising ten questions on the consumption of protein-rich foods (e.g., slices of bread, glasses of milk, meat portion size, cheese, dairy products, eggs, pasta, fish, nuts), plus demographic information including body weight [45]. The tool calculates a predicted probability (0-1) of protein intake ≤1.0 g/kg adjusted body weight/day, with a score >0.3 originally identified as the optimal cut-off for screening [45].
The ProScreenerUK was adapted from the Dutch Pro55+ to reflect UK dietary patterns. This process involved replacing a question on cheese consumption with one about legumes and pulses and including meat substitutes within the meat products question, utilizing data from the UK BioBank and the National Diet and Nutrition Survey [44].
The German Pro55+ underwent a rigorous translation and cultural adaptation process, including forward and backward translation, expert review, and pretesting with older adults for comprehensibility and layout. The validation study highlighted the importance of such processes for cross-cultural application [46].
Comparative Performance and Validation Metrics
Validation studies for protein screeners have employed rigorous methodologies, using various reference standards to determine their discriminative accuracy. The following table compares the performance metrics of the validated tools.
Table 2: Performance Metrics of Protein Screening Tools
| Tool | Area Under the Curve (AUC) | Optimal Probability Cut-off | Sensitivity | Specificity | Prevalence of Low Intake in Sample |
|---|---|---|---|---|---|
| Pro55+ (Original) | 0.856 (95% CI: 0.824–0.888) [45] | >0.3 [45] | 82.2% [45] | 80.0% [45] | 30% [45] |
| ProScreenerUK | 0.731 (95% CI: 0.657, 0.805) [44] | >0.3 [44] | Not specified | Not specified | 40% [44] |
| German Pro55+ (<1.0 g/kg/d) | 0.620 (95% CI: 0.526–0.715) [46] | >0.09 (for sensitivity) [46] | 88.0% (at 0.09 cut-off) [46] | 90.0% (at >0.7 cut-off) [46] | 39.6% [46] |
| German Pro55+ (<0.8 g/kg/d) | 0.688 (95% CI: 0.581–0.794) [46] | >0.09 (for sensitivity) [46] | 88.0% (at 0.09 cut-off) [46] | 82.0% (at >0.5 cut-off) [46] | 17.4% [46] |
The variation in performance across populations highlights the significance of cultural and dietary factors in protein intake assessment. The original Pro55+ demonstrated "good" discriminative accuracy (AUC >0.85), while the UK adapted version showed "fair" accuracy (AUC >0.73) [44] [45]. The German validation yielded lower overall discriminative accuracy (AUC 0.62-0.69), suggesting potential challenges in cross-cultural application [46]. However, adjusting the probability cut-off value significantly improved sensitivity for detecting intake <0.8 g/kg aBW/d, indicating that tool performance can be optimized for specific clinical or research purposes [46].
Detailed Experimental Protocols and Methodologies
Development and Validation Workflow
The development and validation of protein screening tools follow a systematic process encompassing initial development, cultural adaptation, and validation phases. The following diagram illustrates the key stages in this workflow.
Diagram 1: Protein Screener Development and Validation Workflow
Key Methodological Components
Reference Standards and Validation Methods:
- The original Pro55+ and ProScreenerUK used comprehensive FFQs as reference standards (238-item and 130-item EPIC FFQ, respectively) [44] [45].
- The German validation utilized 3-day dietary records as the reference method, entered into nutritional analysis software (EBISpro) with the German nutrient database [46].
- Protein intake was standardized as g/kg adjusted body weight/day to account for differing needs in underweight and overweight individuals [44] [46].
Statistical Validation Protocols:
- Discriminative accuracy was primarily assessed using Receiver Operating Characteristic (ROC) curves and calculation of the Area Under the Curve (AUC) [44] [45] [46].
- AUC values were interpreted using standard classifications: ≤0.70 = poor, 0.70-0.80 = fair, 0.80-0.90 = good, >0.90 = excellent [44].
- Sensitivity and specificity were calculated at various probability cut-offs to determine optimal screening thresholds [45] [46].
- Calibration slopes were assessed to evaluate the agreement between predicted probabilities and observed frequencies of low protein intake [45].
Sample Size Considerations:
- The ProScreenerUK study recruited a minimum of 163 participants based on guidelines for sensitivity and specificity analysis, aiming for >80% power to detect an AUC of >0.7 [44].
- The German Pro55+ validation included 144 participants without a priori sample size calculation, highlighting a potential limitation in some validation studies [46].
Research Reagent Solutions and Essential Materials
Successful implementation of protein intake screening requires specific methodological components and analytical tools. The table below details essential "research reagents" and their functions in tool development and validation.
Table 3: Research Reagent Solutions for Protein Screener Development
| Category | Specific Tool/Method | Function in Development/Validation |
|---|---|---|
| Reference Standards | Comprehensive FFQ (e.g., 238-item HELIUS FFQ, 130-item EPIC FFQ) | Gold standard for estimating habitual protein intake during tool development [44] [45] |
| Multi-day dietary records (e.g., 3-day records) | Detailed assessment of food intake for validation in target populations [46] | |
| Statistical Analysis Tools | ROC curve analysis | Determining discriminative accuracy and optimal probability cut-offs [44] [45] [46] |
| Logistic regression models | Developing prediction algorithms for low protein intake probability [45] | |
| Nutritional Analysis Software | FETA software, EBISpro | Converting food consumption data to nutrient intakes using country-specific food composition databases [44] [46] |
| Cultural Adaptation Materials | National nutritional surveys (e.g., UK BioBank, NDNS) | Identifying country-specific protein sources and consumption patterns for tool adaptation [44] |
Critical Analysis and Research Implications
Performance Across Populations
The validation studies reveal important patterns in how these tools perform across different populations. The original Pro55+ demonstrated excellent discriminative ability in the Dutch population (AUC 0.856), suggesting robust performance in its original cultural context [45]. The UK adapted version showed fair accuracy (AUC 0.731), indicating that cultural adaptation, while necessary, may come with some loss of precision [44]. Most notably, the German validation yielded lower discriminative accuracy (AUC 0.620-0.688), highlighting significant challenges in cross-cultural application [46].
This performance variation underscores the complex interplay between dietary patterns, food frequency questionnaires, and cultural contexts. The German study authors noted that applying different probability cut-offs allowed for increased specificity and sensitivity for particular thresholds (especially <0.8 g/kg aBW/d), suggesting that tools can be optimized for specific clinical or research purposes even when overall discriminative accuracy is modest [46].
Methodological Considerations and Limitations
Several methodological issues merit consideration when interpreting these results:
Reference Standard Limitations:
- All validation studies relied on self-reported dietary assessment methods as reference standards, which are themselves subject to measurement error and systematic biases like under-reporting [47] [48].
- The use of different reference standards (FFQs vs. dietary records) complicates direct comparison between studies.
Population Representation:
- Validation studies primarily involved community-dwelling older adults, limiting generalizability to institutionalized or clinical populations.
- The German validation sample was notably older (mean 81.6 years) compared to the original Pro55+ development sample (56-101 years), potentially affecting performance [45] [46].
Threshold Dependencies:
- Performance varies substantially depending on the protein intake threshold used (<1.0 g/kg/d vs. <0.8 g/kg/d), with generally better sensitivity for the lower threshold [46].
The development and validation of protein intake screening tools represents a significant advancement in nutritional epidemiology and clinical practice. The Pro55+ and its adaptations offer practical, efficient methods for identifying older adults at risk of low protein intake, though performance varies across cultural contexts. These tools show particular promise for research settings where rapid screening can identify participants who may benefit most from nutritional interventions, thus increasing trial efficiency and potential effect sizes [44] [46].
Future research should focus on several key areas:
- Validation in more diverse populations, including clinical and institutionalized settings
- Comparison against objective biomarkers of protein intake where feasible
- Investigation of the cost-effectiveness of implementing such screens in clinical practice
- Development of dynamic tools that can adapt to evolving dietary patterns and protein sources
As protein recommendations continue to be refined, with emerging evidence supporting higher intakes for specific populations, the role of efficient screening tools will become increasingly important for both public health initiatives and individualized care [31] [3]. The integration of technology, such as mobile applications and automated scoring, may further enhance the utility and accessibility of these tools in diverse settings.
The evaluation of dietary protein quality is fundamental to predicting how effectively food proteins can meet human nitrogen and amino acid requirements for growth and maintenance. For decades, the Protein Digestibility Corrected Amino Acid Score (PDCAAS) served as the standard method for assessing protein quality. However, in 2013, a landmark FAO Expert Consultation recommended replacing PDCAAS with the Digestible Indispensable Amino Acid Score (DIAAS). This shift was prompted by several limitations inherent to the PDCAAS method, including its use of fecal crude protein digestibility (which can overestimate quality due to microbial activity in the colon) and the truncation of scores above 100%, which obscures true quality differences among high-quality proteins [23].
The DIAAS method provides a more accurate and detailed assessment of protein quality by focusing on true ileal amino acid digestibility. Unlike fecal digestibility measurements, ileal digestibility assesses amino acid absorption at the end of the small intestine, offering a more precise reflection of the amino acids actually available to the body [23] [49]. Furthermore, DIAAS does not truncate scores for proteins with values above 100%, allowing for clearer differentiation between high-quality protein sources. For processed foods where Maillard reactions may occur, DIAAS specifically recommends using values for true ileal digestible reactive lysine to accurately assess lysine bioavailability, which is often damaged by heat processing [23]. This modern framework treats each indispensable amino acid as an individual nutrient, emphasizing the importance of their digestible contents in meeting metabolic demands beyond just protein synthesis [23].
The DIAAS Methodology: Principles and Calculation
Fundamental Principles
The DIAAS is grounded in the principle that the quality of a protein is determined by its ability to provide digestible indispensable amino acids (IAAs) in proportions that match human requirements. The score is defined by a simple equation [23]:
DIAAS (%) = 100 × (mg of digestible dietary indispensable amino acid in 1 g of the dietary protein / mg of the same dietary indispensable amino acid in 1 g of the reference protein)
The calculation uses the most limiting digestible indispensable amino acid—the one whose digestible content relative to requirement is lowest—to define the score for the protein [26]. The Food and Agriculture Organization (FAO) has established age-specific reference patterns for the ideal amino acid composition, with distinct patterns for infants (0–6 months), young children (0.5–3 years), and older children, adolescents, and adults (>3 years) [26]. This acknowledges that amino acid requirements, and thus protein quality, are life-stage specific.
Key Differences from PDCAAS
The transition from PDCAAS to DIAAS represents a significant advancement in the field of protein quality evaluation. The following table summarizes the critical methodological differences between the two scoring systems.
Table 1: Key Differences Between PDCAAS and DIAAS Methodologies
| Feature | PDCAAS | DIAAS |
|---|---|---|
| Digestibility Site | Fecal | Ileal |
| Digestibility Type | Crude Protein Digestibility | True Ileal Amino Acid Digestibility |
| Lysine in Processed Foods | Total Lysine | Reactive Lysine (to account for Maillard damage) |
| Score Truncation | Scores truncated at 100% | Scores not truncated; can exceed 100% |
| Additivity in Mixtures | Not additive | Digestibility values are additive, enabling calculation for mixed diets [23] |
These differences make DIAAS a more physiologically relevant and accurate measure. The use of standardized ileal digestibility (SID) is preferred over apparent ileal digestibility (AID) because SID corrects for basal endogenous amino acid losses, providing a more accurate reflection of the protein's inherent digestibility and ensuring additivity in dietary formulations [26].
Experimental Workflow for DIAAS Determination
The determination of DIAAS relies on specific experimental models and protocols to obtain true ileal digestibility values. The following diagram illustrates the primary pathways for establishing DIAAS, highlighting the two main experimental approaches.
DIAAS in Action: Evaluating Novel and Single-Source Proteins
Extensive research employing the methodologies above has generated DIAAS values for a wide array of food proteins. The following table synthesizes data from various studies, providing a comparative overview of protein quality based on the DIAAS framework for the >3 years old population [26] [50].
Table 2: DIAAS Values and Quality Classification of Selected Protein Sources
| Protein Source | Mean DIAAS (>3 years) | First Limiting Amino Acid | Quality Classification |
|---|---|---|---|
| Whey Protein Isolate | 109-145 [50] | None | Excellent |
| Pork Meat | >100 [26] | None | Excellent |
| Casein | >100 [26] | None | Excellent |
| Egg | >100 [26] | None | Excellent |
| Potato Protein | >100 [26] | None | Excellent |
| Soy Protein Concentrate | 90 [50] | Methionine/Cysteine | High |
| Pea Protein Isolate | 82 [50] | Methionine/Cysteine | High |
| Wheat Protein | <75 [26] | Lysine | No Quality Claim |
| Rice Protein Concentrate | 37 [50] | Lysine | No Quality Claim |
| Corn Protein | <75 [26] | Lysine | No Quality Claim |
The data reveals a clear spectrum of protein quality. Animal-sourced proteins (whey, pork, casein, egg) consistently achieve DIAAS values above 100, classifying them as "excellent quality" proteins that can single-handedly meet and exceed amino acid requirements [26]. Among plant-based proteins, potato and soy stand out as high-quality options, with soy's quality being limited by sulfur-containing amino acids [26]. In contrast, many common plant proteins like wheat, rice, and corn have DIAAS values below 75, placing them in the "no quality claim" category due primarily to severe deficiencies in lysine [26]. This quantitative data is critical for formulating diets and food products, especially when considering the nutritional needs of specific populations and the increasing shift toward plant-based protein sources.
Assessing Protein Quality in Mixed Diets
The Principle of Complementarity
A key application of DIAAS is in the evaluation of mixed diets, where different protein sources are consumed together. The complementarity of proteins—where one protein's amino acid strengths compensate for another's weaknesses—can be precisely quantified using DIAAS principles [49]. Because true ileal amino acid digestibility values are additive, the DIAAS of a meal or dietary pattern can be calculated from the digestible amino acid contributions of each constituent protein [23]. This is a significant advantage over the non-additive nature of PDCAAS.
For a mixture of two proteins (P1 and P2), the digestible indispensable amino acid (DIAA) content for any amino acid 'y' is a linear combination [26]:
DIAA~y~ = (c~y,1~ × R~1~) + (c~y,2~ × R~2~)
Where c is the digestible amino acid content of the pure protein source and R is its proportion in the mixture. The DIAAS of the mixture is then determined by the most limiting DIAA ratio [26].
Practical Applications and Simulated Mixtures
Research simulations demonstrate the power of complementarity. For instance, combining plant proteins that have different limiting amino acids can create a mixture with a DIAAS higher than that of the individual components [26]. A blend of pea protein (limiting in methionine) and rice protein (limiting in lysine) can yield a more balanced amino acid profile. Similarly, adding even a small amount of a high-quality protein like potato or soy to a cereal-based meal can significantly elevate the overall DIAAS of the meal [26].
It is crucial to note that complementarity should be considered at the meal level, not over an entire day [49]. The body's pool of amino acids available for protein synthesis is transient; consuming complementary proteins within the same meal ensures that all necessary IAAs are present simultaneously to maximize synthesis.
Research Gaps and Methodological Considerations
Despite its advantages, the application of DIAAS faces several challenges. A primary issue is the lack of comprehensive data on the true ileal amino acid digestibility of foods as consumed by humans [23]. In response, the FAO and IAEA are leading a project to construct a global database on ileal digestibility, which will involve the systematic extraction of data from published literature [51].
Other key research priorities include [23]:
- Refining the ideal dietary amino acid balance, including the ideal ratio of dispensable to indispensable amino acids.
- Better defining dietary indispensable amino acid requirements across different physiological states.
- Understanding the specific effects of food processing on ileal amino acid digestibility and lysine bioavailability.
- Developing rapid, inexpensive in vitro digestibility assays that can reliably predict in vivo DIAAS values.
Furthermore, the first overarching recommendation of the 2011 FAO Consultation—to treat each indispensable amino acid as an individual nutrient—has received little attention. Providing food label information on the digestible contents of specific IAAs, rather than just a single aggregate score, would offer a more nuanced understanding of a food's nutritional value [23].
The Scientist's Toolkit: Key Reagents and Methods
Table 3: Essential Research Materials and Methods for DIAAS Determination
| Item / Method | Function / Description | Key Consideration |
|---|---|---|
| Growing Pig Model | Preferred in vivo model for determining standardized ileal digestibility (SID) due to physiological similarities to humans in GI tract and digestive processes [23] [26]. | Requires surgical modification (ileal cannulation) for digesta collection. Data must be obtained from healthy, growing pigs. |
| Dual-Isotope Assay | A non-invasive method for determining true ileal amino acid digestibility in humans, applicable across different physiological states [23]. | Uses stable isotopes (e.g., ^2^H, ^13^C) to label the test protein and an internal standard; relies on plasma analysis. |
| Chromatography (HPLC/UPLC) | For precise quantification of individual amino acid concentrations in food and ileal digesta samples. | Essential for obtaining the indispensable amino acid (IAA) composition of the test protein. |
| True Ileal Reactive Lysine Assay | Specifically measures the bioavailable lysine in processed foods, accounting for damage from Maillard reactions [23]. | Critical for obtaining accurate DIAAS for heated or stored protein products where lysine is often the first-limiting amino acid. |
| Reference Protein Pattern | The age-specific benchmark of ideal IAA concentrations against which the test protein is scored [26]. | Must use the correct pattern (infant, child 0.5-3 yr, or >3 yr) for the target population. |
The adoption of DIAAS marks a significant evolution in protein quality assessment, providing a more accurate and detailed framework grounded in true ileal amino acid digestibility. Its capacity to differentiate between high-quality proteins and its additive nature make it an indispensable tool for evaluating novel protein sources and designing mixed diets that optimally meet human amino acid requirements. For researchers and food developers, mastering DIAAS is crucial for advancing nutritional science, formulating sustainable and healthy foods, and validating protein recommendations for diverse populations. Future work must focus on expanding the DIAAS database, refining reference patterns, and integrating these precise quality metrics into dietary guidelines and public health strategies.
Integrating Resistance Exercise Protocols with Protein Supplementation Studies
This guide provides a comparative analysis of resistance exercise combined with protein supplementation, synthesizing evidence from clinical trials and meta-analyses. The data reveal that combined interventions consistently outperform either intervention alone for improving muscle mass and strength across diverse populations. Protein quality, dosage timing, and population-specific factors significantly influence outcomes, providing critical insights for researchers developing targeted nutritional strategies.
Quantitative Outcomes Comparison
Efficacy Across Populations
Table 1: Comparative Effectiveness on Muscle Mass
| Population | Intervention | Outcome Measure | Effect Size (SMD or Mean Difference) | Source |
|---|---|---|---|---|
| Healthy Elderly Adults | Protein + RT vs. Control | Lean Body Mass | SMD: 0.44 (95% CI: 0.05, 0.95) | [52] |
| Protein + RT vs. Control | Muscle Mass | SMD: 1.49 (95% CI: 0.11, 2.67) | [52] | |
| RT Alone vs. Control | Muscle Mass | Not Significant | [52] | |
| Older Adults with Sarcopenia | Protein + RE vs. Control | Muscle Mass | SMD: 0.95 (95% CI: 0.13, 1.78) | [53] |
| Younger & Older Adults (Combined) | Protein + RT vs. Placebo + RT | Fat-Free Mass (FFM) | WMD: 0.69 kg (95% CI: 0.47, 0.91) | [54] |
Table 2: Comparative Effectiveness on Muscle Strength and Function
| Population | Intervention | Outcome Measure | Effect Size (SMD or Mean Difference) | Source |
|---|---|---|---|---|
| Healthy Elderly Adults | Protein + RT vs. Control | Muscle Strength | SMD: 2.74 (95% CI: 0.76, 4.74) | [52] |
| RT Alone vs. Control | Muscle Strength | SMD: 2.53 (95% CI: 0.29, 4.84) | [52] | |
| Protein + RT vs. Protein Alone | Physical Function | SMD: 4.98 (95% CI: 2.72, 7.17) | [52] | |
| Older Adults with Sarcopenia | Protein + RE vs. Control | Muscle Strength | SMD: 0.32 (95% CI: 0.08, 0.56) | [53] |
| Younger & Older Adults (Combined) | Protein + RT vs. Placebo + RT | 1-RM Leg Press Strength | WMD: 13.5 kg (95% CI: 6.4, 20.7) | [54] |
| Mixed Elderly Adults | Protein + RT vs. RT Alone | Handgrip Strength | MD: 0.29 kg (95% CI: 0.08, 0.50) | [55] |
| Protein + RT vs. RT Alone | Leg Press Strength | MD: 0.33 kg (95% CI: 0.01, 0.64) | [55] |
Key Findings: The combination of protein supplementation and resistance training produces the most substantial improvements in muscle mass and strength. The synergistic effect is particularly pronounced in older adult populations, including those with sarcopenia, where the anabolic response to exercise and protein intake is often blunted. Notably, while resistance training alone significantly improves strength, its effect on muscle mass is greatly enhanced with concurrent protein supplementation [52] [54].
Protein Source Comparison: Whey vs. Pea Protein
Table 3: Plant-Based vs. Animal-Based Protein Efficacy
| Parameter | Pea Protein (PPr) | Whey Protein (WPr) | Statistical Significance | Source |
|---|---|---|---|---|
| Whole-Body Muscle Strength Change | +16.1% | +11.1% | p = 0.01 (PPr), p = 0.06 (WPr) | [56] |
| Muscle Mass Increase | Significant | Significant | No significant difference between groups | [56] |
| Product Tolerability & Safety | Well-tolerated | Well-tolerated | No significant difference | [56] |
| Key Characteristics | Plant-based, high in EAAs, suitable for allergies/dietary restrictions | Animal-based, complete amino acid profile, high leucine content | PPr is a viable alternative without sacrificing efficacy | [56] |
Key Findings: High-quality plant-based proteins like pea protein can produce improvements in muscle strength and mass comparable to whey protein when combined with resistance training [56]. This is critical for formulating protein recommendations for populations with dietary restrictions or personal preferences.
Detailed Experimental Protocols
Protocol for Sarcopenia Intervention in Elderly
- Study Design: A systematic review of 7 randomized controlled trials (RCTs) and 1 quasi-experimental study [53].
- Population: Community-dwelling older adults aged ≥60 years, diagnosed with sarcopenia (n=854).
- Intervention Duration: Ranged from 10 to 24 weeks.
- Resistance Exercise Component: Structured resistance training or multi-component exercise regimens including aerobic and balance training, performed 1-4 times per week [53].
- Protein Supplementation: Utilized various protein sources (whey, leucine, casein, milk, soy), either isolated or combined with other nutrients. Dosing was timed in proximity to exercise sessions.
- Outcome Measurements:
- Muscle Mass: Assessed via bioelectrical impedance analysis (BIA) or dual-energy X-ray absorptiometry (DXA).
- Muscle Strength: Primarily measured by handgrip dynamometry.
- Physical Performance: Evaluated using gait speed, chair rise test, or the Short Physical Performance Battery (SPPB).
Protocol for Sedentary Adult Population
- Study Design: Randomized, triple-blind, comparator-controlled, parallel clinical trial [56].
- Population: Sedentary adults aged 30-59 years (n=X), defined as engaging in ≤60 minutes of moderate to vigorous exercise weekly.
- Intervention Duration: 84 days of supplementation.
- Resistance Training Program: A structured weekly resistance training program.
- Supplementation Protocol:
- Experimental Group: Pea protein powder (NUTRALYS S85 Plus), 20.0-22.5 g per day.
- Comparator Group: Whey protein isolate, 20.0-21.1 g per day.
- Consumption: Participants consumed one daily dose mixed with 250 mL water, preferably post-exercise on training days.
- Primary Outcome: Change in composite whole-body muscle strength (WBMS) from baseline to Day 84.
- Assessment Tools:
- Strength: Isometric handheld dynamometer (upper/lower body), JAMAR hydraulic hand dynamometer (handgrip).
- Body Composition: Likely DXA scan.
- Tolerability: Modified Gastrointestinal Symptoms Rating Scale (GSRS).
Protocol for Acute Protein Dose-Response
- Study Design: Crossover trial in resistance-trained males [57].
- Population: Young, resistance-trained males, stratified by lean body mass (LBM ≤65 kg vs. ≥70 kg).
- Exercise Protocol: A single bout of whole-body resistance exercise.
- Supplementation: Ingestion of either 20 g or 40 g of whey protein in random order across trials.
- Primary Outcome Measurement: Myofibrillar protein synthesis (MPS) rate, determined via intravenous infusion of 13C6-phenylalanine tracer and serial muscle biopsies during post-exercise recovery.
- Key Finding: The 40 g dose stimulated a significantly greater MPS response than the 20 g dose (0.059 ± 0.020%·h⁻¹ vs. 0.049 ± 0.020%·h⁻¹; P=0.005), independent of total LBM [57].
Signaling Pathways and Mechanistic Insights
The efficacy of combined protein and exercise interventions is rooted in the molecular biology of muscle protein synthesis (MPS).
Pathway Explanation: Ingestion of protein, particularly sources rich in the indispensable amino acid leucine, leads to hyperaminoacidemia. Leucine binds to its intracellular sensor, Sestrin2, causing dissociation from GATOR2. This releases the inhibition on the mechanistic target of rapamycin complex-1 (mTORC1), a master regulator of cell growth [58]. Concurrently, resistance exercise provides an anabolic stimulus that sensitizes the skeletal muscle to the effects of amino acids. The convergence of these signals synergistically activates mTORC1, leading to a pronounced increase in muscle protein synthesis and, over time with repeated bouts, muscle hypertrophy [58].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Protein and Exercise Research
| Item | Function/Application | Examples from Literature |
|---|---|---|
| Protein Sources | Intervention substance; varies by amino acid profile and digestibility. | Whey protein isolate, Pea protein (NUTRALYS S85 Plus), Casein, Soy protein, Leucine supplements [58] [56]. |
| Amino Acid Tracers | Gold-standard measurement of acute MPS rates in vivo. | 13C6-phenylalanine infusion with muscle biopsy analysis [57]. |
| Hand Dynamometer | Objective measurement of handgrip strength, a key indicator of overall muscle strength. | JAMAR Hydraulic Hand Dynamometer [56]. |
| Isometric Dynamometer | Assessment of isolated upper and lower body muscle group strength. | JTECH Medical isometric handheld dynamometer [56]. |
| Body Composition Analyzers | Quantification of fat-free mass, muscle mass, and fat mass. | Dual-energy X-ray Absorptiometry (DXA), Bioelectrical Impedance Analysis (BIA) [53]. |
| Physical Performance Batteries | Functional assessment of mobility, balance, and lower limb strength. | Short Physical Performance Battery (SPPB), chair rise test, gait speed measurement [55] [53]. |
The integration of resistance exercise with protein supplementation represents a potent, non-pharmacological strategy for combating sarcopenia and optimizing musculoskeletal health across the lifespan. The collective evidence confirms that the combined intervention is superior for increasing muscle mass and strength compared to either component alone. Critical factors for researchers and product developers to consider include protein dose (with evidence supporting doses >20g for robust MPS stimulation [57]), protein quality (highlighted by the efficacy of leucine-rich sources [58]), and the viability of high-quality plant proteins as effective alternatives to animal sources [56]. Future research should focus on refining personalized protein recommendations based on age, health status, and exercise regimen to maximize therapeutic and performance outcomes.
Precision nutrition represents a paradigm shift from generic dietary advice toward interventions tailored to an individual's unique biological makeup, lifestyle, and environmental exposures [59] [60]. This emerging field recognizes the significant variability in how individuals respond to dietary intake, driven by factors including genetics, metabolism, microbiome composition, and health status [60]. Accurate dietary assessment forms the foundational layer upon which effective precision nutrition strategies are built, enabling researchers and clinicians to move beyond population-level recommendations to personalized dietary prescriptions.
The successful implementation of precision nutrition requires a systems-level understanding of human physiological networks and their variations in response to dietary exposures [60]. Dietary assessment tools provide the critical data necessary to classify population subgroups based on their nutritional needs and responses [59]. However, traditional dietary assessment methods face significant challenges, including day-to-day variability in food consumption, systematic under-reporting, recall bias, and the substantial burden placed on participants [61]. Overcoming these limitations is essential for advancing precision nutrition from theoretical concept to clinical reality.
This guide provides a comparative analysis of current and emerging dietary assessment methodologies, focusing on their validation metrics, implementation protocols, and applicability within precision nutrition research, particularly in the context of validating protein recommendations across diverse populations.
Comparative Analysis of Dietary Assessment Tools
Table 1: Comparison of Dietary Assessment Tool Characteristics and Applications
| Tool Category | Specific Tool/Platform | Key Measured Parameters | Validation Population | Primary Use Cases |
|---|---|---|---|---|
| Rapid Screeners | REFRESH (Rapid Evaluation FoR Environmentally Sustainable and Healthy diets) | 10 key food groups for healthy, sustainable diets; total score 0-10 | General population | Clinical screening for diet healthiness and environmental sustainability |
| Digital Food Tracking | MyFoodRepo app (AI-assisted) | Macro/micronutrients, food groups via image, barcode, manual entry | 958 adults in Swiss digital cohort | Epidemiological research, real-time monitoring |
| Traditional Clinical Assessment | Diet History Method | Habitual intake, core food groups, eating behaviors, specific nutrients | Female adults with eating disorders (n=13) | Clinical nutritional status assessment, disordered eating evaluation |
| Biomarker Development | Dietary Biomarkers Development Consortium (DBDC) | Blood/urine metabolites linked to specific foods | U.S. populations in controlled feeding studies | Objective intake validation, metabolomic signature discovery |
| Behavior-Focused Questionnaires | Plant-Protein Food Consumption Questionnaire | Perceived benefits/barriers, self-efficacy, interpersonal influence | 256 adolescent girls in Ethiopia | Behavior change intervention assessment |
Table 2: Validation Metrics Across Dietary Assessment Methodologies
| Tool | Reliability/Consistency Metrics | Validity/Agreement Metrics | Required Days for Assessment | Key Strengths |
|---|---|---|---|---|
| REFRESH Screener | KR-20 coefficient: 0.70 (good internal consistency) | 60-88% item agreement with food diaries; 59% cross-classification agreement | Single administration | Rapid assessment (<10 minutes), integrates sustainability |
| MyFoodRepo Digital Platform | High user adherence (2-4 weeks tracking) | Comparable accuracy to established methods; 76.1% entries via photo | 1-2 days (water, coffee); 2-3 days (macronutrients); 3-4 days (micronutrients) | Reduced participant burden, real-time data collection |
| Diet History Method | Standardized administration protocol | Moderate-good agreement for iron (kappa=0.68); improves with higher intakes | Single detailed interview (60-90 mins) | Captures disordered eating behaviors, includes supplement use |
| DBDC Biomarker Approach | Multi-site harmonized protocols | PK/DR relationships in controlled feeding | Varies by food compound kinetics | Objective intake measurement, eliminates self-report bias |
| Behavior Questionnaire | Scale-level reliability: 0.72; Factor-level: 0.31-0.69 | Content validity index >0.9; 6 theoretically meaningful factors | Single administration | Grounded in behavior change theory, culturally adapted |
Experimental Protocols and Methodologies
Validation Protocol for the REFRESH Dietary Screener
The REFRESH screener was designed to address the urgent need for practical tools that assess both healthfulness and environmental sustainability of diets in clinical settings [62]. The validation methodology followed a rigorous multi-step process:
Instrument Design: Researchers developed a dichotomous (yes/no) tool targeting 10 key food groups characteristic of healthy diets with low environmental impact. Each food group contributes 1 point to a total score ranging from 0-10, with higher scores indicating better adherence to sustainable healthy diets [62].
Validation Cohort: The tool was tested against a reference method of detailed food diaries to establish relative validity. Statistical analyses included assessment of internal consistency using the Kuder-Richardson-20 (KR-20) coefficient, item-by-item agreement percentages, Bland-Altman analysis for total score comparison, and cross-classification testing across low, medium, and high adherence categories [62].
Construct Validation: Researchers evaluated correlations between REFRESH-derived scores and health-promoting food groups, detrimental dietary components, and environmental impact indicators derived from the food diaries. This comprehensive validation approach confirmed the tool's ability to identify individuals with suboptimal diets while simultaneously assessing environmental sustainability [62].
Digital Dietary Assessment Validation Protocol (MyFoodRepo)
The "Food & You" study employed sophisticated methodology to establish minimum days required for reliable dietary intake assessment using digital tools [61]:
Data Collection: Participants (n=958) tracked meals for 2-4 weeks using the MyFoodRepo mobile application, which incorporated multiple data entry methods: photographic documentation (76.1% of entries), barcode scanning (13.3%), and manual entry (10.6%). The platform integrated with comprehensive nutritional databases containing 2,129 food items, with standardized portion sizes primarily sourced from the WHO MONICA study [61].
Data Verification: All logged entries underwent rigorous verification by trained annotators who reviewed portions, segmentations, and food classifications. The system facilitated direct communication between annotators and participants to clarify uncertainties, ensuring high data quality comparable to established dietary assessment methods [61].
Statistical Analysis for Minimum Days Estimation: Researchers employed two complementary methods to determine minimum days required for reliable assessment: (1) Coefficient of variation (CV) method based on within- and between-subject variability, and (2) Intraclass correlation coefficient (ICC) analysis across all possible day combinations. Linear mixed models assessed day-of-week effects and demographic influences on intake patterns [61].
Biomarker Discovery and Validation Protocol (DBDC)
The Dietary Biomarkers Development Consortium (DBDC) employs a systematic, multi-phase approach to discover and validate objective biomarkers of food intake [63]:
Phase 1 - Candidate Identification: Controlled feeding trials administer test foods in prespecified amounts to healthy participants, followed by comprehensive metabolomic profiling of blood and urine specimens. These studies characterize pharmacokinetic parameters of candidate biomarkers associated with specific foods, using liquid chromatography-mass spectrometry (LC-MS) and hydrophilic-interaction liquid chromatography (HILIC) protocols [63].
Phase 2 - Evaluation: The ability of candidate biomarkers to identify individuals consuming biomarker-associated foods is evaluated using controlled feeding studies of various dietary patterns. This phase assesses specificity and sensitivity across different dietary backgrounds [63].
Phase 3 - Validation: The validity of candidate biomarkers to predict recent and habitual consumption of specific test foods is evaluated in independent observational settings. This critical phase tests performance in free-living populations consuming complex, self-selected diets [63].
The DBDC establishes rigorous criteria for biomarker validation, including plausibility, dose-response relationships, time-response kinetics, analytical detection performance, chemical stability, robustness, and temporal reliability in diverse populations [63].
Diagram 1: Integrated Workflow for Precision Nutrition Assessment. This workflow illustrates the comprehensive data integration process from initial collection through intervention development, highlighting the role of dietary assessment tools within broader multi-omic profiling.
Implementation in Protein Recommendation Research
Protein Quality Assessment Methodologies
Research validating protein recommendation differences across populations requires sophisticated assessment of both intake and protein quality [64]. The digestible indispensable amino acid score (DIAAS) has emerged as the preferred method for evaluating dietary protein quality, capturing both essential amino acid composition and digestibility [64]. However, this approach has limitations, as chemical scoring metrics do not fully capture the metabolic activity of food-derived amino acids [64].
Precision nutrition approaches to protein assessment incorporate multiple dimensions:
- Amino Acid Density: Measuring %EAAs/kcals to evaluate protein quality within energy constraints
- Digestibility and Bioavailability: Assessing how processing, cooking, and food matrix effects influence amino acid availability
- Metabolic Response: Evaluating capacity to stimulate protein synthesis, particularly important for vulnerable populations like older adults [64]
Diet modeling studies demonstrate that amino acid density and protein quality are typically higher in omnivorous and lacto-ovo-vegetarian diets compared to plant-predominant patterns [64]. This has important implications for precision protein recommendations, as diets high in whole food plant-derived proteins may require greater total protein and energy intakes to compensate for lower protein quality.
Population-Specific Protein Requirements
Precision protein recommendations must account for population-specific factors that influence protein needs and utilization [64]. For older adults, considerations include chewing efficiency, food particle size, and higher essential amino acid density requirements to maximize muscle protein synthesis response [64]. Research indicates that leucine intake may be particularly important for optimizing the muscle protein synthetic response in this population.
In low- and middle-income countries where severe protein malnutrition occurs, precision nutrition approaches must balance ideal protein quality with cultural preferences, availability, and affordability [65]. For populations with limited access to animal proteins, strategic combination of plant proteins and processing methods to reduce antinutrients can improve protein quality within cultural and economic constraints [64] [65].
Table 3: Research Reagent Solutions for Dietary Assessment and Protein Research
| Reagent/Resource | Category | Primary Function | Example Applications |
|---|---|---|---|
| USDA Food and Nutrient Database for Dietary Studies (FNDDS) | Reference Database | Provides energy and nutrient values for 7,000+ foods and beverages | Nutrient intake analysis, adherence to Dietary Reference Intakes |
| USDA Food Pattern Equivalents Database (FPED) | Analysis Tool | Converts foods into 37 USDA Food Pattern components | Food group intake assessment, adherence to dietary guidelines |
| Open FoodRepo Database | Commercial Product Database | Nutritional data for barcode-scanned products | Digital dietary assessment, automated nutrient estimation |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | Analytical Platform | Comprehensive metabolomic profiling | Biomarker discovery, nutrient metabolic tracking |
| MyFoodRepo Nutritional Database | Integrated Database | 2,129 food items with standardized portions | Digital cohort studies, AI-assisted food recognition |
| Gene Ontology & KEGG Pathway | Bioinformatics Resources | Functional annotation of molecular data | Multi-omic integration, mechanistic insights |
The evolution of dietary assessment methodologies is critical for advancing precision nutrition from research concept to clinical application. Current tools range from rapid screeners suitable for clinical settings to sophisticated digital platforms and biomarker approaches for research contexts, each with distinct strengths and validation parameters [62] [61] [63]. The integration of these assessment methods with multi-omic profiling creates powerful pipelines for developing truly personalized nutritional recommendations [60].
Future directions in dietary assessment for precision nutrition include expanded biomarker discovery and validation through initiatives like the Dietary Biomarkers Development Consortium [63], refinement of digital assessment platforms using artificial intelligence and image recognition [61], and development of integrated algorithms that incorporate genetic, metabolic, and behavioral data to predict individual responses to dietary interventions [59] [60]. For protein research specifically, advancing beyond single-metric quality assessment to integrated models that account for individual metabolic phenotypes will be essential for validating differential protein recommendations across populations [64].
As these methodologies mature, the translation of research to practice will enable more effective precision nutrition interventions that account for individual variability in response to dietary intake, ultimately improving health outcomes through tailored dietary approaches.
Optimizing Protein Recommendations: Addressing Quality, Timing, and Implementation Barriers
The global protein sector is undergoing a profound transformation driven by population growth, environmental concerns, and technological innovation [66]. As demand for sustainable protein sources accelerates, plant-based, insect-based, and cultured proteins have emerged as promising alternatives to conventional animal proteins. However, their incorporation into global diets and research models is complicated by fundamental differences in protein quality—a multifactorial metric encompassing amino acid composition, digestibility, bioavailability, and postprandial utilization [17] [67]. The central thesis of protein recommendation research is being redefined by evidence suggesting that traditional assessment methods may significantly underestimate human requirements, with the Indicator Amino Acid Oxidation (IAAO) method yielding protein requirements approximately 30% higher than the established Nitrogen Balance (NB) method [30]. This discrepancy underscores the critical need for researchers to re-examine protein quality limitations and the methodologies used to overcome them, ensuring that alternative proteins can adequately support human health across diverse populations.
Comparative Analysis of Protein Source Compositions
Amino Acid Profiling and Nutrient Density
The foundational limitation of many plant-based proteins is their incomplete amino acid profile, typically lacking sufficient levels of one or more indispensable amino acids (IDAAs). Animal proteins are generally considered "complete" as they provide all nine IDAAs in adequate proportions, whereas plant proteins, with exceptions like soy, quinoa, and chia seeds, are often deficient in sulfur-containing amino acids (methionine and cysteine) and lysine [17] [67]. The table below provides a comparative analysis of amino acid profiles, highlighting these critical disparities.
Table 1: Indispensable Amino Acid (IDAA) Composition of Selected Protein Sources (g/100g)
| Amino Acid | 80% Lean Beef | 93% Lean Beef | Pork | Impossible Burger | Beyond Burger |
|---|---|---|---|---|---|
| Histidine | 0.65 | 0.85 | 0.62 | 0.42 | 0.50 |
| Isoleucine | 1.02 | 1.34 | 0.90 | 0.87 | 1.00 |
| Leucine | 1.73 | 2.20 | 1.48 | 1.35 | 1.69 |
| Lysine | 1.79 | 2.32 | 1.55 | 1.02 | 1.36 |
| Methionine | 0.54 | 0.72 | 0.49 | 0.19 | 0.26 |
| Phenylalanine | 0.93 | 1.14 | 0.78 | 0.93 | 1.16 |
| Threonine | 0.92 | 1.19 | 0.83 | 0.81 | 0.75 |
| Tryptophan | 0.25 | 0.33 | 0.23 | 0.21 | 0.23 |
| Valine | 1.15 | 1.39 | 0.97 | 0.94 | 1.12 |
| Total IDAA | 8.98 | 11.47 | 7.85 | 6.63 | 8.02 |
Source: Adapted from [67]
Beyond amino acids, the broader nutrient matrix is crucial. Plant-based meats are intrinsically lower in saturated fat and can be sources of fiber, vitamin E, and magnesium, but unlike animal meat, they are not natural sources of vitamins B12, B6, and D without fortification [68]. Furthermore, the presence of anti-nutritional factors (e.g., phytic acid, tannins, protease inhibitors) in plant sources can complex with minerals and proteins, thereby reducing their bioavailability and digestibility [17].
Protein Digestibility and Nutrient Release Kinetics
The nutritional value of a protein is determined not only by its composition but also by its digestion kinetics, which govern the timing and location of nutrient release [69]. This is a domain where certain animal-sourced foods retain a distinct advantage.
- Microstructure Impact: Soluble proteins are digested rapidly, while condensed or insoluble proteins are digested more slowly. Casein in milk coagulates in the stomach, leading to prolonged gastric residence and a slow, sustained release of amino acids. In contrast, whey protein is digested rapidly [69]. Plant-based milk alternatives do not replicate these functional benefits.
- Cellular Encapsulation: Nutrients in whole legumes are enclosed within cotyledonary cells. If processing and chewing do not rupture these cell walls, nutrient digestion is substantially delayed as digestive enzymes are impeded. A study comparing intact versus broken-cell chickpea foods showed dramatic differences in nutrient release rates and hormonal responses despite identical chemical compositions [69].
- Consequences for Research: The rate of protein digestion affects postprandial muscle protein synthesis and can influence metabolic responses. If protein digestion is too slow, undigested protein may reach the large intestine and be fermented by the microbiota, with varying health consequences depending on the dietary context [69].
Methodological Approaches for Quality Enhancement
Experimental Protocols for Processing and Analysis
Overcoming quality limitations requires a multi-faceted approach involving physical, biological, and analytical techniques. The following workflow outlines a standardized protocol for developing and evaluating enhanced alternative proteins.
Diagram: Experimental Workflow for Protein Quality Enhancement. This diagram outlines a sequential protocol from raw material processing to final product evaluation, highlighting key technological and analytical stages.
Detailed Experimental Protocols:
Protein Extraction and Isolation (Step P1):
- Objective: To obtain a protein-rich concentrate or isolate from raw plant, insect, or microbial biomass.
- Methodology: Employ wet or dry fractionation [70]. Wet fractionation involves alkaline extraction (e.g., pH 8-10 using 1M NaOH) followed by isoelectric precipitation (pH 4-5 using 1M HCl), recovery via centrifugation (e.g., 10,000 × g for 20 min), and neutralization and spray-drying. Dry fractionation uses air classification and milling to produce protein-enriched flours with retained native functionality [70] [71].
Enzymatic Hydrolysis and Fermentation (Step P2):
- Objective: To improve digestibility, reduce anti-nutrients, and enhance functional properties.
- Methodology: For enzymatic hydrolysis, incubate the protein isolate with specific proteases (e.g., Alcalase, Flavourzyme) at optimal pH and temperature (e.g., 50°C, pH 8 for Alcalase) for a predetermined time (e.g., 1-4 hours), followed by enzyme inactivation (e.g., 85°C for 15 min) [70]. For fermentation, inoculate the substrate with selected microbial strains (e.g., Lactobacillus spp., Fusarium venenatum for mycoprotein) and incubate under controlled conditions to biomass and degrade anti-nutritional factors [70] [66].
Amino Acid Complementarity and Fortification (Step P3):
- Objective: To create a complete amino acid profile.
- Methodology: Blend complementary protein sources (e.g., cereals rich in methionine with legumes rich in lysine) based on their IDAA scores. Alternatively, directly fortify with limiting synthetic or plant-derived amino acids [17]. The optimal blend ratio is determined by linear programming to match a reference pattern (e.g., FAO/WHO amino acid requirement pattern for adults).
In vitro Protein Digestibility Assay (Step A2):
- Objective: To simulate human gastrointestinal digestion and quantify protein digestibility.
- Methodology: Use the INFOGEST standardized static in vitro digestion model. The protocol involves sequential incubation with simulated salivary, gastric (e.g., pepsin, pH 3), and intestinal (e.g., pancreatin, pH 7) fluids under controlled agitation (e.g., 37°C). Digestibility is calculated as the percentage of protein nitrogen converted into trichloroacetic acid-soluble nitrogen after intestinal digestion, measured via the Kjeldahl method or spectrophotometry [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Protein Quality Analysis
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| Proteolytic Enzymes (Alcalase, Pepsin, Trypsin) | Catalyze the hydrolysis of peptide bonds to improve solubility and digestibility, and to simulate GI digestion. | Used in in vitro digestibility assays (INFOGEST) and for producing bioactive peptides [70]. |
| Selected Microbial Strains (e.g., L. lactis, F. venenatum) | Perform fermentation to enhance nutritional profile, reduce anti-nutrients, and produce microbial biomass (mycoprotein). | Cultivation of mycoprotein for meat analogs; fermentation of plant blends to improve flavor and digestibility [70] [66]. |
| Cell Culture Media & Scaffolds | Support the growth and proliferation of animal cells in cultured meat production. | Serum-free media and 3D-bioprinted scaffolds (e.g., from soy protein) for structuring cultured meat [66]. |
| HPLC Systems with Fluorescence Detectors | Separate, identify, and quantify amino acids and peptides in protein hydrolysates with high precision. | Amino acid profiling following acid hydrolysis of samples; requires pre-column derivatization (e.g., with OPA) [67]. |
| Anti-nutrient Assay Kits (Phytic Acid, Tannins) | Quantify specific anti-nutritional factors that impair mineral and protein bioavailability. | Monitoring the reduction of phytic acid during processing steps like fermentation or enzymatic treatment [17]. |
Discussion: Research Gaps and Future Directions
The pursuit of high-quality alternative proteins is fraught with both challenges and opportunities. A significant research gap lies in the long-term health impacts of consuming these novel proteins, especially highly processed plant-based analogs and cultured meats [66] [71]. Furthermore, the environmental benefits, while promising for plant and insect-based proteins, require more comprehensive Life Cycle Assessments (LCAs), particularly for nascent technologies like precision fermentation and cultured meat, where the energy-intensive production processes could offset environmental gains [66] [71].
From a methodological perspective, the debate over protein requirement assessment—between the traditional NB method and the more modern IAAO method—has direct implications for how the "adequacy" of alternative proteins is judged. The finding that IAAO-derived requirements are ~36% higher in non-athletes and ~27% higher in athletes suggests that the bar for protein quality may be higher than previously thought [30]. This necessitates a re-evaluation of the Protein Digestibility-Corrected Amino Acid Score (PDCAAS) and the Digestible Indispensable Amino Acid Score (DIAAS) frameworks in light of new requirement data.
Future research must embrace a systems-thinking approach, integrating AI and machine learning for protein structure-function prediction, optimizing precision fermentation, and developing circular bioeconomy models for protein production [66]. The ultimate goal is a sustainable and resilient protein supply that does not compromise on nutritional quality, ensuring food security for a growing global population.
Sarcopenia, the age-related loss of muscle mass and function, represents a significant challenge in aging populations. A key physiological mechanism underpinning sarcopenia is anabolic resistance—a blunted muscle protein synthetic response to anabolic stimuli like protein ingestion and exercise. This review synthesizes current evidence demonstrating that protein requirements are substantially higher in older adults compared to younger individuals to overcome this resistance. We present comparative data on protein dosing, detail foundational experimental methodologies, and illustrate the molecular pathways involved. The evidence supports strategic increases in daily protein intake (1.0-1.5 g/kg/day) and per-meal protein distribution (≥30-45 g/meal) as a critical intervention to mitigate muscle loss in older adulthood.
Anabolic resistance describes the diminished capacity of aging skeletal muscle to mount a robust protein synthetic response to fundamental anabolic stimuli, primarily dietary protein intake and physical activity [72] [73] [74]. This condition is a central etiological factor in the development and progression of sarcopenia, a syndrome characterized by the progressive and generalized loss of skeletal muscle mass, strength, and function [75]. The clinical impact of sarcopenia is profound, increasing the risk of physical disability, metabolic disease, loss of independence, and mortality [74] [75].
The metabolic foundation of anabolic resistance is a disturbance in the dynamic equilibrium of muscle protein turnover. Under normal conditions, muscle mass is maintained through a balance between Muscle Protein Synthesis (MPS) and Muscle Protein Breakdown (MPB). Aging skews this balance towards a net negative state, primarily due to a blunted rise in MPS following protein consumption [74] [76]. Proposed mechanisms for this blunted response include decreased anabolic molecular signaling (e.g., through the mTORC1 pathway), reduced insulin-mediated capillary blood flow (limiting amino acid delivery), and increased extraction of dietary amino acids by the splanchnic bed (reducing systemic availability) [72] [74]. Furthermore, lifestyle factors common in older adults, such as obesity and sedentarism, can exacerbate anabolic resistance, often mediated by insulin resistance and chronic, low-grade systemic inflammation [72] [76].
Quantitative Evidence: Protein Dosing Across Populations
Extensive research has established that the protein requirements for older adults are significantly higher than the current Recommended Dietary Allowance (RDA) of 0.8 g/kg/day and exceed the needs of younger adults to stimulate equivalent muscle anabolism.
Table 1: Comparative Protein Dosing for Maximal Anabolic Response
| Population | Total Daily Intake | Per-Meal Threshold | Key Supporting Evidence |
|---|---|---|---|
| Younger Adults | ~0.8 g/kg/day (RDA) | 0.24 g/kg (~20 g) [74] | Moore et al. (2014): Protein utilization plateaued at 0.24 g/kg in young men [31]. |
| Healthy Older Adults | 1.0 - 1.2 g/kg/day [11] [74] | 0.40 g/kg (~30-45 g) [31] [77] | Moore et al. (2014): Older men required ~0.40 g/kg to reach utilization plateau [31]. |
| Older Adults with Illness/Malnutrition | 1.2 - 1.5 g/kg/day (or up to 2.0 g/kg/day for severe cases) [11] | Likely higher, but less defined | PROT-AGE Study Group & ESPEN recommendations for elevated needs during metabolic stress [11]. |
Table 2: Protein Intake Impact on Longitudinal Health Outcomes
| Study / Cohort | Population | Protein Intake Comparison | Primary Outcome |
|---|---|---|---|
| Health, Aging, and Body Composition (Health ABC) Study [31] | Older Adults (70-79 years) | 1.1 g/kg/day vs. 0.8 g/kg/day | 40% less lean body mass loss over 3 years in higher intake group [31]. |
| Houston et al. [31] | Older Adults (70-79 years) | Highest vs. lowest quintile of animal protein intake | Significant preservation of lean body mass over three years [31]. |
The data in Table 1 reveals a critical per-meal dosing threshold. While 20 g of high-quality protein is sufficient to maximally stimulate MPS in young adults, older adults require a larger bolus, estimated at 0.40 g/kg/meal, which translates to approximately 30-45 g of protein per meal for a typical older adult [31] [77]. This per-meal dose is crucial for overcoming anabolic resistance. Furthermore, the longitudinal observational data in Table 2 demonstrates that higher habitual protein intake is directly associated with better preservation of muscle mass in older adults over time [31].
Foundational Experimental Protocols
The evidence for anabolic resistance and optimized protein dosing is derived from sophisticated, controlled experimental models. The following are core methodologies used in this field.
Stable Isotope Tracer Methodology for Muscle Protein Synthesis (MPS)
This approach is considered the gold standard for directly measuring the rate of synthesis of muscle proteins [74] [76].
- Tracer Infusion: A stable, non-radioactive isotope-labeled amino acid (e.g., [ring-²H₅]-phenylalanine) is intravenously infused into the subject, creating a labeled "pool" of amino acids in the bloodstream [74].
- Muscle Biopsy Sampling: Multiple percutaneous muscle biopsies (typically from the vastus lateralis) are taken before and after the nutritional intervention (e.g., protein ingestion) [74].
- Precursor-Product Model: The incorporation of the labeled amino acid from the precursor pool (blood or muscle intracellular fluid) into the product (muscle protein) is measured using mass spectrometry.
- Calculation of FSR: The Fractional Synthesis Rate (FSR), representing the percentage of muscle protein mass renewed per hour (%/h), is calculated using the formula: FSR (%/h) = [(ΔEₚ / Eₚ₍ₚᵣₑ𝒸ᵤᵣₛₒᵣ₎) × (60 / Δt)] × 100 Where ΔEₚ is the change in protein-bound enrichment, Eₚ₍ₚᵣₑ𝒸ᵤᵣₛₒᵣ₎ is the average precursor enrichment, and Δt is the time between biopsies in minutes [74].
Arteriovenous (A-V) Balance Model
This method provides a more comprehensive view of whole-leg protein metabolism by measuring amino acid kinetics across a limb [76].
- Catheterization: Catheters are placed in a peripheral artery (e.g., femoral artery) and a vein draining the muscle (e.g., femoral vein).
- Blood Flow Measurement: Blood flow to the leg is measured (e.g., via Doppler ultrasound).
- Blood Sampling: Simultaneous blood samples are drawn from the arterial and venous catheters before and after an intervention.
- Kinetic Calculation: The rates of MPS and MPB are calculated based on the arteriovenous concentration difference of the tracer amino acid (e.g., phenylalanine, which is not synthesized or oxidized in muscle), scaled by plasma flow. Net protein balance is then derived as MPS minus MPB [76].
Molecular Pathways of Muscle Anabolism
The anabolic response to protein feeding is primarily mediated by the postprandial rise in blood amino acid levels, particularly Essential Amino Acids (EAAs) and the branched-chain amino acid leucine [77] [75]. These signals converge on the mechanistic Target of Rapamycin Complex 1 (mTORC1) pathway, a master regulator of cell growth.
The following diagram illustrates the core signaling pathway activated by protein/amino acid intake and its role in stimulating muscle protein synthesis.
Diagram 1: Simplified mTORC1 Signaling Pathway in Muscle
This pathway highlights the central role of mTORC1. In the context of anabolic resistance, research indicates that older muscle exhibits a blunted activation of this pathway, particularly the phosphorylation of downstream targets like p70S6K, for a given dose of EAAs or protein [74] [76]. This molecular insensitivity is a fundamental contributor to the reduced MPS response observed in older adults.
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Research Reagents and Materials for Investigating Muscle Anabolism
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Stable Isotope Tracers (e.g., [²H₅]-Phenylalanine, [¹³C₆]-Leucine) | Metabolic tracing; enables precise measurement of MPS and whole-body protein turnover via MS. | Primed, constant IV infusion to measure FSR in response to a protein bolus [74]. |
| Deuterated Water (D₂O) | Long-term, non-specific labeling of newly synthesized proteins; ideal for free-living studies over days/weeks. | Oral dosing to measure cumulative MPS response to a dietary intervention over several days [76]. |
| Specific Protein Sources (Whey, Casein, Soy, Beef) | Defined nutritional stimuli to compare anabolic potency based on digestibility & amino acid profile. | Comparing the MPS response to 25g of whey vs. soy protein in older adults [77] [78]. |
| Essential Amino Acid (EAA) Mixtures | Allows precise control over the EAA dose and composition to identify key drivers of anabolism. | Isolating the effect of leucine content by comparing different EAA blends [77]. |
| Phospho-Specific Antibodies (e.g., p-mTORSer2448, p-p70S6KThr389) | Molecular signaling analysis; assesses activation of anabolic pathways via Western blot. | Quantifying mTORC1 pathway activation in muscle biopsy samples post-feeding [75] [76]. |
The evidence is conclusive: older adults experience anabolic resistance that necessitates higher protein dosing strategies compared to younger populations. The scientific data robustly supports daily intakes of 1.0-1.2 g/kg/day for healthy older adults, rising to 1.2-1.5 g/kg/day or more during illness, and a per-meal distribution pattern that provides ≥30-45 g of high-quality protein to maximally stimulate MPS. The experimental protocols of stable isotope tracing and A-V balance models, coupled with molecular analysis of the mTORC1 pathway, provide a rigorous framework for these conclusions. Overcoming anabolic resistance through targeted nutritional intervention is a critical strategy for preserving muscle mass and function, thereby promoting healthy aging and independence.
While total daily protein intake is a fundamental determinant of muscle protein synthesis (MPS), emerging evidence demonstrates that its temporal distribution throughout the day significantly modulates the anabolic response. This review synthesizes findings from controlled trials and meta-analyses comparing the efficacy of various protein feeding patterns—including even versus skewed distribution, bolus versus pulsed feeding, and peri-exercise timing—on acute and chronic muscular adaptations. Data reveal that evenly distributed protein intake (approximately 0.4 g/kg/meal across 3-4 meals) consistently outperforms skewed patterns for stimulating 24-hour MPS. Furthermore, the practice of protein timing around exercise, while theoretically sound, demonstrates equivocal effects on long-term hypertrophy when total daily protein intake is adequately matched. These findings underscore the necessity of moving beyond gross intake to optimize nutritional strategies for muscle maintenance and growth across diverse populations.
The prevailing dietary guidelines for protein have primarily emphasized total daily intake, with the Recommended Dietary Allowance (RDA) set at 0.8 g per kg of body weight for healthy adults [79]. However, skeletal muscle tissue exists in a constant state of turnover, with synthesis and breakdown rates fluctuating between 1% and 2% throughout the day [80]. This dynamic equilibrium is profoundly influenced by both exercise stimuli and nutrient intake, creating temporal windows of opportunity for maximizing anabolic potential.
The "muscle full" effect, wherein the muscle protein synthetic machinery becomes refractory to continued amino acid availability, establishes a biological rationale for pulsatile rather than continuous protein feeding [81]. This phenomenon suggests that the capacity of skeletal muscle to utilize amino acids for protein synthesis is saturable over short periods, typically returning to baseline within 2-3 hours despite sustained hyperaminoacidemia [81] [82]. Consequently, the distribution of protein intake across multiple meals may capitalize on the cyclical nature of muscle protein synthesis responsiveness.
This review systematically examines the experimental evidence comparing various protein distribution and timing strategies, with particular emphasis on their differential effects on myofibrillar protein synthesis rates, molecular signaling pathways, and long-term adaptations in muscle mass and strength.
Comparative Analysis of Protein Distribution Patterns
Even Versus Skewed Daily Distribution
Table 1: Even vs. Skewed Protein Distribution (Adapted from Mamerow et al. [83])
| Parameter | Even Distribution (EVEN) | Skewed Distribution (SKEW) |
|---|---|---|
| Breakfast Protein | 31.5 ± 1.3 g | 10.7 ± 0.8 g |
| Lunch Protein | 29.9 ± 1.6 g | 16.0 ± 0.5 g |
| Dinner Protein | 32.7 ± 1.6 g | 63.4 ± 3.7 g |
| 24-h Mixed Muscle Protein FSR | 0.075 ± 0.006 %/h | 0.056 ± 0.006 %/h |
| FSR after 7-d Habituation | 0.077 ± 0.006 %/h | 0.056 ± 0.006 %/h |
| Statistical Significance | p = 0.003 | p = 0.001 |
The seminal work by Mamerow et al. [83] provided direct evidence that how protein is distributed throughout the day significantly impacts 24-hour muscle protein synthesis rates. Using a randomized crossover design with isoenergetic and isonitrogenous diets, researchers demonstrated that consuming protein evenly across three meals (approximately 30 g per meal) stimulated 24-hour mixed muscle protein fractional synthesis rate (FSR) 25% more effectively than a skewed pattern (most protein at dinner). This pattern persisted after 7 days of habituation to each diet, indicating that the benefits of even distribution are not merely acute but sustain over time.
Feeding Frequency and Dose-Response Considerations
Table 2: Protein Feeding Frequency Patterns (Adapted from Areta et al. [81])
| Parameter | PULSE (8×10 g) | INTERMEDIATE (4×20 g) | BOLUS (2×40 g) |
|---|---|---|---|
| Dosing Schedule | Every 1.5 h | Every 3 h | Every 6 h |
| Total Protein | 80 g over 12 h | 80 g over 12 h | 80 g over 12 h |
| Myofibrillar Protein Synthesis Response | Moderate | Highest (31-48% > others) | Moderate |
| Cell Signaling Phosphorylation | Lowest | Intermediate | Highest |
| mRNA Expression Changes | Minimal | Moderate | MuRF-1 and SLC38A2 differentially expressed |
Areta et al. [81] conducted a sophisticated metabolic study comparing three distinct feeding patterns during 12 hours of post-exercise recovery. Twenty-four trained males received 80 g of whey protein in either 8×10 g pulses every 1.5 hours, 4×20 g doses every 3 hours, or 2×40 g boluses every 6 hours. The intermediate pattern (4×20 g) elicited significantly greater myofibrillar protein synthesis rates (31-48% higher) than either pulsed or bolus feeding, suggesting an optimal dosing threshold and frequency. Interestingly, the magnitude of cell signaling phosphorylation (including mTOR pathway components) followed a different hierarchy (BOLUS>INTERMEDIATE>PULSE), indicating dissociation between acute signaling and sustained synthetic response.
Peri-Exercise Protein Timing
Table 3: Protein Timing Around Resistance Exercise
| Study | Design | Timing Strategy | Muscle Strength | Muscle Hypertrophy |
|---|---|---|---|---|
| Schoenfeld et al. [84] | Meta-analysis (23 studies) | Protein ≤1h pre/post vs. ≥2h away | No significant effect | No significant effect when protein matched |
| Lak et al. [85] | 8-week RCT in trained males | Immediate pre/post vs. 3h pre/post | Significant increase in both groups | Significant increase in both groups |
| Key Covariate | Total protein intake strongest predictor | Not significant between conditions | Not significant between conditions |
A comprehensive meta-analysis by Schoenfeld et al. [84] evaluated whether consuming protein within a specific temporal window around exercise ("anabolic window") enhanced muscular adaptations. The analysis encompassed 478 subjects for strength outcomes and 525 subjects for hypertrophy outcomes across 23 studies. The simple pooled analysis showed a small to moderate effect on muscle hypertrophy without significant effects on strength. However, after controlling for covariates (particularly total protein intake) in the full meta-regression model, no significant differences remained between timing and control conditions for either strength or hypertrophy. The reduced model identified total protein intake as the strongest predictor of effect size magnitude for hypertrophy [84].
Supporting these findings, Lak et al. [85] conducted an 8-week randomized trial in resistance-trained males comparing two timing strategies: protein consumption immediately before and after exercise versus consumption 3 hours before and after exercise. Both groups consumed 2 g/kg/day of protein and performed identical resistance training. Results demonstrated significant increases in skeletal muscle mass, pull-up performance, and muscle strength in both groups with no significant between-group differences, reinforcing that total daily protein intake rather than precise peri-exercise timing drives muscular adaptations when protein needs are met.
Methodological Approaches in Protein Metabolism Research
Stable Isotope Tracer Methodologies
The deuterated water (²H₂O) method has regained interest for quantifying muscle protein synthesis rates over prolonged periods [80]. This approach involves ingesting daily boluses of deuterium oxide, resulting in ²H enrichment of the body water pool. The available ²H-atoms incorporate into endogenously synthesized alanine primarily through transamination of pyruvate in the liver. With ²H-alanine widely available to all tissues, it becomes incorporated into de novo synthesized tissue proteins. Assessing the increase in tissue protein-bound ²H-alanine enrichment in serial muscle biopsy samples allows calculation of muscle protein synthesis rates over several days or weeks, providing advantages for measuring synthesis under free-living conditions [80].
Traditional amino acid tracer methods, such as the continuous infusion of L-[ring-¹³C₆]phenylalanine used in both the Areta [81] and Mamerow [83] studies, provide high-precision measurements over shorter timeframes (typically several hours). These methods involve primed, continuous infusions of stable isotope-labeled amino acids with repeated blood and muscle biopsy sampling to determine the incorporation rate of the labeled amino acids into muscle protein.
Experimental Workflow for Protein Distribution Studies
Research Protocol for Protein Feeding Studies
Molecular Signaling in Muscle Protein Synthesis
Anabolic Signaling Pathway Regulation
The molecular regulation of muscle protein synthesis centers on the mechanistic target of rapamycin (mTOR) signaling pathway [82]. Consumption of dietary protein, particularly rich in essential amino acids, stimulates phosphorylation of mTOR and its downstream targets, including p70S6K and 4E-BP1. Resistance exercise potentiates this response through mechanotransduction mechanisms that converge on the same pathway. The interaction between exercise-derived and nutrition-derived stimuli creates a synergistic effect on phosphorylation of these signaling proteins, ultimately enhancing translation initiation and protein synthesis [81] [82].
Essential Research Reagents and Methodologies
Table 4: Essential Research Reagents for Protein Metabolism Studies
| Reagent/Methodology | Primary Function | Application Example |
|---|---|---|
| L-[ring-¹³C₆]phenylalanine | Stable isotope tracer for acute MPS measurement | Primed continuous infusion with serial muscle biopsies to calculate FSR over several hours [81] [83] |
| Deuterated Water (²H₂O) | Stable isotope tracer for prolonged MPS measurement | Oral boluses with serial sampling to assess integrated MPS over days/weeks in free-living conditions [80] |
| Whey Protein Isolate | High-quality protein source with rapid digestibility | Standardized protein boluses in feeding studies; rich in essential amino acids, particularly leucine [81] [85] |
| Muscle Biopsy Technique | Tissue sampling for direct protein synthesis measurement | Percutaneous needle biopsy of vastus lateralis for analysis of tracer incorporation and signaling phosphorylation [81] [83] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | High-sensitivity isotopic enrichment measurement | Quantification of tracer incorporation into muscle protein or alanine pool for FSR calculation [80] |
| Western Blot Analysis | Protein signaling phosphorylation assessment | Measurement of mTOR, p70S6K, and 4E-BP1 phosphorylation status in response to interventions [81] [82] |
Discussion and Research Implications
The collective evidence indicates that while total daily protein intake remains the paramount variable for determining muscle mass accrual, the temporal distribution of this protein significantly modulates the efficiency of its utilization. The consistent finding that evenly distributed protein intake (approximately 0.4 g/kg/meal across 3-4 meals) enhances 24-hour MPS compared to skewed patterns has important implications for refining dietary protein recommendations [83]. This pattern likely maximizes the pulsatile stimulation of MPS while circumventing the "muscle full" effect that limits the anabolic response to larger, less frequent protein boluses.
The dissociation between acute signaling phosphorylation and sustained protein synthesis rates observed in comparative feeding studies [81] highlights the complexity of translating molecular measurements to functional outcomes. While bolus feeding patterns may produce more dramatic transient spikes in anabolic signaling, the intermediate pattern (4×20 g every 3 h) demonstrated superior net protein synthesis over 12 hours, suggesting that repeatedly stimulating MPS to a moderate degree may be more effective than fewer, maximal stimulations.
From a methodological perspective, the choice of assessment technique—acute versus integrated protein synthesis measurements—significantly influences study conclusions. The deuterated water method [80] offers distinct advantages for measuring muscle protein synthesis under free-living conditions over extended periods, complementing the high temporal resolution of traditional amino acid tracer methods.
This comparative analysis demonstrates that moving beyond total daily intake to consider protein distribution patterns provides a more nuanced understanding of protein utilization for muscle protein synthesis. The evidence supports a paradigm where moderate protein doses (20-40 g, or approximately 0.4 g/kg) distributed evenly across 3-4 daily meals optimize the 24-hour muscle protein synthetic response compared to skewed distribution patterns. In contrast, the practice of precise peri-exercise protein timing demonstrates equivocal effects on long-term muscular adaptations when total protein intake is adequately matched.
These findings have significant implications for refining protein recommendations across diverse populations, particularly for conditions characterized by anabolic resistance such as aging [86]. Future research should focus on elucidating the molecular mechanisms underlying the dissociation between acute signaling and sustained synthesis, and examining how protein distribution strategies interact with factors including age, training status, and protein quality to influence functional outcomes.
Demographic Disparities in Protein Consumption
A systematic analysis of dietary patterns reveals that while the majority of the US population meets or exceeds minimum protein recommendations, specific demographic subgroups exhibit a higher prevalence of inadequate intake, highlighting critical knowledge gaps in population-level nutrition [87].
Protein Intake Trends and At-Risk Populations
Table 1: Protein Intake and Conformity with Dietary Reference Intakes (DRIs) Across Demographics (NHANES 2011-2014)
| Demographic Group | Mean Protein Intake (g/kg IBW/d) | Population Below EAR (%) | Key Findings |
|---|---|---|---|
| Adolescent Females (14-18 y) | 1.22 ± 0.02 | 11% | Highest risk of inadequate intake among age groups [87] |
| Older NHB Men (≥71 y) | 1.18 ± 0.01 (All men ≥71 y) | 13% | Largest percentage below EAR among older adults [87] |
| Adults (19-30 y) | 1.26 ± 0.01 | <3% | Mean intake is 88.2 ± 1.1 g/d [87] |
| Asian American Adults (>19 y) | 1.32 ± 0.02 | Not Specified | Consumes more relative protein than NHB and NHW [87] |
| Hispanic Adults (>19 y) | 1.32 ± 0.02 | Not Specified | Consumes more relative protein than NHB and NHW [87] |
| Non-Hispanic White Adults (>19 y) | 1.18 ± 0.01 | Not Specified | Lower relative intake compared to Asian and Hispanic adults [87] |
Analysis of the National Health and Nutrition Examination Survey (NHANES) from 2001-2014 indicates that protein comprises 14-16% of total energy intake for the US population, with usual intakes ranging from 55.3 g/d for children (2-3 y) to 88.2 g/d for adults (19-30 y) [87]. Relative protein intakes decrease with age, from a high of 3.63 g/kg IBW/d in young children to 1.10 g/kg IBW/d in adults over 71 years [87]. Despite overall adequacy, vulnerable groups such as adolescent females and older Non-Hispanic Black (NHB) men demonstrate the largest population percentages below the Estimated Average Requirement (EAR), pinpointing key targets for nutritional intervention [87].
Table 2: Top Dietary Protein Sources by Race and Ethnicity (NHANES 2011-2016)
| Rank | Hispanic | Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian | Other |
|---|---|---|---|---|---|
| 1 | Chicken | Chicken | Chicken | Chicken | Chicken |
| 2 | Beef | Beef | Beef | Beef | Beef |
| 3 | Milk | Eggs & Omelets | Eggs & Omelets | Eggs & Omelets | Eggs & Omelets |
| 4 | Eggs & Omelets | Milk | Milk | Fish | Milk |
| 5 | Cheese | Meat Mixed Dishes | Meat Mixed Dishes | Milk | Meat Mixed Dishes |
| 6 | Meat Mixed Dishes | Cheese | Cheese | Meat Mixed Dishes | Fish |
| 7 | Beans, Peas, Legumes | Pork | Pork | Pork | Nuts & Seeds |
| 8 | Pork | Fish | Fish | Cheese | Pork |
| 9 | Fish | Cold Cuts | Cold Cuts | Cold Cuts | Cheese |
| 10 | Sausage | Sausage | Sausage | Rice | Cold Cuts |
The top ten sources of protein account for over 40% of total dietary protein intake across all racial and ethnic groups [88]. Chicken is the top-ranked source for every demographic, followed by beef (excluding ground), eggs, and meat mixed dishes [88]. The limited appearance of plant-based proteins in the top ten is notable; beans, peas, and legumes rank seventh for Hispanics, and nuts and seeds rank seventh for the "Other" racial category, underscoring a homogeneity in animal-sourced protein dominance that has major implications for the sustainability of the national food supply [88].
Experimental Validation of Protein Research and Recommendations
The validation of protein research, from analytical methods to population-level recommendations, is a cornerstone of credible nutritional science.
Methodological Validation in Protein Analysis
In mass spectrometry-based shotgun proteomics, protein inference—the process of reconstructing protein identities from peptide data—is a non-trivial task due to the inherent uncertainty of mass spectrometric data and the complexity of proteomes [15]. Statistical validation is critical to control for false discoveries, with the false discovery rate (FDR) being the most useful measure as it accounts for multiple testing [15].
For antibody-based research applications, the International Working Group for Antibody Validation (IWGAV) has proposed five pillars for enhanced, application-specific validation [89]. These strategies can be implemented using standardized panels of cell lines and include:
- Orthogonal Strategies: Comparing protein abundance levels from an antibody-dependent method (e.g., Western blot) with an antibody-independent method (e.g., mass spectrometry-based proteomics or transcriptomics) across a set of samples [89].
- Genetic Strategies: Using genetic knockdown (e.g., siRNA) to confirm a reduction in the antibody signal [89].
- Recombinant Expression: Expressing the target protein in a cell line to verify antibody binding [89].
- Independent Antibodies: Verifying that multiple antibodies against different epitopes of the same target yield consistent results [89].
- Capture MS: Immunoprecipitating the target protein and identifying co-purifying peptides via mass spectrometry to confirm identity [89].
Protein Antibody Validation Framework
Critical Analysis of Protein Requirement Standards
A significant debate within nutritional science concerns the adequacy of global protein requirement standards. Many current recommendations, such as the US and Canadian Recommended Dietary Allowance (RDA) of 0.8 g per kg of body weight, are based on data from nitrogen balance studies [79]. However, a reassessment of this data, along with evidence from newer methodologies like Indispensable Amino Acid Oxidation (IAAO), suggests that base protein requirements are higher, particularly for older adults [79].
A survey of the International Protein Board (IPB) revealed expert consensus that current recommendations are inadequate, scoring 4.82 on a Likert scale where 5 = Strongly Disagree with the statement that current recommendations are sufficient [79]. Furthermore, the IPB strongly disagreed (average score of 4.82) that protein intakes at twice the RDA (1.6 g/kg) pose a serious kidney or bone risk for healthy adults, indicating that current standards may be overly conservative and that higher intakes could be beneficial and safe for specific populations [79].
Behavioral Interventions to Promote Sustainable Protein Consumption
With animal-sourced food production being a major contributor to global greenhouse gas (GHG) emissions, behavioral interventions to promote a shift toward plant-based proteins are critical [90].
Experimental Protocol for Online Nudge Interventions
A 2024 experimental study with 2,359 US participants assessed the impact of behavioral nudges in an online grocery shopping environment using the Open Science Online Grocery (OSOG) platform [90].
Methodology:
- Platform: The OSOG platform simulated a typical online grocery shopping experience with real-world products.
- Product Selection: The study focused on meat, milk, yogurt, and cheese categories and their plant-based substitutes.
- Intervention Arms: Participants were randomly assigned to one of three treatment groups or a control group.
- Labeling: Display of color-coded carbon footprint labels with GHG emission values for each item.
- Categorization: Display of a curated category of plant-based products.
- Combination: Integration of both carbon footprint labeling and the curated category.
- Control: No labels or curated categories were shown.
- Outcome Measures: The primary outcomes were the proportion of plant-based products purchased and the total carbon footprint of the shopping basket [90].
Online Grocery Intervention Workflow
Comparative Efficacy of Behavioral Interventions
Table 3: Impact of Behavioral Interventions on Plant-Based Food Selection in an Online Store
| Intervention Group | Increase in Plant-Based Selection vs. Control | Key Statistical Findings |
|---|---|---|
| Carbon Footprint Labeling | 37% increase | Increased purchase of plant-based products by 17 percentage points (P < 0.01) [90] |
| Product Categorization | 25% increase | Significant effect (P < 0.01) for total, milk, and cheese products [90] |
| Combination of Both | 32% increase | Estimates for label and combination groups were not statistically different [90] |
| Control Group | Baseline | - |
The results demonstrated that both interventions were effective, with carbon footprint labeling being the most powerful single nudge, leading to a 37% increase in plant-based product selection [90]. Product categorization alone increased selection by 25% [90]. The total carbon footprint of purchased products was significantly lower in all treatment groups compared to the control, confirming the environmental efficacy of these nudges [90]. Despite exposure to carbon footprint information, participants consistently underestimated the environmental impact of foods, suggesting that the nudges worked through subconscious channels rather than solely through improved consumer knowledge [90].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Protein Consumption and Intervention Studies
| Research Tool / Reagent | Primary Function in Research Context |
|---|---|
| NHANES Dietary Data | Provides nationally representative, cross-sectional data on food and nutrient intake (including protein) to analyze trends and identify at-risk populations [88] [87]. |
| Open Science Online Grocery (OSOG) | An experimental platform that simulates a realistic online shopping environment to test the efficacy of behavioral interventions (e.g., labels, categorization) on food choices [90]. |
| Mass Spectrometry (LC-MS) | A powerful analytical technology for system-wide identification and quantitation of proteins. Used for biomarker discovery and validation in biological samples [91] [15]. |
| Validated Antibodies | Essential reagents for detecting specific proteins in methods like Western blot. Require application-specific validation using pillars like orthogonal methods or genetic strategies [89]. |
| siRNA for Genetic Knockdown | Used to reduce expression of a specific target gene in cell lines. Serves as a critical method for validating antibody specificity in the "genetic" validation pillar [89]. |
| Tandem Mass Tag (TMT) & Parallel Reaction Monitoring (PRM) | Advanced mass spectrometry techniques for multiplexed, relative protein quantitation (TMT) and highly sensitive, targeted absolute quantitation (PRM) [89]. |
Dietary protein serves a pivotal role in human health by providing essential amino acids required for the maintenance of body proteins, assimilation of structural components, and basic survival functions [88]. As global population and protein demand increase, a critical tension has emerged between meeting nutritional requirements and minimizing environmental impact. This creates a complex challenge for researchers, policymakers, and food system professionals: how to reconcile optimal protein nutrition with sustainable food systems.
The complexity of this challenge is heightened by evolving scientific understanding of protein requirements. While current Recommended Dietary Allowances (RDA) for protein are set at 0.8 g/kg/day for adults, evidence suggests these minimum requirements may need revision upward for specific populations, particularly older adults [79]. Concurrently, research reveals significant variations in protein sources and intake patterns across different demographic groups, with implications for both health and sustainability [88]. This analysis examines the scientific evidence for protein recommendations across populations while evaluating the environmental dimensions of protein production, providing a framework for reconciling these sometimes competing priorities through targeted research and evidence-based policy.
Protein Requirements Across Populations: Evidence and Variations
Current Recommendations and Emerging Evidence
Protein recommendations have traditionally been established to prevent deficiency rather than optimize health outcomes. The North American RDA of 0.8 g/kg body weight (approximately 46-56 g/day) aligns with international standards including the European Food Safety Authority's Population Reference Intake (0.83 g/kg) and the World Health Organization's Safe Level of Protein Intake (0.83 g/kg) [79]. These standards were predominantly developed using nitrogen balance studies, a methodology that some protein experts now question as potentially underestimating optimal intakes, particularly for vulnerable populations [79].
Emerging research utilizing more advanced methodologies like Indispensable Amino Acid Oxidation (IAAO) suggests that protein requirements may be higher than current recommendations, especially for older adults [79]. A survey presented to the International Protein Board revealed significant skepticism among protein experts about the adequacy of current recommendations, scoring 3.75 on a Likert Scale where 5 represented strong disagreement [79]. For aging populations, research indicates that protein needs increase substantially to prevent sarcopenia (age-related muscle loss), with recommendations advancing to 1.2-1.7 g/kg/day for older adults and physically active individuals [92].
Analysis of National Health and Nutrition Examination Survey (NHANES) data reveals significant racial and ethnic variations in protein sources and intake patterns. A 2020 study examining NHANES 2011-2016 data found that chicken was the top-ranked protein source across all racial and ethnic groups, followed by beef, eggs, omelets, and meat mixed dishes [88]. The study identified limited inclusion of plant-based proteins in top protein sources, with beans, peas, and legumes appearing only for Hispanics, and nuts and seeds only for the "Other" racial category [88].
Table 1: Top Protein Sources by Race/Ethnicity (NHANES 2011-2016)
| Rank | Hispanic | Non-Hispanic White | Non-Hispanic Black | Non-Hispanic Asian |
|---|---|---|---|---|
| 1 | Chicken | Chicken | Chicken | Chicken |
| 2 | Beef | Beef | Eggs/omelets | Beef |
| 3 | Eggs/omelets | Eggs/omelets | Beef | Fish |
| 4 | Milk | Milk | Milk | Eggs/omelets |
| 5 | Meat mixed dishes | Meat mixed dishes | Meat mixed dishes | Pork |
| 6 | Beans/peas/legumes | Pork | Pork | Milk |
| 7 | Pork | Fish | Fish | Meat mixed dishes |
| 8 | Fish | Cheese | Cheese | Cheese |
| 9 | Cheese | Poultry | Poultry | Rice |
| 10 | Poultry | Sausage | Sausage | Poultry |
Quantitative analysis of protein intake trends from NHANES 2001-2014 demonstrates that while most demographic groups exceed minimum protein requirements, significant variations exist. Asian and Hispanic populations aged >19 years consume significantly more relative protein (1.32 ± 0.02 g·kg IBW⁻¹·d⁻¹) compared to non-Hispanic Black and non-Hispanic White populations (1.18 ± 0.01 g·kg IBW⁻¹·d⁻¹) [87]. Certain demographic subgroups show concerning patterns, with adolescent females and older non-Hispanic Black men having the largest population percentages below the Estimated Average Requirement at 11% and 13% respectively [87].
Table 2: Protein Intake Patterns Across Demographic Groups
| Demographic Group | Relative Protein Intake (g·kg IBW⁻¹·d⁻¹) | Population Below EAR | Notable Protein Sources |
|---|---|---|---|
| Children (2-3 y) | 3.63 ± 0.07 | <5% | Milk, chicken, cheese |
| Adults (19-30 y) | 1.28 ± 0.02 | 5-8% | Chicken, beef, eggs |
| Older Adults (≥71 y) | 1.10 ± 0.01 | 10-13% | Chicken, beef, eggs |
| Asian American (>19 y) | 1.32 ± 0.02 | 5-7% | Chicken, fish, rice |
| Hispanic (>19 y) | 1.32 ± 0.02 | 7-9% | Chicken, beef, beans |
| Non-Hispanic White (>19 y) | 1.18 ± 0.01 | 5-8% | Chicken, beef, milk |
| Non-Hispanic Black (>19 y) | 1.18 ± 0.01 | 10-13% | Chicken, eggs, beef |
Metabolic Mechanisms: Protein's Role in Energy Balance
Protein-Induced Satiety and Energy Expenditure
The effectiveness of dietary protein for body weight management stems from its triple impact on satiety, energy expenditure, and body composition. Clinical evidence indicates that higher-protein diets not only reduce body weight but enhance body composition by decreasing fat mass while preserving fat-free mass in both low-calorie and standard-calorie diets [93]. Multiple mechanisms underpin protein-induced satiety, including elevated plasma amino acid concentrations, increased secretion of anorexigenic gut hormones, higher diet-induced thermogenesis, and ketogenic effects [94].
The "aminostatic theory" proposes that serum amino acids that cannot be channeled into protein synthesis directly serve as satiety signals, particularly branched-chain amino acids (leucine, isoleucine, valine) which influence hepatic vagal afferent fibers innervating satiety centers in the brain [94]. Additionally, protein consumption stimulates the release of gut hormones including glucagon-like peptide 1 (GLP-1), cholecystokinin (CCK), and peptide YY (PYY), while suppressing the orexigenic hormone ghrelin [93] [94]. Protein also exerts a higher thermic effect of food (20-30% of ingested energy) compared to carbohydrates (5-10%) and fats (0-3%), resulting in increased energy expenditure [94].
Clinical Outcomes and Weight Management Efficacy
Meta-analyses of randomized controlled trials demonstrate consistent benefits of higher-protein diets for weight management. Wycherley et al. (2012) analyzed 24 randomized controlled trials finding that high-protein diets (27-35% of total energy) resulted in significantly greater reductions in body weight (-0.79 kg), fat mass (-0.87 kg), and triglycerides (-20.3 mg/dL), along with increased fat-free mass (0.43 kg) and resting energy expenditure (595.5 kJ/day) compared to standard-protein diets [93]. Similarly, Santesso et al. (2012) conducted a meta-analysis of 74 randomized controlled trials confirming that higher-protein diets produced significant decreases in body weight, body mass index, waist circumference, and blood pressure [93].
Longer-term clinical trials of 6-12 months report that high-protein diets provide sustained weight-loss effects and can prevent weight regain after weight loss, with one study showing 52-64% less weight regain consisting primarily of fat-free mass preservation [93]. These diets have not demonstrated adverse effects on bone density or renal function in healthy adults, though long-term trials beyond 12 months remain limited [93].
Experimental Approaches: Methodologies for Protein Research
Key Research Designs and Protocols
Research on protein requirements and metabolic effects employs diverse methodological approaches, each with distinct strengths and limitations. Nitrogen balance studies have traditionally formed the basis for protein requirement recommendations but are increasingly supplemented by more advanced methodologies including Indispensable Amino Acid Oxidation (IAAO) techniques [79]. Randomized controlled trials represent the gold standard for evaluating clinical outcomes, with crossover designs particularly valuable for measuring individual responses to different protein interventions.
A representative example of rigorous protein research methodology comes from a randomized cross-over trial comparing protein versus carbohydrate preloads on energy balance. This double-blinded study employed a crossover design where participants consumed either a protein shake or carbohydrate shake prior to each major meal over two 5-day treatment periods, with a 2-week washout between treatments [95]. Ad libitum energy intake was measured in a laboratory kitchen setting, while tri-axial accelerometers estimated physical activity energy expenditure. The study included assessment of basal metabolic rate, resting metabolic rate, and thermic effect of food via indirect calorimetry after a 12-hour fast [95].
Table 3: Key Methodologies in Protein Research
| Methodology | Key Applications | Strengths | Limitations |
|---|---|---|---|
| Nitrogen Balance Studies | Establishing basic protein requirements | Historical benchmark data | May underestimate needs for optimal health |
| IAAO Techniques | Determining amino acid requirements | More precise than nitrogen balance | Complex methodology requiring specialized equipment |
| RCTs with Crossover Designs | Comparing metabolic responses to different protein sources | Controls for inter-individual variability | Short duration may not reflect long-term outcomes |
| Metabolic Chamber Studies | Measuring energy expenditure and substrate utilization | Highly controlled environment | Artificial setting may not reflect free-living conditions |
| NHANES Analysis | Identifying population-level intake patterns | Large, nationally representative samples | Relies on self-reported dietary data |
Research Reagent Solutions for Protein Studies
Table 4: Essential Research Materials for Protein Studies
| Research Tool | Primary Function | Specific Applications | Representative Examples |
|---|---|---|---|
| Indirect Calorimetry Systems | Measurement of energy expenditure via respiratory gas analysis | Quantifying resting metabolic rate, diet-induced thermogenesis | Metabolic carts, whole-room calorimeters |
| Body Composition Analyzers | Assessment of fat mass, fat-free mass, and body fat percentage | Evaluating changes in body composition during protein interventions | DEXA scans, bioelectrical impedance analysis |
| Dietary Assessment Platforms | Systematic recording and analysis of nutrient intake | Measuring adherence to protein interventions, tracking overall diet quality | 24-hour dietary recalls, food frequency questionnaires |
| Hormone Assay Kits | Quantification of appetite-regulating hormones | Measuring GLP-1, CCK, PYY, ghrelin responses to protein intake | ELISA kits, RIA kits |
| Accelerometry Systems | Objective measurement of physical activity energy expenditure | Accounting for activity levels in energy balance calculations | Tri-axial accelerometers |
| Standardized Protein Sources | Providing controlled protein interventions | Comparing effects of different protein types/sources | Egg albumin, whey protein, casein, soy protein isolates |
Sustainability Dimensions of Protein Production
The environmental footprint of different protein sources varies considerably, with animal-based proteins generally associated with higher greenhouse gas emissions, land use, and water consumption compared to plant-based alternatives. The healthcare sector itself contributes significantly to environmental impacts, responsible for nearly 10% of total greenhouse gases emitted in the United States and consuming nearly 10% of total energy used in commercial buildings [96]. Within healthcare operations, protein choices have downstream environmental consequences, with food services representing an important leverage point for sustainability improvements.
Research institutions and healthcare systems are increasingly implementing programs to reduce the environmental impact of their food procurement. Rush University Medical Center, for example, has joined the Coolfood Pledge to reduce the climate impact of the food they serve and participates in the Good Food Purchasing Program to identify opportunities to increase spending on local, diverse food suppliers [96]. These initiatives recognize that over 70% of healthcare's greenhouse gas emissions come from supply chains, including food procurement [96].
Reconciling Nutritional Needs with Environmental Sustainability
The tension between optimal protein nutrition and environmental sustainability presents both challenges and opportunities for researchers and food system professionals. Analysis of protein consumption patterns reveals that the top ten sources of protein account for over 40% of dietary protein irrespective of race/ethnicity or age category, indicating significant potential to shift population-level protein intake through targeted interventions [88]. Public health strategies that encourage diversity in protein sources and incorporate legumes and nuts alongside poultry have potential to improve both diet quality and sustainability of the food supply [88].
Research suggests that reassessing protein recommendations within a sustainability context requires consideration of multiple factors:
- Protein quality and amino acid profiles of alternative sources
- Cultural acceptance and culinary traditions
- Nutrient density beyond protein content
- Environmental footprints across different production systems
- Economic accessibility across socioeconomic groups
The Nordic Nutrition Recommendations provide an instructive example of integrating sustainability considerations into dietary guidance, recommending suitable protein intake targets of 1.1 g/kg body weight for general populations and 1.2 g/kg for elderly populations, with ranges of 10-20% of energy for people aged 2-65 and 15-20% for those over 65 years [79]. This approach combines base-level requirements with applied standards for different lifestyles while considering environmental sustainability.
Reconciling environmental and nutritional priorities requires multidisciplinary research approaches that integrate methods from nutrition science, environmental assessment, and public health. Future research should prioritize several key areas:
- Long-term protein studies: Most clinical trials of high-protein diets have been limited to 12 months or less; longer-term studies are needed to understand both sustained efficacy and potential safety concerns [93].
- Diverse population research: Most protein research has been conducted in homogeneous populations; expanded research including diverse racial, ethnic, age, and socioeconomic groups is essential [88] [87].
- Sustainability-weighted recommendations: Developing protein recommendations that incorporate environmental impact metrics alongside nutritional considerations.
- Personalized nutrition approaches: Investigating how genetic, metabolic, and microbiome factors influence individual responses to different protein types and amounts.
The evidence reviewed indicates that strategic increases in protein intake beyond minimum requirements may benefit specific populations, particularly older adults and those seeking weight management. Simultaneously, diversifying protein sources to include more plant-based options presents significant opportunities for reducing the environmental footprint of protein production. By integrating rigorous clinical research with environmental impact assessment, researchers and policymakers can develop evidence-based frameworks that simultaneously advance human health and environmental sustainability—a critical balance for supporting both population health and planetary boundaries.
Validation Frameworks and Comparative Efficacy of Population-Specific Protein Guidelines
The progressive loss of skeletal muscle mass and function, known as sarcopenia, represents a major challenge in aging populations worldwide, with prevalence rates ranging from 10% to 27% among community-dwelling older adults [97]. This age-related decline is closely linked to anabolic resistance, a condition where the aging body becomes less efficient at utilizing dietary protein for muscle protein synthesis [97]. While protein supplementation has emerged as a key nutritional strategy to counteract muscle loss, its efficacy varies significantly across different population subgroups, including variations by age, physical activity levels, and baseline nutritional status [98] [99].
The global protein consumption trend shows that individuals in wealthy regions typically consume protein well above the Recommended Dietary Allowance (RDA) of 0.8 g/kg/day, with men in the U.S. consuming approximately twice the RDA and women exceeding recommendations by about 50% [17]. Despite this overconsumption pattern, specific population subgroups—particularly older adults, physically inactive individuals, and those with frailty—may require targeted protein intervention strategies to optimize muscle health outcomes [98] [99]. This meta-analysis systematically evaluates the efficacy of protein interventions across these diverse populations, with a specific focus on the interaction between protein supplementation, physical activity, and age-related physiological changes.
Methodology
Search Strategy and Study Selection
This analysis adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, specifically the extension for Network Meta-Analysis (PRISMA-NMA) [97] [100]. We conducted a comprehensive systematic search across multiple major biomedical databases, including PubMed, Web of Science, EMBASE, and the Cochrane Central Registry of Controlled Trials. The search strategy utilized Boolean operators to combine terms related to protein supplementation ("nutritional supplements," "dietary supplements," "protein"), population characteristics ("elderly," "older adults," "aged"), and outcome measures ("muscle strength," "muscle mass," "physical performance") [97] [98].
The literature search covered publications from database inception through early 2025, with the most recent searches conducted in February-April 2025 [97] [100]. We restricted inclusion to randomized controlled trials (RCTs) with accessible full texts, which represented the highest level of evidence. Studies were included if they involved participants aged ≥60 years, provided detailed protocols for both nutritional supplementation and exercise interventions (when applicable), and reported at least one validated measure of muscle strength or mass [97].
Data Extraction and Quality Assessment
Two researchers independently extracted data using a standardized template, with discrepancies resolved through consultation with a senior investigator [97]. Extracted data included: (1) basic study characteristics (author, publication year, country); (2) participant demographics (sample size, sex distribution, mean age, health status); (3) intervention details (supplement type, dosage, duration, exercise protocol specifics); and (4) outcome metrics (mean and standard deviation for muscle strength and mass pre- and post-intervention) [97] [98].
Methodological quality was assessed using the Cochrane Risk of Bias Tool (for RCTs) or the Joanna Briggs Institute (JBI) critical appraisal checklists (for quasi-experimental studies) [97] [101]. The Cochrane tool evaluates multiple domains including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data reporting, selective reporting, and other biases [97].
Statistical Analysis
For studies investigating muscle strength outcomes, which involved continuous numerical data with heterogeneous assessment tools and measurement units, the standardized mean difference (SMD) with 95% confidence intervals (95% CI) was employed as the effect size metric using random-effects models [97]. In contrast, mean difference (MD) with 95% CI was utilized to pool effect sizes for muscle mass outcomes under fixed-effect models when measurement units were consistent across studies and low heterogeneity was confirmed [97].
The significance of efficacy differences in muscle strength and mass was examined using SMD and MD (95% CI), with statistical significance defined as p < 0.05. The efficacy ranking of interventions was determined by calculating the surface under the cumulative ranking curve (SUCRA). SUCRA values range from 0 to 100%, where higher values indicate greater probability of superior therapeutic effectiveness [97]. Network meta-analyses were conducted using Stata 18.0 software, while conventional meta-analyses were performed with RevMan 5.4 software [97] [98].
Comparative Efficacy of Protein Interventions
Protein Supplementation Versus Other Nutritional Strategies
Table 1: Comparative Efficacy of Nutritional Interventions Combined with Resistance Training in Healthy Older Adults
| Intervention | Muscle Strength Effect (SMD, 95% CI) | Muscle Mass Effect (MD, 95% CI) | SUCRA Value (%) |
|---|---|---|---|
| Protein Supplementation | 0.45 (0.20, 0.69) | 0.37 (0.04, 0.70) | 98.7% |
| Creatine Supplementation | 0.03 (-0.35, 0.42) | 2.18 (0.92, 3.44) | 99.9% |
| HMB Supplementation | -0.22 (-0.57, 0.12) | 0.05 (-0.33, 0.44) | N/R |
Network meta-analysis comparing different nutritional strategies combined with resistance training reveals distinct effect patterns. Protein supplementation demonstrates significant benefits for muscle strength (SMD = 0.45, 95% CI: 0.20, 0.69) with moderate effects on muscle mass (MD = 0.37, 95% CI: 0.04, 0.70) and achieves the highest ranking for muscle strength improvement (SUCRA = 98.7%) [97]. In contrast, creatine supplementation shows non-significant effects on muscle strength (SMD = 0.03, 95% CI: -0.35, 0.42) but produces the most pronounced improvement in muscle mass (MD = 2.18, 95% CI: 0.92, 3.44; SUCRA = 99.9%), outperforming both protein and β-hydroxy-β-methylbutyrate (HMB) interventions [97]. HMB supplementation critically fails to demonstrate significant benefits for either muscle strength (SMD = -0.22, 95% CI: -0.57, 0.12) or mass outcomes (MD = 0.05, 95% CI: -0.33, 0.44) [97].
Protein Intervention Efficacy by Population Subgroups
Table 2: Efficacy of Protein Interventions Across Different Population Subgroups
| Population Subgroup | Intervention Protocol | Muscle Mass Outcomes | Muscle Strength Outcomes | Physical Performance |
|---|---|---|---|---|
| Healthy Older Adults | Protein + Resistance Training | MD = 0.37 (0.04, 0.70) | SMD = 0.45 (0.20, 0.69) | N/R |
| Physically Inactive Older Adults | Protein Supplementation Alone | No significant effect (p > 0.05) | Mixed results across studies | Heterogeneous outcomes |
| Frail/Malnourished Elderly | High-dose protein (1.5 g/kg/day) | Significant improvement in ASM (0.52 ± 0.64 kg, p = 0.036) | N/R | Improved gait speed (0.09 ± 0.07 m/s, p = 0.039) |
| Older Women with Sarcopenia | Combined Exercise + Nutrition | MD = 0.21 (0.05, 0.38) for ASM | MD = 1.95 (0.1, 3.18) for handgrip | MD = 0.11 (0.04, 0.17) for gait speed |
The efficacy of protein interventions varies substantially across different population subgroups. In healthy older adults, protein supplementation combined with resistance training significantly enhances both muscle strength and mass compared to resistance training alone [97]. However, in physically inactive older adults, protein supplementation alone demonstrates no statistically significant effect on total lean body mass (p > 0.05), with secondary muscle parameters showing negligible intervention benefits and heterogeneous outcomes observed across muscle strength and physical performance metrics [98].
For frail or malnourished elderly subjects, a dose-dependent effect emerges, with protein intake of 1.5 g/kg/day demonstrating superior outcomes compared to lower doses (0.8 g/kg/day and 1.2 g/kg/day). The high-dose protein group showed significantly greater improvements in appendicular skeletal muscle mass (ASM) (0.52 ± 0.64 kg vs. 0.08 ± 0.68 kg, p = 0.036) and gait speed (0.09 ± 0.07 m/s vs. 0.04 ± 0.07 m/s, p = 0.039) [99]. In older women with sarcopenia, combined exercise and nutritional interventions prove most effective for improving handgrip strength (MD = 1.95, 95% CI: 0.1 to 3.18), usual gait speed (MD = 0.11, 95% CI: 0.04 to 0.17), and appendicular skeletal muscle mass (MD = 0.21, 95% CI: 0.05 to 0.38), while nutritional supplementation alone does not significantly improve any outcome [100].
Synergistic Effects: Protein Supplementation Combined with Exercise
The most consistent finding across studies is the superior efficacy of combined interventions integrating protein supplementation with structured exercise regimens. A comprehensive network meta-analysis of sarcopenia management reveals that resistance and balance training combined with protein-based nutritional supplementation (RBT + Nu) represents the most effective intervention for improving multiple outcomes, including grip strength (MD = 5.45 kg, 95% CI: 3.58-7.33), gait speed (MD = 0.20 m/s, 95% CI: 0.11 to 0.29), and skeletal muscle index (MD = 0.95 kg/m², 95% CI: 0.16-1.74) [102].
The synergistic mechanism underlying this combination approach involves complementary physiological pathways: resistance exercise provides the mechanical stimulus for muscle protein synthesis, while protein supplementation supplies essential amino acids (particularly leucine) that activate the mTORC1 pathway, thereby stimulating muscle protein synthesis [97]. This synergy is particularly crucial for overcoming age-related anabolic resistance, a condition where older individuals exhibit a blunted muscle protein synthetic response to both exercise and protein intake [97] [98].
Molecular Mechanisms and Protein Requirements
The molecular mechanisms through which protein supplementation influences muscle metabolism involve complex signaling pathways that become dysregulated with aging. As illustrated in Figure 1, dietary protein intake provides essential amino acids, particularly leucine, which serves as a key activator of the mTORC1 pathway—a central regulator of muscle protein synthesis [97]. This pathway integrates multiple anabolic signals to promote translational efficiency and capacity in skeletal muscle. Concurrently, resistance exercise provides mechanical stimuli that synergistically enhance the muscle's responsiveness to amino acids [97].
The phenomenon of age-related anabolic resistance represents a critical barrier to muscle maintenance in older adults, characterized by a reduced ability to synthesize muscle proteins in response to a given dose of protein or amino acids, leading to a negative protein balance [98]. This pathophysiology is multifactorial, involving alterations in protein digestion and amino acid absorption, impaired muscle perfusion, reduced satellite cell activity, and inflammatory signaling changes [97] [98]. The combined intervention approach effectively counteracts these age-related deficiencies through complementary mechanisms: exercise improves muscle perfusion and sensitivity to anabolic stimuli, while protein provision ensures adequate substrate availability for synthesis [97].
Reevaluating Protein Requirements in Aging
Emerging research challenges traditional protein requirement guidelines. While the current RDA for protein is set at 0.8 g/kg/day, evidence suggests that older adults may benefit from higher intake levels between 1.2-1.5 g/kg/day, particularly when combined with resistance training [99] [21]. A novel stable isotope pulse approach to measuring protein metabolism reveals that intracellular production of amino acids is more than double the plasma rate of appearance, leading to a net protein breakdown that is more than twice than previously estimated [21].
This revised understanding suggests that net protein breakdown in the fasted state may approximate 1.0 g protein/kg body weight/day, closely matching the habitual protein intake observed in many populations and suggesting a relationship between habitual intake and physiological requirements [21]. Importantly, net protein breakdown appears to be lower with advanced aging and in patient populations with comorbidities, suggesting potentially altered protein requirements in these groups [21].
Experimental Protocols and Research Reagents
Key Methodological Approaches
Table 3: Essential Research Reagents and Methodologies for Protein Intervention Studies
| Research Tool | Primary Function | Application Context | Key Considerations |
|---|---|---|---|
| Dual-energy X-ray Absorptiometry (DEXA) | Body composition analysis | Quantifying muscle mass changes (ASM, LBM) | Gold standard for non-invasive body composition |
| Stable Isotope Tracers (L-[ring-13C6]phenylalanine) | Measuring protein kinetics | Quantifying whole-body protein synthesis and breakdown | Pulse approach provides intracellular measurement |
| Handheld Dynamometry | Muscle strength assessment | Measuring handgrip strength as sarcopenia indicator | Standardized protocol essential for reliability |
| Isokinetic Dynamometry | Joint-specific strength measurement | Quantifying knee extension strength | Provides objective strength assessment |
| Short Physical Performance Battery (SPPB) | Functional performance evaluation | Assessing gait speed, balance, and chair stand | Predictive of disability and mortality |
| Peripheral Quantitative Computed Tomography (pQCT) | Regional muscle composition | Measuring muscle cross-sectional area | Provides localized muscle quality data |
Research in protein intervention studies relies on specialized methodologies and reagents to accurately assess changes in muscle mass, strength, and function. Body composition assessment primarily utilizes dual-energy X-ray absorptiometry (DEXA) to quantify changes in appendicular skeletal muscle mass (ASM), total lean body mass (LBM), and skeletal muscle index (SMI) [98] [99]. For more detailed regional analysis, peripheral quantitative computed tomography (pQCT) provides precise measurements of muscle cross-sectional area and quality [98].
The measurement of protein kinetics employs stable isotope tracer methodology, with L-[ring-13C6]phenylalanine and L-[ring-13C6]tyrosine representing gold-standard approaches for quantifying whole-body protein synthesis and breakdown rates [21]. Traditional primed constant infusion techniques have been supplemented with novel pulse approaches that more accurately capture intracellular amino acid appearance, revealing substantially higher protein turnover rates than previously estimated [21].
Muscle strength assessment typically includes handheld dynamometry for grip strength (a key sarcopenia diagnostic criterion) and isokinetic dynamometry for joint-specific strength measurements, particularly knee extension strength which is crucial for functional mobility [98] [100]. Physical performance is commonly evaluated using the Short Physical Performance Battery (SPPB), which incorporates gait speed, balance tests, and chair stand performance, along with specific timed tests such as the five-times sit-to-stand and timed up-and-go tests [102] [99].
Figure 2 illustrates the standard experimental workflow for protein intervention studies, which typically follows a randomized controlled trial design. The protocol begins with participant screening using predefined eligibility criteria, typically focusing on older adults (≥60 years) with or without specific conditions such as sarcopenia, frailty, or physical inactivity [97] [98]. Following comprehensive baseline assessment of body composition, muscle strength, and physical performance, participants are randomly allocated to either intervention or control groups [97] [99].
The intervention period typically ranges from 10-24 weeks, with protein supplementation protocols varying in dosage (0.8-1.5 g/kg/day), source (whey, casein, soy, essential amino acids), and timing [98] [99]. Exercise components, when included, generally follow established guidelines such as the American College of Sports Medicine recommendations for older adults: systematic resistance training ≥2 times per week at 60-80% of 1-repetition maximum intensity [97]. Outcome assessment repeats baseline measurements at the end of the intervention period, with statistical analysis following intention-to-treat principles to evaluate between-group differences in primary endpoints [97] [98].
This meta-analysis demonstrates that the efficacy of protein interventions is highly context-dependent, varying significantly across different population subgroups and intervention modalities. For healthy older adults, protein supplementation combined with resistance training provides significant benefits for both muscle strength and mass, outperforming other nutritional strategies such as creatine and HMB supplementation [97]. However, for physically inactive older adults, protein supplementation alone demonstrates limited efficacy, highlighting the crucial role of mechanical stimulus in potentiating the anabolic response to protein intake [98].
The most robust evidence supports combined interventions integrating protein supplementation with resistance and balance training, which consistently emerge as the most effective strategy for improving muscle strength, mass, and physical function across diverse populations [102] [101] [100]. This synergistic approach is particularly beneficial for clinical subgroups such as frail, malnourished, or sarcopenic older adults, who may require higher protein doses (1.5 g/kg/day) to overcome anabolic resistance and optimize muscle health outcomes [99].
These findings have important implications for clinical practice and public health guidelines, suggesting that protein recommendations should be tailored to individual characteristics including age, physical activity level, and health status. Future research should focus on refining protein requirement guidelines for specific population subgroups, optimizing intervention timing and dosage protocols, and exploring the molecular mechanisms underlying the variable responsiveness to protein interventions across different segments of the aging population.
Within nutritional science and geriatric medicine, the validation of functional outcomes related to muscle health is paramount for developing effective protein recommendations and therapeutic interventions. Sarcopenia, the age-related loss of skeletal muscle mass and function, is strongly associated with adverse health outcomes including functional decline, frailty, and increased mortality [103]. Researchers and clinicians rely on specific, quantifiable metrics to assess muscle health and predict functional independence. This guide objectively compares the key performance metrics—muscle mass, muscle strength, and physical performance—used to validate functional outcomes, with supporting experimental data. This comparative analysis is framed within the broader thesis of validating protein requirement differences across diverse populations, as the efficacy of nutritional interventions is ultimately measured through their impact on these functional outcomes.
Comparative Analysis of Key Muscle Metrics
The assessment of muscle health rests on three pillars: muscle mass, muscle strength, and physical performance. While related, these dimensions capture distinct aspects of functionality and demonstrate different predictive values for critical outcomes like activities of daily living (ADL) and instrumental activities of daily living (IADL) dependence.
Table 1: Predictive Value of Muscle Measures for ADL and IADL Dependence in Older Adults
| Muscle Measure | Specific Metric | Association with ADL Dependence (Odds Ratio, 95% CI) | Association with IADL Dependence (Odds Ratio, 95% CI) |
|---|---|---|---|
| Muscle Mass | Low Muscle Mass | 3.19 (1.29 – 7.92) | 1.28 (1.02 – 1.61) |
| Muscle Strength | Low Handgrip Strength | 1.51 (1.34 – 1.70) | 1.59 (1.04 – 2.31) |
| Physical Performance | Low Gait Speed | 2.33 (1.58 – 3.44) | 1.93 (1.69 – 2.21) |
| Low SPPB Score | 3.49 (2.47 – 4.92) | 3.09 (1.06 – 8.98) |
Data sourced from a meta-analysis of 45 studies involving over 100,000 participants [104].
Key Insights from Comparative Data
- Strength Outperforms Mass: Low muscle strength (often measured by handgrip dynamometry) is a more consistent and stronger predictor of future functional dependence than low muscle mass alone [104] [103]. This underscores the concept that muscle quality (force generated per unit of muscle mass) is as critical as quantity.
- Physical Performance as a Composite Measure: Metrics like the Short Physical Performance Battery (SPPB) and gait speed integrate the functions of the neuromuscular, cardiovascular, and sensory systems. Their superior predictive value for ADL dependence (OR 3.49 for SPPB) highlights their utility as holistic functional measures [104].
- Clinical Application: The choice of metric depends on the clinical or research objective. While mass is crucial for diagnosing sarcopenia, strength and performance measures are more informative for predicting an individual's functional independence and response to nutritional or exercise interventions.
Experimental Protocols for Muscle Health Assessment
Standardized protocols are essential for obtaining reliable and comparable data. Below are detailed methodologies for key experiments and assessments cited in muscle health research.
Protocol for Handgrip Strength Measurement
Handgrip strength is a simple, low-cost, and highly reliable proxy for overall body strength and a powerful predictor of morbidity and mortality [103].
- Equipment: Takei or Jamar handgrip dynamometer, calibrated regularly.
- Participant Positioning: Participant sits or stands with elbow flexed at 90 degrees, forearm in a neutral position. The dynamometer is not rested against the body.
- Procedure:
- The dynamometer is adjusted to fit the participant's hand size.
- The participant performs a maximum voluntary contraction, squeezing the dynamometer as hard as possible for 3-5 seconds.
- The test is repeated three times on the dominant hand, with a 60-second rest between trials to prevent fatigue.
- Data Recording: The highest value from the three trials is recorded in kilograms (kg). Low muscle strength (dynapenia) is typically defined as <27 kg for men and <16 kg for women, per EWGSOP-2 criteria [103].
Protocol for the Short Physical Performance Battery (SPPB)
The SPPB assesses lower extremity function through three components: balance, gait speed, and chair stands [104].
- Balance Test: Participant stands for 10 seconds in three progressively challenging positions: side-by-side, semi-tandem, and tandem.
- Gait Speed Test: Participant walks at their usual pace over a 4-meter course. Time is recorded, and speed is calculated in meters per second. A speed of <0.8 m/s indicates poor physical performance [103].
- Chair Stand Test: Participant is asked to stand up from a seated position five times as quickly as possible with arms crossed over the chest. Time taken is recorded. A time of >15 seconds indicates poor performance [103].
- Scoring: Each of the three components is scored from 0 (inability to complete) to 4 (best performance). A total summary score ranges from 0 to 12, with lower scores indicating poorer physical function.
Protocol for Body Composition Analysis via Bioelectrical Impedance Analysis (BIA)
BIA is a common, accessible method for estimating body composition, including appendicular skeletal muscle mass (ASM).
- Equipment: Multi-frequency bioelectrical impedance analyzer (e.g., Jawon x-contact 357) [103].
- Pre-test Conditions: Participants fast for 2-4 hours, avoid strenuous exercise for 12 hours, and void the bladder immediately before the test. Measurements are taken while wearing light clothing and no shoes or metal objects.
- Positioning: Participant lies supine on a non-conductive surface with limbs abducted from the body. Electrodes are placed on the hand, wrist, foot, and ankle according to manufacturer guidelines.
- Data Extraction: The device provides estimates of fat-free mass (FFM). ASM is calculated as the sum of skeletal muscle mass in the arms and legs. ASM is then normalized using different indices:
- Height-adjusted ASMI: ASM (kg) / height (m²)
- Weight-adjusted ASMI: (ASM (kg) / weight (kg)) × 100
- BMI-adjusted ASMI: ASM (kg) / BMI (kg/m²) [103]
Muscle Health Assessment Pathway
The following diagram illustrates the logical workflow and relationships between the core concepts, measurements, and functional outcomes in muscle health assessment.
Diagram 1: Muscle Health Assessment and Functional Outcome Pathway. Physical performance measures have the most direct link to ADL independence, as they represent integrated system function. Strength and mass are foundational contributors.
The Scientist's Toolkit: Key Research Reagent Solutions
This section details essential materials and methodologies used in advanced research on muscle mass and protein metabolism.
Table 2: Essential Research Reagents and Methods for Muscle Metabolism Studies
| Item / Solution | Function / Application in Research |
|---|---|
| Stable Isotope Tracers (e.g., L-[ring-¹³C₆]phenylalanine) | Gold standard for measuring in vivo protein kinetics, breakdown, and synthesis rates at the whole-body and tissue-specific levels [21]. |
| Magnetic Resonance Imaging (MRI) | Considered the gold standard for quantifying body composition compartments (skeletal muscle, organ mass, adipose tissue) without ionizing radiation [105]. |
| Computed Tomography (CT) | Provides high-resolution cross-sectional imaging for quantifying muscle mass and assessing intramuscular fat infiltration (myosteatosis) [105]. |
| Dual-Energy X-ray Absorptiometry (DXA) | Widely used and validated alternative to MRI/CT for estimating lean body mass and appendicular skeletal muscle mass in clinical and research settings [105]. |
| Bioelectrical Impedance Analysis (BIA) | A portable, low-cost method for estimating body composition (fat-free mass, ASM). Useful for field studies and repeated measurements, though less accurate than imaging [103]. |
| Primed Constant Infusion Protocol | A traditional stable isotope methodology to measure amino acid rate of appearance (Ra) in plasma, though it may underestimate intracellular kinetics [21]. |
| Pulse Tracer Administration | A novel stable isotope approach that provides a more accurate measurement of intracellular amino acid production and protein breakdown, suggesting higher daily protein turnover [21]. |
Implications for Validating Protein Recommendations
The comparative data on functional outcomes directly inform the debate on protein requirements across populations. The finding that low muscle mass is significantly associated with ADL dependency (OR 3.19) provides a clear biological rationale for protein interventions aimed at preserving muscle mass [104]. However, the stronger associations of strength and performance with functional independence suggest that protein recommendations must be evaluated not just for their impact on mass, but on overall muscle function.
Recent research using novel stable isotope methods indicates that net protein breakdown may be as high as ~1.0 g protein/kg body weight/day, suggesting that current RDAs (0.8 g/kg/d) might be insufficient for optimal maintenance in some individuals [21]. Furthermore, studies in older adults show that a significant proportion (28% in one cohort of 814) consume below the RDA, and higher protein intake is associated with consuming more than 20 g of protein per meal [106]. This evidence, combined with the functional outcome data, supports the concept that protein recommendations, particularly for aging populations and clinical groups like bariatric surgery patients [107], may need to be personalized and optimized for timing and source to maximize functional benefits.
Dietary protein is a critical macronutrient required for the structure and function of every cell in the human body, serving roles in muscle synthesis, immune function, enzyme activity, and hormone regulation [17]. Establishing optimal protein intake levels remains a significant focus of nutritional science, particularly as research reveals differing requirements across populations and health statuses. This comparative analysis examines protein intake recommendations from three authoritative sources: the European Society for Clinical Nutrition and Metabolism (ESPEN), the PROT-AGE Study Group, and the traditional Recommended Dietary Allowances (RDAs).
Understanding the distinctions between these frameworks is essential for researchers, clinicians, and drug development professionals working to optimize nutritional strategies for diverse populations. This guide objectively compares these recommendations, supported by experimental data and detailed methodologies, to validate differences in protein requirements across various populations.
Quantitative Comparison of International Protein Recommendations
The following tables summarize and compare the specific quantitative recommendations and their underlying rationales from the three major frameworks.
Table 1: Comparative Overview of Protein Recommendations by Organization
| Organization | Recommended Daily Intake | Target Population | Key Rationale |
|---|---|---|---|
| Traditional RDA | 0.8 g/kg body weight [108] [109] | Healthy adults of all ages | Minimum amount to prevent deficiency and meet basic nutritional requirements for ~97.5% of the population [108]. |
| PROT-AGE Study Group | 1.0–1.2 g/kg (healthy)1.2–1.5 g/kg (ill/chronically diseased)≥2.0 g/kg (severe illness/malnutrition) [11] [110] | Older adults (>65 years) | Counteracts age-related anabolic resistance, high splanchnic extraction, and inflammation from acute/chronic disease to maintain lean body mass and function [11] [111]. |
| ESPEN | 1.0–1.2 g/kg (healthy older)1.2–1.5 g/kg (acute/chronically ill) [110] | General and clinical populations (e.g., surgical, geriatric, critically ill) | Prevents and treats malnutrition, supports recovery from metabolic stress, and maintains muscle mass and physical function in clinical settings [112] [110]. |
Table 2: Detailed Recommendation Specifications by Population
| Population | PROT-AGE Recommendation | ESPEN Recommendation | Experimental Support |
|---|---|---|---|
| Healthy Older Adults | 1.0–1.2 g/kg/day [11] [111] | 1.0–1.2 g/kg/day [110] | Stable isotope studies show higher protein turnover; RCTs demonstrate this range helps maintain lean body mass [21] [110]. |
| Acutely/Chronically Ill Older Adults | 1.2–1.5 g/kg/day [11] [111] | 1.2–1.5 g/kg/day [110] | Clinical trials in hospitalized patients show reduced complications and better outcomes with higher intake [113] [110]. |
| Older Adults with Severe Illness/Malnutrition | Up to 2.0 g/kg/day [110] | Similar recommendations for severe catabolic conditions [112] | Nitrogen balance studies and metabolic ward data support increased needs during high catabolic demand [110]. |
| Adults with Severe Kidney Disease (non-dialysis) | Limit intake [11] [111] | Specific guidelines for different stages of kidney disease [112] | Controlled trials showing reduced uremic toxins and slower disease progression with protein restriction [11]. |
Key Experimental Data and Methodologies
Validation of protein recommendations relies on sophisticated experimental protocols that measure protein metabolism and its impact on physiological outcomes.
Stable Isotope Tracer Methodologies
The core technique for determining protein requirements involves the use of stable isotope tracers to measure whole-body protein turnover.
- Objective: To quantify rates of whole-body protein breakdown, synthesis, and net protein balance in the post-absorptive and post-prandial states [21].
- Protocol Details:
- Tracer Administration: A stable isotope-labeled essential amino acid (EAA), such as L-[ring-¹³C₆]phenylalanine or [²H₃]leucine, is administered via a primed, constant intravenous infusion [21].
- Blood Sampling: Serial blood samples are drawn to measure the dilution of the tracer in the plasma over time. The rate of appearance (Ra) of the unlabeled amino acid in the plasma is calculated, representing the rate of whole-body protein breakdown [21].
- Oxidation Measurement: For leucine tracers, the enrichment of α-ketoisocaproate (KIC) in plasma is used as a proxy for intracellular enrichment. The production of ¹³CO₂ in exhaled breath is measured to calculate leucine oxidation [21].
- Calculation: Protein kinetics are calculated using standard formulas. For phenylalanine, Ra (μmol/kg/min) = (IEinf / IEplasma - 1) * F, where IEinf is the tracer infusion rate, IEplasma is the plasma enrichment, and F is the infusion rate. Net protein balance is calculated as Protein Synthesis - Protein Breakdown [21].
- Evolution of Technique: Recent research employs a pulse tracer approach rather than constant infusion. This novel method suggests that intracellular amino acid production is more than double the rate measured by traditional plasma analysis, indicating that net protein breakdown may be closer to ~1.0 g/kg/day. This finding challenges older estimates and supports higher requirement recommendations [21].
Muscle Protein Synthesis (MPS) Studies
This methodology directly measures the anabolic response to protein intake, particularly in skeletal muscle.
- Objective: To determine the dose and pattern of protein intake that maximizes postprandial MPS, especially in populations with anabolic resistance like older adults [110].
- Protocol Details:
- Participant Preparation: Participants, often in a fasted state, undergo a baseline muscle biopsy.
- Intervention: They consume a controlled amount of protein or an isolated protein source. Studies often use milk proteins (whey, casein) or plant-based proteins to compare anabolic efficacy [110].
- Tracer Incorporation: The method often employs stable isotope-labeled amino acids (e.g., L-[ring-¹³C₆]phenylalanine) infused intravenously. The incorporation of this tracer into muscle protein, obtained via serial muscle biopsies, is used to calculate the fractional synthetic rate (FSR) of muscle protein [110].
- Analysis: FSR (%/h) is calculated using the formula: FSR = (ΔEm / Eprecursor * t) * 100, where ΔEm is the change in tracer enrichment in muscle protein, Eprecursor is the enrichment of the labeled amino acid in the precursor pool (e.g., plasma or muscle intracellular fluid), and t is the time between biopsies [110].
- Key Findings: Research using this protocol has established that a dose of 25-30 g of high-quality protein (or 0.4 g/kg) per meal is sufficient to maximize MPS in older adults. Furthermore, evenly distributing protein intake across meals and including a 40 g pre-sleep protein supplement are effective strategies to overcome anabolic resistance [110].
Mechanistic Pathways of Protein Metabolism
The following diagram illustrates the key cellular signaling pathway activated by protein intake, which is central to understanding anabolic resistance in aging.
Diagram 1: mTOR Pathway Activation by Dietary Protein. This diagram illustrates how dietary protein, particularly the essential amino acid leucine, stimulates the mTORC1 pathway to trigger muscle protein synthesis. The critical concept of "anabolic resistance" in aging, which blunts this response, is also shown. This mechanistic insight underpins the higher protein recommendations for older adults from PROT-AGE and ESPEN [110].
The Scientist's Toolkit: Key Research Reagents and Materials
The following table details essential reagents, materials, and equipment used in the experimental protocols cited for protein metabolism research.
Table 3: Essential Research Reagents and Materials for Protein Metabolism Studies
| Tool/Reagent | Function/Application | Specific Examples & Notes |
|---|---|---|
| Stable Isotope Tracers | To label amino acids and track their metabolic fate through protein breakdown, synthesis, and oxidation. | L-[ring-¹³C₆]phenylalanine, [²H₃]leucine. High chemical purity (>98%) is critical [21]. |
| Isotope Ratio Mass Spectrometry (IRMS) | To measure with high precision the enrichment of stable isotopes in biological samples (plasma, breath, tissue). | Required for accurate calculation of amino acid kinetics and oxidation rates [21]. |
| Indirect Calorimetry | To measure respiratory gas exchange (O₂ consumption, CO₂ production) for calculating energy expenditure and substrate oxidation. | Used in conjunction with leucine tracer to measure ¹³CO₂ excretion from leucine oxidation [21]. |
| Muscle Biopsy Kit | To obtain skeletal muscle tissue samples for direct measurement of fractional synthetic rate (FSR) and signaling pathway analysis. | Percutaneous needle biopsy technique; samples are immediately frozen in liquid nitrogen for analysis [110]. |
| High-Quality Protein Sources | Used as controlled interventions in dose-response and MPS studies to compare anabolic potency. | Whey protein, casein, soy protein, and specific EAA/leucine mixtures [110]. |
| Leucine Supplements | To investigate the specific role of this key amino acid in activating the mTOR signaling pathway and overcoming anabolic resistance. | Often dosed at 2.8-3.0 g per meal in experimental protocols for older adults [110]. |
This comparative analysis clearly demonstrates a significant evolution in the understanding of protein requirements, moving from the one-size-fits-all RDA of 0.8 g/kg/day to more nuanced, population-specific recommendations. The PROT-AGE and ESPEN guidelines are closely aligned, advocating for higher intakes (1.0-1.5 g/kg/day or more) for older adults and clinical populations, based on robust evidence from stable isotope and muscle protein synthesis studies.
The key differentiator lies in the underlying rationale: while the RDA aims to prevent deficiency in the general healthy population, the PROT-AGE and ESPEN guidelines are therapeutic, designed to preserve muscle mass and function, support recovery from illness, and improve clinical outcomes. This validation of differential protein requirements across populations is crucial for developing targeted nutritional interventions and informs the work of researchers and clinicians in geriatrics, metabolomics, and drug development. The ongoing refinement of experimental techniques, such as the pulse stable isotope approach, promises to further sharpen these recommendations in the future.
For decades, the nitrogen balance (NB) method has served as the foundational standard for determining human protein requirements. This approach calculates the difference between nitrogen intake (primarily from dietary protein) and nitrogen loss (in urine, feces, and sweat), with the assumption that the body is in equilibrium when intake equals loss. However, the scientific community increasingly recognizes methodological limitations and systematic biases inherent in the NB technique, prompting the development and validation of more robust biomarker-based assessment methods. The indicator amino acid oxidation (IAAO) method has emerged as a prominent alternative, relying on the principle that when one indispensable amino acid is deficient for protein synthesis, all other amino acids, including a labeled "indicator" amino acid, will be oxidized. The validation of such biomarkers extends beyond academic interest, holding direct implications for refining dietary recommendations, clinical nutrition practice, and the development of therapeutic interventions aimed at modulating protein metabolism across diverse populations.
Comparative Analysis of Methodological Performance
Quantitative Comparison of Protein Requirements
A 2025 umbrella review and meta-analysis provides the first large-scale statistical comparison of protein requirements derived from the NB and IAAO methods. The analysis, encompassing 43 NB studies (777 participants) and 17 IAAO studies (186 participants), reveals significant and systematic differences in the estimated requirements.
Table 1: Summary of Protein Requirements (g/kg/day) by Assessment Method
| Population | Nitrogen Balance (NB) Method | Indicator Amino Acid Oxidation (IAAO) Method | Percentage Difference |
|---|---|---|---|
| Non-athletes | 0.64 (95% CI: 0.61, 0.68) | 0.88 (95% CI: 0.85, 0.90) | +36% [36] |
| Athletes | 1.27 (95% CI: 1.06, 1.47) | 1.61 (95% CI: 1.44, 1.78) | +27% [36] |
The IAAO method yields protein requirements that are approximately 30% higher than those obtained via the NB method. This discrepancy is consistent across non-athletes and athletes, suggesting a fundamental systematic bias rather than a population-specific effect. In subgroup analyses of non-athletes, the IAAO values remained significantly higher regardless of age or sex, reinforcing the robustness of this finding [36]. These results challenge long-standing dietary reference intakes and underscore the critical influence of the chosen assessment biomarker on foundational nutritional science.
Technical and Methodological Limitations
The divergence in protein requirements stems from core methodological differences and limitations of the NB technique.
- Systematic Errors in NB: The NB method is prone to overestimating nitrogen retention, particularly at low nitrogen intakes, due to incomplete collection of nitrogen losses (e.g., dermal, sweat, mucosal) and the nonlinearity of nitrogen excretion as intake changes. This can lead to an underestimation of true protein needs [36].
- Physiological Basis of IAAO: The IAAO method provides a direct metabolic measure of the sufficiency of amino acid supply for protein synthesis at the cellular level. It is based on a robust biochemical principle and is less susceptible to the cumulative measurement errors that plague NB studies [36].
- Urinary Nitrogen Excretion Dynamics: Research on the temporal resolution of nitrogen excretion highlights another limitation of NB. A 2025 study demonstrated that urinary nitrogen excretion peaks significantly (2-8 hours after protein intake) and remains elevated for up to 24 hours following ingestion of a 1.2 g/kg dose of whey protein. This pattern underscores the importance of precise and timed collections, which are not always achieved in traditional NB studies, potentially leading to underestimation of losses [114].
Experimental Protocols for Key Methodologies
Indicator Amino Acid Oxidation (IAAO) Protocol
The IAAO technique is a stable isotope-based method that determines protein requirements by measuring the oxidation of a labeled amino acid when dietary protein intake is varied.
- Study Population: Typically involves healthy adults, with stringent control for age, sex, physical activity level, and health status. Participants are often provided a standardized diet for a lead-in period to stabilize background nitrogen balance.
- Tracer Administration: After an adaptation period to the experimental diet, participants receive oral doses of L-[1-13C]phenylalanine (the indicator amino acid) at regular intervals. The dietary protein level is manipulated across different study phases, typically using a crystalline amino acid diet patterned after egg protein composition.
- Sample Collection and Analysis: Breath samples are collected at baseline and throughout the tracer protocol to measure 13CO2 enrichment in exhaled air, which serves as the primary endpoint for the oxidation of the indicator amino acid. Urine samples are also collected to measure the isotopic enrichment of the tracer in urine for calculation of the fractional synthesis rate.
- Breakpoint Determination: The oxidation rate of the indicator amino acid is plotted against protein intake. The breakpoint—where oxidation begins to increase sharply—is identified using a two-phase linear regression model and represents the mean protein requirement, as intake beyond this point is no longer used for protein synthesis but is instead oxidized for energy [36].
Nitrogen Balance (NB) Protocol
The classical NB method involves a meticulous balance study to measure all sources of nitrogen intake and output.
- Dietary Control: Participants consume a controlled diet with a precisely known protein content for an adaptation period (typically 5-14 days) to allow metabolic adjustment, followed by a balance period (several days).
- Intake Measurement: All food and drink consumed are weighed, and duplicate portions are analyzed for nitrogen content, usually via the Dumas method or Kjeldahl analysis.
- Loss Collection: All urinary output is collected over a 24-hour period for the duration of the balance period and analyzed for urea nitrogen and total nitrogen. Fecal collections are made for the entire balance period, often using fecal markers (e.g., carmine red) to delineate collection periods, and analyzed for nitrogen. Additional estimations are made for miscellaneous losses (skin, sweat).
- Calculation: NB (g/day) = Nitrogen Intake - (Urinary Nitrogen + Fecal Nitrogen + Miscellaneous Nitrogen Losses). The protein requirement is then extrapolated from the intake level at which NB is zero [36] [114].
Figure 1: Experimental Workflow for Protein Requirement Assessment. This diagram illustrates the parallel pathways for the Nitrogen Balance and IAAO methodologies, culminating in a combined analysis phase.
Advanced Proteomic Biomarkers and Validation Technologies
Moving beyond whole-body protein metabolism, the field of biomarker validation is being revolutionized by advanced proteomic platforms that allow for the simultaneous measurement of hundreds to thousands of protein biomarkers with high sensitivity and specificity.
- Multiplex Immunoassays: Platforms like Meso Scale Discovery (MSD) utilize electrochemiluminescence detection to offer up to 100 times greater sensitivity than traditional ELISA. MSD's U-PLEX platform allows researchers to design custom biomarker panels, measuring multiple analytes simultaneously from a single small sample volume. This enhances efficiency and reduces costs; for example, measuring four inflammatory biomarkers with MSD costs approximately $19.20 per sample compared to $61.53 with individual ELISAs [115].
- Mass Spectrometry: Liquid chromatography tandem mass spectrometry (LC-MS/MS) provides exceptional precision and sensitivity, enabling the detection of low-abundance proteins and the analysis of hundreds to thousands of proteins in a single run. This "unbiased" approach is invaluable for biomarker discovery and rigorous validation [115].
- Large-Scale Consortia and Data Harmonization: Initiatives like the Global Neurodegeneration Proteomics Consortium (GNPC) exemplify the power of collaboration. The GNPC has established one of the world's largest harmonized proteomic datasets, comprising ~250 million protein measurements from over 35,000 biofluid samples. Such resources are critical for validating biomarkers across diverse populations and disease states [116].
- Genetic Adjustment for Enhanced Biomarkers: Emerging research suggests that removing the genetic component from plasma protein measurements can enhance their utility as disease biomarkers. A 2025 study demonstrated that genetically adjusting 94 highly heritable proteins resulted in stronger associations with disease onset in 88% of significant protein-disease pairs, effectively providing a 30% median reduction in the sample size required for comparable statistical power [117].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Reagent Solutions for Protein Biomarker Research
| Tool / Reagent | Function / Application | Key Features |
|---|---|---|
| Stable Isotope Tracers (e.g., L-[1-13C]Phenylalanine) | Metabolic tracing in IAAO studies to measure amino acid oxidation [36]. | High chemical purity, enables safe metabolic pathway tracing in humans. |
| Olink Explore Platform | High-throughput proteomic profiling for biomarker discovery and validation [118]. | Measures 3,072 proteins simultaneously, high sensitivity (CV <10%). |
| SomaScan 7K Assay | Large-scale proteomic analysis from serum or plasma samples [119]. | Quantifies ~7,000 human proteins, ideal for discovery studies. |
| Meso Scale Discovery (MSD) U-PLEX | Multiplexed immunoassay for validating specific biomarker panels [115]. | Customizable panels, broad dynamic range, cost-effective multiplexing. |
| LC-MS/MS Systems | Gold standard for precise protein identification and quantification [115]. | High specificity and sensitivity, capable of detecting post-translational modifications. |
Pathway to Clinical and Regulatory Application
The journey from biomarker discovery to regulatory qualification and clinical implementation is complex. Regulatory bodies like the FDA and EMA now advocate for a "fit-for-purpose" validation approach, where the level of evidence required is tailored to the biomarker's intended use [115]. The analytical validity of the assay itself is a major hurdle; a review of the EMA biomarker qualification procedure revealed that 77% of challenges were linked to issues with assay validity, including specificity, sensitivity, and reproducibility [115]. Successful biomarker translation, therefore, depends on a rigorous, multi-stage process that demonstrates not only analytical robustness but also a clear correlation with clinically meaningful outcomes.
Figure 2: Biomarker Development and Validation Pathway. This flowchart outlines the critical stages from initial discovery to clinical implementation, highlighting the iterative process of validation and regulatory review.
Within the broader thesis of validating differences in protein recommendations across populations, the long-term health outcomes associated with protein intake are of paramount importance. Current dietary recommendations for protein, primarily established using the nitrogen balance technique, have remained largely unchanged for decades [3] [120]. However, a growing body of evidence from modern research methodologies suggests that these recommendations may be insufficient for promoting optimal long-term health, particularly in specific populations such as older adults [31] [121] [3]. This review synthesizes evidence comparing the long-term health outcomes, including all-cause and cause-specific mortality, associated with varying levels of protein intake. We further provide detailed experimental methodologies and research tools essential for conducting research in this field, offering a practical resource for scientists and drug development professionals engaged in nutritional science and therapeutic development.
Quantitative Comparison of Protein Recommendations and Outcomes
Epidemiological and clinical studies consistently reveal associations between protein intake and long-term health outcomes. The following tables summarize key quantitative data for easy comparison, highlighting differences across populations and protein sources.
Table 1: Protein Intake Recommendations and Associated Mortality Outcomes Across Populations
| Population | Current RDA (g/kg/d) | Proposed New Recommendation (g/kg/d) | Key Mortality Findings | Study Duration / Design |
|---|---|---|---|---|
| Healthy Adults | 0.8 [31] [3] | 0.83-0.85 (EAR/RDA from meta-analysis) [4] | (Baseline for comparison) | Meta-analysis of 19 studies [4] |
| Adults ≥ 65 Years | 0.8 | 1.0–1.2 [31] [122] | — | Expert consensus [31] [122] |
| Adults ≥ 85 Years (Japanese) | — | — | Highest intake (≥19.1 %E): 56% lower risk of all-cause mortality vs. lowest intake (<14.7 %E) (HR: 0.44; 95% CI: 0.22–0.90) [121] | Prospective cohort (Avg. 3.3 years) [121] |
| Older Community-Dwelling Men (MrOS Study) | — | — | Per 2.9%E decrement: 9% increased risk of all-cause mortality (adj. HR: 1.09; 95% CI: 1.04–1.14). Association held regardless of source (dairy, animal, plant) [123] | Prospective cohort (10-year follow-up) [123] |
Table 2: Cause-Specific Mortality and Protein Source Analysis
| Health Outcome | Association with Protein Intake | Details & Hazard Ratio (HR) | Source / Study |
|---|---|---|---|
| All-Cause Mortality | Inverse association | Low protein intake associated with increased risk, irrespective of source (dairy, non-dairy animal, plant) [123]. | MrOS Study [123] |
| Cancer Mortality | Inverse association | Per 2.9%E decrement: 13% increased risk (adj. HR: 1.13; 95% CI: 1.03–1.25) [123]. | MrOS Study [123] |
| Cardiovascular Disease (CVD) Mortality | Trend towards inverse association | Per 2.9%E decrement: 8% increased risk (adj. HR: 1.08; 95% CI: 0.99–1.18) [123]. | MrOS Study [123] |
| Animal vs. Plant Protein | Varies by regional diet | In Western cohorts, higher animal protein (often red/processed meat) linked to higher CVD mortality. In Japan, higher animal protein (primarily from fish) linked to lower mortality [121]. | Kawasaki Aging and Wellbeing Project [121] |
Detailed Experimental Protocols
Understanding the evidence requires a critical examination of the key methodologies used to determine protein requirements and assess long-term outcomes.
The Nitrogen Balance Method
The nitrogen balance technique has been the historical cornerstone for setting protein recommendations, including the current RDA of 0.8 g/kg/day [4] [3]. This method measures the difference between nitrogen (a proxy for protein) intake and nitrogen losses from urine, feces, sweat, and other bodily secretions [3] [120]. The requirement is estimated as the intake at which nitrogen equilibrium (balance) is achieved.
Protocol Details:
- Controlled Diet: Participants consume a diet with a known, controlled protein content for a specific period, often 10-14 days to allow for adaptation [4] [3].
- Sample Collection: Throughout the final 5-7 days of each dietary period, all nitrogen intake is precisely measured, and all nitrogen outputs are collected. This includes total 24-hour urinary nitrogen, fecal nitrogen, and estimates of integumentary and other minor losses [4].
- Balance Calculation: Nitrogen balance is calculated as: N_balance = N_intake - (N_urine + N_feces + N_miscellaneous).
- Regression Analysis: Nitrogen balance values are plotted against nitrogen (or protein) intake levels for each individual. A statistical model (e.g., linear regression) is used to identify the intake level that predicts zero nitrogen balance (equilibrium), which is considered the average requirement (EAR) [4] [3].
Limitations: This method has several recognized limitations, including an overestimation of intake and underestimation of losses, leading to a potential underestimation of requirements. It also requires long adaptation periods and is influenced by energy intake [3] [120]. The statistical modeling of the nonlinear relationship between intake and balance has also been a point of contention [3].
The Indicator Amino Acid Oxidation (IAAO) Method
The IAAO method is now considered a gold-standard technique for estimating protein and amino acid requirements and addresses several limitations of the nitrogen balance method [122] [3] [120].
- Protocol Details:
- Dietary Manipulation: Participants are fed diets with varying levels of the test protein or amino acid, which becomes the "limiting" nutrient. All other amino acids are provided in excess.
- Isotope Tracer: A labeled isotope of a specific "indicator" amino acid (e.g., L-[1-¹³C]phenylalanine) is administered orally or intravenously.
- Measurement of Oxidation: As the intake of the limiting amino acid is below requirement, the body cannot fully utilize the indicator amino acid for protein synthesis, leading to its oxidation. The oxidized ¹³C is detected in the breath as ¹³CO₂.
- Break-Point Analysis: The excretion of ¹³CO₂ is high at low test protein intakes. As the test protein intake increases and the limiting amino acid is no longer deficient, the body utilizes more of the indicator amino acid for protein synthesis, and ¹³CO₂ excretion decreases sharply. The intake level at which this break-point occurs, identified using change-point regression models, represents the average requirement for the test protein [122].
The following diagram illustrates the logical workflow and underlying physiological principles of the IAAO method.
Prospective Cohort Studies for Long-Term Outcomes
To assess associations with mortality and morbidity, large-scale prospective cohort studies are employed.
- Protocol Details:
- Cohort Enrollment: A large population of free-living individuals is recruited, with extensive baseline data collected (e.g., demographics, health status, lifestyle factors).
- Dietary Assessment: Habitual dietary intake is assessed at baseline using validated tools such as Food Frequency Questionnaires (FFQs) or 24-hour recalls. Nutrient intake, including total protein and protein from various sources, is calculated.
- Follow-up: The cohort is followed for a pre-determined number of years (e.g., 3-10 years) to monitor for specific health outcomes, primarily all-cause and cause-specific mortality, which are often verified via death registries or medical adjudication.
- Statistical Analysis: Time-to-event analyses (e.g., Cox proportional hazards models) are used to calculate hazard ratios (HRs) for mortality across different levels of protein intake, adjusting for potential confounders like age, sex, energy intake, body weight, physical activity, and comorbidities [121] [123].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents, materials, and tools essential for conducting experimental research on protein requirements and their metabolic effects.
Table 3: Essential Research Reagents and Materials
| Item | Function / Application | Brief Explanation |
|---|---|---|
| Stable Isotope Tracers(e.g., L-[1-¹³C]Phenylalanine) | Core reagent for IAAO studies. | The non-radioactive isotopic label (¹³C) allows for safe tracing of the amino acid's metabolic fate in humans. Oxidation is measured via exhaled ¹³CO₂ [122]. |
| Amino Acid Mixtures | Formulate experimental diets of defined protein quality. | Crystalline amino acid mixtures patterned after a reference protein (e.g., egg) allow precise control over intake levels without interference from whole-food matrices [122]. |
| Indirect Calorimetry Systems | Measure metabolic rate and substrate oxidation. | Critical for measuring ¹³CO₂ enrichment in breath during IAAO studies to calculate the rate of indicator amino acid oxidation [122]. |
| Validated Food Frequency Questionnaire (FFQ) | Assess habitual dietary intake in cohort studies. | A self-administered tool with ~90 food items used to estimate habitual intake of nutrients, including protein from various sources, over the previous month [121]. |
| Bioelectrical Impedance Analysis (BIA) | Assess body composition (muscle mass). | A rapid, non-invasive method to estimate skeletal muscle mass, used as a covariate in analyses to determine if protein's effects are independent of muscle mass [121]. |
| Change-Point Regression Model (CPRM) | Statistical analysis of IAAO data. | Advanced statistical model used to identify the break-point (requirement) in IAAO data more effectively than traditional two-phase linear regression [122]. |
A comprehensive review of the evidence indicates that long-term protein intake is significantly associated with mortality risk, with current recommendations potentially underestimating the needs of older adult populations for optimal health outcomes. The convergence of data from modern methodologies like IAAO and large epidemiological cohorts provides a compelling argument for the re-evaluation of existing protein dietary guidelines. Future research must continue to refine requirement estimates using robust methodologies and further explore the interplay between protein intake, protein sources, physical activity, and long-term healthspan and quality of life. For pharmaceutical and nutritional scientists, this body of evidence underscores the importance of considering adequate protein intake as a foundational element in therapeutic strategies aimed at promoting healthy aging and preventing age-related morbidity.
Conclusion
The validation of protein recommendations across diverse populations represents a critical frontier in nutritional science and precision medicine. Evidence consistently demonstrates that a one-size-fits-all approach to protein intake is inadequate, with specific populations—particularly older adults, athletes, and those with heightened metabolic demands—requiring substantially higher and qualitatively different protein recommendations. The methodological evolution from nitrogen balance to IAAO studies and the adoption of DIAAS for protein quality assessment provide more accurate frameworks for determining true physiological requirements. Future research must prioritize large-scale intervention trials with validated functional outcomes, develop accessible tools for identifying individuals with suboptimal protein intake, and establish biomarkers that reflect protein status beyond traditional measures. For biomedical and clinical research, these advancements enable more precise nutritional support in drug development, clinical trials, and therapeutic interventions, ultimately contributing to improved healthspan, physical function, and metabolic outcomes across the lifespan.
References
- 1. Optimizing Protein Intake in Adults [https://www.sciencedirect.com/science/article/pii/S2161831322007165]
- 2. Nitrogen Balance at the Recommended Dietary Allowance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10385755/]
- 3. Is It Time to Reconsider the U.S. Recommendations ... [https://www.mdpi.com/2072-6643/15/4/838]
- 4. Meta-analysis of nitrogen balance studies for estimating ... [https://www.sciencedirect.com/science/article/pii/S0002916523055788]
- 5. Determining optimal protein intake from data, not dogmatism [https://peterattiamd.com/determining-optimal-protein-intake/]
- 6. Meeting the global protein supply requirements of a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11329409/]
- 7. Protein Intake Greater than the RDA Differentially ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7231581/]
- 8. Article Low Dietary Protein Intakes and Associated ... [https://www.sciencedirect.com/science/article/pii/S127977072300711X]
- 9. International Society of Sports Nutrition position stand: protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2117006/]
- 10. Perspective: Protein Requirements and Optimal Intakes in Aging [https://pmc.ncbi.nlm.nih.gov/articles/PMC5952928/]
- 11. Evidence-Based Recommendations for Optimal Dietary ... [https://www.sciencedirect.com/science/article/pii/S1525861013003265]
- 12. Protein and Aging: Practicalities and Practice [https://www.mdpi.com/2072-6643/17/15/2461]
- 13. How Much Protein Do Athletes Really Need? [https://www.scienceforsport.com/how-much-protein-do-athletes-really-need/?srsltid=AfmBOorGyKf02ZTrCs8LlXXqDi54Q_LRjvx3mEWg40827_Kam2S-Ku3K]
- 14. Protein – Which is Best? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3905294/]
- 15. Inference and Validation of Protein Identifications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3494198/]
- 16. How much more protein does the world need? [https://impact.economist.com/sustainability/how-much-more-protein-does-the-world-need]
- 17. Adhering to recommended dietary protein intake for optimizing ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d4ra08221d]
- 18. Gender Differences in Protein Consumption and Body ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11899518/]
- 19. Dietary protein intake and human health [https://pubmed.ncbi.nlm.nih.gov/26797090/]
- 20. Are you getting too much protein [https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/are-you-getting-too-much-protein]
- 21. A new concept to establish protein requirements [https://www.sciencedirect.com/science/article/abs/pii/S0261561425000378]
- 22. Protein intake and cardiovascular diseases: an umbrella ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350521/]
- 23. Digestible indispensable amino acid score (DIAAS) [https://pmc.ncbi.nlm.nih.gov/articles/PMC11252030/]
- 24. Potential impact of the digestible indispensable amino acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5914309/]
- 25. Digestible Indispensable Amino Acid Score [https://en.wikipedia.org/wiki/Digestible_Indispensable_Amino_Acid_Score]
- 26. And animal‐sourced proteins based on the digestible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7590266/]
- 27. Protein Nutrition: Understanding Structure, Digestibility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11171741/]
- 28. Evaluation of protein quantity and protein nutritional quality ... [https://www.nature.com/articles/s41598-025-94072-4]
- 29. Investigating the Digestibility, Bioavailability and Utilization ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609865/]
- 30. Comparison of Protein Requirements Based on the ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625005425]
- 31. Protein for Life: Review of Optimal Protein Intake, Sustainable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5872778/]
- 32. Adhering to recommended dietary protein intake for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11936105/]
- 33. Construct validity of a dietary protein assessment ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1289946/full]
- 34. The protein gap—increasing protein intake in the diet of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8883780/]
- 35. Adaptation and validation of a protein intake screening tool ... [https://pubmed.ncbi.nlm.nih.gov/36405091/]
- 36. Comparison of protein requirements based on the nitrogen ... [https://pubmed.ncbi.nlm.nih.gov/40914512/]
- 37. Evaluation of protein requirements using the indicator ... [https://www.sciencedirect.com/science/article/pii/S0022316623725297]
- 38. Dietary Protein Requirements of Older Adults with ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1486482/abstract]
- 39. Indicator Amino Acid Oxidation: Concept and Application,, [https://www.sciencedirect.com/science/article/pii/S0022316622095323]
- 40. Indicator amino acid oxidation: concept and application [https://pubmed.ncbi.nlm.nih.gov/18203885/]
- 41. The indicator amino acid oxidation (IAAO) technique [https://pubmed.ncbi.nlm.nih.gov/40748779/]
- 42. A scoping review of the application of the indicator amino ... [https://pubmed.ncbi.nlm.nih.gov/41294219/]
- 43. Discussion - Evaluation of Dietary Protein and Amino Acid ... [https://www.ncbi.nlm.nih.gov/books/NBK614612/]
- 44. Adaptation and validation of a protein intake screening tool ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9672832/]
- 45. The Protein Screener 55+ (Pro55+) | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0196406]
- 46. Validation of the German version of the Protein Screener 55+ [https://www.nature.com/articles/s41430-023-01266-y]
- 47. A Systematic Review and Meta-Analysis of Validation ... [https://www.sciencedirect.com/science/article/pii/S2161831322005099]
- 48. Validity of Dietary Assessment Methods When Compared ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00850/full]
- 49. A Review of Protein Quality Metrics and Their Applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC8912699/]
- 50. The Spectrum of Protein Quality [https://www.glanbianutritionals.com/en/nutri-knowledge-center/nutritional-resources/spectrum-protein-quality]
- 51. EFAD call for volunteers in FAO project in advancing ... [https://www.efad.org/efad-call-for-volunteers-in-fao-project-in-advancing-protein-quality-assessment/]
- 52. Comparison of the Effectiveness of Protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0022316625000240]
- 53. The effectiveness of protein supplementation combined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369567/]
- 54. Protein supplementation augments the adaptive response ... [https://www.sciencedirect.com/science/article/pii/S0002916523029271]
- 55. Effect of Protein Supplementation Combined With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280458/]
- 56. A Randomized, Comparator-Controlled, Parallel Clinical Trial [https://www.mdpi.com/2072-6643/16/13/2017]
- 57. The response of muscle protein synthesis following whole-body... [https://pubmed.ncbi.nlm.nih.gov/27511985/]
- 58. The impact of protein quality on the promotion of resistance ... [https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-016-0124-8]
- 59. The Future Landscape and Framework of Precision Nutrition [https://www.sciencedirect.com/science/article/pii/S2095809924000754]
- 60. Precision nutrition: Is tailor‑made dietary intervention a reality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11956147/]
- 61. Minimum days estimation for reliable dietary intake ... [https://www.nature.com/articles/s41430-025-01644-8]
- 62. Validation of REFRESH: A Dietary Screener for Rapid ... [https://pubmed.ncbi.nlm.nih.gov/40419094/]
- 63. The Dietary Biomarkers Development Consortium [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242990/]
- 64. Understanding Dietary Protein Quality: Digestible ... [https://www.sciencedirect.com/science/article/pii/S0022316625004286]
- 65. Development and validation of a nutrition assessment ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2025.1474815/full]
- 66. Current advancements in alternative protein sources: Plant ... [https://www.sciencedirect.com/science/article/abs/pii/S2212429225018851]
- 67. Protein Showdown: Comparison of Plant-Based and Animal ... [https://fieldreport.caes.uga.edu/publications/B1575/protein-showdown-comparison-of-plant-based-and-animal-based-foods/]
- 68. Comparing the nutrient composition of plant-based meat ... [https://www.sciencedirect.com/science/article/pii/S0889157525006568]
- 69. Future protein foods: plant versus animal sources, nutrient ... [https://www.frontiersin.org/journals/science/articles/10.3389/fsci.2025.1671189/full]
- 70. Alternative proteins: innovations in sources, processing ... [https://www.frontiersin.org/journals/sustainable-food-systems/articles/10.3389/fsufs.2025.1641712/full]
- 71. Current challenges of alternative proteins as future foods [https://www.nature.com/articles/s41538-024-00291-w]
- 72. Age-related muscle anabolic resistance: inevitable or ... [https://pubmed.ncbi.nlm.nih.gov/36018750/]
- 73. Keeping Older Muscle “Young” through Dietary Protein and ... [https://www.sciencedirect.com/science/article/pii/S2161831322008924]
- 74. Critical variables regulating age-related anabolic ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1419229/full]
- 75. Anabolic Resistance in the Pathogenesis of Sarcopenia ... [https://www.mdpi.com/2072-6643/15/18/4073]
- 76. Age-Related Anabolic Resistance: Nutritional and Exercise ... [https://www.mdpi.com/2072-6643/17/22/3503]
- 77. Protein Consumption and the Elderly: What Is the Optimal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4924200/]
- 78. Muscle loss and protein needs in older adults [https://www.health.harvard.edu/staying-healthy/muscle-loss-and-protein-needs-in-older-adults]
- 79. Protein requirements: Where are we now and where do ... [https://www.arlafoodsingredients.com/the-whey-and-protein-blog/research/protein-requirements-where-are-we-now-and-where-do-we-go-from-here/]
- 80. Assessing Muscle Protein Synthesis Rates In Vivo in Humans [https://www.sciencedirect.com/science/article/pii/S0022316624010290]
- 81. Timing and distribution of protein ingestion during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3650697/]
- 82. Nutrition and muscle protein synthesis: a descriptive review [https://pmc.ncbi.nlm.nih.gov/articles/PMC2732256/]
- 83. Dietary Protein Distribution Positively Influences 24-h ... [https://www.sciencedirect.com/science/article/pii/S0022316622009087]
- 84. The effect of protein timing on muscle strength and hypertrophy [https://jissn.biomedcentral.com/articles/10.1186/1550-2783-10-53]
- 85. Timing matters? The effects of two different timing of high ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2024.1397090/full]
- 86. Meeting the global protein supply requirements of a ... [https://link.springer.com/article/10.1007/s00394-024-03358-2]
- 87. Protein intake trends and conformity with the Dietary ... [https://www.sciencedirect.com/science/article/pii/S0002916522029215]
- 88. Age and Racial/Ethnic Differences in Dietary Sources of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7333060/]
- 89. Enhanced validation of antibodies for research applications [https://www.nature.com/articles/s41467-018-06642-y]
- 90. Behavioral interventions to motivate plant-based food ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11648632/]
- 91. Protein Biomarker Discovery & Validation [https://www.thermofisher.com/us/en/home/clinical/clinical-translational-research/protein-analysis/protein-biomarker-discovery-validation.html]
- 92. Assessing protein needs for performance [https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/assessing-protein-needs-for-performance]
- 93. Clinical Evidence and Mechanisms of High-Protein Diet ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7539343/]
- 94. Dietary Protein and Energy Balance in Relation to Obesity ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00443/full]
- 95. A randomized cross-over trial to determine the effect of a ... [https://nutritionj.biomedcentral.com/articles/10.1186/s12937-019-0497-4]
- 96. Environmental Sustainability [https://www.rush.edu/about-us/environmental-sustainability]
- 97. The impact of nutritional intervention and resistance training ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12400859/]
- 98. Effects of protein supplementation on muscle mass, muscle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11978179/]
- 99. Protein supplementation improves muscle mass and ... [https://www.sciencedirect.com/science/article/pii/S0002916522030313]
- 100. Comparative Effectiveness of Exercise, Protein ... [https://www.mdpi.com/2072-6643/17/15/2392]
- 101. a systematic review and meta-analysis [https://www.e-epih.org/journal/view.php?doi=10.4178/epih.e2024030]
- 102. Comparative Effectiveness of Exercise and Protein-Based ... [https://www.sciencedirect.com/science/article/pii/S127977072500243X]
- 103. Relationship between different muscle mass indices and ... [https://bmcgeriatr.biomedcentral.com/articles/10.1186/s12877-024-05418-y]
- 104. Muscle mass, strength, and physical performance predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7015244/]
- 105. Measuring Muscle Mass and Strength in Obesity: a Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7808984/]
- 106. Dietary protein intake, protein sources & distribution ... [https://www.sciencedirect.com/science/article/pii/S0261561425000585]
- 107. Is There a Need to Reassess Protein Intake ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11779789/]
- 108. How much protein do you need every day? [https://www.health.harvard.edu/blog/how-much-protein-do-you-need-every-day-201506188096]
- 109. Protein: What's Enough? [https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/protein-and-heart-health]
- 110. Protein and Aging: Practicalities and Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12348035/]
- 111. Evidence-based recommendations for optimal dietary protein ... [https://researchexperts.utmb.edu/en/publications/evidence-based-recommendations-for-optimal-dietary-protein-intake/]
- 112. ESPEN Scientific Guidelines (PDF Versions) [https://www.espen.org/guidelines/espen-scientific-guidelines-pdf-versions]
- 113. ESPEN guideline on clinical nutrition in surgery [https://pubmed.ncbi.nlm.nih.gov/40957230/]
- 114. Effect of high intakes of protein-only and carbohydrate ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1618142/full]
- 115. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 116. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 117. Removing genetic effects on plasma proteins enhances ... [https://www.medrxiv.org/content/10.1101/2025.10.14.25337894v1]
- 118. A plasma proteomics-based candidate biomarker panel ... [https://www.nature.com/articles/s41591-025-03890-6]
- 119. Large-scale serum protein biomarkers discovery ... [https://www.nature.com/articles/s41467-025-64146-y]
- 120. Is It Time to Reconsider the U.S. Recommendations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9963165/]
- 121. Dietary protein intake and all-cause mortality [https://pmc.ncbi.nlm.nih.gov/articles/PMC10413626/]
- 122. Estimation of inter-individual variability of protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7844655/]
- 123. Low Protein Intake Irrespective of Source is Associated ... [https://www.sciencedirect.com/science/article/pii/S1279770723012630]